Neurobehavioral Disorders Characterization Management Downs Syndrome Association October
Neurobehavioral Disorders: Characterization & Management Down’s Syndrome Association October 2006 George T Capone, M. D. Kennedy Krieger Institute
The Challenge of Trisomy 21
Neurobehavioral Disorders Overview Typical, learned behavior or neurobehavior disorder? Medical considerations When to consider medication management Other treatments Disruptive disorders spectrum - ADHD, ODD, DBD Repetitive movements - SMD Autism spectrum - ASD
Down Syndrome & Behavior Concerns Most children with DS (75 -85%) do NOT have a coexisting neurobehavioral disorder Some children with DS (~15 -25%) do have a significant neurobehavioral disorder Many parents of children with DS have real behavioral concerns Age-, stage-specific behaviors; transient or persistent behaviors ? Learned behaviors or complex neurobehavioral symptomatology ?
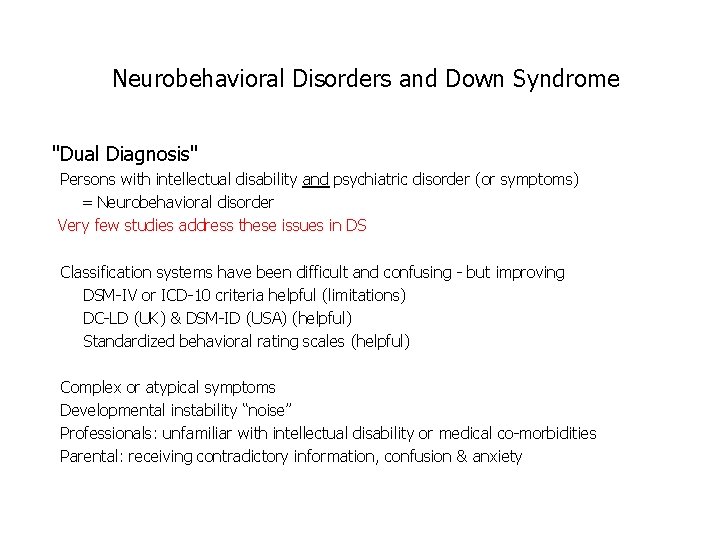
Neurobehavioral Disorders and Down Syndrome "Dual Diagnosis" Persons with intellectual disability and psychiatric disorder (or symptoms) = Neurobehavioral disorder Very few studies address these issues in DS Classification systems have been difficult and confusing - but improving DSM-IV or ICD-10 criteria helpful (limitations) DC-LD (UK) & DSM-ID (USA) (helpful) Standardized behavioral rating scales (helpful) Complex or atypical symptoms Developmental instability “noise” Professionals: unfamiliar with intellectual disability or medical co-morbidities Parental: receiving contradictory information, confusion & anxiety
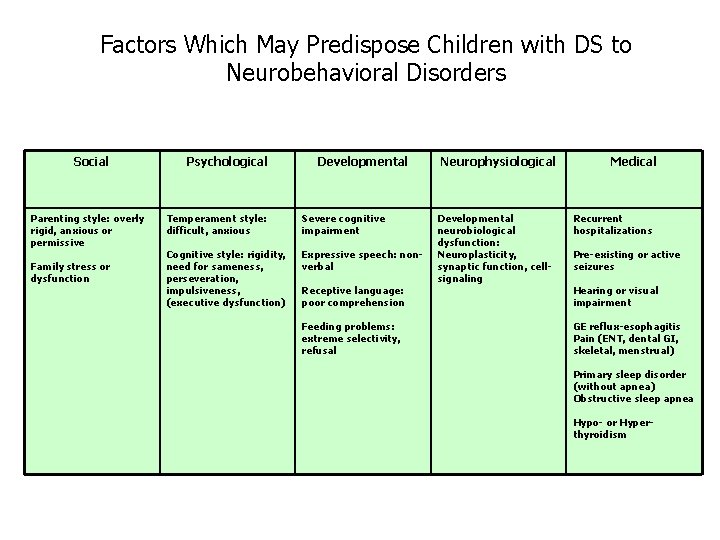
Factors Which May Predispose Children with DS to Neurobehavioral Disorders Social Parenting style: overly rigid, anxious or permissive Family stress or dysfunction Psychological Developmental Temperament style: difficult, anxious Severe cognitive impairment Cognitive style: rigidity, need for sameness, perseveration, impulsiveness, (executive dysfunction) Expressive speech: nonverbal Receptive language: poor comprehension Feeding problems: extreme selectivity, refusal Neurophysiological Developmental neurobiological dysfunction: Neuroplasticity, synaptic function, cellsignaling Medical Recurrent hospitalizations Pre-existing or active seizures Hearing or visual impairment GE reflux-esophagitis Pain (ENT, dental GI, skeletal, menstrual) Primary sleep disorder (without apnea) Obstructive sleep apnea Hypo- or Hyperthyroidism
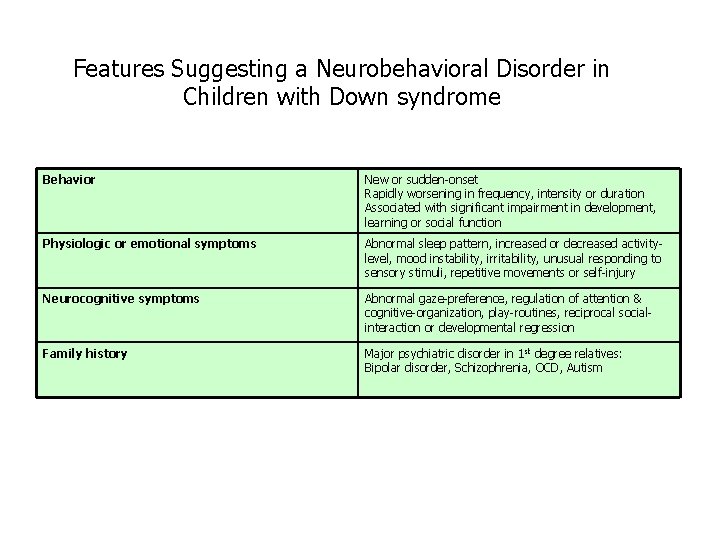
Features Suggesting a Neurobehavioral Disorder in Children with Down syndrome Behavior New or sudden-onset Rapidly worsening in frequency, intensity or duration Associated with significant impairment in development, learning or social function Physiologic or emotional symptoms Abnormal sleep pattern, increased or decreased activitylevel, mood instability, irritability, unusual responding to sensory stimuli, repetitive movements or self-injury Neurocognitive symptoms Abnormal gaze-preference, regulation of attention & cognitive-organization, play-routines, reciprocal socialinteraction or developmental regression Family history Major psychiatric disorder in 1 st degree relatives: Bipolar disorder, Schizophrenia, OCD, Autism
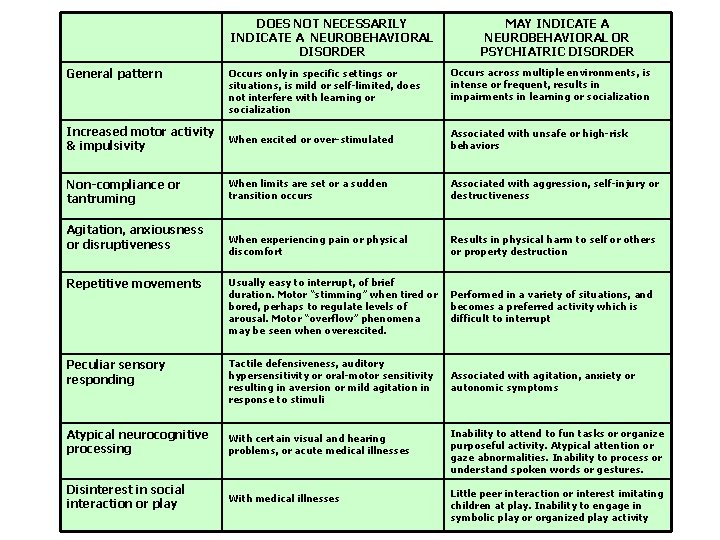
DOES NOT NECESSARILY INDICATE A NEUROBEHAVIORAL DISORDER General pattern Occurs only in specific settings or situations, is mild or self-limited, does not interfere with learning or socialization MAY INDICATE A NEUROBEHAVIORAL OR PSYCHIATRIC DISORDER Occurs across multiple environments, is intense or frequent, results in impairments in learning or socialization Increased motor activity & impulsivity When excited or over-stimulated Associated with unsafe or high-risk behaviors Non-compliance or tantruming When limits are set or a sudden transition occurs Associated with aggression, self-injury or destructiveness When experiencing pain or physical discomfort Results in physical harm to self or others or property destruction Repetitive movements Usually easy to interrupt, of brief duration. Motor “stimming” when tired or bored, perhaps to regulate levels of arousal. Motor “overflow” phenomena may be seen when overexcited. Performed in a variety of situations, and becomes a preferred activity which is difficult to interrupt Peculiar sensory responding Tactile defensiveness, auditory hypersensitivity or oral-motor sensitivity resulting in aversion or mild agitation in response to stimuli Associated with agitation, anxiety or autonomic symptoms Atypical neurocognitive processing With certain visual and hearing problems, or acute medical illnesses Inability to attend to fun tasks or organize purposeful activity. Atypical attention or gaze abnormalities. Inability to process or understand spoken words or gestures. Disinterest in social interaction or play With medical illnesses Little peer interaction or interest imitating children at play. Inability to engage in symbolic play or organized play activity Agitation, anxiousness or disruptiveness
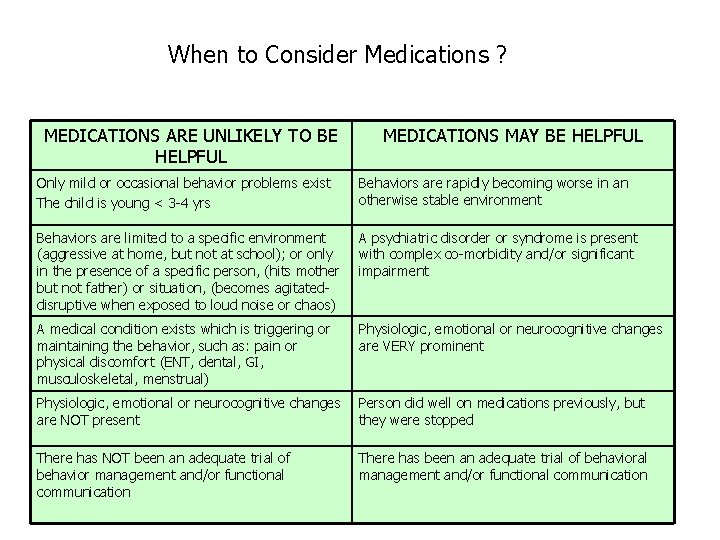
When to Consider Medications ? MEDICATIONS ARE UNLIKELY TO BE HELPFUL MEDICATIONS MAY BE HELPFUL Only mild or occasional behavior problems exist The child is young < 3 -4 yrs Behaviors are rapidly becoming worse in an otherwise stable environment Behaviors are limited to a specific environment (aggressive at home, but not at school); or only in the presence of a specific person, (hits mother but not father) or situation, (becomes agitateddisruptive when exposed to loud noise or chaos) A psychiatric disorder or syndrome is present with complex co-morbidity and/or significant impairment A medical condition exists which is triggering or maintaining the behavior, such as: pain or physical discomfort (ENT, dental, GI, musculoskeletal, menstrual) Physiologic, emotional or neurocognitive changes are VERY prominent Physiologic, emotional or neurocognitive changes are NOT present Person did well on medications previously, but they were stopped There has NOT been an adequate trial of behavior management and/or functional communication There has been an adequate trial of behavioral management and/or functional communication
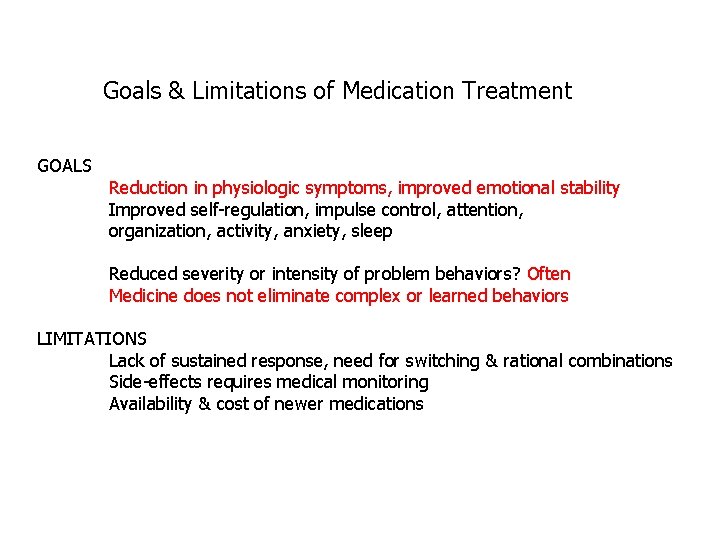
Goals & Limitations of Medication Treatment GOALS Reduction in physiologic symptoms, improved emotional stability Improved self-regulation, impulse control, attention, organization, activity, anxiety, sleep Reduced severity or intensity of problem behaviors? Often Medicine does not eliminate complex or learned behaviors LIMITATIONS Lack of sustained response, need for switching & rational combinations Side-effects requires medical monitoring Availability & cost of newer medications
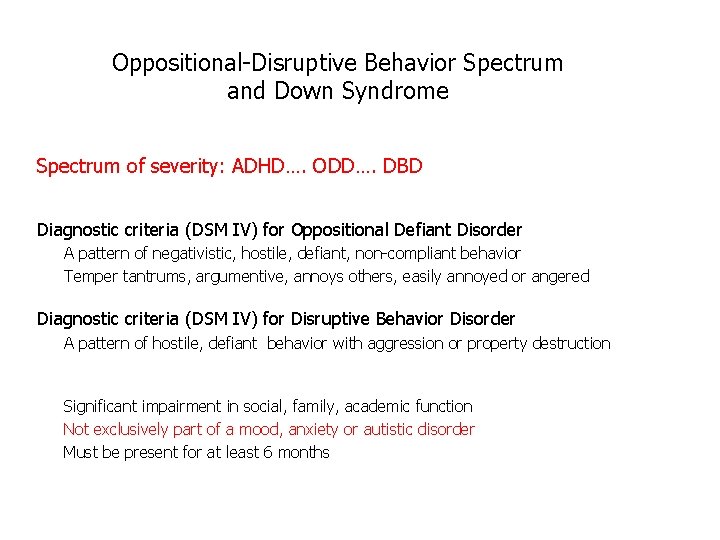
Oppositional-Disruptive Behavior Spectrum and Down Syndrome Spectrum of severity: ADHD…. ODD…. DBD Diagnostic criteria (DSM IV) for Oppositional Defiant Disorder A pattern of negativistic, hostile, defiant, non-compliant behavior Temper tantrums, argumentive, annoys others, easily annoyed or angered Diagnostic criteria (DSM IV) for Disruptive Behavior Disorder A pattern of hostile, defiant behavior with aggression or property destruction Significant impairment in social, family, academic function Not exclusively part of a mood, anxiety or autistic disorder Must be present for at least 6 months
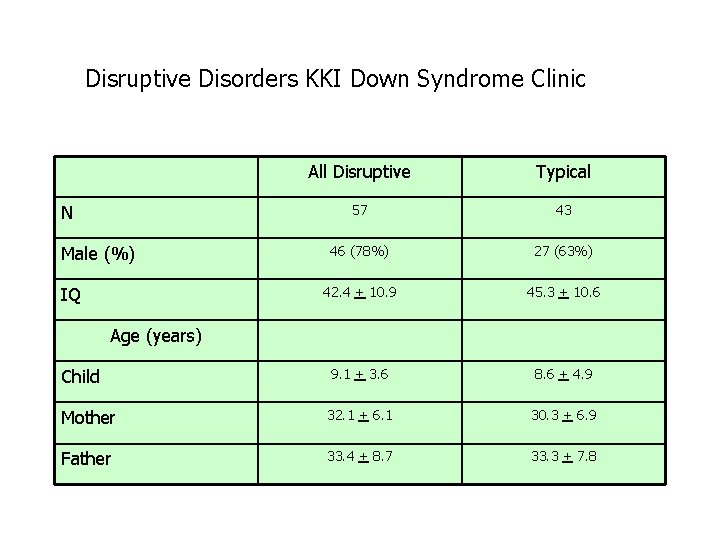
Disruptive Disorders KKI Down Syndrome Clinic All Disruptive Typical 57 43 46 (78%) 27 (63%) 42. 4 + 10. 9 45. 3 + 10. 6 Child 9. 1 + 3. 6 8. 6 + 4. 9 Mother 32. 1 + 6. 1 30. 3 + 6. 9 Father 33. 4 + 8. 7 33. 3 + 7. 8 N Male (%) IQ Age (years)
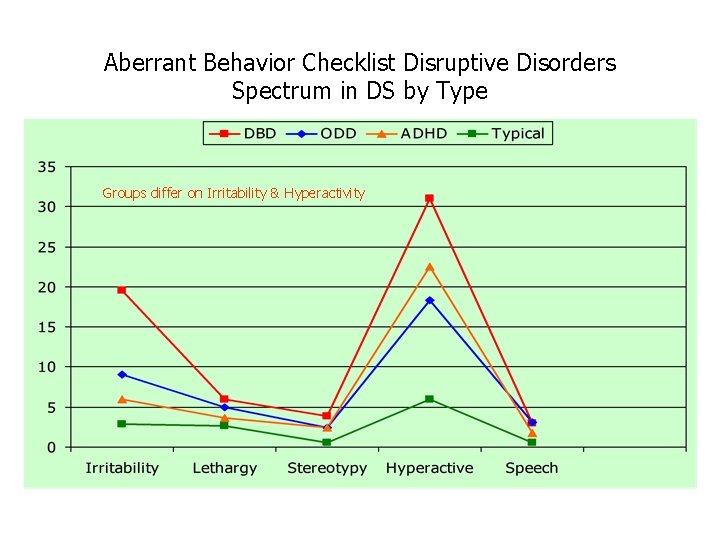
Aberrant Behavior Checklist Disruptive Disorders Spectrum in DS by Type Groups differ on Irritability & Hyperactivity
Disruptive Behavior Disorders Considerations Occult pain (sinuses, ears, gastric, dental) Sleep disturbance or apnea Underlying ADHD-impulsivity, anxiety or mood disorder Communication (expressive) skills Expectations at home and school Management style – transitions, requests, limit-setting Discipline Environment at home & school – lack of structure
Disruptive Behavior Disorders Treatments Safety monitoring- running, climbing, jumping Behavior management – RECOGNIZE the antecedents & triggers Medications – specific target symptoms Functional communication - augmentive communication device Environment – picture schedules Education of caretakers and teachers In home services – respite for families
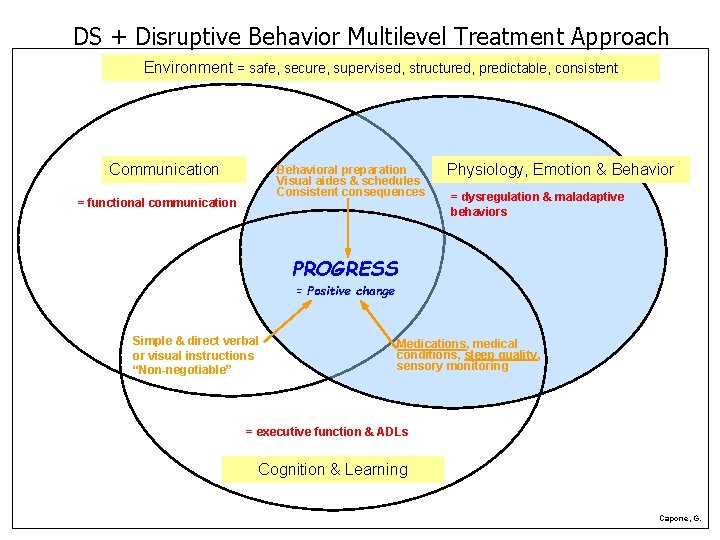
DS + Disruptive Behavior Multilevel Treatment Approach Environment = safe, secure, supervised, structured, predictable, consistent Communication Behavioral preparation Visual aides & schedules Consistent consequences = functional communication Physiology, Emotion & Behavior = dysregulation & maladaptive behaviors PROGRESS = Positive change Simple & direct verbal or visual instructions “Non-negotiable” Medications, medical conditions, sleep quality, sensory monitoring = executive function & ADLs Cognition & Learning Capone, G.
Guanfacine for Hyperactivity-Impulsivity Subjects = 15 (14 M, 1 F) Age = 7. 6 + 2. 0 yr Type: ADHD only=1, ADHD+ODD=4, ADHD+DBD=10 Cognition: moderate-severe MR Medication Dose = 1. 0 mg per day (divided AM + PM) Treatment period = 139 + 41 days
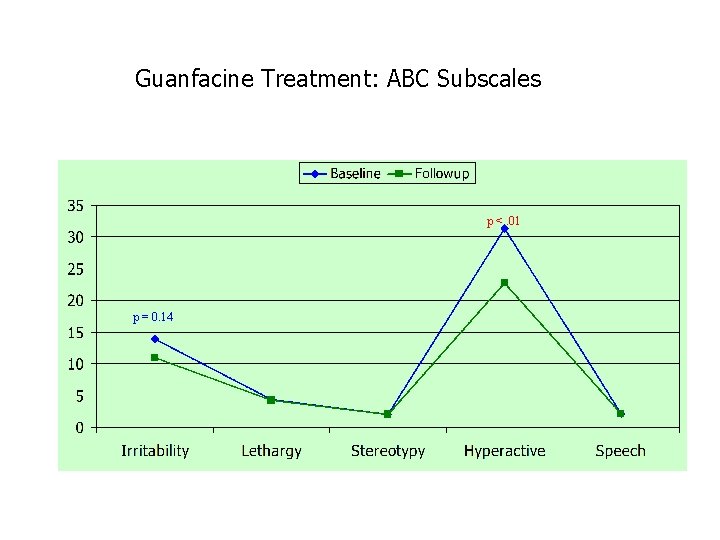
Guanfacine Treatment: ABC Subscales p <. 01 p = 0. 14
Executive Prefrontal Functions
Executive Prefrontal Functions Critical to the regulation of behavior and cognition Inhibition – the ability to stop or delay a first response or resist interference by distracting thoughts or stimuli Flexibility - the ability to shift and transition adaptively between activities or thoughts Emotional Control - the capacity to modify emotional expression and select the most adaptive response for the situation
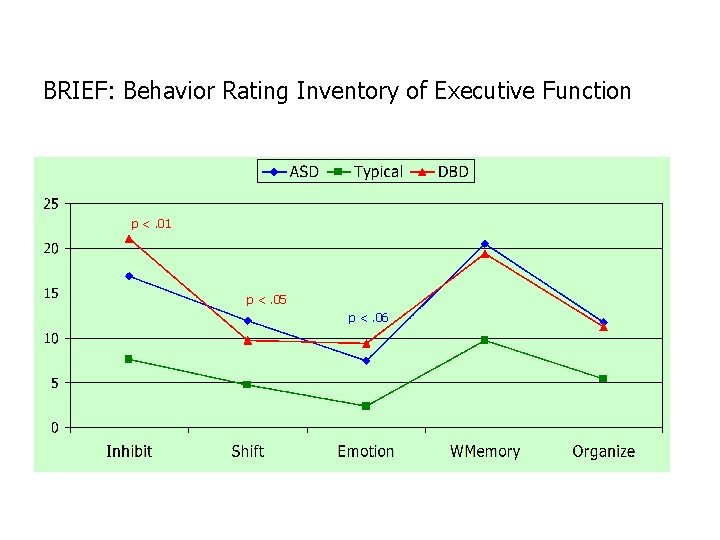
BRIEF: Behavior Rating Inventory of Executive Function p <. 01 p <. 05 p <. 06
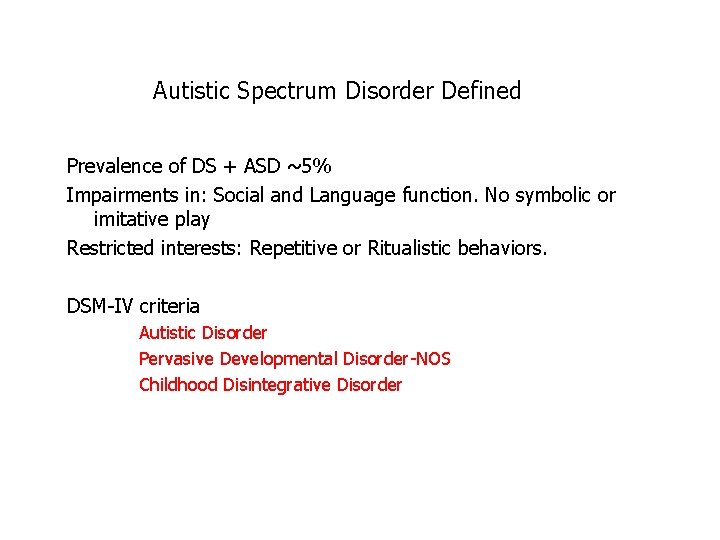
Autistic Spectrum Disorder Defined Prevalence of DS + ASD ~5% Impairments in: Social and Language function. No symbolic or imitative play Restricted interests: Repetitive or Ritualistic behaviors. DSM-IV criteria Autistic Disorder Pervasive Developmental Disorder-NOS Childhood Disintegrative Disorder
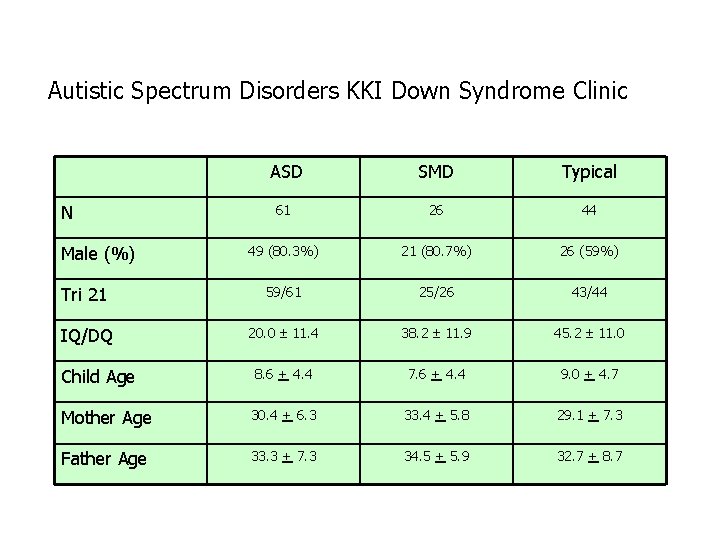
Autistic Spectrum Disorders KKI Down Syndrome Clinic ASD SMD Typical 61 26 44 49 (80. 3%) 21 (80. 7%) 26 (59%) Tri 21 59/61 25/26 43/44 IQ/DQ 20. 0 11. 4 38. 2 11. 9 45. 2 11. 0 Child Age 8. 6 + 4. 4 7. 6 + 4. 4 9. 0 + 4. 7 Mother Age 30. 4 + 6. 3 33. 4 + 5. 8 29. 1 + 7. 3 Father Age 33. 3 + 7. 3 34. 5 + 5. 9 32. 7 + 8. 7 N Male (%)
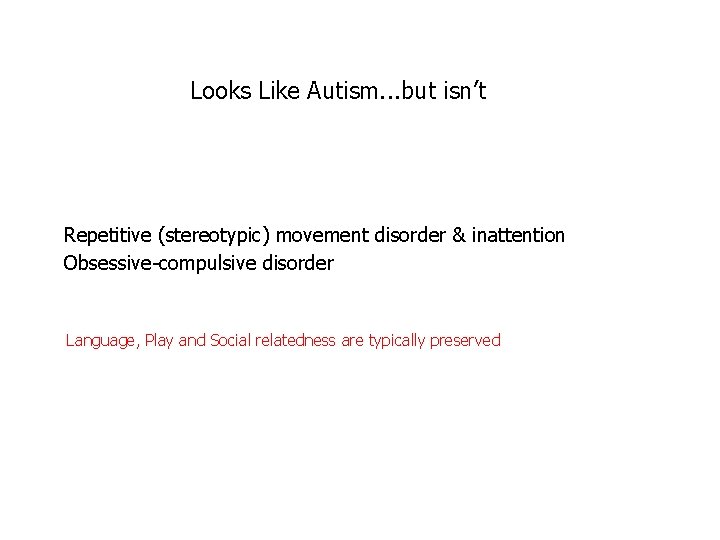
Looks Like Autism. . . but isn’t Repetitive (stereotypic) movement disorder & inattention Obsessive-compulsive disorder Language, Play and Social relatedness are typically preserved
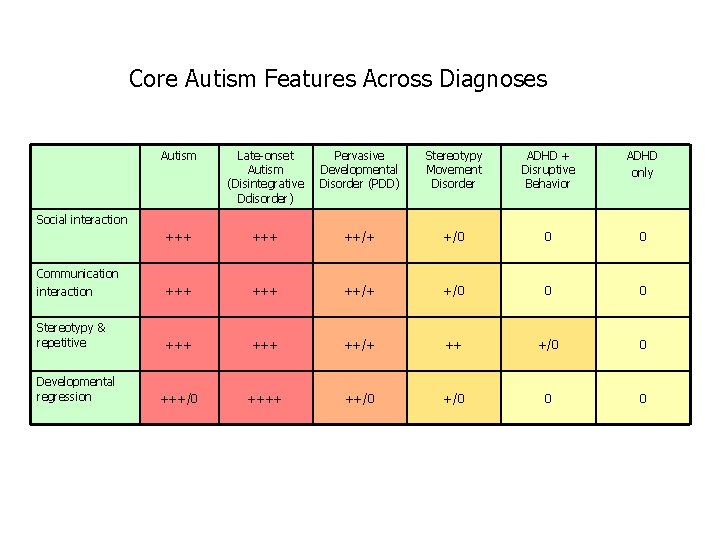
Core Autism Features Across Diagnoses Autism Late-onset Autism (Disintegrative Ddisorder) Pervasive Developmental Disorder (PDD) Stereotypy Movement Disorder ADHD + Disruptive Behavior ADHD only +++ ++/+ +/0 0 0 Communication interaction +++ ++/+ +/0 0 0 Stereotypy & repetitive +++ ++/+ ++ +/0 0 +++/0 ++++ ++/0 0 0 Social interaction Developmental regression
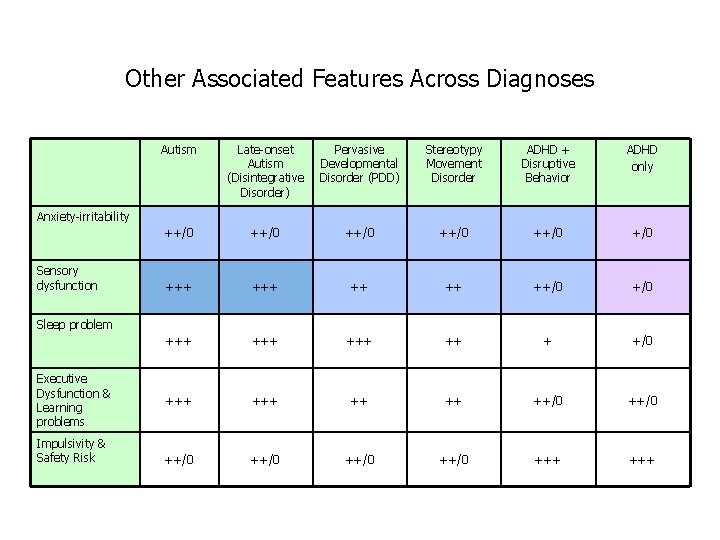
Other Associated Features Across Diagnoses Autism Late-onset Autism (Disintegrative Disorder) Pervasive Developmental Disorder (PDD) Stereotypy Movement Disorder ADHD + Disruptive Behavior ADHD only ++/0 ++/0 +++ ++/0 +++ +++ ++ + +/0 +++ ++/0 ++/0 +++ Anxiety-irritability Sensory dysfunction Sleep problem Executive Dysfunction & Learning problems Impulsivity & Safety Risk
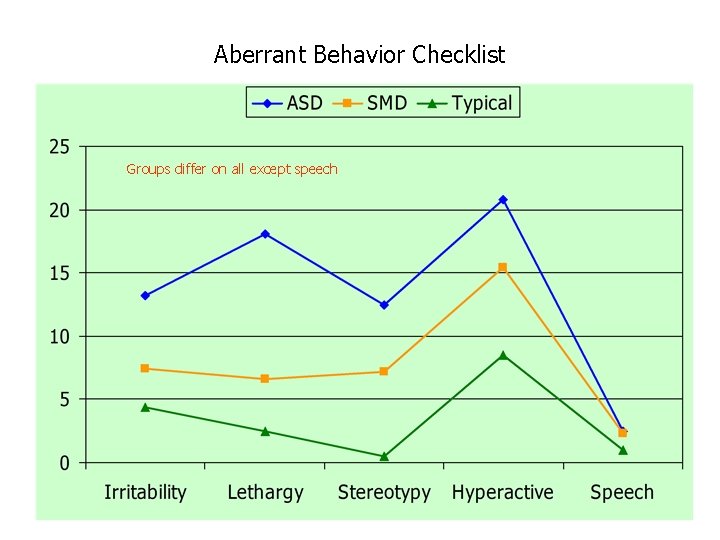
Aberrant Behavior Checklist Groups differ on all except speech
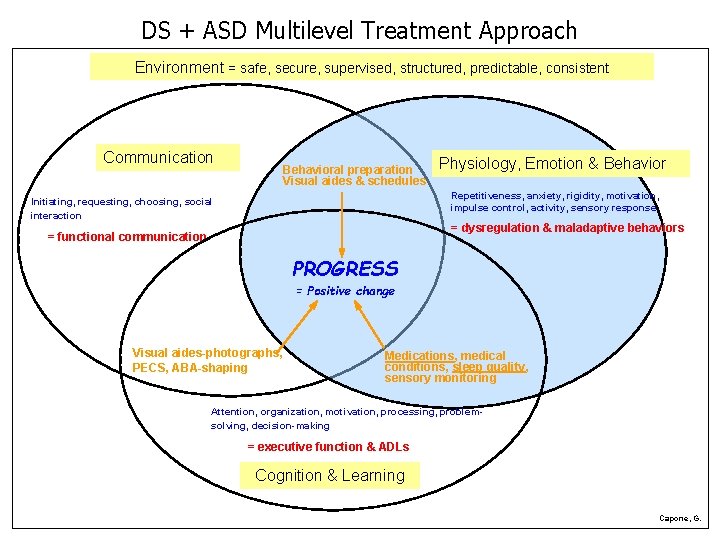
DS + ASD Multilevel Treatment Approach Environment = safe, secure, supervised, structured, predictable, consistent Communication Behavioral preparation Visual aides & schedules Physiology, Emotion & Behavior Repetitiveness, anxiety, rigidity, motivation, impulse control, activity, sensory response Initiating, requesting, choosing, social interaction = dysregulation & maladaptive behaviors = functional communication PROGRESS = Positive change Visual aides-photographs, PECS, ABA-shaping Medications, medical conditions, sleep quality, sensory monitoring Attention, organization, motivation, processing, problemsolving, decision-making = executive function & ADLs Cognition & Learning Capone, G.
Implications for Children with Down Syndrome Neurobehavioral disorders are complex Need for improved recognition & understanding Need for different approaches to education & therapy Need for multilevel treatment approach Try not to blame yourself or others Need for acceptance of “differentness” All parents need to support each other

Thank you…
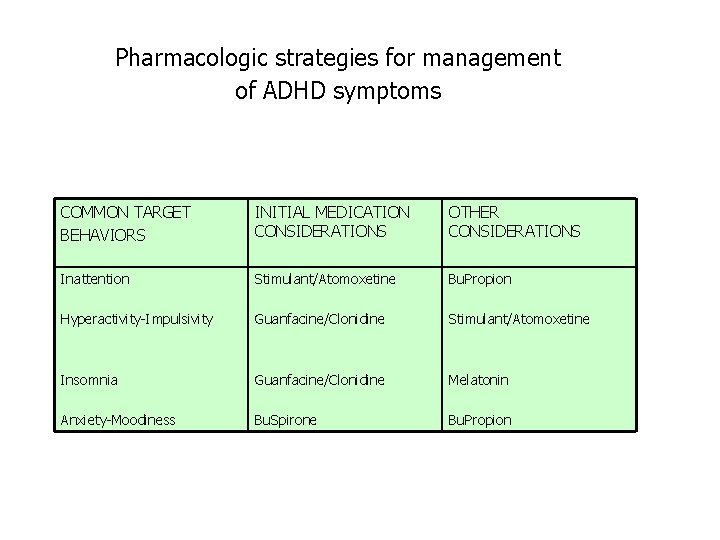
Pharmacologic strategies for management of ADHD symptoms COMMON TARGET BEHAVIORS INITIAL MEDICATION CONSIDERATIONS OTHER CONSIDERATIONS Inattention Stimulant/Atomoxetine Bu. Propion Hyperactivity-Impulsivity Guanfacine/Clonidine Stimulant/Atomoxetine Insomnia Guanfacine/Clonidine Melatonin Anxiety-Moodiness Bu. Spirone Bu. Propion
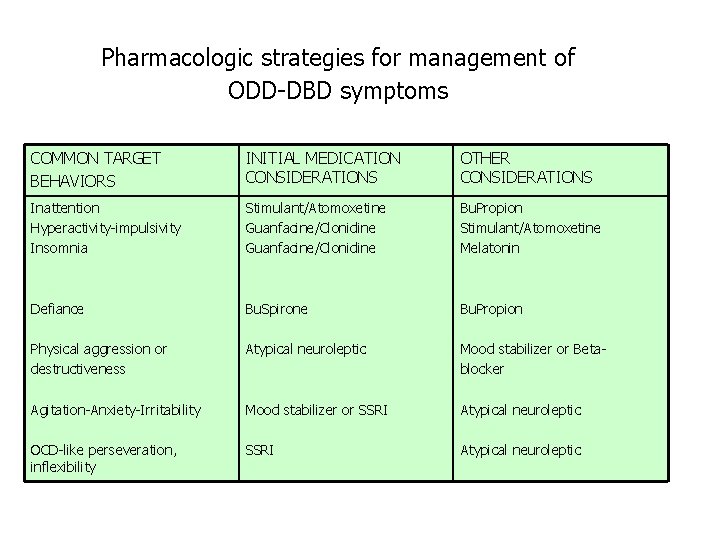
Pharmacologic strategies for management of ODD-DBD symptoms COMMON TARGET BEHAVIORS INITIAL MEDICATION CONSIDERATIONS OTHER CONSIDERATIONS Inattention Hyperactivity-impulsivity Insomnia Stimulant/Atomoxetine Guanfacine/Clonidine Bu. Propion Stimulant/Atomoxetine Melatonin Defiance Bu. Spirone Bu. Propion Physical aggression or destructiveness Atypical neuroleptic Mood stabilizer or Betablocker Agitation-Anxiety-Irritability Mood stabilizer or SSRI Atypical neuroleptic OCD-like perseveration, inflexibility SSRI Atypical neuroleptic
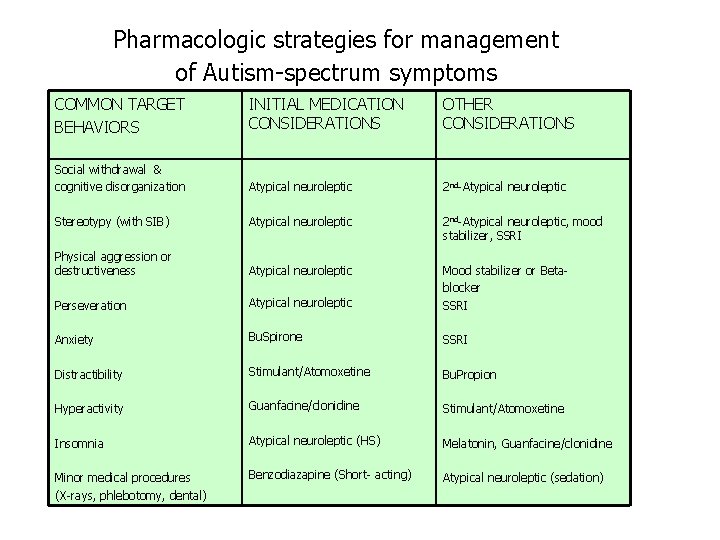
Pharmacologic strategies for management of Autism-spectrum symptoms COMMON TARGET BEHAVIORS INITIAL MEDICATION CONSIDERATIONS OTHER CONSIDERATIONS Social withdrawal & cognitive disorganization Atypical neuroleptic 2 nd-Atypical neuroleptic Stereotypy (with SIB) Atypical neuroleptic 2 nd-Atypical neuroleptic, mood stabilizer, SSRI Physical aggression or destructiveness Atypical neuroleptic Perseveration Atypical neuroleptic Mood stabilizer or Betablocker SSRI Anxiety Bu. Spirone SSRI Distractibility Stimulant/Atomoxetine Bu. Propion Hyperactivity Guanfacine/clonidine Stimulant/Atomoxetine Insomnia Atypical neuroleptic (HS) Melatonin, Guanfacine/clonidine Minor medical procedures (X-rays, phlebotomy, dental) Benzodiazapine (Short- acting) Atypical neuroleptic (sedation)
- Slides: 33