Neurologic Emergencies traumatic brain injury TBI Todd M
Neurologic Emergencies: traumatic brain injury (TBI) Todd M. Bishop, DVM, DACVIM (Neurology) Thursday February 6 th, 2014
Lecture Outline • • Basic pathophysiology Clinical signs Neurologic exam Therapeutic interventions Diagnostic testing Prognosis When to refer
Pathophysiology • Primary brain (direct) injury – contusion, compression, laceration, hemorrhage • Secondary brain (indirect) injury – – – – ischemia swelling (edema) Intracellular accumulation of Na+ & Ca++ activation of the coagulation, complement, & arachidonic acid cascades oxygen free radical production ATP depletion cytokine induction extracellular accumulation of glutamate, NO, lactic acid
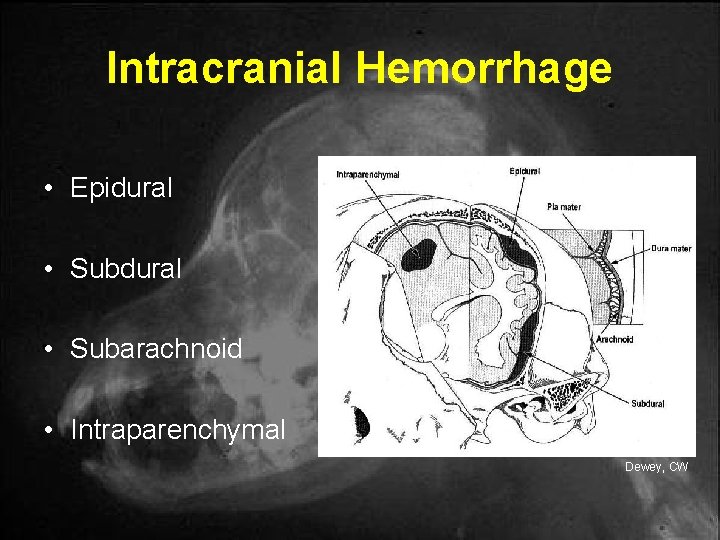
Intracranial Hemorrhage • Epidural • Subarachnoid • Intraparenchymal Dewey, CW
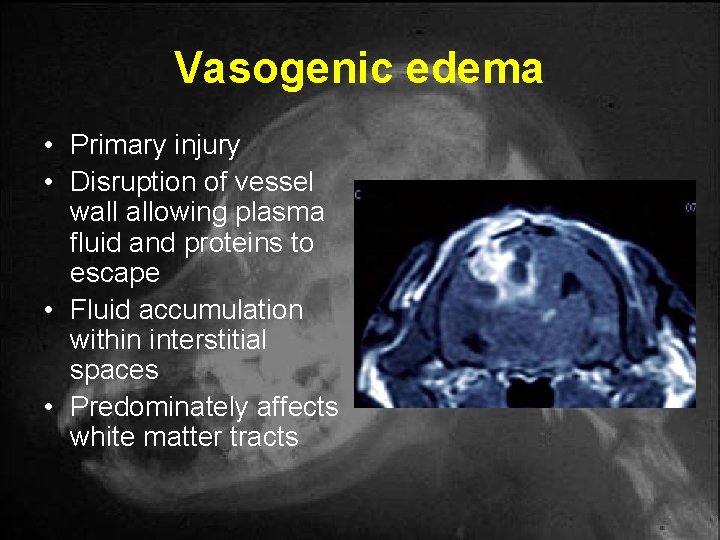
Vasogenic edema • Primary injury • Disruption of vessel wall allowing plasma fluid and proteins to escape • Fluid accumulation within interstitial spaces • Predominately affects white matter tracts
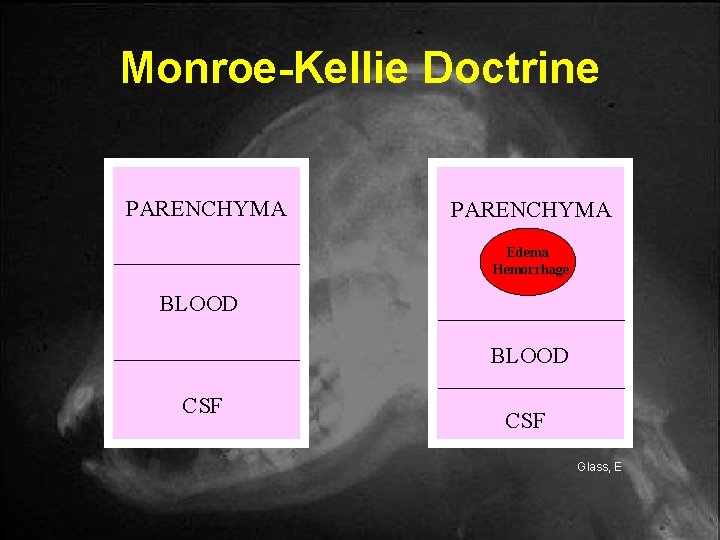
Monroe-Kellie Doctrine PARENCHYMA Edema Hemorrhage BLOOD CSF Glass, E
Intracranial Pressure (ICP) • Pressure exerted by tissues and fluids within the cranial vault • Normal ICP = 5 – 12 mm. Hg
Signs of ↑ ICP • • Systemic hypertension w/ bradycardia Altered mentation Anisocoria Vestibulo-ocular reflex (VOR) Pupillary light reflex (PLR) alterations Decerebrate rigidity Decerebellate rigidity Altered respiratory patterns
![The Cushing’s Reflex ↑ ICP ↓ CBF ↑ cerebral [CO 2] Chemoreceptor stim Sympathetic The Cushing’s Reflex ↑ ICP ↓ CBF ↑ cerebral [CO 2] Chemoreceptor stim Sympathetic](http://slidetodoc.com/presentation_image/748e09ace95e47d47e4974f6774e2ab7/image-9.jpg)
The Cushing’s Reflex ↑ ICP ↓ CBF ↑ cerebral [CO 2] Chemoreceptor stim Sympathetic stim ↑ Vasomotor tone ↑ MAP Baroreceptor stim Vagal response ↓ HR HYPERTENSION with a reflex BRADYCARDIA
Mentation • • • Alert Depressed Dull, vague, distant Obtunded Semicomatosed (stuporous) Comatosed
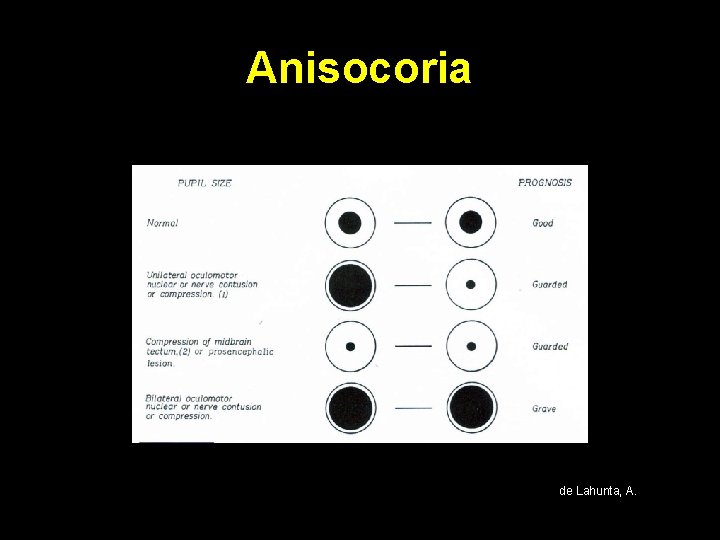
Anisocoria de Lahunta, A.
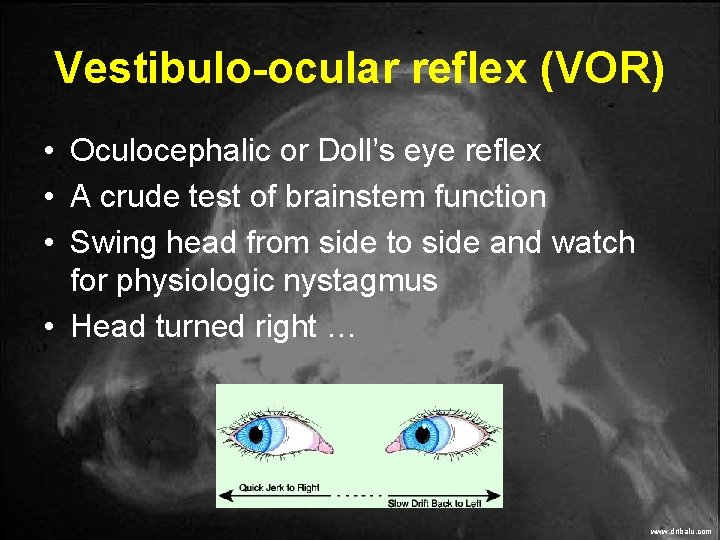
Vestibulo-ocular reflex (VOR) • Oculocephalic or Doll’s eye reflex • A crude test of brainstem function • Swing head from side to side and watch for physiologic nystagmus • Head turned right … www. drtbalu. com
Decerebrate rigidity • • • Rostral brainstem lesion (midbrain-pons) Extension of all 4 limbs Opisthotonos Stupor or coma Pinpoint or widely dilated, nonresponsive pupils • POOR PROGNOSIS
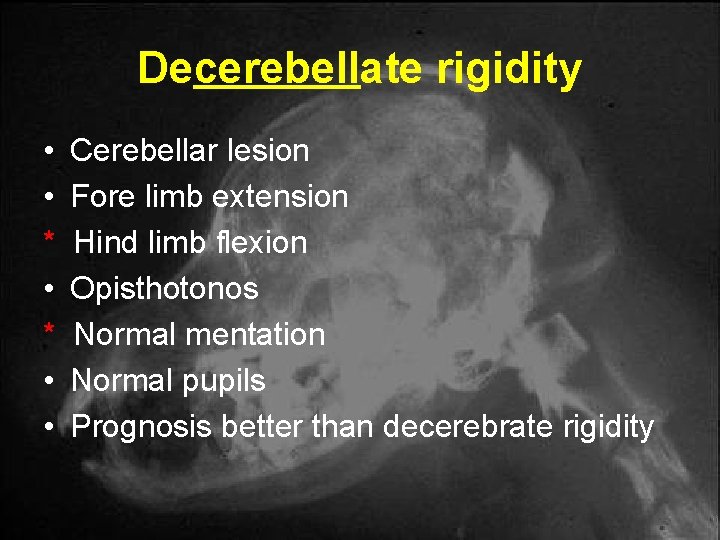
Decerebellate rigidity • • * • • Cerebellar lesion Fore limb extension Hind limb flexion Opisthotonos Normal mentation Normal pupils Prognosis better than decerebrate rigidity
Initial assessment • A - airway • B - breathing • C - cardiovascular status (IV access) * Assess and treat the ABC’s prior to the neurologic exam! * Hypoxemia and hypovolemia (hypotension) are commonly observed with head trauma
Minimum database • • • Packed Cell Volume (PCV) Total Solids (TS) Blood glucose (BG) Electrolytes (Na+. K+. Cl-) Blood Pressure Pulse Oximetry
Fluid therapy • • Hetastarch: 5 ml/kg IV over 5 -10 mins. 7% Na. Cl: 4 -5 ml/kg IV over 3 -5 mins. Dextran 70: 5 ml/kg IV over 5 -10 mins. Crystalloids* : – 80 -90 ml/kg/hr (dogs) – 50 -60 ml/kg/hr (cats) * use sparingly as may exacerbate cerebral edema (low pressure resuscitation)
Mannitol Theory • Osmotic diuretic that ↓ ICP via: • reflex cerebral vasoconstriction due to ↓ blood viscosity (first 2 -3 minutes) • Osmotically drawing fluid (edema) from the EVS to IVS (within 15 -30 minutes) • ↓ CSF production • Free-radical scavenging http: //www. neogen. com/Web. Ready. Graphics/AS_Products/Mannitol. jpg
Mannitol Administration • • Dose: 0. 5 -1. 0 g/kg IV over 10 -20 minutes Effects of Mannitol last for 2 – 5 hours No more than 3 doses in a 24 hour period Furosemide synergy: 2 -5 mg/kg IV a few minutes prior to Mannitol • Do Not give as a CRI! * Give after patient is hemodynamically stable
Potential Mannitol Side-effects • Hypernatremia and hyperosmolarity • Rebound hypertension • Exacerbation of intracranial hemorrhage • Reverse osmotic shift
Corticosteroids? • No longer the standard of care in TBI • May provide free-radical scavenging activity • Adjunctive treatment in patients: – not responding to typical resuscitative attempts – cerebral edema confirmed on brain imaging http: //darbydrug. com/prodimage/2286712. jpg
Oxygenation • Hypoxemia common in head trauma – Pneumothorax – Pulmonary contusions – Non-cardiogenic pulmonary edema (NCPE) • Attempt to maintain Pa. O 2 >90 mm. Hg using: – Nasal cannula @ 100 ml/kg/min – Transtracheal catheter @ 50 ml/kg/min – Oxygen cage/tent – Flow-by or face mask
Hyperventilation • Hypoventilation can be assessed with: – End-tidal CO 2 monitor – Arterial blood gas (Pa. CO 2) • Goal is to maintain Pa. CO 2 btwn 25 -35 mm. Hg – Pa. CO 2 > 35 → vasodilation → ↑ ICP – Pa. CO 2 < 25 → vasoconstriction → ↓ CPP (CBF) * Some patients may require ventilation
Miscellaneous therapies • • • Elevated head 15 -30° Avoid jugular vein compression Artificial tears Palpate & express bladder (vs. UCS) Change recumbency Physical therapy • Hypothermia? (89. 6 -93. 2° F) • Pentobarbital coma? • Oxygen free-radical scavengers (Lazaroids)?
Basic systemic work-up • • • Complete neurologic exam (multifocal) Thorough orthopedic exam Thoracic radiographs Abdominal radiographs vs. ultrasound CBC, Chem profile, UA, Coag panel, EKG
Diagnostic Imaging • Radiographs of skull • Radiographs of cervical spine • CT scan • MRI
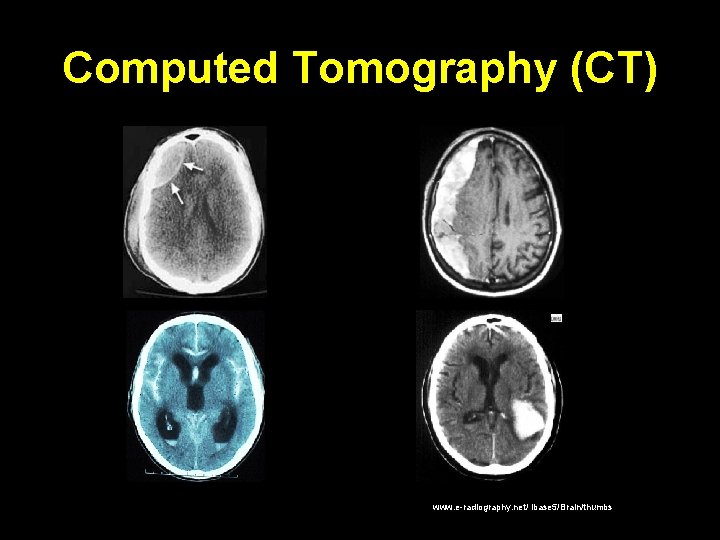
Computed Tomography (CT) www. e-radiography. net/ ibase 5/Brain/thumbs
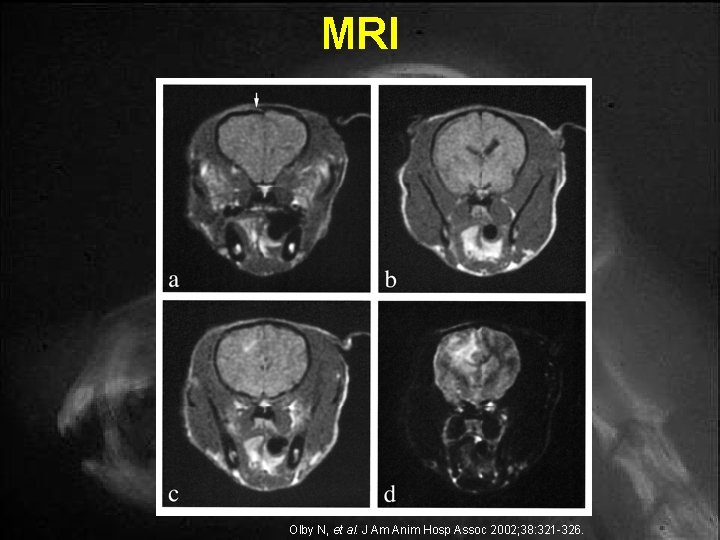
MRI Olby N, et al. J Am Anim Hosp Assoc 2002; 38: 321 -326.
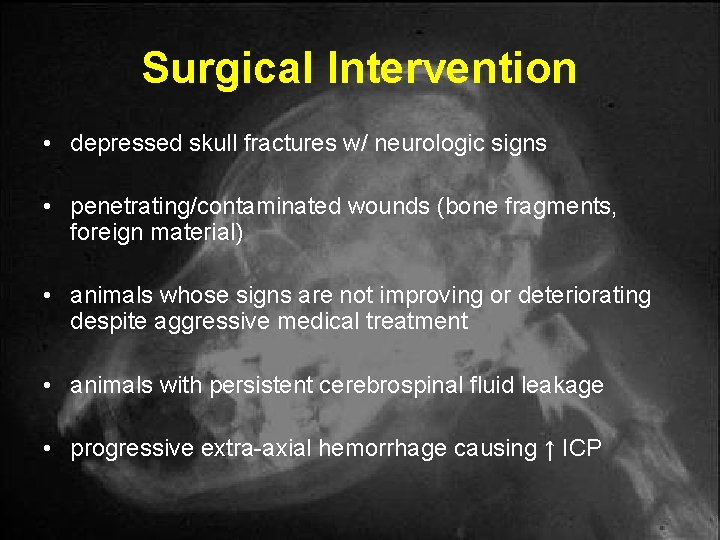
Surgical Intervention • depressed skull fractures w/ neurologic signs • penetrating/contaminated wounds (bone fragments, foreign material) • animals whose signs are not improving or deteriorating despite aggressive medical treatment • animals with persistent cerebrospinal fluid leakage • progressive extra-axial hemorrhage causing ↑ ICP
Prognosis • Overall prognosis always guarded! • Stuporous or comatosed with dilated unresponsive pupils (poor) • Coma lasting >48 hrs (grave) • Absent brainstem reflexes – VOR, BAER or caloric test negative (grave)
Prognosis • CT lesions do not correlate with prognosis • Gender, weight, age and presence of skull fractures do not predict survival • Hyperglycemia (negative prognostic indicator in people, not proven in vet med) • See MGCS for more prognostic details
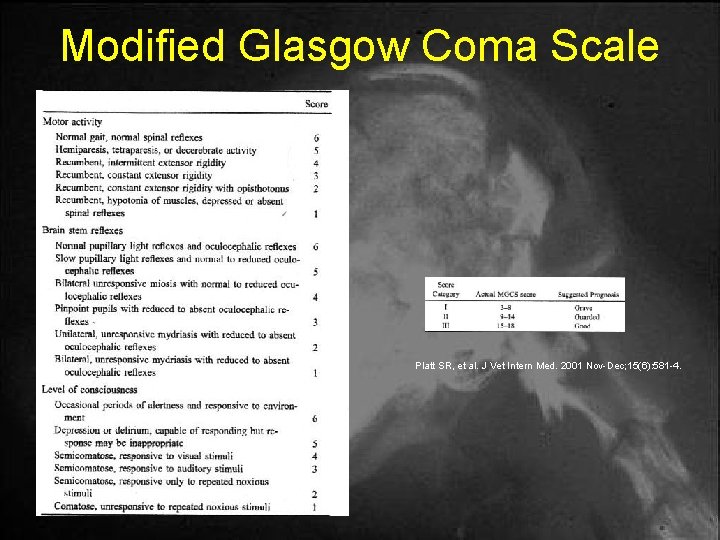
Modified Glasgow Coma Scale Platt SR, et al. J Vet Intern Med. 2001 Nov-Dec; 15(6): 581 -4.
Complications • • cardiac dysrhythmias (brain-heart syndrome) coagulopathies neurogenic pulmonary edema central diabetes insipidus (CDI) aspiration pneumonia meningitis post-trauma epilepsy
When to refer a TBI case … • After the following has been performed: – initial assessment (ABCs) – Minimum database – Preliminary resuscitation – Basic systemic work-up • Once the patient is stable !!! • When a patient is not responding to typical medical interventions
- Slides: 34