NEUROMUSCULAR BLOCKADE REVERSAL PRACTICE JULIA LIENESCH CARRIE MCMAHON
NEUROMUSCULAR BLOCKADE REVERSAL PRACTICE JULIA LIENESCH & CARRIE MCMAHON GONZAGA UNIVERSITY PROVIDENCE SACRED HEART MEDICAL CENTER MARCH 20, 2014
STATEMENT OF THE PROBLEM �Residual neuromuscular blockade and its management are well-established topics in current literature �The incidence of residual blockade has not significantly declined even with the introduction of intermediate acting paralytics �From 2000 -2008, 15 studies revealed 20 -65% of postoperative incidence TOFR <0. 9 Associated with hypoxia, weakness, aspiration, impairment of the hypoxic ventilatory drive, and respiratory failure

RESIDUAL BLOCKADE DEFINITION �Residual blockade definition TOFR of < 0. 9 Clinical signs and symptoms of muscle weakness in the postoperative period �Evolution of TOFR standard for extubation 0. 7 0. 8 currently 0. 9 Increased respiratory events, pharyngeal dysfunction, and aspiration risk with TOFR <0. 9 (Eriksson et al, 1997)
PURPOSE STATEMENT “The purpose of this study was to assess, through survey, current practices among CRNAs in states from various regions regarding the use of reversal agents after pharmacologic neuromuscular blockade. ”
RESEARCH QUESTIONS 1. To what degree are reversal agents being given by CRNAs after the administration of neuromuscular blocking agents? 2. What are the benefits and risks of neuromuscular blockade reversal? 3. What factors influence CRNAs’ management of neuromuscular blockade reversal? 4. How is the dose of reversal agent determined?
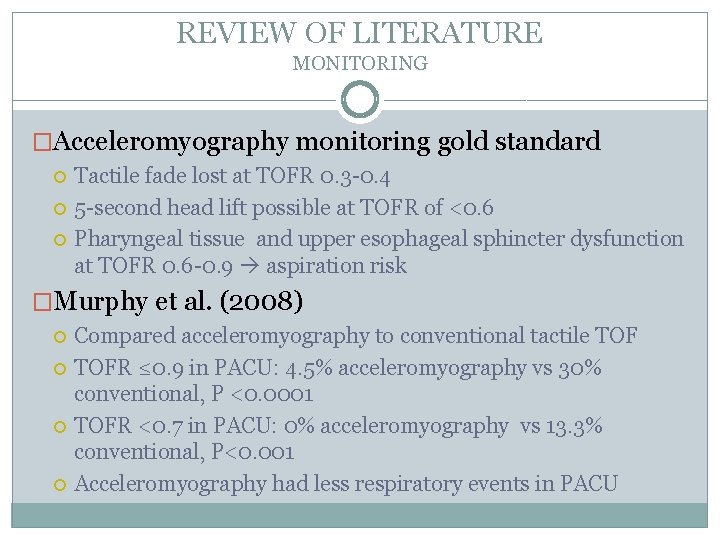
REVIEW OF LITERATURE MONITORING �Acceleromyography monitoring gold standard Tactile fade lost at TOFR 0. 3 -0. 4 5 -second head lift possible at TOFR of <0. 6 Pharyngeal tissue and upper esophageal sphincter dysfunction at TOFR 0. 6 -0. 9 aspiration risk �Murphy et al. (2008) Compared acceleromyography to conventional tactile TOFR ≤ 0. 9 in PACU: 4. 5% acceleromyography vs 30% conventional, P <0. 0001 TOFR <0. 7 in PACU: 0% acceleromyography vs 13. 3% conventional, P<0. 001 Acceleromyography had less respiratory events in PACU
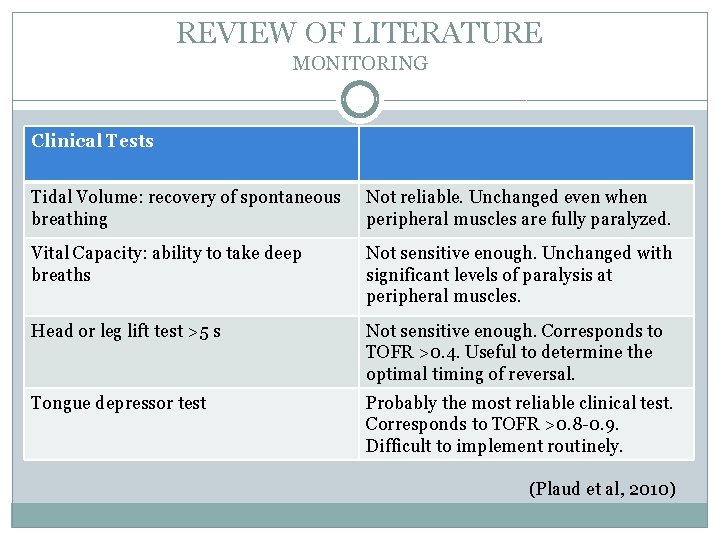
REVIEW OF LITERATURE MONITORING Clinical Tests Tidal Volume: recovery of spontaneous breathing Not reliable. Unchanged even when peripheral muscles are fully paralyzed. Vital Capacity: ability to take deep breaths Not sensitive enough. Unchanged with significant levels of paralysis at peripheral muscles. Head or leg lift test >5 s Not sensitive enough. Corresponds to TOFR >0. 4. Useful to determine the optimal timing of reversal. Tongue depressor test Probably the most reliable clinical test. Corresponds to TOFR >0. 8 -0. 9. Difficult to implement routinely. (Plaud et al, 2010)
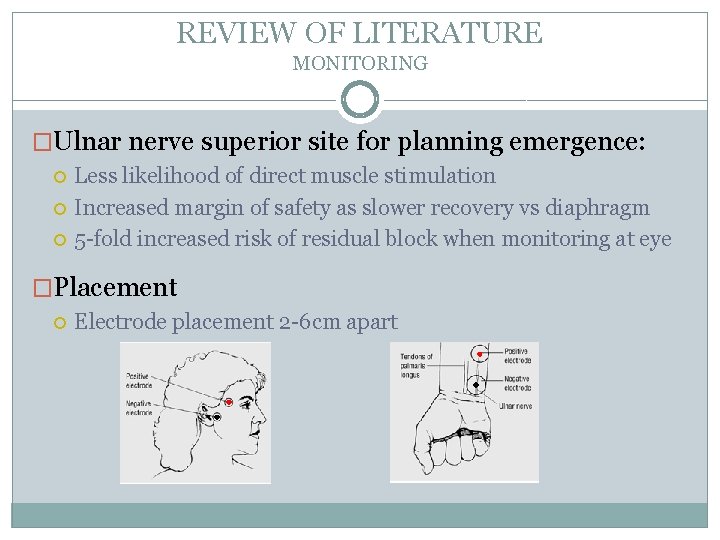
REVIEW OF LITERATURE MONITORING �Ulnar nerve superior site for planning emergence: Less likelihood of direct muscle stimulation Increased margin of safety as slower recovery vs diaphragm 5 -fold increased risk of residual block when monitoring at eye �Placement Electrode placement 2 -6 cm apart
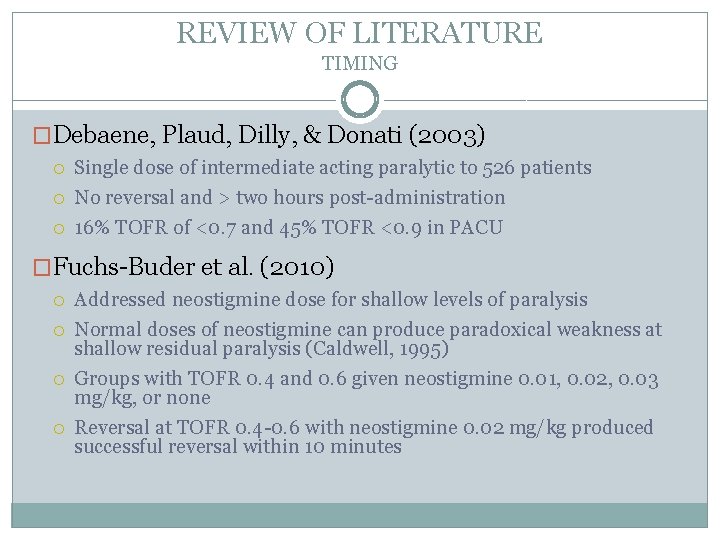
REVIEW OF LITERATURE TIMING �Debaene, Plaud, Dilly, & Donati (2003) Single dose of intermediate acting paralytic to 526 patients No reversal and > two hours post-administration 16% TOFR of <0. 7 and 45% TOFR <0. 9 in PACU �Fuchs-Buder et al. (2010) Addressed neostigmine dose for shallow levels of paralysis Normal doses of neostigmine can produce paradoxical weakness at shallow residual paralysis (Caldwell, 1995) Groups with TOFR 0. 4 and 0. 6 given neostigmine 0. 01, 0. 02, 0. 03 mg/kg, or none Reversal at TOFR 0. 4 -0. 6 with neostigmine 0. 02 mg/kg produced successful reversal within 10 minutes
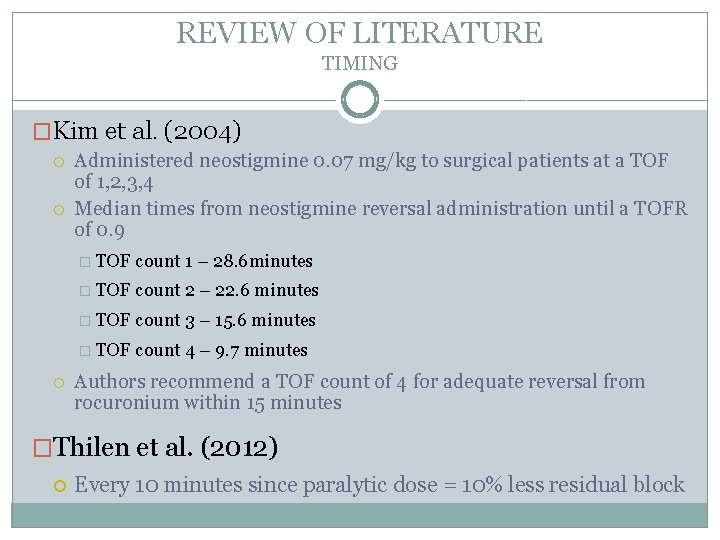
REVIEW OF LITERATURE TIMING �Kim et al. (2004) Administered neostigmine 0. 07 mg/kg to surgical patients at a TOF of 1, 2, 3, 4 Median times from neostigmine reversal administration until a TOFR of 0. 9 � TOF count 1 – 28. 6 minutes � TOF count 2 – 22. 6 minutes � TOF count 3 – 15. 6 minutes � TOF count 4 – 9. 7 minutes Authors recommend a TOF count of 4 for adequate reversal from rocuronium within 15 minutes �Thilen et al. (2012) Every 10 minutes since paralytic dose = 10% less residual block
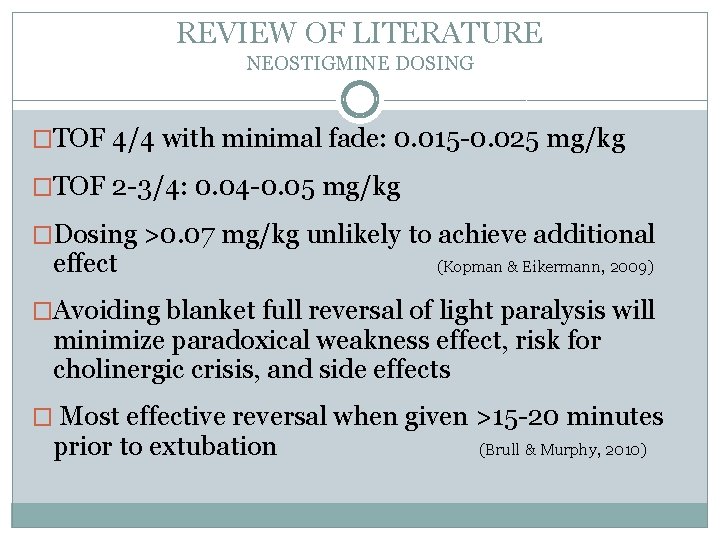
REVIEW OF LITERATURE NEOSTIGMINE DOSING �TOF 4/4 with minimal fade: 0. 015 -0. 025 mg/kg �TOF 2 -3/4: 0. 04 -0. 05 mg/kg �Dosing >0. 07 mg/kg unlikely to achieve additional effect (Kopman & Eikermann, 2009) �Avoiding blanket full reversal of light paralysis will minimize paradoxical weakness effect, risk for cholinergic crisis, and side effects � Most effective reversal when given >15 -20 minutes prior to extubation (Brull & Murphy, 2010)
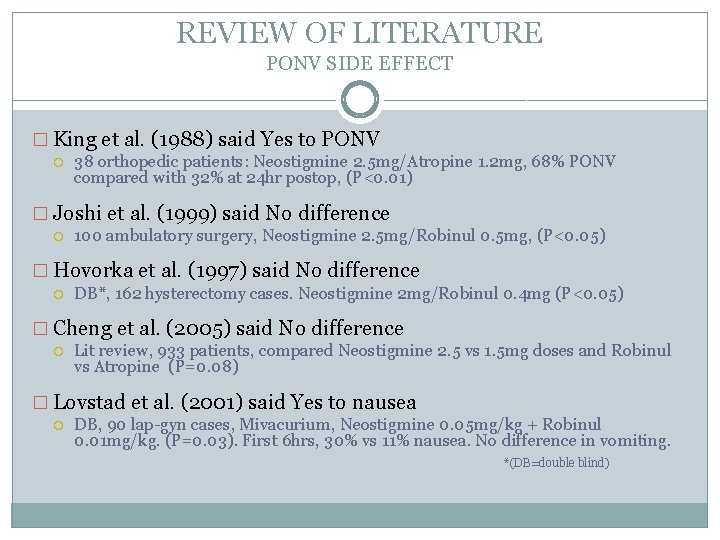
REVIEW OF LITERATURE PONV SIDE EFFECT � King et al. (1988) said Yes to PONV 38 orthopedic patients: Neostigmine 2. 5 mg/Atropine 1. 2 mg, 68% PONV compared with 32% at 24 hr postop, (P<0. 01) � Joshi et al. (1999) said No difference 100 ambulatory surgery, Neostigmine 2. 5 mg/Robinul 0. 5 mg, (P<0. 05) � Hovorka et al. (1997) said No difference DB*, 162 hysterectomy cases. Neostigmine 2 mg/Robinul 0. 4 mg (P<0. 05) � Cheng et al. (2005) said No difference Lit review, 933 patients, compared Neostigmine 2. 5 vs 1. 5 mg doses and Robinul vs Atropine (P=0. 08) � Lovstad et al. (2001) said Yes to nausea DB, 90 lap-gyn cases, Mivacurium, Neostigmine 0. 05 mg/kg + Robinul 0. 01 mg/kg. (P=0. 03). First 6 hrs, 30% vs 11% nausea. No difference in vomiting. *(DB=double blind)
METHODOLOGY �Qualitative study �Online survey utilizing Survey. Monkey �Survey distributed via state CRNA organizations �Participants 289 CRNA survey participants Participating states: WA, AZ, NC, MD
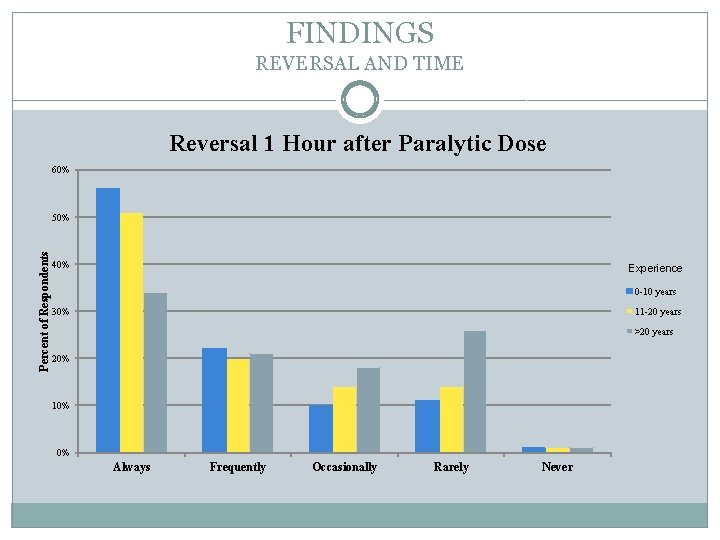
FINDINGS REVERSAL AND TIME Reversal 1 Hour after Paralytic Dose 60% Percent of Respondents 50% 40% Experience 0 -10 years 11 -20 years 30% >20 years 20% 10% 0% Always Frequently Occasionally Rarely Never
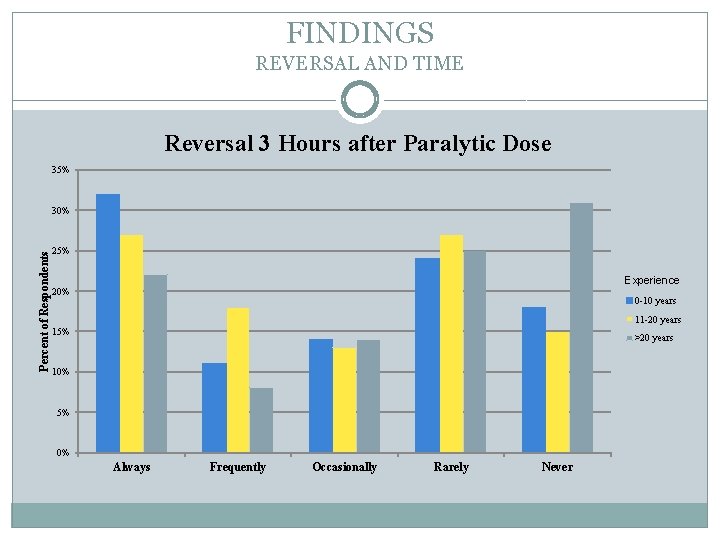
FINDINGS REVERSAL AND TIME Reversal 3 Hours after Paralytic Dose 35% Percent of Respondents 30% 25% Experience 20% 0 -10 years 11 -20 years 15% >20 years 10% 5% 0% Always Frequently Occasionally Rarely Never
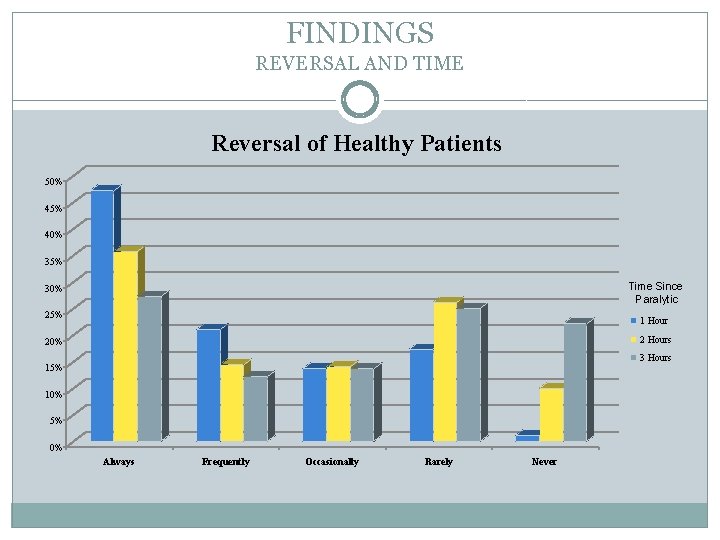
FINDINGS REVERSAL AND TIME Reversal of Healthy Patients 50% 45% 40% 35% Time Since Paralytic 30% 25% 1 Hour 2 Hours 20% 3 Hours 15% 10% 5% 0% Always Frequently Occasionally Rarely Never
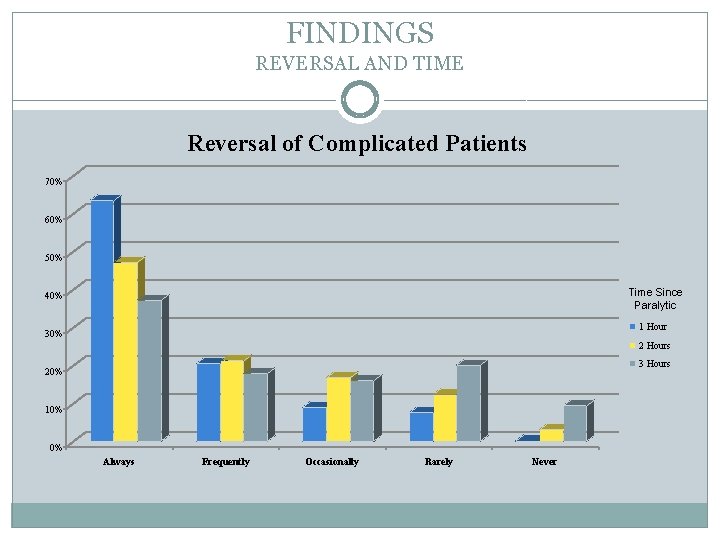
FINDINGS REVERSAL AND TIME Reversal of Complicated Patients 70% 60% 50% Time Since Paralytic 40% 1 Hour 30% 2 Hours 3 Hours 20% 10% 0% Always Frequently Occasionally Rarely Never
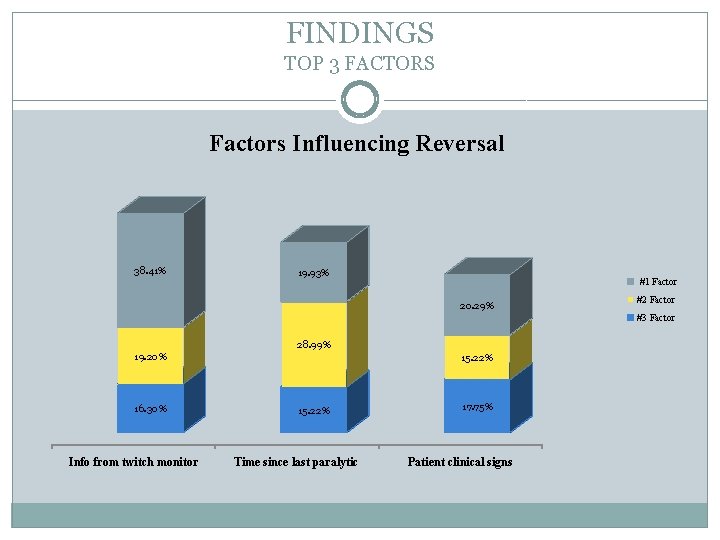
FINDINGS TOP 3 FACTORS Factors Influencing Reversal 38. 41% 19. 93% #1 Factor 20. 29% #2 Factor #3 Factor 28. 99% 19. 20% 16. 30% Info from twitch monitor 15. 22% Time since last paralytic 17. 75% Patient clinical signs
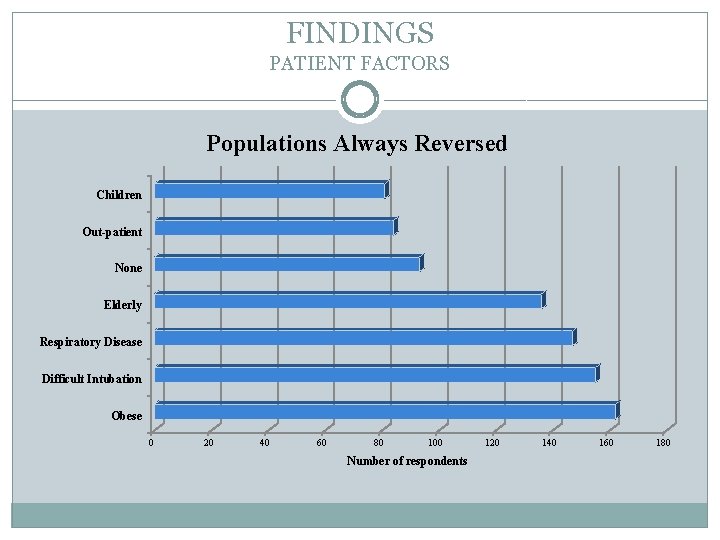
FINDINGS PATIENT FACTORS Populations Always Reversed Children Out-patient None Elderly Respiratory Disease Difficult Intubation Obese 0 20 40 60 80 100 Number of respondents 120 140 160 180
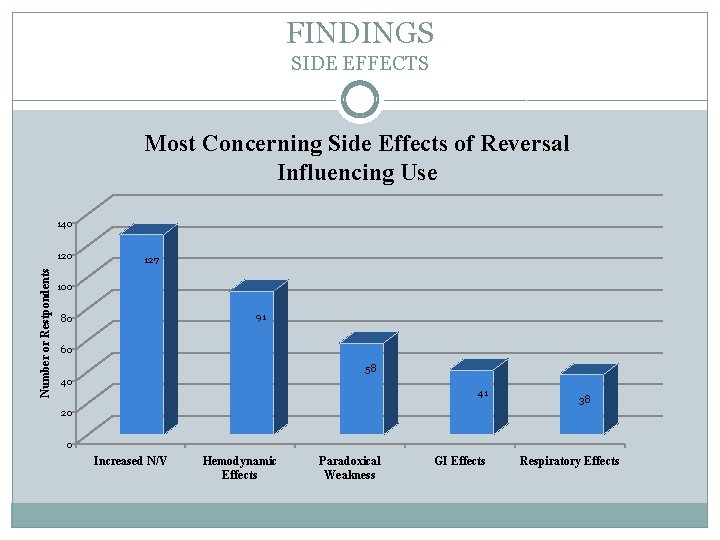
FINDINGS SIDE EFFECTS Most Concerning Side Effects of Reversal Influencing Use 140 Number or Restpondents 120 127 100 91 80 60 58 40 41 38 20 0 Increased N/V Hemodynamic Effects Paradoxical Weakness GI Effects Respiratory Effects
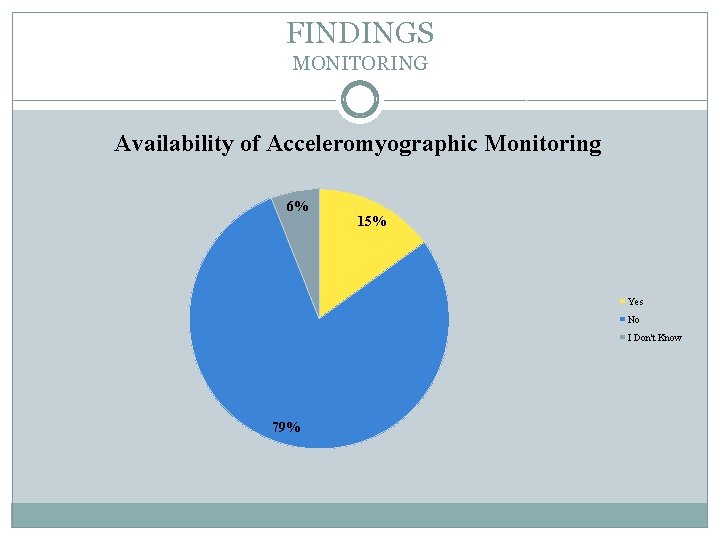
FINDINGS MONITORING Availability of Acceleromyographic Monitoring 6% 15% Yes No I Don't Know 79%
RECOMMENDATIONS �Time from last paralytic dose is not an adequate determinant of residual blockade �Monitoring of blockade should be standard practice Acceleromyography superior as tactile fade lost at TOFR of 0. 4 �Not all patients need a full reversal dose Risk for paradoxical weakness and increased side effects Majority can benefit from a partial reversal dose Increased PONV is inconclusive and appears to be dose-dependent �Faster recovery after reversal with increasing TOF count �Allow 15 -20 minutes after reversal for maximal effect
REFERENCES � Brull, S. J. , & Murphy, G. S. (2010). Residual neuromuscular block: lessons unlearned. Part II: methods to reduce the risk of residual weakness. Anesthesia and Analgesia, 111(1), 129 -140. � Cheng, C. , Sessler, D. I. , & Apfel, C. C. (2005). Does neostigmine administration produce a clinically important increase in postoperative nausea and vomiting? Anesthesia & Analgesia, 101, 1349 -55. � Debaene, B. , Plaud, B. , Dilly, M. , & Donati, F. (2003). Residual paralysis in the PACU after a single intubating dose of nondepolarizing muscle relaxant with an intermediate duration of action. Anesthesiology, 98(5), 1042 -1048. Retrieved from http: //journals. lww. com/anesthesiology/Fulltext/2003/05000/Residual_Paralysis_in_t he_PACU_after_a_Single. 4. aspx � Eriksson, L. I. , Sundman, E. , Olsson, R. , Nilsson, L. , Witt, H. , Ekberg, O. , & Kuylenstierna, R. (1997). Functional assessment of the pharynx at rest and during swallowing in partially paralyzed humans: Simultaneous videomanometry and mechanomyography of awake human volunteers. Anesthesiology, 87(5), 1035 -1043. Retrieved from http: //www. ncbi. nlm. nih. gov/pubmed/9366453 � Fuchs-Buder, T. , Meistelman, C. , Alla, F. , Grandjean, A. , Wuthrich, Y. , & Donati, F. (2010). Antagonism of low degrees of Atracurium-induced neuromuscular blockade. Anesthesiology, 112(1), 34 -40.
REFERENCES � Hovorka, J. , Korttila, K. , Nelskyla, K. , Soikkeli, A. , Sarvela, J. , Paatero, H. , . . . Yli-Hankala, A. (1997). Reversal of neuromuscular blockade with neostigmine has no effect on the incidence or severity of postoperative nausea and vomiting. Anesthesia & Analgesia, 85, 1359 -61. � Joshi, G. P. , Garg, S. A. , Hailey, A. , & Yu, S. Y. (1999). The effects of antagonizing residual neuromuscular blockade by neostigmine and glycopyrrolate on nausea and vomiting after ambulatory surgery. Anesthesia & Analgesia, 89, 628 -31. � Kim, K. , Cheong, M. , Lee, H. , Lee, J. (2004) Tactile assessment for the reversibility of rocuronium induced neuromuscular blockade during propofol or sevoflurane anesthesia. Anesthesia Analgesia, 99, 1080 -1085. � King, M. T. , Milazkiewicz, R. , Carli, F. , & Deacock, A. R. (1988). Influence of neostigmine on postoperative vomiting. British Journal of Anaesthesia, 61, 403 -6. � Kopman, A. F. , & Eikermann, M. (2009). Antagonism of non-depolarising neuromuscular block: current practice. Anaesthesia, 64, 22 -30.
REFERENCES � Lovstad, R. Z. , Thagaard, K. S. , Berner, N. S. , & Raeder, J. C. (2001). Neostigmine 5 mcg/kg with glycopyrrolate increases postoperative nausea in women after laparoscopic gynaecological surgery. Acta Anaesthesiologica, 45, 495 -500. � Murphy, G. S. , Szokol, J. W. , Marymont, J. H. , Greenberg, S. B. , Avram, M. J. , Vender, J. S. , & Nisman, M. (2008). Intraoperative Acceleromyographic Monitoring Reduces the Risk of Residual Neuromuscular Blockade and Adverse Respiratory Events in the Postanesthesia Care Unit. Anesthesiology, 109, 389 -398. � Plaud, B. , Debane, B. , Donati, F. , Marty, J. (2010) Residual paralysis after emergence from anesthesia. Anesthesiology, 112(4), 1013 -1022. � Thilen, S. R. , Hansen, B. E. , Ramaiah, R. , Kent, C. D. , Treggiari, M. M. , & Bhananker, S. M. (2012). Intraoperative neuromuscular monitoring site and residual paralysis. Anesthesiology, 117, 964 -972.
- Slides: 25