NIHSS ASSESSMENT AND MODIFIED RANKIN SCALE Clinical Education





- Slides: 38
NIHSS ASSESSMENT AND MODIFIED RANKIN SCALE Clinical Education Marshall Browning Hospital ASRH
Objectives �Discuss National Institute of Health Stroke Scale (NIHSS) �Be able to perform & accurately score the NIHSS �Discuss common pitfalls
What is the NIHSS? �Standardized and repeatable assessment of stroke patients ◦ High intra/interobserver reliability (RNs/physicians) �Clinical research and communication tool �Can predict stroke severity & outcomes

What is the NIHSS not? �It is NOT a complete neurologic evaluation & does not substitute for one �Will miss some posterior circulation strokes, will miss small isolated cortical strokes (i. e. strokes which affect only the distal hand) �Neurologic examination can be thought of as a “flexible tool”
What does it do? � 15 parts �Tests language, vision, motor, sensory, coordination � 0 = no detectable deficits
Common pitfall You don’t do this every day, so you are not sure how exactly to perform or score the exam. That is why we updated our NIHSS forms. They have explicit instructions copied directly from the NIH. For more stroke materials go to: https: //stroke. nih. gov Do NOT try to depend on your memory to accurately perform the NIHSS.
Same way, Every Time • To ensure reliability and reproducibility of results, examiner-patient interactions should be as uniform as possible. • Administer the stroke scale in the exact order. • Avoid coaching the patient. • Accept the patient’s first effort. • Score only what the patient DOES, not what you think they can do. • Include all deficits in scoring, even those from prior strokes.

1 a – Level of consciousness 0 = Alert; keenly responsive. 1 = Not alert; but arousable by minor stimulation to obey, answer, or respond. 2 = Not alert; requires repeated stimulation to attend, or is obtunded and requires strong or painful stimulation to make movements (not stereotyped). 3 = Responds only with reflex motor or autonomic effects or totally unresponsive, flaccid, and areflexic.
1 b – Level of consciousness (Questions) � Ask patient the month & age � No partial credit for being close � Accept the first answer only 0 = Answers both questions correctly. 1 = Answers one question correctly. 2 = Answers neither question correctly. • Impaired in patients with aphasia. • Most commonly seen with strokes in the left MCA territory. • Can be seen with gross encephalopathy.
1 c – Level of consciousness (Commands) � Ask patient to open and close eyes � Ask patient to grip and release the non-paretic hand � If the patient does not respond, demonstrate the command. Some patients may not be able to respond to your verbal cues, but be able to mimic your demonstration. � 0 � 1 � 2 This is consistent with impaired comprehension from stroke, most commonly seen with left MCA territory strokes. = Performs both tasks correctly. = Performs one task correctly. = Performs neither task correctly.
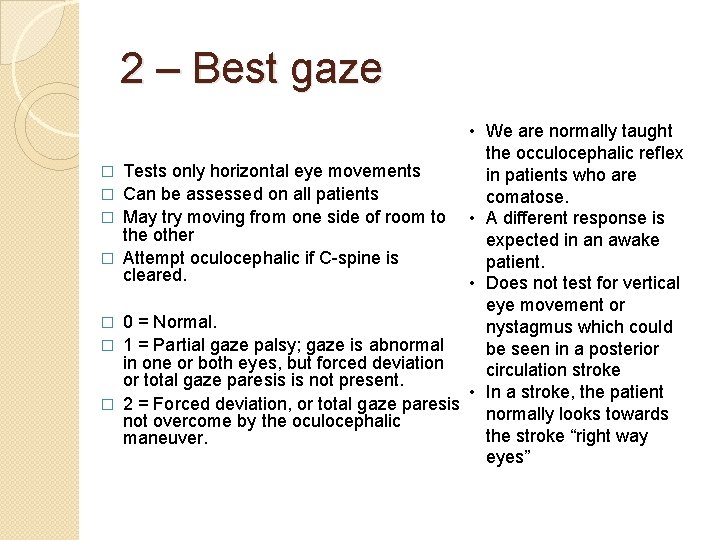
2 – Best gaze � � � � • We are normally taught the occulocephalic reflex Tests only horizontal eye movements in patients who are Can be assessed on all patients comatose. May try moving from one side of room to • A different response is the other expected in an awake Attempt oculocephalic if C-spine is patient. cleared. • Does not test for vertical eye movement or 0 = Normal. nystagmus which could 1 = Partial gaze palsy; gaze is abnormal be seen in a posterior in one or both eyes, but forced deviation circulation stroke or total gaze paresis is not present. • In a stroke, the patient 2 = Forced deviation, or total gaze paresis normally looks towards not overcome by the oculocephalic the stroke “right way maneuver. eyes”
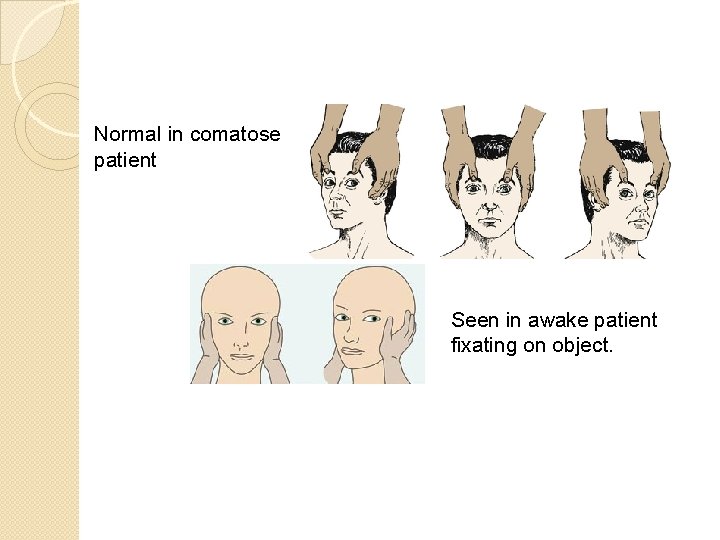
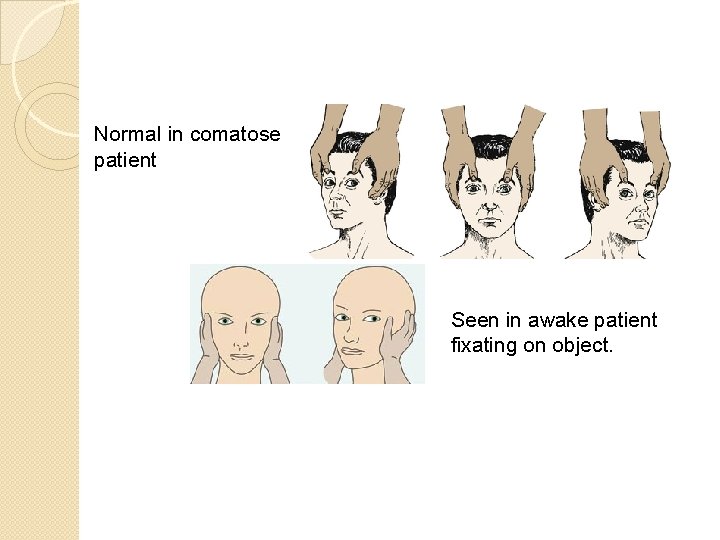
Normal in comatose patient Seen in awake patient fixating on object.
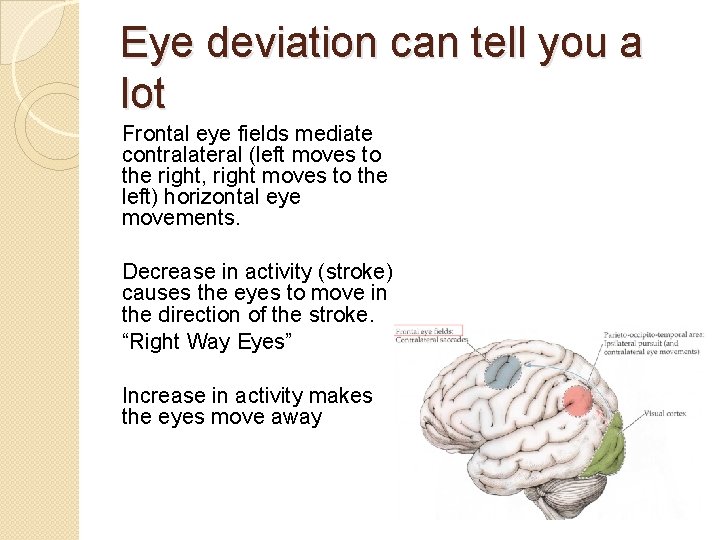
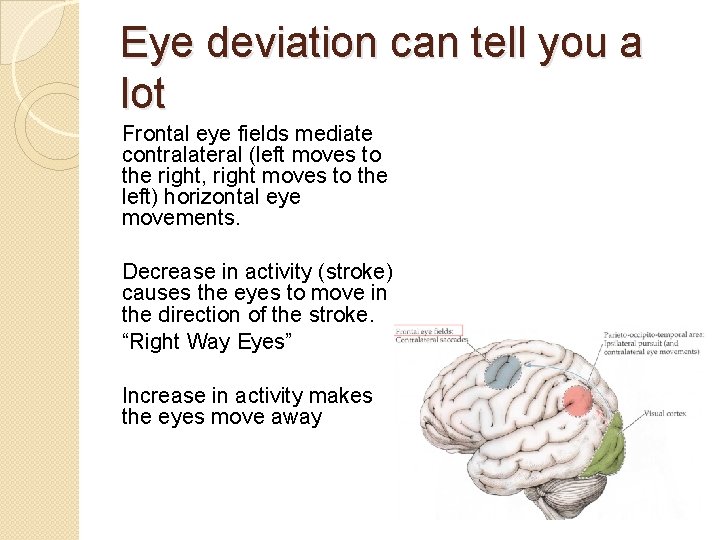
Eye deviation can tell you a lot Frontal eye fields mediate contralateral (left moves to the right, right moves to the left) horizontal eye movements. Decrease in activity (stroke) causes the eyes to move in the direction of the stroke. “Right Way Eyes” Increase in activity makes the eyes move away
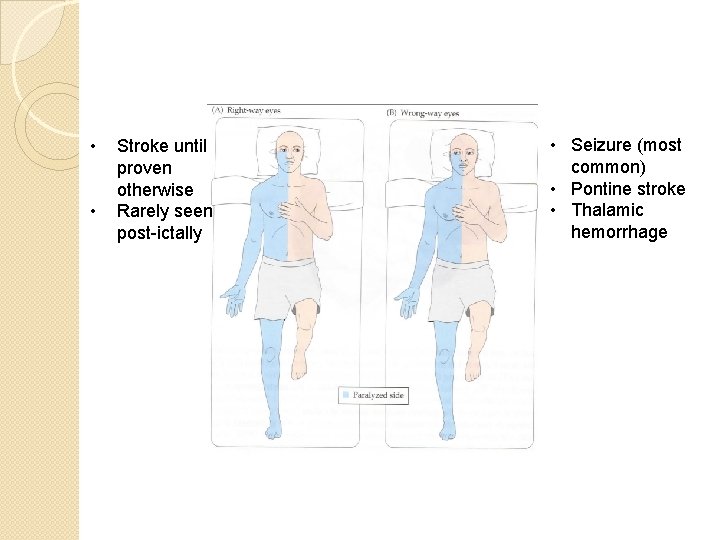
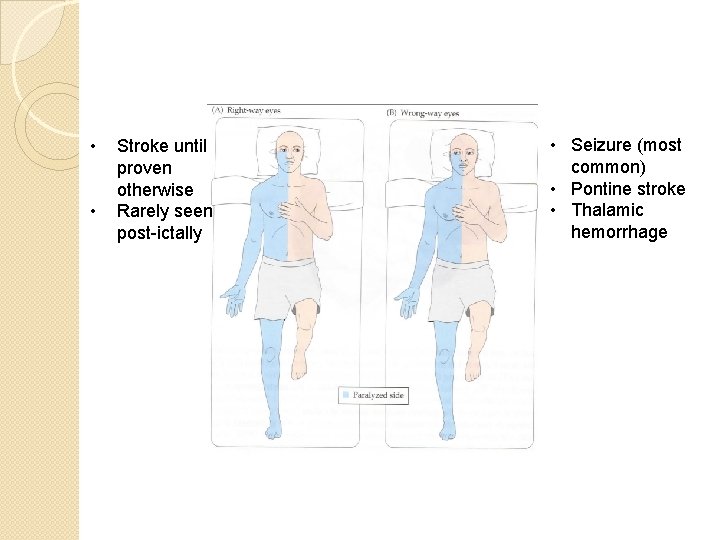
• • Stroke until proven otherwise Rarely seen post-ictally • Seizure (most common) • Pontine stroke • Thalamic hemorrhage
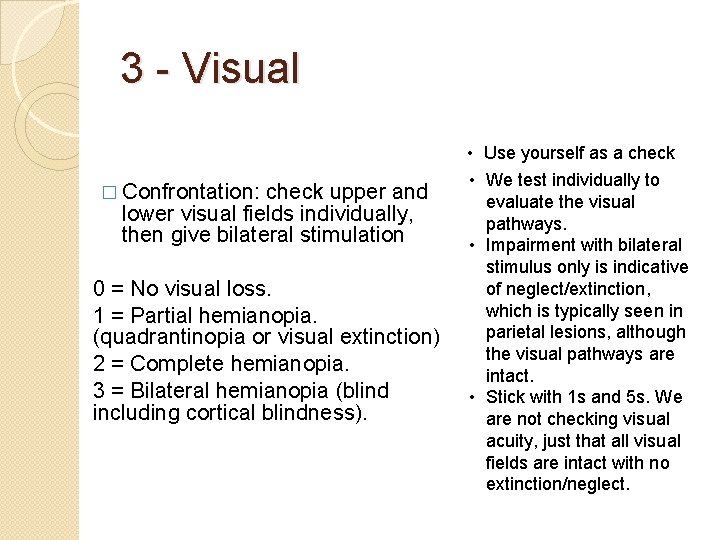
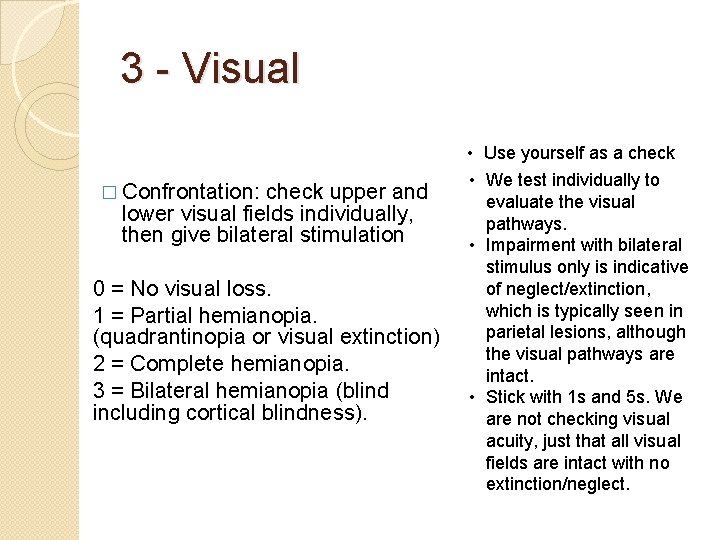
3 - Visual � Confrontation: check upper and lower visual fields individually, then give bilateral stimulation 0 = No visual loss. 1 = Partial hemianopia. (quadrantinopia or visual extinction) 2 = Complete hemianopia. 3 = Bilateral hemianopia (blind including cortical blindness). • Use yourself as a check • We test individually to evaluate the visual pathways. • Impairment with bilateral stimulus only is indicative of neglect/extinction, which is typically seen in parietal lesions, although the visual pathways are intact. • Stick with 1 s and 5 s. We are not checking visual acuity, just that all visual fields are intact with no extinction/neglect.
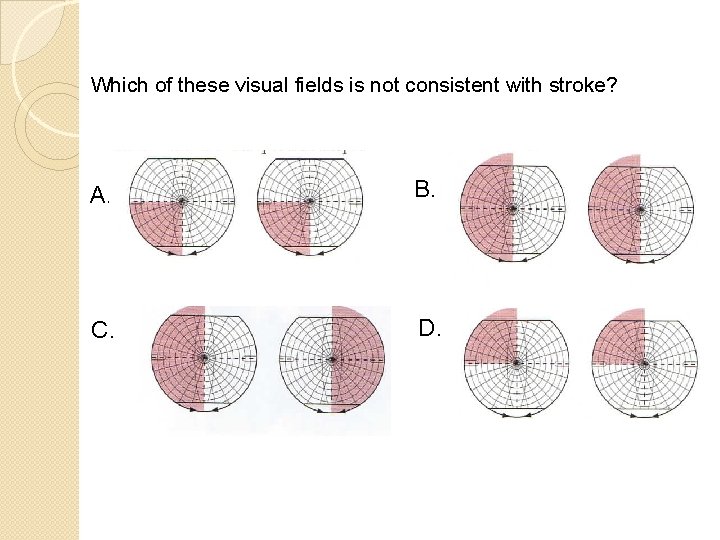
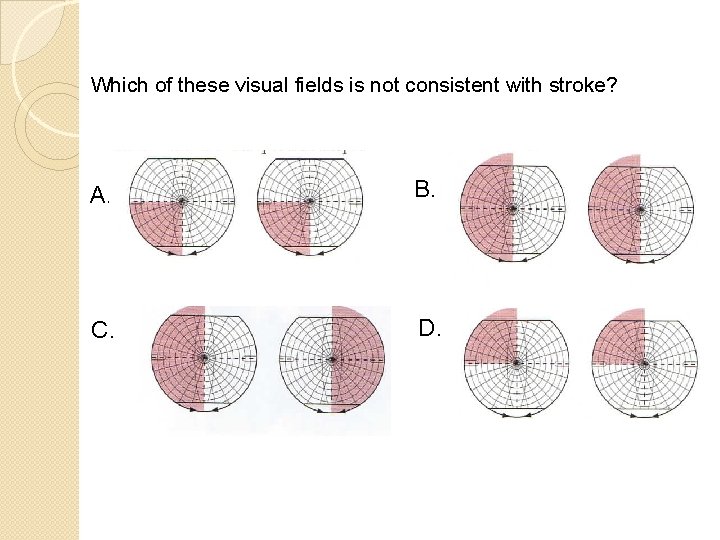
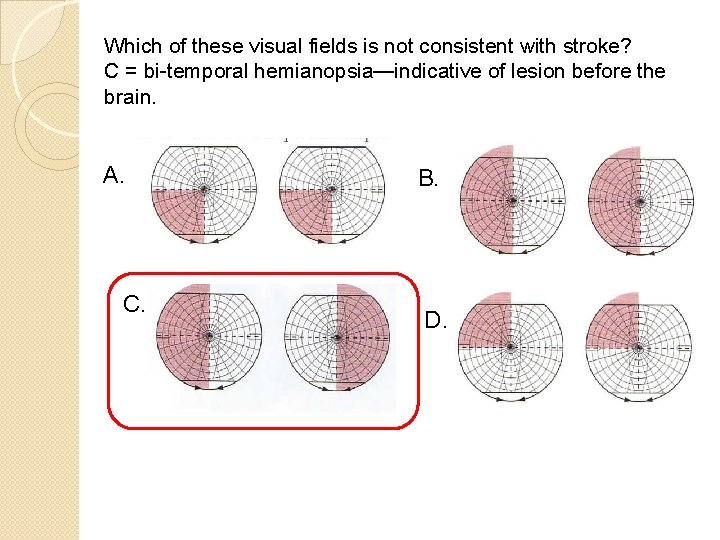
Which of these visual fields is not consistent with stroke? A. B. C. D.
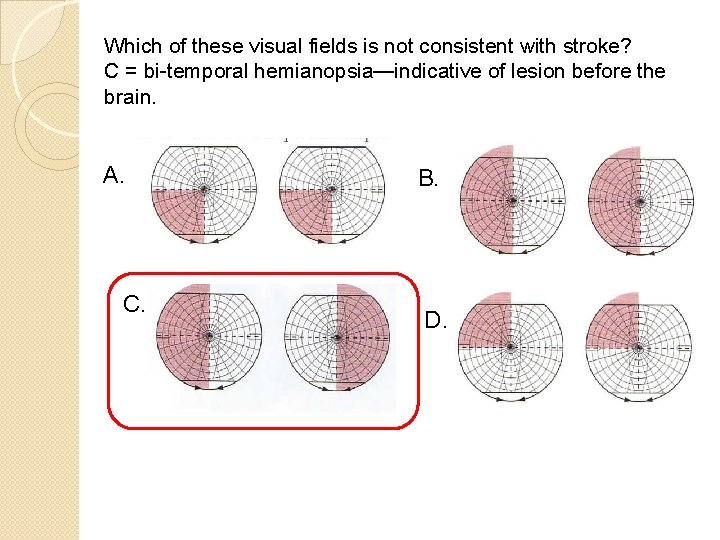
Which of these visual fields is not consistent with stroke? C = bi-temporal hemianopsia—indicative of lesion before the brain. A. C. B. D.
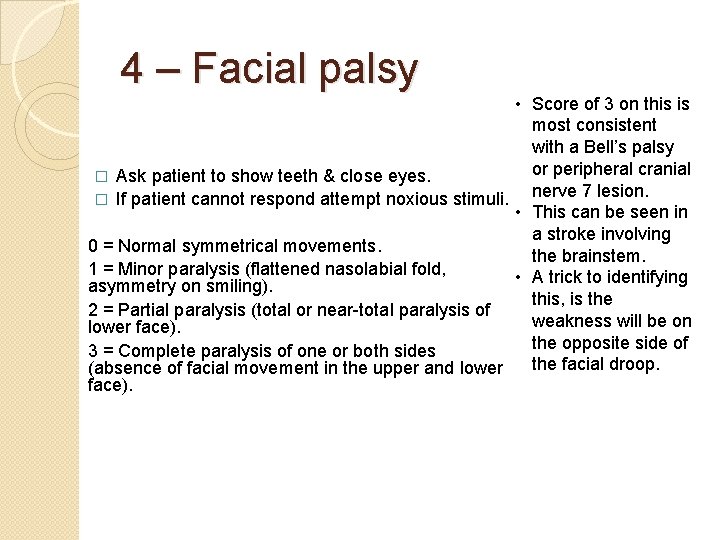
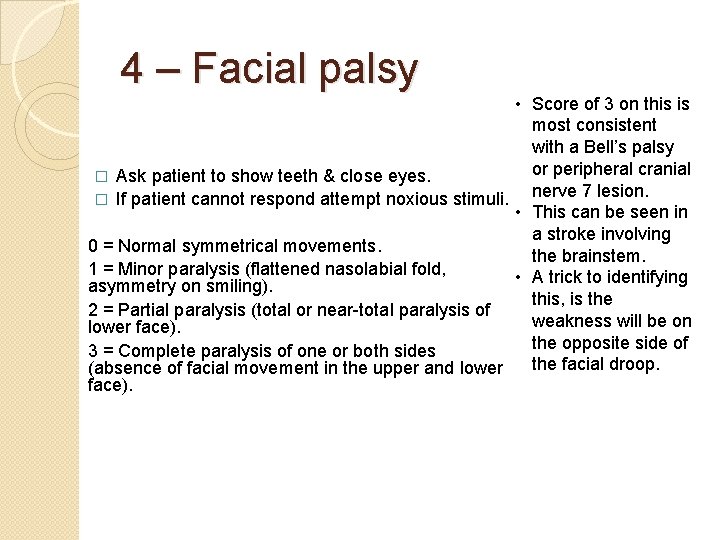
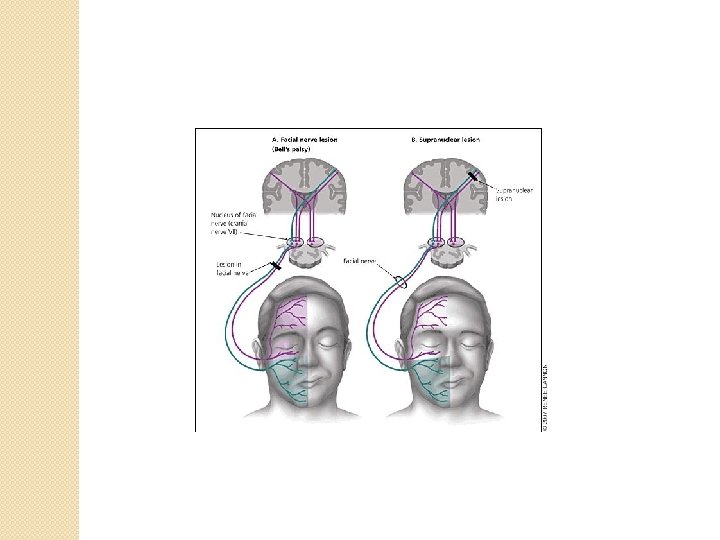
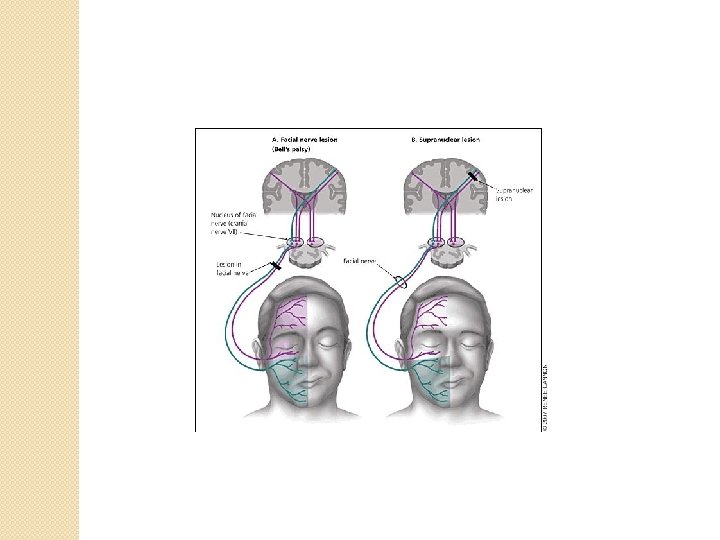
4 – Facial palsy • Score of 3 on this is most consistent with a Bell’s palsy or peripheral cranial � Ask patient to show teeth & close eyes. nerve 7 lesion. � If patient cannot respond attempt noxious stimuli. • This can be seen in a stroke involving 0 = Normal symmetrical movements. the brainstem. 1 = Minor paralysis (flattened nasolabial fold, • A trick to identifying asymmetry on smiling). this, is the 2 = Partial paralysis (total or near-total paralysis of weakness will be on lower face). the opposite side of 3 = Complete paralysis of one or both sides the facial droop. (absence of facial movement in the upper and lower face).
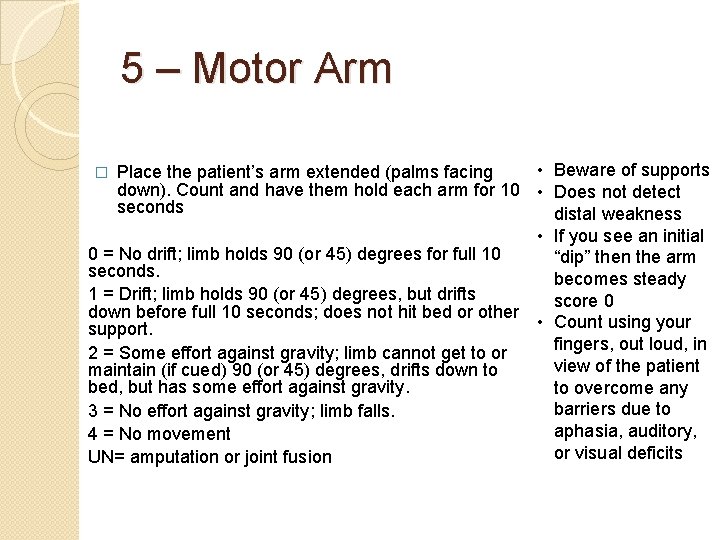
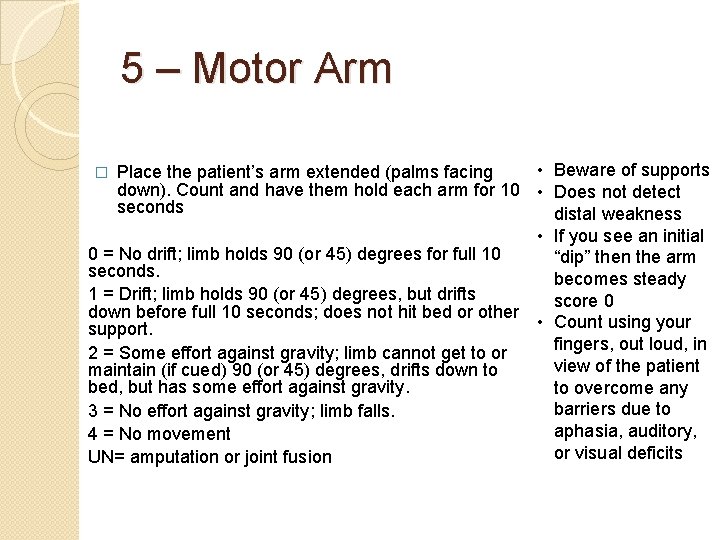
5 – Motor Arm • Beware of supports Place the patient’s arm extended (palms facing down). Count and have them hold each arm for 10 • Does not detect seconds distal weakness • If you see an initial 0 = No drift; limb holds 90 (or 45) degrees for full 10 “dip” then the arm seconds. becomes steady 1 = Drift; limb holds 90 (or 45) degrees, but drifts score 0 down before full 10 seconds; does not hit bed or other • Count using your support. fingers, out loud, in 2 = Some effort against gravity; limb cannot get to or view of the patient maintain (if cued) 90 (or 45) degrees, drifts down to bed, but has some effort against gravity. to overcome any barriers due to 3 = No effort against gravity; limb falls. aphasia, auditory, 4 = No movement or visual deficits UN= amputation or joint fusion �
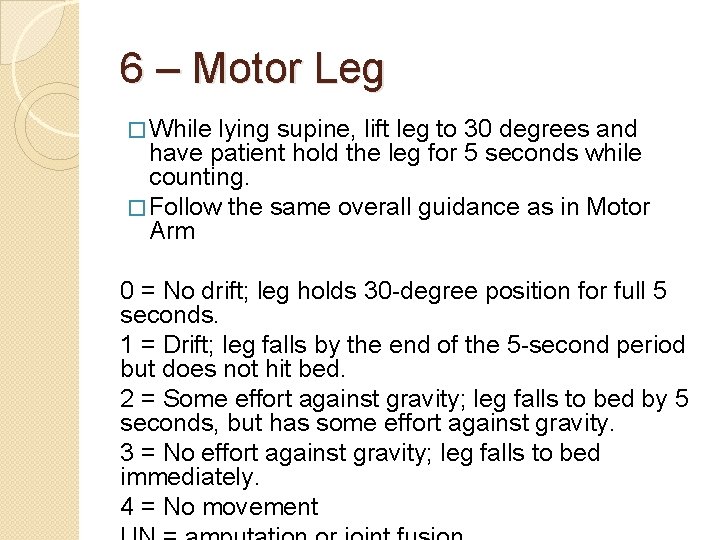
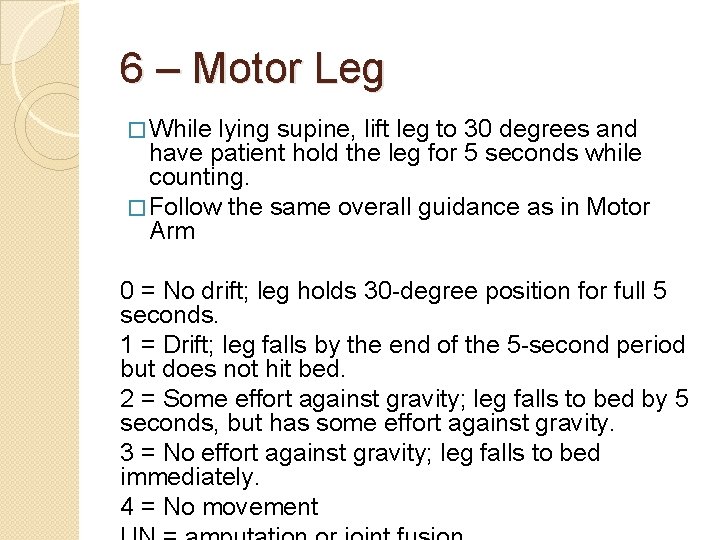
6 – Motor Leg � While lying supine, lift leg to 30 degrees and have patient hold the leg for 5 seconds while counting. � Follow the same overall guidance as in Motor Arm 0 = No drift; leg holds 30 -degree position for full 5 seconds. 1 = Drift; leg falls by the end of the 5 -second period but does not hit bed. 2 = Some effort against gravity; leg falls to bed by 5 seconds, but has some effort against gravity. 3 = No effort against gravity; leg falls to bed immediately. 4 = No movement
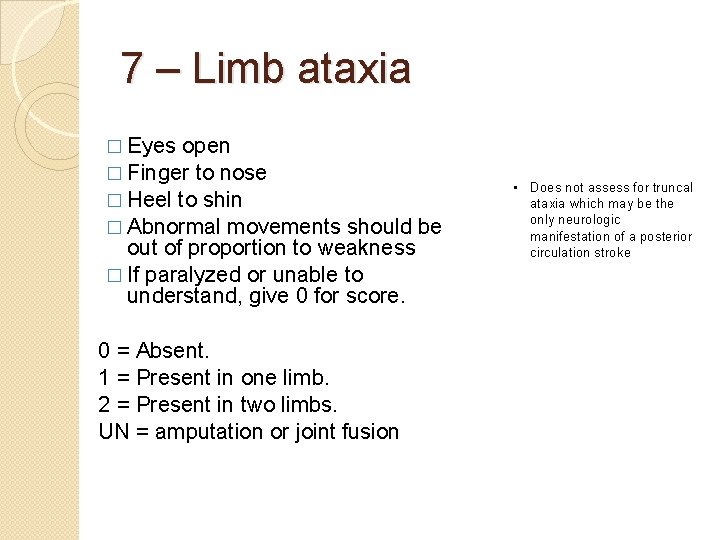
7 – Limb ataxia � Eyes open � Finger to nose � Heel to shin � Abnormal movements should be out of proportion to weakness � If paralyzed or unable to understand, give 0 for score. 0 = Absent. 1 = Present in one limb. 2 = Present in two limbs. UN = amputation or joint fusion • Does not assess for truncal ataxia which may be the only neurologic manifestation of a posterior circulation stroke
Apraxia and ataxia Apraxia (noun) Total or partial loss of the ability to perform coordinated movements or manipulate objects in the absence of motor or sensory impairment; specifically, a disorder of motor planning. Think initiation Ataxia (noun) Lack of coordination while performing voluntary movements, which may appear to be clumsiness, inaccuracy, or instability. Think coordination.
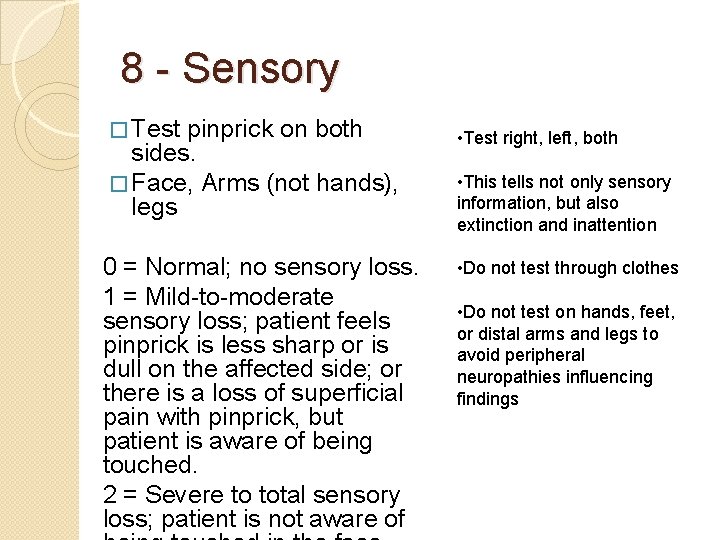
8 - Sensory � Test pinprick on both sides. � Face, Arms (not hands), legs 0 = Normal; no sensory loss. 1 = Mild-to-moderate sensory loss; patient feels pinprick is less sharp or is dull on the affected side; or there is a loss of superficial pain with pinprick, but patient is aware of being touched. 2 = Severe to total sensory loss; patient is not aware of • Test right, left, both • This tells not only sensory information, but also extinction and inattention • Do not test through clothes • Do not test on hands, feet, or distal arms and legs to avoid peripheral neuropathies influencing findings
Communication Matters

9 – Best language What is happening in this picture?
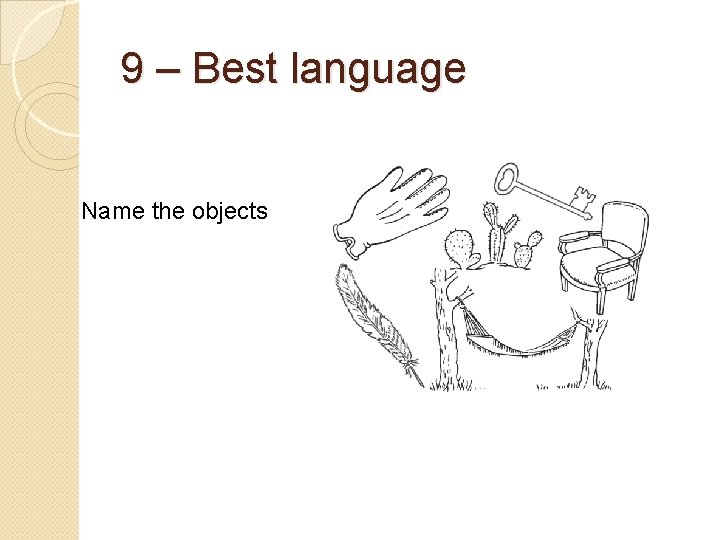
9 – Best language Name the objects

9 – Best language Read this out loud
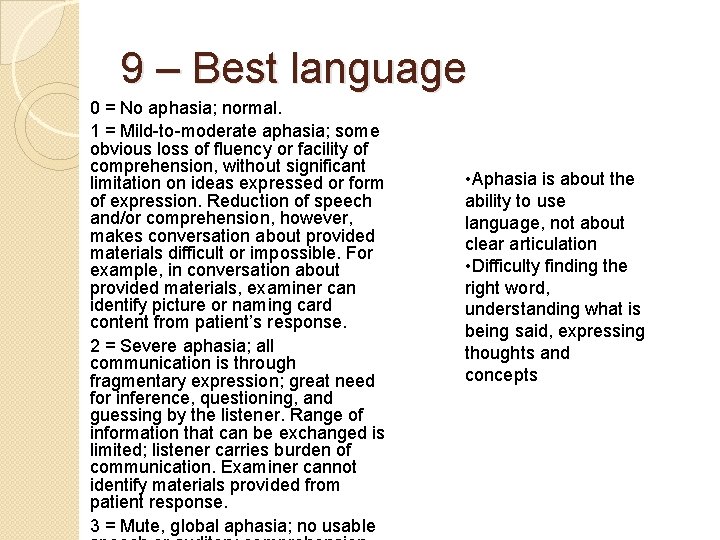
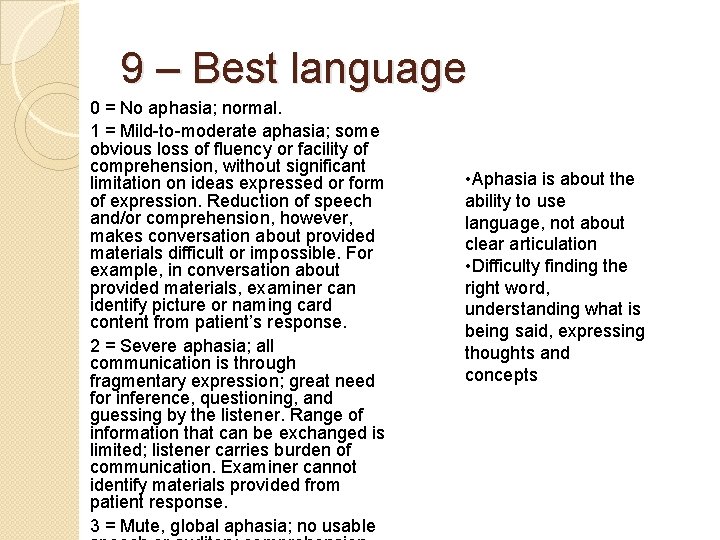
9 – Best language 0 = No aphasia; normal. 1 = Mild-to-moderate aphasia; some obvious loss of fluency or facility of comprehension, without significant limitation on ideas expressed or form of expression. Reduction of speech and/or comprehension, however, makes conversation about provided materials difficult or impossible. For example, in conversation about provided materials, examiner can identify picture or naming card content from patient’s response. 2 = Severe aphasia; all communication is through fragmentary expression; great need for inference, questioning, and guessing by the listener. Range of information that can be exchanged is limited; listener carries burden of communication. Examiner cannot identify materials provided from patient response. 3 = Mute, global aphasia; no usable • Aphasia is about the ability to use language, not about clear articulation • Difficulty finding the right word, understanding what is being said, expressing thoughts and concepts
There is much more to the S in FAST than just slurred speech
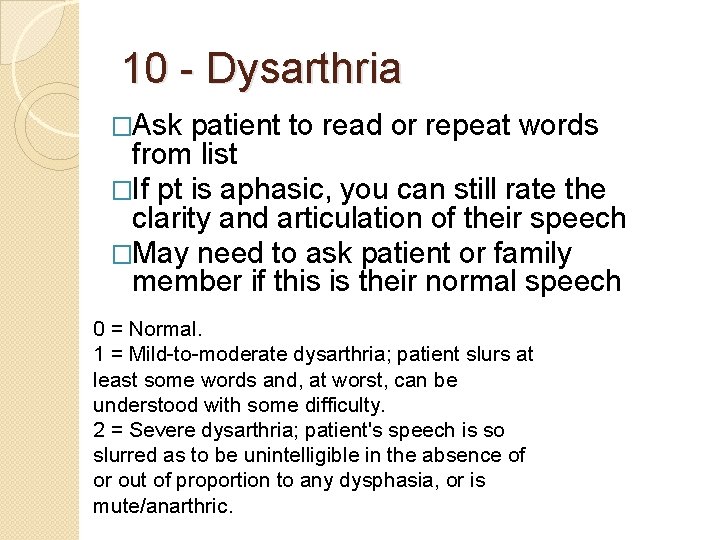
10 - Dysarthria �Ask patient to read or repeat words from list �If pt is aphasic, you can still rate the clarity and articulation of their speech �May need to ask patient or family member if this is their normal speech 0 = Normal. 1 = Mild-to-moderate dysarthria; patient slurs at least some words and, at worst, can be understood with some difficulty. 2 = Severe dysarthria; patient's speech is so slurred as to be unintelligible in the absence of or out of proportion to any dysphasia, or is mute/anarthric.

10 --Dysarthria Read or repeat
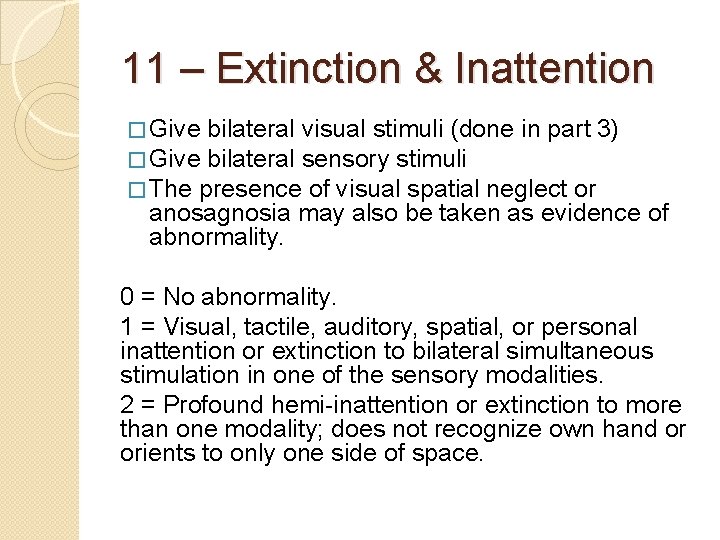
11 – Extinction & Inattention � Give bilateral visual stimuli (done in part 3) � Give bilateral sensory stimuli � The presence of visual spatial neglect or anosagnosia may also be taken as evidence of abnormality. 0 = No abnormality. 1 = Visual, tactile, auditory, spatial, or personal inattention or extinction to bilateral simultaneous stimulation in one of the sensory modalities. 2 = Profound hemi-inattention or extinction to more than one modality; does not recognize own hand or orients to only one side of space.
Questions?
References https: //www. nih. gov/ Blumenfeld, Neuroanatomy through Clinical Cases “Overview of the evaluation of stroke, ” Uptodate. com Adams H, Davis P, Hansen M, et al. "Baseline NIH Stroke Scale score strongly predicts outcome after stroke - A report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST)". Muir KW, Weir CJ, Murray GD, Povey C, Lees KR (1996). "Comparison of neurological scales and scoring systems for acute stroke prognosis". Stroke. 27: 1817– 1820. Neurology, 2015. Brian Katz et all, “Interrater Reliability of the National Institutes of Health Stroke Scale: Rating by Emergency Room Physicians and Neurologists in a Population-Based Study”
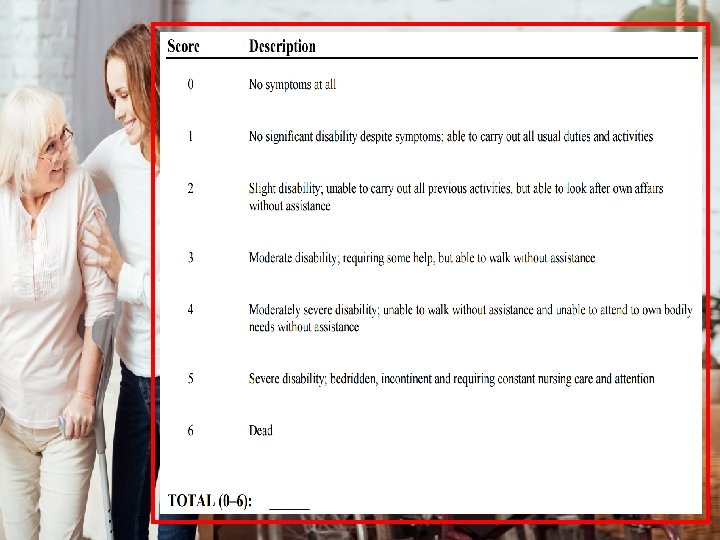
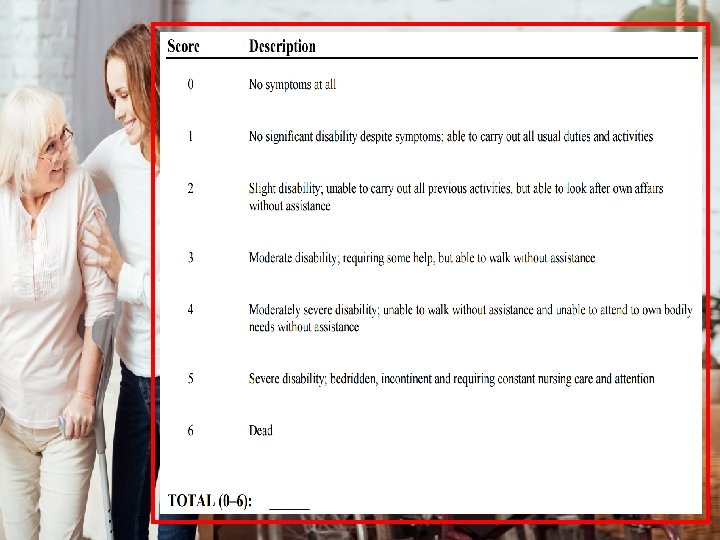
MRS (modified Rankin Scale) t u The modified Rankin Scale (m. RS) is a commonly used scale for measuring the degree of disability or dependence in the daily activities of people who have suffered a stroke or other causes of neurological disability. u It has become the most widely used clinical outcome measure for stroke clinical trials.
MRS – Summary and Key Points u The MRS is a standard function outcome measure in clinical stroke trials u The exam is scored based on current overall function, not just what is attributed to stroke deficits Questions?