Nitric Oxide in the Preterm systematic reviews Keith


- Slides: 36
Nitric Oxide in the Preterm: systematic reviews Keith J Barrington CHU Sainte Justine Montréal Canada
The systematic review Update of the Cochrane Review 13 RCTs of i. NO in preterm infants with respiratory disease Varying eligibility, age of use, indications, dose, duration. Decided Post Hoc to divide them into 3 groups Early rescue Late ‘rescue’ Early routine treatment
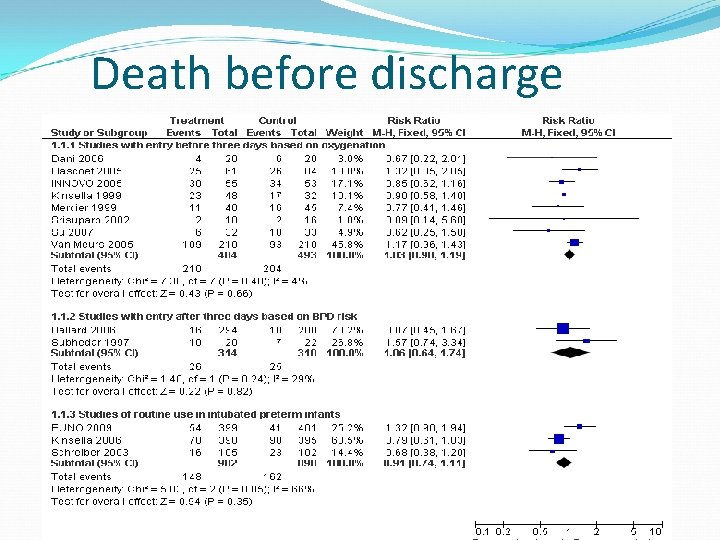
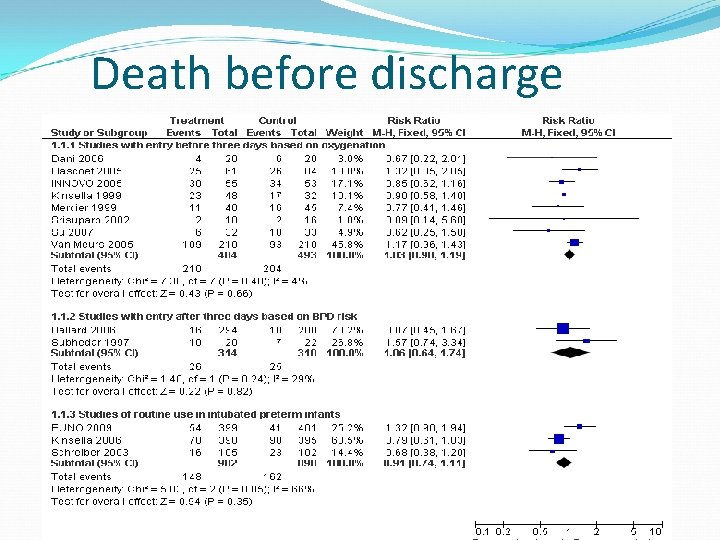
Death before discharge
Mortality None of the individual trials show a statistically significant reduction. Meta-analysis of the first 2 trials of early routine use previously showed potential difference: which was marginally significant. Potentially important magnitude of effect, but the estimate lacked precision. Adding the data from the abstract of the EUNO trial: now no difference, RR 0. 91 (95% CI 0. 74, 1. 11) The early rescue, and later treatment in infants at risk of BPD groups show no effect on mortality.
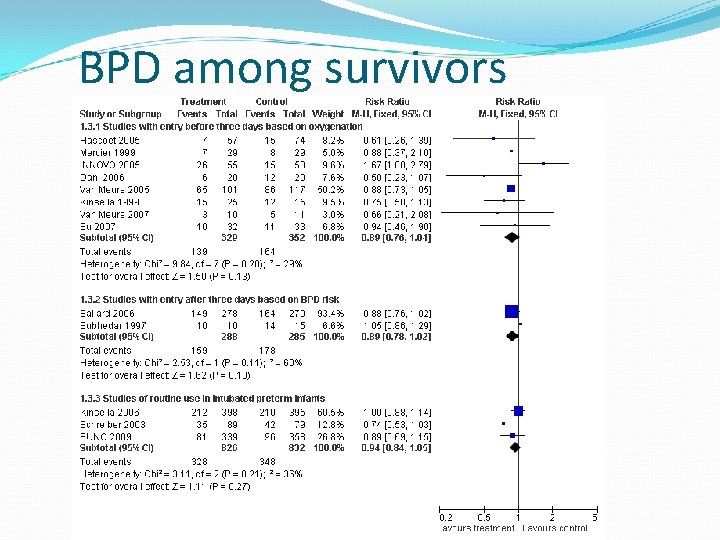
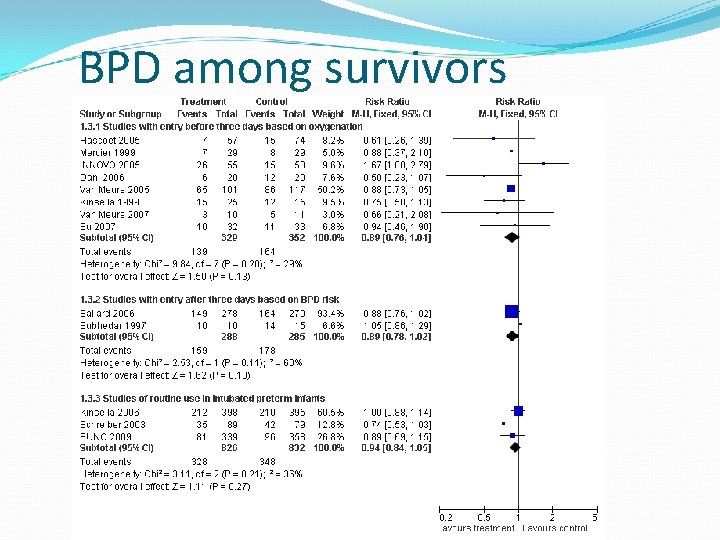
BPD among survivors

Death or BPD
Survival without bronchopulmonary dysplasia Early rescue treatment studies: no apparent benefit subgroup analysis of Van Meurs et al reduction in infants > 1 kg birthweight. Early routine treatment: modest and almost significant reduction in the combined outcome of death or BPD RR 0. 93, 95% CI 0. 86 1. 01. Heterogeneity I 2 = 34%, Kinsella + EUNO: no benefit. Subgroup analysis of Kinsella suggested lower risk infants (BW >1000 g) had a benefit. In Schreiber, subgroup analysis suggested only the less sick infants (OI less than the median) benefited.
Survival without bronchopulmonary dysplasia Ballard et al report: significant benefit of inhaled nitric in improving survival without BPD. However the figures given, 165/294 vs. 182/288 are not significant using Rev. Man to calculate RR. Difference due to use of multiple outputation as planned, a statistical way of correcting for possible coherence among multiples, (1 st of multiples to be eligible randomized, therefore entered as a cluster, should be analyzed as a cluster). Subgroup analysis: reduction in combined death or BPD when started at 7 - 14 d, less severe disease may increase chance of benefit.
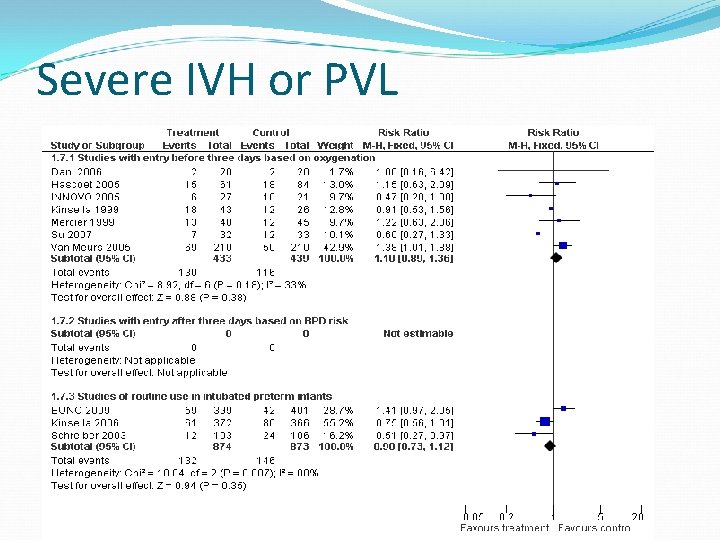
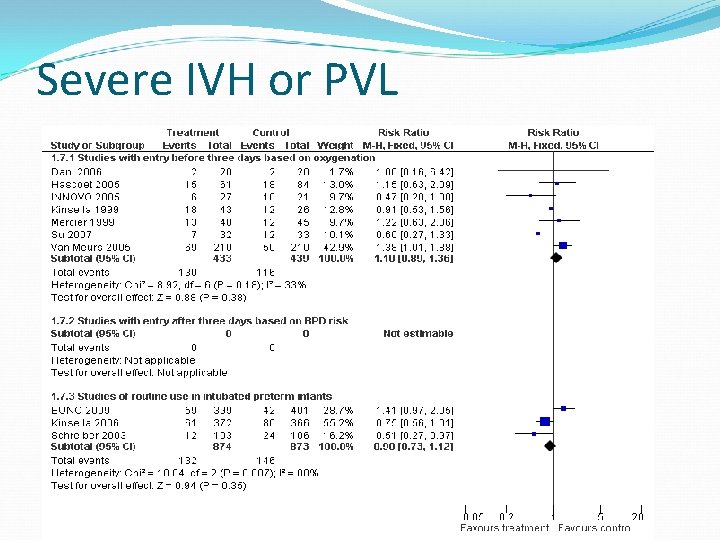
Severe IVH or PVL
Brain Injury Early rescue studies: no significant effect, the direction of the difference is toward increased serious IVH Not significant at p<0. 05, BUT potential evidence of harm should always be taken seriously, especially when there is no evidence of benefit. Later entry based on BPD risk not expected to affect IVH incidence. With the addition of EUNO 2009, early routine use shows no effect on brain injury, either severe IVH or combined outcome of severe IVH or PVL. Heterogeneity I 2= 80%

Brain Injury Previous analysis suggested a potential benefit in the early routine treatment group EUNO had a higher baseline OI, but a lower mortality than the other early routine treatment trials, Do these characteristics explain the difference, or is it just chance?
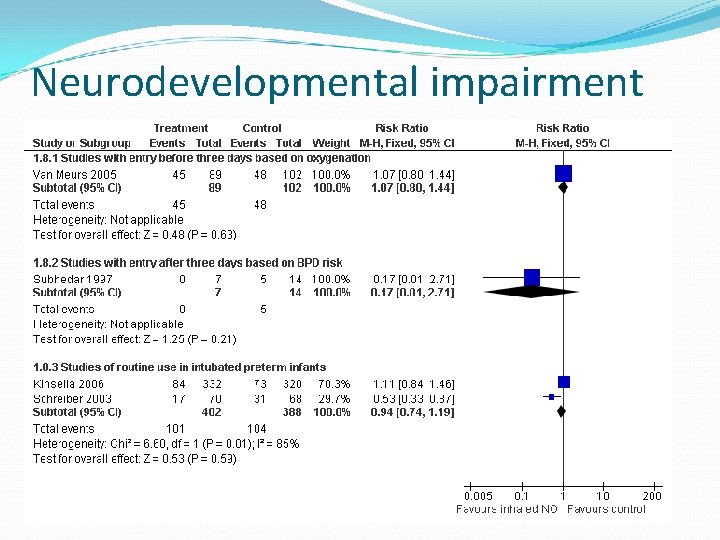
Neurodevelopmental impairment
Sensitivity analysis I have performed a sensitivity analysis of the early rescue treatment studies, eliminating the studies with very early primary outcomes, the studies with potential crossover, and studies with very small samples Analyses including Innovo, Kinsella 1999, and Van Meurs 2005, total n=566 Conclusions are substantially unchanged
Problems with the meta-analysis Great variation in study design Different eligibility criteria Postnatal age severity of illness criteria Different primary outcomes Variable duration of therapy Variable doses
IPD meta-analysis The standard review and meta-analysis suggested that there might be significant benefits in certain groups of infants: But no clear indications for therapy were evident Don’t want to miss benefits Nor potential harms In some groups of infants
IPD meta-analysis Obtaining original information on all the enrolled subjects Allows: Intention to treat analysis Consistency of definitions (if enough information was collected) Analyses of subgroups across trials Identification of patient characteristics associated with positive or negative responses
Meta Analysis of Preterm Patients on inhaled Nitric Oxide Collaboration Inhaled nitric oxide in preterm infants: a systematic review and individual patient data meta-analysis
MAPPi. NO aims/objectives • • To determine whether inhaled nitric oxide in preterm infants receiving assisted ventilation improves survival without morbidity, specifically without: – CLD – cerebral injury – retinal injury – long-term disability To determine whether the effects of inhaled nitric oxide differ according to the risk profile of the patient in terms of: – gestational age at birth – severity of illness – antenatal steroid use – postnatal age at the time of randomization – ventilation mode at randomization – administration of exogenous surfactant – inhaled nitric dosage and duration of nitric oxide administration
Reasons for IPD in MAPPi. NO • determine whether certain patient or treatment characteristics may predict benefit from inhaled nitric oxide in the premature infants (patientlevel subgroup analyses) • define CLD the same way across trials • aim to analyse all endpoints in all patients in all trials, to avoid biases associated with selective publication endpoints • address additional research questions • improve trial identification, interpretation & dissemination via collaborative approach
Results: a general approach • main analyses used log-binomial regression models adjusted for trial • subgroup analyses used poisson regression models with robust error variance due to issues with model convergence • endpoints between siblings from multiple births • the primary analyses were adjusted for multiple births using the multiple outputation approach (1000 repetitions) • sensitivity analysis: generalized estimating equations (GEE) used to analyse the two main endpoints of interest
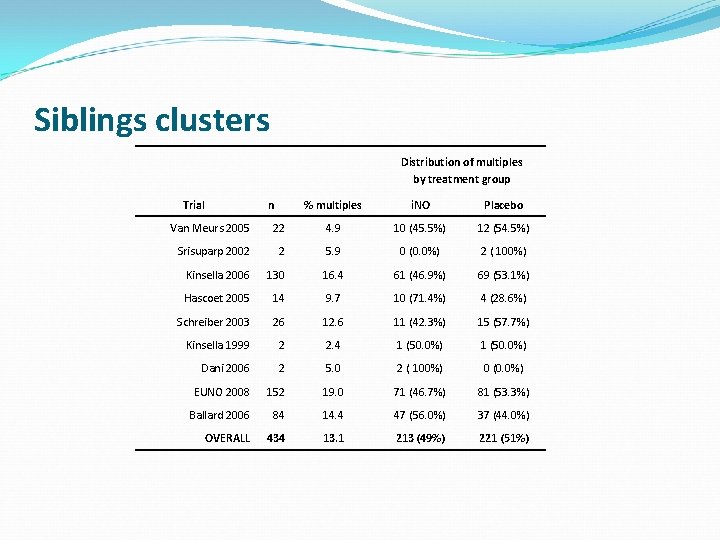
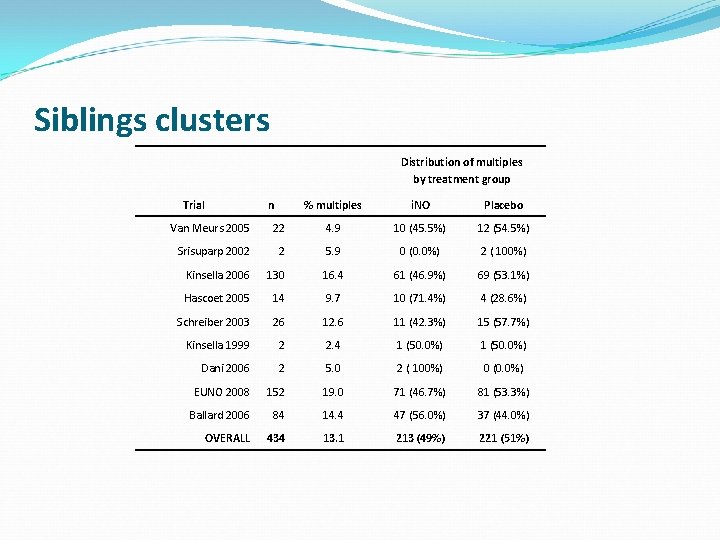
Siblings clusters Distribution of multiples by treatment group Trial n % multiples i. NO Placebo Van Meurs 2005 22 4. 9 10 (45. 5%) 12 (54. 5%) Srisuparp 2002 2 5. 9 0 (0. 0%) 2 ( 100%) Kinsella 2006 130 16. 4 61 (46. 9%) 69 (53. 1%) Hascoet 2005 14 9. 7 10 (71. 4%) 4 (28. 6%) Schreiber 2003 26 12. 6 11 (42. 3%) 15 (57. 7%) Kinsella 1999 2 2. 4 1 (50. 0%) Dani 2006 2 5. 0 2 ( 100%) 0 (0. 0%) EUNO 2008 152 19. 0 71 (46. 7%) 81 (53. 3%) Ballard 2006 84 14. 4 47 (56. 0%) 37 (44. 0%) OVERALL 434 13. 1 213 (49%) 221 (51%)
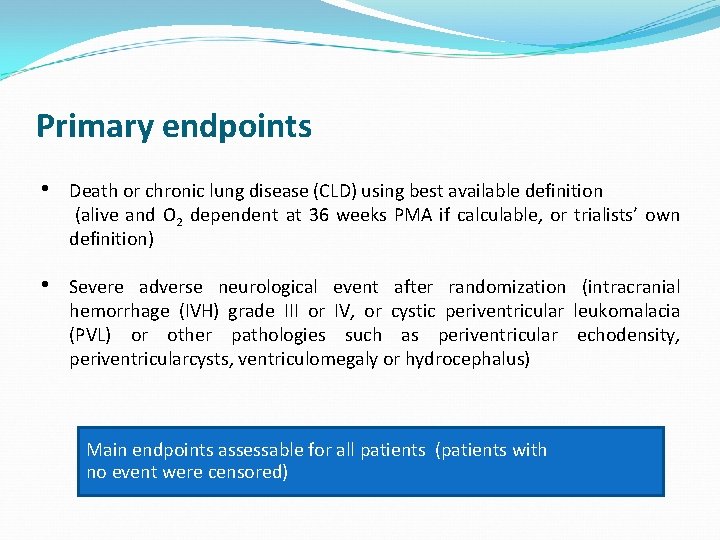
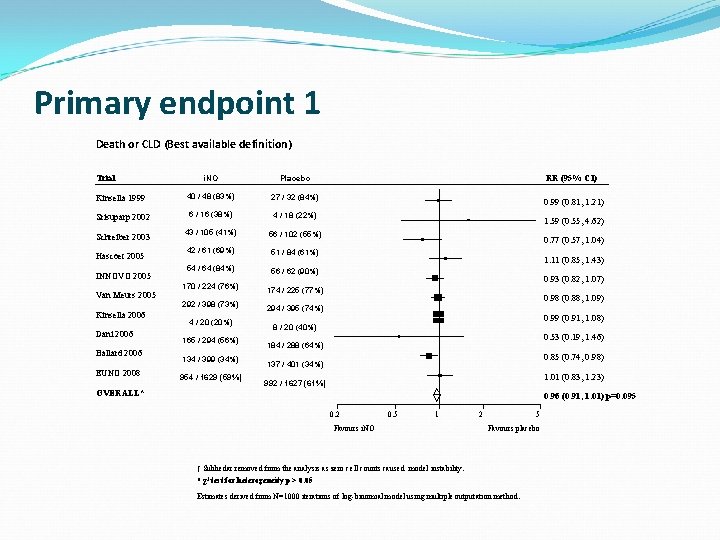
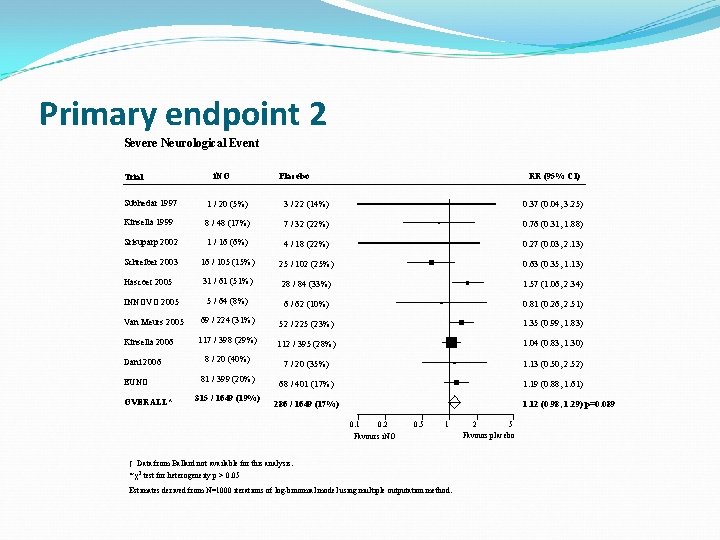
Primary endpoints • Death or chronic lung disease (CLD) using best available definition (alive and O 2 dependent at 36 weeks PMA if calculable, or trialists’ own definition) • Severe adverse neurological event after randomization (intracranial hemorrhage (IVH) grade III or IV, or cystic periventricular leukomalacia (PVL) or other pathologies such as periventricular echodensity, periventricularcysts, ventriculomegaly or hydrocephalus) Main endpoints assessable for all patients (patients with no event were censored)
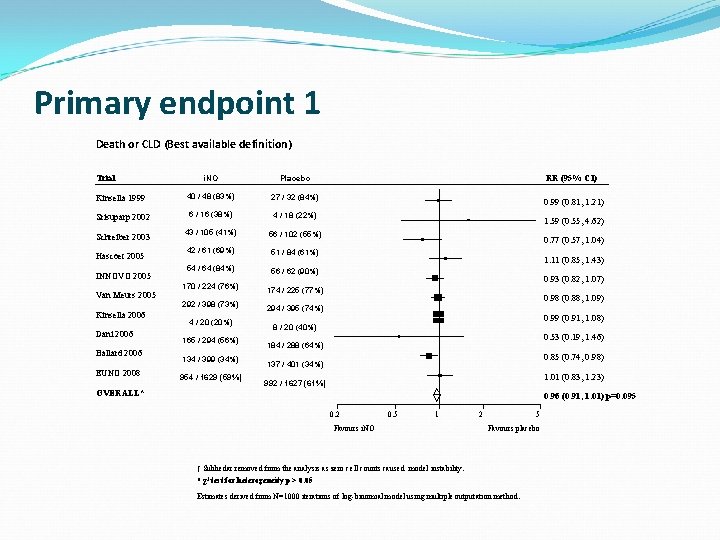
Primary endpoint 1 Death or CLD (Best available definition) i. NO Placebo Kinsella 1999 40 / 48 (83%) 27 / 32 (84%) Srisuparp 2002 6 / 16 (38%) 4 / 18 (22%) Schreiber 2003 43 / 105 (41%) 56 / 102 (55%) 42 / 61 (69%) 51 / 84 (61%) 54 / 64 (84%) 56 / 62 (90%) 170 / 224 (76%) 174 / 225 (77%) 292 / 398 (73%) 294 / 395 (74%) Trial Hascoet 2005 INNOVO 2005 Van Meurs 2005 Kinsella 2006 Dani 2006 Ballard 2006 EUNO 2008 4 / 20 (20%) 165 / 294 (56%) 134 / 399 (34%) 954 / 1629 (59%) RR (95% CI) 0. 99 (0. 81, 1. 21) 1. 59 (0. 55, 4. 62) 0. 77 (0. 57, 1. 04) 1. 11 (0. 85, 1. 43) 0. 93 (0. 82, 1. 07) 0. 98 (0. 88, 1. 09) 0. 99 (0. 91, 1. 08) 8 / 20 (40%) 0. 53 (0. 19, 1. 46) 184 / 288 (64%) 0. 85 (0. 74, 0. 98) 137 / 401 (34%) 1. 01 (0. 83, 1. 23) 992 / 1627 (61%) OVERALL* 0. 96 (0. 91, 1. 01) p=0. 095 0. 2 0. 5 1 Favours i. NO 2 5 Favours placebo † Subhedar removed from the analysis as zero cell counts caused model instability. * χ2 test for heterogeneity p > 0. 05 Estimates derived from N=1000 iterations of log-binomial model using multiple outputation method.
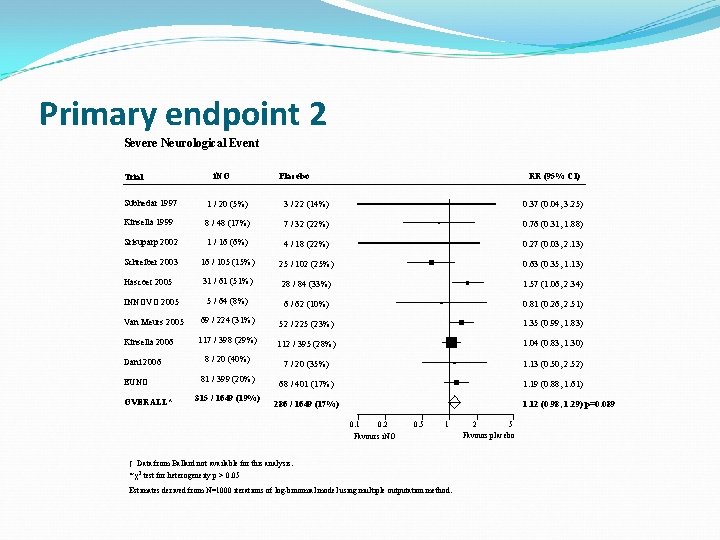
Primary endpoint 2 Severe Neurological Event Trial i. NO Placebo RR (95% CI) Subhedar 1997 1 / 20 (5%) 3 / 22 (14%) 0. 37 (0. 04, 3. 25) Kinsella 1999 8 / 48 (17%) 7 / 32 (22%) 0. 76 (0. 31, 1. 88) Srisuparp 2002 1 / 16 (6%) 4 / 18 (22%) 0. 27 (0. 03, 2. 13) Schreiber 2003 16 / 105 (15%) 25 / 102 (25%) 0. 63 (0. 35, 1. 13) Hascoet 2005 31 / 61 (51%) 28 / 84 (33%) 1. 57 (1. 06, 2. 34) INNOVO 2005 5 / 64 (8%) 6 / 62 (10%) 0. 81 (0. 26, 2. 51) Van Meurs 2005 69 / 224 (31%) 52 / 225 (23%) 1. 35 (0. 99, 1. 83) Kinsella 2006 117 / 398 (29%) 112 / 395 (28%) 1. 04 (0. 83, 1. 30) 8 / 20 (40%) 7 / 20 (35%) 1. 13 (0. 50, 2. 52) 68 / 401 (17%) 1. 19 (0. 88, 1. 61) Dani 2006 EUNO OVERALL* 81 / 399 (20%) 315 / 1649 (19%) 286 / 1649 (17%) 1. 12 (0. 98, 1. 29) p=0. 089 0. 1 0. 2 0. 5 1 Favours i. NO † Data from Ballard not available for this analysis. * χ2 test for heterogeneity p > 0. 05 Estimates derived from N=1000 iterations of log-binomial model using multiple outputation method. 2 5 Favours placebo
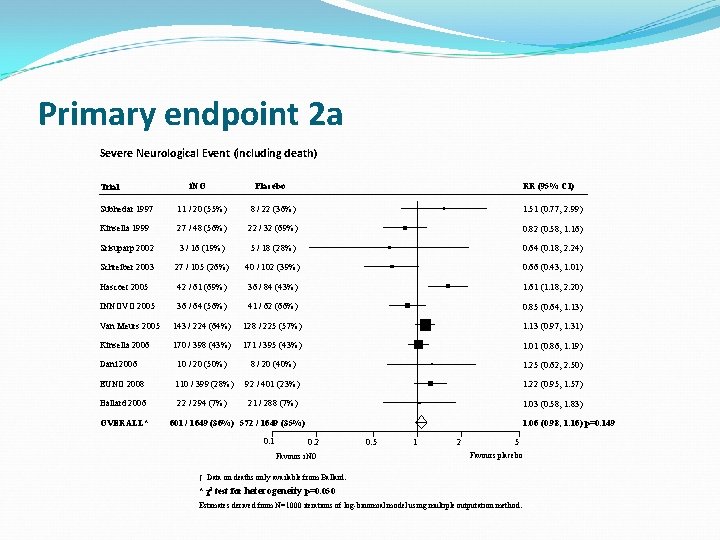
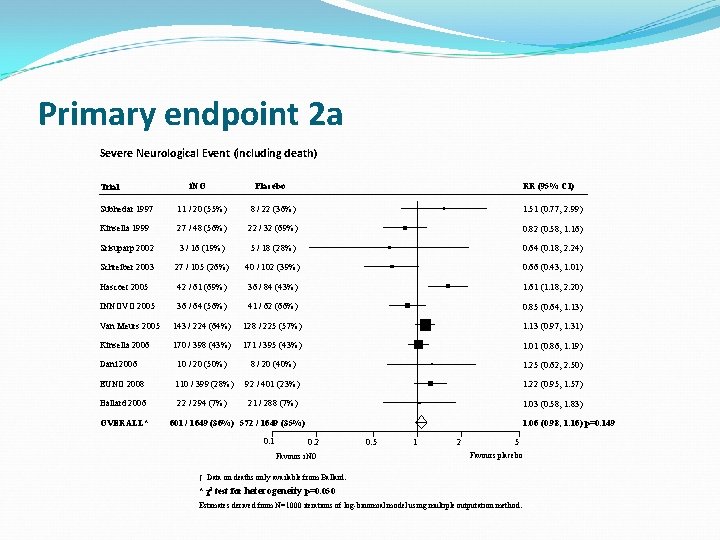
Primary endpoint 2 a Severe Neurological Event (including death) Trial i. NO Placebo RR (95% CI) Subhedar 1997 11 / 20 (55%) 8 / 22 (36%) 1. 51 (0. 77, 2. 99) Kinsella 1999 27 / 48 (56%) 22 / 32 (69%) 0. 82 (0. 58, 1. 16) Srisuparp 2002 3 / 16 (19%) 5 / 18 (28%) 0. 64 (0. 18, 2. 24) Schreiber 2003 27 / 105 (26%) 40 / 102 (39%) 0. 66 (0. 43, 1. 01) Hascoet 2005 42 / 61 (69%) 36 / 84 (43%) 1. 61 (1. 18, 2. 20) INNOVO 2005 36 / 64 (56%) 41 / 62 (66%) 0. 85 (0. 64, 1. 13) Van Meurs 2005 143 / 224 (64%) 128 / 225 (57%) 1. 13 (0. 97, 1. 31) Kinsella 2006 170 / 398 (43%) 171 / 395 (43%) 1. 01 (0. 86, 1. 19) Dani 2006 10 / 20 (50%) 8 / 20 (40%) 1. 25 (0. 62, 2. 50) EUNO 2008 110 / 399 (28%) 92 / 401 (23%) 1. 22 (0. 95, 1. 57) Ballard 2006 22 / 294 (7%) 21 / 288 (7%) 1. 03 (0. 58, 1. 83) OVERALL* 601 / 1649 (36%) 572 / 1649 (35%) 0. 1 1. 06 (0. 98, 1. 16) p=0. 149 0. 2 Favours i. NO 0. 5 1 2 5 Favours placebo † Data on deaths only available from Ballard. * χ2 test for heterogeneity p=0. 050 Estimates derived from N=1000 iterations of log-binomial model using multiple outputation method.
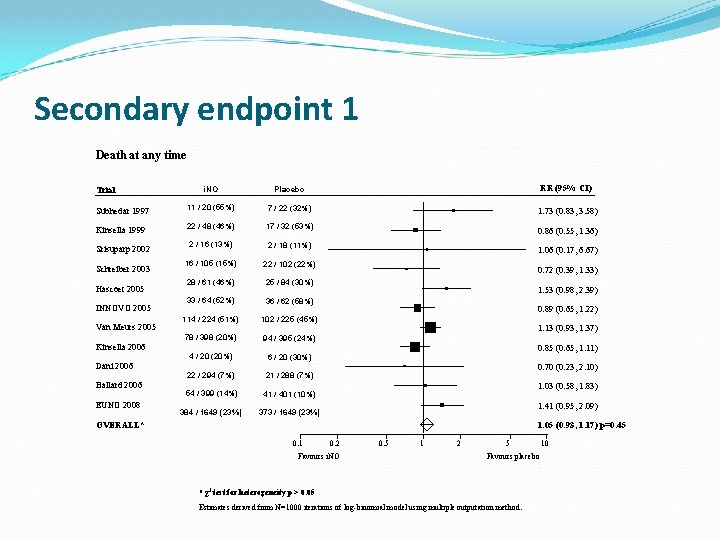
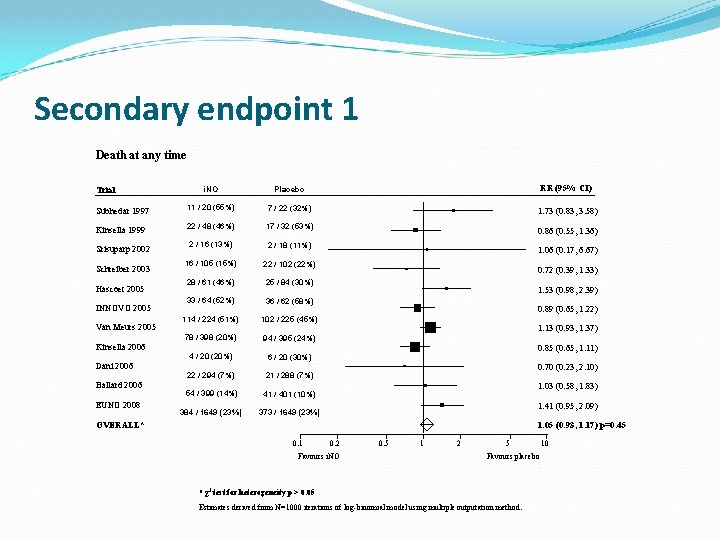
Secondary endpoint 1 Death at any time i. NO Placebo RR (95% CI) Subhedar 1997 11 / 20 (55%) 7 / 22 (32%) 1. 73 (0. 83, 3. 58) Kinsella 1999 22 / 48 (46%) 17 / 32 (53%) 2 / 16 (13%) 2 / 18 (11%) 16 / 105 (15%) 22 / 102 (22%) 28 / 61 (46%) 25 / 84 (30%) 33 / 64 (52%) 36 / 62 (58%) 114 / 224 (51%) 102 / 225 (45%) 78 / 398 (20%) 94 / 395 (24%) 4 / 20 (20%) 6 / 20 (30%) 22 / 294 (7%) 21 / 288 (7%) 54 / 399 (14%) 41 / 401 (10%) 384 / 1649 (23%) 373 / 1649 (23%) Trial Srisuparp 2002 Schreiber 2003 Hascoet 2005 INNOVO 2005 Van Meurs 2005 Kinsella 2006 Dani 2006 Ballard 2006 EUNO 2008 0. 86 (0. 55, 1. 36) 1. 06 (0. 17, 6. 67) 0. 72 (0. 39, 1. 33) 1. 53 (0. 98, 2. 39) 0. 89 (0. 65, 1. 22) 1. 13 (0. 93, 1. 37) 0. 85 (0. 65, 1. 11) 0. 70 (0. 23, 2. 10) 1. 03 (0. 58, 1. 83) 1. 41 (0. 95, 2. 09) OVERALL* 1. 05 (0. 93, 1. 17) p=0. 45 0. 1 0. 2 Favours i. NO 0. 5 1 2 5 Favours placebo * χ2 test for heterogeneity p > 0. 05 Estimates derived from N=1000 iterations of log-binomial model using multiple outputation method. 10
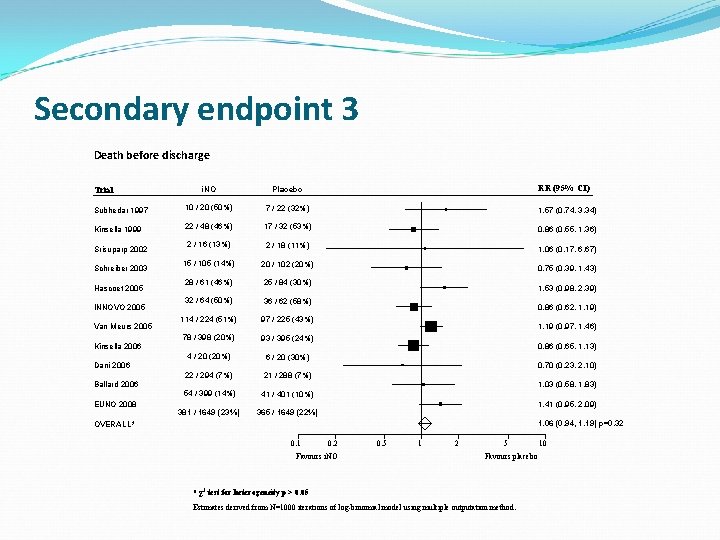
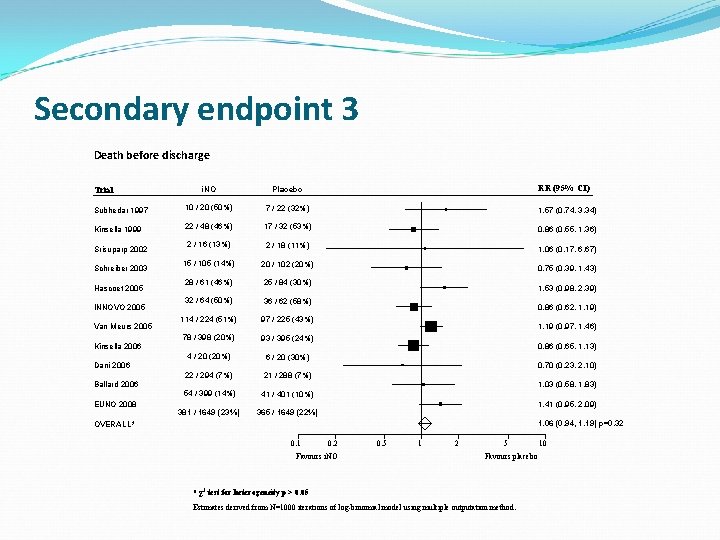
Secondary endpoint 3 Death before discharge RR (95% CI) i. NO Placebo Subhedar 1997 10 / 20 (50%) 7 / 22 (32%) 1. 57 (0. 74, 3. 34) Kinsella 1999 22 / 48 (46%) 17 / 32 (53%) 0. 86 (0. 55, 1. 36) 2 / 16 (13%) 2 / 18 (11%) 1. 06 (0. 17, 6. 67) 15 / 105 (14%) 20 / 102 (20%) 28 / 61 (46%) 25 / 84 (30%) 32 / 64 (50%) 36 / 62 (58%) 114 / 224 (51%) 97 / 225 (43%) 78 / 398 (20%) 93 / 395 (24%) 4 / 20 (20%) 6 / 20 (30%) 22 / 294 (7%) 21 / 288 (7%) 54 / 399 (14%) 41 / 401 (10%) 381 / 1649 (23%) 365 / 1649 (22%) Trial Srisuparp 2002 Schreiber 2003 Hascoet 2005 INNOVO 2005 Van Meurs 2005 Kinsella 2006 Dani 2006 Ballard 2006 EUNO 2008 0. 75 (0. 39, 1. 43) 1. 53 (0. 98, 2. 39) 0. 86 (0. 62, 1. 19) 1. 19 (0. 97, 1. 46) 0. 86 (0. 65, 1. 13) 0. 70 (0. 23, 2. 10) 1. 03 (0. 58, 1. 83) 1. 41 (0. 95, 2. 09) 1. 06 (0. 94, 1. 19) p=0. 32 OVERALL* 0. 1 0. 2 Favours i. NO 0. 5 1 2 5 Favours placebo * χ2 test for heterogeneity p > 0. 05 Estimates derived from N=1000 iterations of log-binomial model using multiple outputation method. 10
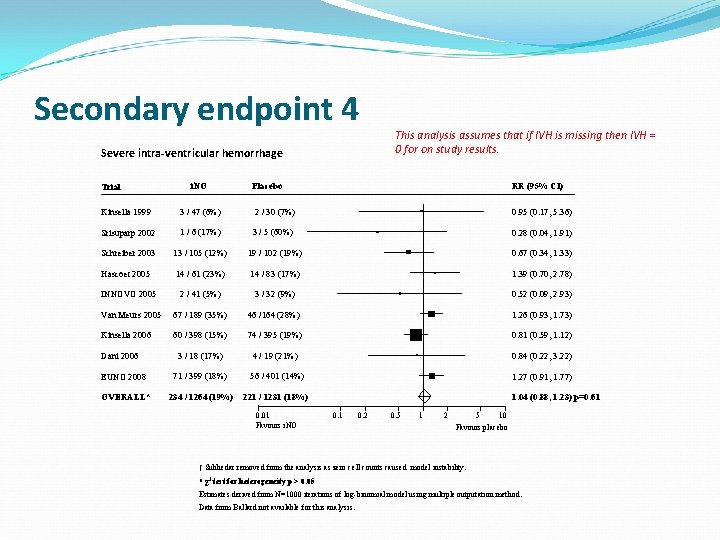
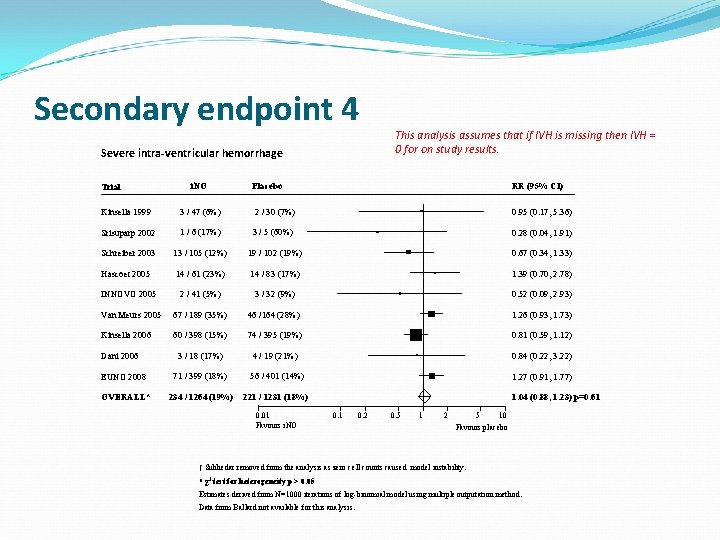
Secondary endpoint 4 Severe intra-ventricular hemorrhage Trial i. NO This analysis assumes that if IVH is missing then IVH = 0 for on study results. Placebo RR (95% CI) Kinsella 1999 3 / 47 (6%) 2 / 30 (7%) 0. 95 (0. 17, 5. 36) Srisuparp 2002 1 / 6 (17%) 3 / 5 (60%) 0. 28 (0. 04, 1. 91) Schreiber 2003 13 / 105 (12%) 19 / 102 (19%) 0. 67 (0. 34, 1. 33) Hascoet 2005 14 / 61 (23%) 14 / 83 (17%) 1. 39 (0. 70, 2. 78) INNOVO 2005 2 / 41 (5%) 3 / 32 (9%) 0. 52 (0. 09, 2. 93) Van Meurs 2005 67 / 189 (35%) 46 /164 (28%) 1. 26 (0. 93, 1. 73) Kinsella 2006 60 / 398 (15%) 74 / 395 (19%) 0. 81 (0. 59, 1. 12) 3 / 18 (17%) 4 / 19 (21%) 0. 84 (0. 22, 3. 22) EUNO 2008 71 / 399 (18%) 56 / 401 (14%) 1. 27 (0. 91, 1. 77) OVERALL* 234 / 1264 (19%) 221 / 1231 (18%) Dani 2006 0. 01 Favours i. NO 1. 04 (0. 88, 1. 23) p=0. 61 0. 2 0. 5 1 2 5 10 Favours placebo † Subhedar removed from the analysis as zero cell counts caused model instability. * χ2 test for heterogeneity p > 0. 05 Estimates derived from N=1000 iterations of log-binomial model using multiple outputation method. Data from Ballard not available for this analysis.
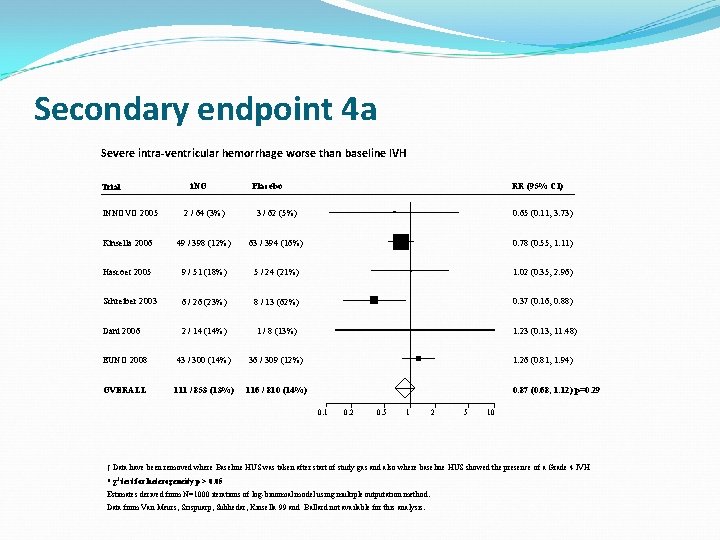
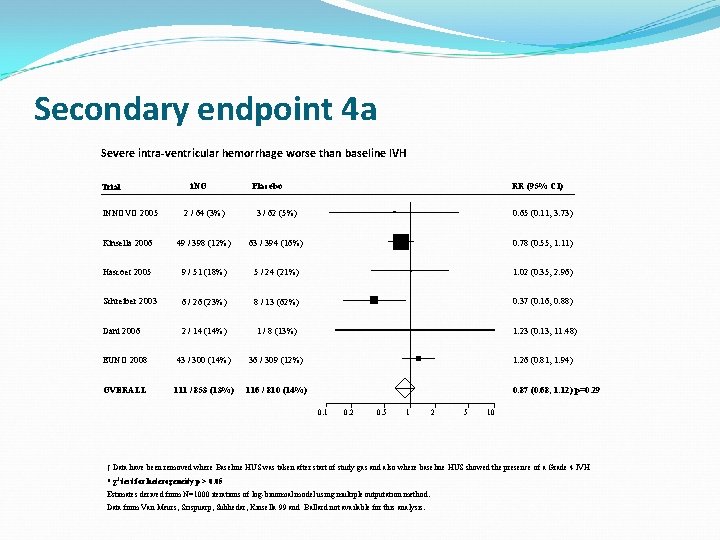
Secondary endpoint 4 a Severe intra-ventricular hemorrhage worse than baseline IVH Trial INNOVO 2005 i. NO Placebo RR (95% CI) 2 / 64 (3%) 3 / 62 (5%) 0. 65 (0. 11, 3. 73) Kinsella 2006 49 / 398 (12%) 63 / 394 (16%) 0. 78 (0. 55, 1. 11) Hascoet 2005 9 / 51 (18%) 5 / 24 (21%) 1. 02 (0. 35, 2. 96) Schreiber 2003 6 / 26 (23%) 8 / 13 (62%) 0. 37 (0. 16, 0. 88) Dani 2006 2 / 14 (14%) 1 / 8 (13%) 1. 23 (0. 13, 11. 48) EUNO 2008 43 / 300 (14%) 36 / 309 (12%) 1. 26 (0. 81, 1. 94) OVERALL 111 / 853 (13%) 116 / 810 (14%) 0. 87 (0. 68, 1. 12) p=0. 29 0. 1 0. 2 0. 5 1 2 5 10 † Data have been removed where Baseline HUS was taken after start of study gas and also where baseline HUS showed the presence of a Grade 4 IVH * χ2 test for heterogeneity p > 0. 05 Estimates derived from N=1000 iterations of log-binomial model using multiple outputation method. Data from Van Meurs, Srispuarp, Subhedar, Kinsella 99 and Ballard not available for this analysis.
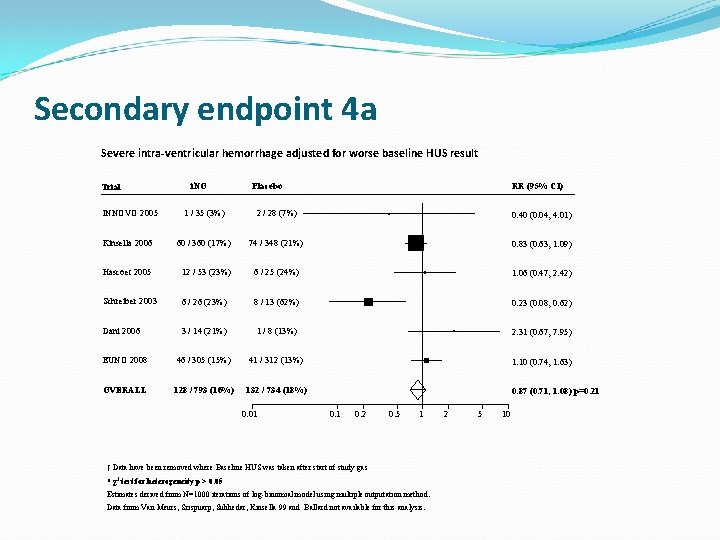
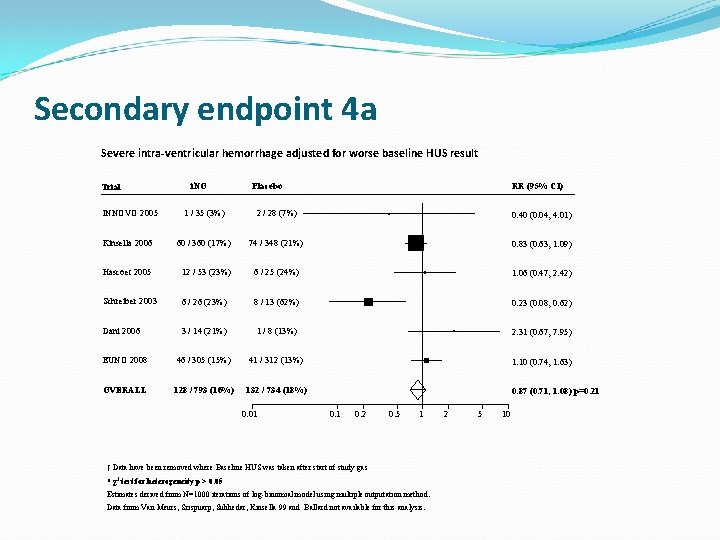
Secondary endpoint 4 a Severe intra-ventricular hemorrhage adjusted for worse baseline HUS result Trial INNOVO 2005 i. NO Placebo RR (95% CI) 1 / 35 (3%) 2 / 28 (7%) 0. 40 (0. 04, 4. 01) Kinsella 2006 60 / 360 (17%) 74 / 348 (21%) 0. 83 (0. 63, 1. 09) Hascoet 2005 12 / 53 (23%) 6 / 25 (24%) 1. 06 (0. 47, 2. 42) Schreiber 2003 6 / 26 (23%) 8 / 13 (62%) 0. 23 (0. 08, 0. 62) Dani 2006 3 / 14 (21%) 1 / 8 (13%) 2. 31 (0. 67, 7. 95) EUNO 2008 46 / 305 (15%) 41 / 312 (13%) 1. 10 (0. 74, 1. 63) OVERALL 128 / 793 (16%) 132 / 734 (18%) 0. 87 (0. 71, 1. 08) p=0. 21 0. 01 0. 2 0. 5 1 † Data have been removed where Baseline HUS was taken after start of study gas * χ2 test for heterogeneity p > 0. 05 Estimates derived from N=1000 iterations of log-binomial model using multiple outputation method. Data from Van Meurs, Srispuarp, Subhedar, Kinsella 99 and Ballard not available for this analysis. 2 5 10
Subgroup Analyses (death or CLD)
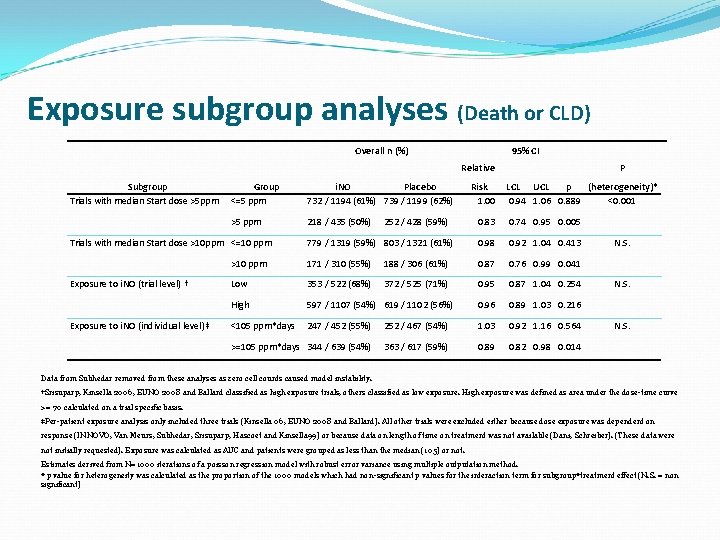
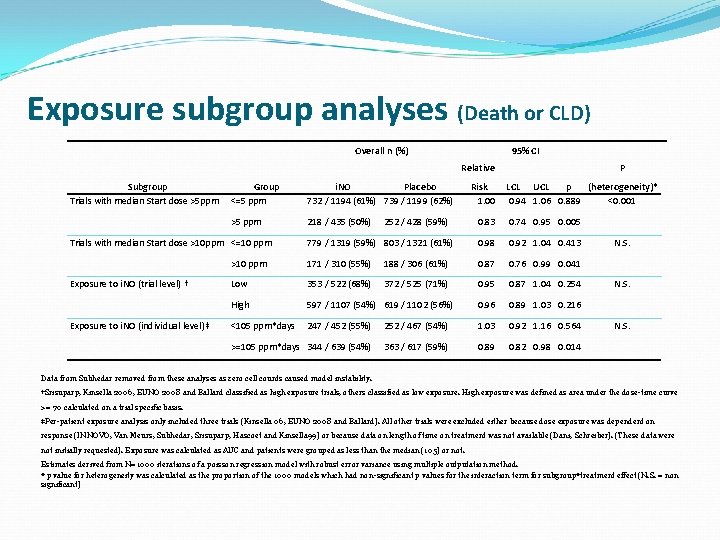
Exposure subgroup analyses (Death or CLD) Overall n (%) 95% CI Relative Subgroup Trials with median Start dose >5 ppm Group <=5 ppm i. NO Placebo 732 / 1194 (61%) 739 / 1199 (62%) >5 ppm 218 / 435 (50%) Exposure to i. NO (trial level) † Exposure to i. NO (individual level)‡ LCL UCL p (heterogeneity)* 0. 94 1. 06 0. 889 <0. 001 0. 83 0. 74 0. 95 0. 005 779 / 1319 (59%) 803 / 1321 (61%) 0. 98 0. 92 1. 04 0. 413 >10 ppm 171 / 310 (55%) 188 / 306 (61%) 0. 87 0. 76 0. 99 0. 041 Low 353 / 522 (68%) 372 / 525 (71%) 0. 95 0. 87 1. 04 0. 254 High 597 / 1107 (54%) 619 / 1102 (56%) 0. 96 0. 89 1. 03 0. 216 <105 ppm*days 247 / 452 (55%) 252 / 467 (54%) 1. 03 0. 92 1. 16 0. 564 >=105 ppm*days 344 / 639 (54%) 363 / 617 (59%) 0. 89 0. 82 0. 98 0. 014 Trials with median Start dose >10 ppm <=10 ppm 252 / 428 (59%) Risk 1. 00 P N. S. Data from Subhedar removed from these analyses as zero cell counts caused model instability. †Srisuparp, Kinsella 2006, EUNO 2008 and Ballard classified as high exposure trials, others classified as low exposure. High exposure was defined as area under the dose-time curve >= 70 calculated on a trial specific basis. ‡Per-patient exposure analysis only included three trials (Kinsella 06, EUNO 2008 and Ballard). All other trials were excluded either because dose exposure was dependent on response (INNOVO, Van Meurs, Subhedar, Srisuparp, Hascoet and Kinsella 99) or because data on length of time on treatment was not available (Dani, Schreiber). (These data were not initially requested). Exposure was calculated as AUC and patients were grouped as less than the median (105) or not. Estimates derived from N=1000 iterations of a poisson regression model with robust error variance using multiple outputation method. * p value for heterogeneity was calculated as the proportion of the 1000 models which had non-significant p values for the interaction term for subgroup*treatment effect (N. S. = non significant)
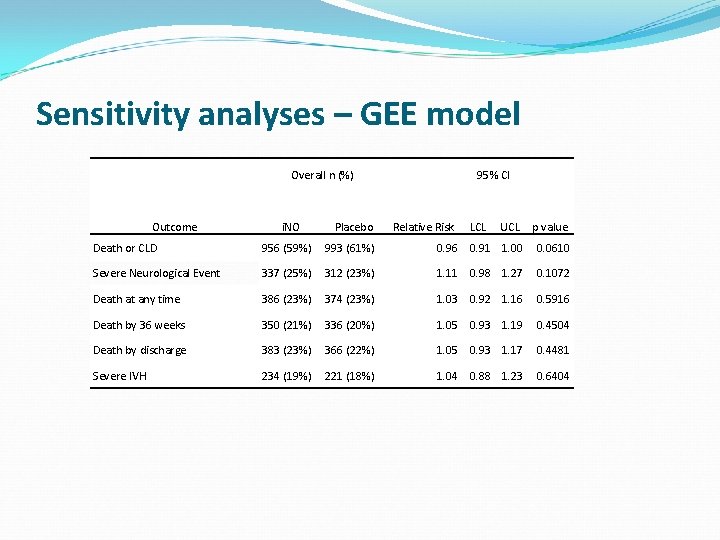
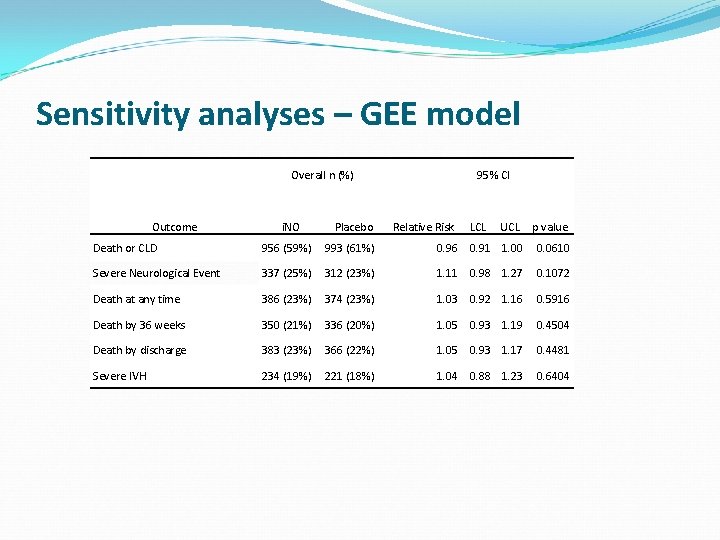
Sensitivity analyses – GEE model Overall n (%) Outcome i. NO Placebo 95% CI Relative Risk LCL UCL p value Death or CLD 956 (59%) 993 (61%) 0. 96 0. 91 1. 00 0. 0610 Severe Neurological Event 337 (25%) 312 (23%) 1. 11 0. 98 1. 27 0. 1072 Death at any time 386 (23%) 374 (23%) 1. 03 0. 92 1. 16 0. 5916 Death by 36 weeks 350 (21%) 336 (20%) 1. 05 0. 93 1. 19 0. 4504 Death by discharge 383 (23%) 366 (22%) 1. 05 0. 93 1. 17 0. 4481 Severe IVH 234 (19%) 221 (18%) 1. 04 0. 88 1. 23 0. 6404
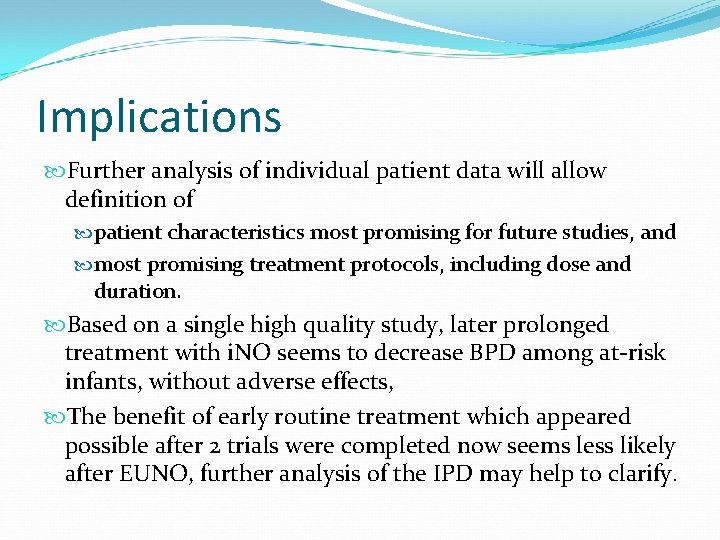
Implications Further analysis of individual patient data will allow definition of patient characteristics most promising for future studies, and most promising treatment protocols, including dose and duration. Based on a single high quality study, later prolonged treatment with i. NO seems to decrease BPD among at-risk infants, without adverse effects, The benefit of early routine treatment which appeared possible after 2 trials were completed now seems less likely after EUNO, further analysis of the IPD may help to clarify.
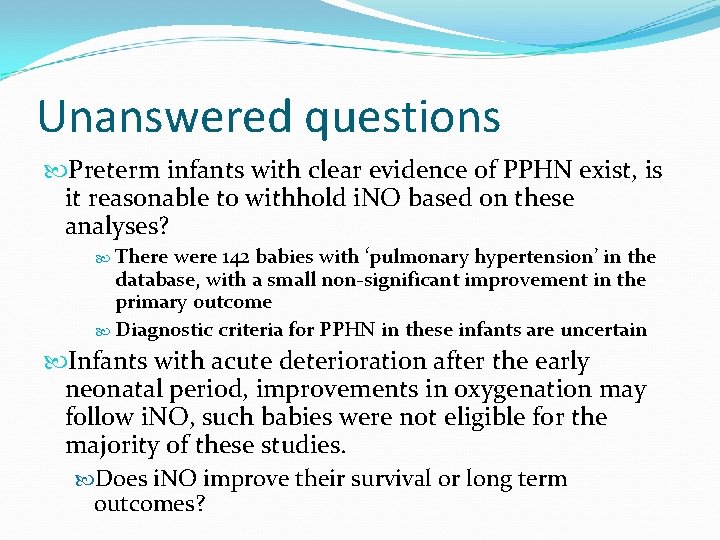
Unanswered questions Preterm infants with clear evidence of PPHN exist, is it reasonable to withhold i. NO based on these analyses? There were 142 babies with ‘pulmonary hypertension’ in the database, with a small non-significant improvement in the primary outcome Diagnostic criteria for PPHN in these infants are uncertain Infants with acute deterioration after the early neonatal period, improvements in oxygenation may follow i. NO, such babies were not eligible for the majority of these studies. Does i. NO improve their survival or long term outcomes?
Implications for further research Most promising appears to be infants at high risk for BPD who are still intubated at 7 days of age Treatment should be prolonged and commence at more than 5 ppm