Newborn Resuscitation Program NRP By Dr Mohamed Abdelmaaboud
Newborn Resuscitation Program (NRP) By Dr. Mohamed Abdelmaaboud, MD Prof and Head of Pediatric Department Minia University
7 th Edition NRP Guidelines 5 year evidence based topic review by The International Liaison Committee On Resuscitation.
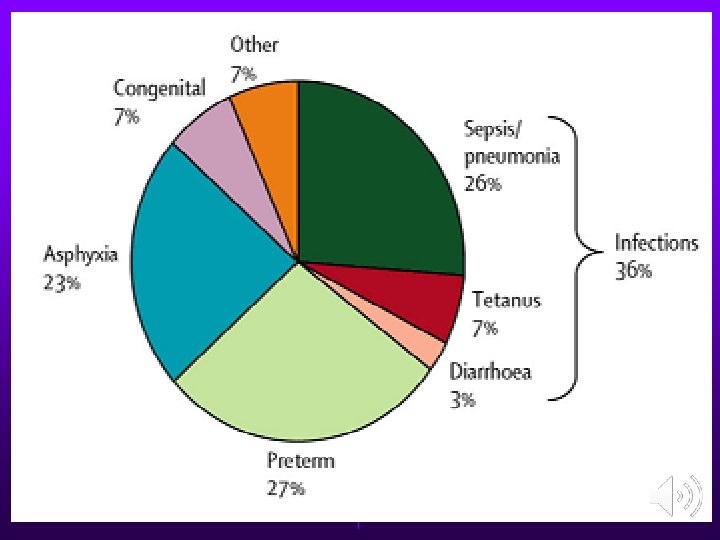
Burden of the problem Birth asphyxia. 23% of the causes of neonatal deaths. Long term neurological complications. Death. NNR (Neonatal resuscitation) : simple, inexpensive, cost effective method. • Problem: NNR often not initiated, incorrect use of methods. • • •
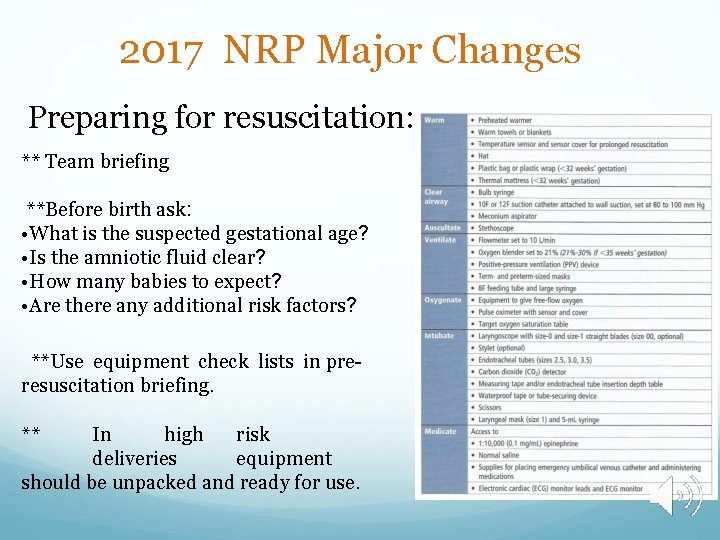
2017 NRP Major Changes Preparing for resuscitation: ** Team briefing **Before birth ask: • What is the suspected gestational age? • Is the amniotic fluid clear? • How many babies to expect? • Are there any additional risk factors? **Use equipment check lists in preresuscitation briefing. ** In high risk deliveries equipment should be unpacked and ready for use.
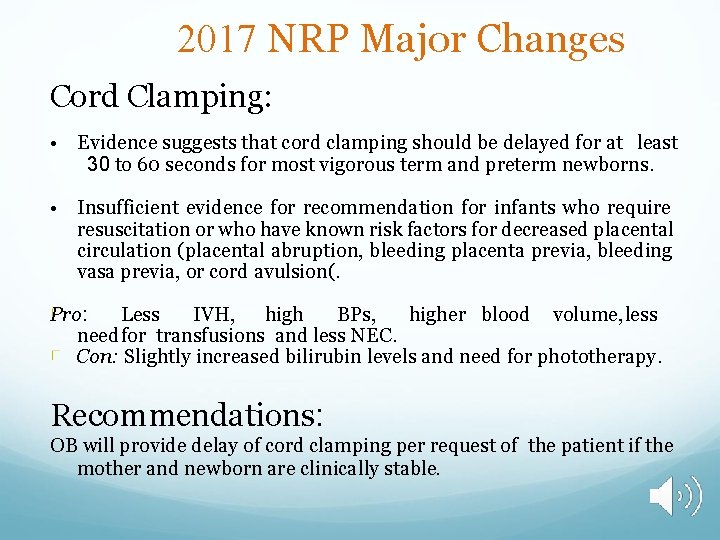
2017 NRP Major Changes Cord Clamping: • Evidence suggests that cord clamping should be delayed for at least 30 to 60 seconds for most vigorous term and preterm newborns. • Insufficient evidence for recommendation for infants who require resuscitation or who have known risk factors for decreased placental circulation (placental abruption, bleeding placenta previa, bleeding vasa previa, or cord avulsion(. Pro: Less IVH, high BPs, higher blood volume, less needfor transfusions and less NEC. Con: Slightly increased bilirubin levels and need for phototherapy. Recommendations: OB will provide delay of cord clamping per request of the patient if the mother and newborn are clinically stable.
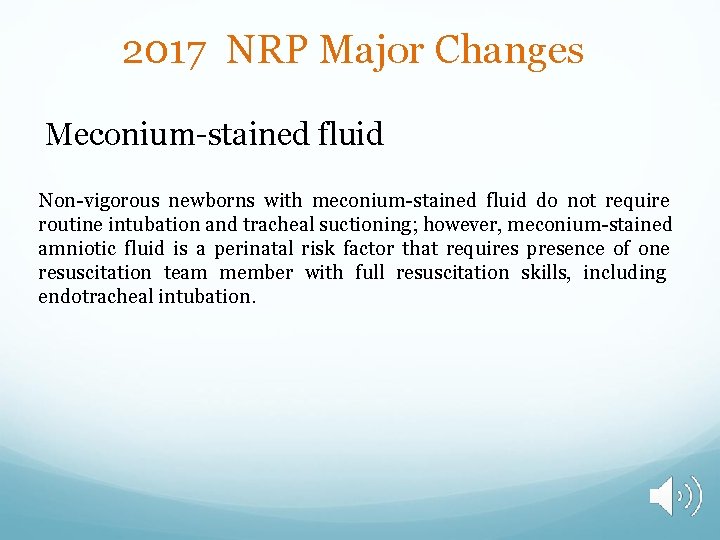
2017 NRP Major Changes Meconium-stained fluid Non-vigorous newborns with meconium-stained fluid do not require routine intubation and tracheal suctioning; however, meconium-stained amniotic fluid is a perinatal risk factor that requires presence of one resuscitation team member with full resuscitation skills, including endotracheal intubation.
The Golden minute • The “first minute after birth” • Anxiety for parents, health providers • Period of transition from intrauterine to extra uterine life • Major: No/minimal assistance • 10%: assistance to begin breathing at birth • 1%: extensive resuscitative measures • First Golden Minute Project: skill based training
Factors for successful NNR • • Anticipation: call a skilled personnel Adequate preparation Accurate evaluation, algorithm based Prompt initiation of support
Resuscitation: initial steps • • • Provide warmth Head position “ sniffing position” Clearing the airway Drying the baby Tactile stimulation for breathing
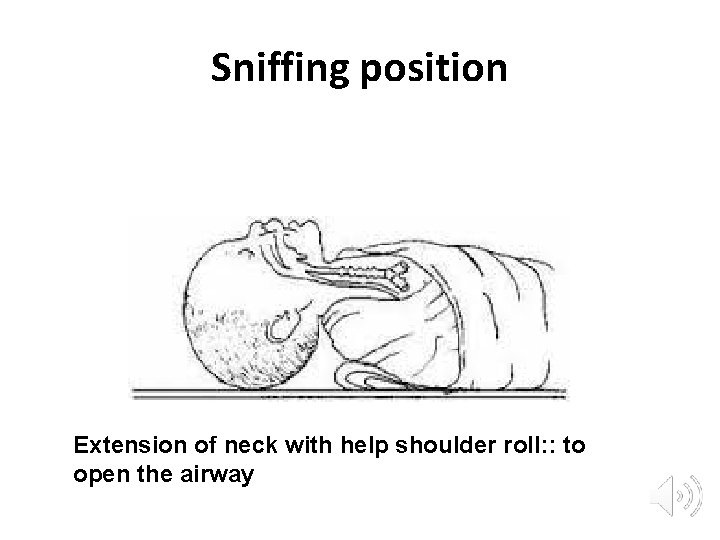
Sniffing position Extension of neck with help shoulder roll: : to open the airway
Newly born infant • Specifically the Infant at time of birth • (A)Do not require resuscitation • (B)Require resuscitation • Rapid assessment of 3 characters – Term gestation? – Crying or breathing? – Good muscle tone?
Newly born infant Term gestation? Crying or breathing? Good muscle tone? YES : Do not require resuscitation – Dry – Skin to skin contact – Covered with dry linen to maintain temperature – Ongoing observation: breathing, color, activity
Newly born infant Term gestation? Crying or breathing? Good muscle tone? NO : require resuscitation; One/more of the following actions in sequence – Initial steps in stabilization(warmth, clear airway, dry, stimulate) – Ventilation – Chest compressions – Administration of epinephrine& /or volume expansion

AAP Algorithm
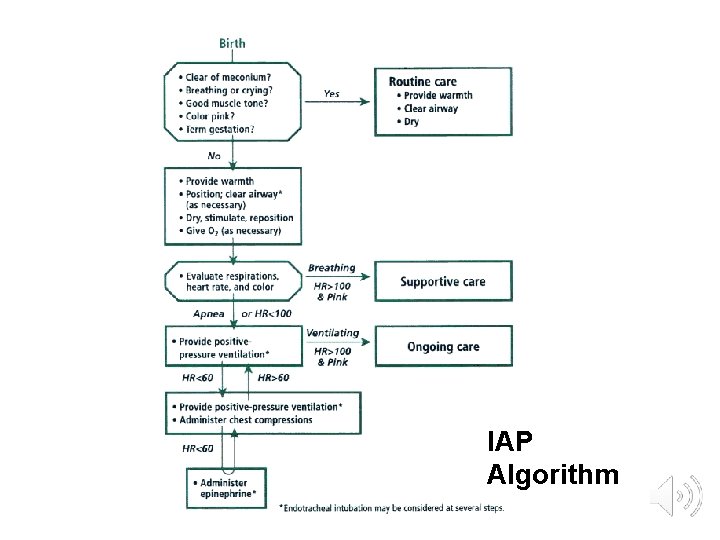
IAP Algorithm
The golden minute • < 30 seconds: complete initial steps • • Warmth Drying Clear airway if necessary Stimulate • 30 -60 seconds: assess 2 vital characteristics • Respiration (apnea/gasping/labored/unlabored) • Heart rate (<100/>100 bpm)
< 60 seconds of birth • If gasping/apnea If heart rate<100 beats per minute PPV( positive pressure ventilation) Spo 2 monitoring by pulse oximeter • Simultaneous evaluation of 3 vitals • Heart Rate, • Respiration, • oxygenation status
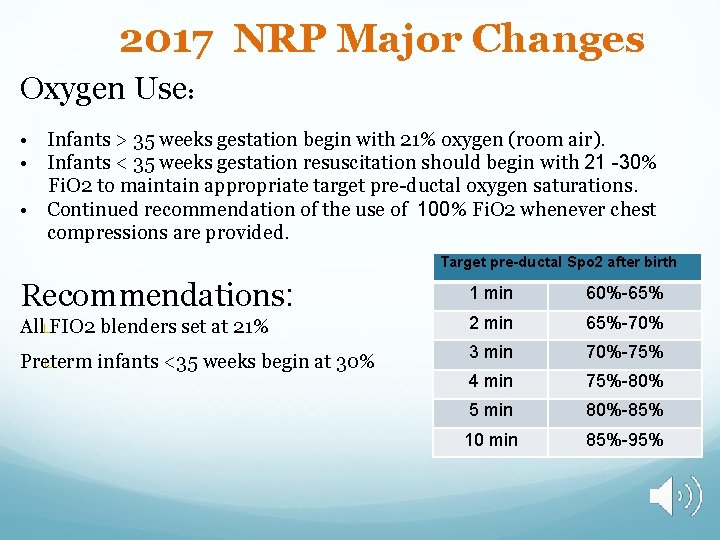
2017 NRP Major Changes Oxygen Use: • Infants > 35 weeks gestation begin with 21% oxygen (room air). • Infants < 35 weeks gestation resuscitation should begin with 21 -30% Fi. O 2 to maintain appropriate target pre-ductal oxygen saturations. • Continued recommendation of the use of 100% Fi. O 2 whenever chest compressions are provided. Target pre-ductal Spo 2 after birth Recommendations: 1 min 60%-65% All FIO 2 blenders set at 21% 2 min 65%-70% Preterm infants <35 weeks begin at 30% 3 min 70%-75% 4 min 75%-80% 5 min 80%-85% 10 min 85%-95%
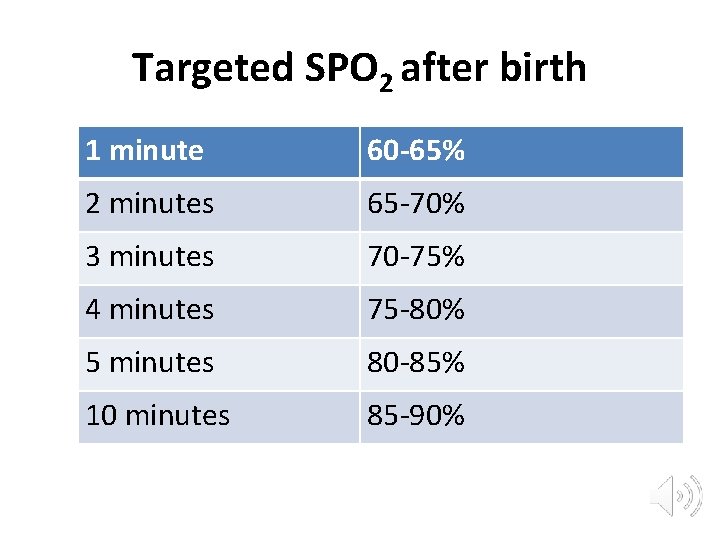
Targeted SPO 2 after birth 1 minute 60 -65% 2 minutes 65 -70% 3 minutes 70 -75% 4 minutes 75 -80% 5 minutes 80 -85% 10 minutes 85 -90%
Increase in heart rate is the most sensitive indicator of a successful response to each step practiced
PPV: Positive Pressure Ventilation Form of assisted ventilation Needed when there is no improvement in HR Also assess chest wall movements Should be delivered at rate of 40 -60 breaths /min, maintain HR>100 /min • Devices: BMV, ET (endotracheal tube), LMA(laryngeal mask airway) • •
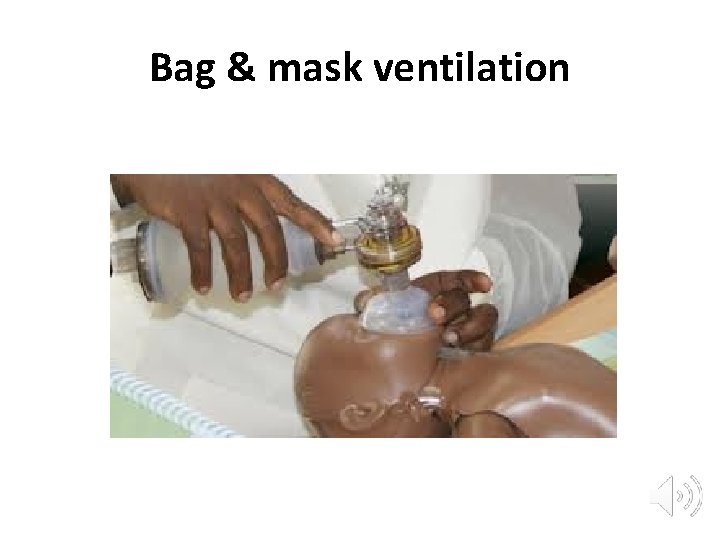
Bag & mask ventilation
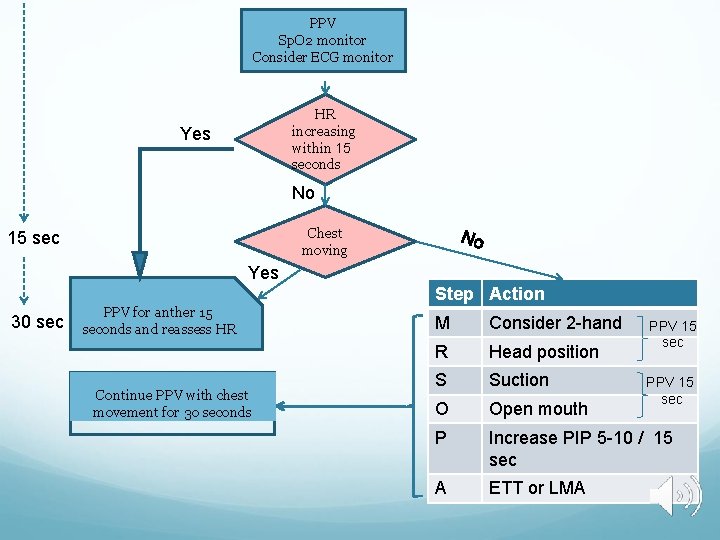
PPV Sp. O 2 monitor Consider ECG monitor HR increasing within 15 seconds Yes No Chest moving 15 sec Yes Step Action 30 sec PPV for anther 15 seconds and reassess HR Continue PPV with chest movement for 30 seconds M Consider 2 -hand R Head position S Suction O Open mouth P Increase PIP 5 -10 / 15 sec A ETT or LMA PPV 15 sec
Endotracheal tube • Initial endotracheal suctioning of non vigorous meconium stained new-born. • If BMV is ineffective/prolonged. • When chest compressions are performed.
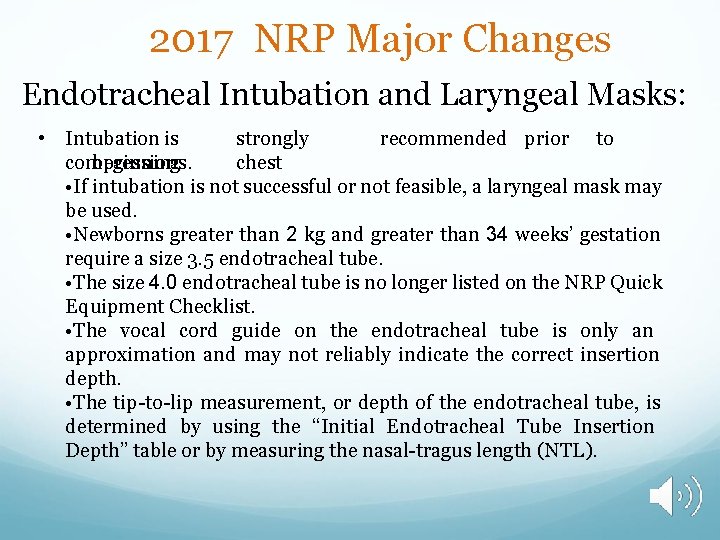
2017 NRP Major Changes Endotracheal Intubation and Laryngeal Masks: • Intubation is strongly recommended prior to compressions. beginning chest • If intubation is not successful or not feasible, a laryngeal mask may be used. • Newborns greater than 2 kg and greater than 34 weeks’ gestation require a size 3. 5 endotracheal tube. • The size 4. 0 endotracheal tube is no longer listed on the NRP Quick Equipment Checklist. • The vocal cord guide on the endotracheal tube is only an approximation and may not reliably indicate the correct insertion depth. • The tip-to-lip measurement, or depth of the endotracheal tube, is determined by using the “Initial Endotracheal Tube Insertion Depth” table or by measuring the nasal-tragus length (NTL).
Endotracheal tube
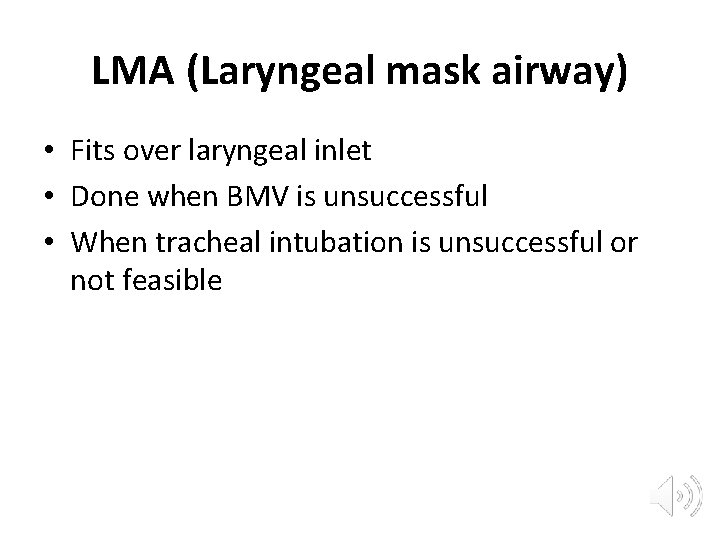
LMA (Laryngeal mask airway) • Fits over laryngeal inlet • Done when BMV is unsuccessful • When tracheal intubation is unsuccessful or not feasible
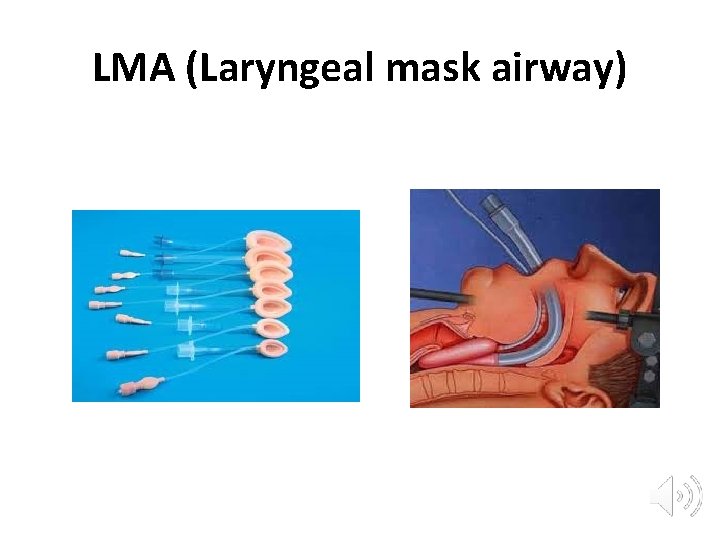
LMA (Laryngeal mask airway)
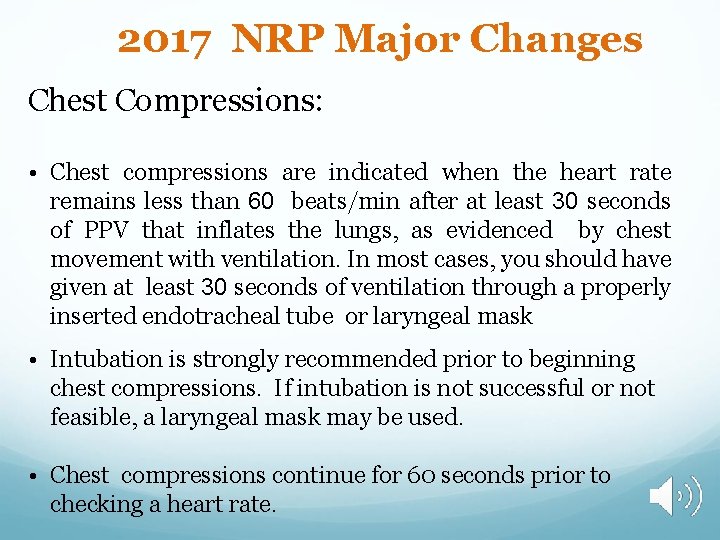
2017 NRP Major Changes Chest Compressions: • Chest compressions are indicated when the heart rate remains less than 60 beats/min after at least 30 seconds of PPV that inflates the lungs, as evidenced by chest movement with ventilation. In most cases, you should have given at least 30 seconds of ventilation through a properly inserted endotracheal tube or laryngeal mask • Intubation is strongly recommended prior to beginning chest compressions. If intubation is not successful or not feasible, a laryngeal mask may be used. • Chest compressions continue for 60 seconds prior to checking a heart rate.
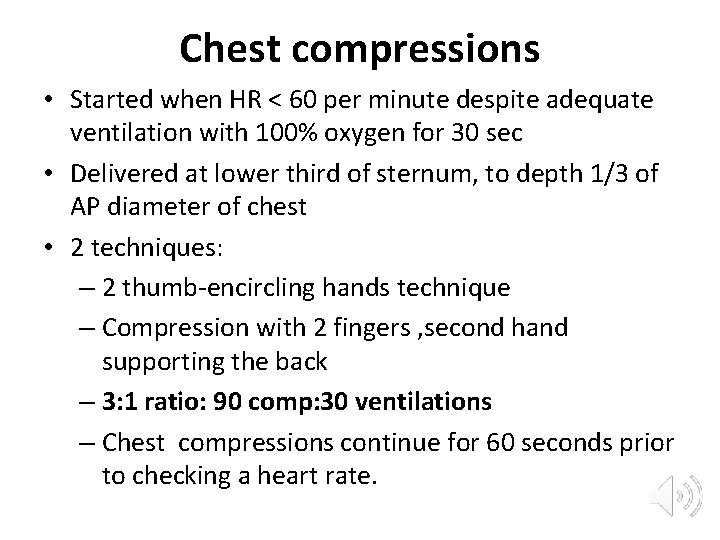
Chest compressions • Started when HR < 60 per minute despite adequate ventilation with 100% oxygen for 30 sec • Delivered at lower third of sternum, to depth 1/3 of AP diameter of chest • 2 techniques: – 2 thumb-encircling hands technique – Compression with 2 fingers , second hand supporting the back – 3: 1 ratio: 90 comp: 30 ventilations – Chest compressions continue for 60 seconds prior to checking a heart rate.
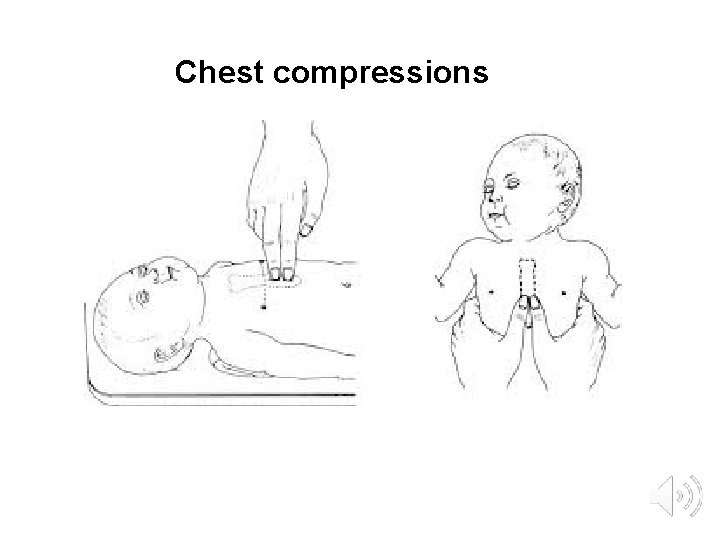
Chest compressions
Medications • Rarely indicated • Most important step to treat bradycardia is establishing adequate ventilation • HR remains < 60 bpm, despite adequate ventilation (ET) with 100% Oxygen & chest compressions • Epinephrine or volume expansion or both
Epinephrine • Route of administration: intravenous(IV), ideal • Recommended dose: 0. 01 -0. 03 mg/kg per dose • Desired concentration: 1: 10, 000 0. 1 mg/ml
Volume expansion • • Suspected or known blood loss Isotonic crystalloid solution Blood Dose calculation: 10 ml/kg
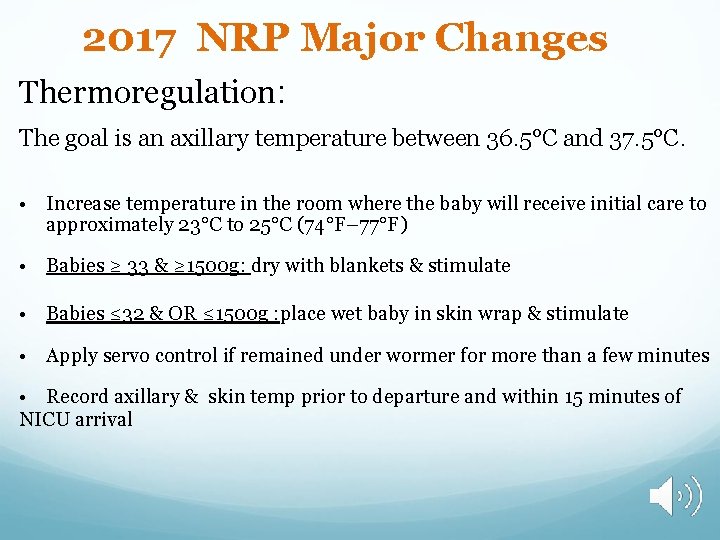
2017 NRP Major Changes Thermoregulation: The goal is an axillary temperature between 36. 5°C and 37. 5°C. • Increase temperature in the room where the baby will receive initial care to approximately 23°C to 25°C (74°F– 77°F) • Babies ≥ 33 & ≥ 1500 g: dry with blankets & stimulate • Babies ≤ 32 & OR ≤ 1500 g : place wet baby in skin wrap & stimulate • Apply servo control if remained under wormer for more than a few minutes • Record axillary & skin temp prior to departure and within 15 minutes of NICU arrival
Post resuscitation care • • Needed for those who required PPV At risk of deterioration Need monitoring , evaluation NICU may be necessary
NNR : not indicated • • Conditions with certainly early death Extreme prematurity(GA < 24 weeks) Birth weight <500 g Futile conditions such as Anencephaly and Chromosomal abnormalities: Trisomy 13 and Trisomy 18
NNR: nearly always indicated • • High rate of survival Acceptable morbidity GA ≥ 24 weeks Those with most congenital malformations
NNR? • Conditions associated with uncertain prognosis • Survival borderline • Parental desires concerning initiation of resuscitation should be supported
Discontinuing resuscitative efforts • Newly born baby with no detectable heart rate, consider stopping NNR if the heart rate remains undetectable for 10 minutes
MCQ 1 For successful neonatal resuscitation following is/are needed except: 1. Anticipation 2. Adequate preparation 3. Skilled personnel 4. Delayed initiation of support
MCQ 2 • All the following are true in relation to initial steps of neonatal resuscitation except 1. Provide warmth 2. Tactile stimulation 3. Clear airway and intubation 4. Drying the baby
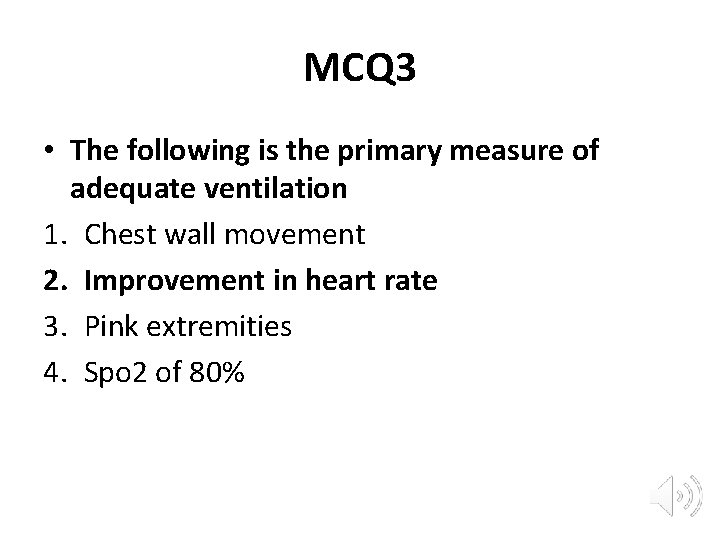
MCQ 3 • The following is the primary measure of adequate ventilation 1. Chest wall movement 2. Improvement in heart rate 3. Pink extremities 4. Spo 2 of 80%
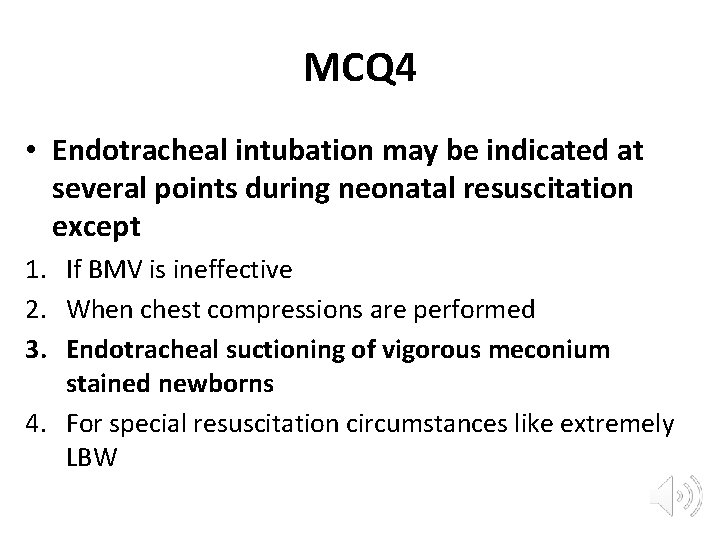
MCQ 4 • Endotracheal intubation may be indicated at several points during neonatal resuscitation except 1. If BMV is ineffective 2. When chest compressions are performed 3. Endotracheal suctioning of vigorous meconium stained newborns 4. For special resuscitation circumstances like extremely LBW
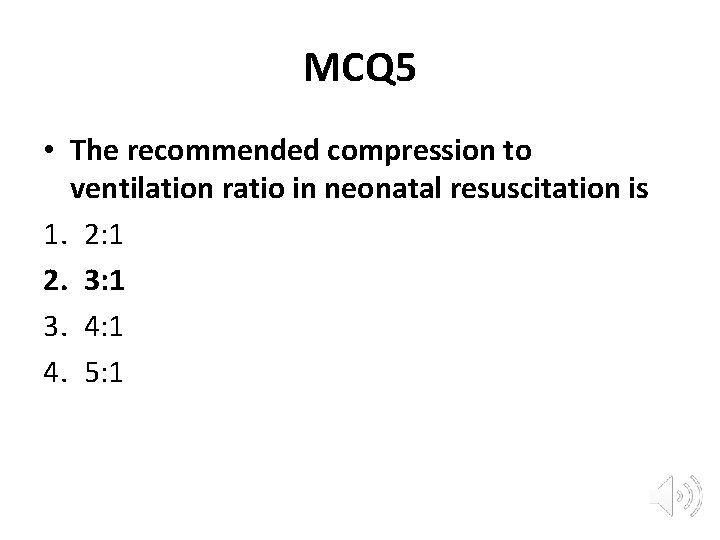
MCQ 5 • The recommended compression to ventilation ratio in neonatal resuscitation is 1. 2: 1 2. 3: 1 3. 4: 1 4. 5: 1
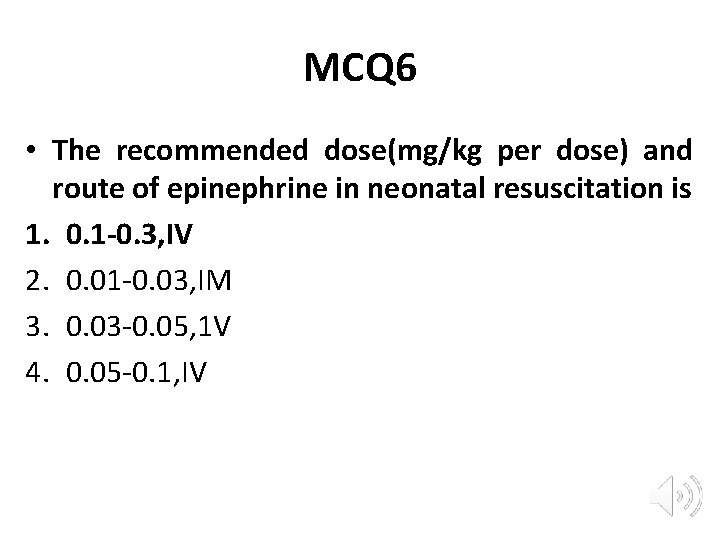
MCQ 6 • The recommended dose(mg/kg per dose) and route of epinephrine in neonatal resuscitation is 1. 0. 1 -0. 3, IV 2. 0. 01 -0. 03, IM 3. 0. 03 -0. 05, 1 V 4. 0. 05 -0. 1, IV
MCQ 7 • Recommended method/clinical indicator of confirming ET placement is 1. Condensation in ET 2. Chest movement 3. Equal breath sounds on auscultation 4. Exhaled C 02 Detection
2017 NRP Major Changes http: //www 2. aap. org/nrp/ https: //eccguidelines. heart. org/index. php/circulatio n/cpr-ecc-guidelines-2/part-13 -neonatalresuscitation/

- Slides: 52