NITMED TUTORIALS SOME CLINICAL PICTURES 1 Picture 1















































- Slides: 175
NITMED TUTORIALS SOME CLINICAL PICTURES 1
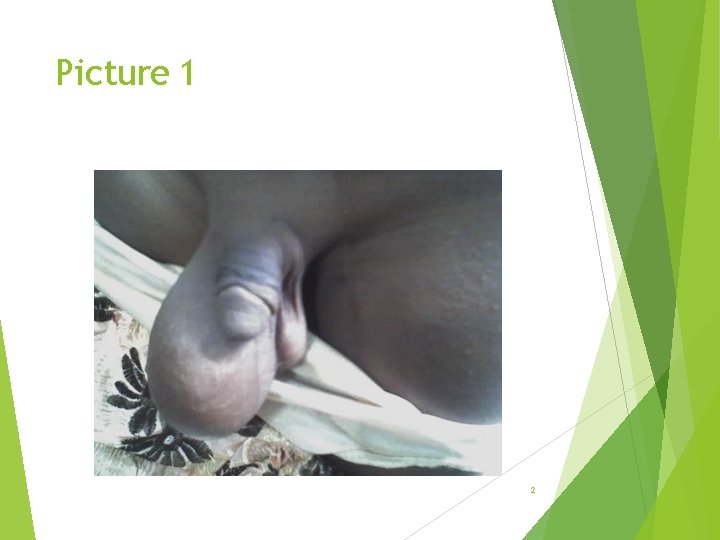
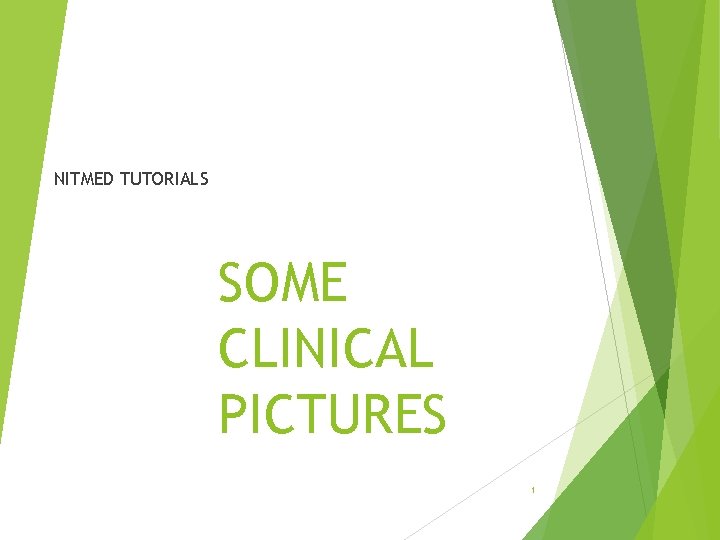
Picture 1 2
Questions Describe and give differential diagnose Classify and treat if the swelling brilliantly transilluminate and cannot be felt separate from the testis 3

Answers Differential Hernia Hydrocele Other differentials; Lipoma of the cord Lymphangiectasis of the cord Varicocele Funiculitis 4
Hydrocele Abnormal collection of fluid within the tunica vaginalis of the testis. Classification as; Communicating and non-communicating Or Congenital acquired; primary or secondary 5
Primary/idiopathic Congenital Infantile Funicular Encysted hydrocele of the cord Hydrocele of canal of nuck Vaginal hydrocele Secondary Trauma Inflammation- epididymoorchitis Lymphatic obstruction-filariasis Tumour 6
Treatment Paeditrics ; herniotomy Adult; hydrocelectomy 7
Picture 2 bbinyunus 2002@gmail. com 8
Questions Describe the pathology What are the types What is the timetable of testicular descent What factor affect testicular descent How is it treated What are the complications bbinyunus 2002@gmail. com 9
Answers Left undescended testes True undescended or retractile Timetable; 3 rd month intrauterine- iliac fossa 7 th month of fetal life- deep inguinal ring Later part of 7 th month travels down the inguinal canal 8 th month IU- superficial ring 9 th month shortly before birth drop into the scrotum Right testis descends before left bbinyunus 2002@gmail. com 10
Factors affecting descent Favours; Shorting of gubernaculum Differential body growth in relation to gubernaculum Raise intraabdoinal pressure Higher body temperature inside the abdomen Development and maturation of epididymis Hormones; h. CG, testosterone and DHT bbinyunus 2002@gmail. com 11
Factors interfering Retroperitoneal adhesion Obstruction at the deep ring Short vas deferens Short testicular vessels Short pampiniform plexus Insufficient pull by the gubernaculum testis Deficient hormonal stimulation Prune belly External exposure to estrogen during the 1 st trimester bbinyunus 2002@gmail. com 12

Treatment Orchidopexy ; before 2 year Orchiectomy ; Atrophic testis Adolescence and adult ; risk of malignant transformation Intra-abdominal that cannot be brought down Complication Infertility Trauma/torsion/tomour Hernia inflammation bbinyunus 2002@gmail. com 13

bbinyunus 2002@gmail. com 14
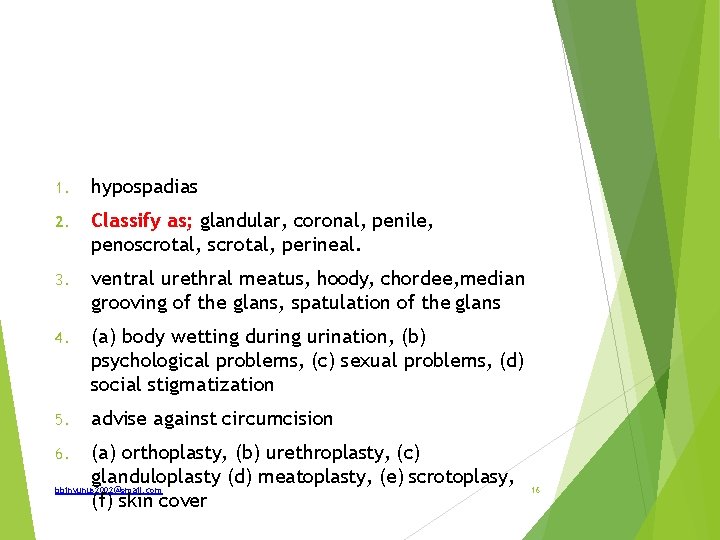
1. 2. 3. 4. 5. 6. identify this pathology how is it classify mention two diagnostic clinical features in this photo. what could be two major problems if unrepaired? what will you advise the parents against? list three components of surgical repair. bbinyunus 2002@gmail. com 15
1. hypospadias 2. Classify as; glandular, coronal, penile, penoscrotal, perineal. 3. ventral urethral meatus, hoody, chordee, median grooving of the glans, spatulation of the glans 4. (a) body wetting during urination, (b) psychological problems, (c) sexual problems, (d) social stigmatization 5. advise against circumcision (a) orthoplasty, (b) urethroplasty, (c) glanduloplasty (d) meatoplasty, (e) scrotoplasy, bbinyunus 2002@gmail. com (f) skin cover 6. 16

bbinyunus 2002@gmail. com 17
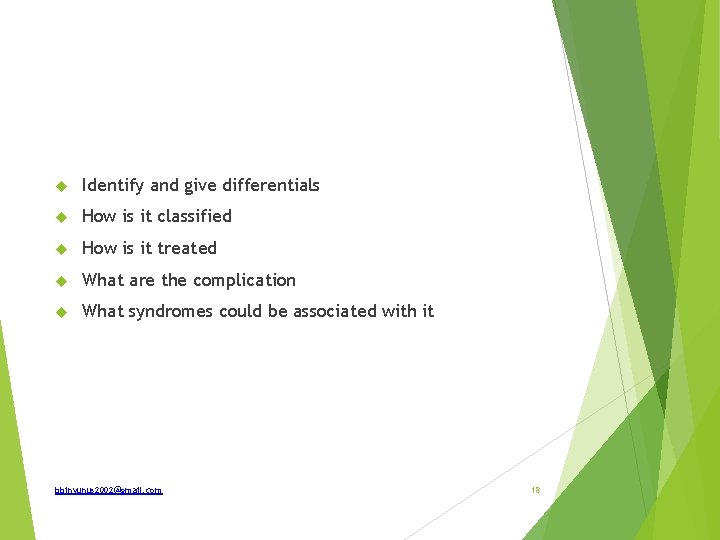
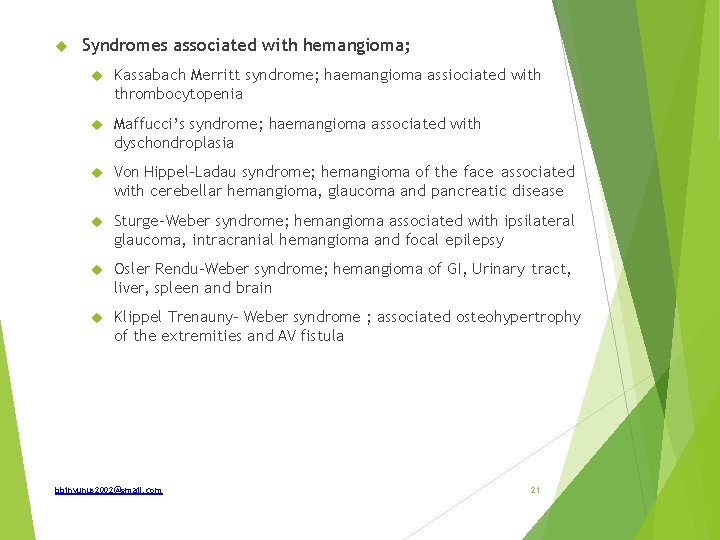
Identify and give differentials How is it classified How is it treated What are the complication What syndromes could be associated with it bbinyunus 2002@gmail. com 18

Capillary hemangioma Strawberry hemangioma Portwine stain(naevus flammeus) Salmon patch Hemangioma are classified as Capillary, cavernous or mixed Treatment Reassure and observe lesion regresses spontaneously (during this period, cosmetic creams can be used to camoflage) Corticosteroids; intralesional triamsinolone or oral prednisolone Sclerotherapy Embolization Laser therapy Surgical excision Radiotherapy bbinyunus 2002@gmail. com 19
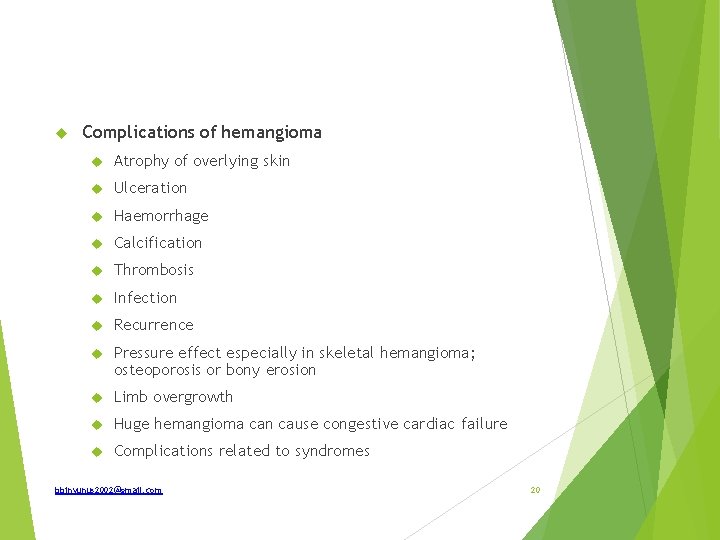
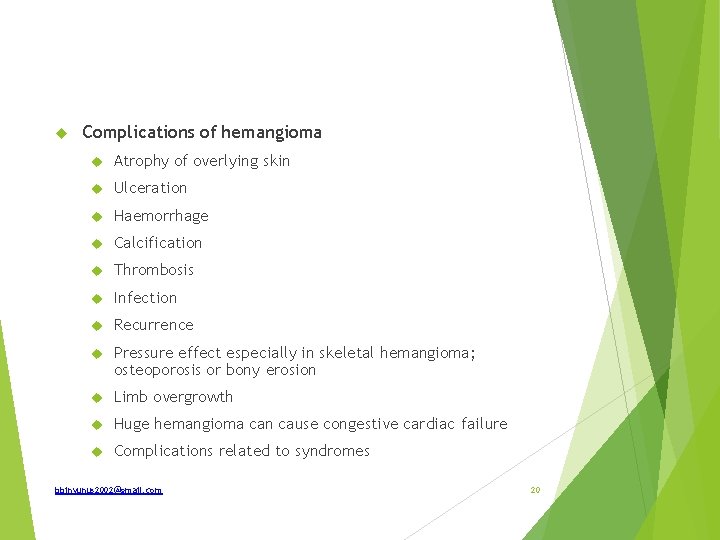
Complications of hemangioma Atrophy of overlying skin Ulceration Haemorrhage Calcification Thrombosis Infection Recurrence Pressure effect especially in skeletal hemangioma; osteoporosis or bony erosion Limb overgrowth Huge hemangioma can cause congestive cardiac failure Complications related to syndromes bbinyunus 2002@gmail. com 20
Syndromes associated with hemangioma; Kassabach Merritt syndrome; haemangioma assiociated with thrombocytopenia Maffucci’s syndrome; haemangioma associated with dyschondroplasia Von Hippel-Ladau syndrome; hemangioma of the face associated with cerebellar hemangioma, glaucoma and pancreatic disease Sturge-Weber syndrome; hemangioma associated with ipsilateral glaucoma, intracranial hemangioma and focal epilepsy Osler Rendu-Weber syndrome; hemangioma of GI, Urinary tract, liver, spleen and brain Klippel Trenauny- Weber syndrome ; associated osteohypertrophy of the extremities and AV fistula bbinyunus 2002@gmail. com 21

bbinyunus 2002@gmail. com 22
What is the common name of this lesion? What is the other name that it is also called that depicts its pathogenesis? What is the pathogenesis? List two (2) other sites of occurrence, though less frequent Name a striking lesion, though infrequent, that may be associated List 2 diagnostic clinical signs of this lesion. List two (2) effective modalities of treatment. Complications bbinyunus 2002@gmail. com 23
Cystic hygroma Lymphangioma or hydrocele of the neck Types; capillary, cavernous lymphangioma and cystic hygroma Pathogenesis; benign proliferation of the lymphatic tissue that donot communicates freely with the lymphatic system. Sites 1. Posterior triangle of the neck— 75%—most common site. Eventually may extend upwards in the neck 2. Axilla— 20% 3. Cheek 4. Tongue—lymphangiogenetic macroglossia 5. Groin 6. Mediastinum 7. Often multiple sites bbinyunus 2002@gmail. com 24
May be associated with macroglosia Swelling is smooth, soft, fluctuant (cystic), not compressible, brilliantly transilluminant. It is not reducible completely. Treatment Surgical excision Sclerotherapy ; for recurrent lesion. Scelosant ; bleomycin, sodium tetradecyl sulphate and glucose, Ok-432 External beam radiation Complications ; Airway obstruction, infection, hemorrhage into cyst, insinuation into major structures, obstructed labour bbinyunus 2002@gmail. com 25
bbinyunus 2002@gmail. com 26
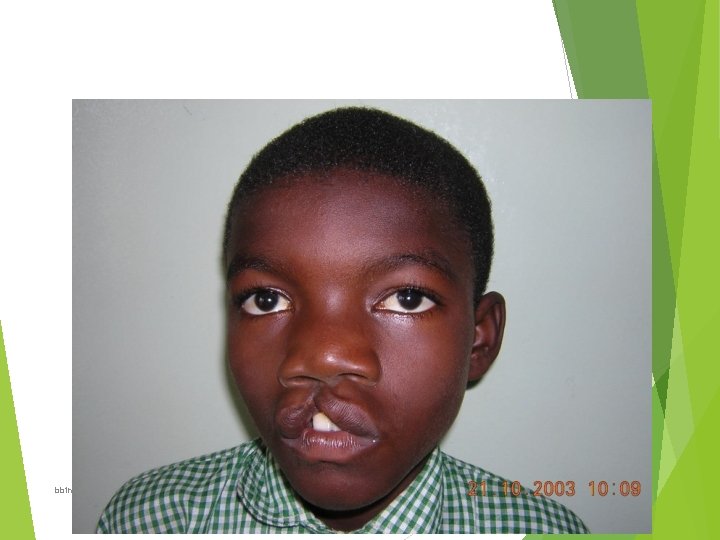
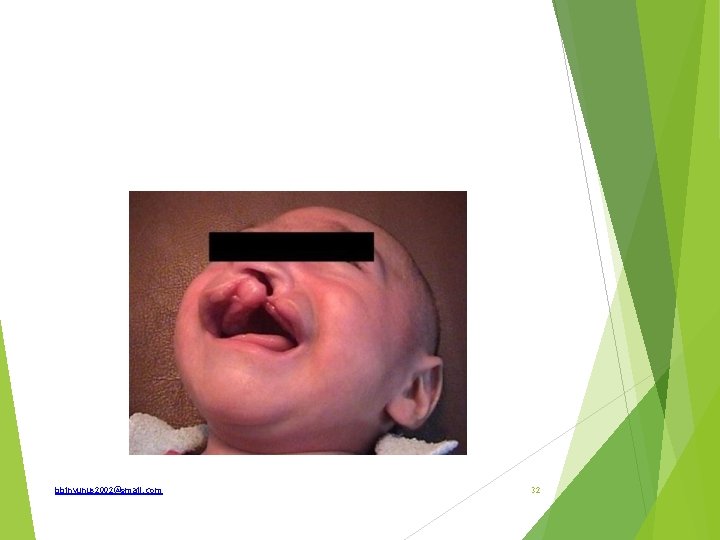
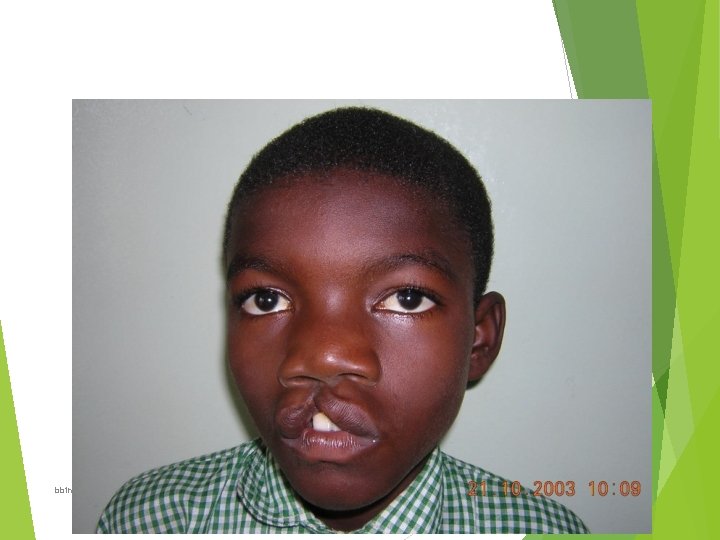
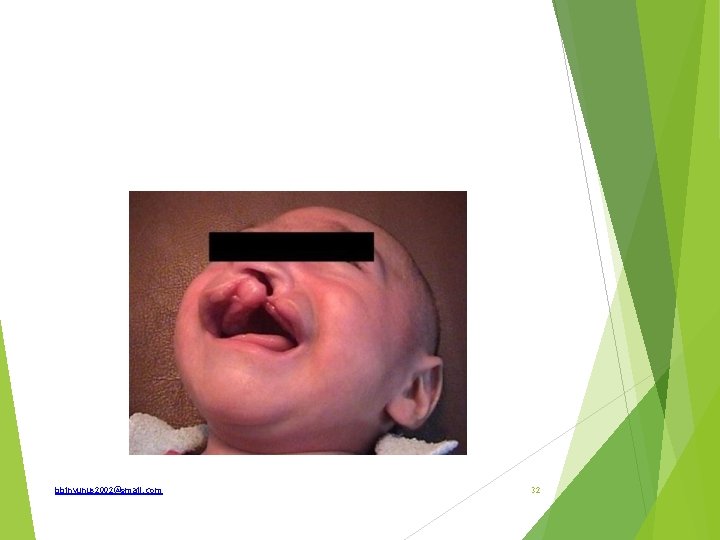
Identify this abnormality How is it classified What is the aetio-pathology? List 2 clinical conditions that may be associated. List 3 complications of this condition. State the timing and type of a corrective operative technique for this condition. • State another specialist, apart from a plastic surgeon, that should be involved in management of this boy • • • 27
Cleft lip Classification; Central cleft- rare Lateral cleft Unilateral or bilateral Complete(extend into the nostril) or incomplete Simple or compound(associated with cleft of alveolus) Complicated(associated with cleft palate) or uncomplicated Aetio-pathology Both genetic and environmental factor 15% are familial through male sex-linked recessive gene bbinyunus 2002@gmail. com 28
Nutritional deficiency; Vit B, Vit A folic acid. Rubella infection Drugs; steroid, phenytoin, diazepam Anoxia Radiation Stress Advance maternal age Diabetic Consanguineous marriage In association with other syndrome; bbinyunus 2002@gmail. com 29
Cleft palate and VACTARL abnormality Complications of cleft lip; Cosmetically ugly Defective suction during breast feeding Dental irregularity Defective speech with particularly with labial letters ; B, F, M, P, V, W Timing for corrective operation Millard rule of 10; child should fulfil ≥ 10 weeks 10 lbs (4. 6 kg) Hb 10 g bbinyunus 2002@gmail. com 30
So the operation is performed when the child is 2. 53 month Patient’s nutrition is accepted for GA and operation Lips element are larger and repair is precise and easy Dropper feed is easier post operatively to facilitate healing Operative technique Millard’s rotation advancement flap Tennison- Randall triangular flap Multidisiplinary ; plastic surgeon, orthodontist, paedodentist, paediatrcian, speech therapist, ENT surgeons bbinyunus 2002@gmail. com 31
bbinyunus 2002@gmail. com 32
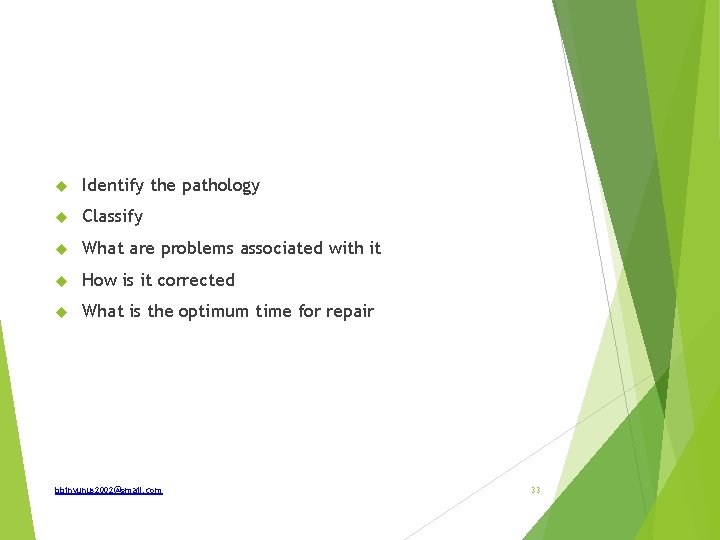
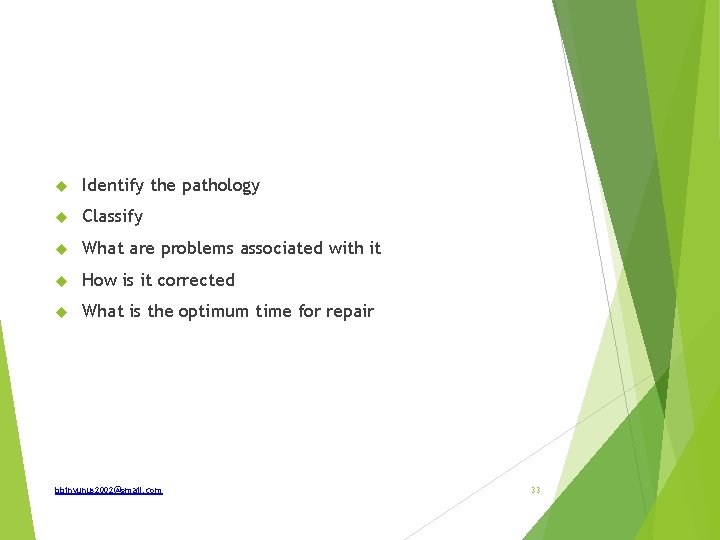
Identify the pathology Classify What are problems associated with it How is it corrected What is the optimum time for repair bbinyunus 2002@gmail. com 33
Cleft lip and palate Classification of cleft palate Incomplete Bifida uvula Cleft of soft palate along its entire length Cleft of the whole length of the soft palate and the posterior part of the hard palate. (intra-maxillary) Complete Cleft soft palate and whole length of the had palate bbinyunus 2002@gmail. com 34
Problems associated with cleft palate; Defective suction Defective speech consonant like; B, D, K, P, T Defective smell Defective hearing and chronic otitis media Repeated respiratory tract infection Chances of aspiration bronchopneumonia Defective dentition because of irregular development of alveolus Cosmetically ugly look particularly when associated with cleft lip bbinyunus 2002@gmail. com 35

Treatment of cleft palate Von Langenbeck palatoplasty V-Y pushback palatoplasty Furlow Others The optimum time for repair 14 -18 month ie before the child can speak (however current trend 9 month -1 year because child start making effort to produce understandable sounds ) bbinyunus 2002@gmail. com 36

bbinyunus 2002@gmail. com 37
List there (3) differential diagnosis of this lesion What is the definitive diagnosis of these swellings that are soft (but not cystic) and tender on examination ? What is the other name the condition is known as which is based on its features? How is it classify Complications bbinyunus 2002@gmail. com 38
Differentials; Lipoma Neurofibroma Cystic swellings Dercum’s disease(adipose dolorosa) – multiple neurolipomatosis Lipoma Classification of lipoma; Encapsulated or diffuse (in relation to capsule) Fibrolipoma, neavolipoma or neurolipoma (histological) bbinyunus 2002@gmail. com 39

Classification Solitary or multiple (number) Sessile or pednculated (shape) Anatomical Subcuteneous Sub-fascial Intermuscular Intramuscular Subperisteal Subsynovial Intra-articular Submucous Subserosal Subdural or extradural bbinyunus 2002@gmail. com 40
Complications of lipoma; Cosmetically urgly Necrosis due to repeated trauma Calcification Haemorrhage Infection Lipomatosis may cause huge enlarment and deformity Liposarcoma Myxomatous degeneration Ulceration bbinyunus 2002@gmail. com 41
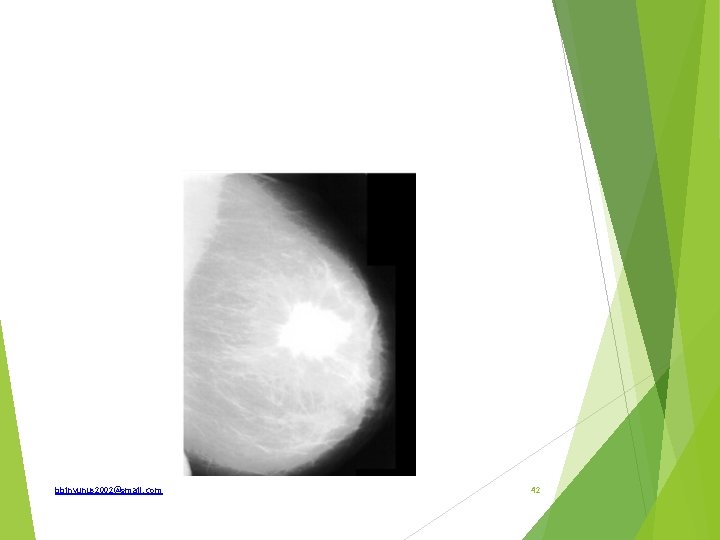
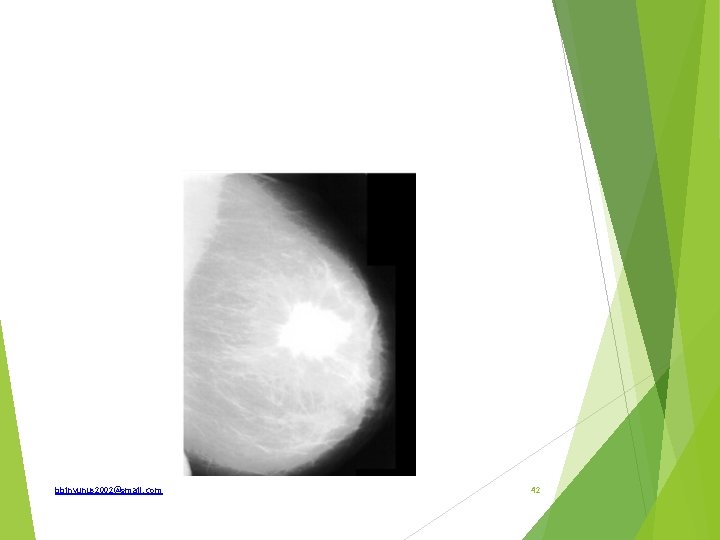
bbinyunus 2002@gmail. com 42
What investigation is shown What are the indications How is it reported What are mammographic findings of malignancy bbinyunus 2002@gmail. com 43
Mammography Indications; Screening ; women >50 year or >35 years with risk factors Diagnostic mammography to evaluate existing feature of breast disease Obese patient Whenever breast conservation is planned To rule out tumour in the contralateral breast Mammography guided biopsy Follow up of benign breast disease with malignant potential Follow up after conservative breast surgery mastalgia bbinyunus 2002@gmail. com 44
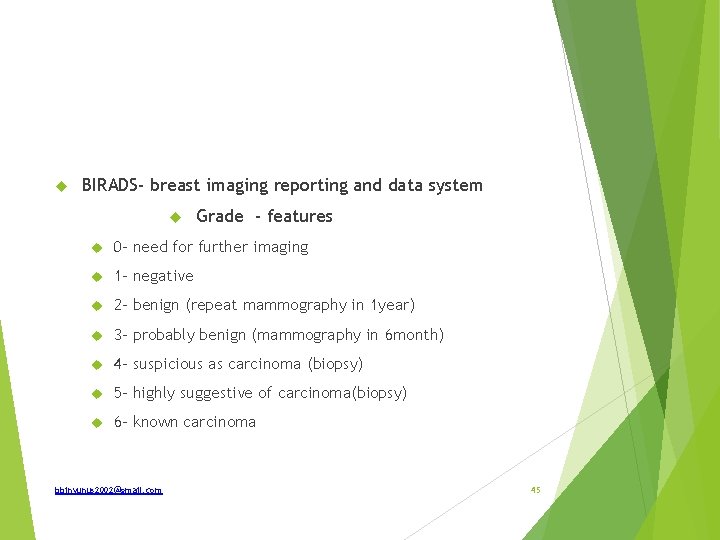
BIRADS- breast imaging reporting and data system Grade - features 0 - need for further imaging 1 - negative 2 - benign (repeat mammography in 1 year) 3 - probably benign (mammography in 6 month) 4 - suspicious as carcinoma (biopsy) 5 - highly suggestive of carcinoma(biopsy) 6 - known carcinoma bbinyunus 2002@gmail. com 45

Mammographic findings of malignancy; Microcalcification Branching calcification Spiculations Ductal distortion Mass effect Loss of symmetry Clustering bbinyunus 2002@gmail. com 46

bbinyunus 2002@gmail. com 47
Spot diagnosis How is pathology classified How would this patient be treated bbinyunus 2002@gmail. com 48

Ans; Double-bubble sign- duodenal atresia Types of atresia; Type 1 -mucosal defect with continuity of the wall-20% Type 2 - lumen atretic with fibrous cord btw proximal and distal lumen Type 3 a – complete atresia with V shape mesenteric defect Type 3 b- apple peel or chrismas tree deformity Type 4 – multiple atresia Adequate resuscitation N-G tube decompression Iv fluid, fluid and electrolyte correction Antibiotic prophylaxis Vit K prophylaxis Doudenoduodenostomy bbinyunus 2002@gmail. com 49
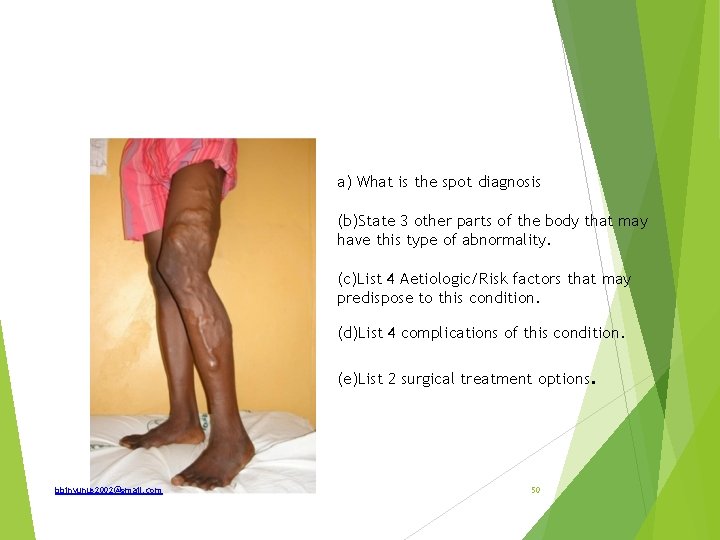
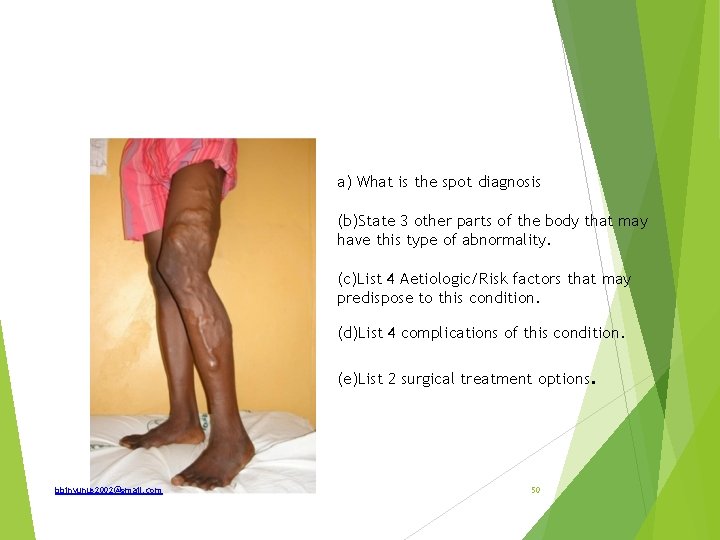
a) What is the spot diagnosis (b)State 3 other parts of the body that may have this type of abnormality. (c)List 4 Aetiologic/Risk factors that may predispose to this condition. (d)List 4 complications of this condition. (e)List 2 surgical treatment options. bbinyunus 2002@gmail. com 50
Answers (a) Varicose veins (b) Oesophageal varices; haemorrhoidal venous plexus; pampiniform venous plexus, (c) Occupation (Prolonged standing), congenital absence or incompetence of valves, obstruction to venous return eg intra abdominal tumour or pregnancy, recurrent thrombophlebitis, A-V malformations, iliac vein thrombosis (d) lipodermatosclerosis, venous ulcer, eczema and dermatitis, haemorrhage; periostitis, ankylosis of joints, thrombophlebitis, calcification, equinovarus deformity. (e) Tredenlenberg operation, Venous stripping, Subfascial ligation of Cocket and Dodd, Subfascial endoscopic perforator ligation surgery, Endoluminal laser ablation bbinyunus 2002@gmail. com 51

bbinyunus 2002@gmail. com 52
(a) What is the condition in this picture called? (b) Mention 4 deformities present? (c) What are the pathological lesions causing these deformities ? (d) Mention 2 congenital conditions that may be associated with this condition. )What are the treatment modalities bbinyunus 2002@gmail. com 53
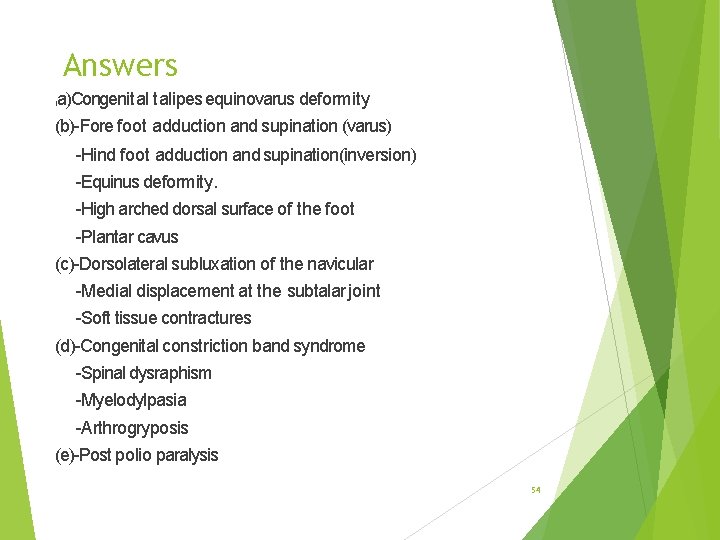
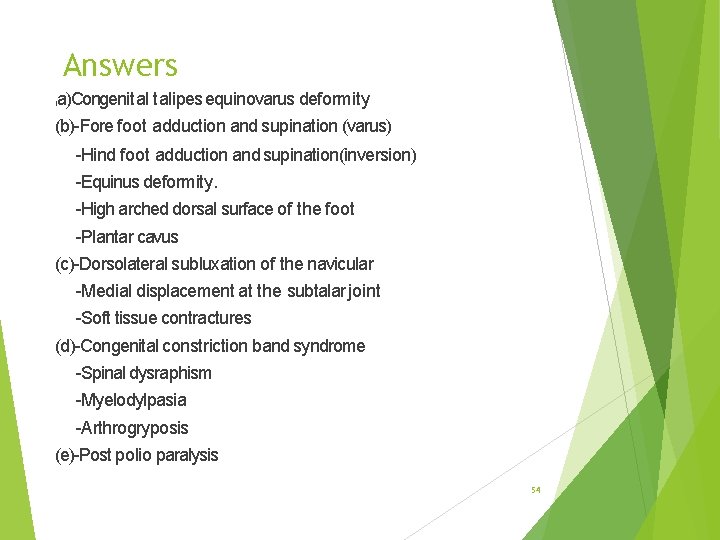
Answers a)Congenital talipes equinovarus deformity ( (b)-Fore foot adduction and supination (varus) -Hind foot adduction and supination(inversion) -Equinus deformity. -High arched dorsal surface of the foot -Plantar cavus (c)-Dorsolateral subluxation of the navicular -Medial displacement at the subtalar joint -Soft tissue contractures (d)-Congenital constriction band syndrome -Spinal dysraphism -Myelodylpasia -Arthrogryposis (e)-Post polio paralysis 54
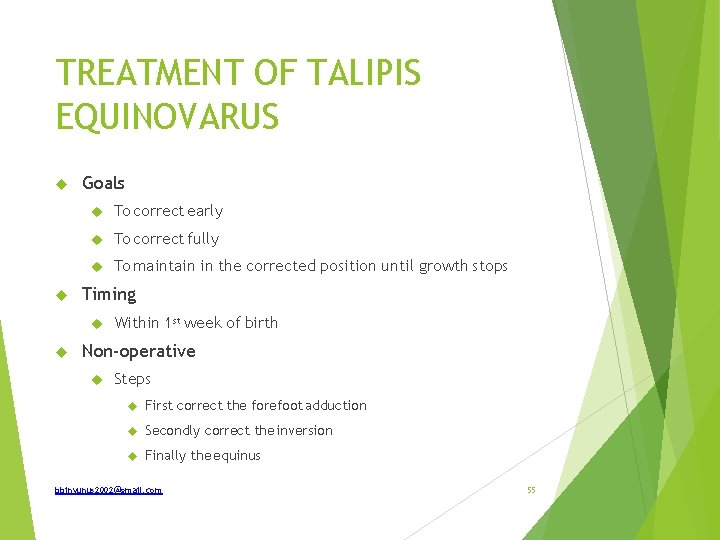
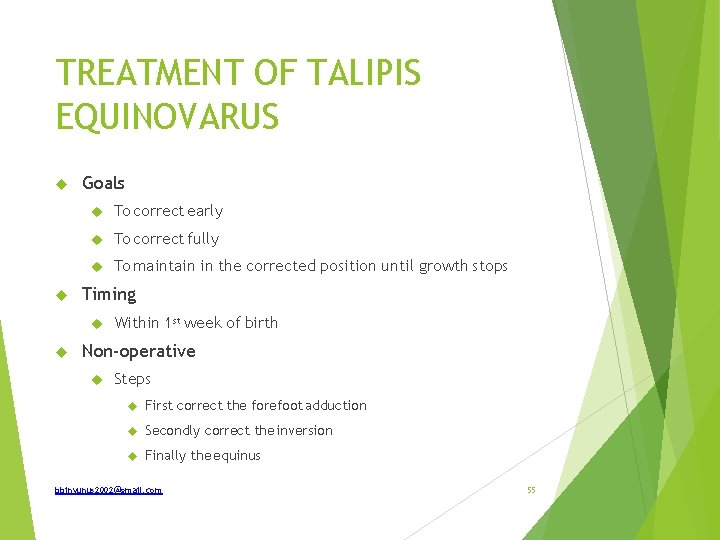
TREATMENT OF TALIPIS EQUINOVARUS Goals To correct early To correct fully To maintain in the corrected position until growth stops Timing Within 1 st week of birth Non-operative Steps First correct the forefoot adduction Secondly correct the inversion Finally the equinus bbinyunus 2002@gmail. com 55

Operative treatment; Indications; when plateau have reach in non operative treatment Response not obtained after 6 month Resistant cases declares themselves after 8 -12 weeks of serial manipulation and strpping Relapsed cases Rigid club foot Late presentation after 6 months of age Complementary to conservative treatment Treatment is soft tissue release on the medial side of the foot and lenghting of tendoachillis bbinyunus 2002@gmail. com 56
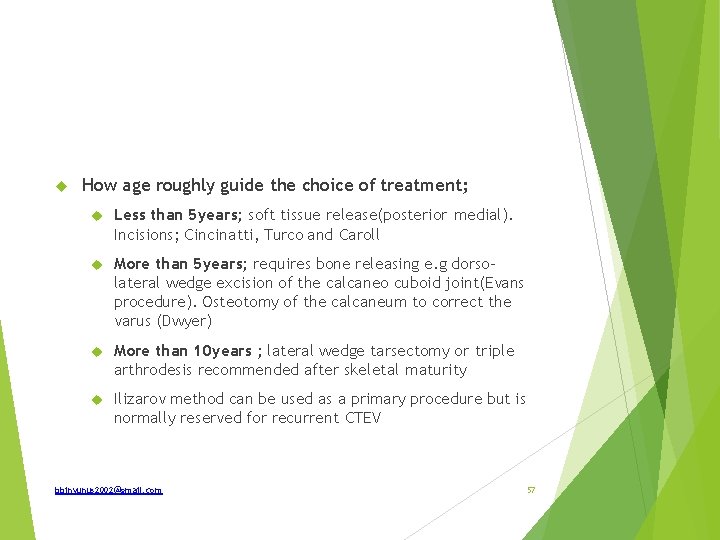
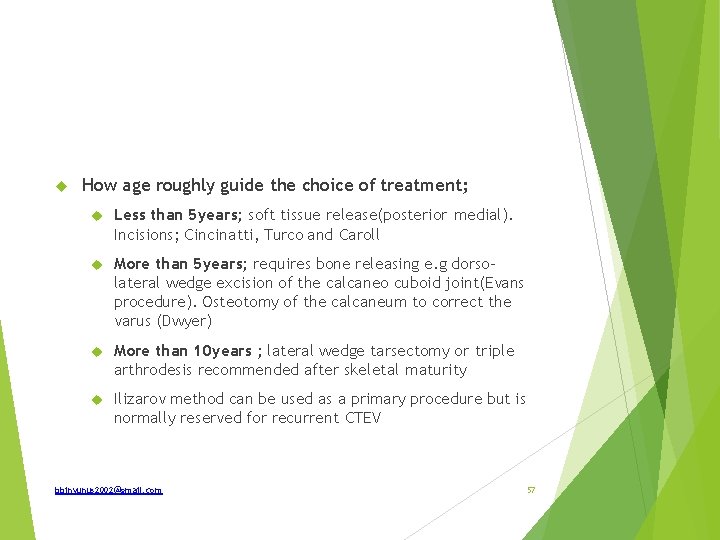
How age roughly guide the choice of treatment; Less than 5 years; soft tissue release(posterior medial). Incisions; Cincinatti, Turco and Caroll More than 5 years; requires bone releasing e. g dorsolateral wedge excision of the calcaneo cuboid joint(Evans procedure). Osteotomy of the calcaneum to correct the varus (Dwyer) More than 10 years ; lateral wedge tarsectomy or triple arthrodesis recommended after skeletal maturity Ilizarov method can be used as a primary procedure but is normally reserved for recurrent CTEV bbinyunus 2002@gmail. com 57

bbinyunus 2002@gmail. com 58
Defined the above image Classify What are the indications What are the complications bbinyunus 2002@gmail. com 59
Colostomy; an artificial colo-cutaneous fistula on the anterior abdominal wall for the purpose of discharging faeces and flatus. Types; According to duration Temporal Permanent According to anatomical location; Sigmoid colostomy Transverse colostomy Caecostomy Desending colostomy bbinyunus 2002@gmail. com 60

According to appearance; End colostomy Loop colostomy Double- barreled colostomy According to function Diverting or defuntioning Decompression colostomy bbinyunus 2002@gmail. com 61
Indications for colostomy Congenital malformations Anal atresia Hirschsprung’s disease Neoplasm Colon carcinoma Rectal carcinoma Inflammatory - intrinsic and extrinsic Chronic diverticular disease Crohn’s disease Lymphogranuoma venesum Radiation injury to colon Endometriosis of the colon or rectum bbinyunus 2002@gmail. com 62
Colorectal Fistulas Colocutaneous Rectovaginal Vesicocolic Trauma Large colonic injuries with faecal contamination Rectal injury bbinyunus 2002@gmail. com 63
Surgical Operation Distal anastomosis (FAP) Low rectal excision Miscellaneous Volvulus of sigmoid colon or caecum Severe or persistent colonic hypomotility Anal incontinence from repeated operation for inflammatory perianal disease Paraplegia, extensive decubitus ulcer/severe burns or infection of the perineum. bbinyunus 2002@gmail. com 64

complications Immediates Bleeding Necrosis of distal end of stoma Electrolyte derangement Intermediate Retraction Prolapse Stenosis Intestinal obstruction Fistula Abscess Stricture Parastomal cellulitis- skin excoriation Intraperitoneal abscess bbinyunus 2002@gmail. com 65
Lat e Colostomy hernia Colostomy diarrhea Recurrence of malignancy Psychological trauma bbinyunus 2002@gmail. com 66

bbinyunus 2002@gmail. com 67
a)What is the function of this tube in this picture? (b)State 3 indications (c)State 4 complications/problems associated with the use (d)State 2 contraindications to use of this tube What are the types bbinyunus 2002@gmail. com 68
Gastrostomy feeding tube Severe malnutrition, major surgeries, severe sepsis, trauma, head and neck surgeries, oesophageal obstruction. It is done if feeding is required for more than one month. Leak-gastric fistula, displacement, blockage of tube, tube migration, diarrhea, bloating, abdominal cramp, wound infection. Previous gastric surgeries, intestinal obstruction, gastric outlet obstruction. bbinyunus 2002@gmail. com 69
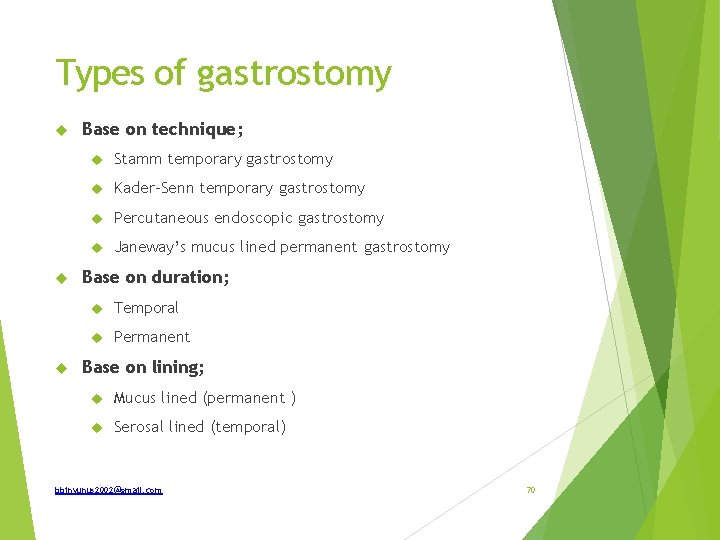
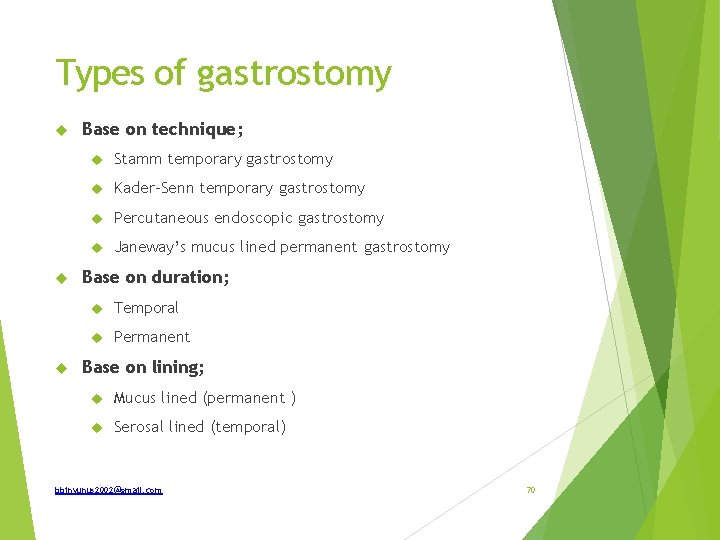
Types of gastrostomy Base on technique; Stamm temporary gastrostomy Kader-Senn temporary gastrostomy Percutaneous endoscopic gastrostomy Janeway’s mucus lined permanent gastrostomy Base on duration; Temporal Permanent Base on lining; Mucus lined (permanent ) Serosal lined (temporal) bbinyunus 2002@gmail. com 70

bbinyunus 2002@gmail. com 71
Give differential diagnosis What are the risk factors for breast ca Mention 2 syndromes associated with breast ca What are the pathological types What are the prognostic factors bbinyunus 2002@gmail. com 72
Differential diagnosis; Carcinoma of the breast Tuberculosis of the breast Traumatic fat necrosis Chronic breast abscess Risk factors for breast ca; Very high risk; Therapeutic radiation Family history in two 1 st degree relative Family history of breast and ovarian cancer BRAC 1 and BRAC 2 mutation carrier or first degree relatives with mutation bbinyunus 2002@gmail. com 73

Moderate to high risk; Age > 60 years History of DCIS, LCIS Cancer of the contralateral breast Slight to moderate risk Nulliparity Early menarchy, late menarchy HRT Obesity Alcohol Benign breast disease bbinyunus 2002@gmail. com 74
Syndromes associated with breast ca; Li Fraumeni syndrome Cowden’s syndrome Ataxia telangiectasia Pathological types Non invasive a) Ductalcarcinoma-in-situ b) Lobularcarcinoma-in-situ bbinyunus 2002@gmail. com 75
Invasive a)Invasive ductal carcinoma b) Invasive ductal carcinoma with a predominant intraductal componenl c)Invasive lobular carcinoma d} Mucinou scarcinoma c) Medullary carcinoma f) Papillary carcinoma g) Tubular carcinoma bbinyunus 2002@gmail. com 76
h) Adenoid cystic carcinoma i) Secretory (juvenile) carcinoma j) Apocrine ca k) Carcinoma with metaplasia i) Squamous type ii) Spindle - cell type iii) Cartilaginous and osseous Iype iv) Mixed type l) Inflammatory carcinoma m) Others bbinyunus 2002@gmail. com 77
Prognostic factors I. Absence or presence of axillary node metastases. 2 Presence or absence of systemic dissemination. 3. Menstrual status of the patient. 4. Biological propensity and grade of the tumour. 5. Size of the tumour at the time of diagnosis. 6. Hormone dependence. bbinyunus 2002@gmail. com 78
PREDICTIVE FACTORS; these predicts the probability of a tumour to respond to certain drugs ER, PR positive tumours have a good response to hormonal manipulation. HER-2/neu overexpression. They do not respond to hormonal manipulaton, are resistant to CMF and show partial resistance to anthracyclines. However, they respond to trastuzumab (herceptin) p 53 mutation also shows resistance to anthracyclines but have greater sensitivity to taxanes. Age below 35 years tend to have high grade tumours with poor response to treatment. bbinyunus 2002@gmail. com 79

bbinyunus 2002@gmail. com 80
Identify Classify Aetiology How is it treated What is thyroid storm and how is it managed Ans Thyrotoxicosis Types Primary (graves disease) Secondary bbinyunus 2002@gmail. com 81

Aetiology; Auto- immune Genetic – autosomal dominant non-autoimmune hereditary familial thyrotoxicosis Iodine induce – Jod Basedow thyrotoxicosis Treatment; 3 forms Antithyroid drug therapy Radioactive iodine Surgery bbinyunus 2002@gmail. com 82
Drud therapy; Indications; Children Adolescents Female patient who is reliable to take drugs and attend follow up Impalpable thyroid Heart failure Recurrence after subtotal thyroidectomy bbinyunus 2002@gmail. com 83
Drugs 1. Carbimazole or metimazole 10 -15 mg tds. They prevent binding of iodine to tyrosine and MIT and DIT to T 3 and T 4 2. Proply or methyl- thiouracil 100 -200 mg tds acts like carbimazole 3. Sodium or potassium perchlorate 800 mg daily. They prevent trapping of iodine. Maintenance is 100 -200 mg daily Propranolol, a B- adrenergic blocker is added 40 mg tds to relieve palpitations Phenobarbitone or diazepam are give to reduce anxiety bbinyunus 2002@gmail. com 84
Symptoms improve in 7 -14 days and when patient becomes euthyroid usually in 4 weeks, the antithyroids are reduce to maintenance for 12 -18 months and then stopped. 50% of patients relapse in 1 -6 months. Drug toxicity; Skin rashes, arthralgia, agranulocytosis, and rarely aplastic anaemia. Monthly white cell and red cell counts are done and treatments stopped if leucopenia or sore throat occurs. bbinyunus 2002@gmail. com 85
Radio- active iodine I¹³¹ taken up irradiates and destroys the thyroid gland. Patient should be made euthyroid before giving the radioactive iodine since only 50% becomes euthyroid Not given below 45 years for fear of malignancy later and pregnant women Problems ; Ophthalmoplegia 15% Hypothyroidism 10% in one year and at 5 years 40 -50% bbinyunus 2002@gmail. com 86

Surgery; Subtotal thyroidectomy is performed after patient is made euthyroid Leaving about 4 g (2 g on each lobe), or 1/8 of the gland by visual estimation or by comparative weighing of tissue remove and tissue left behind Complications; Early Respiratory obstruction; hemorrhage, bilateral abductor paralysis of the vocal cord from damage of recurrent laryngeal nerve, tracheal collapse, oedema from intubation Hypothyroidism Recurrent laryngeal nerve paralysis Thyrotoxic crisis Wound infection Late ; hypothyroidism, recurrence, keloid bbinyunus 2002@gmail. com 87
Thyroid storm (thyrotoxic crisis); Acute exacerbation of thyrotoxicosis and occurs in patient who is not euthyroid at the time of operation. Occurs 6 -24 hours post surgery, patient is restless, maniacal with profuse sweating, severe dehydration, circulatory collapse, hypotension, hyperpyrexia(40°C), tarchycardia, hyperventilation, tremours, vomiting and diarrhea. Treatment; Iv hydrocortisone Propranolol 20 mg 6 hourly Proplythiouracil via N-G tube Diazepam or phenobarbitone Lugol’s iodine IV fluids to correct dehydration Tepid sponging IV PCM Oxygen may also be given bbinyunus 2002@gmail. com 88
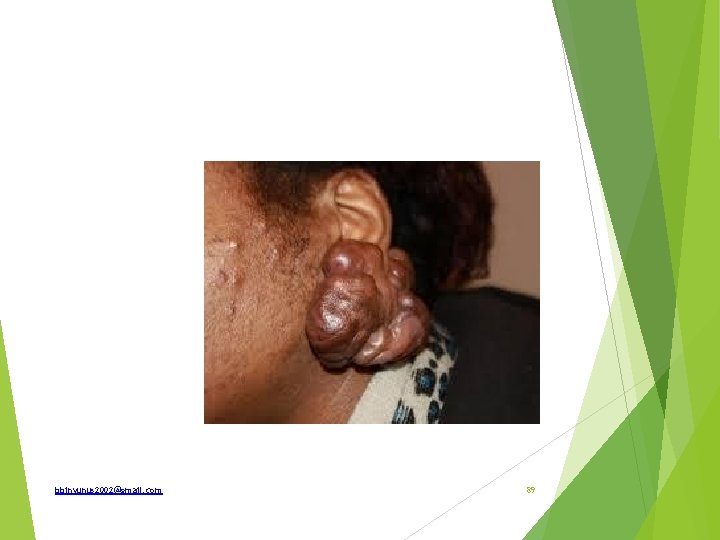
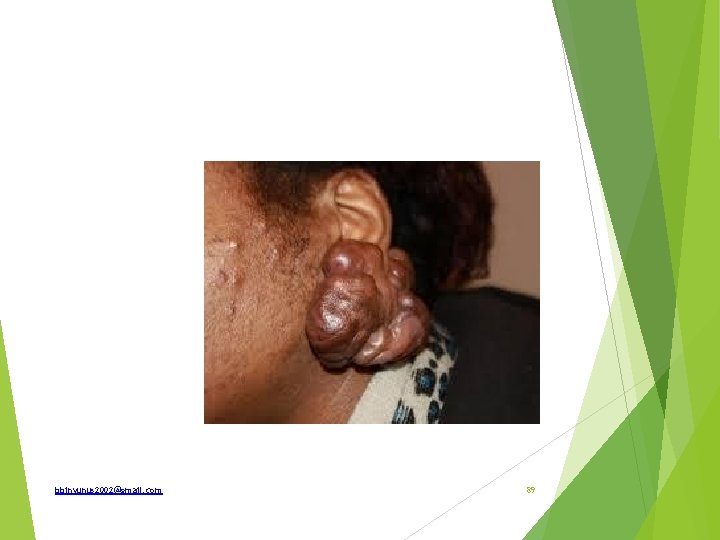
bbinyunus 2002@gmail. com 89
Identify What are the sites of predilection Types complications How is it treated How does it differs from hypertrophic scar bbinyunus 2002@gmail. com 90
Keloid Genetic predisposition Preponderance in Africans Commoner in adolescence, highest incidence is btw 1030 years Commoner in females Persons suffering from TB are more prone Most common site is the sternum Does not occur in palms or sole bbinyunus 2002@gmail. com 91
Area of predilection; sternum, earlobe, face, neck, lower extremities, breast, chest, back and abdomen. Types Progressive(claw-like processes) and non-progressive Acquired and spontenous Complications Ulceration Infection Malignant transformation; fibrosarcoma Itching and tenderness bbinyunus 2002@gmail. com 92

Treatment ; very difficult Multimodality; occlusive dressing, compression therapy, intralesional steroid injection, cryosurgery, excision, radiotherapy and leser surgery Excision and radiotherapy Excision and triamcinolone injection Triple therapy; surgery, radiotherapy and triamcinolone injection Compression therapy Recent involution; intralesional interferon, 5 FU, doxorubicine, bleomycin, verapamil, retinoic acid etc bbinyunus 2002@gmail. com 93
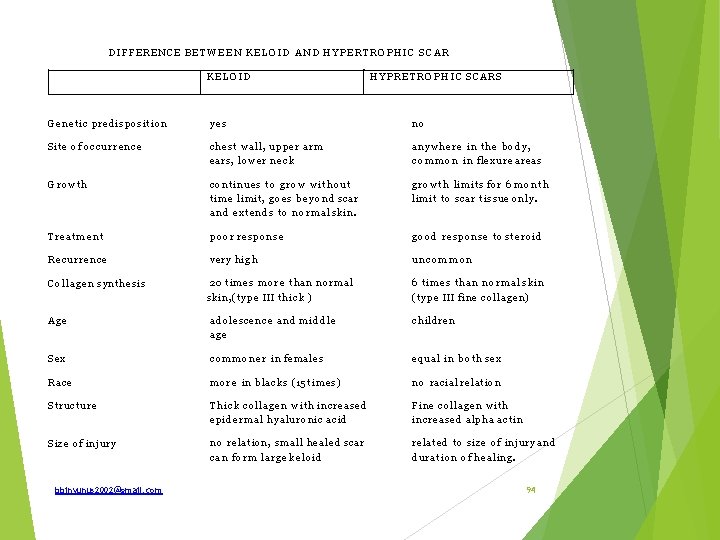
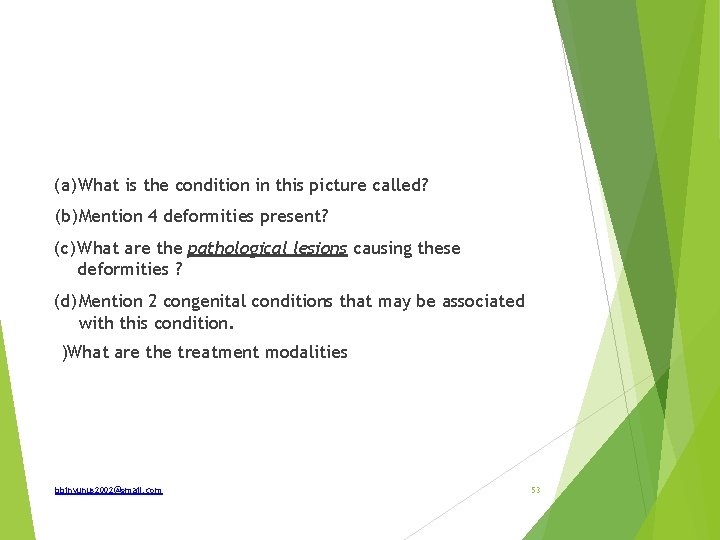
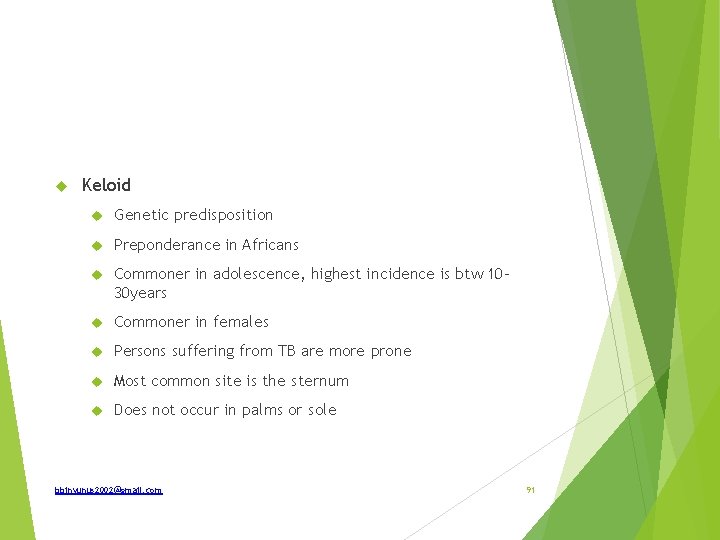
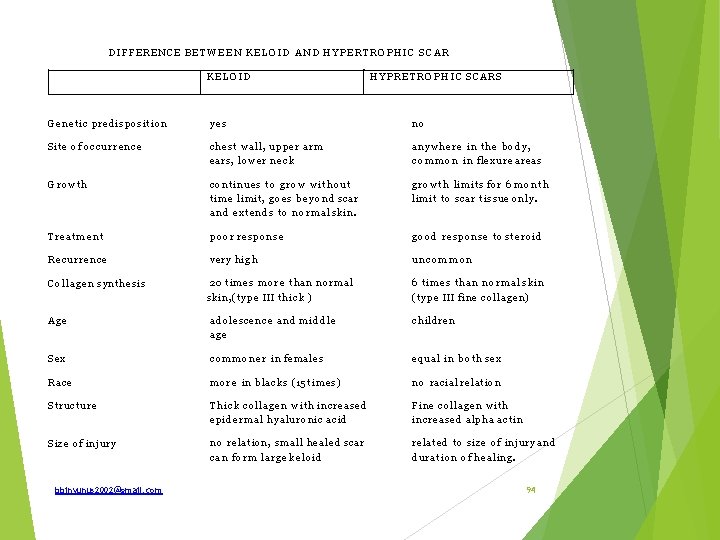
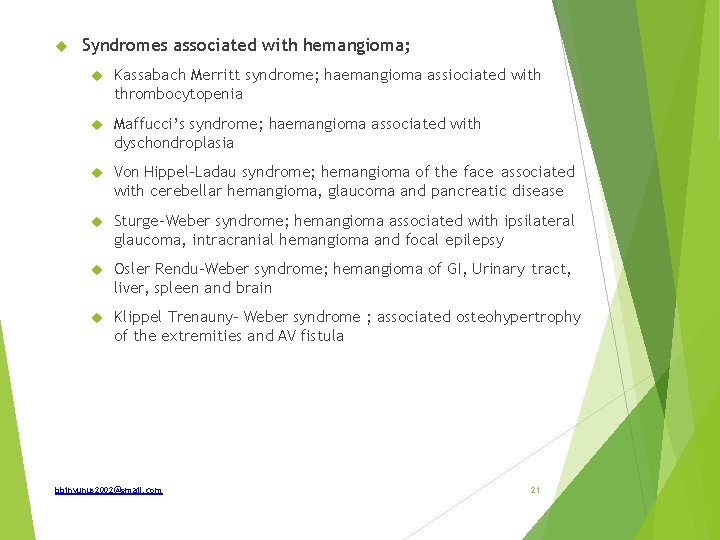
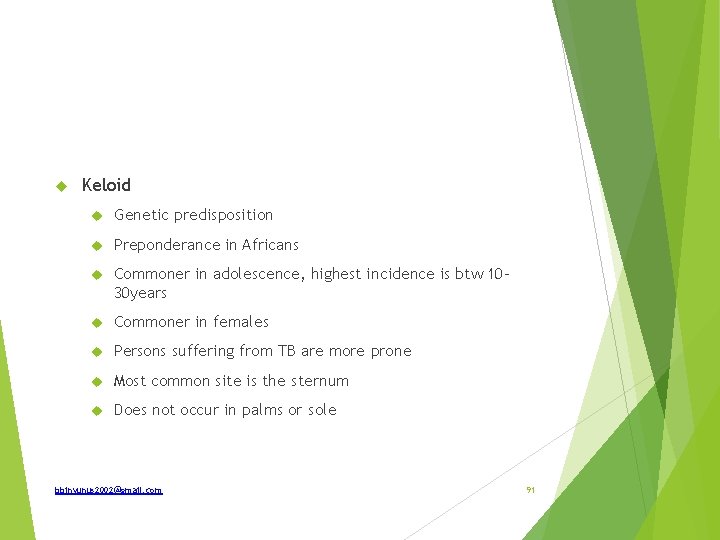
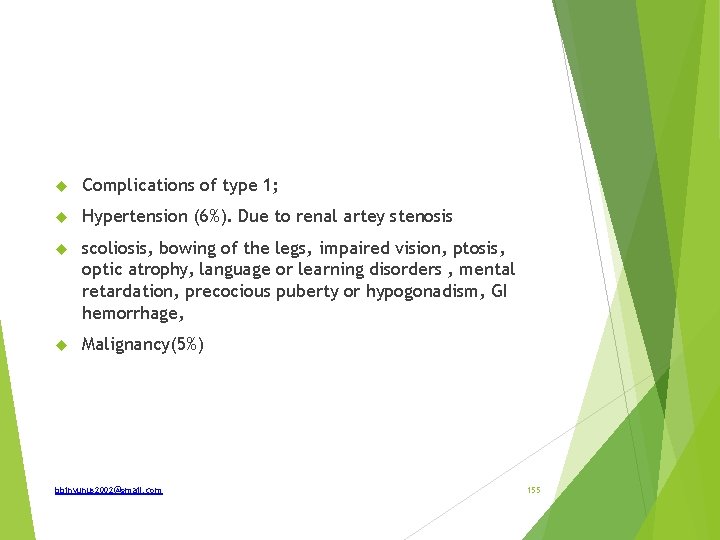
DIFFERENCE B E T W E E N K E L O I D A N D H Y P E R T R O P H I C S C A R KELOID H Y P R E T R O P H I C SCARS G e n e t i c predisposition yes no Site of o c c u r r e n c e chest wall, upp er a r m ears, l o w e r n e c k a n y w h e r e in t h e b o d y , c o m m o n in flexure areas G row th co ntinues t o g r o w w i t h o u t t i m e limit, g o e s b e y o n d scar a n d ex ten ds t o n o r m a l skin. g r o w t h limits for 6 m o n t h limit t o scar tissue only. T rea tm e n t p o o r response g o o d response t o steroid Recurrence very h i g h uncom m on C o l l a g e n synthesis 20 times m o r e th an n o r m a l skin, (type III t hick ) 6 times t h a n n o r m a l skin (type III fine collagen) Age adolesc ence a n d m i d d l e age c h ildre n Sex c o m m o n e r in females eq ual in b o t h sex Race m o r e in blacks (15 times) n o racial relation S truc tu re T h i c k colla ge n w i t h increased epi dermal hyaluronic acid Fine collagen wit h increased alpha actin Size of injury n o relation, small h e a l e d scar c a n f o r m large ke loid related t o size of injury a n d duration of healing. bbinyunus 2002@gmail. com 94

bbinyunus 2002@gmail. com 95
Identify and how is it prevented What are the complications How is it treated bbinyunus 2002@gmail. com 96
Complications; Keloid or hypertrophic scar Deformity and limitation of movement False ankylosis Marjolin’s ulcer Cosmetically ugly Treatment; Timing ; 6 month -1 year when scar has matured Contracture release and grafting Method of release; single or multiple Z-plasty at the point of maximum tension bbinyunus 2002@gmail. com 97
Post burns contracture From full thickness burns Neglected Superficial burns which undergoes infection and ulceration Prevention Proper treatment of superficial burns Adequate splintage of part in extension during healing Prevention of infection Early skin grafting Early physiotherapy bbinyunus 2002@gmail. com 98

bbinyunus 2002@gmail. com 99
Differential diagnosis What are the various types of malignant melanoma Which has the worst prognosis What are other site lesion could be found What features make a lesion suspicious How is it staged Treatment options Prognosis bbinyunus 2002@gmail. com 100
Differential diagnosis; Malignant melanoma Squamous cell ca Basal cell ca Seborrhoeic keratosis Cuteneous agiomata Pyogenic granuloma Kaposi sarcoma bbinyunus 2002@gmail. com 101
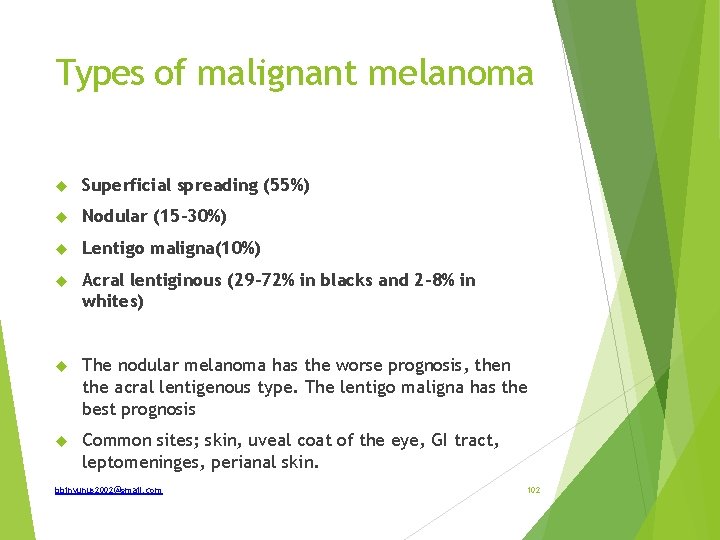
Types of malignant melanoma Superficial spreading (55%) Nodular (15 -30%) Lentigo maligna(10%) Acral lentiginous (29 -72% in blacks and 2 -8% in whites) The nodular melanoma has the worse prognosis, then the acral lentigenous type. The lentigo maligna has the best prognosis Common sites; skin, uveal coat of the eye, GI tract, leptomeninges, perianal skin. bbinyunus 2002@gmail. com 102
Origin De novo 10% Pre-existing naevus 90% Signs of malignant changes in a benign naevus; Pain Itching Satellitism >6 mm Deepening of pigmentation Crust formation Inflammatory changes ulceration Bleeding Irregularities of edges Lymph node metastesis bbinyunus 2002@gmail. com 103
S tagin g TNM – see text Treatment; Excision + elective lymph node dissection (ELND) ELND is recommended only in patient with palpable or proven lymphadenopathy Immunotherapy; cytokine and interferon as adjuvant New immune and gene therapies; vaccine and gene therapy Melanoma are radio and chemo- resistant bbinyunus 2002@gmail. com 104
Prognosis Clinical indicators Sex ; better in females Age ; better in younger < 60 years Site; worse in scalp, feet, hands and trunk Pre-existing naevus ; better prognosis Skin colour ; non- white poorer prognosis Pathological indicators; Tumour thickness (Breslow’s level); < 0. 7 mm good, >1. 5 mm likelihood to metastesis, >3. 5 mm greater tendency to met. Ulceration; poor prognosis Nodular, acral lentigenous and genital; unfavorable prognosis Clark’s level (invasion) Size of tumour; <2 cm without spread good Type of melanoma; lentigo maligna good prognosis bbinyunus 2002@gmail. com 105
Breslow’s classification (1970): Based on thickness of invasion bbinyunus 2002@gmail. com 106
Clark’s levels Level 1: Only in epidermis Level 2: Extension into papillary dermis Level 3: Filling of papillary dermis completely Level 4: Extension into reticular dermis Level 5: Extension into subcutaneous tissue bbinyunus 2002@gmail. com 107

bbinyunus 2002@gmail. com 108
Defined Classify What are the causes What abnormalities may be associated with it How is it treated Differential diagnosis How does OFC changes with age bbinyunus 2002@gmail. com 109
Excessive accumulation of cerebrospinal fluid (CSF) in the ventricles and subarachnoid spaces due to disturbance in its formation, flow or absorption Classification; 1. Communicating(non-obstructive) or non-communicating(obstructive) 2. Congenital or acquired 3. Hydrocephalus with increased ICP or Normal pressure Hydrocephalus Causes ; Increase CSF production; choroid plexus papilloma and choroid plexus carcinoma CSF flow obstruction; aqueductal stenosis, brain lesion and tumour, infections, intraventricular bleeds, Dandy Walker cyst Reduce CSF absorption; obstruction at the arachnoid granulations, otitic hydrocephalus, sinus thrombosis, arachnoiditis Familial causes; Bicker’s Adam syndrome, an X-linked recessive abnormality bbinyunus 2002@gmail. com 110
Associated abnormalities Dandy-Walker syndrome Arnold-Chiari malformation Spina bifida Aqueductal stenosis bbinyunus 2002@gmail. com 111

Treatment; Medical; pre-operatively is commenced; Acetazolamide- a carbonic anhydrase inhibitor Furosemide- has synergistic action with acetazolamide Surgery Shunting procedure ; Ventriculo-peritonel Ventriculo-pleural Ventriculo-atrial Lumboperitoneal Torchedsen shunt bbinyunus 2002@gmail. com 112
Differential diagnosis; Hydrocephalus ex-vacuo Hydrancephaly Familial big head OFC- occipito-frontal circumference At birth average 35 cm 1 st year it increase by 12 cm to 47 cm In the 1 st 3 months, increase by 2 cm/month (gain of 6 cm) In the next 3 months increase by 1 cm/month (gain of 3 cm) In the last 6 months increase by 0. 5 cm/month (gain of 3 cm) bbinyunus 2002@gmail. com 113

bbinyunus 2002@gmail. com 114
What are the type Risk factors Prenatal diagnosis What problems may be associated with it How is it treated bbinyunus 2002@gmail. com 115
Types ; Spinal bifida occulta Spinal bifida aperta (cystica) Risks factors; Pre-conception maternal folic acid deficiency Maternal exposure to excessive heat during time of fetal embryogenesis Use of valproic acid (an anticonvulsant) during pregnancy Previous birth of a child with NTD Maternal cocaine abuse bbinyunus 2002@gmail. com 116
Prenatal diagnosis; Maternal serum alpha-fetoprotein at 15 -20 weeks is more than twice for that gestational age Prenatal ultrasound detects 90 -95% of spinal bifida Amniotic fluid alpha-fetoprotein is very high Extreme maternal age Complicated pregnancies e. g toxemia, hydramnois, malpresentations Associated anomalies Hydrocephalus Club foot Fecal incontinence Urine incontinence bbinyunus 2002@gmail. com 117

Treatment; Multidisiplinary Myelomeningocele excision and repair Serial manipulation of club foot Incontinence at an older age Complications of surgery Wound infection and meningitis CSF leak Hydrocephalus Nerve or spinal cord injury bbinyunus 2002@gmail. com 118
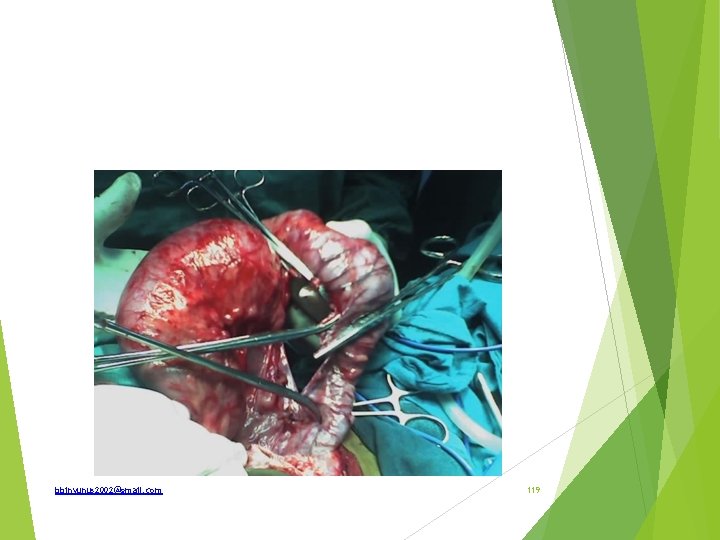
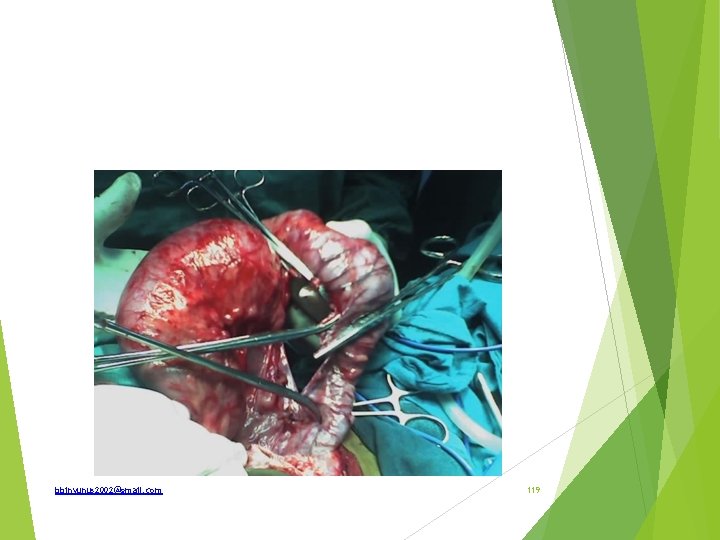
bbinyunus 2002@gmail. com 119
(a) State 3 descriptive features of the bowel in this picture (b) What is the likely diagnosis (c) State 3 investigation necessary to confirm this diagnosis (d) What surgery was being carried out (e) State 2 complications of this surgery bbinyunus 2002@gmail. com 120
(a) Megacolon, transition zone and collapsed bowel segament (b) Hirschsprung’s disease (c) Barium enema, rectal biopsy, anorectal manometry (d) Soaves Pull through surgery (e) Rectal prolapsed/retraction, gangrene, bowel perforation bbinyunus 2002@gmail. com 121

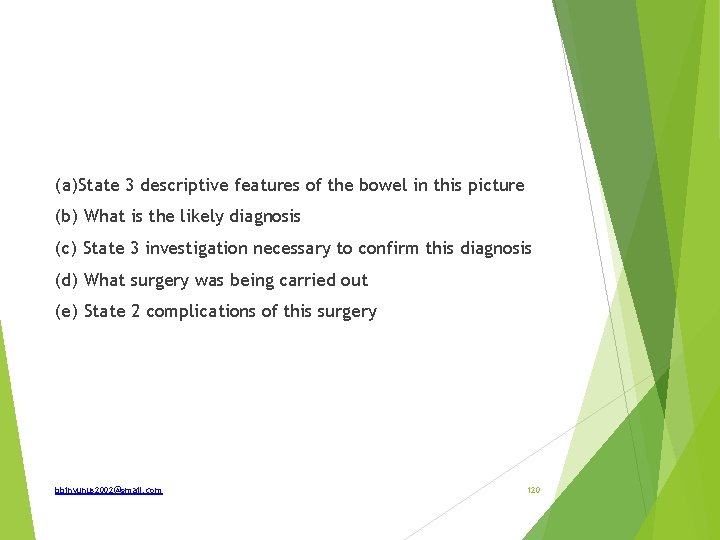
PIX 4 bbinyunus 2002@gmail. com 122
(a)What is the spot diagnosis? (b) State 2 differential diagnosis (c)What is the embryologic origin of this condition? (d)State 3 possible complications (e)Classify this condition bbinyunus 2002@gmail. com 123
(a)Sacrococcygeal teratoma (b)Spinal bifida; Lipoma (c)Primitive streak (d) Infection, Ulceration, malignant transformation (e) -Type I predominantly external with minimal presacral component -Type II external with a significant intrapelvic component -Type III external with predominant pelvic mass with intra abdominal extension -Type IV entirely presacral without external or pelvic extension bbinyunus 2002@gmail. com 124
bbinyunus 2002@gmail. com 125
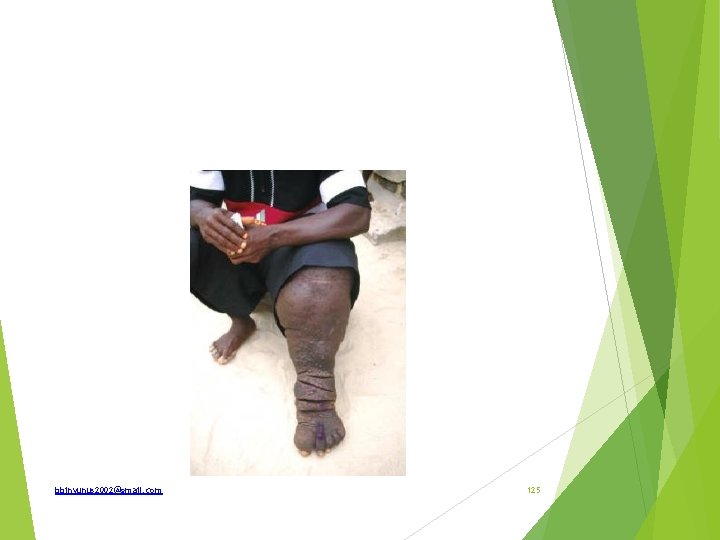
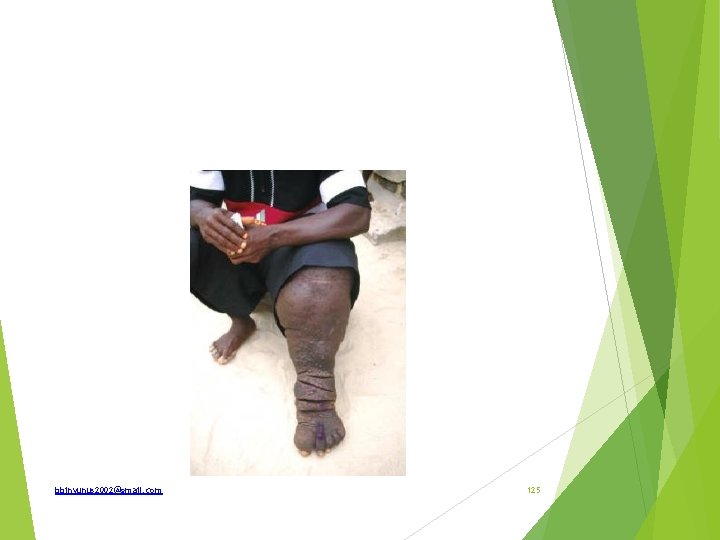
Defined Classify Modalities of treatment Lymphoedema; is interstitial oedema of lymphatic origin resulting in protein-rich fluid accumulation in the interstitial compartment. Classification ; Primary Secondary bbinyunus 2002@gmail. com 126

Primary ; developmental defects of subcutaneous lymphatic channels. There are 3 types; Lymphoedema congenital(10%) ; aplasia < 2 year of age 10 -25% of all primary lymphedema When Sporadic or familial (Milroy's disease) More common in males Lower extremity is involved 2 times more frequently than the upper extremity 2/3 patients have bilateral lymphedema bbinyunus 2002@gmail. com 127
Lymphedema praecox (75%) : hypoplasia (reduced number and caliber) Evident after birth and before age 35 years Most often arises during puberty 65 -80% of all primary lymphedema cases Females are affected 4 times 70% of cases are unilateral, with the left lower extremity being involved bbinyunus 2002@gmail. com 128

Lymphoedema tarda (15%); not evident until 35 years or older Rarest form of primary lymphedema Only 10 -15% of cases Hyperplasic pattern, with tortuous lymphatics increased in caliber and number Absent or incompetent valves bbinyunus 2002@gmail. com 129
Secondary lymphedema; Trauma Surgery—inguinal block or axillary block dissection/postmastectomy with axillary clearance Filarial lymphoedema due to Wuchereria bancrofti—common cause in coastal region Tuberculosis Syphilis Fungal infection Advanced malignancy—hard, fixed lymph nodes in axilla orin inguinal region Postradiotherapy lymphoedema Bacterial infection Rare causes: Rheumatoid arthritis, snake, and insect bite, DVT, chronic venous insufficiency bbinyunus 2002@gmail. com 130
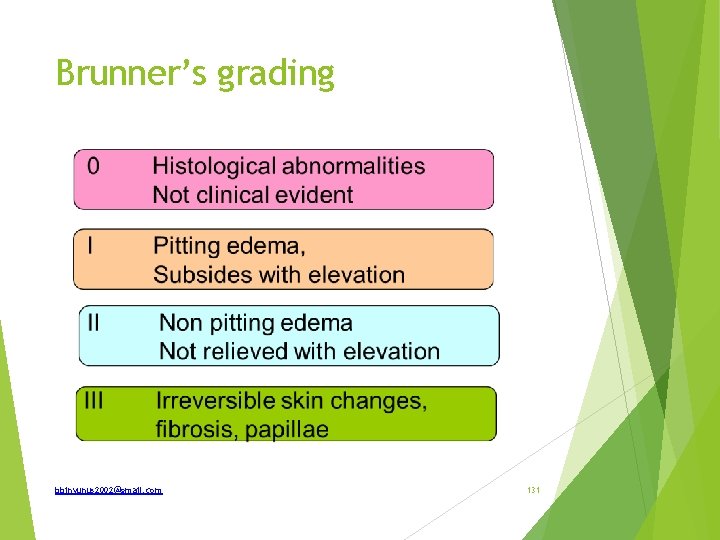
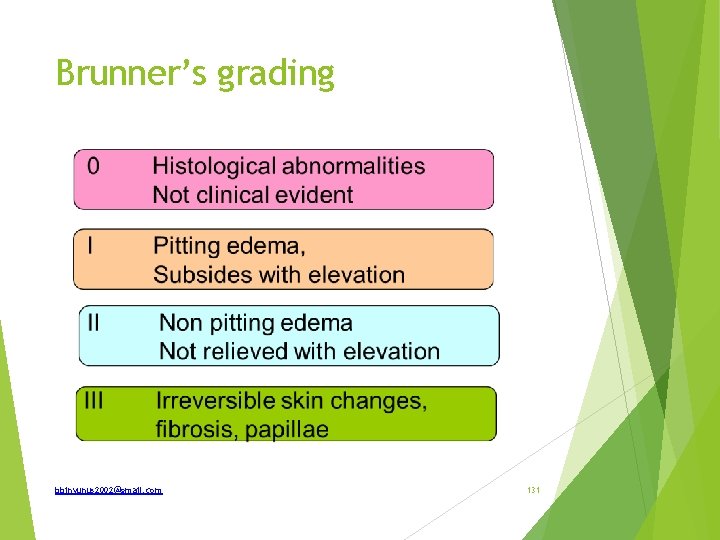
Brunner’s grading bbinyunus 2002@gmail. com 131
Treatment Modalities Conservative; Hygiene of affected limb Limb elevation Compression stockings once swelling is reduced Physiotherapy External pneumatic compression Surgery Debulking operations ; Homan’s procedure Charlse procedure Sistrunk procedure Thompson’s procedure bbinyunus 2002@gmail. com 132

Bypass surgery Lymphaticovenous anastomosis Lymphaticolyphatic anastomosis Enteromesenteric bridges Omental bridges Skin and muscle flap bbinyunus 2002@gmail. com 133
bbinyunus 2002@gmail. com 134
Identify and how is it treated Polydactyly Excision and wound closure bbinyunus 2002@gmail. com 135
bbinyunus 2002@gmail. com 136
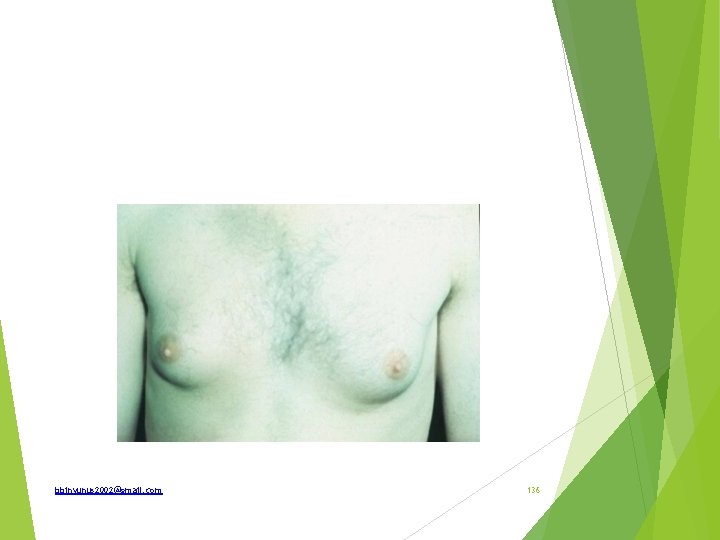
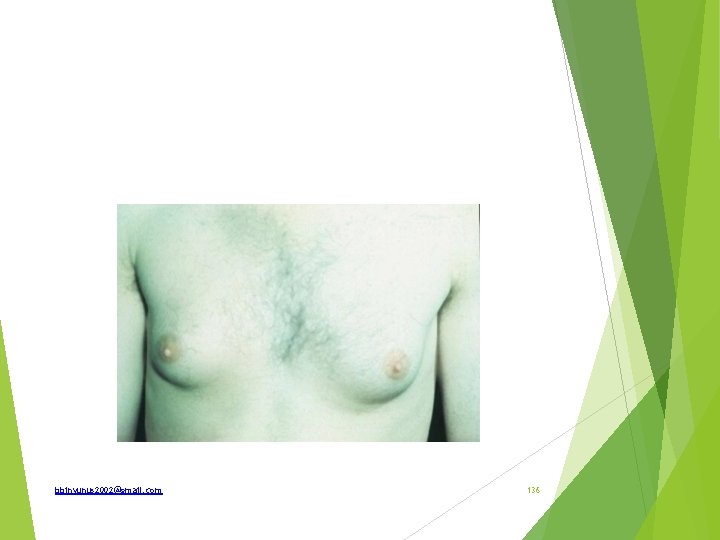
Identify the lesion in this 24 year man How is it classified What are the differential diagnosis if unilateral What are relevant investigation What are the modalities of treatment bbinyunus 2002@gmail. com 137

Gynaecomastia Grade; 1 - minor breast enlargement with no redundant skin 2 a- moderate breast enlargement with no redundant skin 2 b-moderate breast enlargement with redundant skin 3 - grossly enlarged breast Unilateral enlargement; Breast cancer Fibroadenoma Fibrocystic changes Phylloides tumour bbinyunus 2002@gmail. com 138

Investigations Hormonal assay; testosterone, estrogen, LH, FSH, prolactin, TFT LFT Abdominal USS, testicular USS, CXR Biopsy; FNAC Treatment; over 80% regress spontenously ; If the cause found and treated Subcutenous mastectomy; via an infra-mammary incision or endoscopic with small distant incision to prevent breast scar Danazol 200 mg bd for 3 month reduces breast in 50% Tamoxifen 20 mg od cause complete regression in 80% of middle aged bbinyunus 2002@gmail. com 139
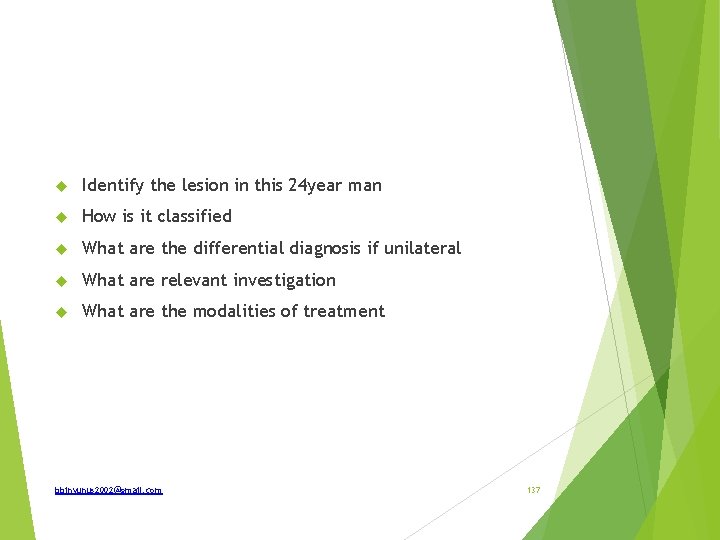
bbinyunus 2002@gmail. com 140
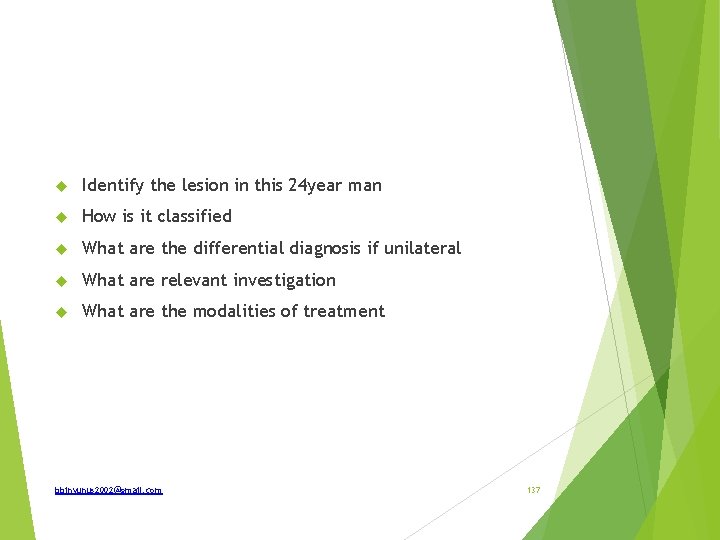
List 3 differential diagnosis If the swelling moves with tongue protrusion how is it treated Differential diagnosis; Thyroglossal cyst Ectopic thyroid Pretracheal lymph node Dermoid cyst Solitary nodule of thyroid—isthmus Submental lymph node collar stud abscess Subhyoid bursa bbinyunus 2002@gmail. com 141
Treatment of thyroglossal cyst Sistrunk operation: Excision of cyst and also full tract upto the foramen caecum is done along with removal of central part of the hyoid bone, as the tract passes through it. bbinyunus 2002@gmail. com 142

bbinyunus 2002@gmail. com 143
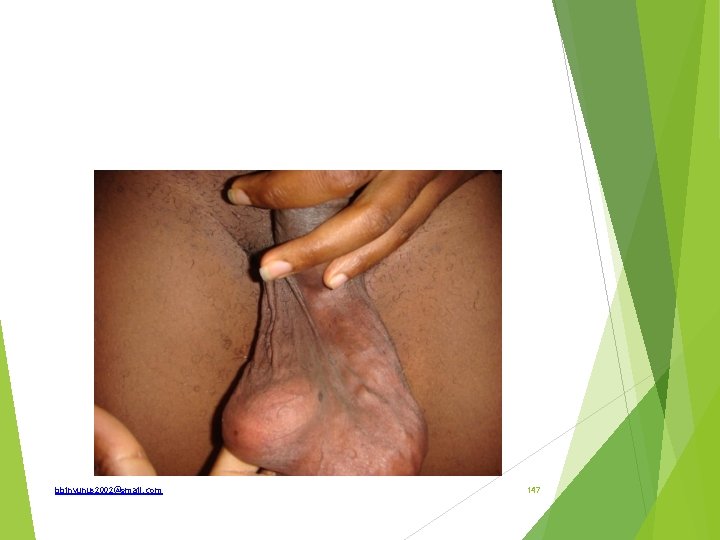
Identify What is the incidence How is the spectrum of the disease How is it treated Bladder extrophy (ectopia vesicae) Incidence; 1/10, 000 -50, 000. M: F is 2: 1 Other associated pathology; widely separated pubic rami, externally rotated femora, epispadia. May be associated with other genital, neuronal or anorectal anomalies, undescended testes, inguinal hernia. Cause of death; ascending pyelonephritis 200 time risks of carcinoma. -adenocarcinoma bbinyunus 2002@gmail. com 144
Treatment Defect is repaired early to prevent metaplasia and malignant changes Bladder is closed or augumented by ileum Bladder neck reconstruction Pubic rami is approximated Anterior abdominal wall closed At times, the bladder is excised and continent urinary diversion done and later epispadia repair bbinyunus 2002@gmail. com 145
Spectrum Covered extrophy (only apical portion of the bladder is involved the anterior abdominal wall muscle is intact) Epispedia Ectopia vesicae Cloacal extrophy bbinyunus 2002@gmail. com 146
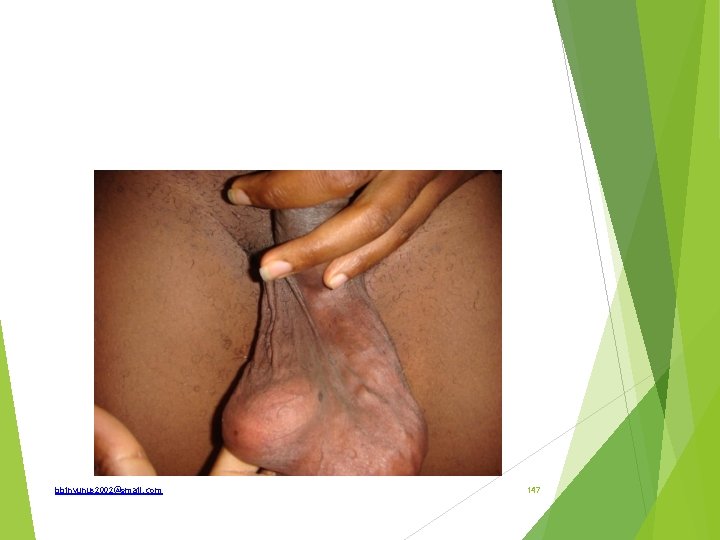
bbinyunus 2002@gmail. com 147
Spot diagnosis What are the types What side is commoner and why Important signs How is it graded How are the types differentiated An important complication What are the modalities of treatment bbinyunus 2002@gmail. com 148
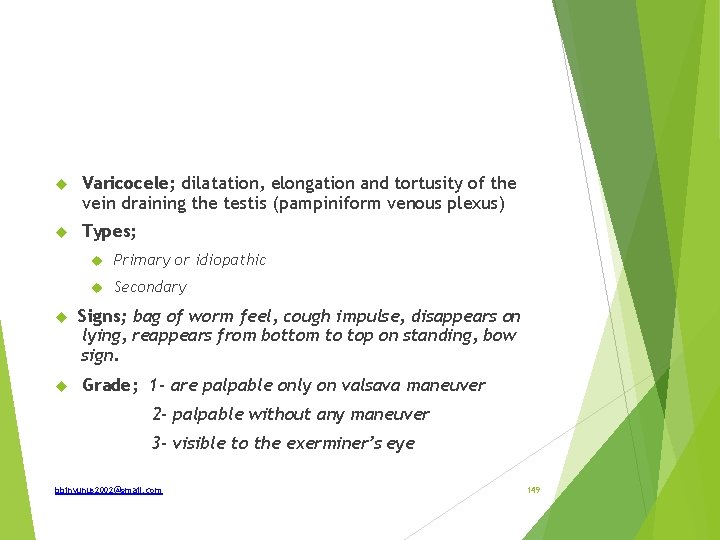
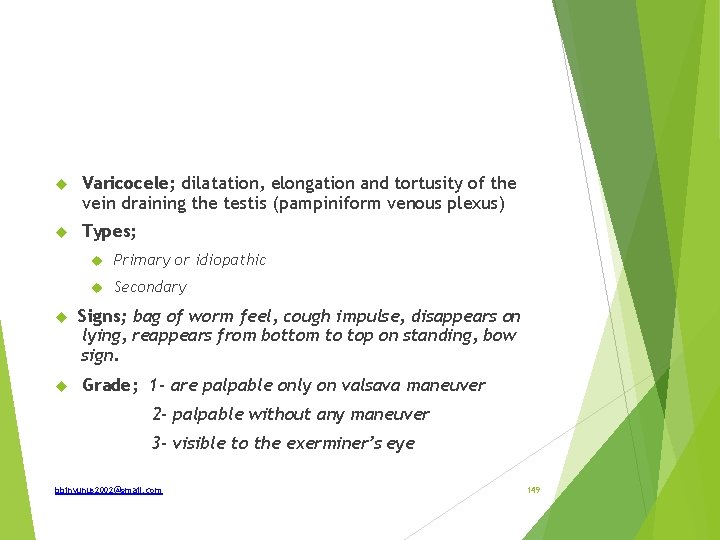
Varicocele; dilatation, elongation and tortusity of the vein draining the testis (pampiniform venous plexus) Types; Primary or idiopathic Secondary Signs; bag of worm feel, cough impulse, disappears on lying, reappears from bottom to top on standing, bow sign. Grade; 1 - are palpable only on valsava maneuver 2 - palpable without any maneuver 3 - visible to the exerminer’s eye bbinyunus 2002@gmail. com 149
Commoner on the left side because; Left spermatic vein drains into the left renal vein at rigth angle Left testicular vein is longer Absent valve at the termination of left spermatic vein Left renal vein is crossed by and may be compressed by left colon, may also be obstructed by left renal artery Metastatic renal tumour may cause obstruction of the vein Primary varicocele empties as the scrotum is elevated when patient is lying while secondary does not. bbinyunus 2002@gmail. com 150

Complication Infertility Conservative Surgery Treatment open Open ligation of varicocele – scrotal, inguinal approach(ivanissevitch procedure) and suprainguinal extraperitoneal approach (Palomo approach) Laparoscopic embolisation bbinyunus 2002@gmail. com 151

bbinyunus 2002@gmail. com 152
Generalised neurofibromatosis or Von Recklinghausen’s disease Neurofibroma; a benign tumour containing a mixture of neural(ectodermal) and fibrous(mesodermal) element. It arise not from the nerve proper but from endoneurium which is a supporting connective nerve tissue Types; Type 1 and type 2 bbinyunus 2002@gmail. com 153
Type 1 Autosomal dominant with defective gene on chromosome 17 Diagnostic criteria; two or more of; six or more cafe-au -lait > 5 mm in diameter if prepubertal individuals and> 15 mm in postpubertal individuals, Two or more neurofibroma or one plexiform neurofibroma, freckles in the axilla or groin, optic glioma, Two or more iris hamartomas, a distinctive osseous lesion such as sphenoid dysplasia or thing of long bone cortex with or without pseudoarthrosis , A first degree relative with NF-l. bbinyunus 2002@gmail. com 154
Complications of type 1; Hypertension (6%). Due to renal artey stenosis scoliosis, bowing of the legs, impaired vision, ptosis, optic atrophy, language or learning disorders , mental retardation, precocious puberty or hypogonadism, GI hemorrhage, Malignancy(5%) bbinyunus 2002@gmail. com 155
Type 2 Autosomal dominant with defect on chromosome 22 Diagnostic criteria are; Bilateral 8 th nerve masses seen with appropriate imaging techniques (e. g. CT, MRl) or One 8 th nerve mass With two of the following: neurofibroma, meningioma. , glioma, Schwannomas or posterior lenticular opacity. Complications; hearing loss. tinnitus, dizziness, loss of balance, headaches, fits. There may be a first-degree relative with NF-2. bbinyunus 2002@gmail. com 156

bbinyunus 2002@gmail. com 157

bbinyunus 2002@gmail. com 158
treatment All patients must be reviewed yearly. Surgery is employed only when there is severe cosmetic deformity , increase in. size, Evidence of malignant change, functional disturbance or pain A progressive 8 th nerve tumour that causes tinnitus or vertigo is removed while bilateral hearing remains. Any signs of epilepsy should be investigated and responsible tumours removed. Genetic counselling should also be given bbinyunus 2002@gmail. com 159

bbinyunus 2002@gmail. com 160
Identify Differential diagnosis What are radiological findings in infantile blount’s disease and angles of radiological importance Treatment bbinyunus 2002@gmail. com 161
Genu varum Differential diagnosis; Physiologic genu varum Pathologic conditions Metabolic bone disease – rickets, hypophosphatemia Asymmetrical bone arrest or retardation- blount disease, trauma near the growth epiphysis of femur, osteomyelitis, tumour affecting the lower end of femur and upper tibia. Bone dysplasia; metaphysical chrondrodysplasia Congenital; deficient tibia relative to long fibula Neuromuscular; in adult, degenerative disorders(osteoarthritis of the knee) and paget’s disease are important causes. bbinyunus 2002@gmail. com 162
AP and lateral Xray ; Flattening or disappearance of the medial aspect of the epiphysis and apparent increase in the height of the lateral aspect of the epiphyseal plate Breaking of the proximal medial tibial metaphysis Fragmentation with a protuberant step deformity Angles of radiological importance; Metaphysial- diaphyseal angle Tibiofemoral angle Metaphyseal- epiphyseal angle bbinyunus 2002@gmail. com 163
Metaphyseal-diaphyseal angle is important in differentiating Blount’s disease from physiological bowing in a child less than 2 years MDA< 11° normalphysiologic bowing MDA 11 -15° equivocal MDA> 15° blount disease bbinyunus 2002@gmail. com 164
Treatment Non-surgical; Observation and trial of bracing (2 -5 years) Surgical Corrective osteotomy aiming at 6 -10° of valgus Others; Hemiepiphysiodesis Asymmetric physeal extraction External fixation with distraction osteogenesis bbinyunus 2002@gmail. com 165

bbinyunus 2002@gmail. com 166

Identify What are the causes Treatment Genu valgum (knock knee) Causes; Idiopathic Bone softening; rickets, osteomalecia, paget disease Laxity of ligament; medial collateral ligament Trauma; lateral tibial condyle Ostheoathritis Muscle weakness NB; intermalleola distance > 10 cm bbinyunus 2002@gmail. com 167

Treatment Non-operative Idopathic- ignored <7 years Raising inner side of the heel by 3 -4 mm Using splint Operative; For > 10 years Risk factor corrected Stapling innerside of epiphysis to stop growing Supracondylar osteotomy, after growth is completed bbinyunus 2002@gmail. com 168

bbinyunus 2002@gmail. com 169
State two (2) differential diagnoses. Give one major reason why Burkitt’s tumour is not a likely differential diagnosis of this particular lesion. State (a) types of Surgical treatment that may be offered and (b) for which types of cases? List two major complications that may follow surgical treatment in this specific case. bbinyunus 2002@gmail. com 170
Differentials 1. Benign Parotid tumour a. Pleomorphic adenoma (mixed parotid tumour) – 60% b. Monomorphic adenoma (Adenolymphoma - Warthin's Tumour) – 10% 2. Malignant Parotid tumour a. Mucoepidermoid tumour ) b. Acinic cell tumour ) – 4% c. Adenoid cystic carcinoma ) Investigations 1. FNAC helps to diagnose most cases of malignancies but it is not always reliable. Frozen section also gives some false-positive results. 2. CT is the most accurate investigation. It helps to determine the local and regional extent of the disease. Treatment Superficial/total Parotidectomy 1. Benign mixed tumors arising in the lateral lobe. Wide excision to prevent recurrence. a. Identify the facial nerve and branches b. Facial nerve may be excised if involved in malignancy c. Medial lobe involvement may require a total parotidectomy bbinyunus 2002@gmail. com 171
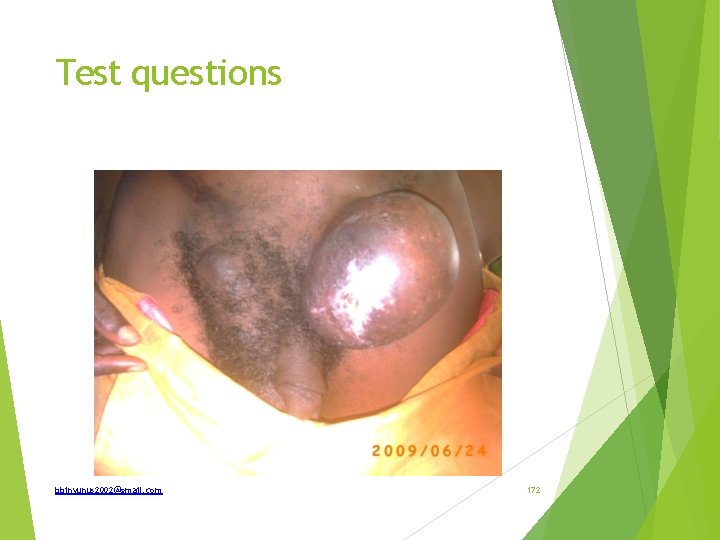
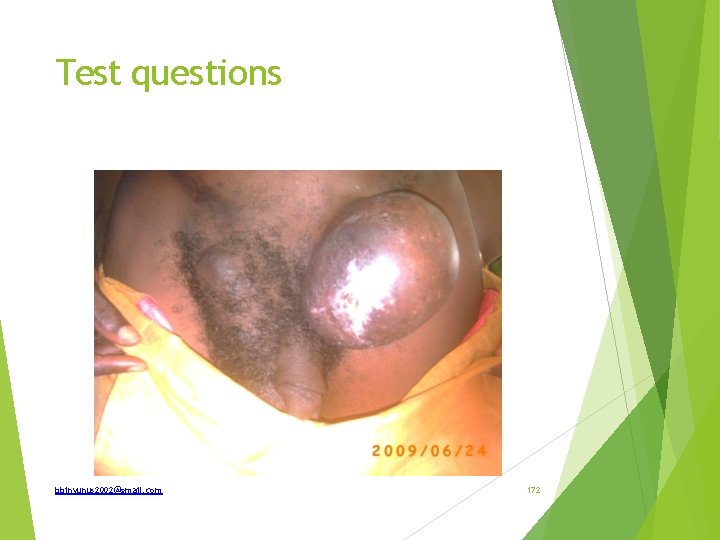
Test questions bbinyunus 2002@gmail. com 172

bbinyunus 2002@gmail. com 173
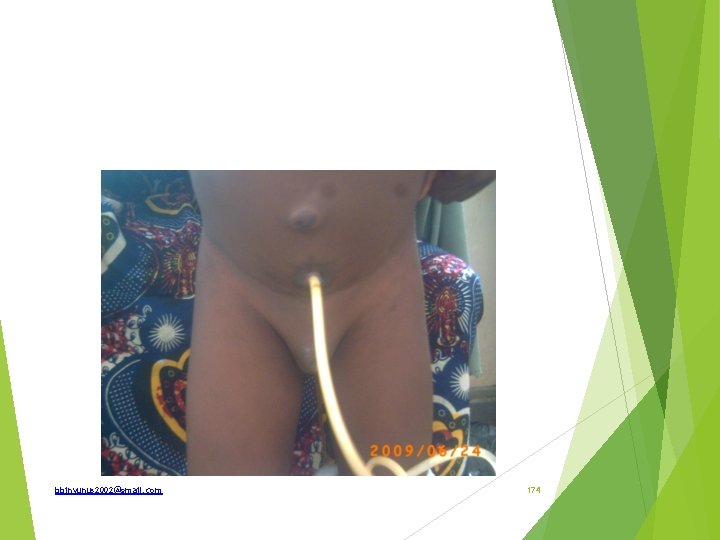
bbinyunus 2002@gmail. com 174
Appreciation Dr Bashir Bn. Yunus bbinyunus 2002@gmail. com 175