Neurology Video Case Presentation William Omar Contreras Lopez


- Slides: 21
Neurology Video Case Presentation • William Omar Contreras Lopez MD • MDS-PAS School for Young Neurologists Atlanta, February 21 -22, 2015
• CC: Progressive abnormal movements • HPI: 19 years-old, Male, with no past medical history. Presenting with 3 weeks of: • Progressive non-rhythmic involuntary horizontal and vertical eyes movements. • Global cerebellar ataxia • Sudden quick jerks of muscle • NO fever, cough, diarrhea, rash, known tick bites, sick contact, recent vaccination, breathing and swallowing were normal. • There was no prior history of infection, medications or drugs intake. Neurological Examination: • He was unable to walk, read, feed himself, speak clearly or maintain visual fixation.
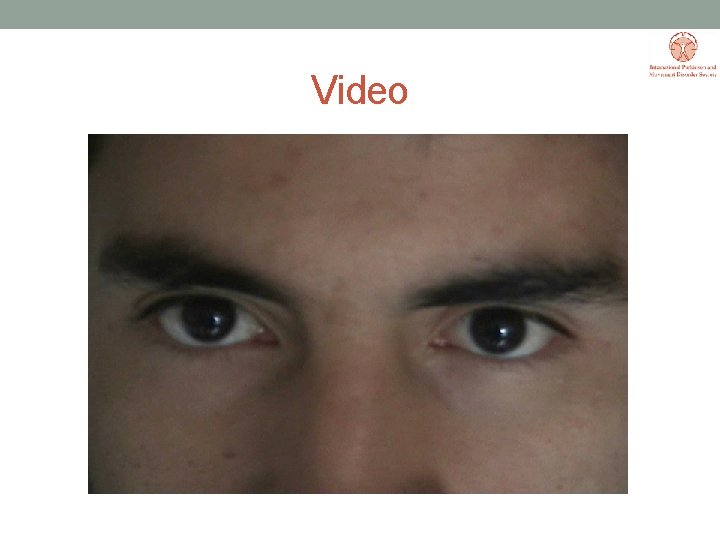
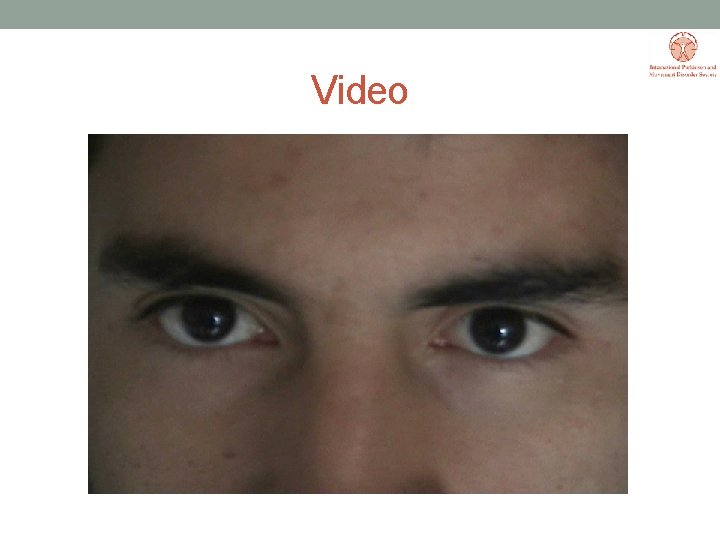
Video
Investigation: - Blood test = Serology Tests, HIV, Whipple, Mycoplasma, Dengue, Syphylis were negative - Brain MRI = Unremarkable - CSF = Normal - Chest and abdominal CT without abnormalities. - Whole body PET-Scan = No changes
Investigation: • Mechanisms: autoimmune? Infeccious? • Metilprednisolone 5 g (1 g/day) – no improvement • After 6 months new screening tests
Follow-up 6 months: • Mediastinal mass 6 months after onset of Symptoms • Biopsy not conclusive reporting a necrosis process • The patient is operated by chest surgery • After total Resection the Pathologie was: Dysgerminoma • The patient received Chemotherapy and after 2 months he was symptoms free
Video
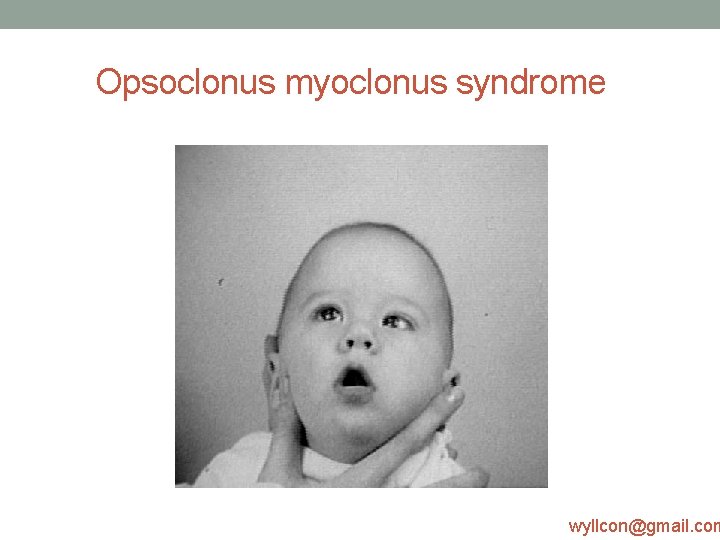
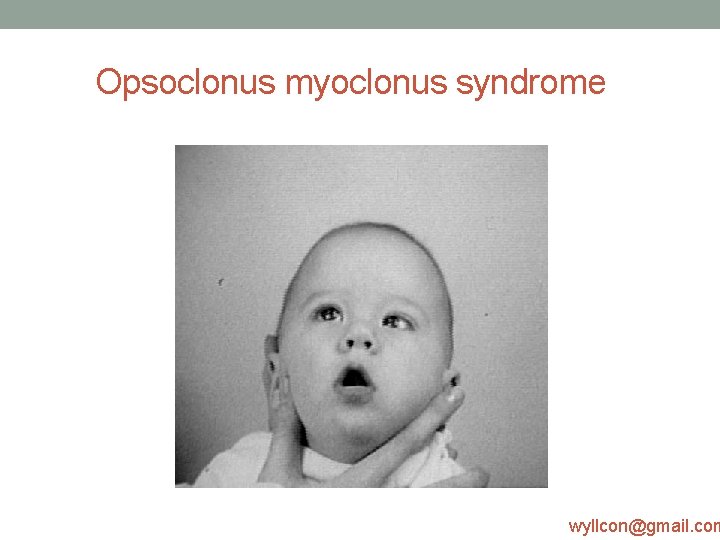
Opsoclonus myoclonus syndrome wyllcon@gmail. com
Opsoclonus myoclonus syndrome • OMS was first described by Marcel Kinsbourne in 1962. • Other names for OMS include: * Opsoclonus-Myoclonus-Ataxia (OMA) * Paraneoplastic Opsoclonus-Myoclonus Ataxia (POMA) * Kinsbourne syndrome * Myoclonic Encephalopathy of Infants * Dancing Eyes-Dancing Feet syndrome * Dancing Eyes syndrome
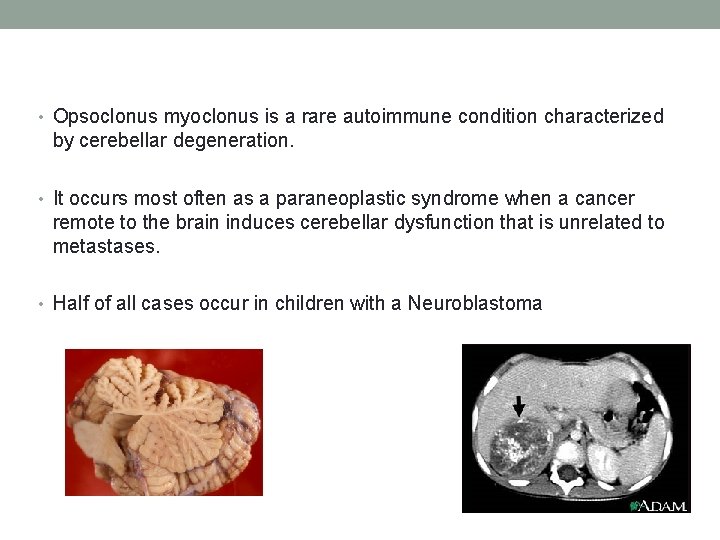
• Opsoclonus myoclonus is a rare autoimmune condition characterized by cerebellar degeneration. • It occurs most often as a paraneoplastic syndrome when a cancer remote to the brain induces cerebellar dysfunction that is unrelated to metastases. • Half of all cases occur in children with a Neuroblastoma
• Most adults with opsoclonus myoclonus have neoplastic, infectious, metabolic, or idiopathic etiologies. • Signs of cerebellar dysfunction noted at presentation include opsoclonus, myoclonus and ataxia, hence the name “dancing eyes, dancing feet syndrome. ” • Opsoclonus is characterized by rapid, involuntary eye movements that are dysrhythmic and uncoordinated.
Symptoms include: • Opsoclonus: rapid, involuntary, multivectorial, unpredictable, conjugate fast eye movements without intersaccadic intervals • Myoclonus: refers to sudden, quick jerks of a muscle or muscle group • • Cerebellar ataxia: Truncal and appendicular Dysphasia Mutism Lethargy Irritability or malaise Drooling Strabismus Vomiting Sleep disturbances
OMS • Neuronal damage is induced by antibodies usually related to the primary pathology. Neoplastic cells produce substances that are toxic to cerebellar neurons. • Treatment targets the etiology and also employs steroids, plasmapheresis, immunosuppressive agents, or other antiinflammatory therapies • Children with opsoclonus myoclonus resulting from a neuroblastoma often retain neurological sequelae. • Adult cases of opsoclonus myoclonus with idiopathic or infectious etiologies have a more favorable prognosis than those with neoplastic origins.
• Cerebellar nuclei are occasional targets of inflammatory injury in many autoimmune reactions and paraneoplastic disorders. • In OM, symptoms develop when intracellular and surface-binding Ig. G 3 antibodies in serum and cerebrospinal fluid (CSF) specifically bind to and damage inhibitory Purkinje cells and granular neurons in the dorsal vermis of the cerebellum. • However, the exact mechanism is not entirely clear, because some cases may remain negative for autoantibodies and exhibit normal Ig. G 3 concentrations. • The antibody types vary widely
• PE can clinically identify OM. • Patients with OM should immediately undergo a complete evaluation for cancer and infection. • Abnormal immunoglobulin analyses and other laboratory findings may be nonspecific since there are no diagnostic biomarkers for paraneoplastic OM. • CSF studies often document paraneoplastic antibodies, mild increases in proteins, and a lymphocytic pleocytosis consistent with inflammatory changes. • Identify the B lymphocytes that produce the offending antibodies.
Opsoclonus myoclonus • The most important treatment is directed at the etiology, providing aggressive intervention for cancer or infection. • Administering immune modulating therapies like steroids, immunoglobulins, adrenocorticotropic hormone, plasmapheresis, or immunosuppressive agents may reduce inflammation. • Rituximab and ofatumumab are two monoclonal B-cell antibodies reported as helpful in children when added to other immunotherapies. • Clonazepam might diminish some of the movement disturbances.

Opsoclonus myoclonus • Children with OM secondary to a neuroblastoma usually retain chronic, disabling developmental dysfunction with cognitive and neurological sequellae. • Chronicity is primarily determined by the severity of the initial pathology, which is proportional to the degree of autoimmune dysfunction. • Other factors in determining prognosis are the age of onset, cancer type and stage, degree and timing of neurological involvement, degree of tumor eradication, treatment effectiveness, and the number of tumor or infectioninduced OM recurrences. • At all ages, the prognosis is more favorable in OM of infectious or idiopathic origins.
Take Home Message • Opsoclonus Myoclonus Syndrome (OMS) is a rare neurological disorder of unknown causes which appears to be the result of an autoimmune process involving the nervous system. • After a diagnosis of OMS is made, an associated neuroblastoma is discovered in half of cases, with median delay of 3 months. • It is, unfortunately, common for misdiagnosis and long delays in diagnosis due to the extreme lack of physician education and awareness of this rare disorder. Early diagnosis and treatment is crucial for inducing a neurological remission. wyllcon@gmail. com
Thank you wyllcon@gmail. com
Adittional information • Because OMS is so rare and occurs at an average of 19 months (6 to 36 months), a diagnosis can be slow. Some cases have been misdiagnosed as having been caused by a virus. After a diagnosis of OMS is made, an associated neuroblastoma is discovered in half of cases, with median delay of 3 months. • About half of all cases are associated with neuroblastoma and most of the others are suspected to be associated with a low-grade neuroblastoma that spontaneously regressed before detection. It is one of the few paraneoplastic (meaning 'indirectly caused by cancer') syndromes that occurs in both children and adults, although the mechanism of immune dysfunction underlying the adult syndrome is probably quite different. • It is hypothesized that a viral infection (perhaps St. Louis encephalitis, Epstein-Barr, Coxsackie B, or enterovirus) causes the remaining cases, though a direct connection has not been proven. • OMS is not generally considered an infectious disease. OMS is not passed on genetically

Treatment • There is no known definitive cure for OMS. However, several drugs have proven to be effective in its treatment. • Some of medication used to treat the symptoms are: • * ACTH has shown improvements in symptoms but can result in an incomplete recovery with • • • residual deficits. * Corticosteroids (such as prednisone or methylprednisolone) used at high dosages (500 mg - 2 g per day intravenously for a course of 3 to 5 days) can accelerate regression of symptoms. Subsequent very gradual tapering with pills generally follows. Most patients require high doses for months to years before tapering. * Intravenous Immunoglobulins (IVIg) are often used with varying results. * Several other immunosuppressive drugs, such as cyclophosphamide and azathioprine, may be helpful in some cases. * Chemotherapy for neuroblastoma may be effective, although data is contradictory and unconvincing at this point in time. * Rituximab has been used with encouraging results. See Immunologic and Clinical Responses to Rituximab in a Child With Opsoclonus-Myoclonus Syndrome Michael R. Pranzatelli, MD, Elizabeth D. Tate, FNP-C, MN, Anna L. Travelstead, BS, MT(ASCP)§ and Darryl Longee, MD • * Other medications are used to treat symptoms without influencing the nature of the disease (symptomatic treatment): • o Trazodone can be useful against irritability and sleep problems • * Additional treatment options include plasmapheresis ("washing the blood", showing similarities to dialysis) for severe, steroid-unresponsive relapses.