NICE guidelines for management of labour First stage
NICE guidelines for management of labour: First stage of labour Bronselaer Bart 21 -02 -2008 Pretoria, South Africa
Aim of guideline • Clinical guidelines have been defined as ‘systematically developed statements which assist clinicians and patients in making decisions about appropriate treatment for specific conditions’. • The guideline has been developed with the aim of providing guidance on care of healthy women and their babies during childbirth.

Normal labour: Friedman’s curve (1967)

Normal labour: First stage Definition • Latent first stage of labour – a period of time, not necessarily continuous, when: – there are painful contractions, and – there is some cervical change, including cervical effacement and dilatation up to 4 cm. • Active first stage of labour – when: – there are regular painful contractions, and – there is progressive cervical dilatation from 4 cm.
Duration of the first stage • Length of established first stage of labour varies between women. First labours last on average 8 hours and are unlikely to last over 18 hours. Second and subsequent labours last on average 5 hours and are unlikely to last over 12 hours • Cervical dilatation of 2 cm in 4 hours for first labours (0, 5 cm/h)
Duration of the first stage: South-Africa • Philpott and Castle 1972: - Introduction of Alert line in primigravidae - Cervical dilatation of 1 cm in 1 hour - slowest progressing 20% of primigravidae
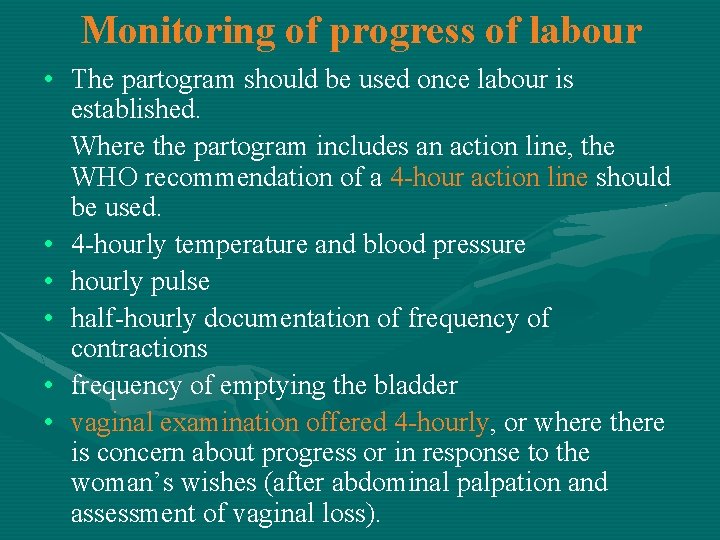
Monitoring of progress of labour • The partogram should be used once labour is established. Where the partogram includes an action line, the WHO recommendation of a 4 -hour action line should be used. • 4 -hourly temperature and blood pressure • hourly pulse • half-hourly documentation of frequency of contractions • frequency of emptying the bladder • vaginal examination offered 4 -hourly, or where there is concern about progress or in response to the woman’s wishes (after abdominal palpation and assessment of vaginal loss).

WHO partogram
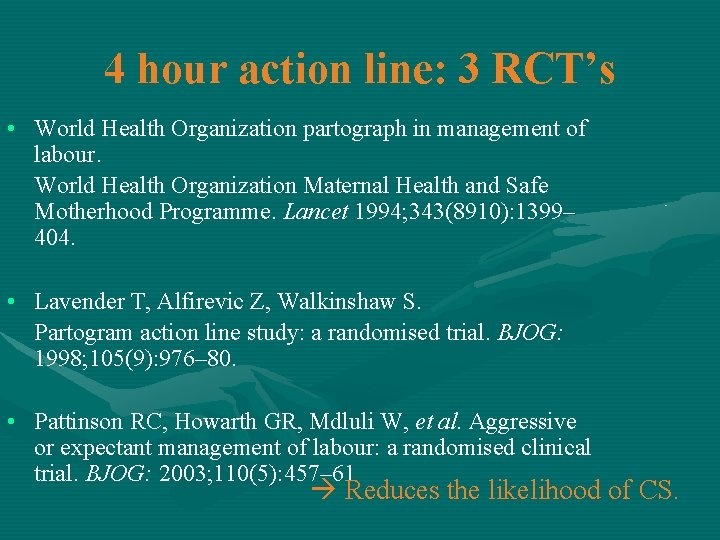
4 hour action line: 3 RCT’s • World Health Organization partograph in management of labour. World Health Organization Maternal Health and Safe Motherhood Programme. Lancet 1994; 343(8910): 1399– 404. • Lavender T, Alfirevic Z, Walkinshaw S. Partogram action line study: a randomised trial. BJOG: 1998; 105(9): 976– 80. • Pattinson RC, Howarth GR, Mdluli W, et al. Aggressive or expectant management of labour: a randomised clinical trial. BJOG: 2003; 110(5): 457– 61 Reduces the likelihood of CS.
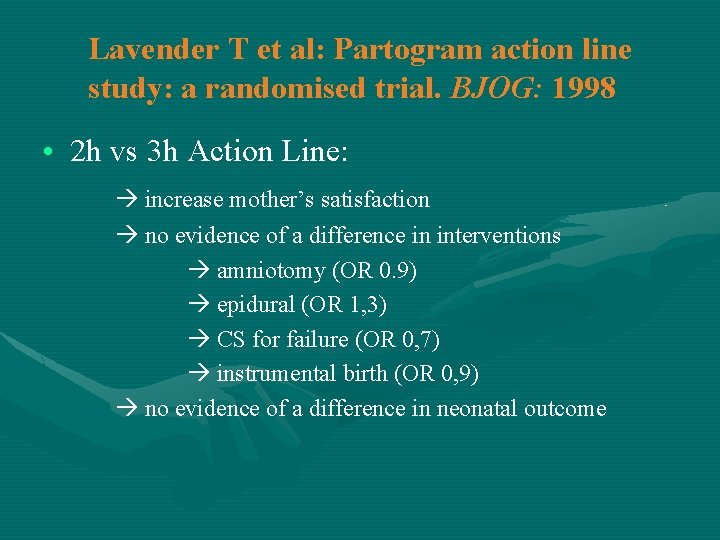
Lavender T et al: Partogram action line study: a randomised trial. BJOG: 1998 • 2 h vs 3 h Action Line: increase mother’s satisfaction no evidence of a difference in interventions amniotomy (OR 0. 9) epidural (OR 1, 3) CS for failure (OR 0, 7) instrumental birth (OR 0, 9) no evidence of a difference in neonatal outcome
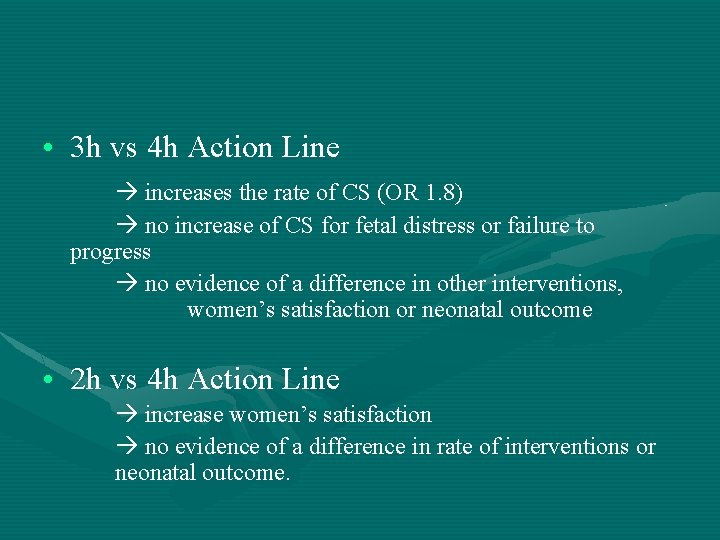
• 3 h vs 4 h Action Line increases the rate of CS (OR 1. 8) no increase of CS for fetal distress or failure to progress no evidence of a difference in other interventions, women’s satisfaction or neonatal outcome • 2 h vs 4 h Action Line increase women’s satisfaction no evidence of a difference in rate of interventions or neonatal outcome.
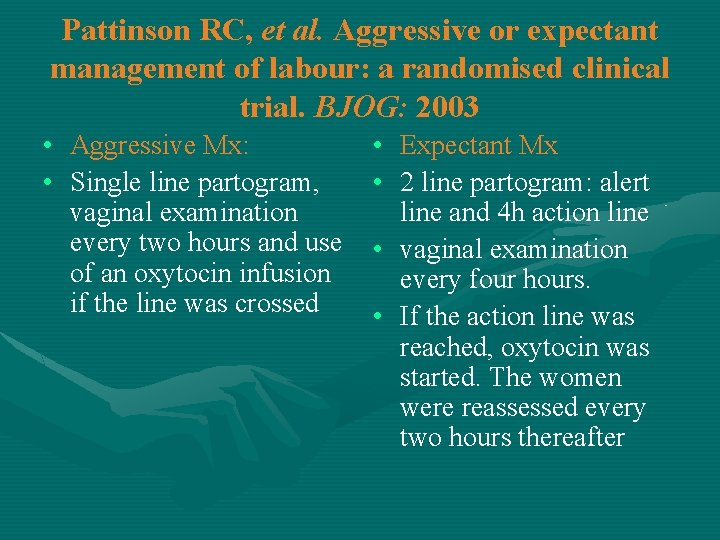
Pattinson RC, et al. Aggressive or expectant management of labour: a randomised clinical trial. BJOG: 2003 • Aggressive Mx: • Single line partogram, vaginal examination every two hours and use of an oxytocin infusion if the line was crossed • Expectant Mx • 2 line partogram: alert line and 4 h action line • vaginal examination every four hours. • If the action line was reached, oxytocin was started. The women were reassessed every two hours thereafter
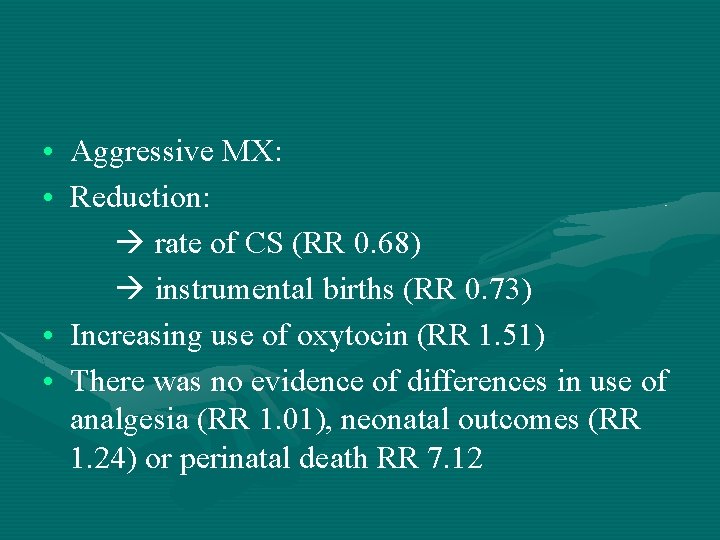
• Aggressive MX: • Reduction: rate of CS (RR 0. 68) instrumental births (RR 0. 73) • Increasing use of oxytocin (RR 1. 51) • There was no evidence of differences in use of analgesia (RR 1. 01), neonatal outcomes (RR 1. 24) or perinatal death RR 7. 12
• Evidence from low income settings show that the use of partograms, that have an action line, increases vaginal birth and reduces maternal morbidity. • A 4 hour action line is associated with fewer intrapartum interventions than a 2 hour action line with the same outcomes. • There is no current evidence on the efficacy or otherwise of partograms without action or alert lines. Placing an action line earlier than that recommended by the WHO (at 4 hours) increases interventions without any benefit in outcomes to either woman or baby.
4 hourly vaginal examination • Abukhalil et al. 1996; 109 nulliparous in spt labour at term 2 hourly VS 4 hourly VE no significant difference in duration of labour no difference in the number of VEs increase maternal and neonatal sepsis when PPROM
• In normally progressing labour, amniotomy should not be performed routinely. • Combined early amniotomy with use of oxytocin should not be used routinely.

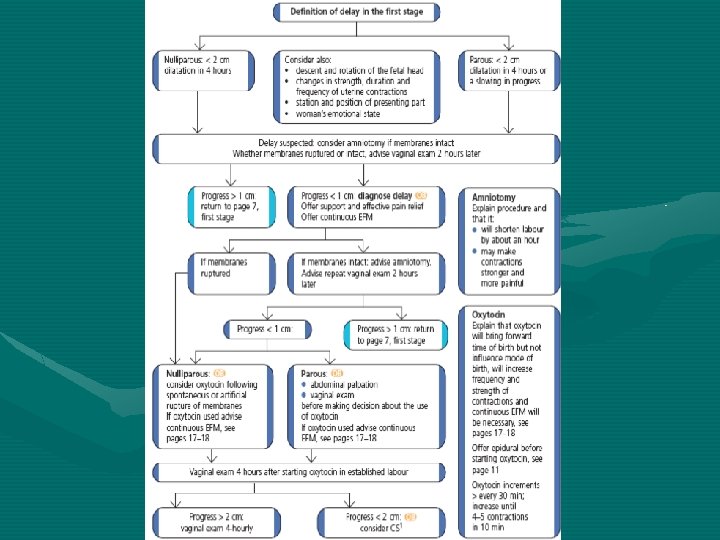
Delay in active first stage of labour • Cervical dilatation of less than 2 cm in 4 hours for first labours (< 0, 5 cm/h) • Cervical dilatation of less than 2 cm in 4 hours or a slowing in the progress of labour for second or subsequent labours • Descent and rotation of the fetal head • Changes in the strength, duration and frequency of uterine contractions.
Managing active phase South Africa • 2 hourly VE, Transfer line • Progress to left of alert line: Continu monitoring mother and fetus • Progress crosses alert line: Make diagnose and act: 4 P’s (Patient, Power, Passenger, Passage)
Patient, Passenger • Malposition, maternal distress, pain, dehydration improve maternal status, reassess in 2 h if left of TL: reassess in 2 h if crosses TL: consider C/S
Power • Poor contractions: start Oxytocinon safely Passage • Disproportion: consider C/S

Thank You
- Slides: 22