NEUROSCIENCES 232 Parkinsons Disease David D Song M




- Slides: 25
NEUROSCIENCES 232: Parkinson’s Disease David D. Song, M. D. , Ph. D. Department of Neurosciences University of California, San Diego

Parkinson’s Disease:

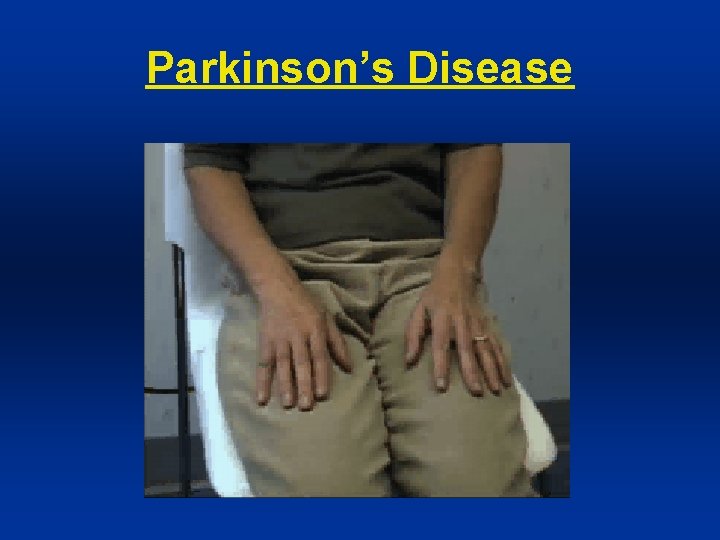
PD: Clinical Manifestations • “Pill Rolling” Tremor (at Rest 4 -6 Htz) • Shuffling gait (Festination) • Masked Facies (Hypomimia) • Micrographia • Hypophonia • Drooling • Dysphagia

PD: Micrographia
PD: Classic Clinical Triad (Cardinal Signs) • Bradykinesia (slowness of movement; with hypokinesia (reduced amplitude) and may have akinesia, the absence of movement) • Rigidity (increased tone, can be “lead pipe” or “cog-wheel”; distinct from spasticity and paratonia) • Resting Tremor (tremor more at rest or when distracted and less with action; may be “pill-rolling” when involving hands)
PD: Fourth Cardinal Sign • Postural Instability (typically mild or absent at initial presentation)
Parkinson’s Disease
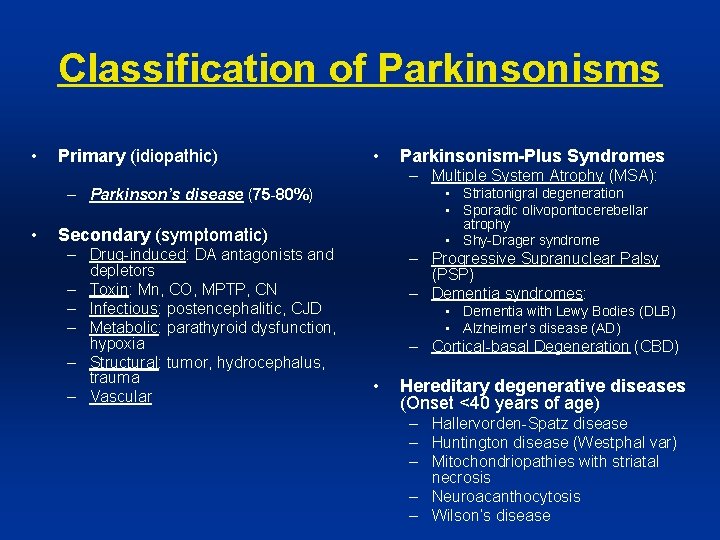
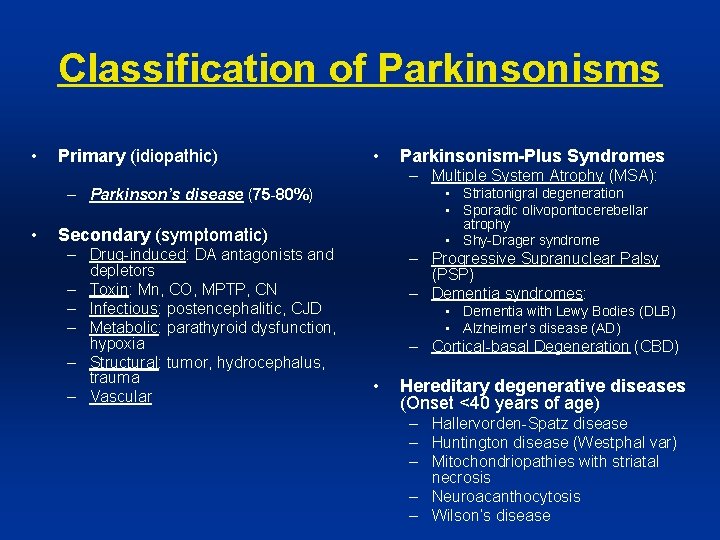
Classification of Parkinsonisms • Primary (idiopathic) • Parkinsonism-Plus Syndromes – Multiple System Atrophy (MSA): • Striatonigral degeneration • Sporadic olivopontocerebellar atrophy • Shy-Drager syndrome – Parkinson’s disease (75 -80%) • Secondary (symptomatic) – Drug-induced: DA antagonists and depletors – Toxin: Mn, CO, MPTP, CN – Infectious: postencephalitic, CJD – Metabolic: parathyroid dysfunction, hypoxia – Structural: tumor, hydrocephalus, trauma – Vascular – Progressive Supranuclear Palsy (PSP) – Dementia syndromes: • Dementia with Lewy Bodies (DLB) • Alzheimer’s disease (AD) – Cortical-basal Degeneration (CBD) • Hereditary degenerative diseases (Onset <40 years of age) – Hallervorden-Spatz disease – Huntington disease (Westphal var) – Mitochondriopathies with striatal necrosis – Neuroacanthocytosis – Wilson’s disease

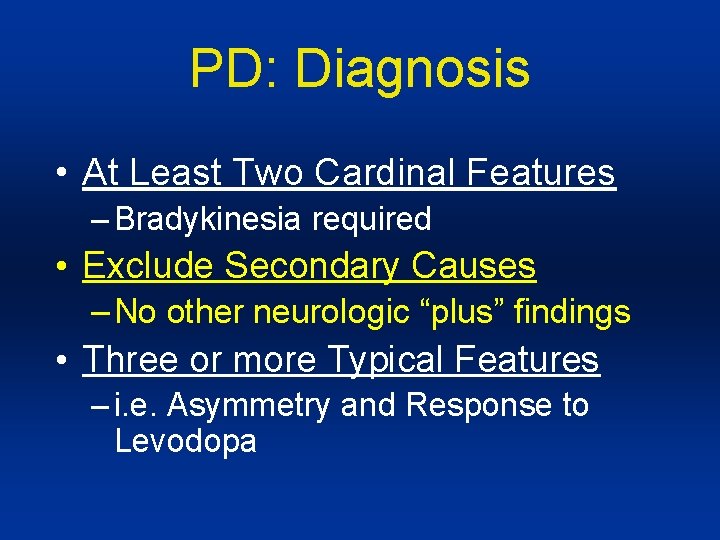
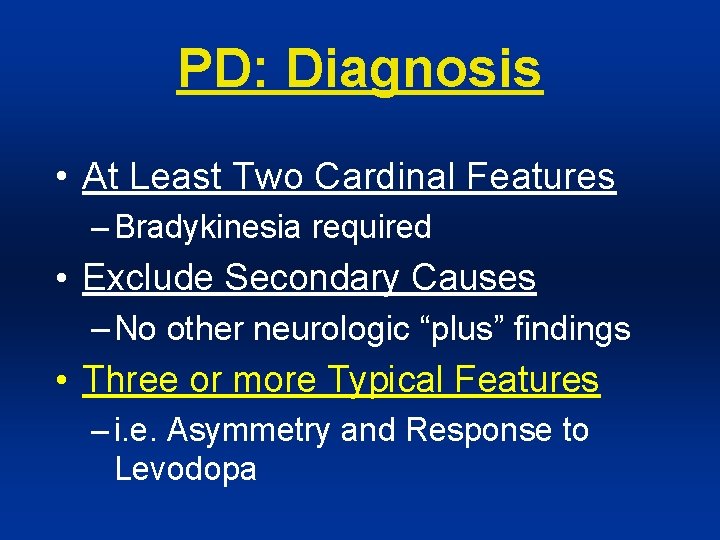
PD: Diagnosis • At Least Two Cardinal Features – Bradykinesia required • Exclude Secondary Causes – No other neurologic “plus” findings • Three or more Typical Features – i. e. Asymmetry and Response to Levodopa
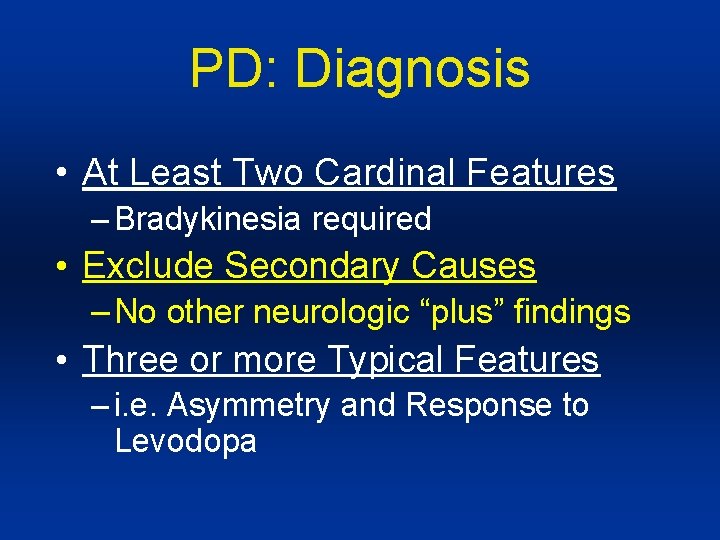
PD: Diagnosis • At Least Two Cardinal Features – Bradykinesia required • Exclude Secondary Causes – No other neurologic “plus” findings • Three or more Typical Features – i. e. Asymmetry and Response to Levodopa
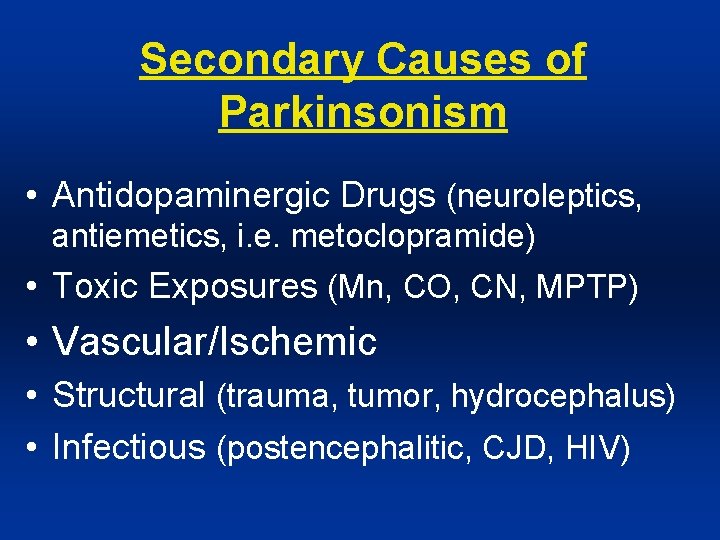
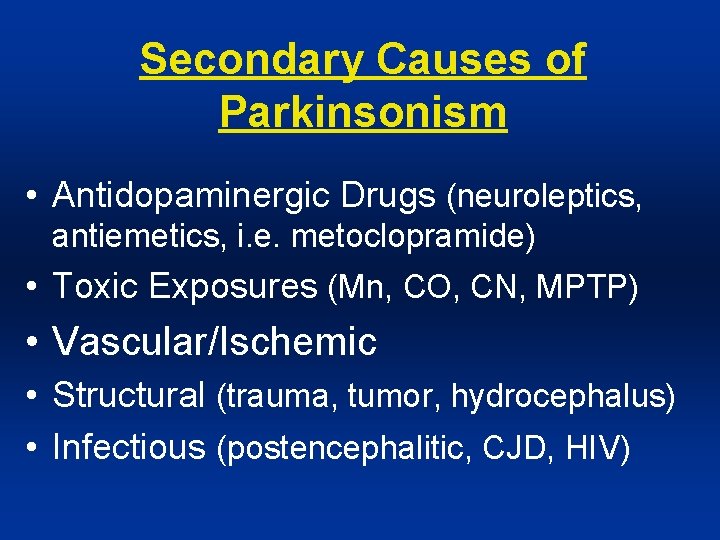
Secondary Causes of Parkinsonism • Antidopaminergic Drugs (neuroleptics, antiemetics, i. e. metoclopramide) • Toxic Exposures (Mn, CO, CN, MPTP) • Vascular/Ischemic • Structural (trauma, tumor, hydrocephalus) • Infectious (postencephalitic, CJD, HIV)
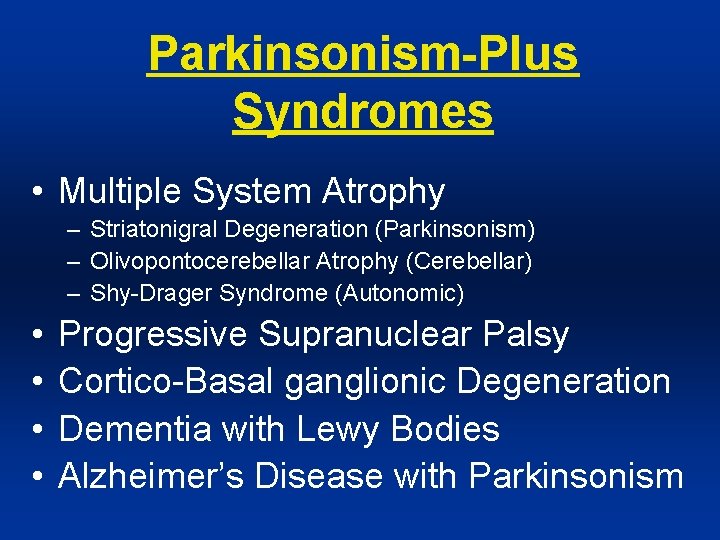
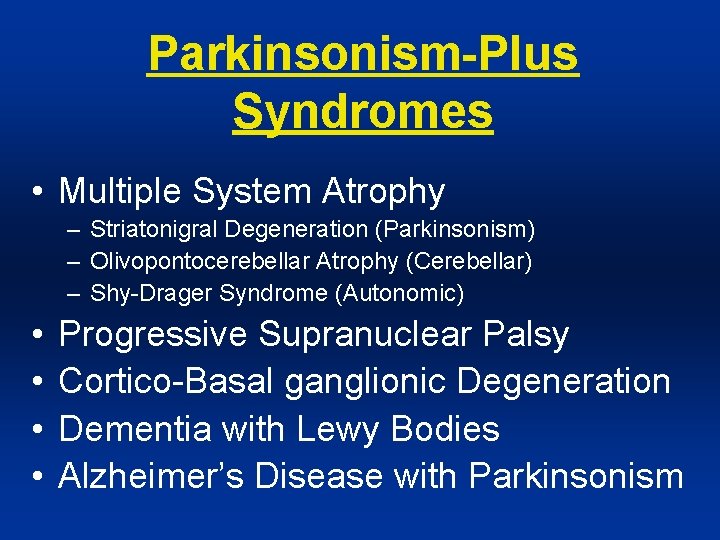
Parkinsonism-Plus Syndromes • Multiple System Atrophy – Striatonigral Degeneration (Parkinsonism) – Olivopontocerebellar Atrophy (Cerebellar) – Shy-Drager Syndrome (Autonomic) • • Progressive Supranuclear Palsy Cortico-Basal ganglionic Degeneration Dementia with Lewy Bodies Alzheimer’s Disease with Parkinsonism
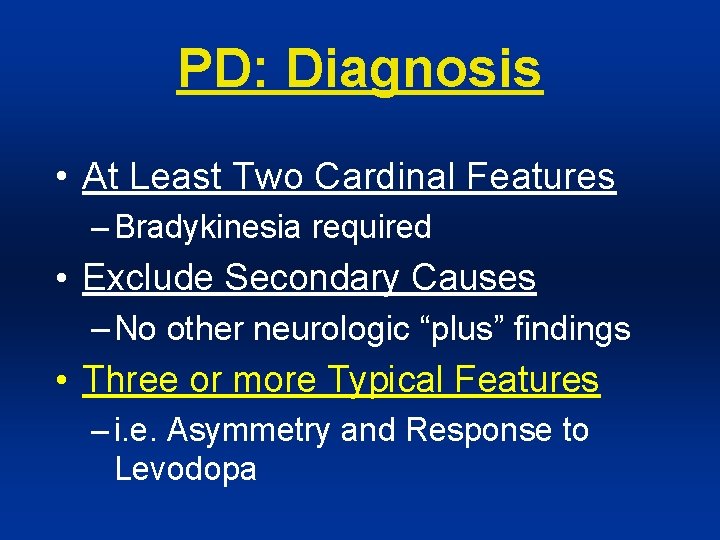
PD: Diagnosis • At Least Two Cardinal Features – Bradykinesia required • Exclude Secondary Causes – No other neurologic “plus” findings • Three or more Typical Features – i. e. Asymmetry and Response to Levodopa
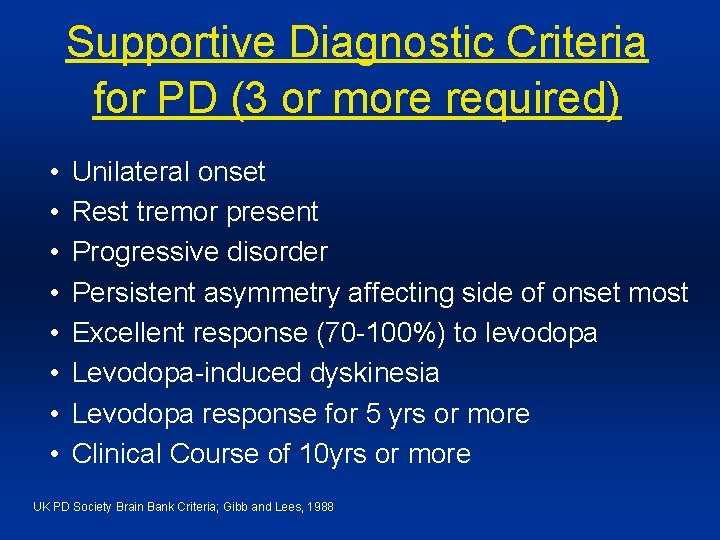
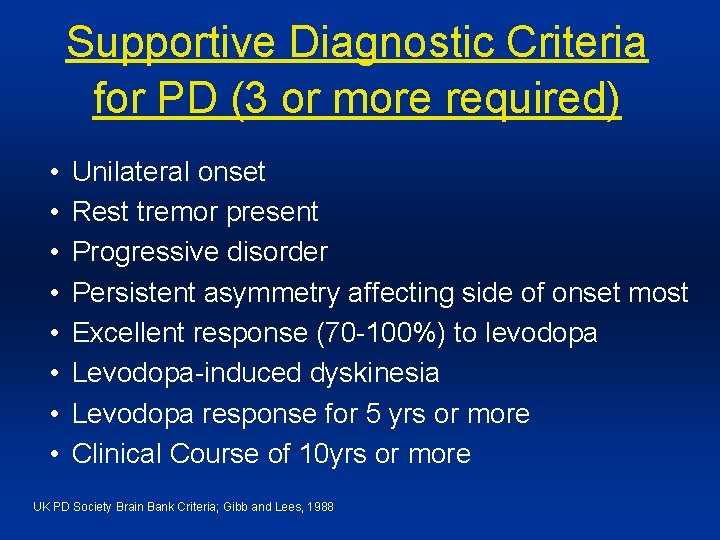
Supportive Diagnostic Criteria for PD (3 or more required) • • Unilateral onset Rest tremor present Progressive disorder Persistent asymmetry affecting side of onset most Excellent response (70 -100%) to levodopa Levodopa-induced dyskinesia Levodopa response for 5 yrs or more Clinical Course of 10 yrs or more UK PD Society Brain Bank Criteria; Gibb and Lees, 1988
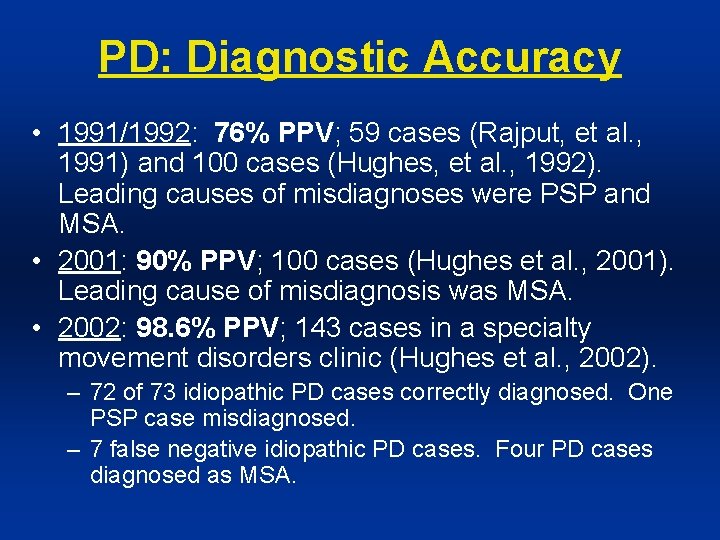
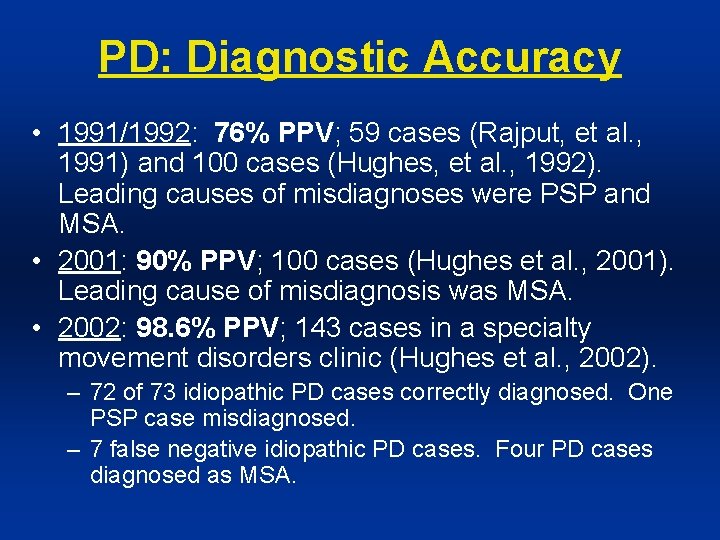
PD: Diagnostic Accuracy • 1991/1992: 76% PPV; 59 cases (Rajput, et al. , 1991) and 100 cases (Hughes, et al. , 1992). Leading causes of misdiagnoses were PSP and MSA. • 2001: 90% PPV; 100 cases (Hughes et al. , 2001). Leading cause of misdiagnosis was MSA. • 2002: 98. 6% PPV; 143 cases in a specialty movement disorders clinic (Hughes et al. , 2002). – 72 of 73 idiopathic PD cases correctly diagnosed. One PSP case misdiagnosed. – 7 false negative idiopathic PD cases. Four PD cases diagnosed as MSA.
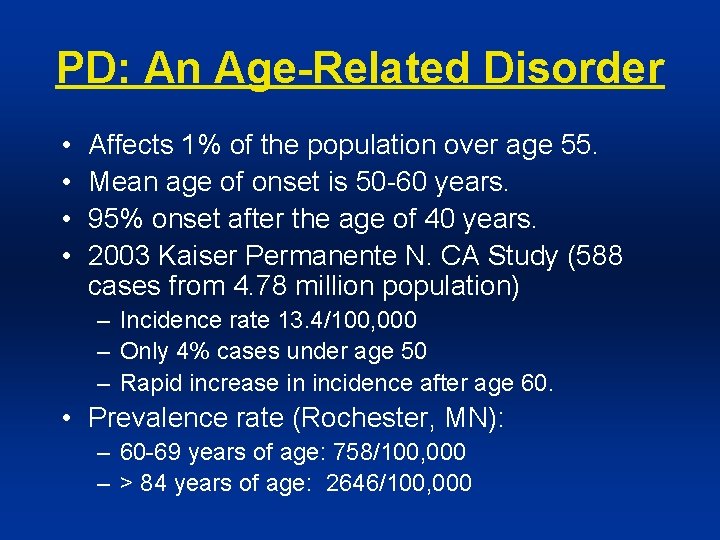
PD: An Age-Related Disorder • • Affects 1% of the population over age 55. Mean age of onset is 50 -60 years. 95% onset after the age of 40 years. 2003 Kaiser Permanente N. CA Study (588 cases from 4. 78 million population) – Incidence rate 13. 4/100, 000 – Only 4% cases under age 50 – Rapid increase in incidence after age 60. • Prevalence rate (Rochester, MN): – 60 -69 years of age: 758/100, 000 – > 84 years of age: 2646/100, 000
PD Risk: Environment • Increased Risk: – Farming – Rural residence – Herbicide/pesticide exposures • Decreased Risk: – Cigarette smoking – Caffeine – Drinking alcohol
PD Risk: Genetics • 1: 20 Lifetime risk with one first-degree relative (vs. 1: 40 in the general population). • 1: 5 Lifetime risk with two first-degree relatives. • Familial cases relatively rare (5 -10%) • Autosomal Dominant • • Alpha-synuclein/SNCA (PARK 1 and 5) Ubiquitin carboxyhydrolase L 1/UCH-L 1 (PARK 3) Tau/MAPT (PARK 4) Dardarin/LRRK 2 (PARK 8) • Autosomal Recessive • Parkin/PRKN (PARK 2) • PINK-1 (PARK 6) • DJ-1 (PARK 7)
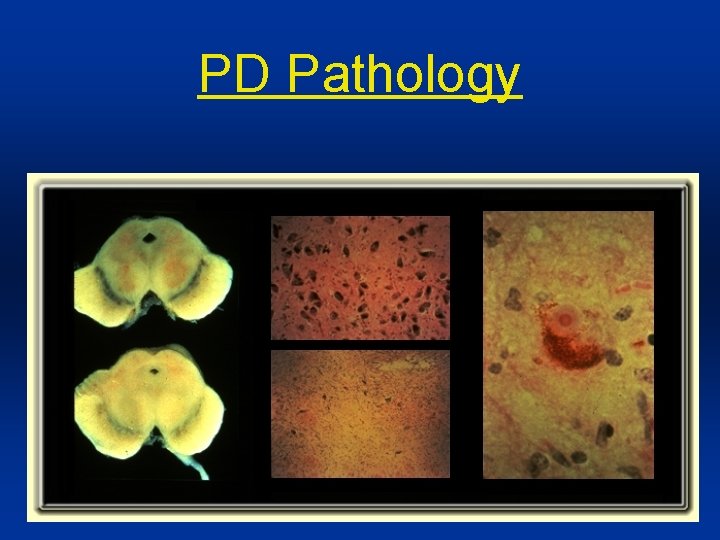
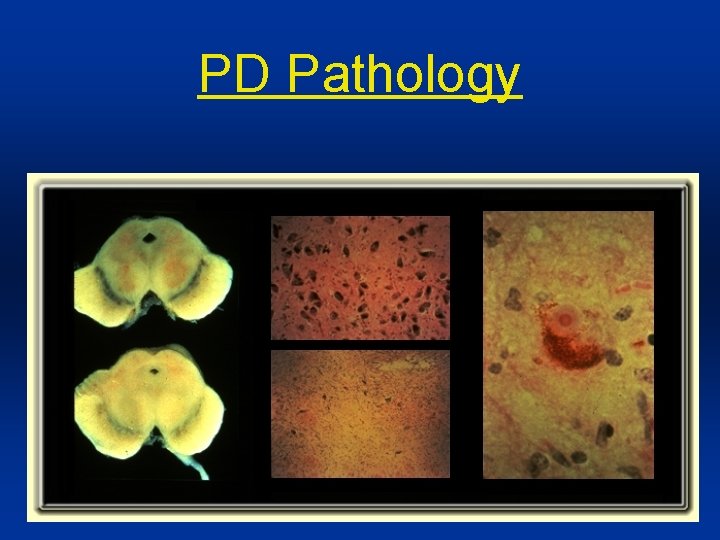
PD Pathology
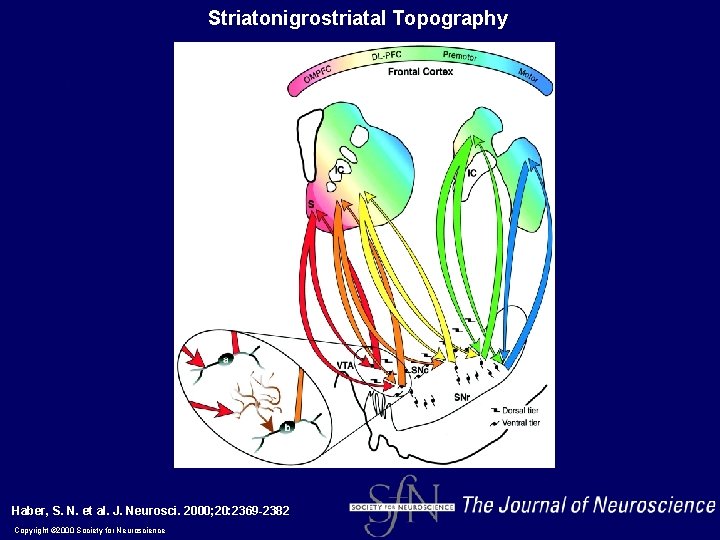
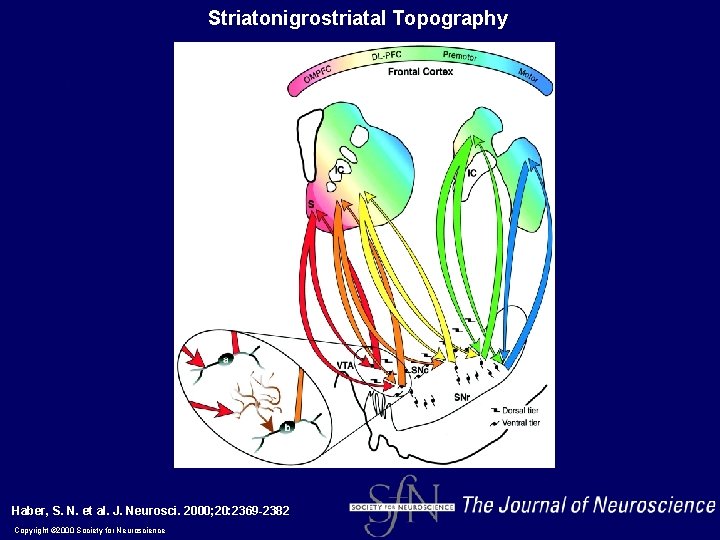
Striatonigrostriatal Topography Haber, S. N. et al. J. Neurosci. 2000; 20: 2369 -2382 Copyright © 2000 Society for Neuroscience
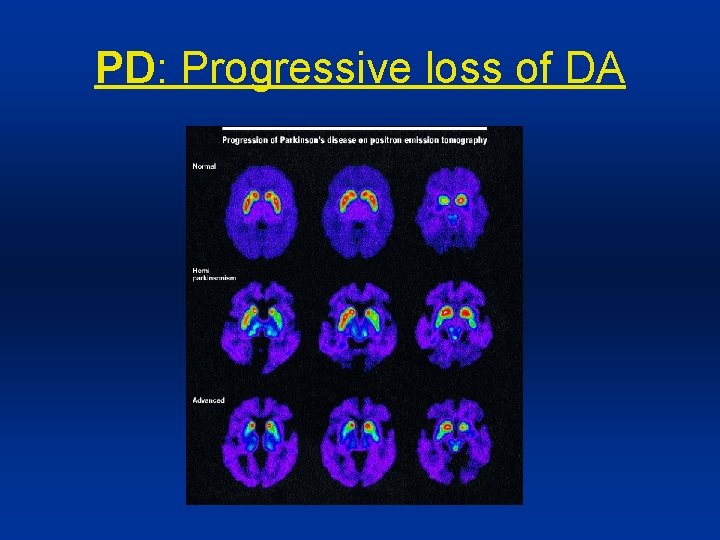
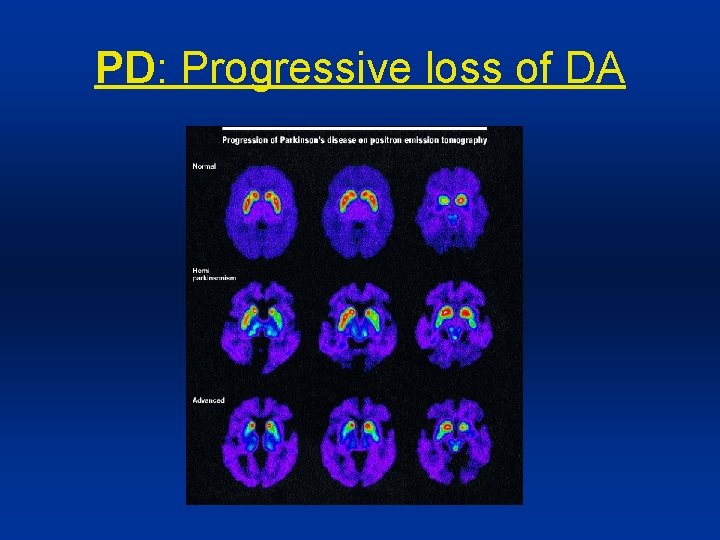
PD: Progressive loss of DA
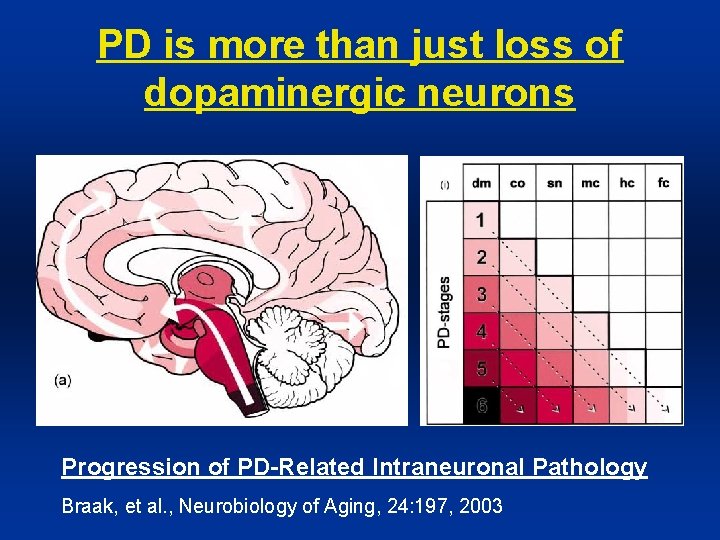
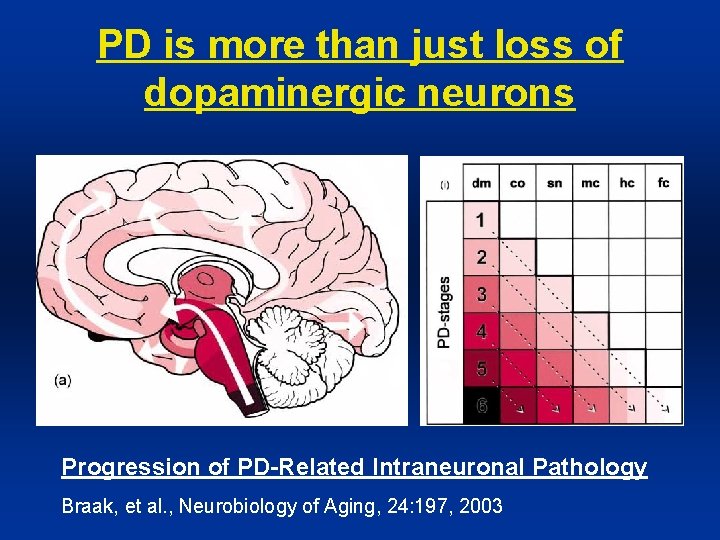
PD is more than just loss of dopaminergic neurons Progression of PD-Related Intraneuronal Pathology Braak, et al. , Neurobiology of Aging, 24: 197, 2003
PD Non-Motor Complications: Common and Disabling • Neuropsychiatric – – – Cognitive Dysfunction/Dementia Hallucinations/Psychosis Compulsive Behavior Depression Anxiety • Sleep Disorders • Autonomic Disorders – – – Orthostatic Hypotension Urologic Sexual Dysfunction Constipation Sweating • Sensory Symptoms/Pain
Parkinson’s Disease
Web Resources • Parkinson’s Disease Foundation (www. pdf. org) • National Parkinson Foundation (www. parkinson. org) • National Institute of Neurological Disorders and Stroke (www. ninds. nih. gov) • WEMOVE (wemove. org)