Neurodermatoradiology of the Head Neck Vascular Cutaneous Anomalies

![References 1. Leaute-Labreze C. [Propranolol in infantile hemangiomas]. Arch Pediatr. 2015; 22(4): 452 -5. References 1. Leaute-Labreze C. [Propranolol in infantile hemangiomas]. Arch Pediatr. 2015; 22(4): 452 -5.](https://slidetodoc.com/presentation_image_h/16f17245c861520001da41c8f229d36d/image-40.jpg)
- Slides: 40
Neurodermatoradiology of the Head & Neck Vascular Cutaneous Anomalies and Associated Syndromes Stephanie Mc. Cann MD; Daniel Ginat MD, MS; Gregory Christoforidis MD Department of Radiology e. Ed. E-133
Disclosures The authors have no disclosures. Neurodermatoradiology
Introduction • Vascular cutaneous anomalies include a diverse group of lesions that can have specific clinical and diagnostic imaging features, particularly when associated with syndromes. • Dermatologists may refer patients for imaging of suspected vascular neurodermatological anomalies in order to evaluate the extent of disease, uncover any potentially associated abnormalities, and for planning and gauging the efficacy of treatment. • Thus, radiologists are in well-poised to assist clinicians in synthesizing clinical data and guide the appropriateness of imaging. Neurodermatoradiology
Purpose • This educational exhibit exploits a multidisciplinary approach to the work up on head and neck vascular cutaneous anomalies with a focus on imaging. • In particular, relevant background, clinical findings, and distinctive multimodality imaging features of selected vascular cutaneous abnormalities are reviewed. • After completing this educational exhibit, the participant should: – Be able to accurately differentiate subtypes of vascular cutaneous anomalies based on clinical presentation and imaging features. – Recognize the constellation of findings in selected cerebrofacial arteriovenous metameric syndromes and vascular phakomatoses. – Recommend appropriate imaging studies to evaluate various vascular cutaneous anomalies based on clinical history and presentation. Neurodermatoradiology
Outline 1. Relevant anatomical considerations 2. Multidisciplinary problem solving approach 3. Vascular tumors 4. Low-flow vascular malformations 5. High-flow vascular malformations 6. Syndromes associated with vascular tumors and malformations Neurodermatoradiology
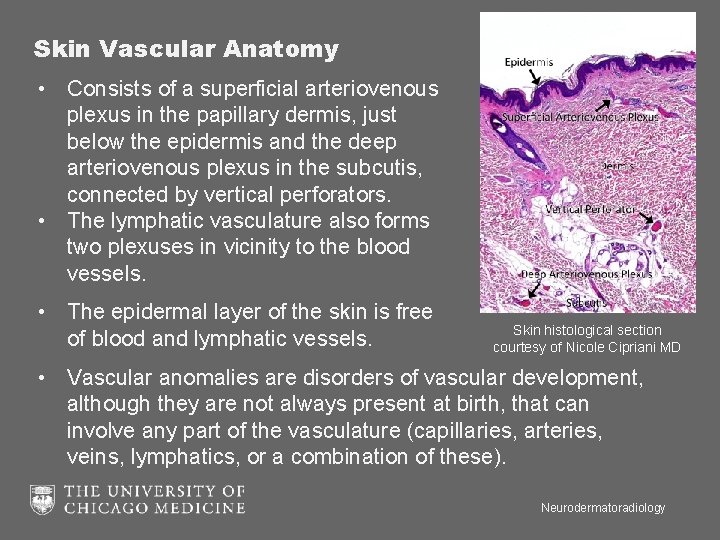
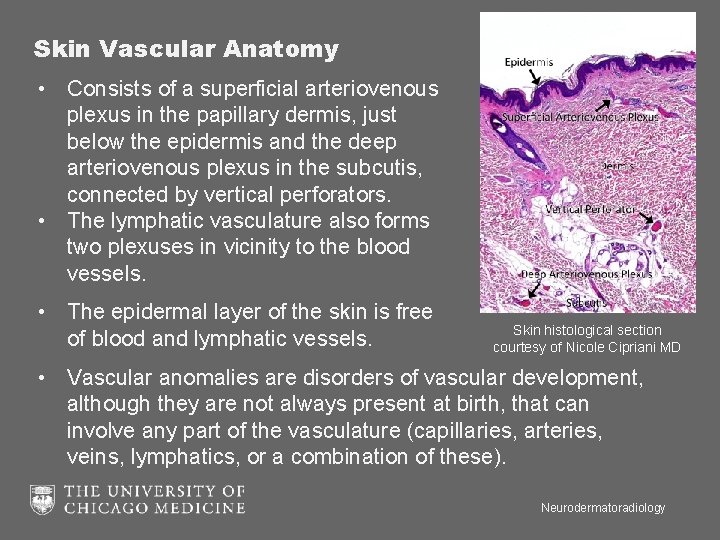
Skin Vascular Anatomy • Consists of a superficial arteriovenous plexus in the papillary dermis, just below the epidermis and the deep arteriovenous plexus in the subcutis, connected by vertical perforators. • The lymphatic vasculature also forms two plexuses in vicinity to the blood vessels. • The epidermal layer of the skin is free of blood and lymphatic vessels. Skin histological section courtesy of Nicole Cipriani MD • Vascular anomalies are disorders of vascular development, although they are not always present at birth, that can involve any part of the vasculature (capillaries, arteries, veins, lymphatics, or a combination of these). Neurodermatoradiology
Summary of Multidisciplinary Problem Solving ▪ Categorization ▪ Tumors versus malformations ▪ Clinical history/natural history: proliferation after birth and subsequent regression suggests certain types of hemangioma, for example ▪ Imaging ▪ MRI and CT: extent, tissue involvement, presurgical planning ▪ MRA/V, CTA, DSA, lymphangiography, and Doppler ultrasound: evaluate type of lesion ▪ Serial evaluation of treatment changes for lesions with deep extent ▪ Syndromes Associated with Vascular Lesions ▪ Complete physical exam and review of systems to evaluate for other neurologic, solid organ, osseous, and gastrointestinal abnormalities ▪ Dedicated imaging to evaluate for associated findings Neurodermatoradiology
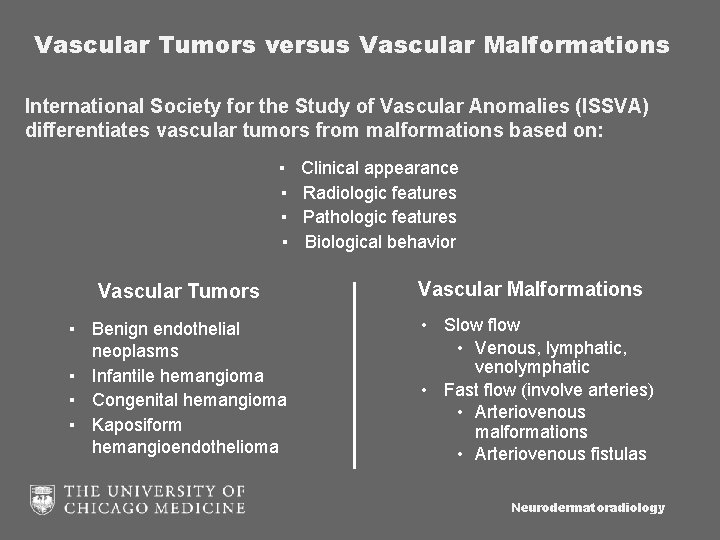
Vascular Tumors versus Vascular Malformations International Society for the Study of Vascular Anomalies (ISSVA) differentiates vascular tumors from malformations based on: ▪ ▪ Vascular Tumors ▪ Benign endothelial neoplasms ▪ Infantile hemangioma ▪ Congenital hemangioma ▪ Kaposiform hemangioendothelioma Clinical appearance Radiologic features Pathologic features Biological behavior Vascular Malformations • Slow flow • Venous, lymphatic, venolymphatic • Fast flow (involve arteries) • Arteriovenous malformations • Arteriovenous fistulas Neurodermatoradiology
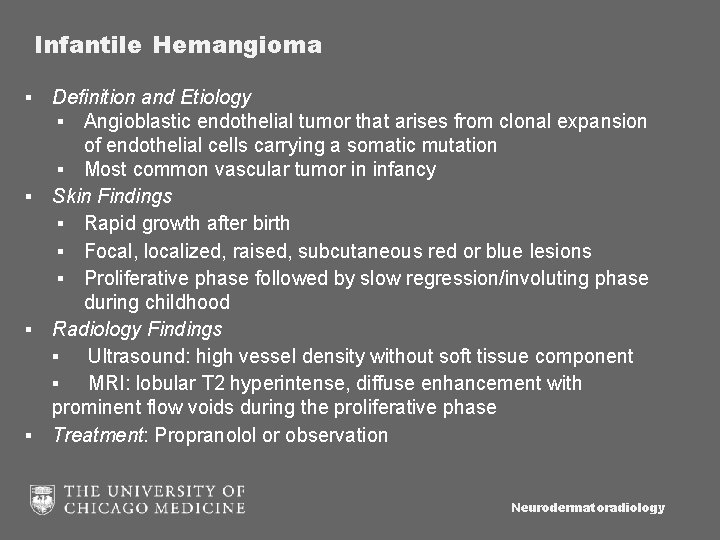
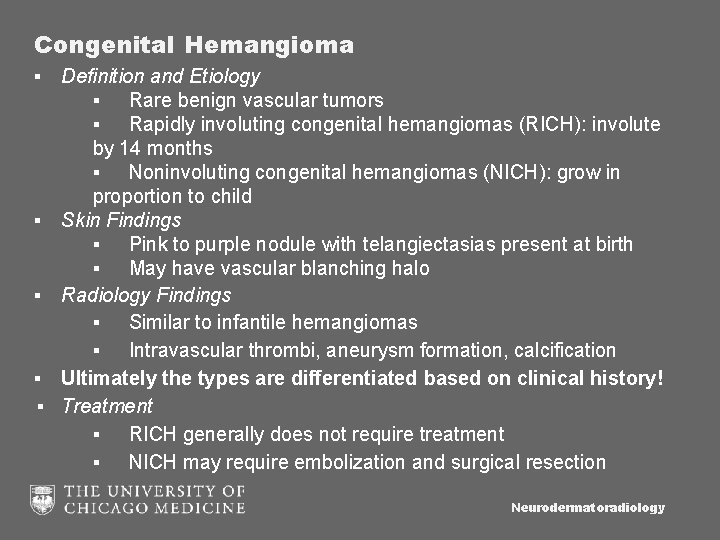
Infantile Hemangioma ▪ Definition and Etiology ▪ Angioblastic endothelial tumor that arises from clonal expansion of endothelial cells carrying a somatic mutation ▪ Most common vascular tumor in infancy ▪ Skin Findings ▪ Rapid growth after birth ▪ Focal, localized, raised, subcutaneous red or blue lesions ▪ Proliferative phase followed by slow regression/involuting phase during childhood ▪ Radiology Findings ▪ Ultrasound: high vessel density without soft tissue component ▪ MRI: lobular T 2 hyperintense, diffuse enhancement with prominent flow voids during the proliferative phase ▪ Treatment: Propranolol or observation Neurodermatoradiology
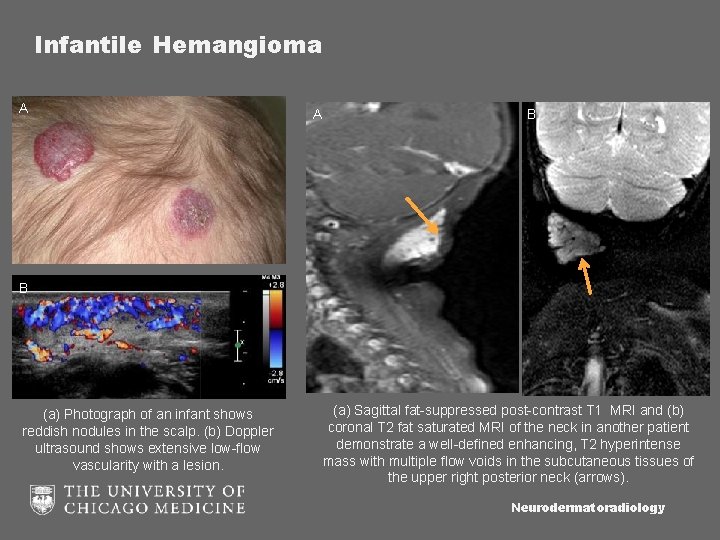
Infantile Hemangioma A A B B (a) Photograph of an infant shows reddish nodules in the scalp. (b) Doppler ultrasound shows extensive low-flow vascularity with a lesion. (a) Sagittal fat-suppressed post-contrast T 1 MRI and (b) coronal T 2 fat saturated MRI of the neck in another patient demonstrate a well-defined enhancing, T 2 hyperintense mass with multiple flow voids in the subcutaneous tissues of the upper right posterior neck (arrows). Neurodermatoradiology
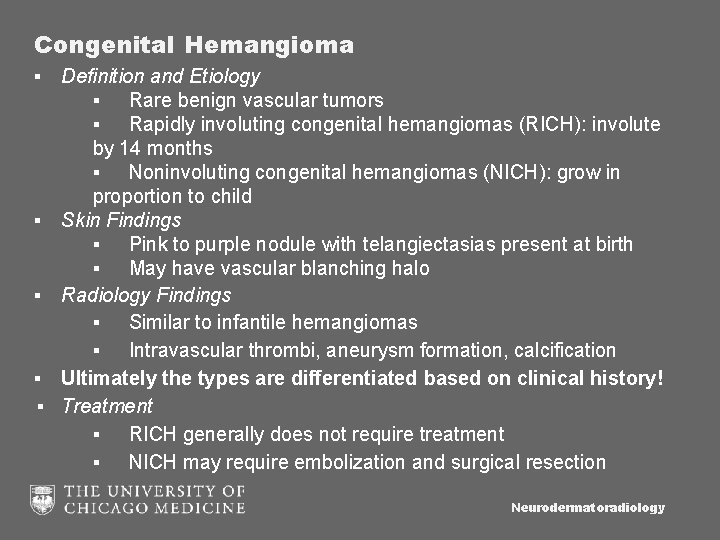
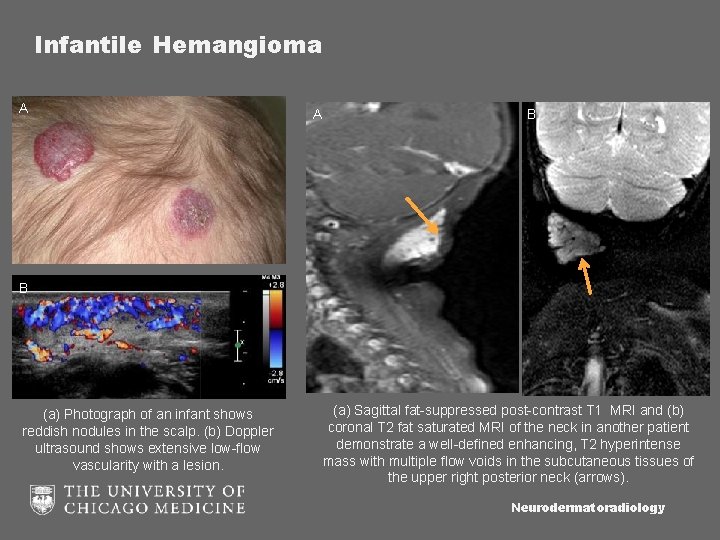
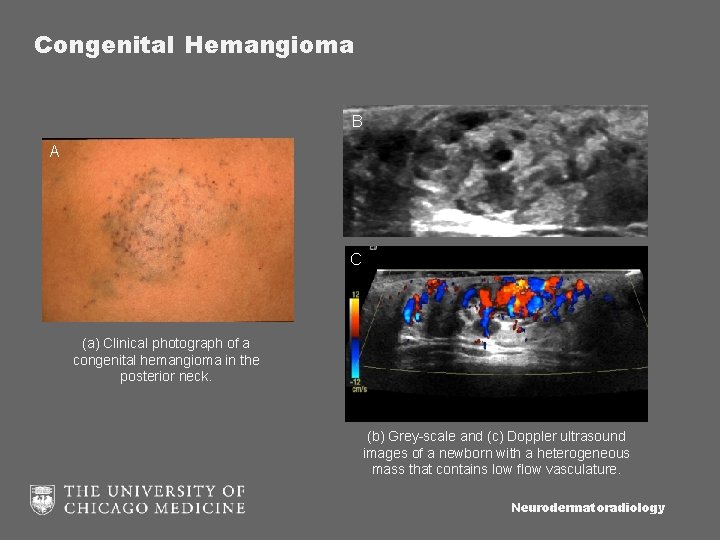
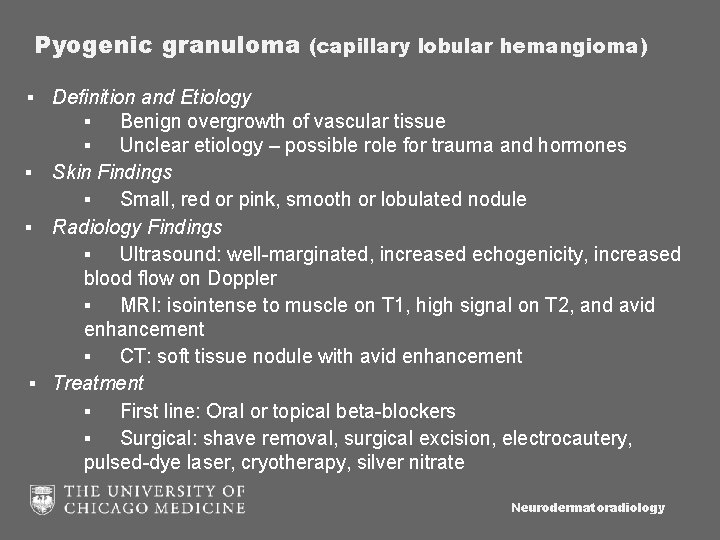
Congenital Hemangioma ▪ Definition and Etiology ▪ Rare benign vascular tumors ▪ Rapidly involuting congenital hemangiomas (RICH): involute by 14 months ▪ Noninvoluting congenital hemangiomas (NICH): grow in proportion to child ▪ Skin Findings ▪ Pink to purple nodule with telangiectasias present at birth ▪ May have vascular blanching halo ▪ Radiology Findings ▪ Similar to infantile hemangiomas ▪ Intravascular thrombi, aneurysm formation, calcification ▪ Ultimately the types are differentiated based on clinical history! ▪ Treatment ▪ RICH generally does not require treatment ▪ NICH may require embolization and surgical resection Neurodermatoradiology
Congenital Hemangioma B A C (a) Clinical photograph of a congenital hemangioma in the posterior neck. (b) Grey-scale and (c) Doppler ultrasound images of a newborn with a heterogeneous mass that contains low flow vasculature. Neurodermatoradiology
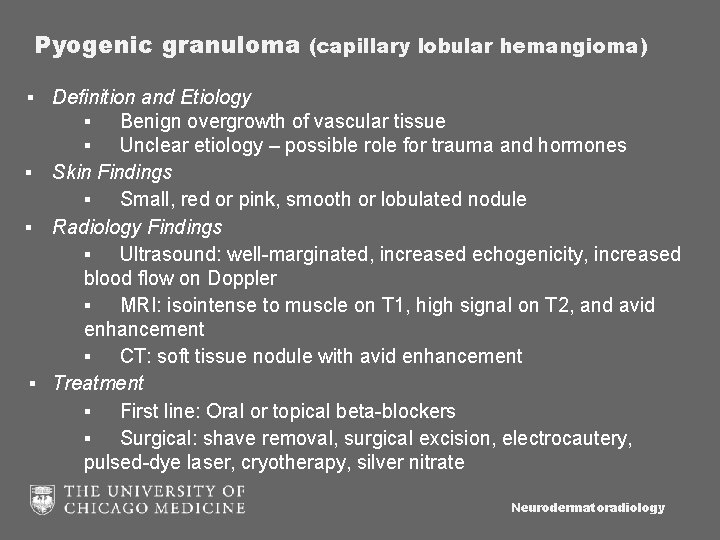
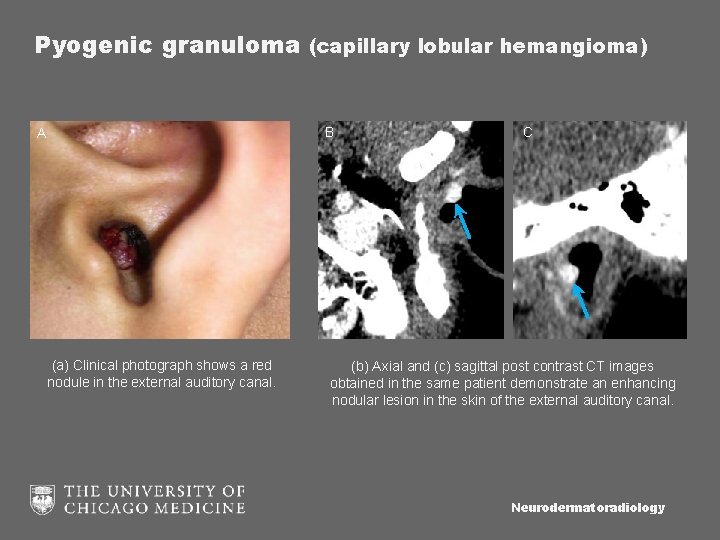
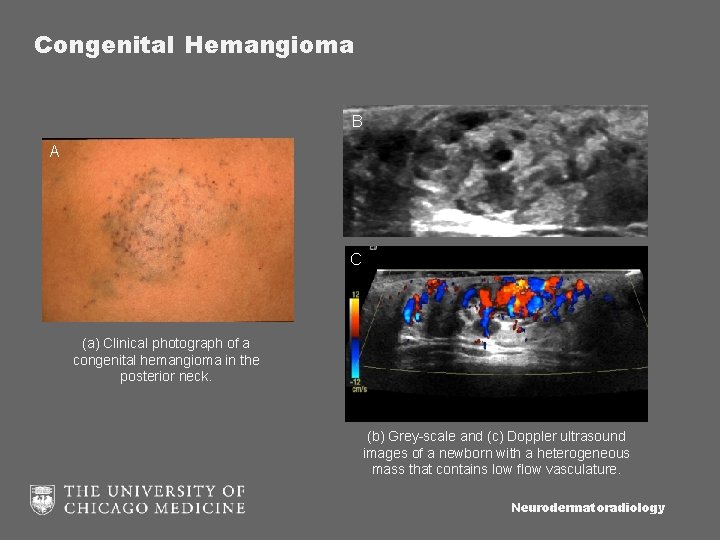
Pyogenic granuloma (capillary lobular hemangioma) ▪ Definition and Etiology ▪ Benign overgrowth of vascular tissue ▪ Unclear etiology – possible role for trauma and hormones ▪ Skin Findings ▪ Small, red or pink, smooth or lobulated nodule ▪ Radiology Findings ▪ Ultrasound: well-marginated, increased echogenicity, increased blood flow on Doppler ▪ MRI: isointense to muscle on T 1, high signal on T 2, and avid enhancement ▪ CT: soft tissue nodule with avid enhancement ▪ Treatment ▪ First line: Oral or topical beta-blockers ▪ Surgical: shave removal, surgical excision, electrocautery, pulsed-dye laser, cryotherapy, silver nitrate Neurodermatoradiology
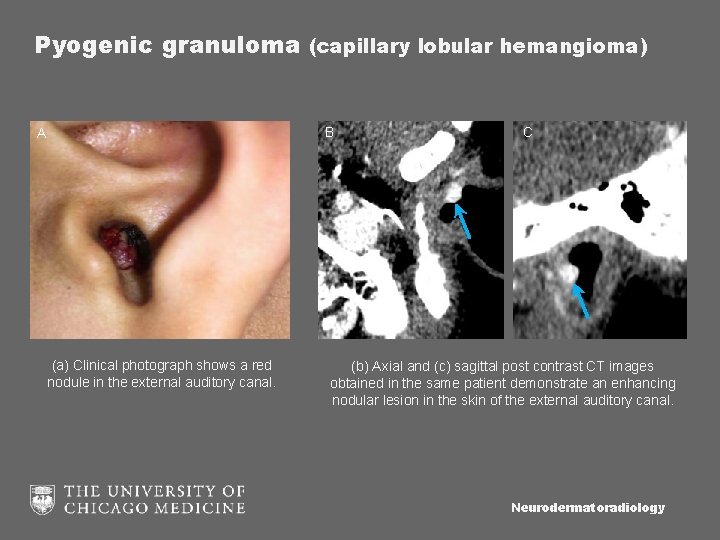
Pyogenic granuloma (capillary lobular hemangioma) B A (a) Clinical photograph shows a red nodule in the external auditory canal. C (b) Axial and (c) sagittal post contrast CT images obtained in the same patient demonstrate an enhancing nodular lesion in the skin of the external auditory canal. Neurodermatoradiology
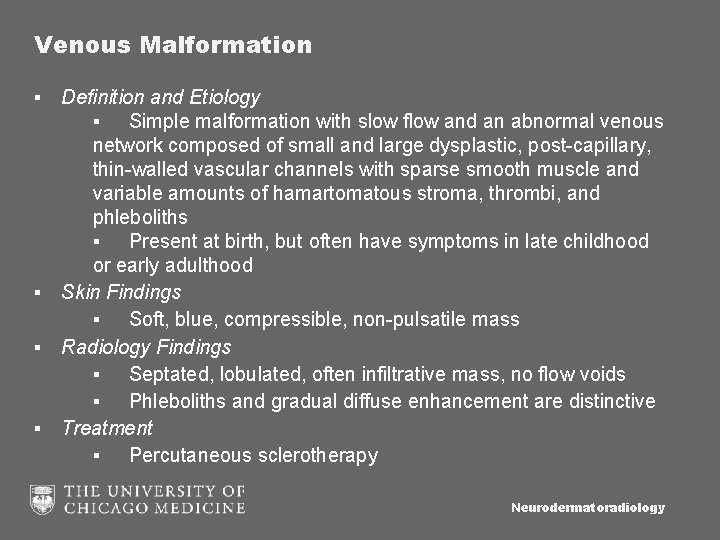
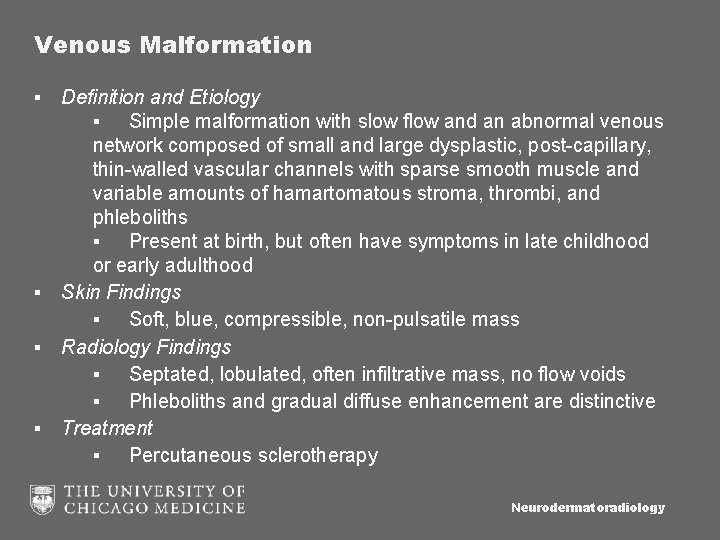
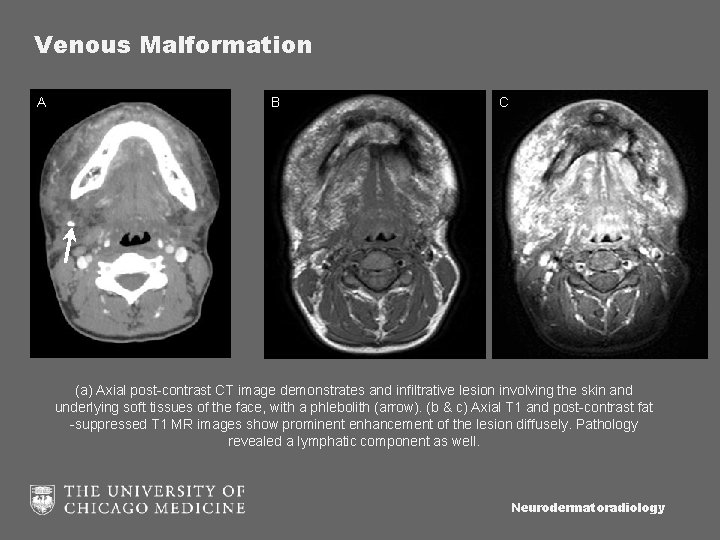
Venous Malformation ▪ Definition and Etiology ▪ Simple malformation with slow flow and an abnormal venous network composed of small and large dysplastic, post-capillary, thin-walled vascular channels with sparse smooth muscle and variable amounts of hamartomatous stroma, thrombi, and phleboliths ▪ Present at birth, but often have symptoms in late childhood or early adulthood ▪ Skin Findings ▪ Soft, blue, compressible, non-pulsatile mass ▪ Radiology Findings ▪ Septated, lobulated, often infiltrative mass, no flow voids ▪ Phleboliths and gradual diffuse enhancement are distinctive ▪ Treatment ▪ Percutaneous sclerotherapy Neurodermatoradiology
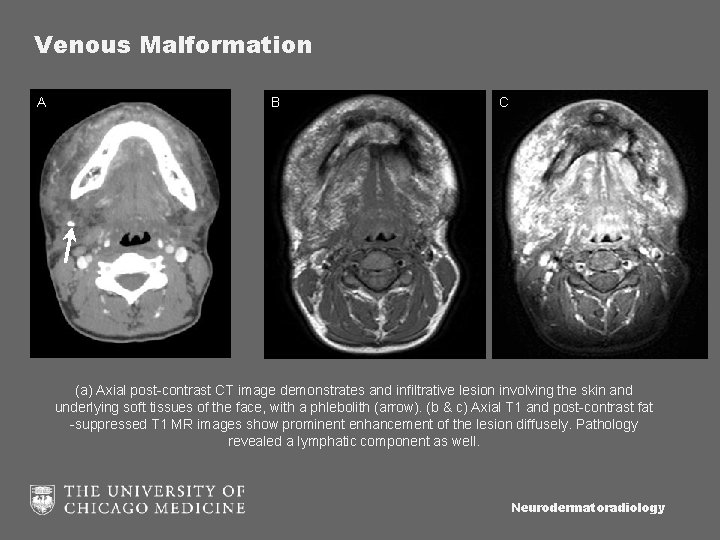
Venous Malformation A B C (a) Axial post-contrast CT image demonstrates and infiltrative lesion involving the skin and underlying soft tissues of the face, with a phlebolith (arrow). (b & c) Axial T 1 and post-contrast fat -suppressed T 1 MR images show prominent enhancement of the lesion diffusely. Pathology revealed a lymphatic component as well. Neurodermatoradiology
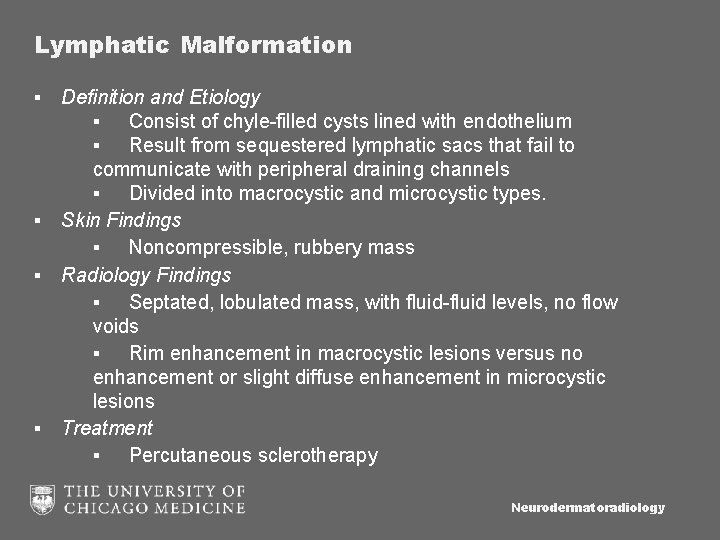
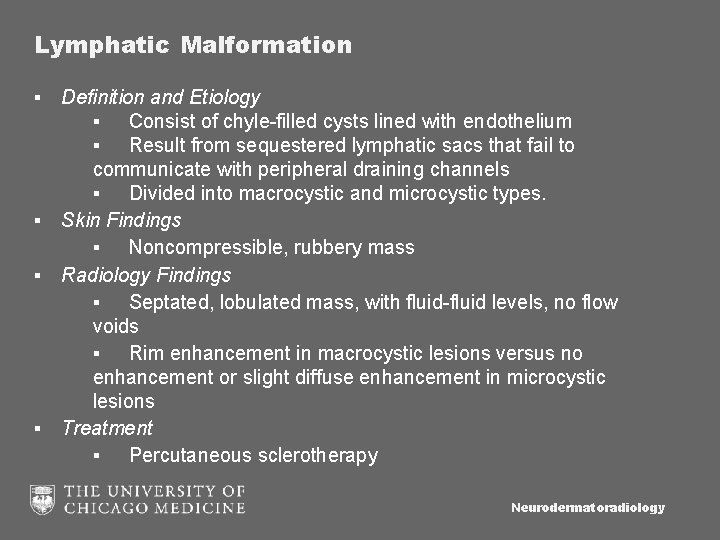
Lymphatic Malformation ▪ Definition and Etiology ▪ Consist of chyle-filled cysts lined with endothelium ▪ Result from sequestered lymphatic sacs that fail to communicate with peripheral draining channels ▪ Divided into macrocystic and microcystic types. ▪ Skin Findings ▪ Noncompressible, rubbery mass ▪ Radiology Findings ▪ Septated, lobulated mass, with fluid-fluid levels, no flow voids ▪ Rim enhancement in macrocystic lesions versus no enhancement or slight diffuse enhancement in microcystic lesions ▪ Treatment ▪ Percutaneous sclerotherapy Neurodermatoradiology
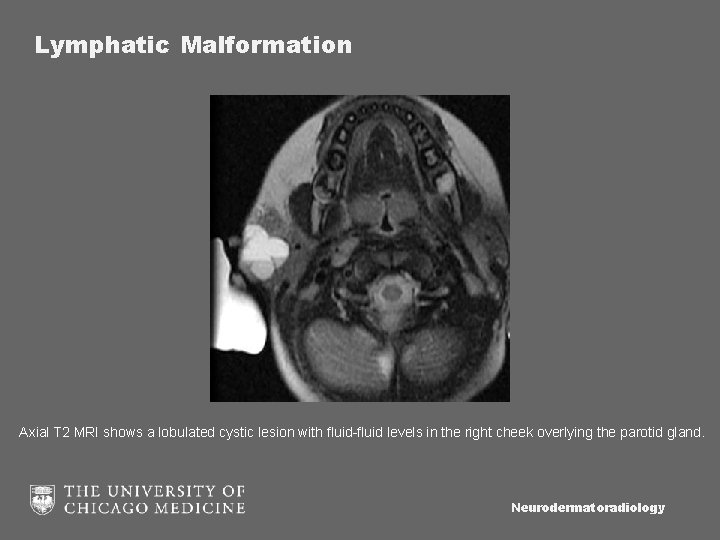
Lymphatic Malformation Axial T 2 MRI shows a lobulated cystic lesion with fluid-fluid levels in the right cheek overlying the parotid gland. Neurodermatoradiology
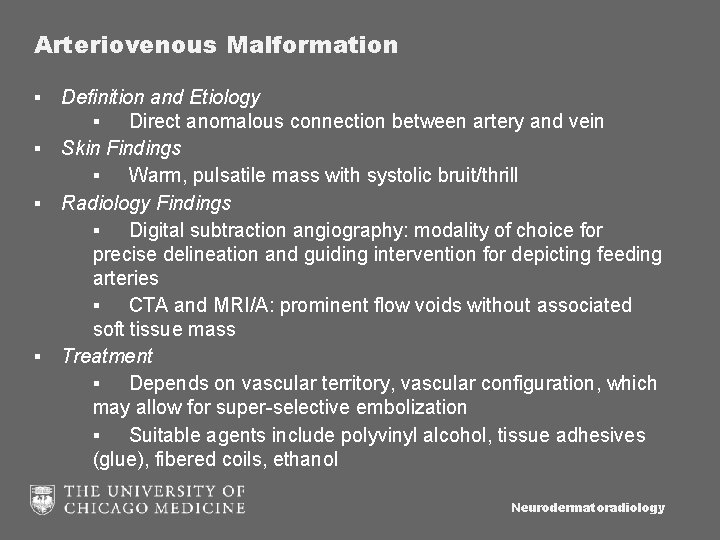
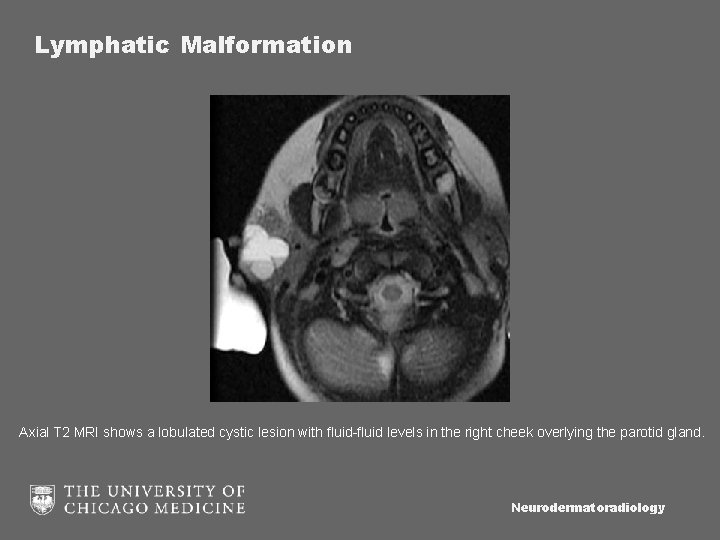
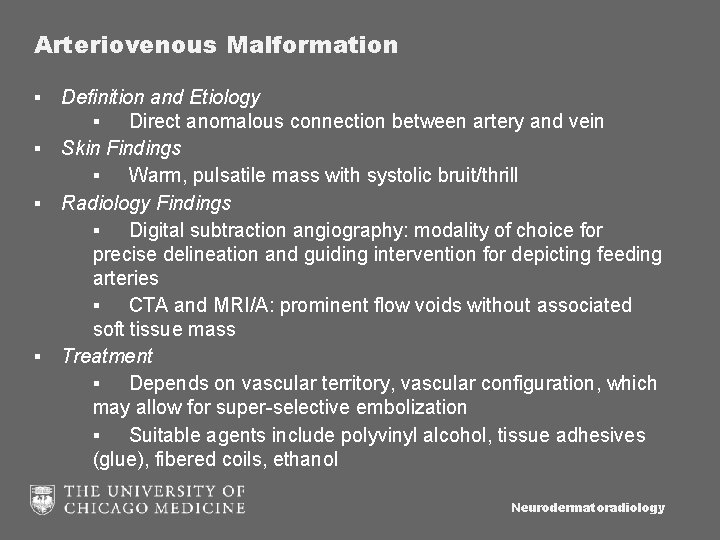
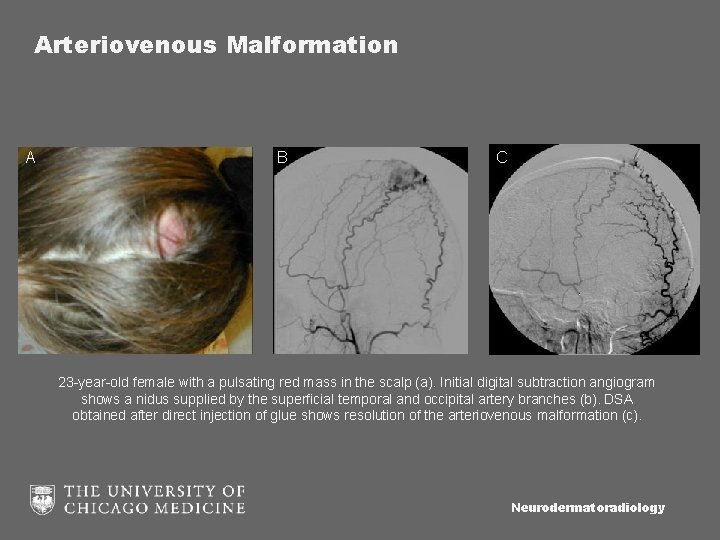
Arteriovenous Malformation ▪ Definition and Etiology ▪ Direct anomalous connection between artery and vein ▪ Skin Findings ▪ Warm, pulsatile mass with systolic bruit/thrill ▪ Radiology Findings ▪ Digital subtraction angiography: modality of choice for precise delineation and guiding intervention for depicting feeding arteries ▪ CTA and MRI/A: prominent flow voids without associated soft tissue mass ▪ Treatment ▪ Depends on vascular territory, vascular configuration, which may allow for super-selective embolization ▪ Suitable agents include polyvinyl alcohol, tissue adhesives (glue), fibered coils, ethanol Neurodermatoradiology
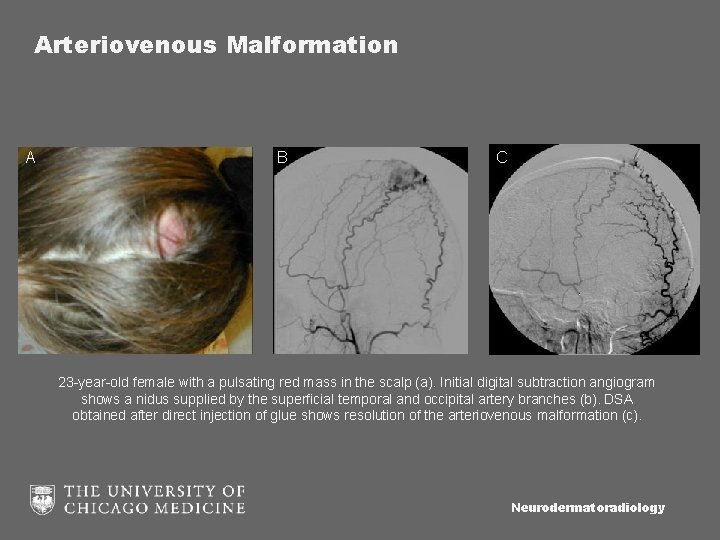
Arteriovenous Malformation A B C 23 -year-old female with a pulsating red mass in the scalp (a). Initial digital subtraction angiogram shows a nidus supplied by the superficial temporal and occipital artery branches (b). DSA obtained after direct injection of glue shows resolution of the arteriovenous malformation (c). Neurodermatoradiology
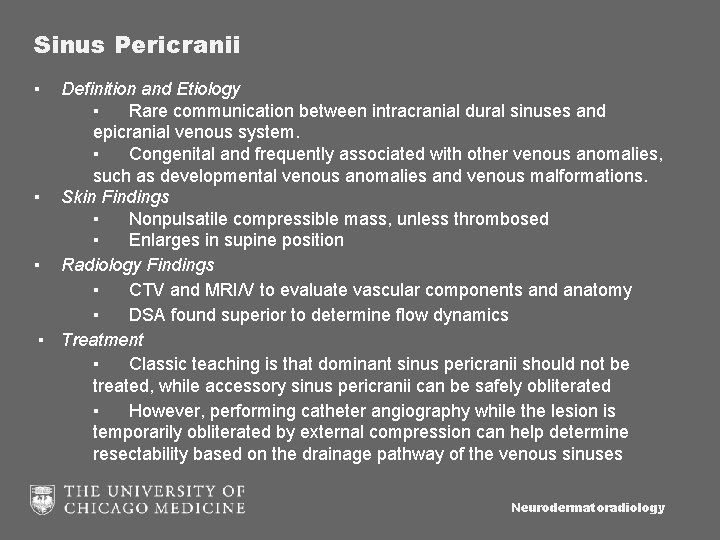
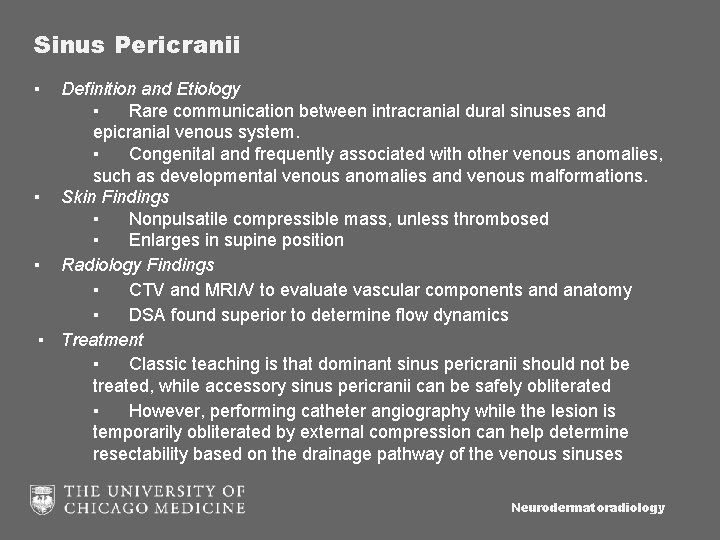
Sinus Pericranii ▪ Definition and Etiology ▪ Rare communication between intracranial dural sinuses and epicranial venous system. ▪ Congenital and frequently associated with other venous anomalies, such as developmental venous anomalies and venous malformations. ▪ Skin Findings ▪ Nonpulsatile compressible mass, unless thrombosed ▪ Enlarges in supine position ▪ Radiology Findings ▪ CTV and MRI/V to evaluate vascular components and anatomy ▪ DSA found superior to determine flow dynamics ▪ Treatment ▪ Classic teaching is that dominant sinus pericranii should not be treated, while accessory sinus pericranii can be safely obliterated ▪ However, performing catheter angiography while the lesion is temporarily obliterated by external compression can help determine resectability based on the drainage pathway of the venous sinuses Neurodermatoradiology
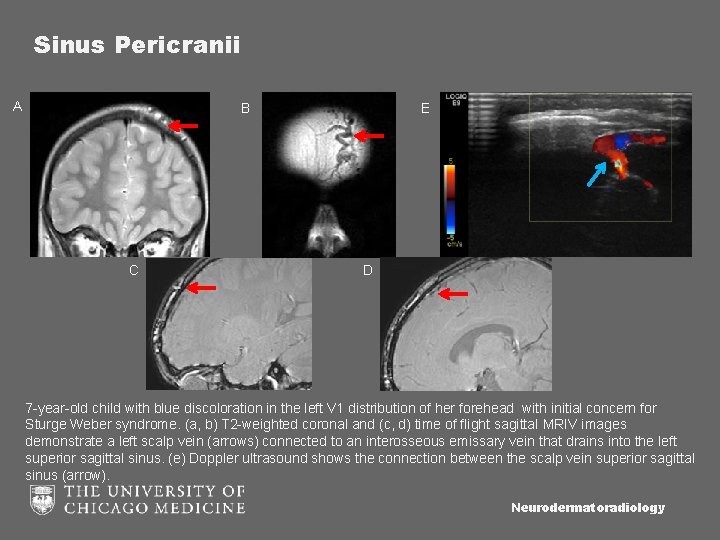
Sinus Pericranii A B C E D 7 -year-old child with blue discoloration in the left V 1 distribution of her forehead with initial concern for Sturge Weber syndrome. (a, b) T 2 -weighted coronal and (c, d) time of flight sagittal MRIV images demonstrate a left scalp vein (arrows) connected to an interosseous emissary vein that drains into the left superior sagittal sinus. (e) Doppler ultrasound shows the connection between the scalp vein superior sagittal sinus (arrow). Neurodermatoradiology
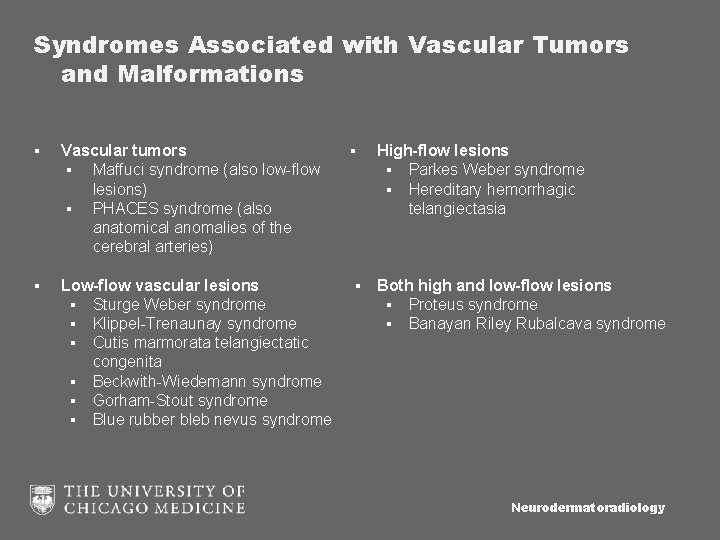
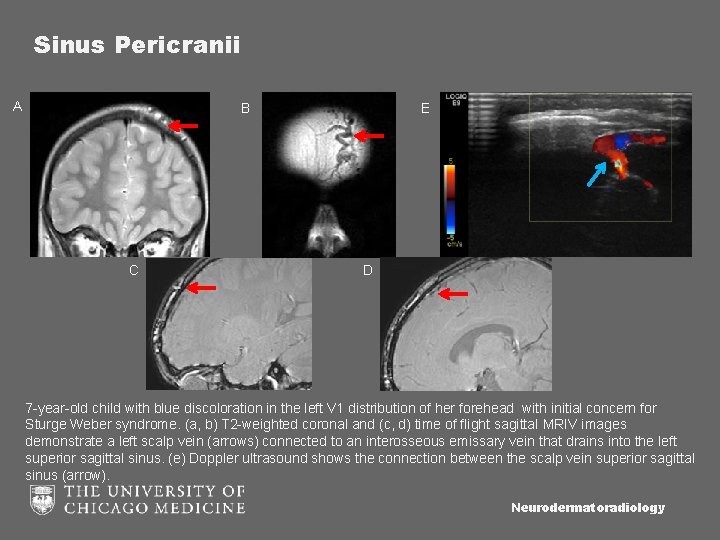
Syndromes Associated with Vascular Tumors and Malformations ▪ Vascular tumors ▪ Maffuci syndrome (also low-flow lesions) ▪ PHACES syndrome (also anatomical anomalies of the cerebral arteries) ▪ High-flow lesions ▪ Parkes Weber syndrome ▪ Hereditary hemorrhagic telangiectasia ▪ Low-flow vascular lesions ▪ Sturge Weber syndrome ▪ Klippel-Trenaunay syndrome ▪ Cutis marmorata telangiectatic congenita ▪ Beckwith-Wiedemann syndrome ▪ Gorham-Stout syndrome ▪ Blue rubber bleb nevus syndrome ▪ Both high and low-flow lesions ▪ Proteus syndrome ▪ Banayan Riley Rubalcava syndrome Neurodermatoradiology
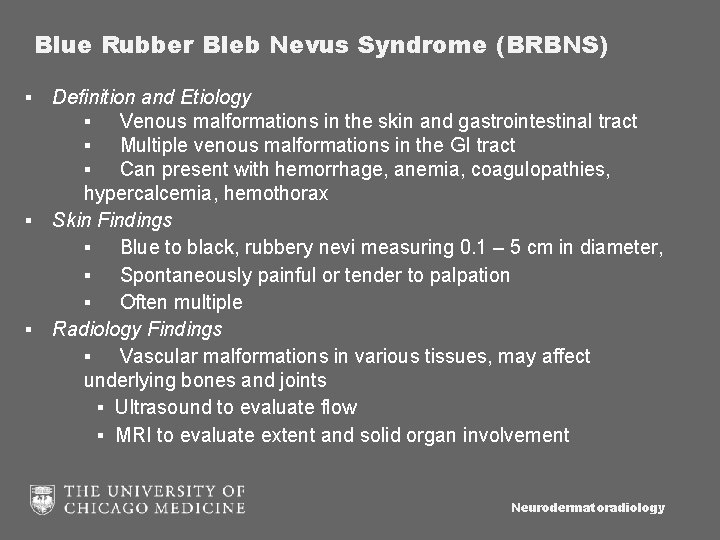
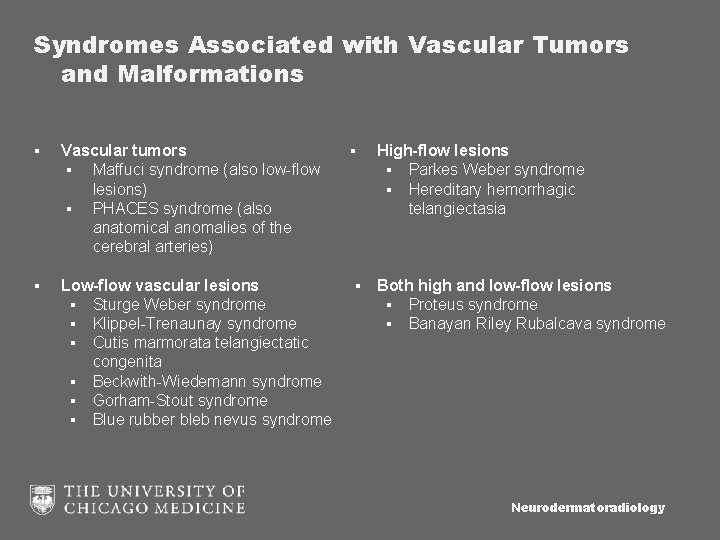
Blue Rubber Bleb Nevus Syndrome (BRBNS) ▪ Definition and Etiology ▪ Venous malformations in the skin and gastrointestinal tract ▪ Multiple venous malformations in the GI tract ▪ Can present with hemorrhage, anemia, coagulopathies, hypercalcemia, hemothorax ▪ Skin Findings ▪ Blue to black, rubbery nevi measuring 0. 1 – 5 cm in diameter, ▪ Spontaneously painful or tender to palpation ▪ Often multiple ▪ Radiology Findings ▪ Vascular malformations in various tissues, may affect underlying bones and joints ▪ Ultrasound to evaluate flow ▪ MRI to evaluate extent and solid organ involvement Neurodermatoradiology

Blue Rubber Bleb Nevus Syndrome (BRBNS) A B C Courtesy of V Petronic-Rosic, MD (a) Photograph of a patient with BRBNS demonstrates numerous dark nevi in the forearm. (b) Axial T 2 weighted image of numerous T 2 -hyperintense subcutaneous , intramuscular, and thyroidal vascular malformations in the chest. (c) Post-contrast axial T 1 images demonstrate enhancement of the venous malformations. Neurodermatoradiology
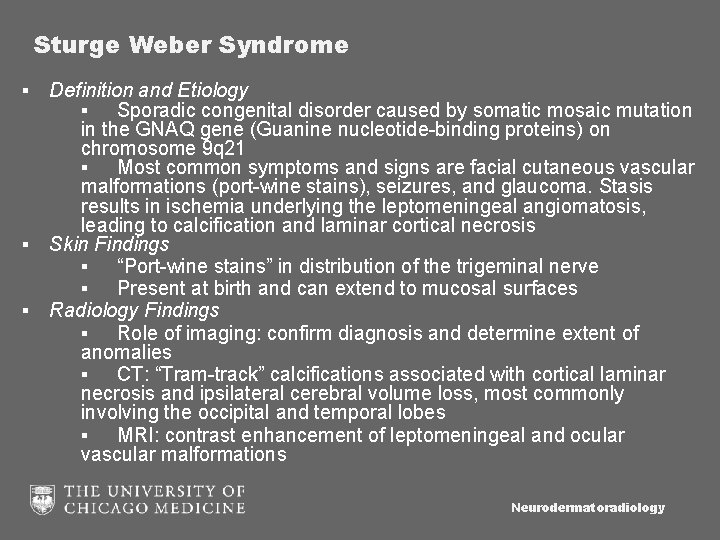
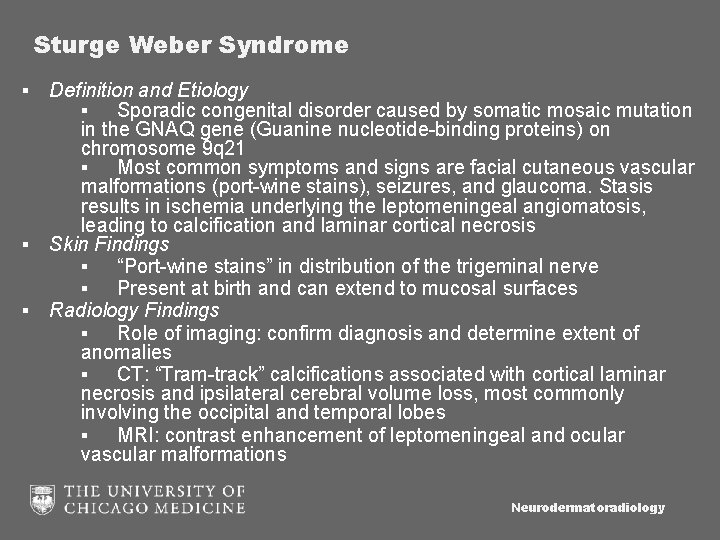
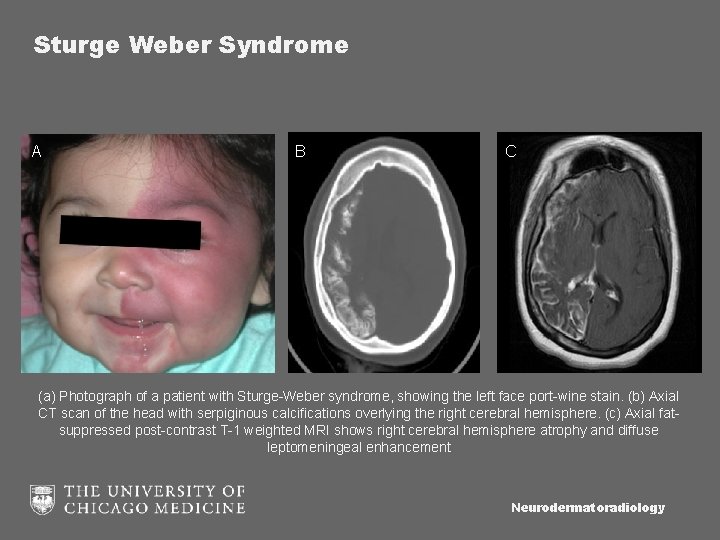
Sturge Weber Syndrome ▪ Definition and Etiology ▪ Sporadic congenital disorder caused by somatic mosaic mutation in the GNAQ gene (Guanine nucleotide-binding proteins) on chromosome 9 q 21 ▪ Most common symptoms and signs are facial cutaneous vascular malformations (port-wine stains), seizures, and glaucoma. Stasis results in ischemia underlying the leptomeningeal angiomatosis, leading to calcification and laminar cortical necrosis ▪ Skin Findings ▪ “Port-wine stains” in distribution of the trigeminal nerve ▪ Present at birth and can extend to mucosal surfaces ▪ Radiology Findings ▪ Role of imaging: confirm diagnosis and determine extent of anomalies ▪ CT: “Tram-track” calcifications associated with cortical laminar necrosis and ipsilateral cerebral volume loss, most commonly involving the occipital and temporal lobes ▪ MRI: contrast enhancement of leptomeningeal and ocular vascular malformations Neurodermatoradiology
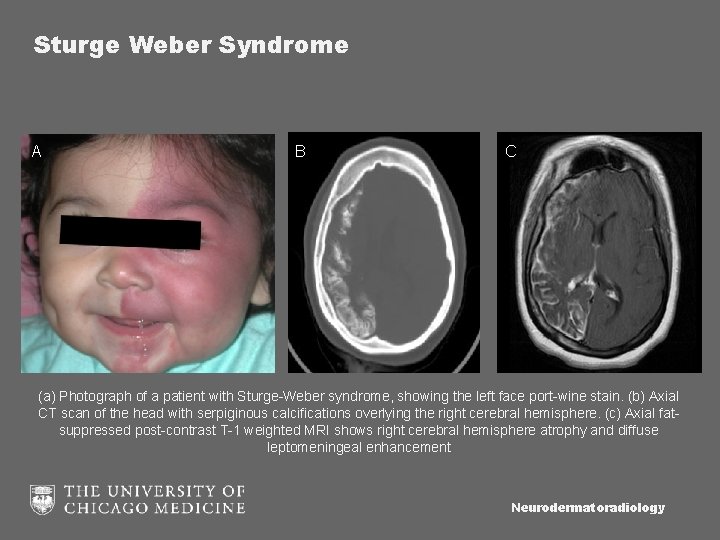
Sturge Weber Syndrome A B C (a) Photograph of a patient with Sturge-Weber syndrome, showing the left face port-wine stain. (b) Axial CT scan of the head with serpiginous calcifications overlying the right cerebral hemisphere. (c) Axial fatsuppressed post-contrast T-1 weighted MRI shows right cerebral hemisphere atrophy and diffuse leptomeningeal enhancement Neurodermatoradiology
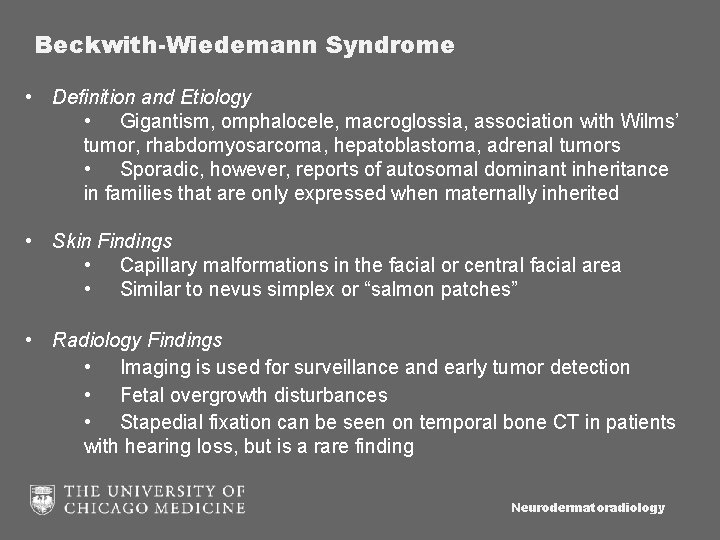
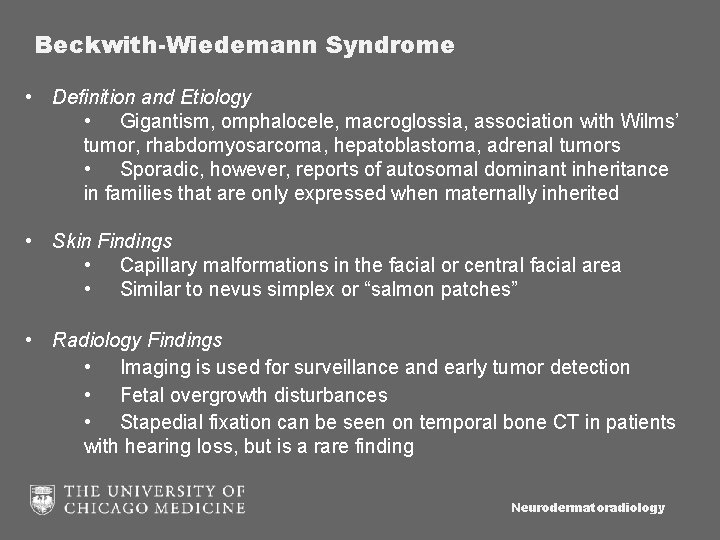
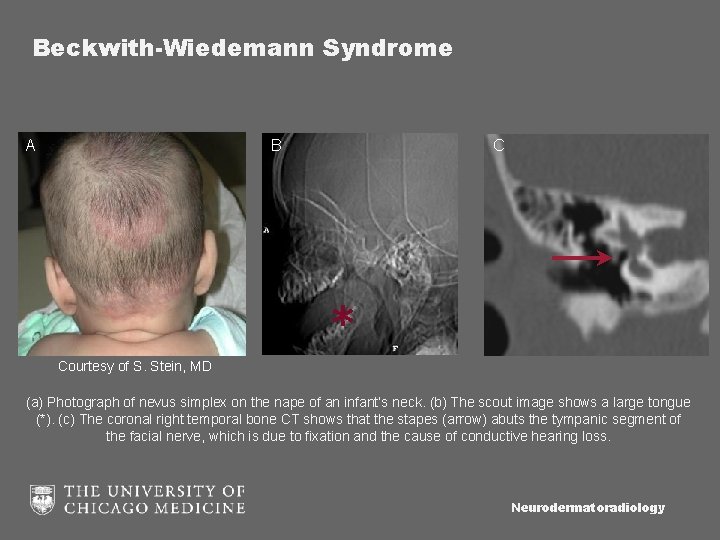
Beckwith-Wiedemann Syndrome • Definition and Etiology • Gigantism, omphalocele, macroglossia, association with Wilms’ tumor, rhabdomyosarcoma, hepatoblastoma, adrenal tumors • Sporadic, however, reports of autosomal dominant inheritance in families that are only expressed when maternally inherited • Skin Findings • Capillary malformations in the facial or central facial area • Similar to nevus simplex or “salmon patches” • Radiology Findings • Imaging is used for surveillance and early tumor detection • Fetal overgrowth disturbances • Stapedial fixation can be seen on temporal bone CT in patients with hearing loss, but is a rare finding Neurodermatoradiology
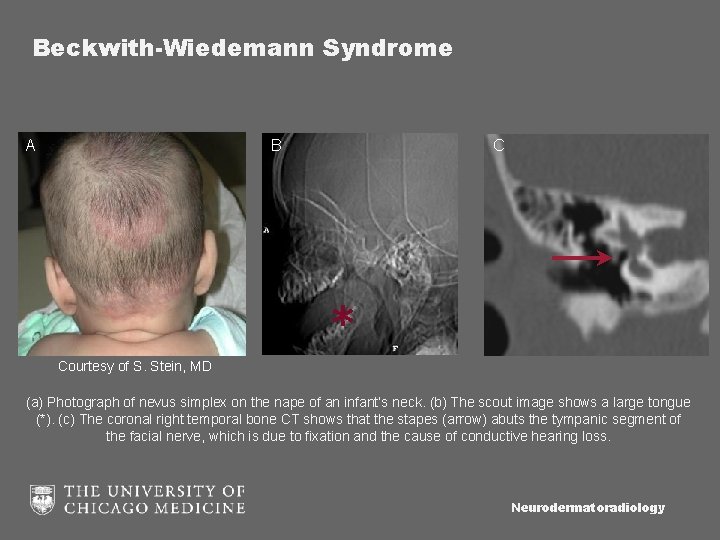
Beckwith-Wiedemann Syndrome A B Courtesy of S. Stein, MD C * (a) Photograph of nevus simplex on the nape of an infant’s neck. (b) The scout image shows a large tongue (*). (c) The coronal right temporal bone CT shows that the stapes (arrow) abuts the tympanic segment of the facial nerve, which is due to fixation and the cause of conductive hearing loss. Neurodermatoradiology
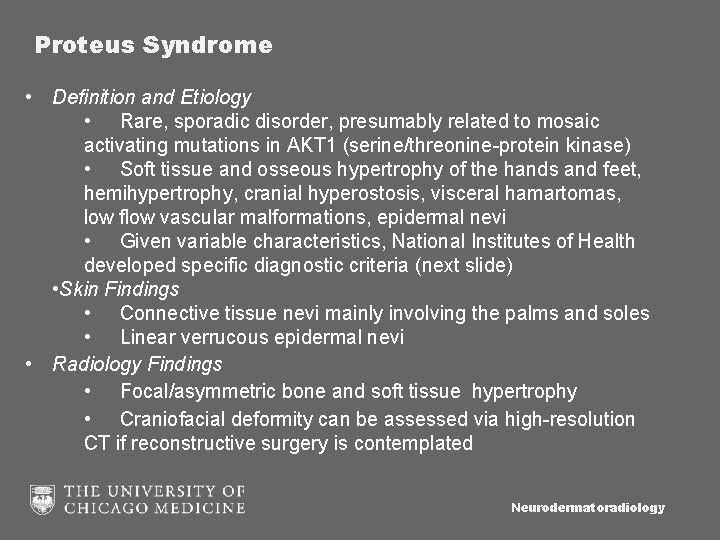
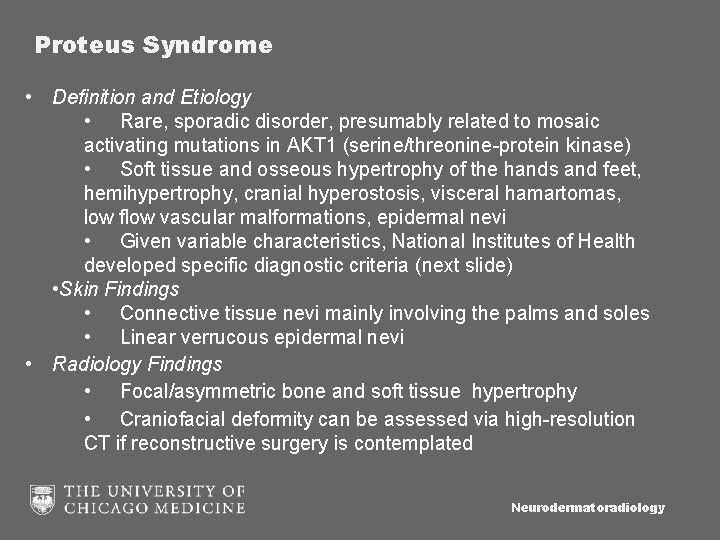
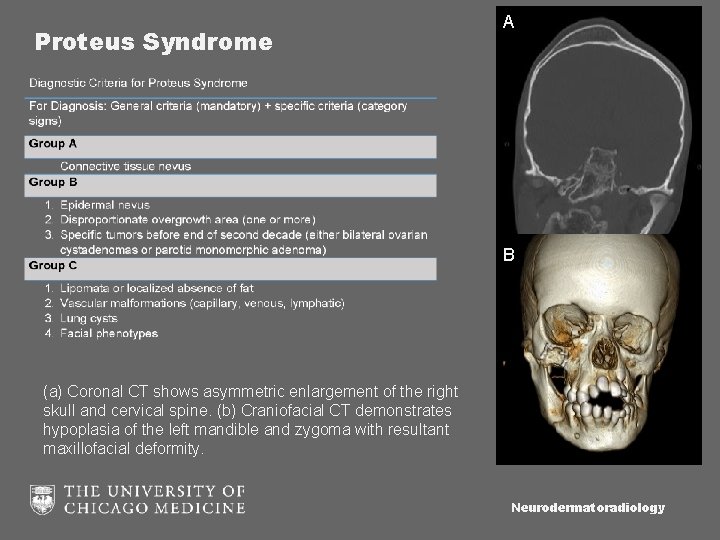
Proteus Syndrome • Definition and Etiology • Rare, sporadic disorder, presumably related to mosaic activating mutations in AKT 1 (serine/threonine-protein kinase) • Soft tissue and osseous hypertrophy of the hands and feet, hemihypertrophy, cranial hyperostosis, visceral hamartomas, low flow vascular malformations, epidermal nevi • Given variable characteristics, National Institutes of Health developed specific diagnostic criteria (next slide) • Skin Findings • Connective tissue nevi mainly involving the palms and soles • Linear verrucous epidermal nevi • Radiology Findings • Focal/asymmetric bone and soft tissue hypertrophy • Craniofacial deformity can be assessed via high-resolution CT if reconstructive surgery is contemplated Neurodermatoradiology
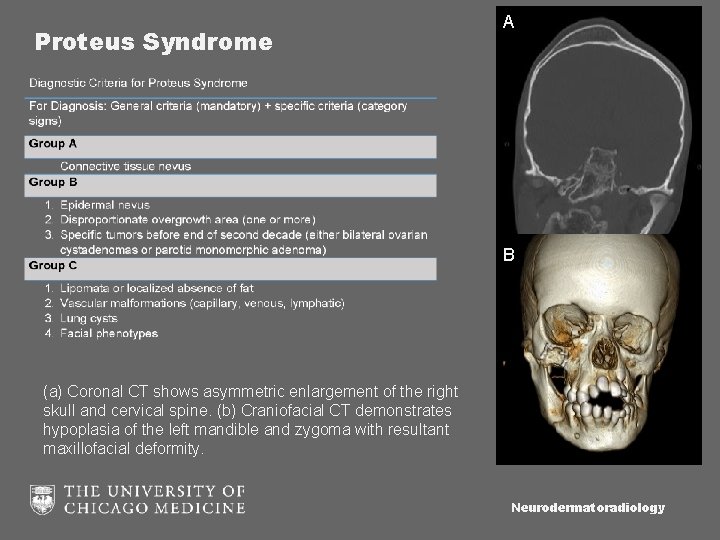
Proteus Syndrome A B (a) Coronal CT shows asymmetric enlargement of the right skull and cervical spine. (b) Craniofacial CT demonstrates hypoplasia of the left mandible and zygoma with resultant maxillofacial deformity. Neurodermatoradiology
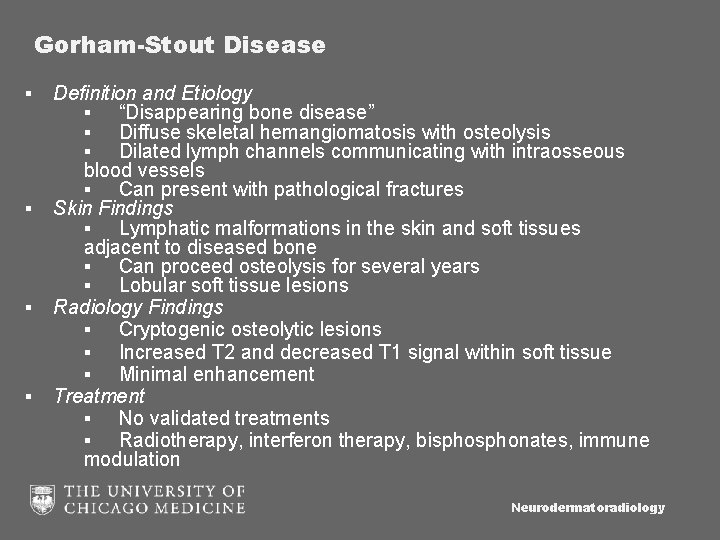
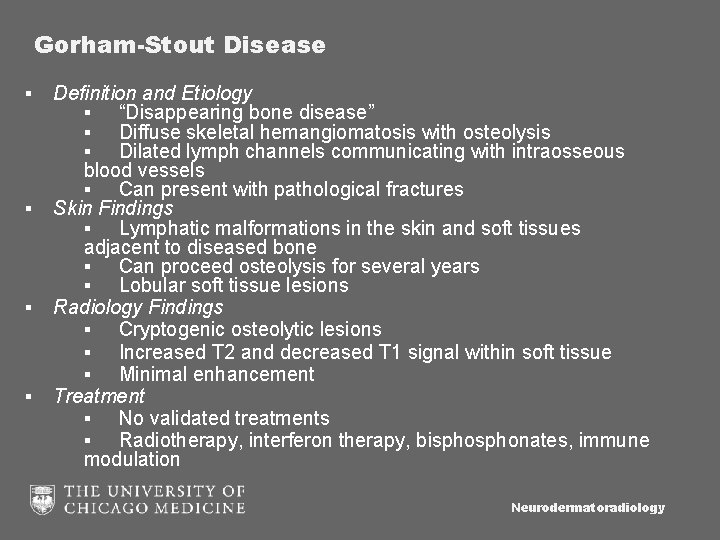
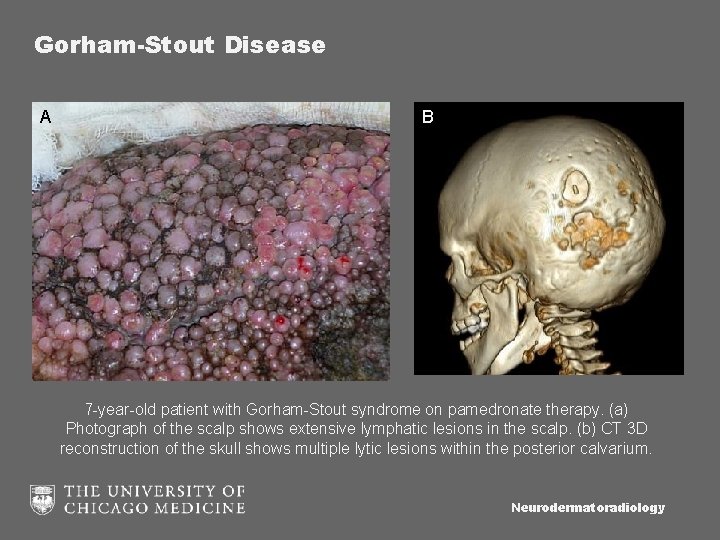
Gorham-Stout Disease ▪ ▪ Definition and Etiology ▪ “Disappearing bone disease” ▪ Diffuse skeletal hemangiomatosis with osteolysis ▪ Dilated lymph channels communicating with intraosseous blood vessels ▪ Can present with pathological fractures Skin Findings ▪ Lymphatic malformations in the skin and soft tissues adjacent to diseased bone ▪ Can proceed osteolysis for several years ▪ Lobular soft tissue lesions Radiology Findings ▪ Cryptogenic osteolytic lesions ▪ Increased T 2 and decreased T 1 signal within soft tissue ▪ Minimal enhancement Treatment ▪ No validated treatments ▪ Radiotherapy, interferon therapy, bisphonates, immune modulation Neurodermatoradiology
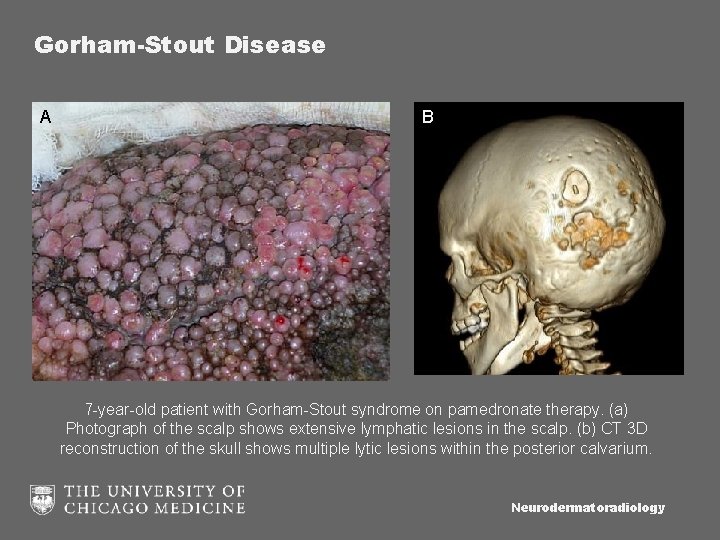
Gorham-Stout Disease A B 7 -year-old patient with Gorham-Stout syndrome on pamedronate therapy. (a) Photograph of the scalp shows extensive lymphatic lesions in the scalp. (b) CT 3 D reconstruction of the skull shows multiple lytic lesions within the posterior calvarium. Neurodermatoradiology
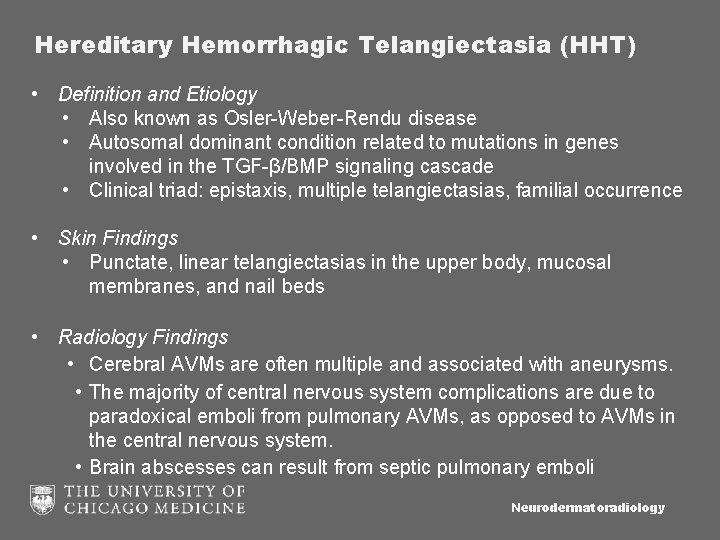
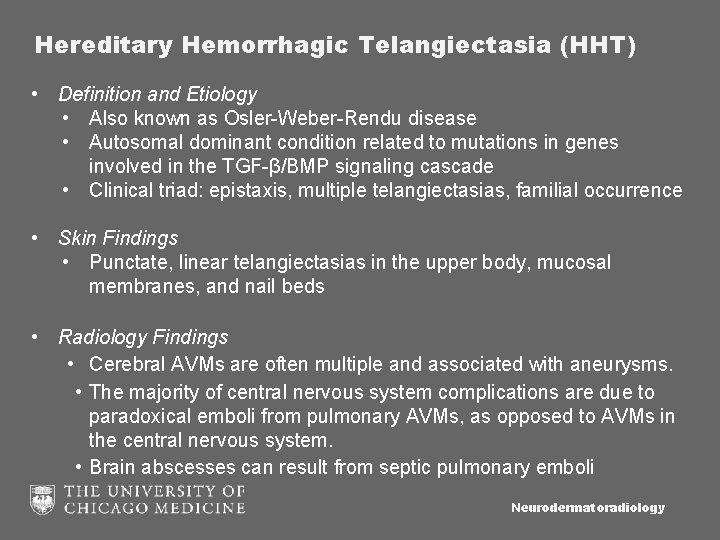
Hereditary Hemorrhagic Telangiectasia (HHT) • Definition and Etiology • Also known as Osler-Weber-Rendu disease • Autosomal dominant condition related to mutations in genes involved in the TGF-β/BMP signaling cascade • Clinical triad: epistaxis, multiple telangiectasias, familial occurrence • Skin Findings • Punctate, linear telangiectasias in the upper body, mucosal membranes, and nail beds • Radiology Findings • Cerebral AVMs are often multiple and associated with aneurysms. • The majority of central nervous system complications are due to paradoxical emboli from pulmonary AVMs, as opposed to AVMs in the central nervous system. • Brain abscesses can result from septic pulmonary emboli Neurodermatoradiology
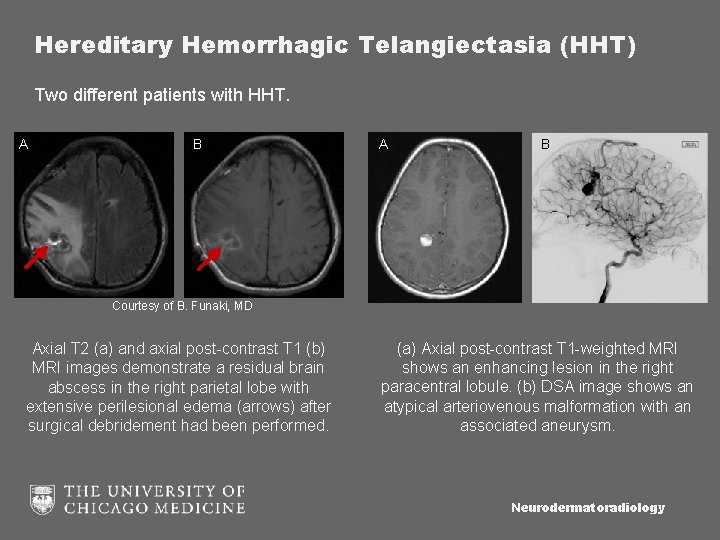
Hereditary Hemorrhagic Telangiectasia (HHT) Two different patients with HHT. A B Courtesy of B. Funaki, MD Axial T 2 (a) and axial post-contrast T 1 (b) MRI images demonstrate a residual brain abscess in the right parietal lobe with extensive perilesional edema (arrows) after surgical debridement had been performed. (a) Axial post-contrast T 1 -weighted MRI shows an enhancing lesion in the right paracentral lobule. (b) DSA image shows an atypical arteriovenous malformation with an associated aneurysm. Neurodermatoradiology
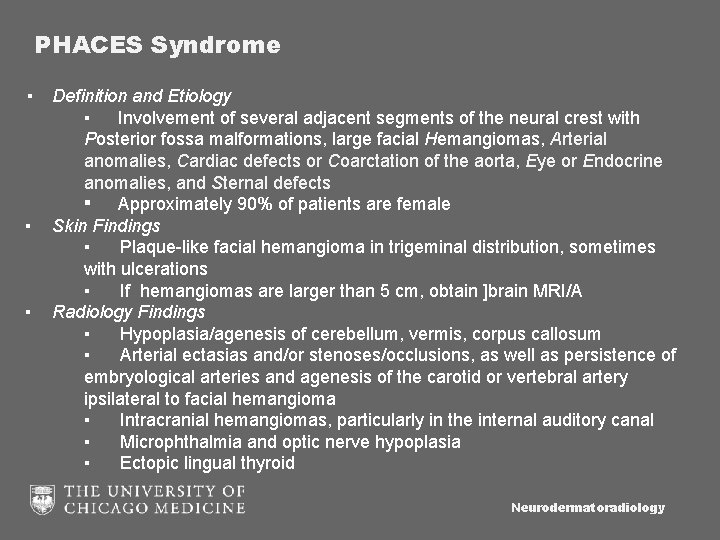
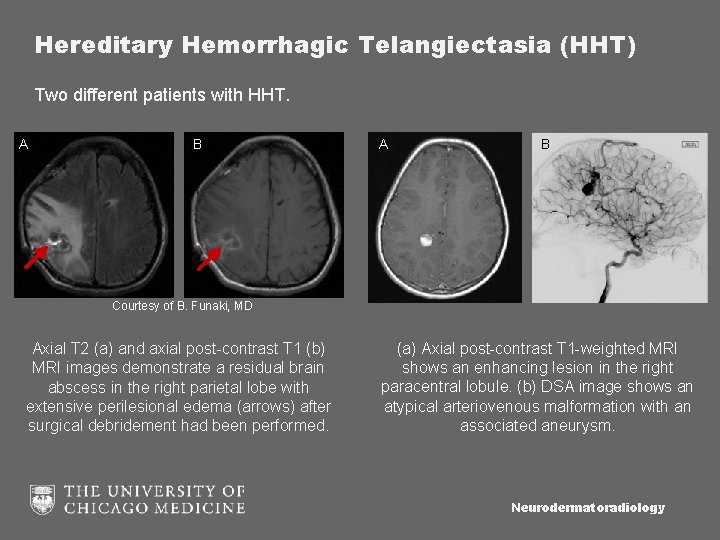
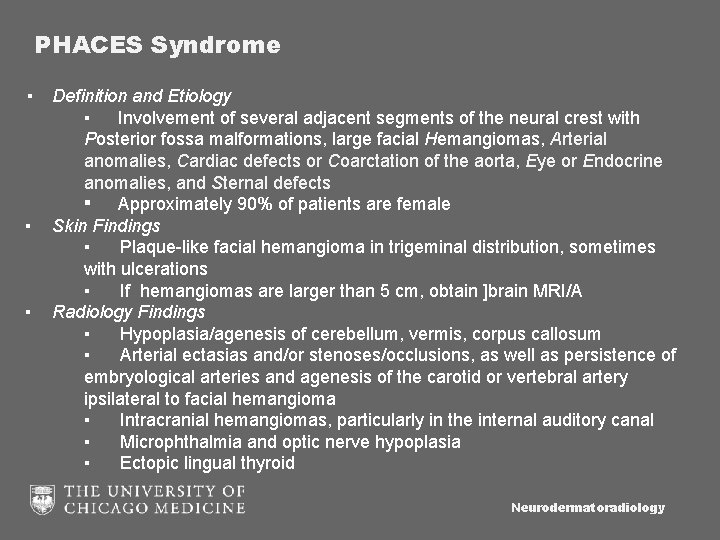
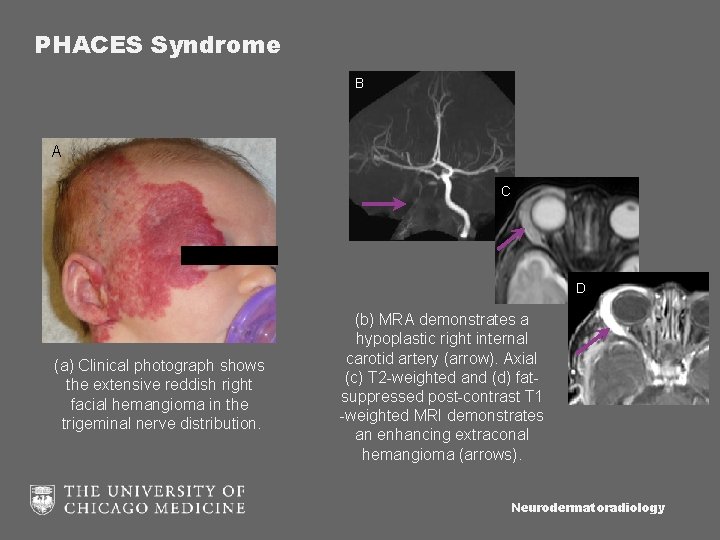
PHACES Syndrome ▪ ▪ ▪ Definition and Etiology ▪ Involvement of several adjacent segments of the neural crest with Posterior fossa malformations, large facial Hemangiomas, Arterial anomalies, Cardiac defects or Coarctation of the aorta, Eye or Endocrine anomalies, and Sternal defects ▪ Approximately 90% of patients are female Skin Findings ▪ Plaque-like facial hemangioma in trigeminal distribution, sometimes with ulcerations ▪ If hemangiomas are larger than 5 cm, obtain ]brain MRI/A Radiology Findings ▪ Hypoplasia/agenesis of cerebellum, vermis, corpus callosum ▪ Arterial ectasias and/or stenoses/occlusions, as well as persistence of embryological arteries and agenesis of the carotid or vertebral artery ipsilateral to facial hemangioma ▪ Intracranial hemangiomas, particularly in the internal auditory canal ▪ Microphthalmia and optic nerve hypoplasia ▪ Ectopic lingual thyroid Neurodermatoradiology
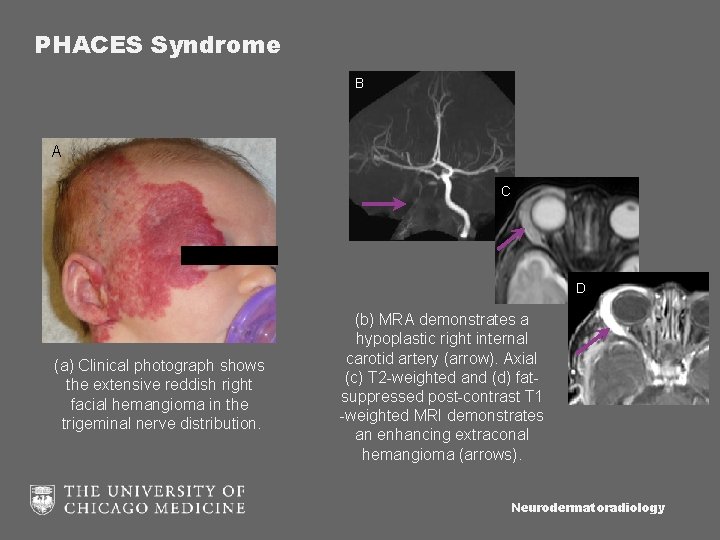
PHACES Syndrome B A C D (a) Clinical photograph shows the extensive reddish right facial hemangioma in the trigeminal nerve distribution. (b) MRA demonstrates a hypoplastic right internal carotid artery (arrow). Axial (c) T 2 -weighted and (d) fatsuppressed post-contrast T 1 -weighted MRI demonstrates an enhancing extraconal hemangioma (arrows). Neurodermatoradiology
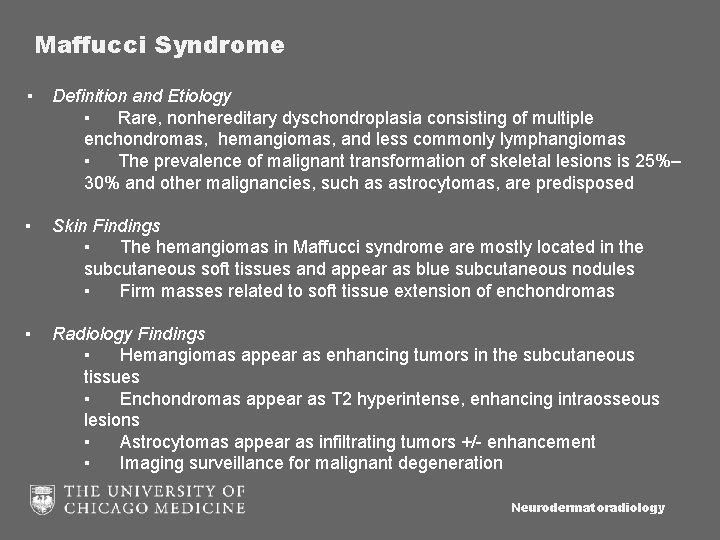
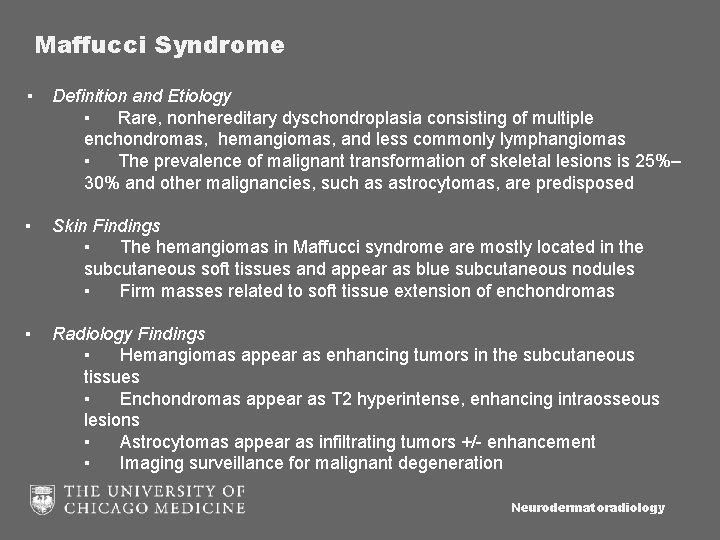
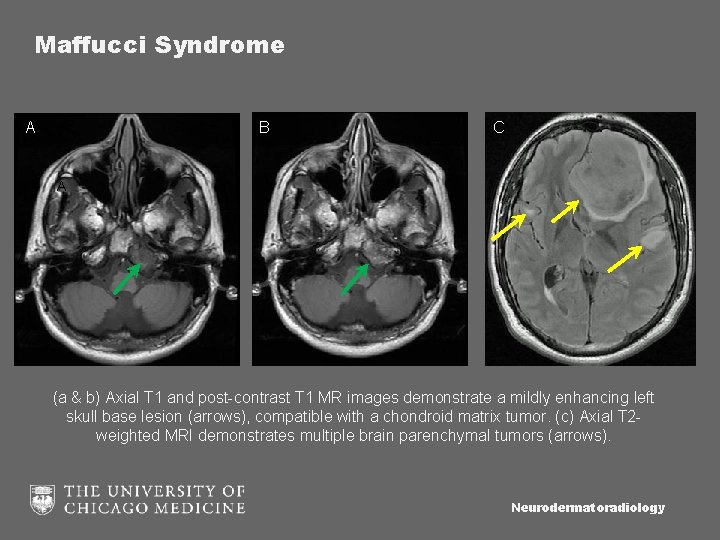
Maffucci Syndrome ▪ Definition and Etiology ▪ Rare, nonhereditary dyschondroplasia consisting of multiple enchondromas, hemangiomas, and less commonly lymphangiomas ▪ The prevalence of malignant transformation of skeletal lesions is 25%– 30% and other malignancies, such as astrocytomas, are predisposed ▪ Skin Findings ▪ The hemangiomas in Maffucci syndrome are mostly located in the subcutaneous soft tissues and appear as blue subcutaneous nodules ▪ Firm masses related to soft tissue extension of enchondromas ▪ Radiology Findings ▪ Hemangiomas appear as enhancing tumors in the subcutaneous tissues ▪ Enchondromas appear as T 2 hyperintense, enhancing intraosseous lesions ▪ Astrocytomas appear as infiltrating tumors +/- enhancement ▪ Imaging surveillance for malignant degeneration Neurodermatoradiology
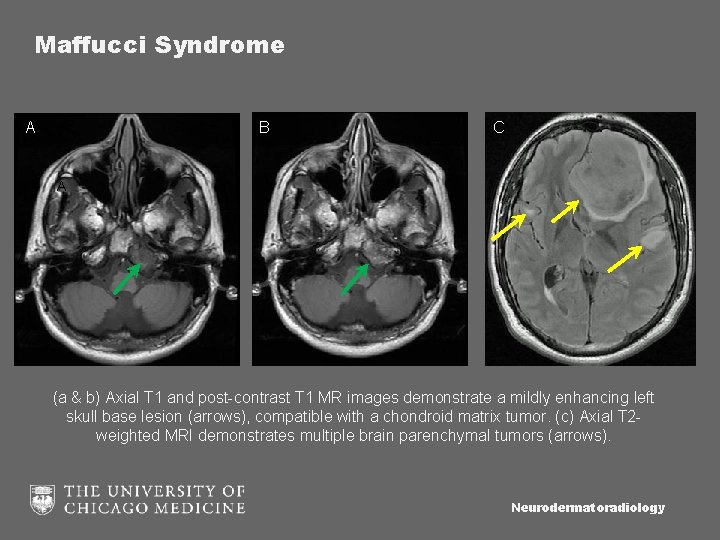
Maffucci Syndrome A B C A (a & b) Axial T 1 and post-contrast T 1 MR images demonstrate a mildly enhancing left skull base lesion (arrows), compatible with a chondroid matrix tumor. (c) Axial T 2 weighted MRI demonstrates multiple brain parenchymal tumors (arrows). Neurodermatoradiology
![References 1 LeauteLabreze C Propranolol in infantile hemangiomas Arch Pediatr 2015 224 452 5 References 1. Leaute-Labreze C. [Propranolol in infantile hemangiomas]. Arch Pediatr. 2015; 22(4): 452 -5.](https://slidetodoc.com/presentation_image_h/16f17245c861520001da41c8f229d36d/image-40.jpg)
References 1. Leaute-Labreze C. [Propranolol in infantile hemangiomas]. Arch Pediatr. 2015; 22(4): 452 -5. 2. Dubois J, Alison M. Vascular anomalies: what a radiologist needs to know. Pediatr Radiol. 2010; 40(6): 895 -905. 3. Flors L, Leiva-Salinas C, Maged IM, et al. MR imaging of soft-tissue vascular malformations: diagnosis, classification, and therapy follow-up. Radiographics. United States 2011; p. 1321 -40; discussion 40 -1. 4. Nozaki T, et al. Syndromes associated with vascular tumors and malformations: a pictoral review. Radiographics. 2013; 33(1): 175 -195 5. Kumar MS, Kumar MH, Sivakumar V, Kumar SH. A diagnostic challenge: pyogenic granuloma or oral focal mucinosis. BMJ Case Rep. 2015; 2015. 6. Lee DG, Lee SK, Chang HW, et al. CT features of lobular capillary hemangioma of the nasal cavity. AJNR Am J Neuroradiol. 2010; 31(4): 749 -54. 7. Navarro OM, Laffan EE, Ngan BY. Pediatric soft-tissue tumors and pseudo-tumors: MR imaging features with pathologic correlation: part 1. Imaging approach, pseudotumors, vascular lesions, and adipocytic tumors. Radiographics. United States 2009; p. 887 -906. 8. Moake JL. Thrombotic microangiopathies. N Engl J Med. United States 2002; p. 589 -600. 9. Buonanno FS, Cooper MR, Moody DM, Laster DW, Ball MR, Toole JF. Neuroradiologic aspects of cerebral disseminated intravascular coagulation. AJNR Am J Neuroradiol. 1980; 1(3): 245 -50. Neurodermatoradiology