New Approaches to Monitoring Heart Failure Before Symptoms
New Approaches to Monitoring Heart Failure Before Symptoms Appear William T. Abraham, MD, FACP, FACC Professor of Medicine Chief, Division of Cardiovascular Medicine Associate Director, Davis Heart & Lung Research Institute The Ohio State University Columbus, Ohio 1
Can Implantable Monitors Predict Worsening Heart Failure? Asymptomatic fluid retention Change in impedance or pressure Worsening heart failure Can this prevent hospitalization for worsening heart failure? 2
Intrathoracic Impedance as a Measure of Heart Failure Clinical Status 3
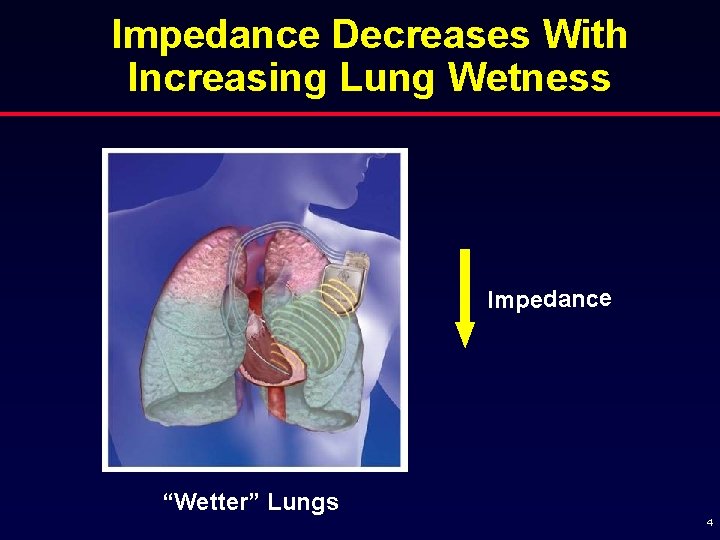
Impedance Decreases With Increasing Lung Wetness Impedance “Wetter” Lungs 4
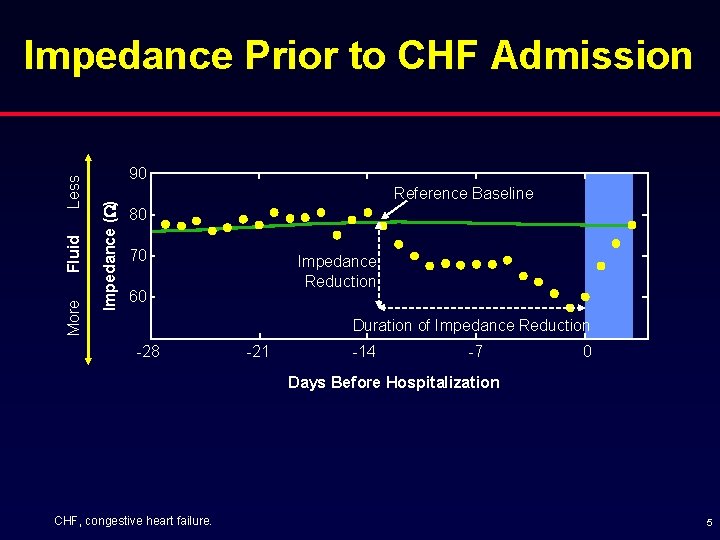
90 Impedance (W) More Fluid Less Impedance Prior to CHF Admission Reference Baseline 80 70 Impedance Reduction 60 Duration of Impedance Reduction -28 -21 -14 -7 0 Days Before Hospitalization CHF, congestive heart failure. 5
Evidence Supporting the Use of Intrathoracic Impedance § Animal studies § Completed MID-He. FT study: Medtronic Impedance Diagnostics in Heart Failure Trial § Ongoing FAST study: Fluid Accumulation Status Trial 6
MID-He. FT Study § MIDHe. FT study – 33 patients, 628 months of follow-up (as of 9/1/03) – 25 hospitalizations for fluid overload from 10 patients – Demonstrated an inverse correlation between impedance and both PCWP and net fluid I/O in patients hospitalized for fluid overload – Demonstrated consistent decreases in impedance in the days preceding hospitalization (ie, predicted hospitalization!) PCWP, pulmonary capillary wedge pressure; I/O, in/out. Yu C-M, et al. Circulation. 2005; 112: 841 -848. 7
MID-He. FT Study Results § Intrathoracic impedance decline preceded the onset of symptoms by mean lead time of 10. 3 days (P<0. 0001) § Retrospective analysis of the clinical data showed that intrathoracic impedances gradually decreased over approximately 2 weeks prior to HF hospitalization (14 days, P<0. 0001) with a total reduction of 11. 3% § Using a single detection threshold for all patients, the Opti. Vol algorithm would have detected 76% of admissions for fluid overload, with an average of only one false warning for every 322 days of patient monitoring HF, heart failure Yu C-M, et al. Circulation. 2005; 112: 841 -848. 8
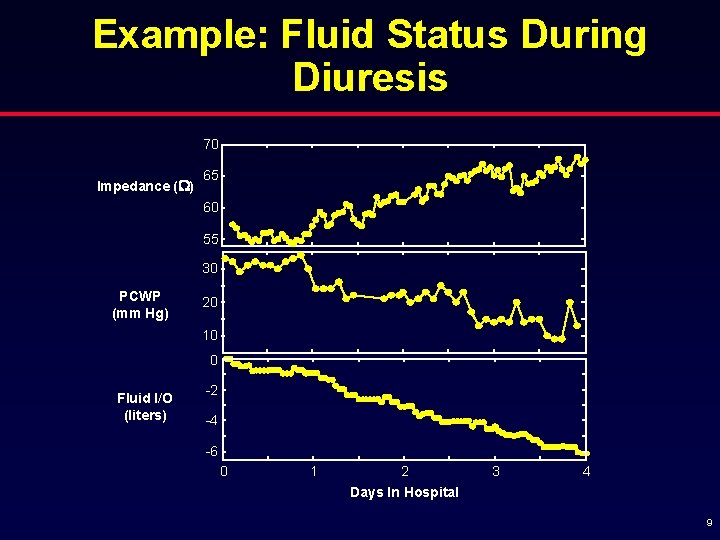
Example: Fluid Status During Diuresis 70 Impedance (W) 65 60 55 30 PCWP (mm Hg) 20 10 0 Fluid I/O (liters) -2 -4 -6 0 1 2 3 4 Days In Hospital 9
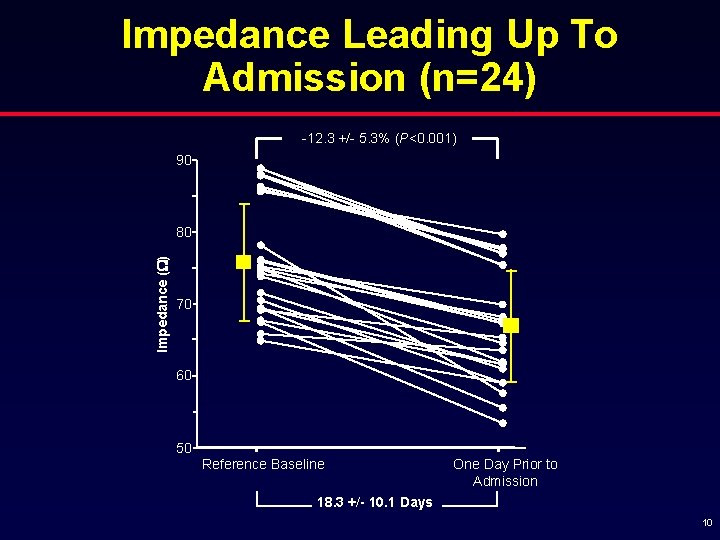
Impedance Leading Up To Admission (n=24) -12. 3 +/- 5. 3% (P<0. 001) 90 Impedance (W) 80 70 60 50 Reference Baseline One Day Prior to Admission 18. 3 +/- 10. 1 Days 10
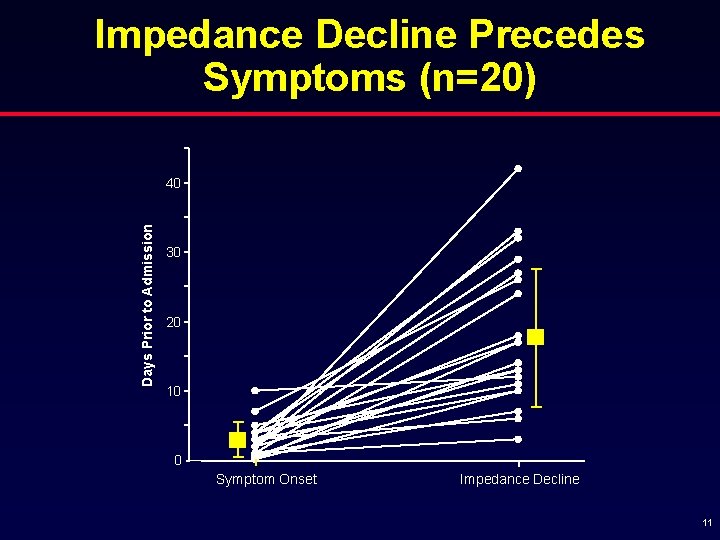
Impedance Decline Precedes Symptoms (n=20) Days Prior to Admission 40 30 20 10 0 Symptom Onset Impedance Decline 11
Automated Detection of Decreases in Intrathoracic Impedance That Precede Hospitalization for CHF 12
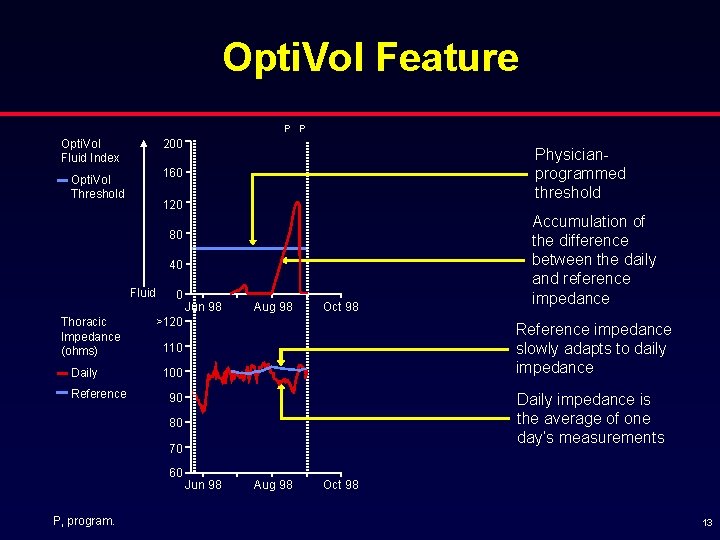
Opti. Vol Feature P P 200 Opti. Vol Fluid Index Physicianprogrammed threshold 160 Opti. Vol Threshold 120 80 40 Fluid Thoracic Impedance (ohms) Daily Reference 0 Jun 98 Aug 98 Oct 98 >120 Reference impedance slowly adapts to daily impedance 110 100 Daily impedance is the average of one day’s measurements 90 80 70 60 P, program. Accumulation of the difference between the daily and reference impedance Jun 98 Aug 98 Oct 98 13
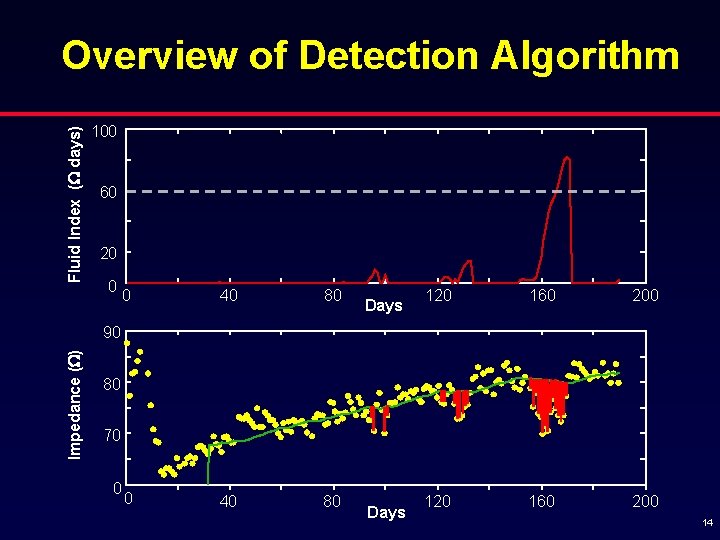
Fluid Index (W days) Overview of Detection Algorithm 100 60 20 0 0 40 80 Days 120 160 200 Impedance (W) 90 80 70 0 Days 14
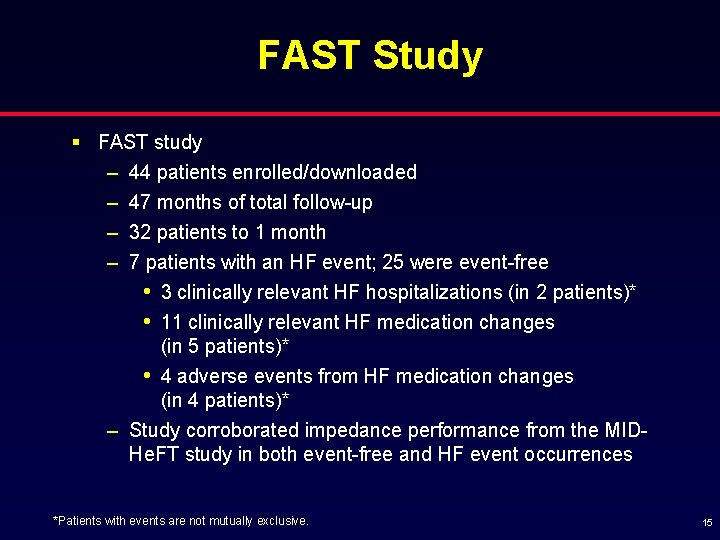
FAST Study § FAST study – 44 patients enrolled/downloaded – 47 months of total follow-up – 32 patients to 1 month – 7 patients with an HF event; 25 were event-free • 3 clinically relevant HF hospitalizations (in 2 patients)* • 11 clinically relevant HF medication changes (in 5 patients)* • 4 adverse events from HF medication changes (in 4 patients)* – Study corroborated impedance performance from the MIDHe. FT study in both event-free and HF event occurrences *Patients with events are not mutually exclusive. 15
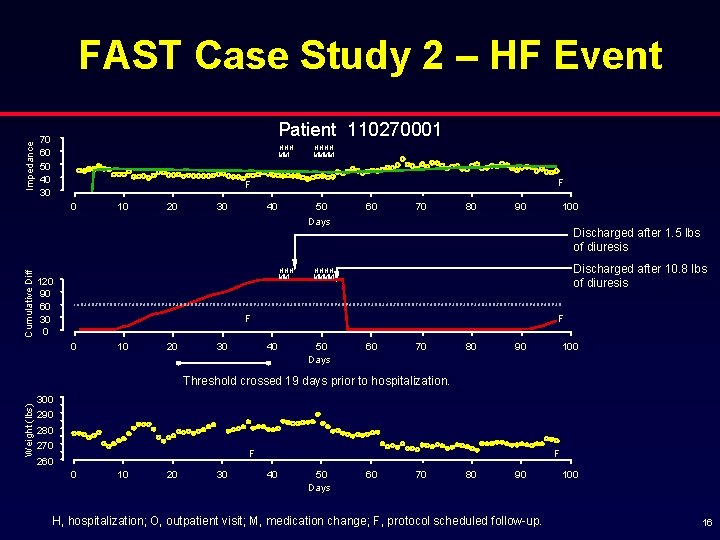
Impedance FAST Case Study 2 – HF Event Patient 110270001 70 60 50 40 30 HHH MM F F 0 Cumulative Diff HHHH MMMM 10 20 30 40 50 Days HHH MM 120 90 60 30 0 60 70 80 90 Discharged after 1. 5 lbs of diuresis Discharged after 10. 8 lbs of diuresis HHHH MMMM F F 0 10 20 30 100 40 50 Days 60 70 80 90 100 Weight (lbs) Threshold crossed 19 days prior to hospitalization. 300 290 280 270 F 260 0 10 20 30 F 40 50 Days 60 70 80 90 H, hospitalization; O, outpatient visit; M, medication change; F, protocol scheduled follow-up. 100 16
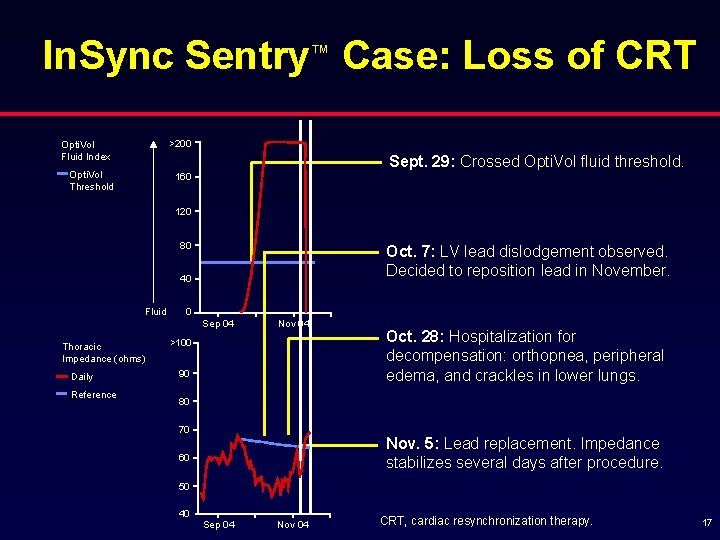
In. Sync Sentry™ Case: Loss of CRT >200 Opti. Vol Fluid Index Sept. 29: Crossed Opti. Vol fluid threshold. Opti. Vol Threshold 160 120 80 Oct. 7: LV lead dislodgement observed. Decided to reposition lead in November. 40 Fluid 0 Sep 04 Thoracic Impedance (ohms) Daily Reference Nov 04 >100 90 Oct. 28: Hospitalization for decompensation: orthopnea, peripheral edema, and crackles in lower lungs. 80 70 Nov. 5: Lead replacement. Impedance stabilizes several days after procedure. 60 50 40 Sep 04 Nov 04 CRT, cardiac resynchronization therapy. 17
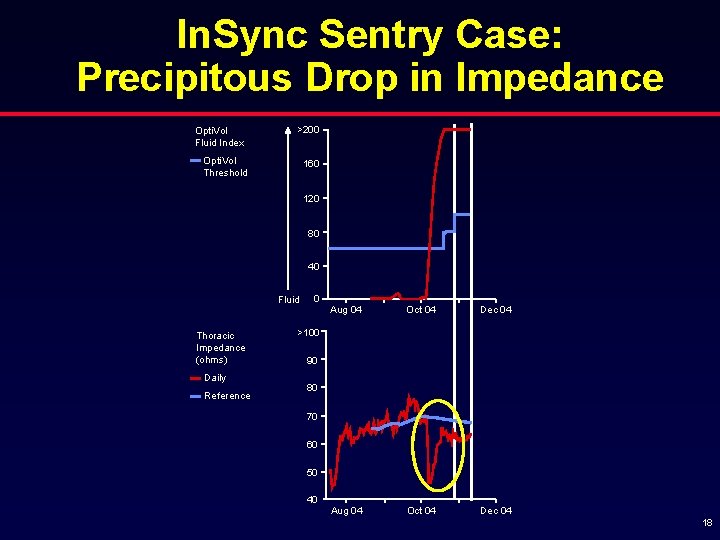
In. Sync Sentry Case: Precipitous Drop in Impedance Opti. Vol Fluid Index >200 Opti. Vol Threshold 160 120 80 40 Fluid Thoracic Impedance (ohms) Daily Reference 0 Aug 04 Oct 04 Dec 04 >100 90 80 70 60 50 40 18
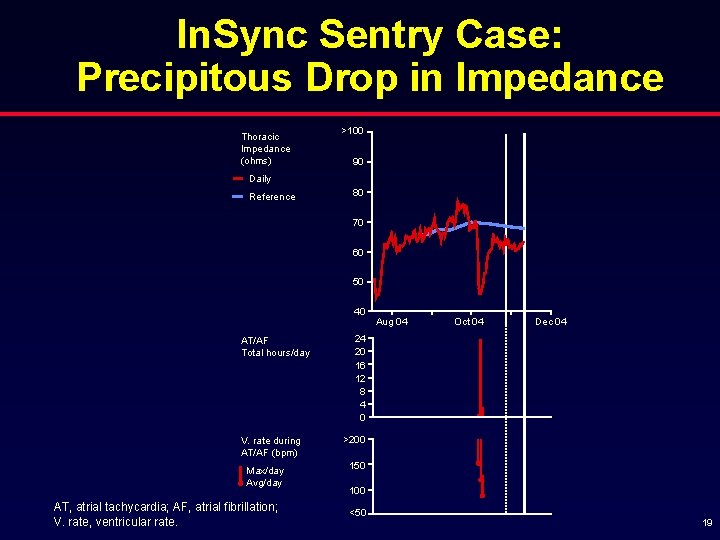
In. Sync Sentry Case: Precipitous Drop in Impedance Thoracic Impedance (ohms) >100 90 Daily Reference 80 70 60 50 40 AT/AF Total hours/day V. rate during AT/AF (bpm) Max/day Avg/day AT, atrial tachycardia; AF, atrial fibrillation; V. rate, ventricular rate. Aug 04 Oct 04 Dec 04 24 20 16 12 8 4 0 >200 150 100 <50 19
Implantable Hemodynamic Monitoring Systems 20
Implantable Hemodynamic Monitor 21
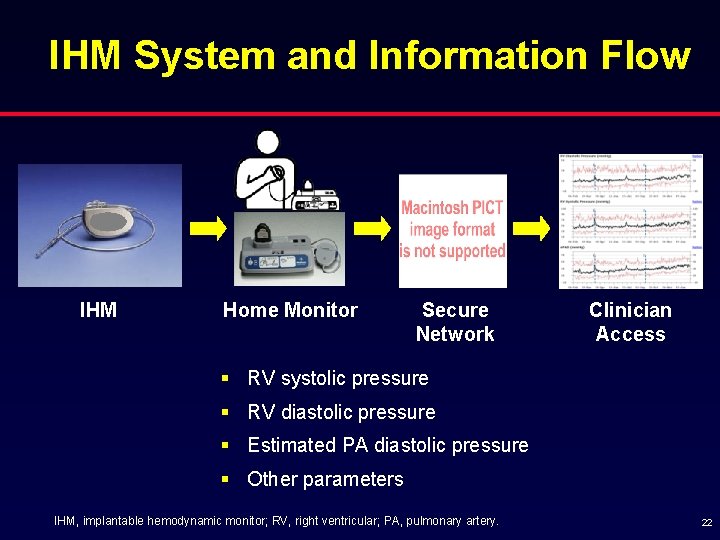
IHM System and Information Flow IHM Home Monitor Secure Network Clinician Access § RV systolic pressure § RV diastolic pressure § Estimated PA diastolic pressure § Other parameters IHM, implantable hemodynamic monitor; RV, right ventricular; PA, pulmonary artery. 22
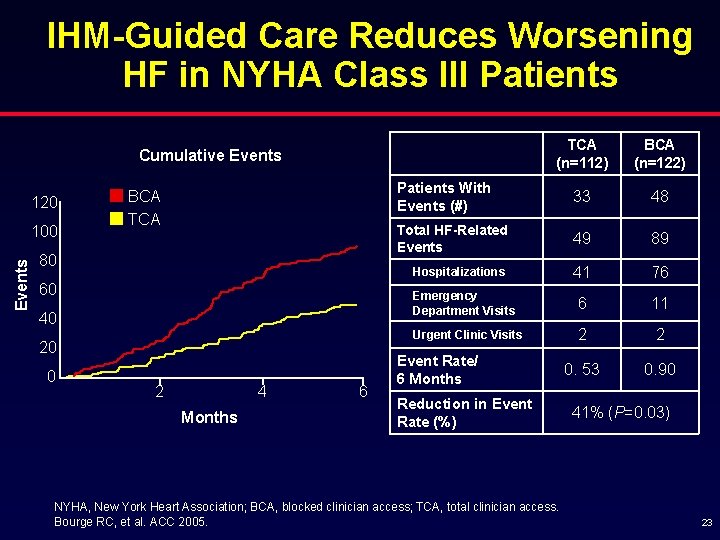
IHM-Guided Care Reduces Worsening HF in NYHA Class III Patients TCA (n=112) BCA (n=122) Patients With Events (#) 33 48 Total HF-Related Events 49 89 Hospitalizations 41 76 Emergency Department Visits 6 11 Urgent Clinic Visits 2 2 0. 53 0. 90 Cumulative Events 120 Events 100 BCA TCA 80 60 40 20 0 2 4 Months 6 Event Rate/ 6 Months Reduction in Event Rate (%) NYHA, New York Heart Association; BCA, blocked clinician access; TCA, total clinician access. Bourge RC, et al. ACC 2005. 41% (P=0. 03) 23
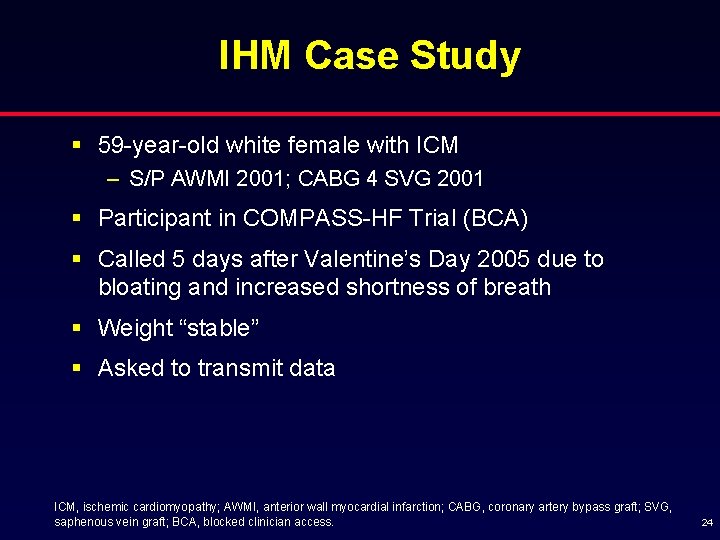
IHM Case Study § 59 -year-old white female with ICM – S/P AWMI 2001; CABG 4 SVG 2001 § Participant in COMPASS-HF Trial (BCA) § Called 5 days after Valentine’s Day 2005 due to bloating and increased shortness of breath § Weight “stable” § Asked to transmit data ICM, ischemic cardiomyopathy; AWMI, anterior wall myocardial infarction; CABG, coronary artery bypass graft; SVG, saphenous vein graft; BCA, blocked clinician access. 24
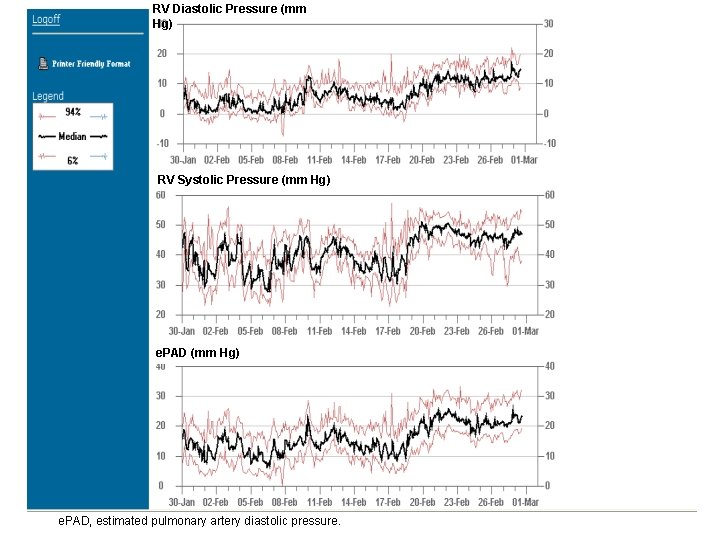
RV Diastolic Pressure (mm Hg) RV Systolic Pressure (mm Hg) e. PAD, estimated pulmonary artery diastolic pressure. 25
IHM Case Study § Had celebrated Valentine’s Day by going out to eat – At an Indian restaurant! – Very thirsty – increased fluids § Diuretics increased 26
Summary § Long-term trends in intrathoracic impedance may provide an early warning of impending episodes of decompensation in outpatients § Implantable hemodynamic monitoring (IHM) enables the day-to-day management of ventricular filling pressures in CHF patients § Intrathoracic impedance and IHM represent complimentary and promising new technologies for the management of HF 27
- Slides: 27