New York State Health Home State Plan Amendment


- Slides: 33
New York State Health Home State Plan Amendment and Provider Application July 21, 2011 1
Draft Health Home State Plan Amendments NYSDOH submitted two draft SPAs to CMS on June 30, 2011 One SPA targeted the Managed Long Term Care population; the other targeted the chronic medical/behavioral health population The focus of today will be on the SPA targeting the chronic medical/behavioral health population Available on the NYSDOH Health Home Website at: http: //nyhealth. gov/health_care/medicaid/program/medicaid_health_homes/ind ex. htm 2
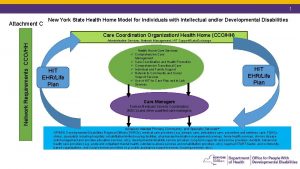
Health Home Application States required to describe all designated providers, composition of teams, and methods used to assure providers adhere to standards. State support health home provider services (i. e. coordination and access to services, use of IT to link services) must be defined. Requires a comprehensive description of the rate-setting policies that assure health home payment method is consistent with the goals of efficiency, economy, and quality of care. 3
Health Home Application States set initial quality measures until CMS releases a core set of quality measures. CMS requires states to collect and report information required for state and CMS evaluation including tracking of avoidable hospital admissions, cost savings, and monitoring of use of HIT. Additional guidance forthcoming. 4
Health Home Approval CMS expects to work closely with states prior to submission. No time limit for SPA submission to receive 90% FMAP. 8 Quarters are rolling. States may need to amend SPA to come into compliance with final regulatory requirements. CMS encourages states to consider utilizing technologies to provide health home services and improve care coordination. Further guidance will be forthcoming in the future. 5
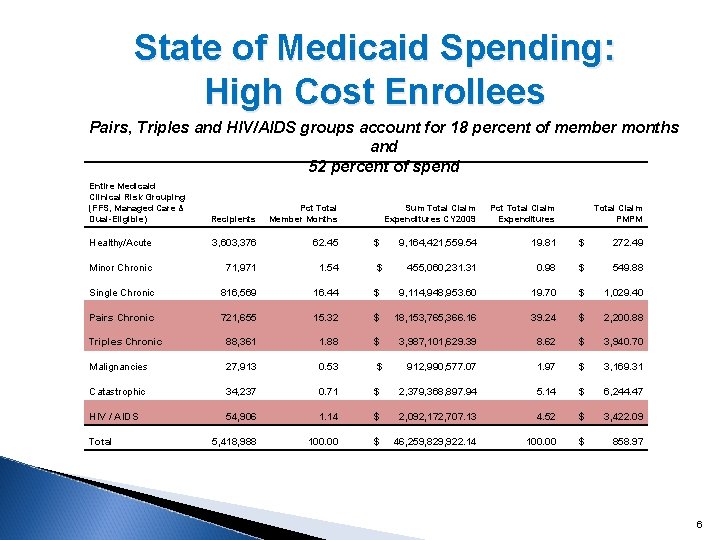
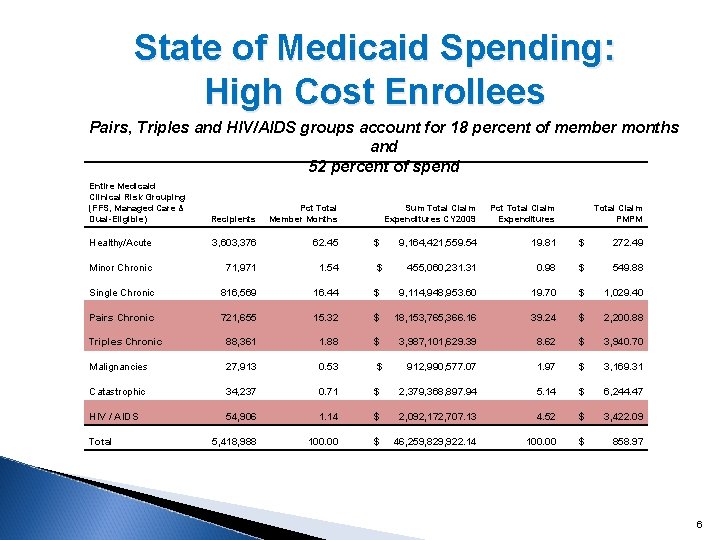
State of Medicaid Spending: High Cost Enrollees Pairs, Triples and HIV/AIDS groups account for 18 percent of member months and 52 percent of spend Entire Medicaid Clinical Risk Grouping (FFS, Managed Care & Dual-Eligible) Recipients Pct Total Member Months Sum Total Claim Expenditures CY 2009 Pct Total Claim Expenditures Total Claim PMPM Healthy/Acute 3, 603, 376 62. 45 $ 9, 164, 421, 559. 54 19. 81 $ 272. 49 Minor Chronic 71, 971 1. 54 $ 455, 060, 231. 31 0. 98 $ 549. 88 Single Chronic 816, 569 16. 44 $ 9, 114, 948, 953. 60 19. 70 $ 1, 029. 40 Pairs Chronic 721, 655 15. 32 $ 18, 153, 765, 366. 16 39. 24 $ 2, 200. 88 88, 361 1. 88 $ 3, 987, 101, 629. 39 8. 62 $ 3, 940. 70 Malignancies 27, 913 0. 53 $ 912, 990, 577. 07 1. 97 $ 3, 169. 31 Catastrophic 34, 237 0. 71 $ 2, 379, 368, 897. 94 5. 14 $ 6, 244. 47 54, 906 1. 14 $ 2, 092, 172, 707. 13 4. 52 $ 3, 422. 09 5, 418, 988 100. 00 $ 46, 259, 829, 922. 14 100. 00 $ 858. 97 Triples Chronic HIV / AIDS Total 6
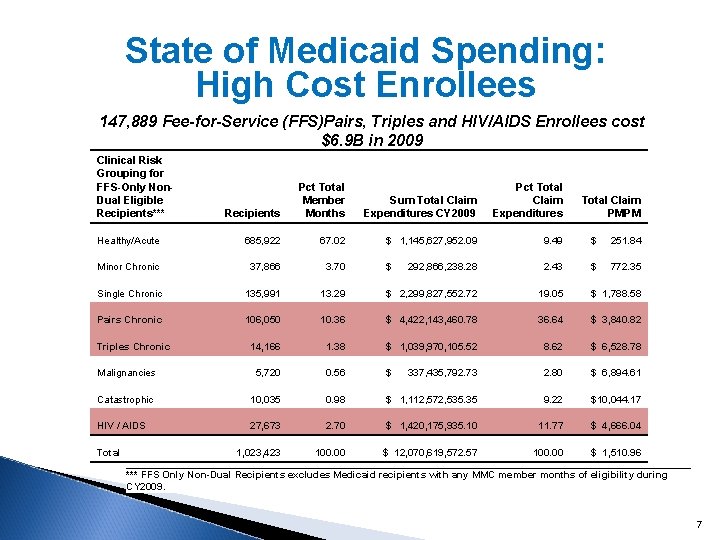
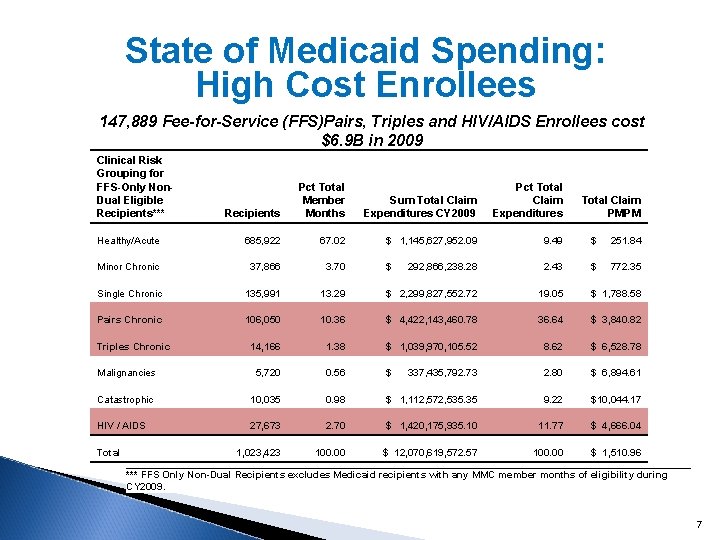
State of Medicaid Spending: High Cost Enrollees 147, 889 Fee-for-Service (FFS)Pairs, Triples and HIV/AIDS Enrollees cost $6. 9 B in 2009 Clinical Risk Grouping for FFS-Only Non. Dual Eligible Recipients*** Recipients Pct Total Member Months Sum Total Claim Expenditures CY 2009 Pct Total Claim Expenditures Total Claim PMPM Healthy/Acute 685, 922 67. 02 $ 1, 145, 627, 952. 09 9. 49 $ 251. 84 Minor Chronic 37, 866 3. 70 $ 292, 866, 238. 28 2. 43 $ 772. 35 Single Chronic 135, 991 13. 29 $ 2, 299, 827, 552. 72 19. 05 $ 1, 788. 58 Pairs Chronic 106, 050 10. 36 $ 4, 422, 143, 460. 78 36. 64 $ 3, 840. 82 14, 166 1. 38 $ 1, 039, 970, 105. 52 8. 62 $ 6, 528. 78 Malignancies 5, 720 0. 56 $ 337, 435, 792. 73 2. 80 $ 6, 894. 61 Catastrophic 10, 035 0. 98 $ 1, 112, 572, 535. 35 9. 22 $10, 044. 17 27, 673 2. 70 $ 1, 420, 175, 935. 10 11. 77 $ 4, 666. 04 1, 023, 423 100. 00 $ 12, 070, 619, 572. 57 100. 00 $ 1, 510. 96 Triples Chronic HIV / AIDS Total *** FFS Only Non-Dual Recipients excludes Medicaid recipients with any MMC member months of eligibility during CY 2009. 7
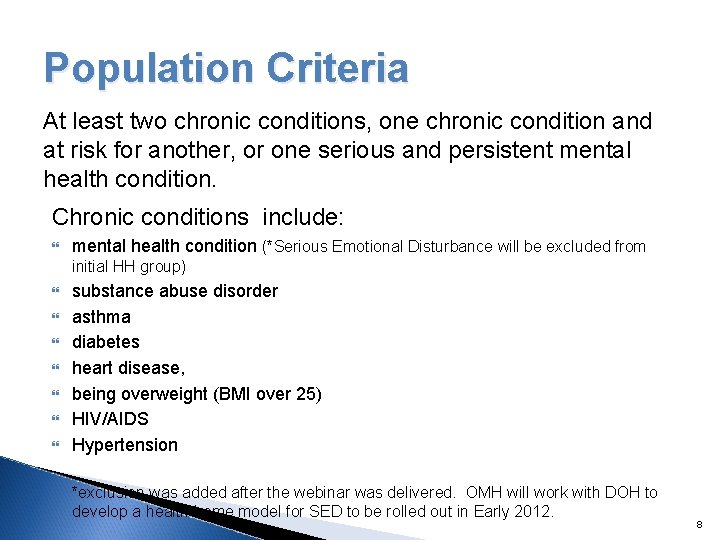
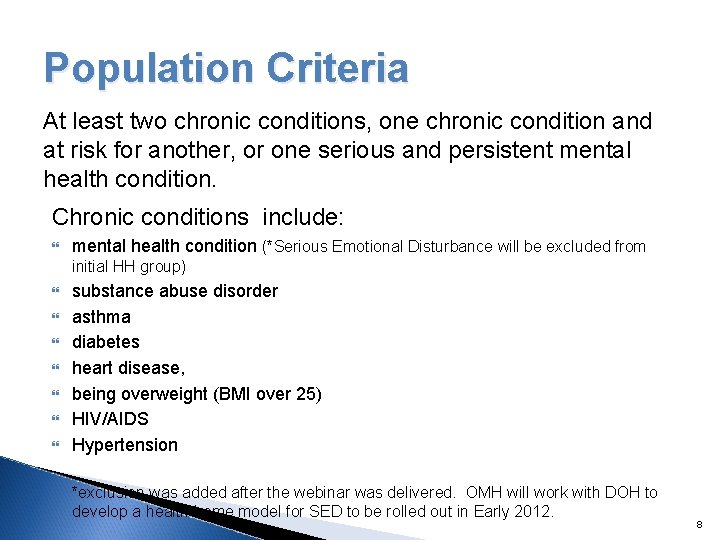
Population Criteria At least two chronic conditions, one chronic condition and at risk for another, or one serious and persistent mental health condition. Chronic conditions include: mental health condition (*Serious Emotional Disturbance will be excluded from initial HH group) substance abuse disorder asthma diabetes heart disease, being overweight (BMI over 25) HIV/AIDS Hypertension *exclusion was added after the webinar was delivered. OMH will work with DOH to develop a health home model for SED to be rolled out in Early 2012. 8
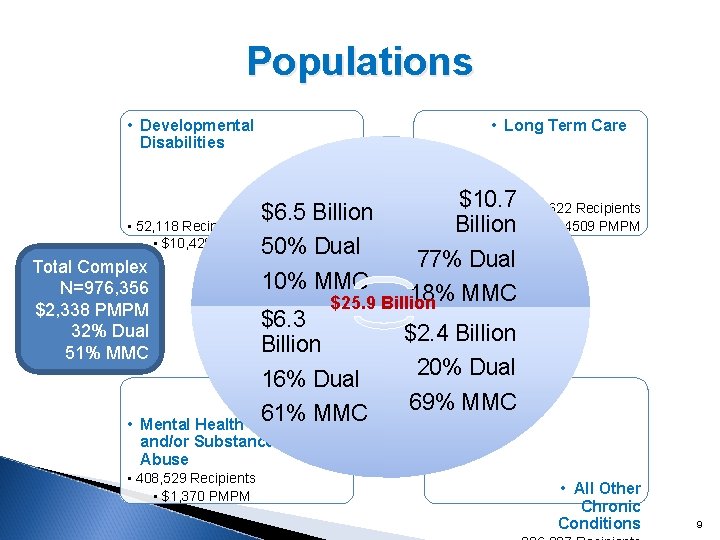
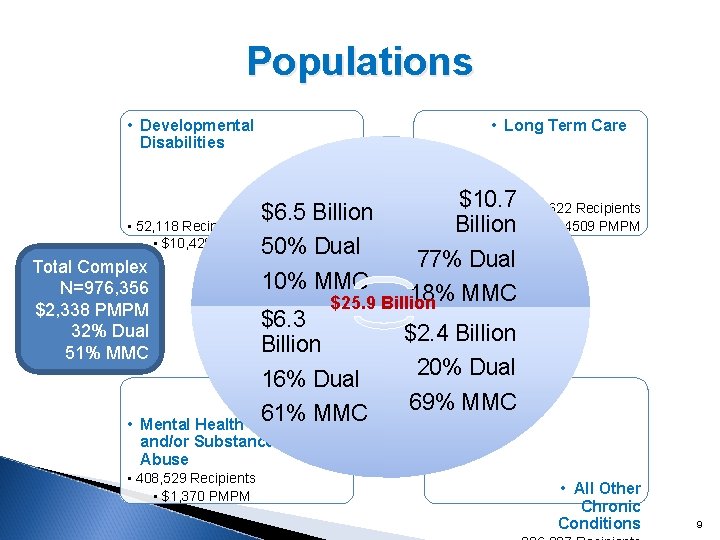
Populations • Developmental Disabilities • Long Term Care $10. 7 • 209, 622 Recipients Billion • $4509 PMPM 77% Dual 10% MMC 18% MMC $25. 9 Billion $6. 3 $2. 4 Billion 20% Dual 16% Dual 69% MMC 61% MMC $6. 5 Billion • 52, 118 Recipients • $10, 429 PMPM 50% Dual Total Complex N=976, 356 $2, 338 PMPM 32% Dual 51% MMC • Mental Health and/or Substance Abuse • 408, 529 Recipients • $1, 370 PMPM • All Other Chronic Conditions 9
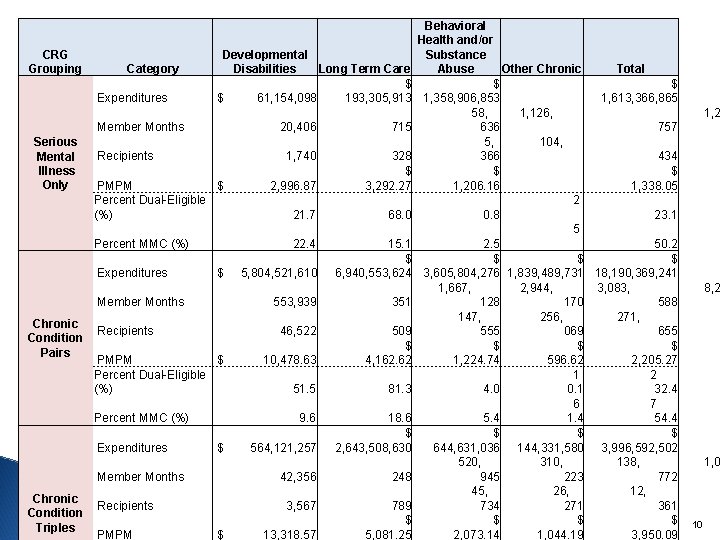
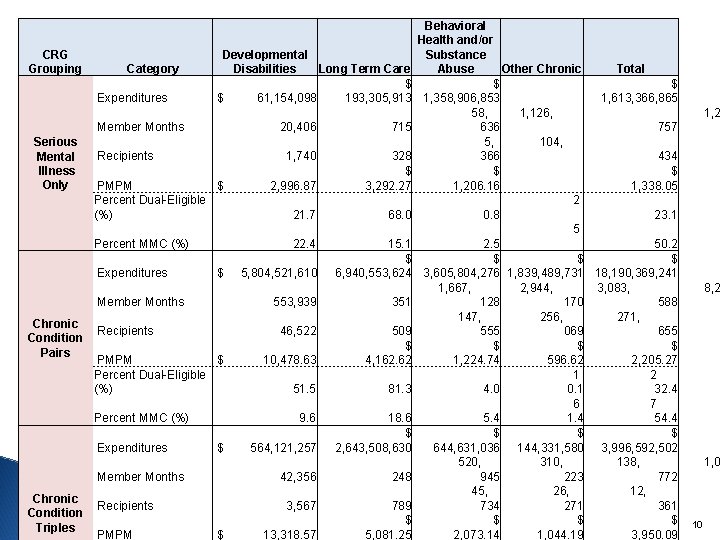
Behavioral Health and/or CRG Developmental Substance Grouping Category Disabilities Long Term Care Abuse Other Chronic Total $ $ $ Expenditures $ 61, 154, 098 193, 305, 913 1, 358, 906, 853 1, 613, 366, 865 58, 1, 126, 1, 2 Member Months 20, 406 715 636 757 5, 104, Serious Recipients 1, 740 328 366 434 Mental Illness $ Only PMPM $ 2, 996. 87 3, 292. 27 1, 206. 16 1, 338. 05 Percent Dual-Eligible 2 (%) 21. 7 68. 0 0. 8 23. 1 5 Percent MMC (%) 22. 4 15. 1 2. 5 50. 2 $ $ $ Expenditures $ 5, 804, 521, 610 6, 940, 553, 624 3, 605, 804, 276 1, 839, 489, 731 18, 190, 369, 241 1, 667, 2, 944, 3, 083, 8, 2 Member Months 553, 939 351 128 170 588 147, 256, 271, Chronic Recipients 46, 522 509 555 069 655 Condition $ $ Pairs PMPM $ 10, 478. 63 4, 162. 62 1, 224. 74 596. 62 2, 205. 27 Percent Dual-Eligible 1 2 (%) 51. 5 81. 3 4. 0 0. 1 32. 4 6 7 Percent MMC (%) 9. 6 18. 6 5. 4 1. 4 54. 4 $ $ $ Expenditures $ 564, 121, 257 2, 643, 508, 630 644, 631, 036 144, 331, 580 3, 996, 592, 502 520, 310, 138, 1, 0 Member Months 42, 356 248 945 223 772 45, 26, 12, Chronic Recipients 3, 567 789 734 271 361 Condition $ $ 10 Triples PMPM $ 13, 318. 57 5, 081. 25 2, 073. 14 1, 044. 19 3, 950. 09
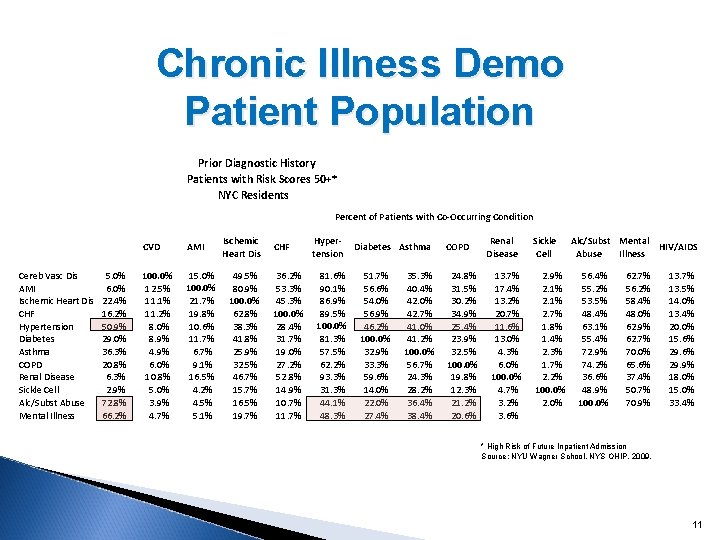
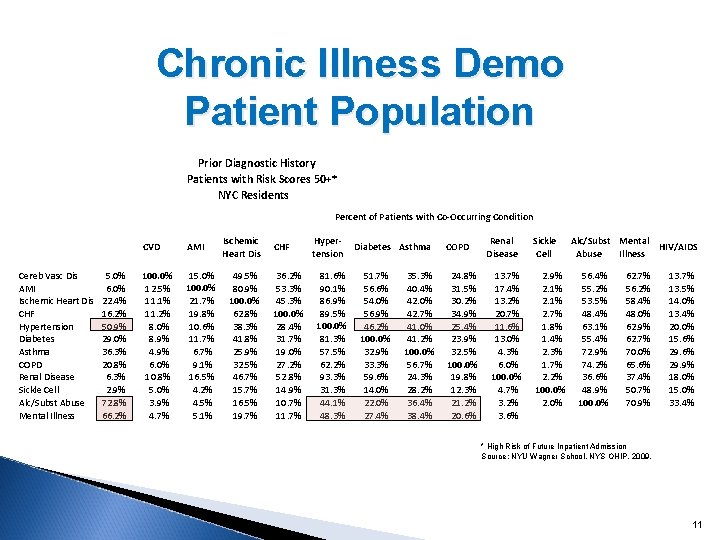
Chronic Illness Demo Patient Population Prior Diagnostic History Patients with Risk Scores 50+* NYC Residents Percent of Patients with Co-Occurring Condition Cereb Vasc Dis AMI Ischemic Heart Dis CHF Hypertension Diabetes Asthma COPD Renal Disease Sickle Cell Alc/Subst Abuse Mental Illness 5. 0% 6. 0% 22. 4% 16. 2% 50. 9% 29. 0% 36. 3% 20. 8% 6. 3% 2. 9% 72. 8% 66. 2% CVD AMI 100. 0% 12. 5% 11. 1% 11. 2% 8. 0% 8. 9% 4. 9% 6. 0% 10. 8% 5. 0% 3. 9% 4. 7% 15. 0% 100. 0% 21. 7% 19. 8% 10. 6% 11. 7% 6. 7% 9. 1% 16. 5% 4. 2% 4. 5% 5. 1% Ischemic Heart Dis 49. 5% 80. 9% 100. 0% 62. 8% 38. 3% 41. 8% 25. 9% 32. 5% 46. 7% 15. 7% 16. 5% 19. 7% CHF 36. 2% 53. 3% 45. 3% 100. 0% 28. 4% 31. 7% 19. 0% 27. 2% 52. 8% 14. 9% 10. 7% 11. 7% Hypertension 81. 6% 90. 1% 86. 9% 89. 5% 100. 0% 81. 3% 57. 5% 62. 2% 93. 3% 31. 3% 44. 1% 48. 3% Diabetes Asthma 51. 7% 56. 6% 54. 0% 56. 9% 46. 2% 100. 0% 32. 9% 33. 3% 59. 6% 14. 0% 22. 0% 27. 4% 35. 3% 40. 4% 42. 0% 42. 7% 41. 0% 41. 2% 100. 0% 56. 7% 24. 3% 28. 2% 36. 4% 38. 4% COPD 24. 8% 31. 5% 30. 2% 34. 9% 25. 4% 23. 9% 32. 5% 100. 0% 19. 8% 12. 3% 21. 2% 20. 6% Renal Disease 13. 7% 17. 4% 13. 2% 20. 7% 11. 6% 13. 0% 4. 3% 6. 0% 100. 0% 4. 7% 3. 2% 3. 6% Sickle Cell 2. 9% 2. 1% 2. 7% 1. 8% 1. 4% 2. 3% 1. 7% 2. 2% 100. 0% 2. 0% Alc/Subst Mental HIV/AIDS Abuse Illness 56. 4% 55. 2% 53. 5% 48. 4% 63. 1% 55. 4% 72. 9% 74. 2% 36. 6% 48. 9% 100. 0% 62. 7% 56. 2% 58. 4% 48. 0% 62. 9% 62. 7% 70. 0% 65. 6% 37. 4% 50. 7% 70. 9% 13. 7% 13. 5% 14. 0% 13. 4% 20. 0% 15. 6% 29. 9% 18. 0% 15. 0% 33. 4% * High Risk of Future Inpatient Admission Source: NYU Wagner School, NYS OHIP, 2009. 11
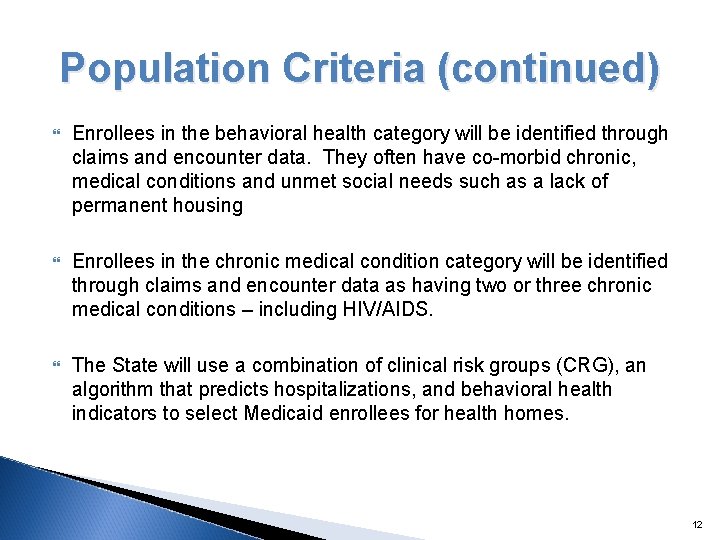
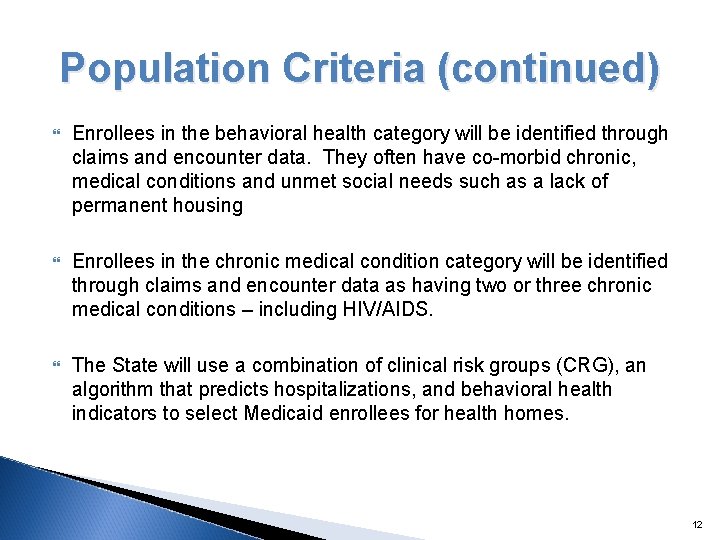
Population Criteria (continued) Enrollees in the behavioral health category will be identified through claims and encounter data. They often have co-morbid chronic, medical conditions and unmet social needs such as a lack of permanent housing Enrollees in the chronic medical condition category will be identified through claims and encounter data as having two or three chronic medical conditions – including HIV/AIDS. The State will use a combination of clinical risk groups (CRG), an algorithm that predicts hospitalizations, and behavioral health indicators to select Medicaid enrollees for health homes. 12
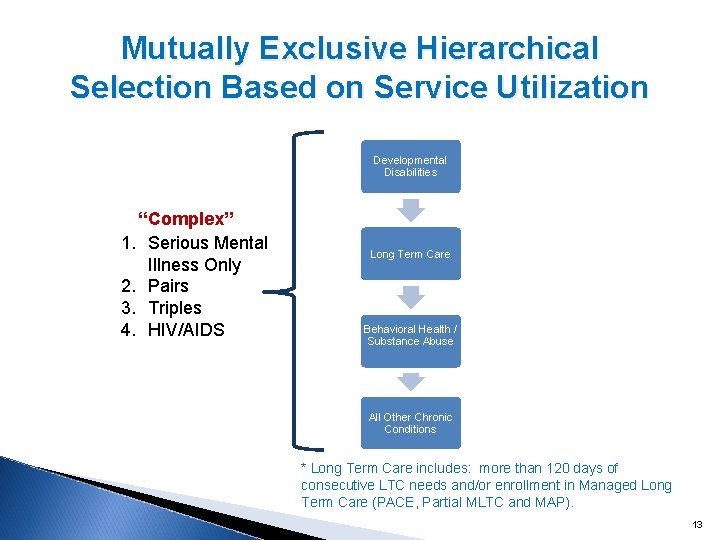
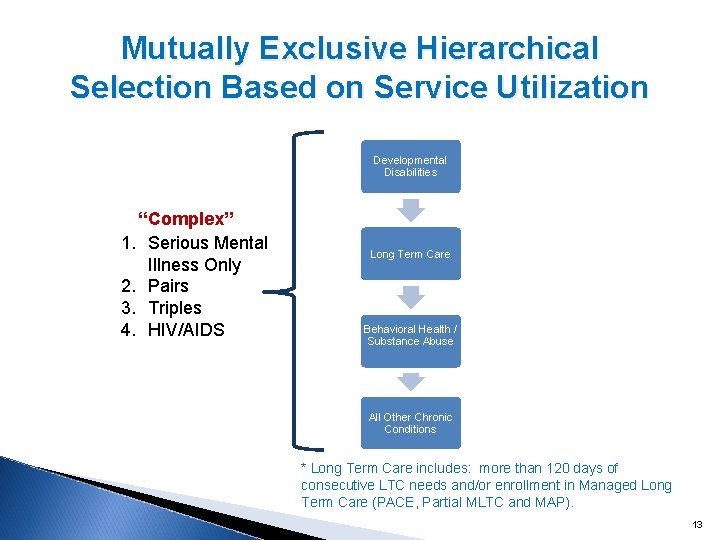
Mutually Exclusive Hierarchical Selection Based on Service Utilization Developmental Disabilities “Complex” 1. Serious Mental Illness Only 2. Pairs 3. Triples 4. HIV/AIDS Long Term Care Behavioral Health / Substance Abuse All Other Chronic Conditions * Long Term Care includes: more than 120 days of consecutive LTC needs and/or enrollment in Managed Long Term Care (PACE, Partial MLTC and MAP). 13
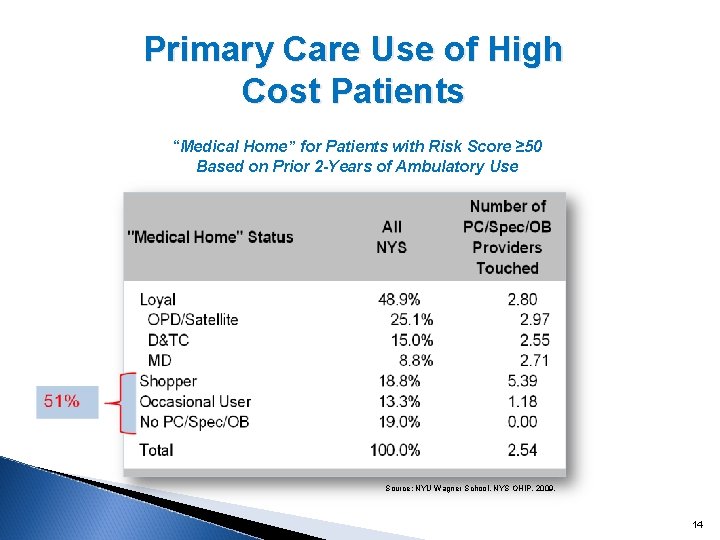
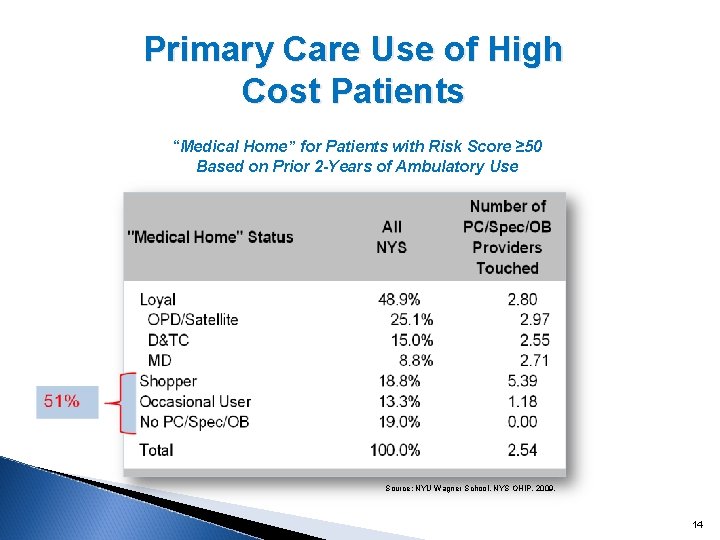
Primary Care Use of High Cost Patients “Medical Home” for Patients with Risk Score ≥ 50 Based on Prior 2 -Years of Ambulatory Use Source: NYU Wagner School, NYS OHIP, 2009. 14
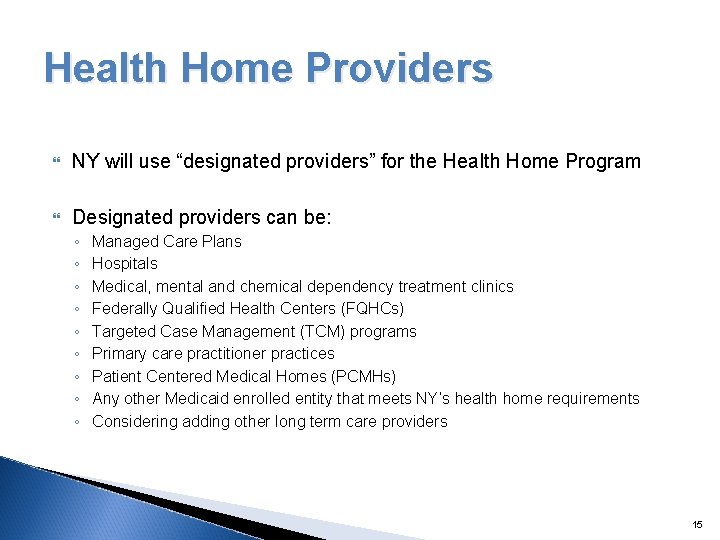
Health Home Providers NY will use “designated providers” for the Health Home Program Designated providers can be: ◦ ◦ ◦ ◦ ◦ Managed Care Plans Hospitals Medical, mental and chemical dependency treatment clinics Federally Qualified Health Centers (FQHCs) Targeted Case Management (TCM) programs Primary care practitioner practices Patient Centered Medical Homes (PCMHs) Any other Medicaid enrolled entity that meets NY’s health home requirements Considering adding other long term care providers 15
Health Home Providers (continued) NY is seeking applicants that : ◦ have strong medical, behavioral, and social service community providers connections ◦ use multi-disciplinary teams of medical, behavioral , TCM, and social services providers that can assure appropriate and timely access to services. Each patient enrollee will be assigned a single care manager who is responsible for managing and coordinating their care. There will be only one care plan for each patient enrollee. All members of the health home team will report back to the care manager on patient status, treatment options, actions taken, and outcomes. Health homes will be responsible for reducing or eliminating costs associated with avoidable inpatient and emergency room visits and improving patient outcomes. 16
Provider Qualification Standards General Qualifications Must be enrolled (or be eligible for enrollment) in the NYS Medicaid program and agree to comply with all Medicaid program requirements. Can either directly provide, or subcontract for the provision of, health home services. Responsible for all health home program requirements, including services performed by the subcontractor. Care coordination and integration of heath care services will be provided to all health home enrollees by an interdisciplinary team of providers, where each individual’s care is under the direction of a dedicated care manager who is accountable for assuring access to medical and behavioral health care services and community social supports as defined in the enrollee care management plan. Must meet standards for delivery of six core health home services as described in following slides. Must provide written documentation that clearly demonstrates how the requirements are being met. 17

Provider Qualification Standards Health home providers will be required to provide the following health home services in accordance with federal and State requirements: ◦ Comprehensive care management An individualized patient centered care plan based on a comprehensive health risk assessment – must meet physical, mental health, chemical dependency and social service needs. ◦ Care coordination and health promotion One care manager will ensure that the care plan is followed by coordinating and arranging for the provision of services, supporting adherence to treatment recommendations, and monitoring and evaluating the enrollee’s needs. The health home provider will promote evidence based wellness and prevention by linking patient enrollees with resources for smoking cessation, diabetes, asthma, hypertension, selfhelp recovery resources, and other services based on need and patient preference. ◦ Comprehensive transitional care Prevention of avoidable readmissions to inpatient facilities and oversight of proper and timely follow-up care. ◦ Patient and family support Individualized care plan must be shared with patient enrollee and family members or other caregivers. Patient and family preferences are considered. 18
Provider Qualifications (continued) Health home providers will be required to provide the following health home services in accordance with federal and State requirements: ◦ Referral to community and social support services Provider will identify and coordinate community and social supports ◦ Use of health information technology (HIT) when feasible Health home providers will be encouraged to utilize RHIOs or a qualified entity to access patient data and to develop partnerships that maximize the use of HIT across providers. Health home provider applicants must submit a plan with their application for achieving compliance with the final health home HIT requirements within 18 months of program implementation 19
Quality Reporting Measures and Evaluation NY will be using quality measures that fall into the following categories: ◦ ◦ Measures collected from claims and encounters Measures currently collected by managed care plans Measures per NQF and/or meaningful use measures New measures that meet federal reporting requirements ◦ Referral to community and social support services Provider will identify and coordinate community and social supports ◦ Use of health information technology (HIT) when feasible Health home providers will be encouraged to utilize RHIOs or a qualified entity to access patient data and to develop partnerships that maximize the use of HIT across providers. Health home provider applicants must submit a plan with their application for achieving compliance with the final health home HIT requirements within 18 months of program implementation 20
Payment Methodology Health home providers will be paid a per member per month (PMPM) care management fee that is adjusted based on region, enrollment volume, case mix, and in the near future, patient functional status. A case finding PMPM payment, at a reduced amount, is available for the first few months to reimburse for outreach and engagement. Once a patient is assigned a care manager and enrolled in the health home program, the active care management fee may be billed. Managed care plans will pay contracted health home providers State set rates for health home services. When managed care plans provide a portion of the health home service and “downstream” providers do a separate portion, the plan will split the State set PMPM proportionally with the “downstream” provider based on relative effort. 21
Payment Methodology (continued) Quality Incentive-The active care management fee will be paid in two installments with the final installment paid once the health home provider meets state quality metrics. If the state achieves service savings, after a year, it is expected that health home providers will be able to participate in a shared savings pool. 22
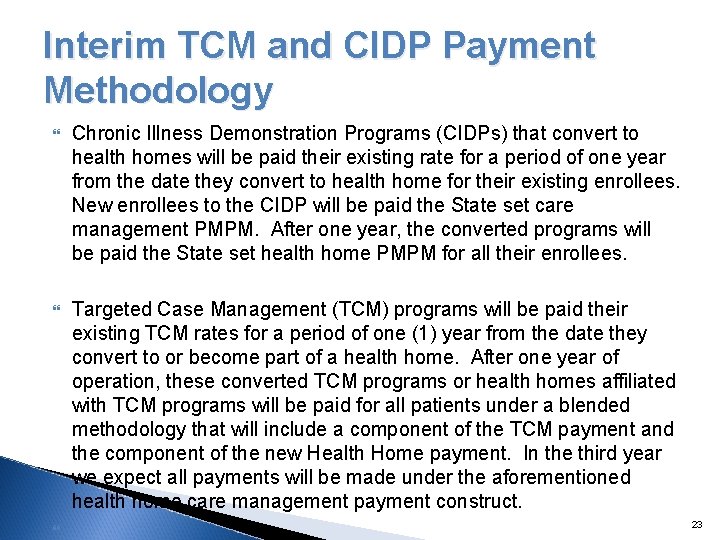
Interim TCM and CIDP Payment Methodology Chronic Illness Demonstration Programs (CIDPs) that convert to health homes will be paid their existing rate for a period of one year from the date they convert to health home for their existing enrollees. New enrollees to the CIDP will be paid the State set care management PMPM. After one year, the converted programs will be paid the State set health home PMPM for all their enrollees. Targeted Case Management (TCM) programs will be paid their existing TCM rates for a period of one (1) year from the date they convert to or become part of a health home. After one year of operation, these converted TCM programs or health homes affiliated with TCM programs will be paid for all patients under a blended methodology that will include a component of the TCM payment and the component of the new Health Home payment. In the third year we expect all payments will be made under the aforementioned health home care management payment construct. 23
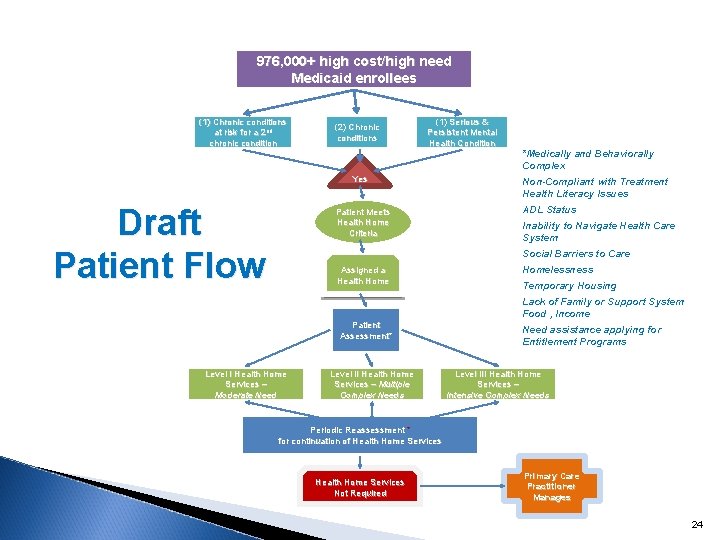
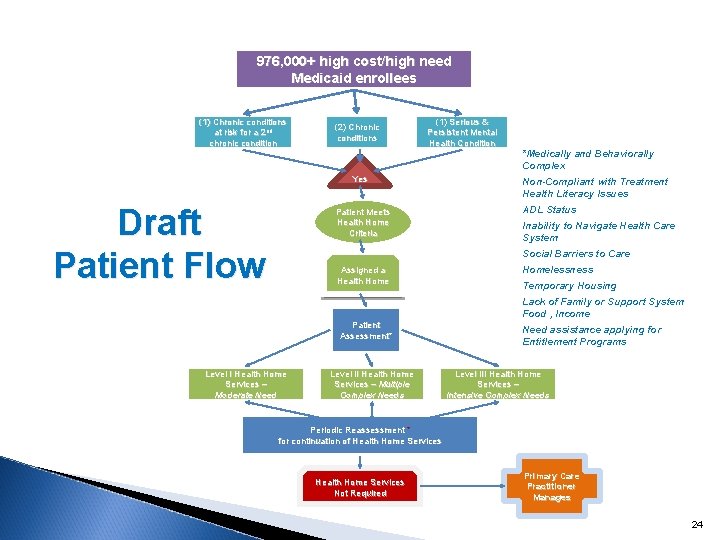
976, 000+ high cost/high need Medicaid enrollees (1) Chronic conditions at risk for a 2 nd chronic condition (2) Chronic conditions (1) Serious & Persistent Mental Health Condition Yes Draft Patient Flow Patient Meets Health Home Criteria *Medically and Behaviorally Complex Non-Compliant with Treatment Health Literacy Issues ADL Status Inability to Navigate Health Care System Social Barriers to Care Assigned a Health Homelessness Temporary Housing Lack of Family or Support System Food , Income Patient Assessment* Level I Health Home Services – Moderate Need Level II Health Home Services – Multiple Complex Needs Need assistance applying for Entitlement Programs Level III Health Home Services – Intensive Complex Needs Periodic Reassessment * for continuation of Health Home Services Not Required Primary Care Practitioner Manages 24
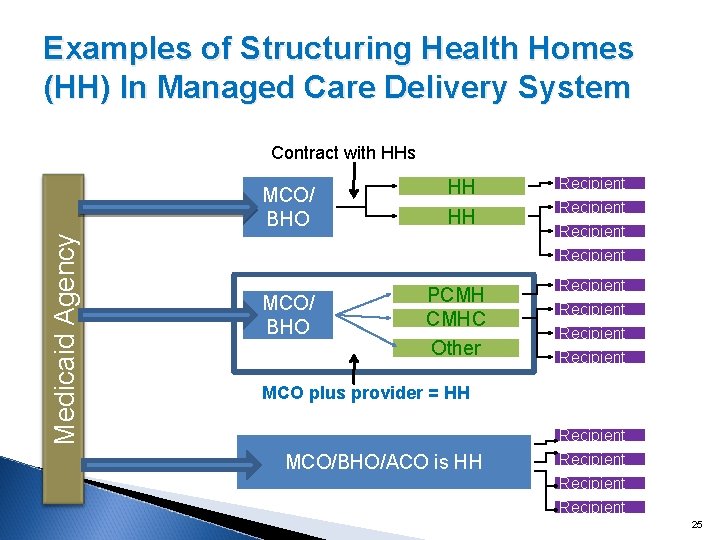
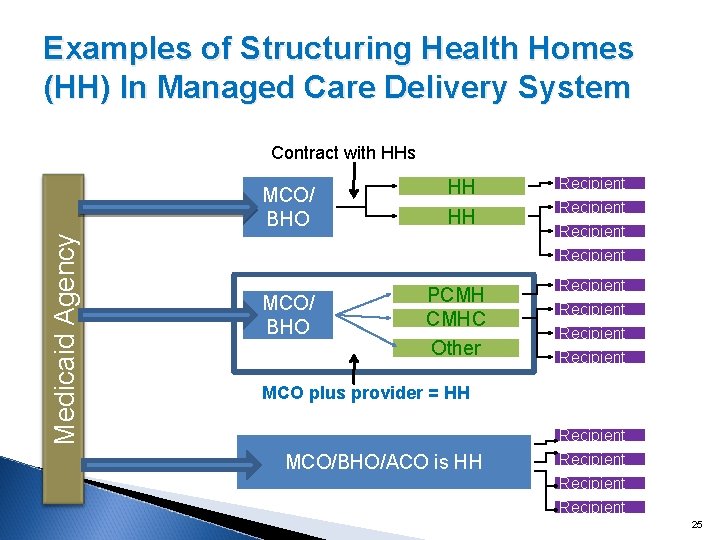
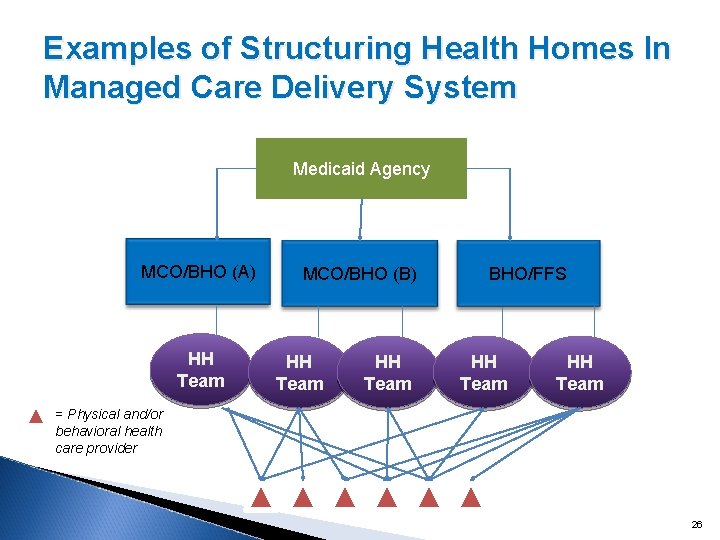
Examples of Structuring Health Homes (HH) In Managed Care Delivery System Contract with HHs Medicaid Agency MCO/ BHO HH HH PCMH CMHC Other Recipient Recipient MCO plus provider = HH MCO/BHO/ACO is HH Recipient 25
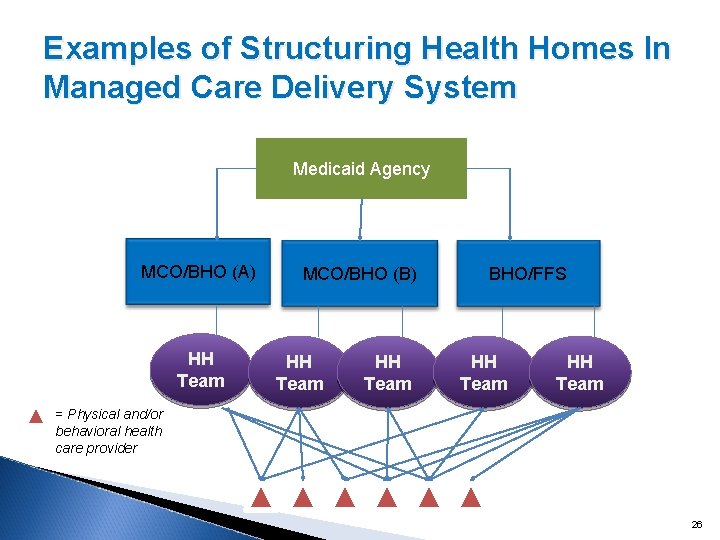
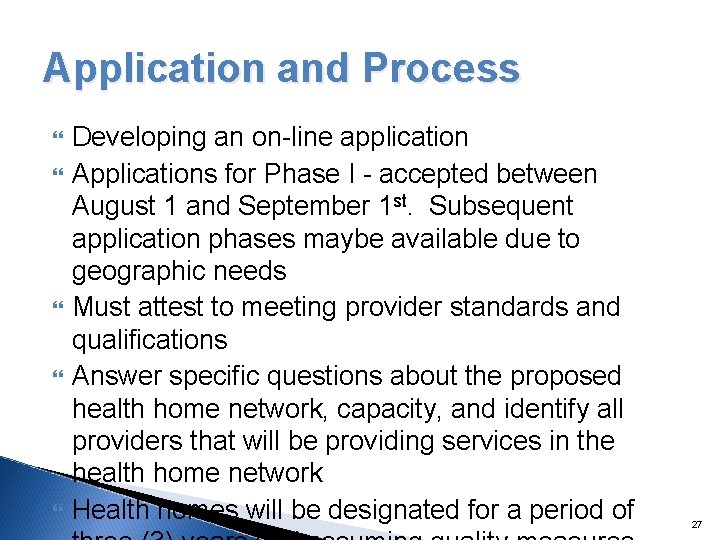
Examples of Structuring Health Homes In Managed Care Delivery System Medicaid Agency MCO/BHO (A) HH Team MCO/BHO (B) HH Team BHO/FFS HH Team = Physical and/or behavioral health care provider 26
Application and Process Developing an on-line application Applications for Phase I - accepted between August 1 and September 1 st. Subsequent application phases maybe available due to geographic needs Must attest to meeting provider standards and qualifications Answer specific questions about the proposed health home network, capacity, and identify all providers that will be providing services in the health home network Health homes will be designated for a period of 27
What makes a Strong Applications will have: ◦ One or more hospital systems ◦ Connections with TCM/CIDPs/MATS programs ◦ Multiple ambulatory care sites with both physical, behavioral and substance abuse specialization, ◦ Community based organizations, including housing, ◦ Managed care plans Applications will either pass or be notified of what elements are missing from the proposal The Department may request that multiple applications from the same geographic area work together and submit a single proposal. 28
Implementation Status Enrollment target – October 2011. Broad Expert Group assisted with development of Interim Health Home Provider Qualifications. CMS and SAMSHA consults occurred with DOH, OMH, OASAS and the Aids Institute. Draft quality measures have been developed with state stakeholders – out for review by Advisory Group. 29
(continued) Implementation Status Draft finance model has been developed with state agencies – out for review by Advisory Group. Draft state plan has been submitted for CMS feedback. 30

Issues Under Consideration Finalizing roles for health plans/BHOs in the delivery of home health systems. Changing how care management is currently provided (e. g. , extending it out to the point of care). Leveraging existing health plan infrastructure (e. g. , data and reporting, provider networks, etc. ). Patient Assignment Algorithms Conversion of TCM Programs Shared Savings Shared Risk 31
Questions Submitted on SPA Over 200 questions were received covering 17 categories Today we will address the most commonly asked questions of the ones submitted. Questions on the SPA will be accepted until Friday, July 22 nd Answers to the questions received will be posted on the health home website in 2 weeks. 32
Need More Information? Have Questions or want to comment? NYS Health Home Web site (links to many relevant materials): http: //nyhealth. gov/health_care/medicaid/progra m/medicaid_health_homes/index. htm. Questions and/or comments regarding New York's implementation of health homes can be directed to hh 2011@health. state. ny. us. 33
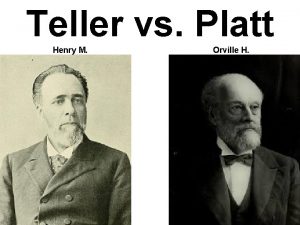
 Platt and teller amendments
Platt and teller amendments New york, new jersey, pennsylvania, and delaware
New york, new jersey, pennsylvania, and delaware Marquee cinema
Marquee cinema Strengths and weaknesses of the articles of confederation
Strengths and weaknesses of the articles of confederation Both new hampshire and new york desire more territory
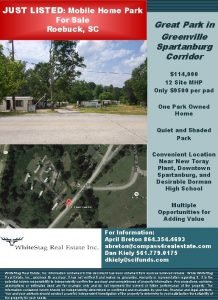
Both new hampshire and new york desire more territory New mobile home sales oak springs mobile home community
New mobile home sales oak springs mobile home community New mobile home sales oak springs mobile home community
New mobile home sales oak springs mobile home community Nymhca
Nymhca New york nurse practitioner association
New york nurse practitioner association Nys student aid payment application
Nys student aid payment application New york state teacher certification examinations
New york state teacher certification examinations New york state standards science
New york state standards science Nys math test 2016
Nys math test 2016 Nerfc
Nerfc Ny state vegetable
Ny state vegetable Environmental facilities corporation
Environmental facilities corporation New york state professional firefighters association
New york state professional firefighters association New york state immunization information system
New york state immunization information system New york state association of transportation engineers
New york state association of transportation engineers Nys industries for the disabled
Nys industries for the disabled New york state division of criminal justice services
New york state division of criminal justice services Nysrc
Nysrc Nysdot hdm
Nysdot hdm Nys tax practitioner hotline
Nys tax practitioner hotline New york state nurse practitioner scope of practice
New york state nurse practitioner scope of practice New york state fish
New york state fish New york state nickname
New york state nickname Emedny formulary
Emedny formulary New york state amateur hockey association
New york state amateur hockey association New york state county highway superintendents association
New york state county highway superintendents association Business etiquette in new york
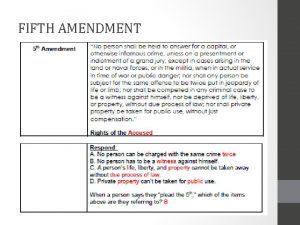
Business etiquette in new york Procedural vs substantive due process
Procedural vs substantive due process Merriweather library buffalo new york
Merriweather library buffalo new york East and west egg great gatsby
East and west egg great gatsby