Neurologic Support Lauren Chisholm PAC Brain Injury Primary
Neurologic Support Lauren Chisholm PA-C
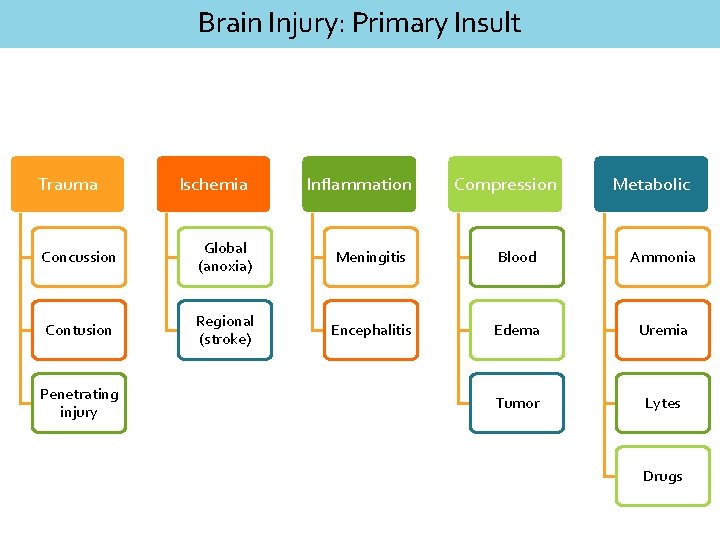
Brain Injury: Primary Insult Trauma Ischemia Inflammation Compression Metabolic Concussion Global (anoxia) Meningitis Blood Ammonia Contusion Regional (stroke) Encephalitis Edema Uremia Tumor Lytes Penetrating injury Drugs
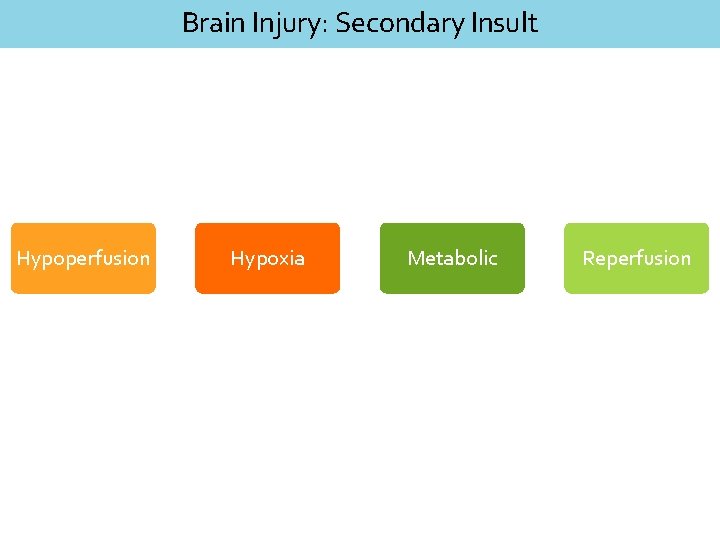
Brain Injury: Secondary Insult Hypoperfusion Hypoxia Metabolic Reperfusion
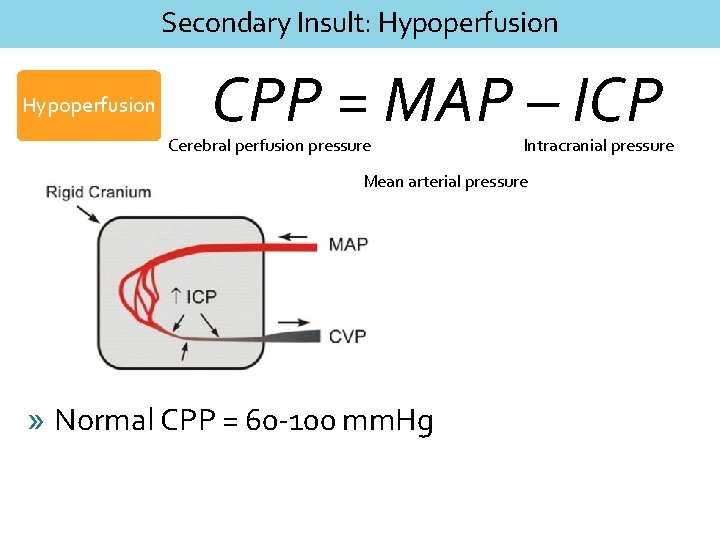
Secondary Insult: Hypoperfusion CPP = MAP – ICP Cerebral perfusion pressure Intracranial pressure Mean arterial pressure » Normal CPP = 60 -100 mm. Hg
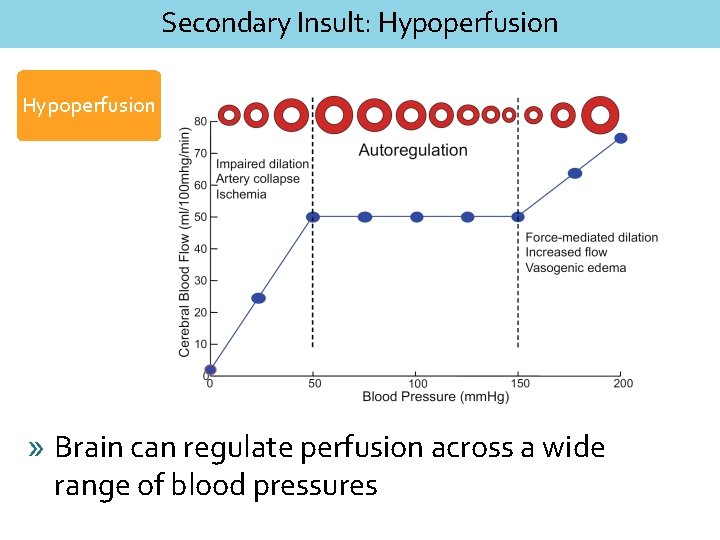
Secondary Insult: Hypoperfusion » Brain can regulate perfusion across a wide range of blood pressures
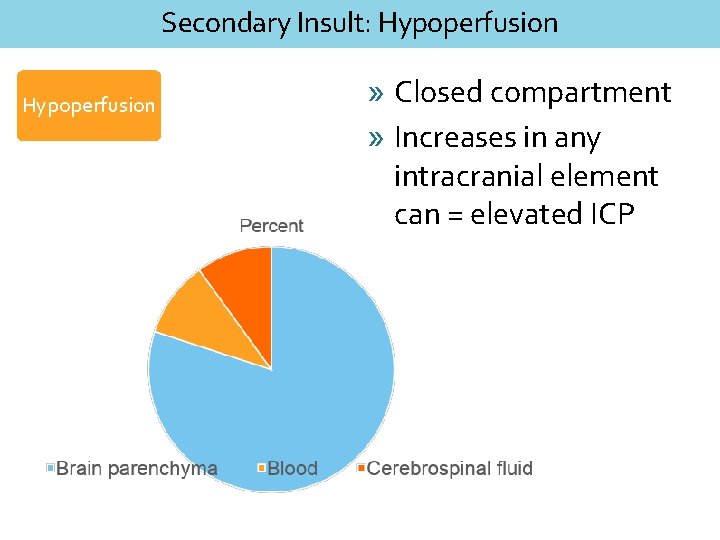
Secondary Insult: Hypoperfusion » Closed compartment » Increases in any intracranial element can = elevated ICP
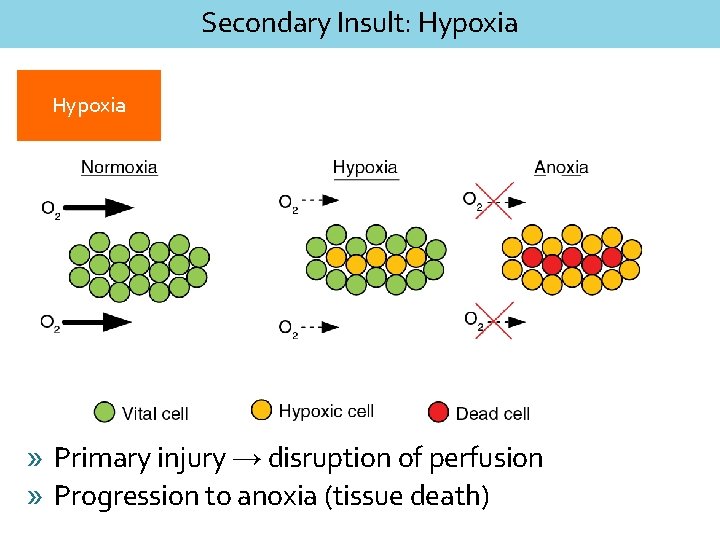
Secondary Insult: Hypoxia » Primary injury → disruption of perfusion » Progression to anoxia (tissue death)
Secondary Insult: Metabolic » Abnormalities in acid/base, electrolyte regulation
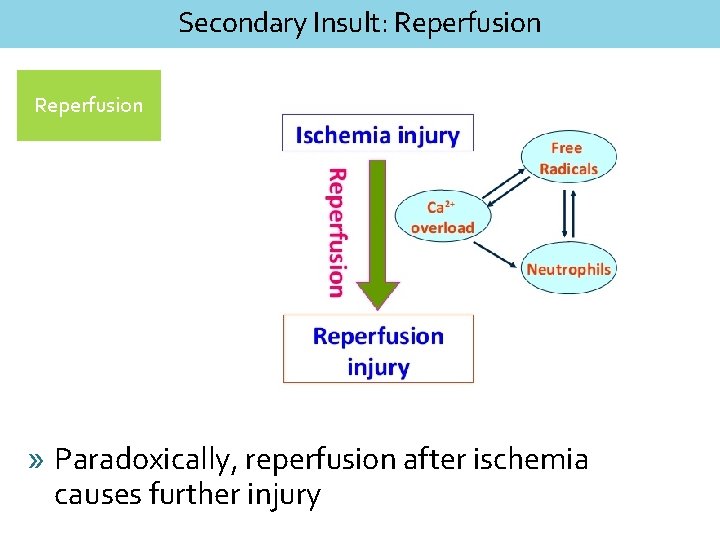
Secondary Insult: Reperfusion » Paradoxically, reperfusion after ischemia causes further injury
Neurologic Support: Take Home Identify & correct the primary insult (if you can) Understand & prevent secondary insults
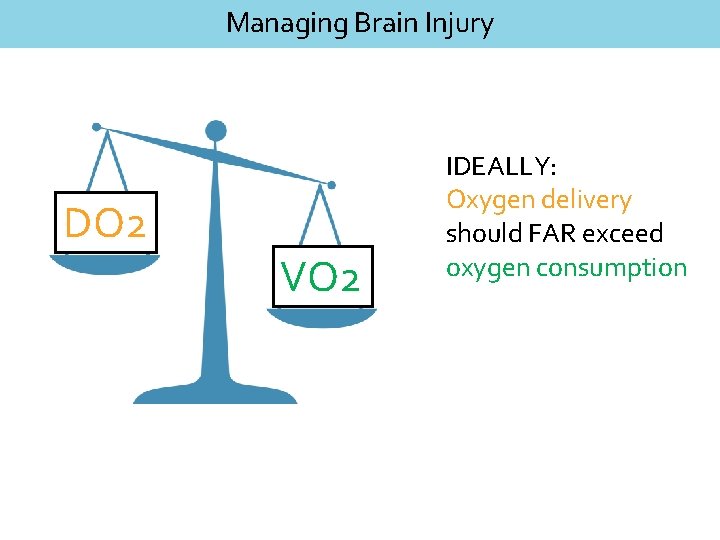
Managing Brain Injury DO 2 VO 2 IDEALLY: Oxygen delivery should FAR exceed oxygen consumption
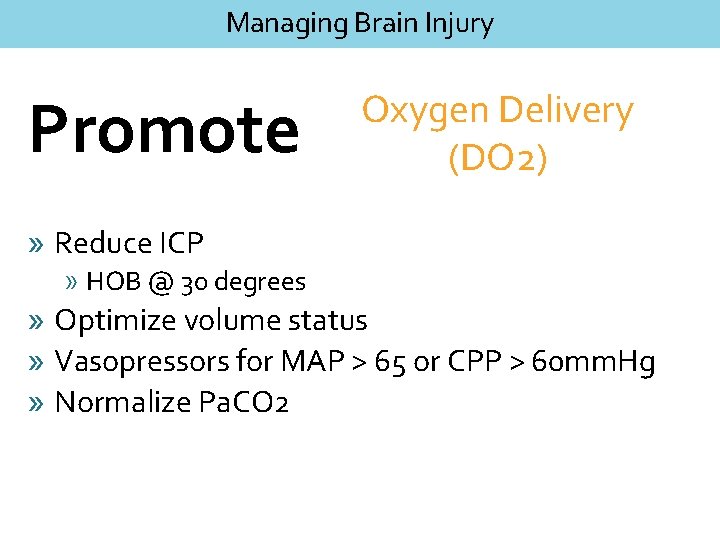
Managing Brain Injury Promote Oxygen Delivery (DO 2) » Reduce ICP » HOB @ 30 degrees » Optimize volume status » Vasopressors for MAP > 65 or CPP > 60 mm. Hg » Normalize Pa. CO 2
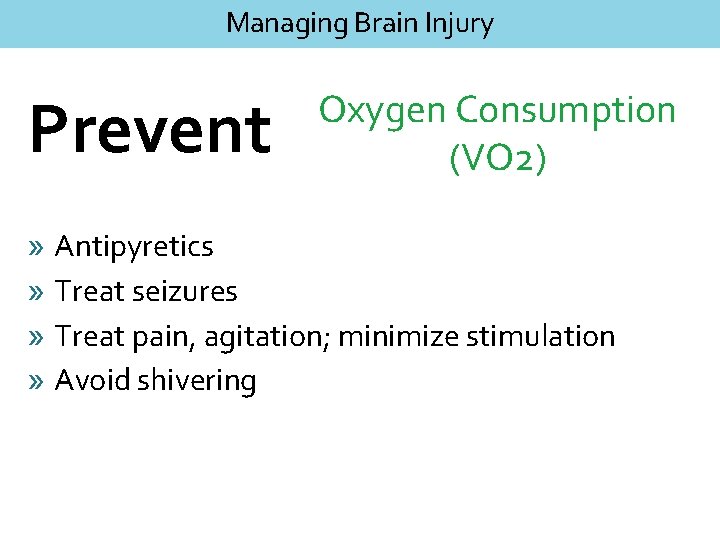
Managing Brain Injury Prevent Oxygen Consumption (VO 2) » Antipyretics » Treat seizures » Treat pain, agitation; minimize stimulation » Avoid shivering
Assessment Primary and Secondary
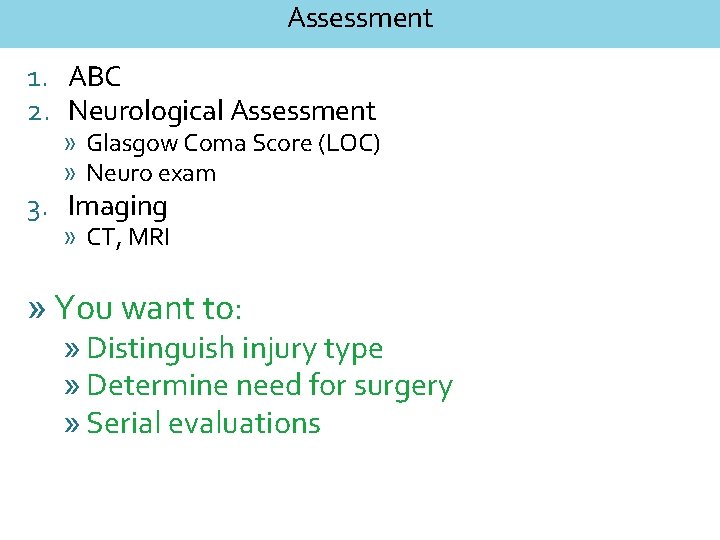
Assessment 1. ABC 2. Neurological Assessment » Glasgow Coma Score (LOC) » Neuro exam 3. Imaging » CT, MRI » You want to: » Distinguish injury type » Determine need for surgery » Serial evaluations
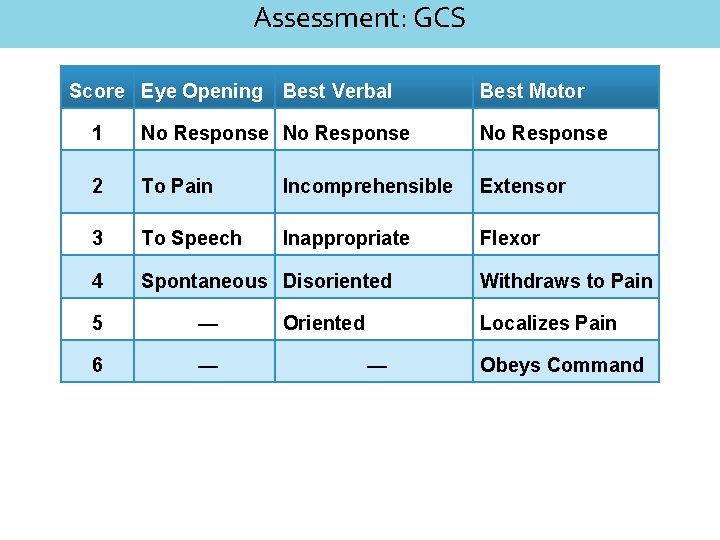
Assessment: GCS Score Eye Opening Best Verbal Best Motor 1 No Response 2 To Pain Incomprehensible Extensor 3 To Speech Inappropriate Flexor 4 Spontaneous Disoriented 5 — 6 — Oriented Withdraws to Pain Localizes Pain — Obeys Command
Things that should scare you » Lateralizing findings » Decreased LOC » Pupillary asymmetry » Dysconjugate gaze » Change in respiratory pattern » Cushing’s reflex » Hypertension, bradycardia
» Professional pitcher, hit in head after pitch » LOC for ~ 1 min » No focal deficits on exam, A&Ox 4, normal vital signs
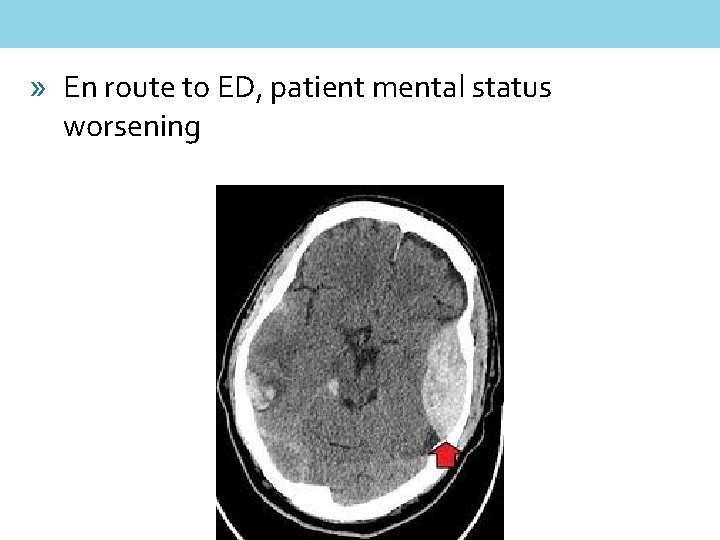
» En route to ED, patient mental status worsening
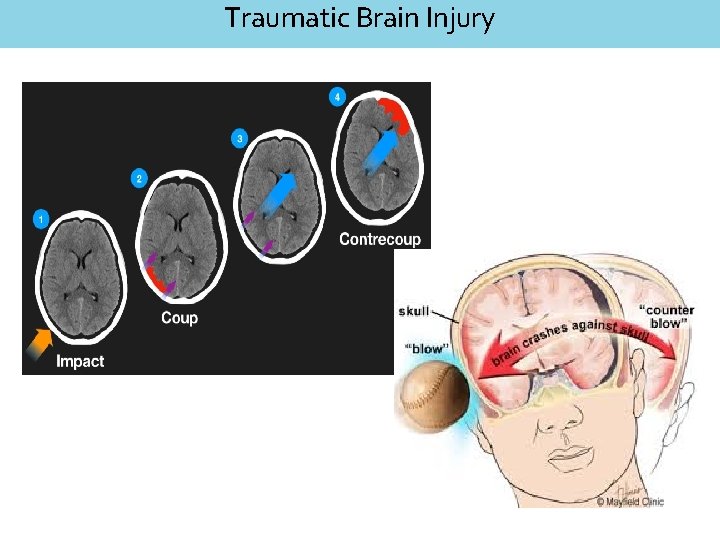
Traumatic Brain Injury
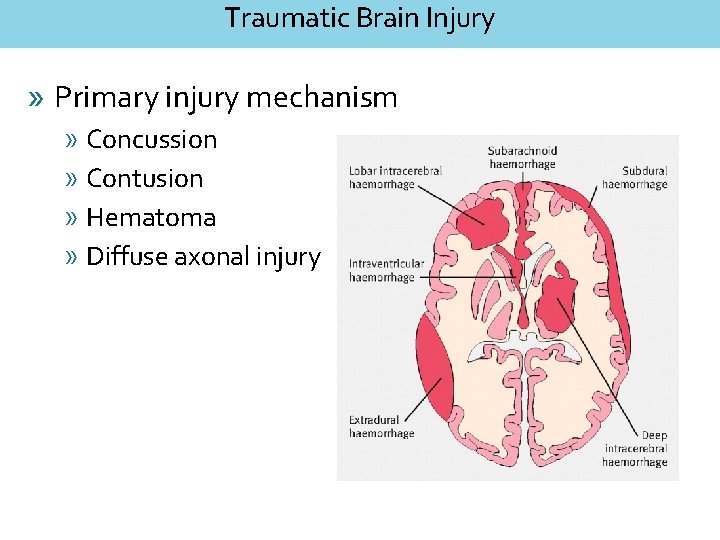
Traumatic Brain Injury » Primary injury mechanism » Concussion » Contusion » Hematoma » Diffuse axonal injury
Traumatic Brain Injury » Ensure no spinal cord injury » Hypotension » Bradycardia » Respiratory compromise » Other associated trauma » Thoracic » Abdominal
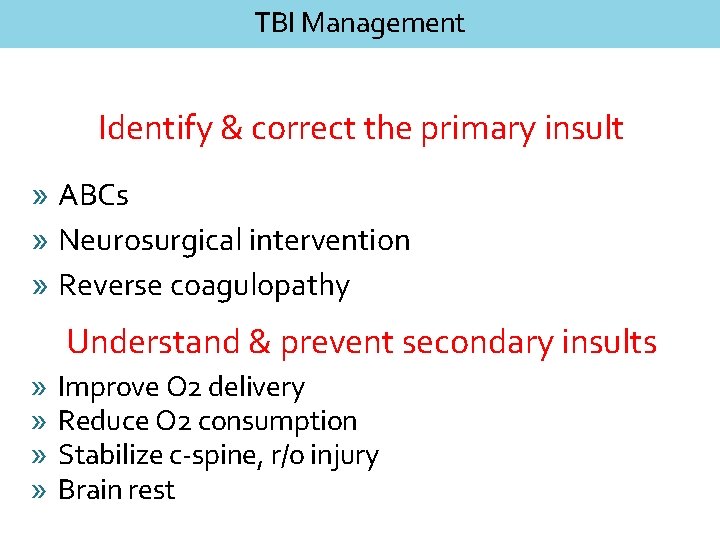
TBI Management Identify & correct the primary insult » ABCs » Neurosurgical intervention » Reverse coagulopathy Understand & prevent secondary insults » » Improve O 2 delivery Reduce O 2 consumption Stabilize c-spine, r/o injury Brain rest
» 63 y/o male presents with R sided hemiparesis, facial droop » Takes coumadin for a fib
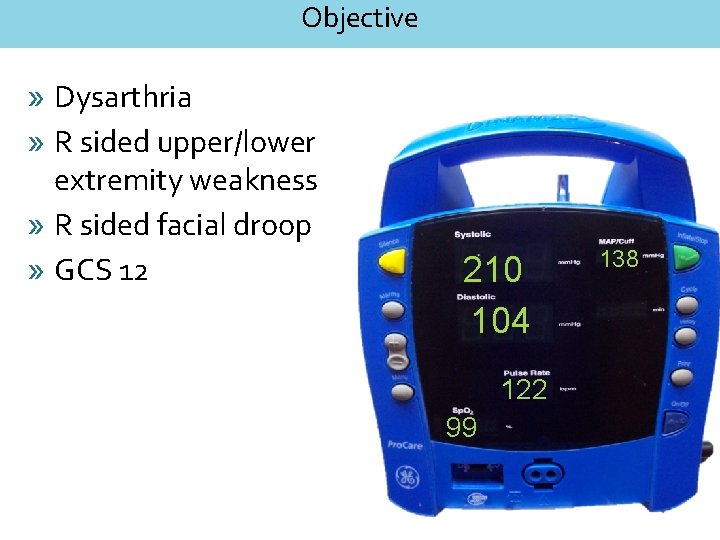
Objective » Dysarthria » R sided upper/lower extremity weakness » R sided facial droop » GCS 12 210 104 122 99 138
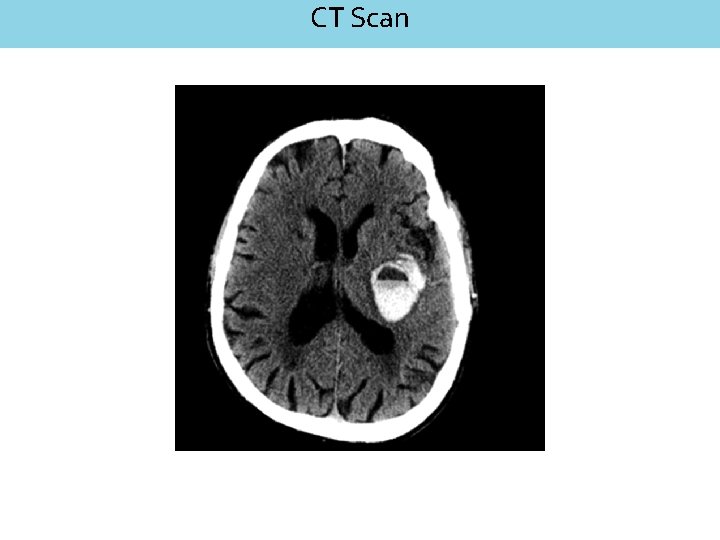
CT Scan
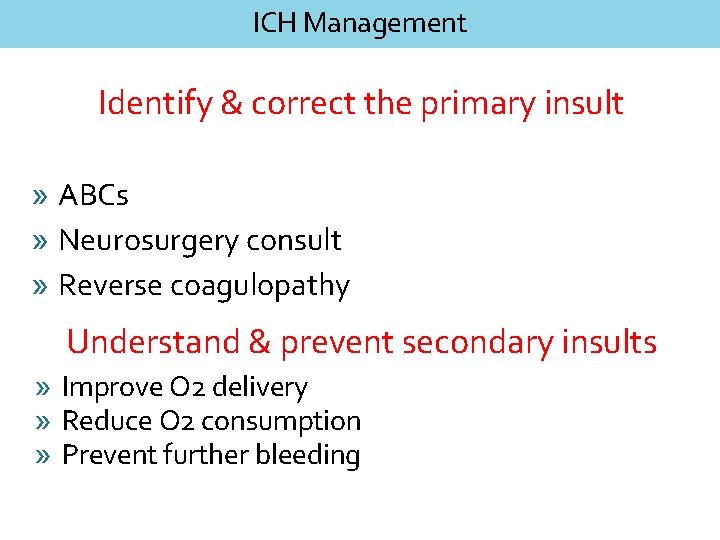
ICH Management Identify & correct the primary insult » ABCs » Neurosurgery consult » Reverse coagulopathy Understand & prevent secondary insults » Improve O 2 delivery » Reduce O 2 consumption » Prevent further bleeding
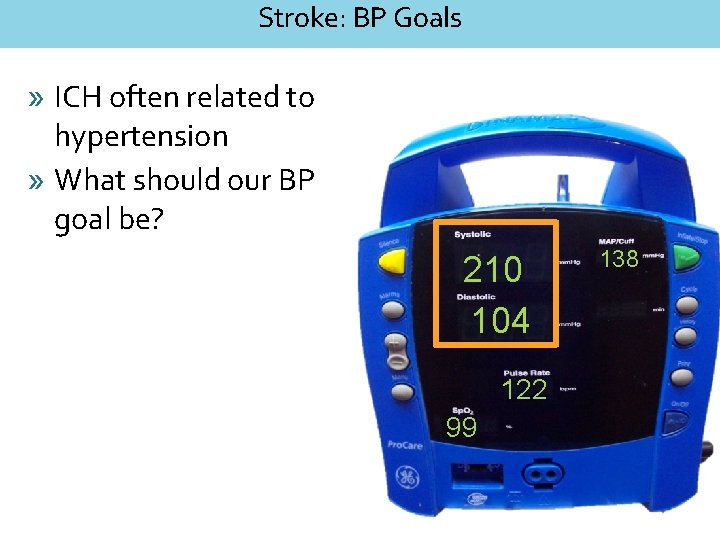
Stroke: BP Goals » ICH often related to hypertension » What should our BP goal be? 210 104 122 99 138
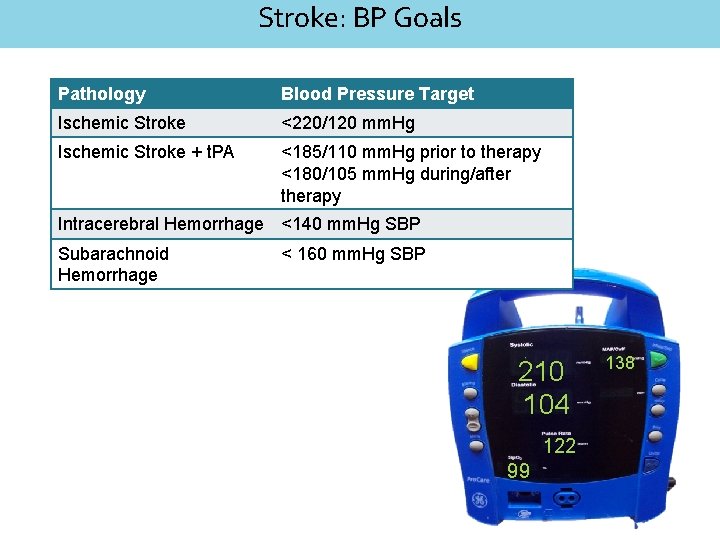
Stroke: BP Goals Pathology Blood Pressure Target Ischemic Stroke <220/120 mm. Hg Ischemic Stroke + t. PA <185/110 mm. Hg prior to therapy <180/105 mm. Hg during/after therapy Intracerebral Hemorrhage <140 mm. Hg SBP Subarachnoid Hemorrhage < 160 mm. Hg SBP 210 104 122 99 138
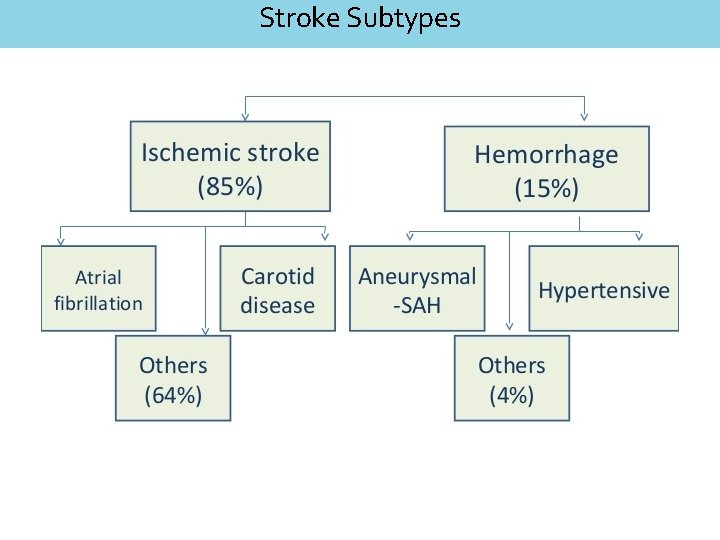
Stroke Subtypes
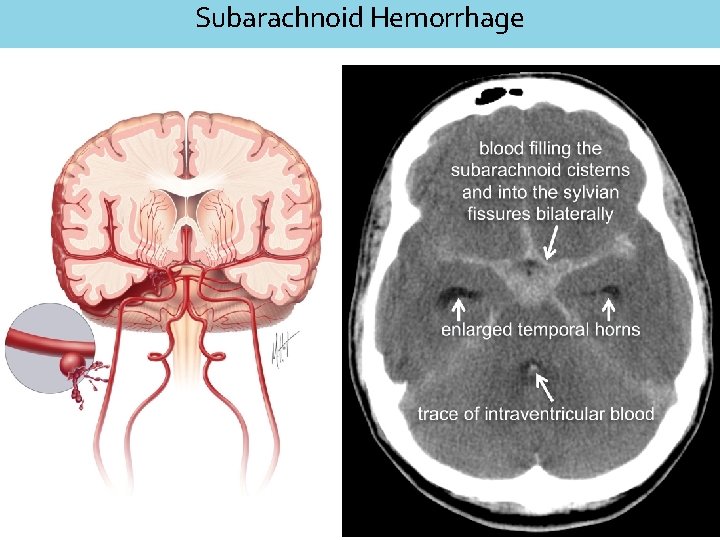
Subarachnoid Hemorrhage
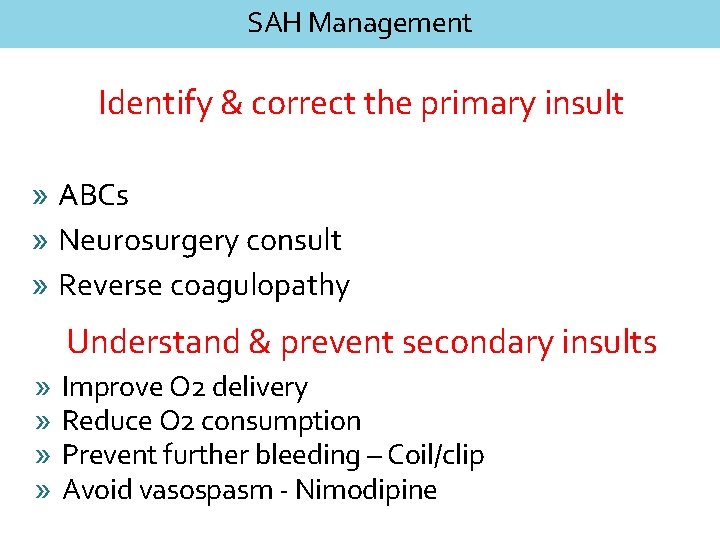
SAH Management Identify & correct the primary insult » ABCs » Neurosurgery consult » Reverse coagulopathy Understand & prevent secondary insults » » Improve O 2 delivery Reduce O 2 consumption Prevent further bleeding – Coil/clip Avoid vasospasm - Nimodipine
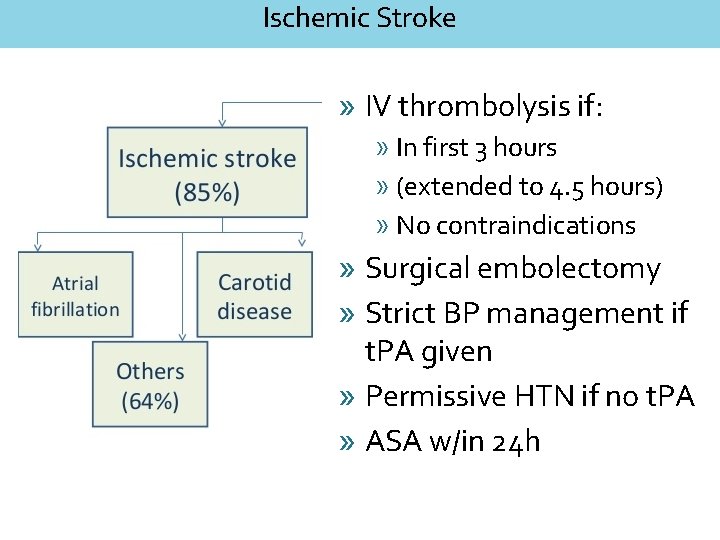
Ischemic Stroke » IV thrombolysis if: » In first 3 hours » (extended to 4. 5 hours) » No contraindications » Surgical embolectomy » Strict BP management if t. PA given » Permissive HTN if no t. PA » ASA w/in 24 h
» 70 y/o male admitted for sepsis 2/2 UTI » Found by RN on floor, lifted back into bed » STAT team called for unresponsiveness
Acute Encephalopathy » Hypoglycemia » Liver failure (ammonia) » Renal failure (uremia) » Sepsis, shock » Electrolytes » Drugs
Acute Encephalopathy » Check BG » Draw labs » Consider CT Head » LP, empiric abx if meningitis suspected
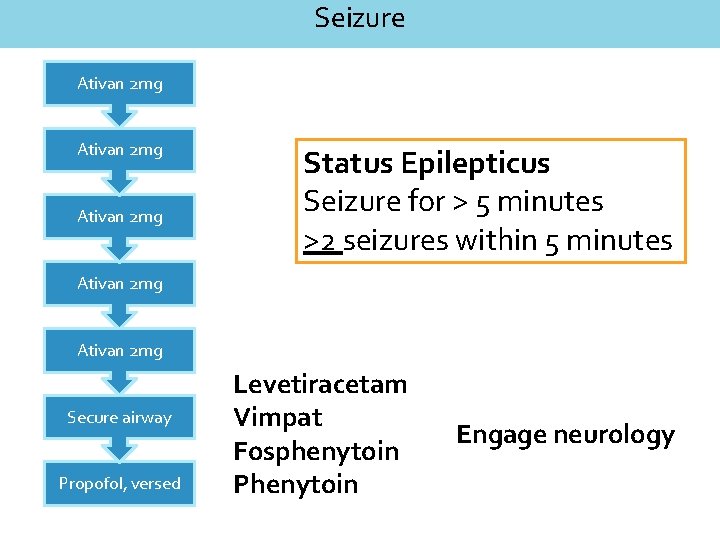
Seizure Ativan 2 mg Status Epilepticus Seizure for > 5 minutes >2 seizures within 5 minutes Ativan 2 mg Secure airway Propofol, versed Levetiracetam Vimpat Fosphenytoin Phenytoin Engage neurology
- Slides: 37