Neurology Phase 3 B Ellie Tanqueray Becky Marlor
Neurology Phase 3 B Ellie Tanqueray & Becky Marlor The Peer Teaching Society is not liable for false or misleading information…
Aims: • To revise relevant clinical neuroanatomy • To be able to diagnose neurological conditions and understand their basic management: – – Stroke / TIA Seizures MS Headache The Peer Teaching Society is not liable for false or misleading information…
HEADACHE • RED FLAGS – Thunderclap headache – First and worst headache – Unilateral headache – Headache worse on coughing/in morning/on bending forwards – Persisting headache and scalp tenderness in >50 s – Fever/neck stiffness accompanying headache – Change in pattern of usual headaches – Decreased level of consciousness The Peer Teaching Society is not liable for false or misleading information…
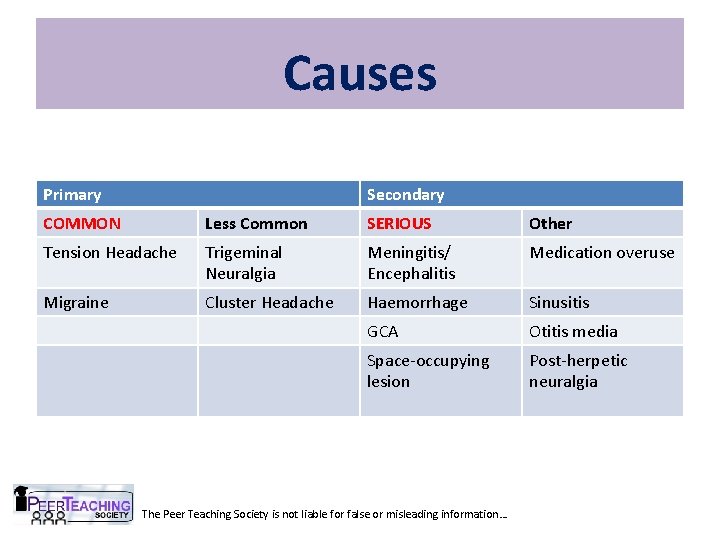
Causes Primary Secondary COMMON Less Common SERIOUS Other Tension Headache Trigeminal Neuralgia Meningitis/ Encephalitis Medication overuse Migraine Cluster Headache Haemorrhage Sinusitis GCA Otitis media Space-occupying lesion Post-herpetic neuralgia The Peer Teaching Society is not liable for false or misleading information…
Tension Headache – TIGHT BAND across forehead – Bilateral – Pressure/tightness – Mild/moderate intensity • Rx: – Reassurance that it is nothing serious – Avoiding triggers – Physical Rx – ice packs, massage, relaxation – NSAIDs first line – ibuprofen, diclofenac – Paracetamol if intolerant to NSAIDs The Peer Teaching Society is not liable for false or misleading information…
Migraine • Thought to be caused by dilatation of intracerebral vessels and oedema • Triggers: CHOCOLATE: CHeese, Oral contraceptives, Caffeine (or its withdrawal), alcoh. OL, Anxiety, Travel, Exercise Triggers found in 50% The Peer Teaching Society is not liable for false or misleading information…
Migraine • Prodrome – hours to days before – Altered mood – depression/euphoria – Irritability – Fatigue – Muscle stiffness • Aura – 5 mins to an hour before headache onset – Transient visual, sensory, motor, speech disturbances – Typically flickering lights, spots, zigzag lines, blind spots The Peer Teaching Society is not liable for false or misleading information…
Migraine • Pain phase – Throbbing/pulsatile headache, usually unilateral – Moderate/severe pain – Worse on movement/physical activity – N&V – Photophobia & Phonophobia • Postdrome – May persist for some days – Sore feeling, impaired thinking – Tiredness, ‘hangover’ feeling The Peer Teaching Society is not liable for false or misleading information…
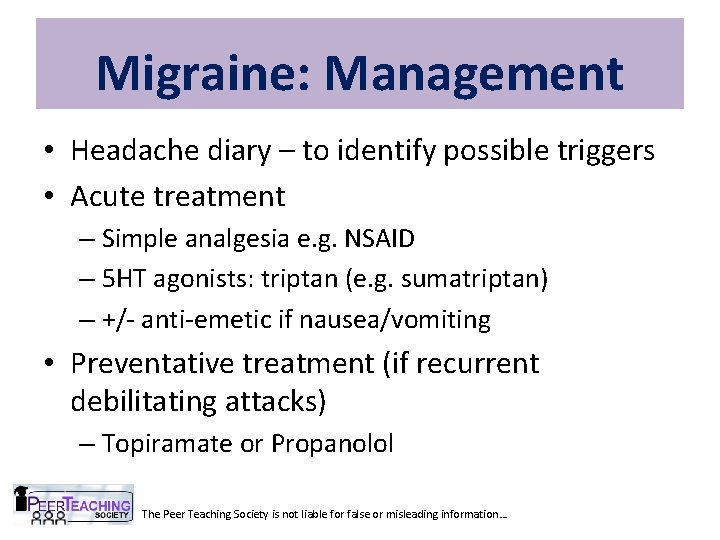
Migraine: Management • Headache diary – to identify possible triggers • Acute treatment – Simple analgesia e. g. NSAID – 5 HT agonists: triptan (e. g. sumatriptan) – +/- anti-emetic if nausea/vomiting • Preventative treatment (if recurrent debilitating attacks) – Topiramate or Propanolol The Peer Teaching Society is not liable for false or misleading information…
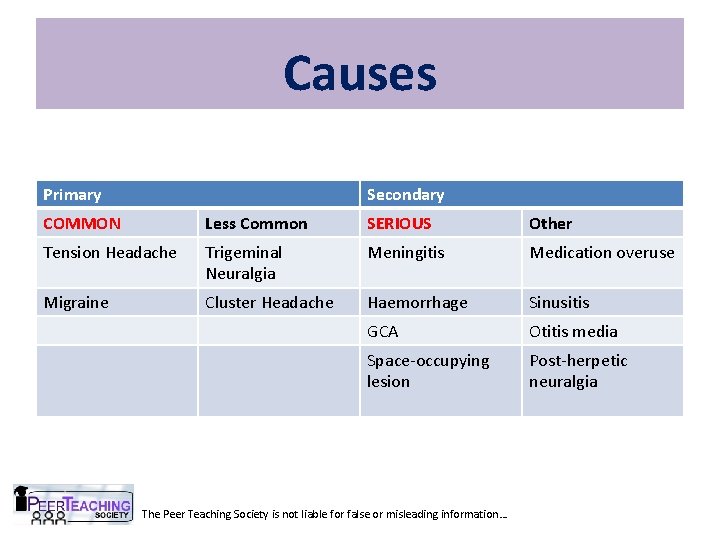
Causes Primary Secondary COMMON Less Common SERIOUS Other Tension Headache Trigeminal Neuralgia Meningitis Medication overuse Migraine Cluster Headache Haemorrhage Sinusitis GCA Otitis media Space-occupying lesion Post-herpetic neuralgia The Peer Teaching Society is not liable for false or misleading information…
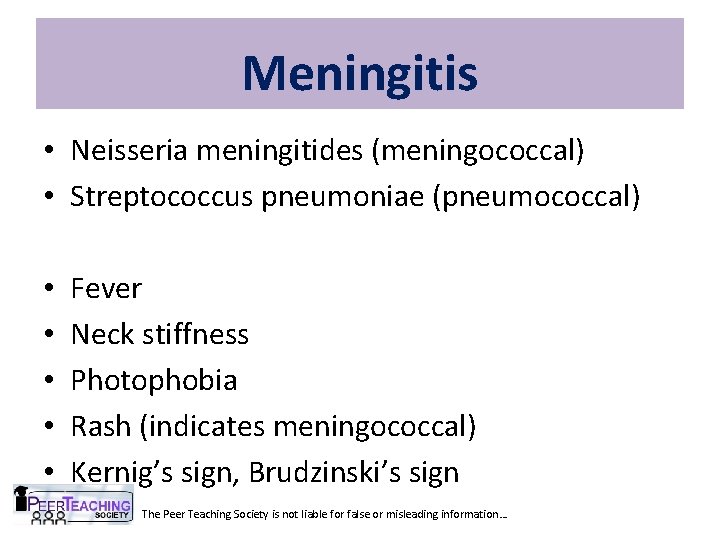
Meningitis • Neisseria meningitides (meningococcal) • Streptococcus pneumoniae (pneumococcal) • • • Fever Neck stiffness Photophobia Rash (indicates meningococcal) Kernig’s sign, Brudzinski’s sign The Peer Teaching Society is not liable for false or misleading information…
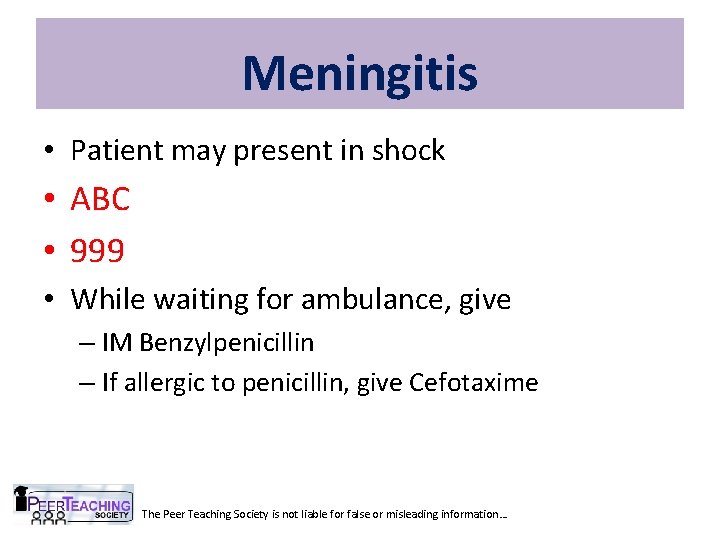
Meningitis • Patient may present in shock • ABC • 999 • While waiting for ambulance, give – IM Benzylpenicillin – If allergic to penicillin, give Cefotaxime The Peer Teaching Society is not liable for false or misleading information…
Meningitis: Investigations • Bloods: FBC, U&E, LFT, CRP, lactate, blood glucose, clotting • Microbiology: blood culture, throat swab • LP – ONLY IF NO ICP • What do we look for on LP? The Peer Teaching Society is not liable for false or misleading information…
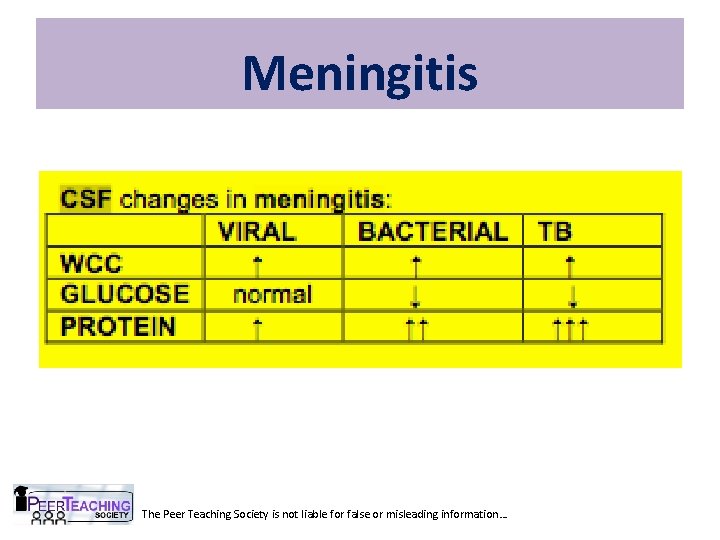
Meningitis The Peer Teaching Society is not liable for false or misleading information…
Meningitis: Management • Antibiotics – IV Cefotaxime/Ceftriaxone • Amend on basis of microbiology results • Dexamethasone – reduces oedema. Must ensure on right Abx first. • Isolate pt for 1 st 24 hrs • Notify HPA • Prophylaxis of household contacts – Rifampicin and meningococcal vaccine The Peer Teaching Society is not liable for false or misleading information…
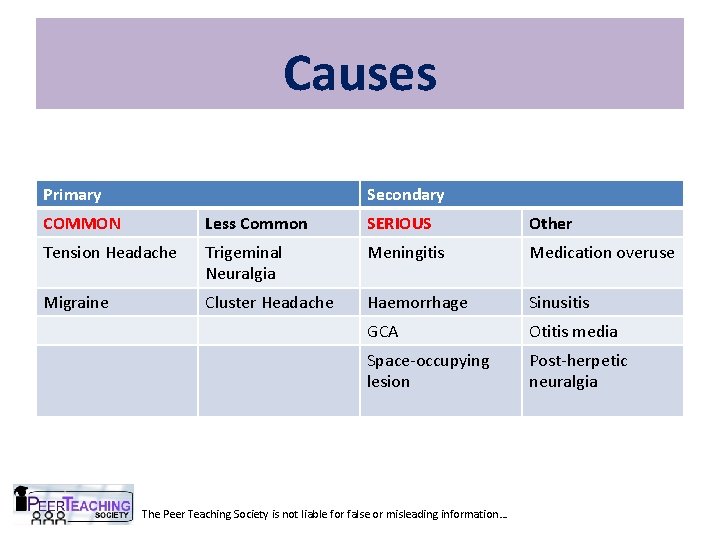
Causes Primary Secondary COMMON Less Common SERIOUS Other Tension Headache Trigeminal Neuralgia Meningitis Medication overuse Migraine Cluster Headache Haemorrhage Sinusitis GCA Otitis media Space-occupying lesion Post-herpetic neuralgia The Peer Teaching Society is not liable for false or misleading information…
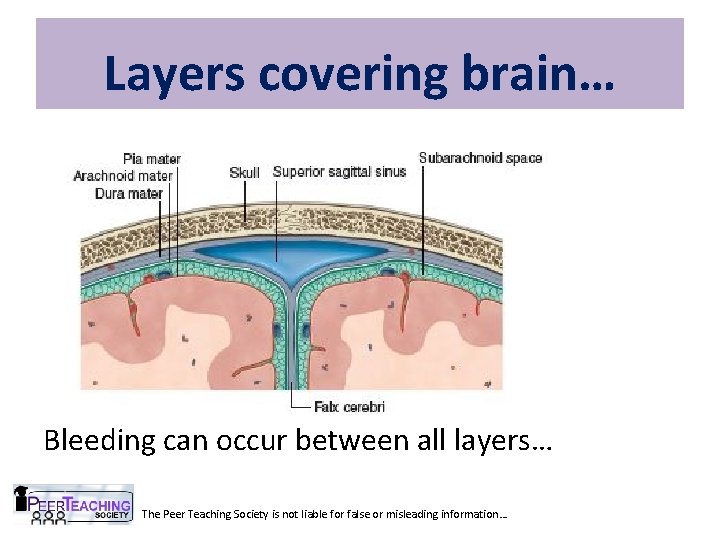
Layers covering brain… Bleeding can occur between all layers… The Peer Teaching Society is not liable for false or misleading information…
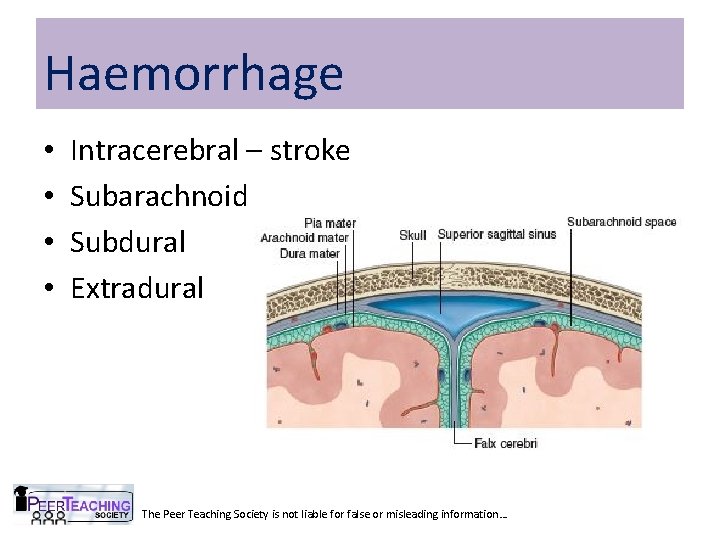
Haemorrhage • • Intracerebral – stroke Subarachnoid Subdural Extradural The Peer Teaching Society is not liable for false or misleading information…
Subarachnoid Haemorrhage • Spontaneous arterial bleeding into subarachnoid space • Causes – Berry aneurysm rupture 85% – Non-aneurysmal haemorrhage 10% – Other 5% due to vascular anomalies e. g. AVM The Peer Teaching Society is not liable for false or misleading information…
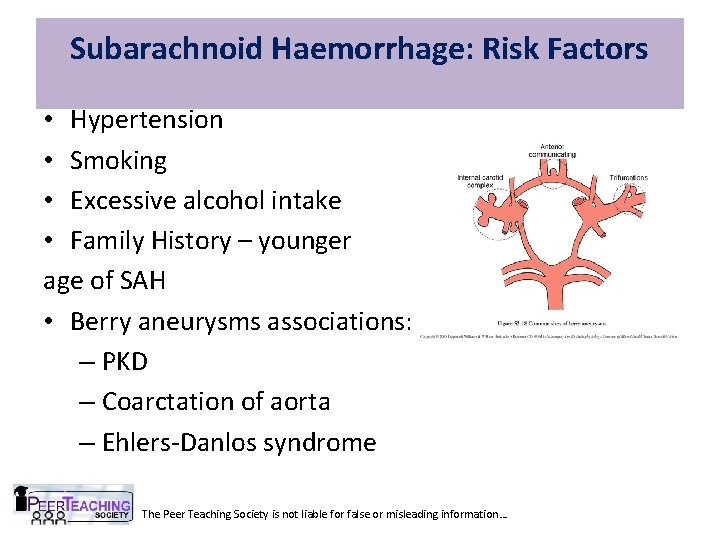
Subarachnoid Haemorrhage: Risk Factors • Hypertension • Smoking • Excessive alcohol intake • Family History – younger age of SAH • Berry aneurysms associations: with: – PKD – Coarctation of aorta – Ehlers-Danlos syndrome The Peer Teaching Society is not liable for false or misleading information…
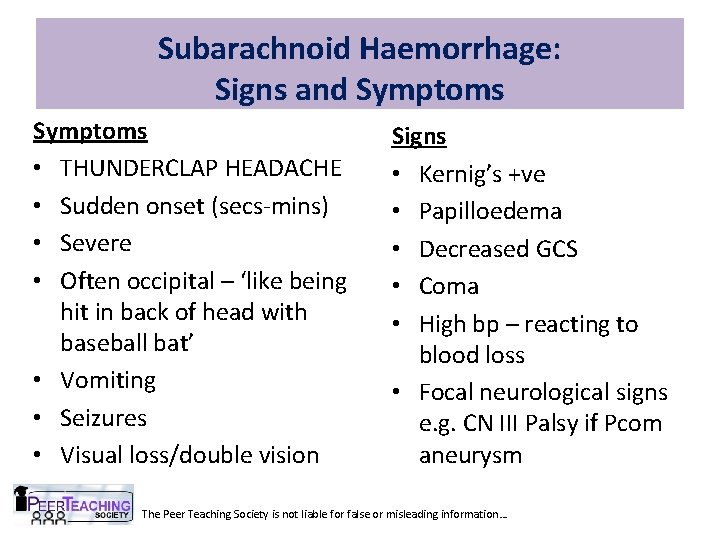
Subarachnoid Haemorrhage: Signs and Symptoms • THUNDERCLAP HEADACHE • Sudden onset (secs-mins) • Severe • Often occipital – ‘like being hit in back of head with baseball bat’ • Vomiting • Seizures • Visual loss/double vision Signs • Kernig’s +ve • Papilloedema • Decreased GCS • Coma • High bp – reacting to blood loss • Focal neurological signs e. g. CN III Palsy if Pcom aneurysm The Peer Teaching Society is not liable for false or misleading information…
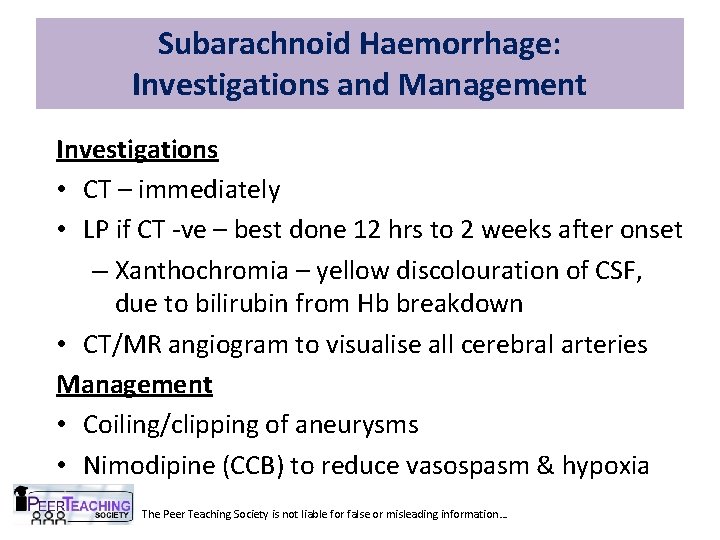
Subarachnoid Haemorrhage: Investigations and Management Investigations • CT – immediately • LP if CT -ve – best done 12 hrs to 2 weeks after onset – Xanthochromia – yellow discolouration of CSF, due to bilirubin from Hb breakdown • CT/MR angiogram to visualise all cerebral arteries Management • Coiling/clipping of aneurysms • Nimodipine (CCB) to reduce vasospasm & hypoxia The Peer Teaching Society is not liable for false or misleading information…
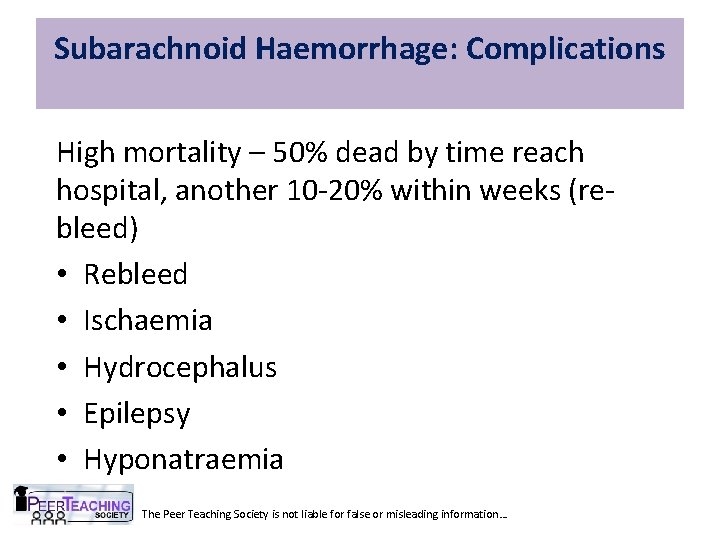
Subarachnoid Haemorrhage: Complications High mortality – 50% dead by time reach hospital, another 10 -20% within weeks (rebleed) • Rebleed • Ischaemia • Hydrocephalus • Epilepsy • Hyponatraemia The Peer Teaching Society is not liable for false or misleading information…
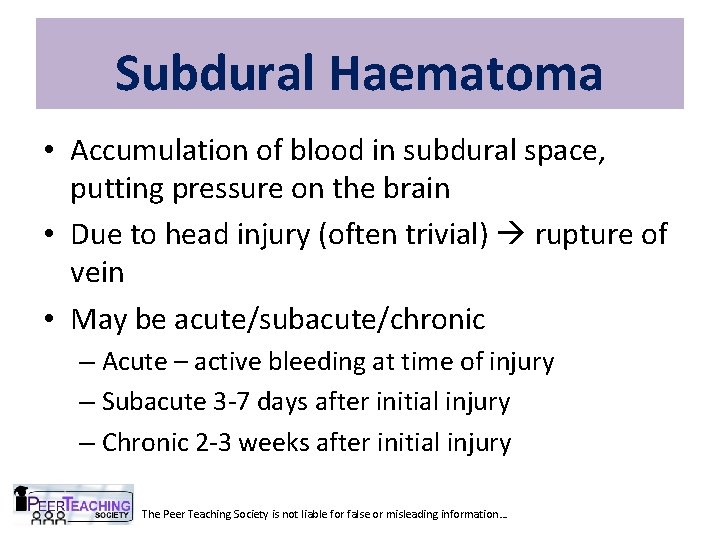
Subdural Haematoma • Accumulation of blood in subdural space, putting pressure on the brain • Due to head injury (often trivial) rupture of vein • May be acute/subacute/chronic – Acute – active bleeding at time of injury – Subacute 3 -7 days after initial injury – Chronic 2 -3 weeks after initial injury The Peer Teaching Society is not liable for false or misleading information…
Subdural Haematoma: Risk Factors • Age – cerebral atrophy tension on veins more easily injured • Alcohol abuse low platelets ↑ risk of fall/head injury cerebral atrophy • Anticoagulants – aspirin, warfarin therapy The Peer Teaching Society is not liable for false or misleading information…
Subdural Haematoma: Acute • Usually presents soon after moderate/severe head injury • +/- loss of consciousness The Peer Teaching Society is not liable for false or misleading information…
Subdural Haematoma: Chronic • Presents 2 -3 weeks after trauma – often trivial injury • Gradually progressive symptoms over days/weeks – Gradually evolving neurological deficit • Limb weakness • Speech difficulty • Drowsiness/confusion • Personality changes – Gradually progressive headache The Peer Teaching Society is not liable for false or misleading information…
Subdural Haematoma: Inv and Management Investigations • CT – crescent-shaped • Blood tests – FBC, U&E, LFTs – Coagulation screen Management - Refer – may need surgery - May resolve spontaneously The Peer Teaching Society is not liable for false or misleading information…
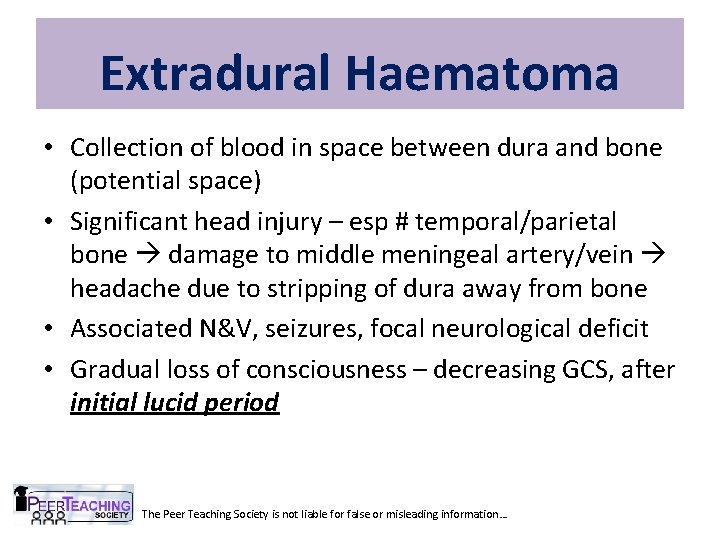
Extradural Haematoma • Collection of blood in space between dura and bone (potential space) • Significant head injury – esp # temporal/parietal bone damage to middle meningeal artery/vein headache due to stripping of dura away from bone • Associated N&V, seizures, focal neurological deficit • Gradual loss of consciousness – decreasing GCS, after initial lucid period The Peer Teaching Society is not liable for false or misleading information…
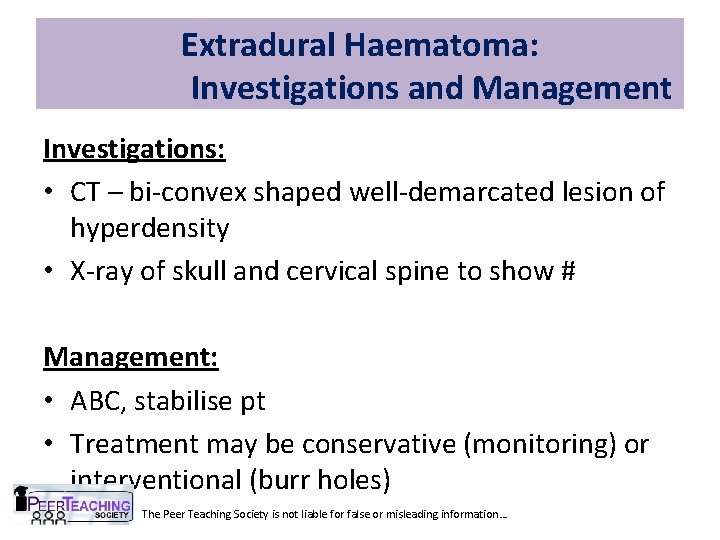
Extradural Haematoma: Investigations and Management Investigations: • CT – bi-convex shaped well-demarcated lesion of hyperdensity • X-ray of skull and cervical spine to show # Management: • ABC, stabilise pt • Treatment may be conservative (monitoring) or interventional (burr holes) The Peer Teaching Society is not liable for false or misleading information…
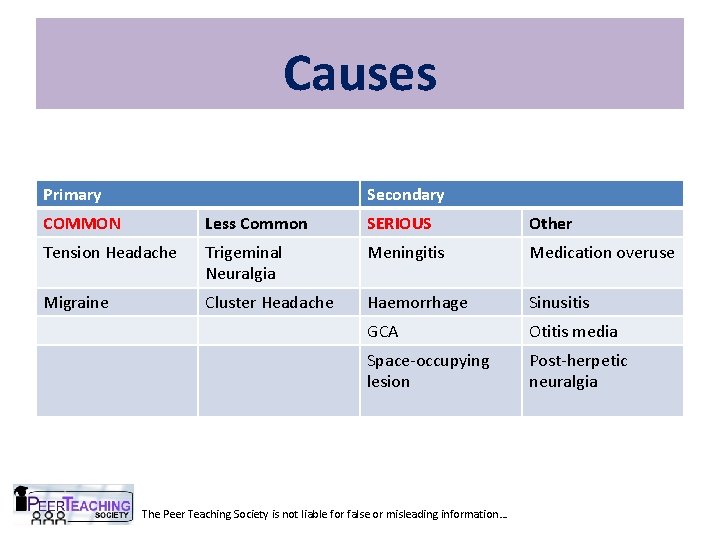
Causes Primary Secondary COMMON Less Common SERIOUS Other Tension Headache Trigeminal Neuralgia Meningitis Medication overuse Migraine Cluster Headache Haemorrhage Sinusitis GCA Otitis media Space-occupying lesion Post-herpetic neuralgia The Peer Teaching Society is not liable for false or misleading information…
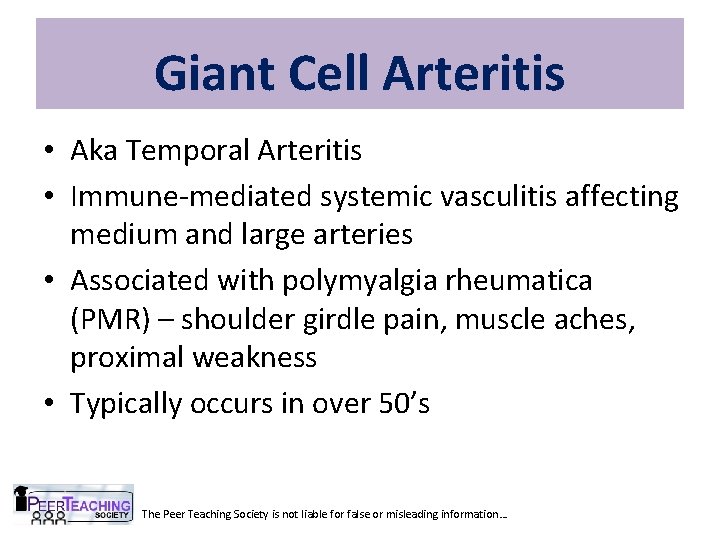
Giant Cell Arteritis • Aka Temporal Arteritis • Immune-mediated systemic vasculitis affecting medium and large arteries • Associated with polymyalgia rheumatica (PMR) – shoulder girdle pain, muscle aches, proximal weakness • Typically occurs in over 50’s The Peer Teaching Society is not liable for false or misleading information…
Giant Cell Arteritis: Presentation Temporal headache Myalgia Fever Malaise Scalp tenderness – pain on combing hair, resting head on pillow • Jaw/tongue claudication – pain on chewing • Visual symptoms e. g. diplopia • • • The Peer Teaching Society is not liable for false or misleading information…
Giant Cell Arteritis: Signs • Scalp tenderness • On palpation of temporal artery: – Absent pulse – Beaded – Tender – Enlarged The Peer Teaching Society is not liable for false or misleading information…
Giant Cell Arteritis: Investigations • FBC – anaemia • ESR – significantly elevated >50 • Temporal artery biopsy: – Mononuclear cell or granulomatous inflammation – Multinucleated giant cells – But negative biopsy doesn’t mean no GCA – SKIP LESIONS The Peer Teaching Society is not liable for false or misleading information…
Giant Cell Arteritis: Treatment • STEROIDS – high dose prednisolone • Low dose aspirin – reduces visual loss and stroke • If long-standing disease, immunosuppressants e. g. methotrexate The Peer Teaching Society is not liable for false or misleading information…
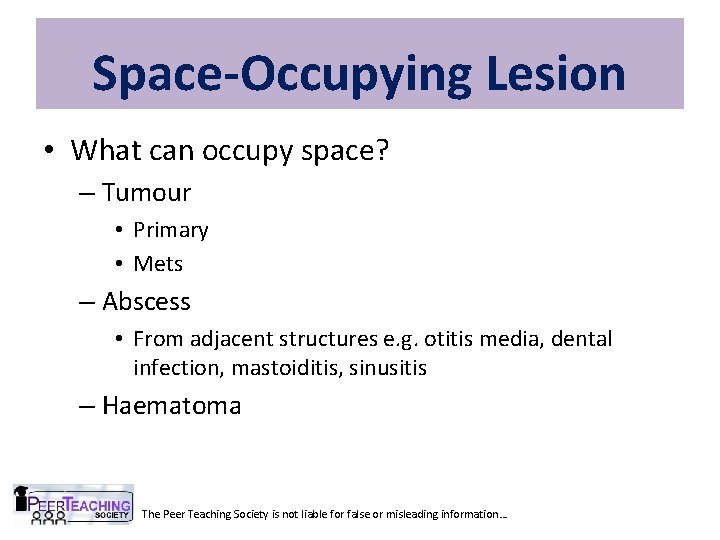
Space-Occupying Lesion • What can occupy space? – Tumour • Primary • Mets – Abscess • From adjacent structures e. g. otitis media, dental infection, mastoiditis, sinusitis – Haematoma The Peer Teaching Society is not liable for false or misleading information…
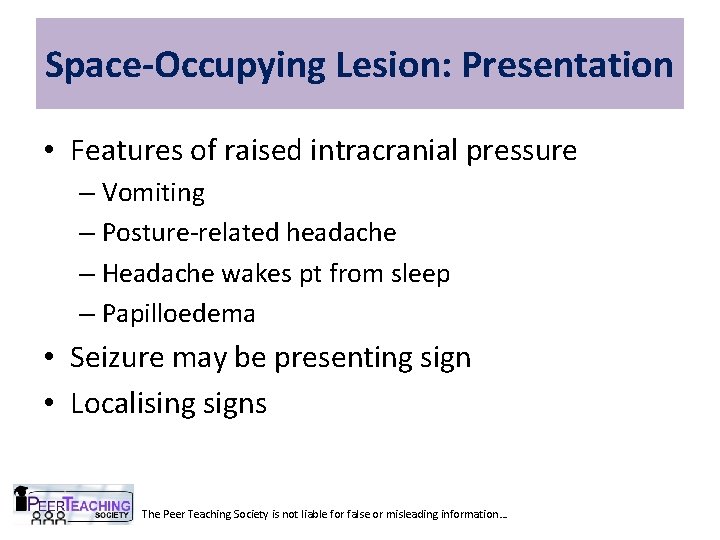
Space-Occupying Lesion: Presentation • Features of raised intracranial pressure – Vomiting – Posture-related headache – Headache wakes pt from sleep – Papilloedema • Seizure may be presenting sign • Localising signs The Peer Teaching Society is not liable for false or misleading information…
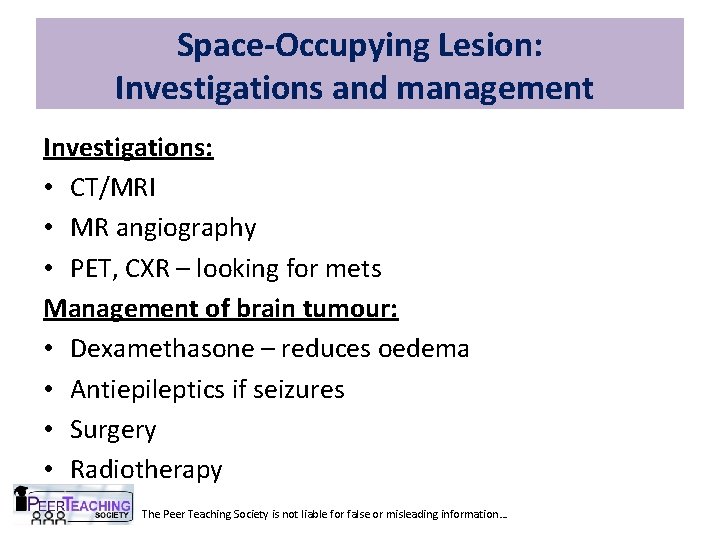
Space-Occupying Lesion: Investigations and management Investigations: • CT/MRI • MR angiography • PET, CXR – looking for mets Management of brain tumour: • Dexamethasone – reduces oedema • Antiepileptics if seizures • Surgery • Radiotherapy The Peer Teaching Society is not liable for false or misleading information…
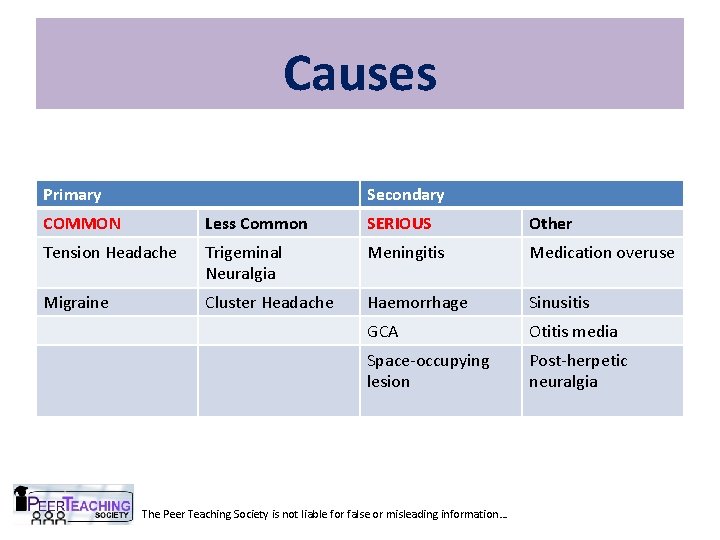
Causes Primary Secondary COMMON Less Common SERIOUS Other Tension Headache Trigeminal Neuralgia Meningitis Medication overuse Migraine Cluster Headache Haemorrhage Sinusitis GCA Otitis media Space-occupying lesion Post-herpetic neuralgia The Peer Teaching Society is not liable for false or misleading information…
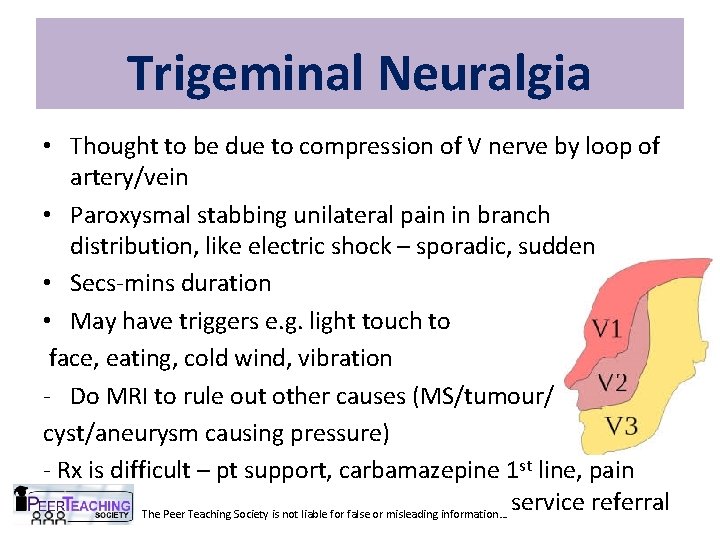
Trigeminal Neuralgia • Thought to be due to compression of V nerve by loop of artery/vein • Paroxysmal stabbing unilateral pain in branch distribution, like electric shock – sporadic, sudden • Secs-mins duration • May have triggers e. g. light touch to face, eating, cold wind, vibration - Do MRI to rule out other causes (MS/tumour/ cyst/aneurysm causing pressure) - Rx is difficult – pt support, carbamazepine 1 st line, pain service referral The Peer Teaching Society is not liable for false or misleading information…
Cluster Headache • Attacks of severe unilateral pain around eye, may wake pt • Associated symptoms: autonomic – Eye watering – Conjunctival redness – Rhinorrhoea • Most common in – Men – Smokers • Clusters (1 -2 attacks daily) last 1 -3 months then remission • Acute Rx: 100% O 2 and sumatriptan. Preventative Rx: The Peer Teaching Society is not liable for false or misleading information… verapamil
Medication Overuse Headache • Frequent headaches • Caused by regular painkillers/triptans for headaches/migraine • Management: – Explain to pt – Stop painkillers worse/more frequent headaches for around 1 week before improvement The Peer Teaching Society is not liable for false or misleading information…
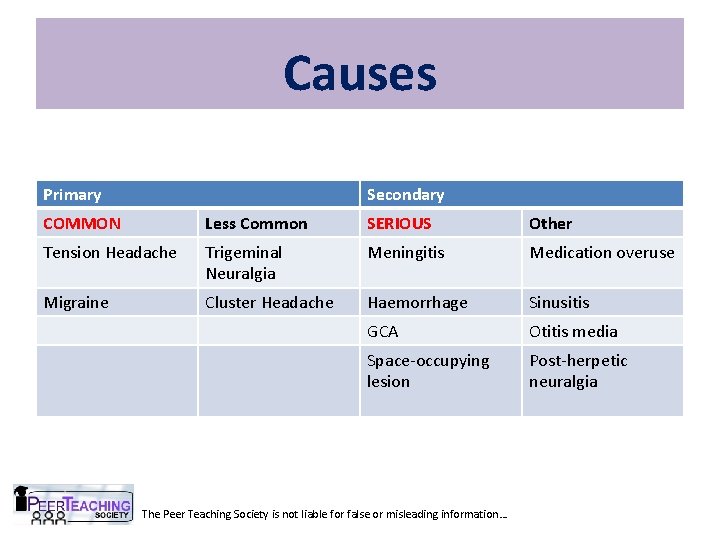
Causes Primary Secondary COMMON Less Common SERIOUS Other Tension Headache Trigeminal Neuralgia Meningitis Medication overuse Migraine Cluster Headache Haemorrhage Sinusitis GCA Otitis media Space-occupying lesion Post-herpetic neuralgia The Peer Teaching Society is not liable for false or misleading information…
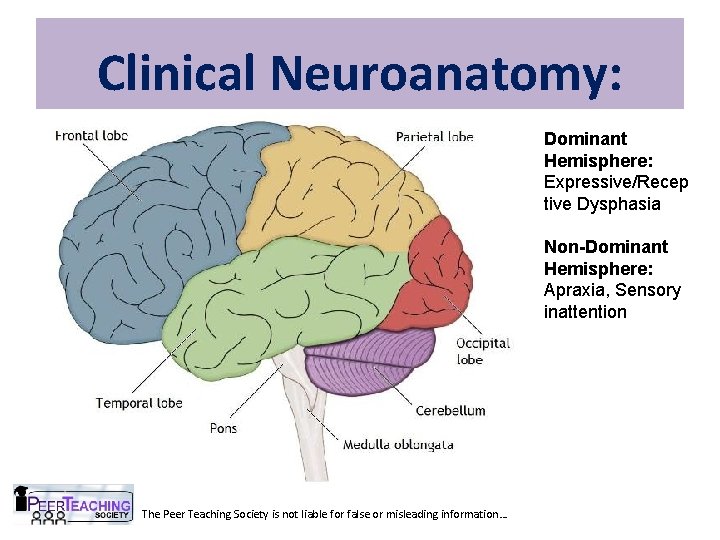
Clinical Neuroanatomy: Dominant Hemisphere: Expressive/Recep tive Dysphasia Non-Dominant Hemisphere: Apraxia, Sensory inattention The Peer Teaching Society is not liable for false or misleading information…
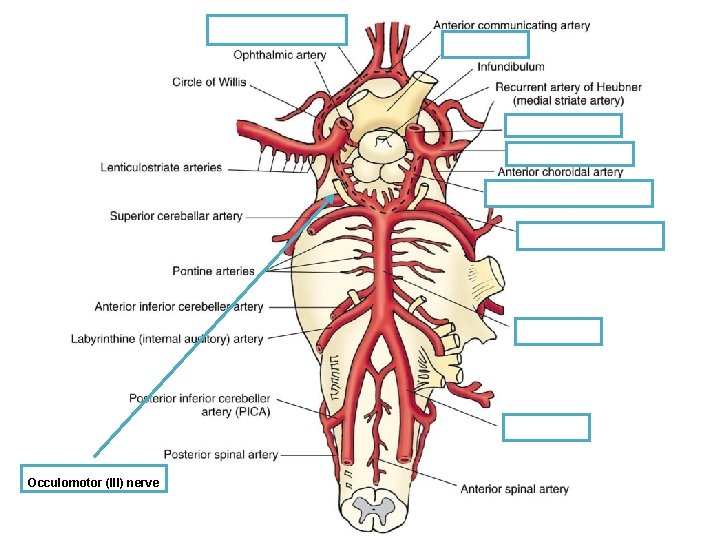
Occulomotor (III) nerve
The Peer Teaching Society is not liable for false or misleading information…
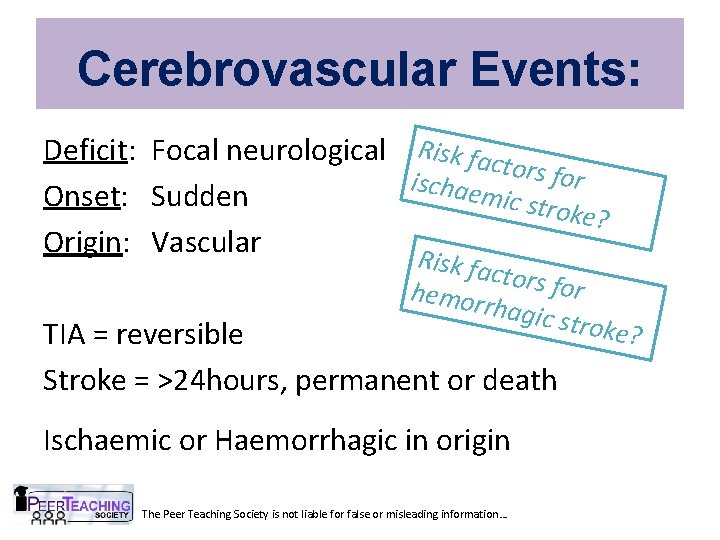
Cerebrovascular Events: Deficit: Focal neurological Risk fact o rs for ischae mic str Onset: Sudden oke? Origin: Vascular R isk fac tors fo r hemor rhagic stroke? TIA = reversible Stroke = >24 hours, permanent or death Ischaemic or Haemorrhagic in origin The Peer Teaching Society is not liable for false or misleading information…
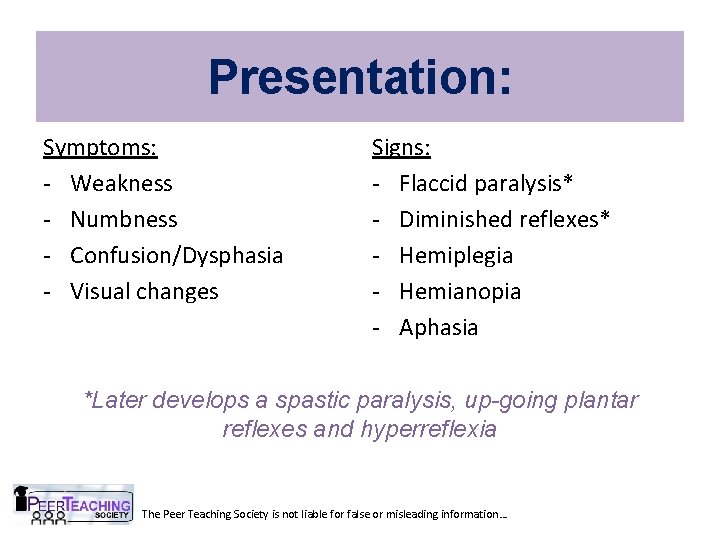
Presentation: Symptoms: - Weakness - Numbness - Confusion/Dysphasia - Visual changes Signs: - Flaccid paralysis* - Diminished reflexes* - Hemiplegia - Hemianopia - Aphasia *Later develops a spastic paralysis, up-going plantar reflexes and hyperreflexia The Peer Teaching Society is not liable for false or misleading information…
DDx Weakness: Cerebral infarction Cerebral haemorrhage Spinal infarction Subdural/Extradural haematoma Epilepsy (Todd’s Paralysis) MS Intracranial lesion – tumour or abscess !! Remember Bells Palsy (Differences? ) The Peer Teaching Society is not liable for false or misleading information…
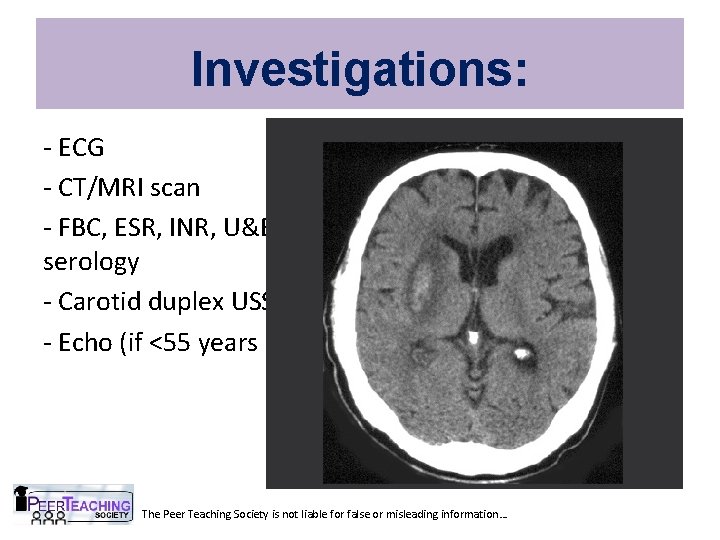
Investigations: - ECG - CT/MRI scan - FBC, ESR, INR, U&E, Glucose, Cholesterol, Syphillis serology - Carotid duplex USS (if anterior circulation) - Echo (if <55 years old or multiple territories) The Peer Teaching Society is not liable for false or misleading information…
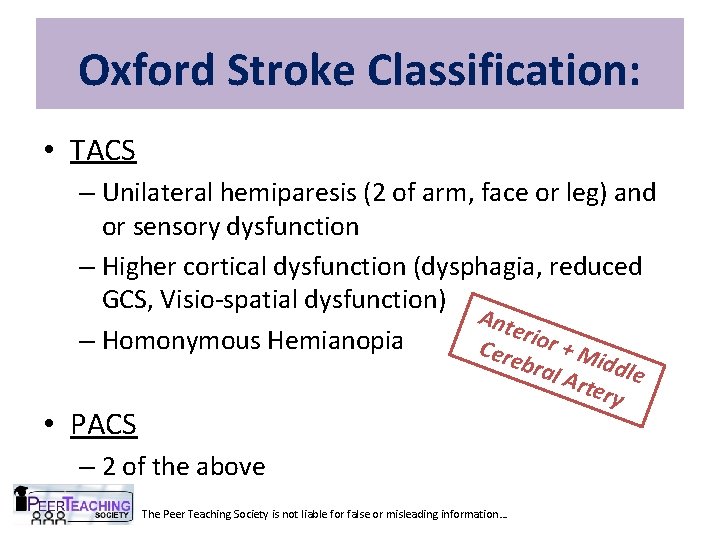
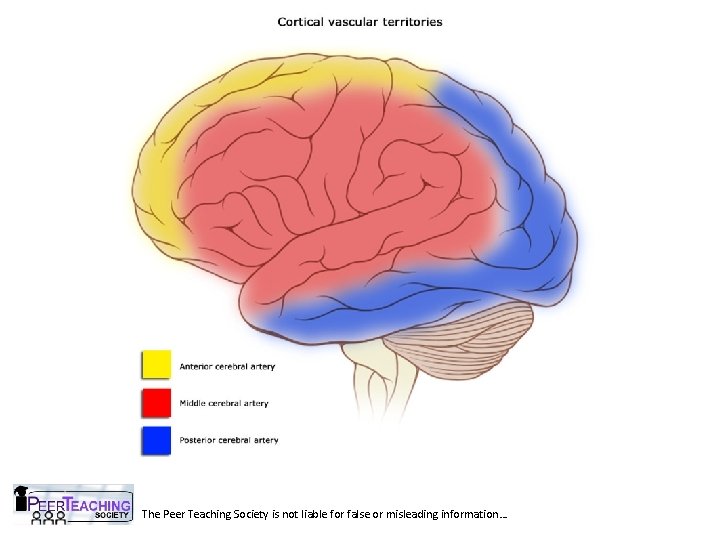
Oxford Stroke Classification: • TACS – Unilateral hemiparesis (2 of arm, face or leg) and or sensory dysfunction – Higher cortical dysfunction (dysphagia, reduced GCS, Visio-spatial dysfunction) Ant erio – Homonymous Hemianopia r+M Cer ebra iddl e l Ar tery • PACS – 2 of the above The Peer Teaching Society is not liable for false or misleading information…
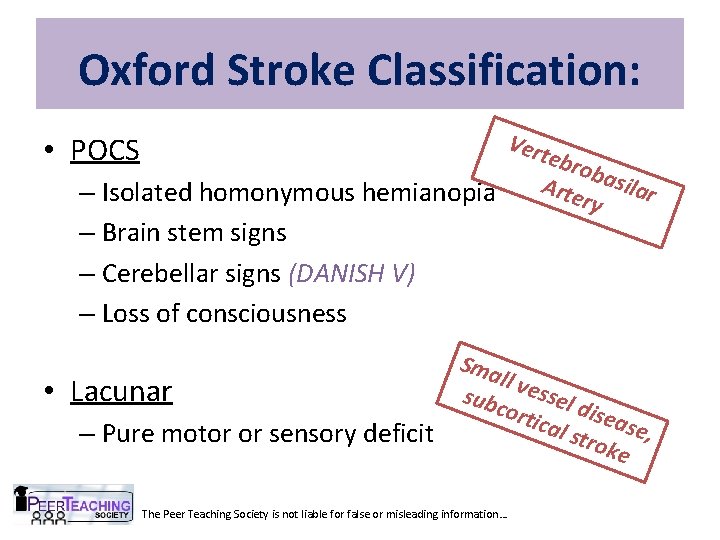
Oxford Stroke Classification: Vert ebro bas ilar Arte – Isolated homonymous hemianopia ry • POCS – Brain stem signs – Cerebellar signs (DANISH V) – Loss of consciousness • Lacunar – Pure motor or sensory deficit Sma ll ve ssel sub cort d ical isease , stro ke The Peer Teaching Society is not liable for false or misleading information…
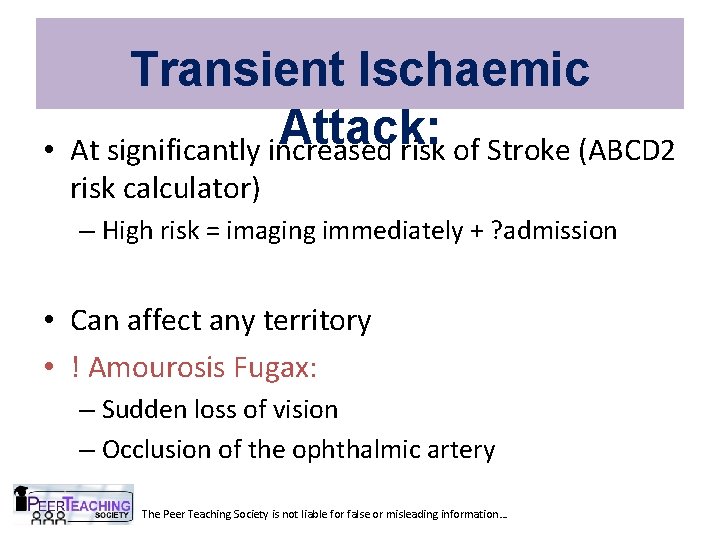
• Transient Ischaemic Attack: At significantly increased risk of Stroke (ABCD 2 risk calculator) – High risk = imaging immediately + ? admission • Can affect any territory • ! Amourosis Fugax: – Sudden loss of vision – Occlusion of the ophthalmic artery The Peer Teaching Society is not liable for false or misleading information…
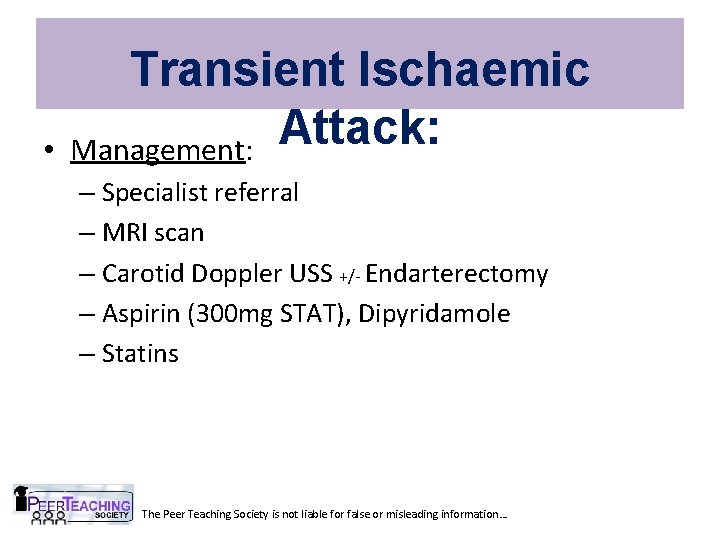
• Transient Ischaemic Attack: Management: – Specialist referral – MRI scan – Carotid Doppler USS +/- Endarterectomy – Aspirin (300 mg STAT), Dipyridamole – Statins The Peer Teaching Society is not liable for false or misleading information…
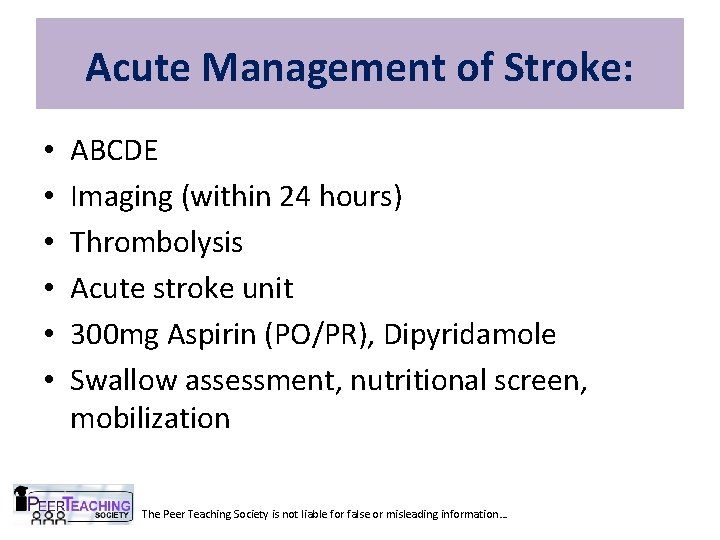
Acute Management of Stroke: • • • ABCDE Imaging (within 24 hours) Thrombolysis Acute stroke unit 300 mg Aspirin (PO/PR), Dipyridamole Swallow assessment, nutritional screen, mobilization The Peer Teaching Society is not liable for false or misleading information…
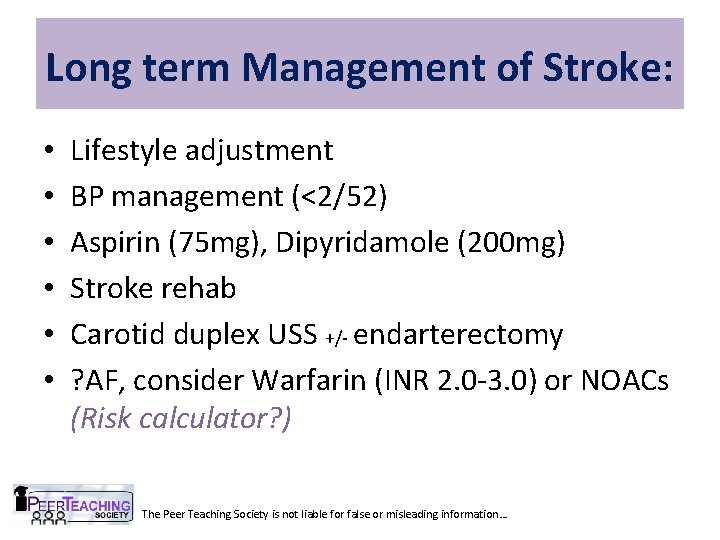
Long term Management of Stroke: • • • Lifestyle adjustment BP management (<2/52) Aspirin (75 mg), Dipyridamole (200 mg) Stroke rehab Carotid duplex USS +/- endarterectomy ? AF, consider Warfarin (INR 2. 0 -3. 0) or NOACs (Risk calculator? ) The Peer Teaching Society is not liable for false or misleading information…
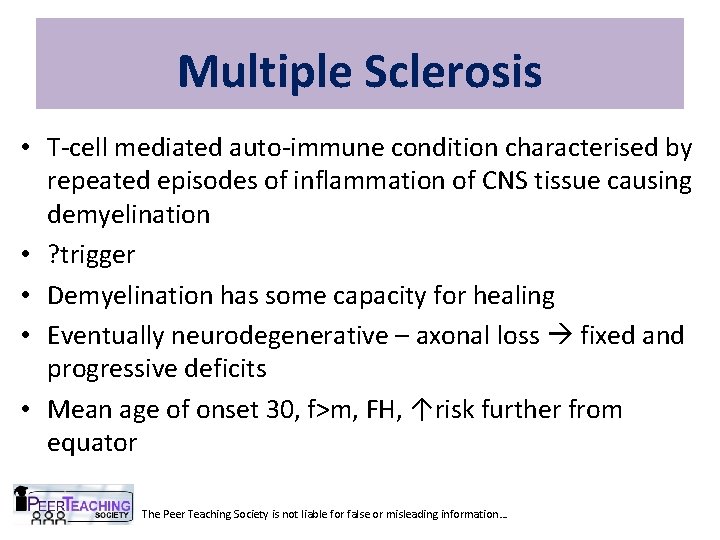
Multiple Sclerosis • T-cell mediated auto-immune condition characterised by repeated episodes of inflammation of CNS tissue causing demyelination • ? trigger • Demyelination has some capacity for healing • Eventually neurodegenerative – axonal loss fixed and progressive deficits • Mean age of onset 30, f>m, FH, ↑risk further from equator The Peer Teaching Society is not liable for false or misleading information…
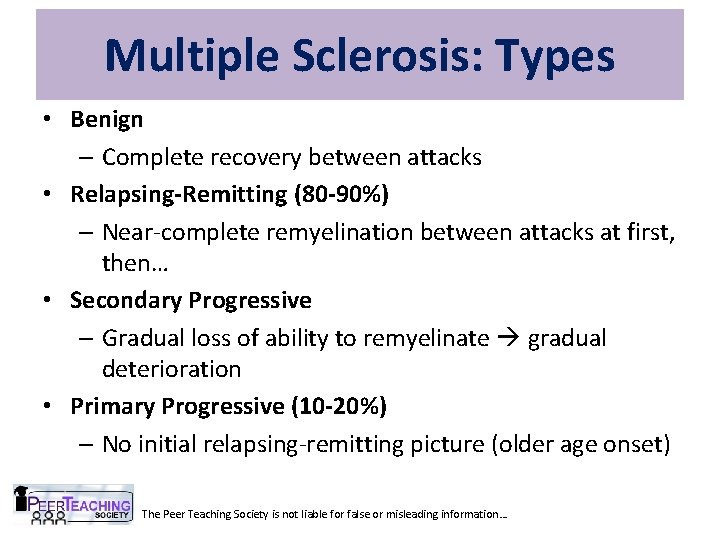
Multiple Sclerosis: Types • Benign – Complete recovery between attacks • Relapsing-Remitting (80 -90%) – Near-complete remyelination between attacks at first, then… • Secondary Progressive – Gradual loss of ability to remyelinate gradual deterioration • Primary Progressive (10 -20%) – No initial relapsing-remitting picture (older age onset) The Peer Teaching Society is not liable for false or misleading information…
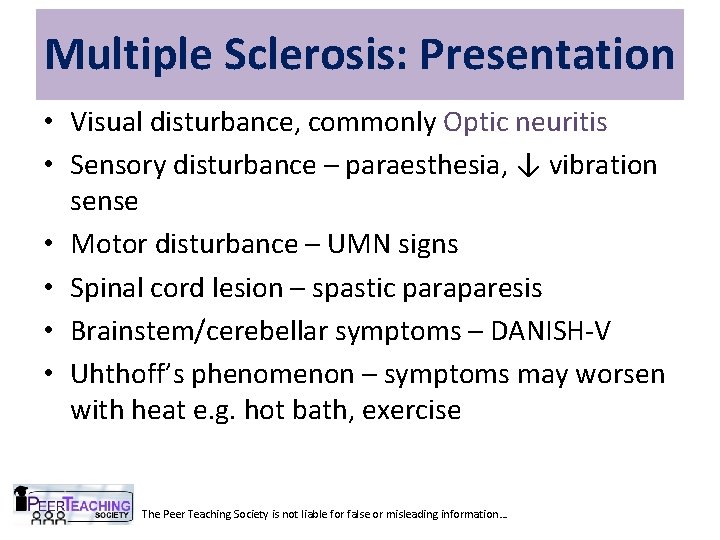
Multiple Sclerosis: Presentation • Visual disturbance, commonly Optic neuritis • Sensory disturbance – paraesthesia, ↓ vibration sense • Motor disturbance – UMN signs • Spinal cord lesion – spastic paraparesis • Brainstem/cerebellar symptoms – DANISH-V • Uhthoff’s phenomenon – symptoms may worsen with heat e. g. hot bath, exercise The Peer Teaching Society is not liable for false or misleading information…
Optic Neuritis • Inflammation of optic nerve • Many causes – MS – demyelination – Important to rule out other causes e. g. ischaemia (GCA), DM, infection, drug-induced • Triad of features: – Reduced vision – Eye pain – worse on movement – Impaired colour vision – dyschromatopsia • RAPD – Marcus Gunn pupil The Peer Teaching Society is not liable for false or misleading information…
Multiple Sclerosis: Diagnosis • Clinical diagnosis with evidence to support • MRI brain and spinal cord – plaques of demyelination – periventricular lesions most common • Disseminated in time and space • VEP – delayed in optic neuropathy • LP – oligoclonal Ig. G bands in CSF but not serum (ie compare serum with CSF) The Peer Teaching Society is not liable for false or misleading information…
Multiple Sclerosis: Treatment • Of acute episodes – aim to shorten relapse – IV methylprednisolone 3 -5 days – Then oral for 3 weeks, gradually reducing dose • If >2 relapses in 2 yrs – immunomodulation – Interferon (1α, 1β) – decreases relapse frequency – Monoclonal antibodies e. g. natalizumab – or immunosuppression e. g. azathioprine • Treat symptoms – next slide The Peer Teaching Society is not liable for false or misleading information…
Multiple Sclerosis: Treatment of symptoms • Muscle spasticity – baclofen, diazepam • Urgency/frequency – intermittent selfcatheterisation if large residual volume, oxybutynin for detrusor instability • Bowels – lactulose for constipation, or loperamide to reduce bowel motility • Pain – analgesics – pain ladder • Treat infection/trauma promptly – may worsen MS The Peer Teaching Society is not liable for false or misleading information…
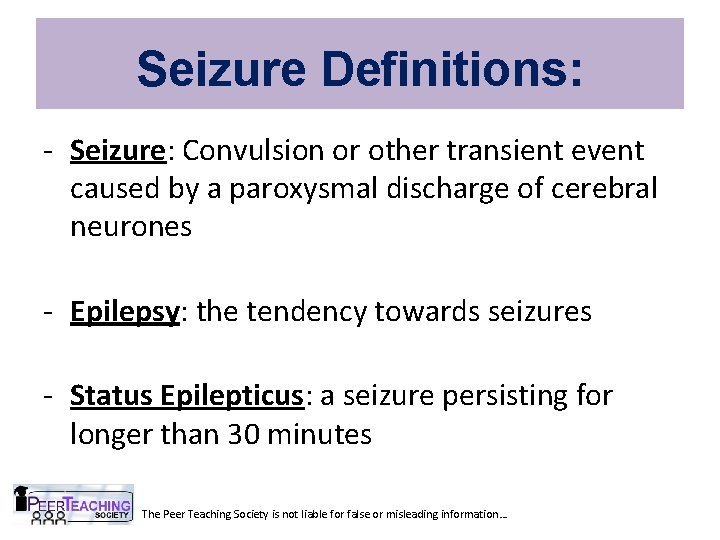
Seizure Definitions: - Seizure: Convulsion or other transient event caused by a paroxysmal discharge of cerebral neurones - Epilepsy: the tendency towards seizures - Status Epilepticus: a seizure persisting for longer than 30 minutes The Peer Teaching Society is not liable for false or misleading information…
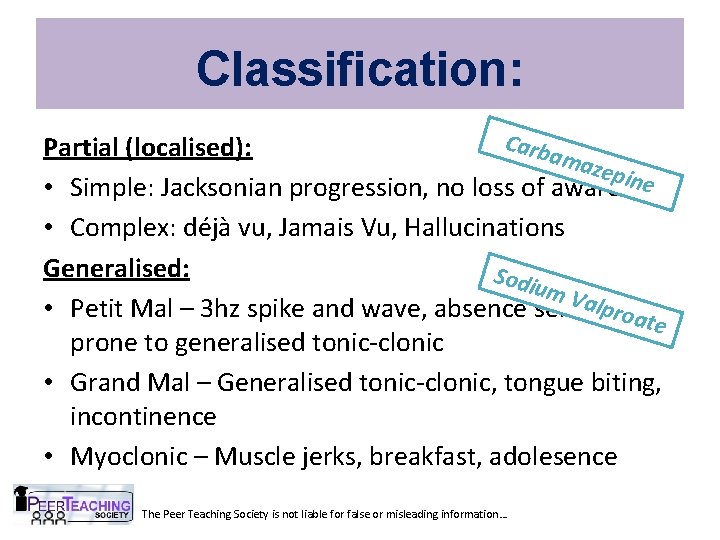
Classification: Carb Partial (localised): ama zepin e • Simple: Jacksonian progression, no loss of awareness • Complex: déjà vu, Jamais Vu, Hallucinations Generalised: Sodi um V alpro • Petit Mal – 3 hz spike and wave, absence seizures, ate prone to generalised tonic-clonic • Grand Mal – Generalised tonic-clonic, tongue biting, incontinence • Myoclonic – Muscle jerks, breakfast, adolesence The Peer Teaching Society is not liable for false or misleading information…
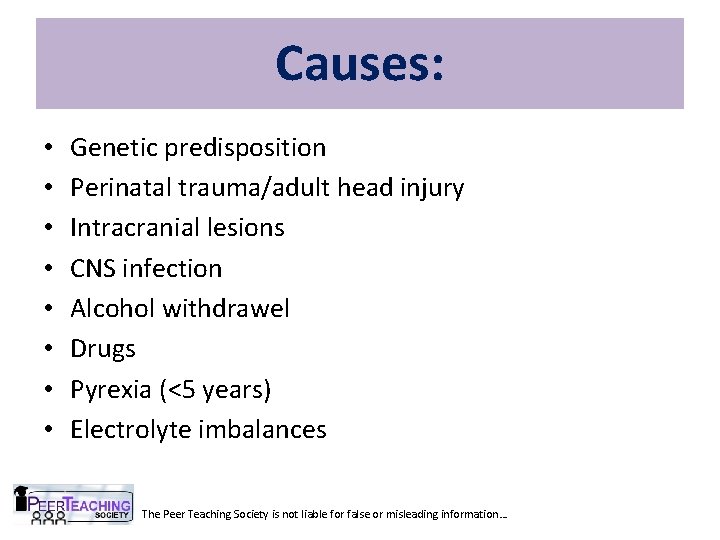
Causes: • • Genetic predisposition Perinatal trauma/adult head injury Intracranial lesions CNS infection Alcohol withdrawel Drugs Pyrexia (<5 years) Electrolyte imbalances The Peer Teaching Society is not liable for false or misleading information…
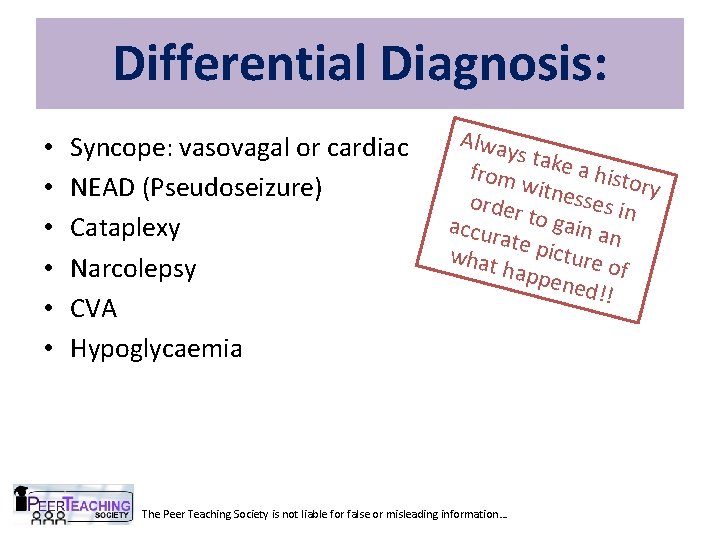
Differential Diagnosis: • • • Syncope: vasovagal or cardiac NEAD (Pseudoseizure) Cataplexy Narcolepsy CVA Hypoglycaemia Alwa ys tak e a hi from story witne sses i order n t o g a accur ate p in an icture what of happ ened !! The Peer Teaching Society is not liable for false or misleading information…
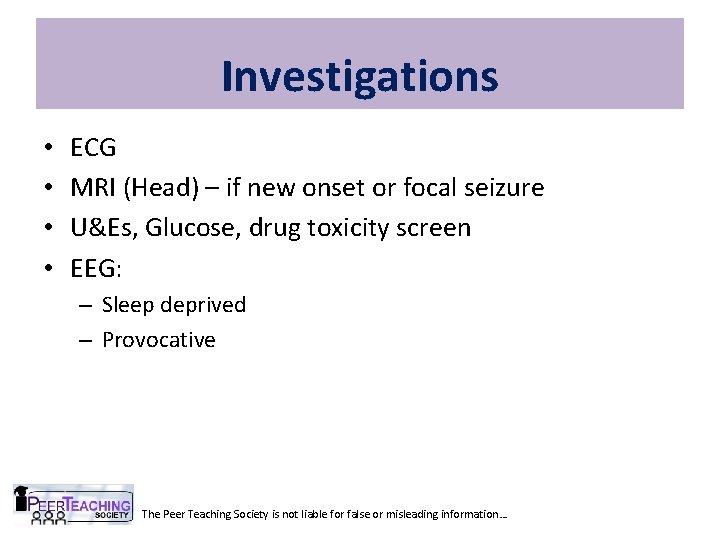
Investigations • • ECG MRI (Head) – if new onset or focal seizure U&Es, Glucose, drug toxicity screen EEG: – Sleep deprived – Provocative The Peer Teaching Society is not liable for false or misleading information…
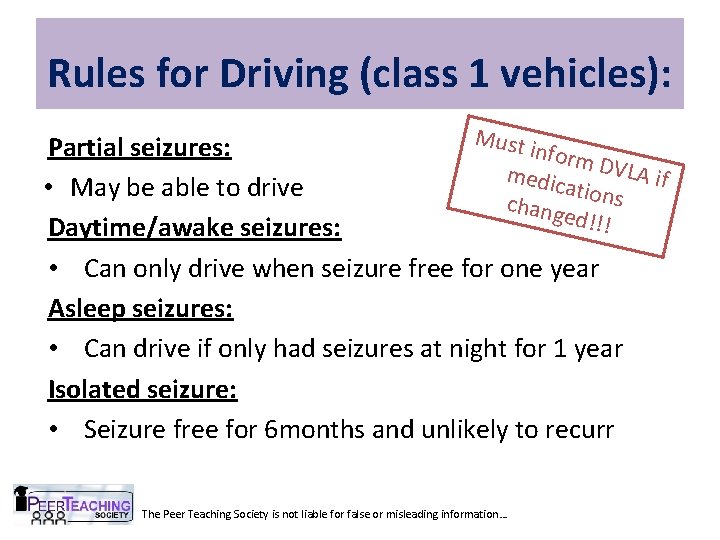
Rules for Driving (class 1 vehicles): Must Partial seizures: inform medic DVLA if ations • May be able to drive chang ed!!! Daytime/awake seizures: • Can only drive when seizure free for one year Asleep seizures: • Can drive if only had seizures at night for 1 year Isolated seizure: • Seizure free for 6 months and unlikely to recurr The Peer Teaching Society is not liable for false or misleading information…
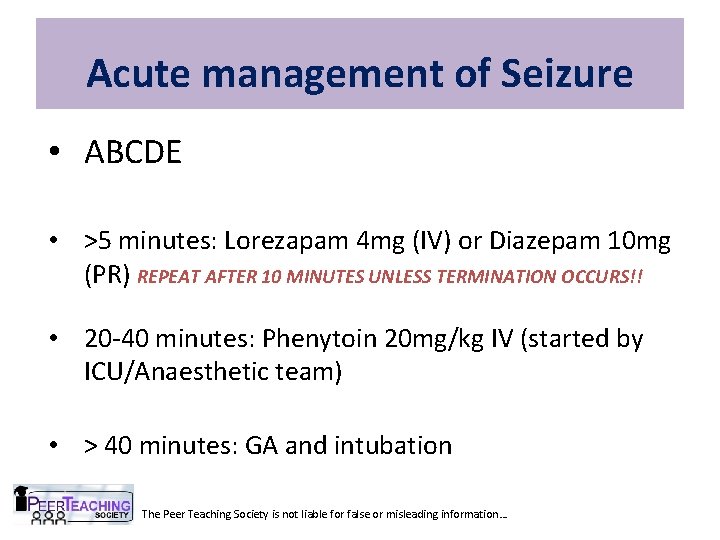
Acute management of Seizure • ABCDE • >5 minutes: Lorezapam 4 mg (IV) or Diazepam 10 mg (PR) REPEAT AFTER 10 MINUTES UNLESS TERMINATION OCCURS!! • 20 -40 minutes: Phenytoin 20 mg/kg IV (started by ICU/Anaesthetic team) • > 40 minutes: GA and intubation The Peer Teaching Society is not liable for false or misleading information…
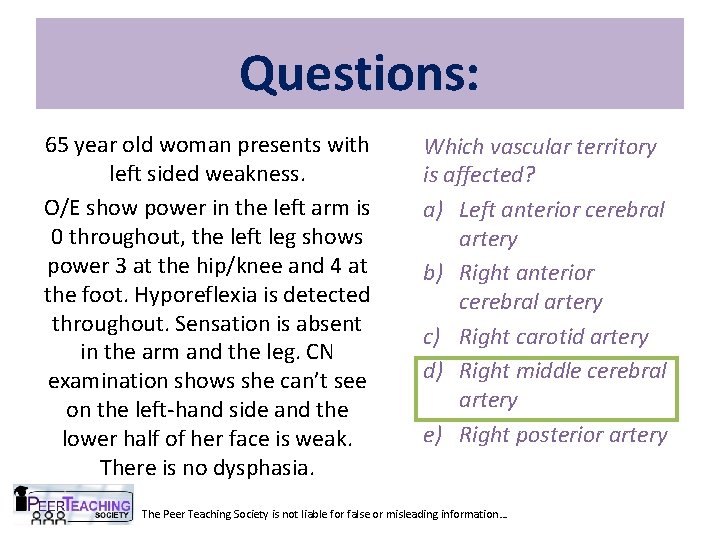
Questions: 65 year old woman presents with left sided weakness. O/E show power in the left arm is 0 throughout, the left leg shows power 3 at the hip/knee and 4 at the foot. Hyporeflexia is detected throughout. Sensation is absent in the arm and the leg. CN examination shows she can’t see on the left-hand side and the lower half of her face is weak. There is no dysphasia. Which vascular territory is affected? a) Left anterior cerebral artery b) Right anterior cerebral artery c) Right carotid artery d) Right middle cerebral artery e) Right posterior artery The Peer Teaching Society is not liable for false or misleading information…
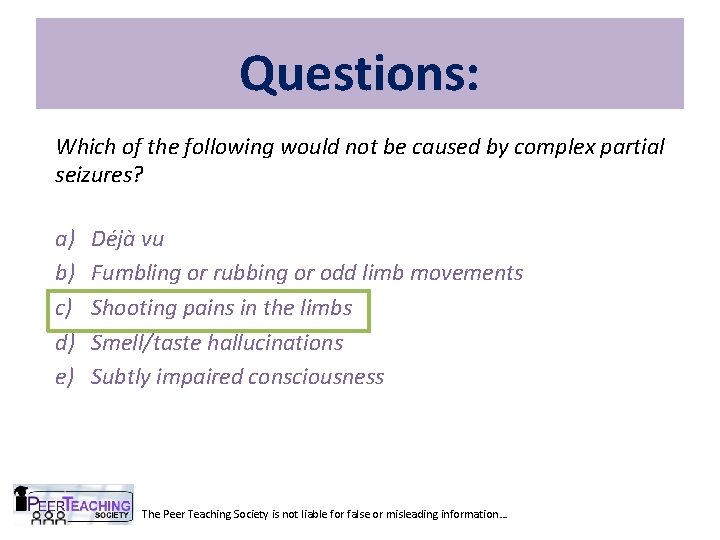
Questions: Which of the following would not be caused by complex partial seizures? a) b) c) d) e) Déjà vu Fumbling or rubbing or odd limb movements Shooting pains in the limbs Smell/taste hallucinations Subtly impaired consciousness The Peer Teaching Society is not liable for false or misleading information…
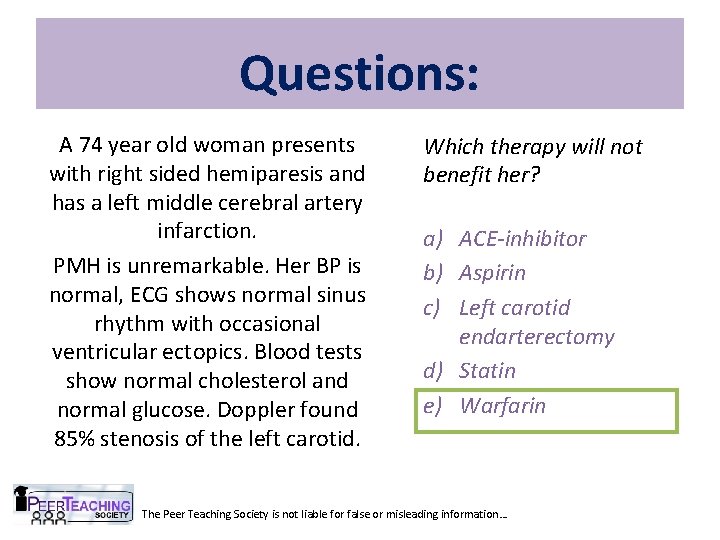
Questions: A 74 year old woman presents with right sided hemiparesis and has a left middle cerebral artery infarction. PMH is unremarkable. Her BP is normal, ECG shows normal sinus rhythm with occasional ventricular ectopics. Blood tests show normal cholesterol and normal glucose. Doppler found 85% stenosis of the left carotid. Which therapy will not benefit her? a) ACE-inhibitor b) Aspirin c) Left carotid endarterectomy d) Statin e) Warfarin The Peer Teaching Society is not liable for false or misleading information…
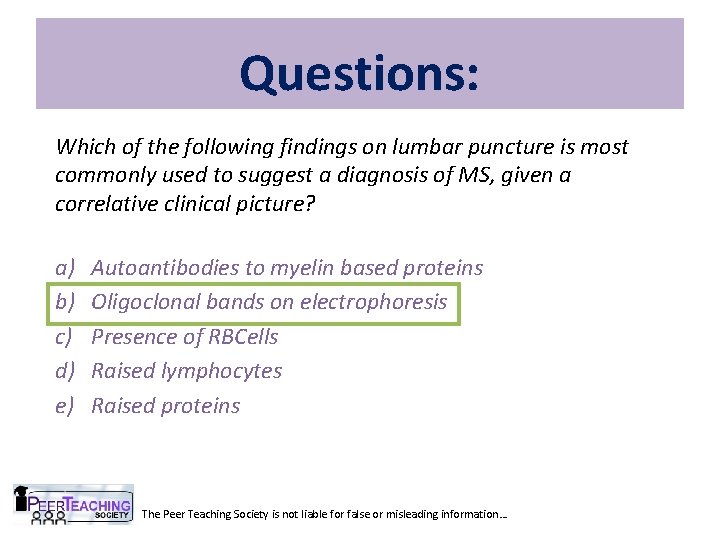
Questions: Which of the following findings on lumbar puncture is most commonly used to suggest a diagnosis of MS, given a correlative clinical picture? a) b) c) d) e) Autoantibodies to myelin based proteins Oligoclonal bands on electrophoresis Presence of RBCells Raised lymphocytes Raised proteins The Peer Teaching Society is not liable for false or misleading information…
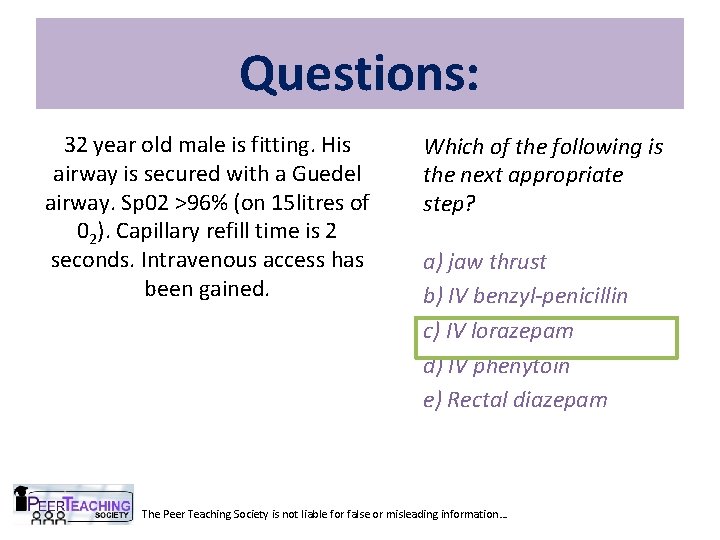
Questions: 32 year old male is fitting. His airway is secured with a Guedel airway. Sp 02 >96% (on 15 litres of 02). Capillary refill time is 2 seconds. Intravenous access has been gained. Which of the following is the next appropriate step? a) jaw thrust b) IV benzyl-penicillin c) IV lorazepam d) IV phenytoin e) Rectal diazepam The Peer Teaching Society is not liable for false or misleading information…
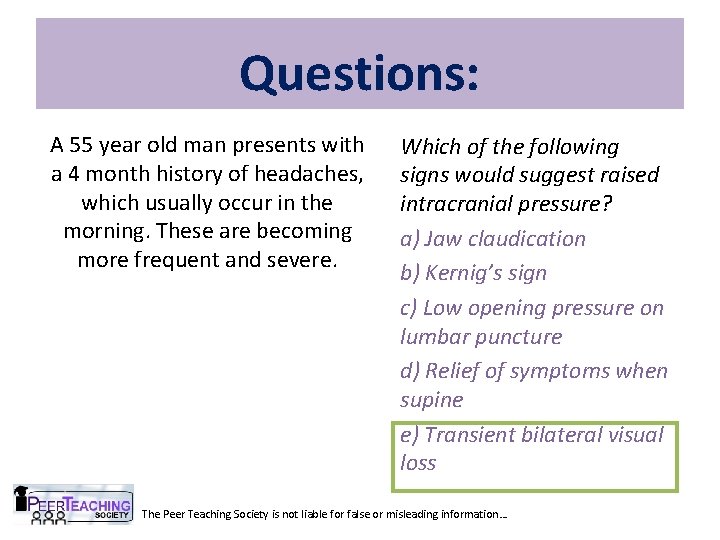
Questions: A 55 year old man presents with a 4 month history of headaches, which usually occur in the morning. These are becoming more frequent and severe. Which of the following signs would suggest raised intracranial pressure? a) Jaw claudication b) Kernig’s sign c) Low opening pressure on lumbar puncture d) Relief of symptoms when supine e) Transient bilateral visual loss The Peer Teaching Society is not liable for false or misleading information…
- Slides: 77