NEURAXIAL ANESTHESIA aka Epidurals and Spinals a very
- Slides: 15
NEURAXIAL ANESTHESIA aka Epidurals and Spinals - a very brief overview -
WHY DO WE DO THIS? • Both epidural and spinal injection of local anesthetic medications (+/- other meds) result in sensory and motor blockade – the location and density of both depend on a variety of factors • Very dense blockade can be used for surgical analgesia (typically spinal) • Catheters (typically epidural) can be placed for postoperative pain control
EPIDURAL VS. SPINAL EPIDURAL • Injection into potential space, requires larger volumes • Primarily numbs nerve roots – anesthesia typically in a band-like bilateral distribution of a few spinal levels • More commonly used for placement of catheter for ongoing pain control • Less risk of hypotension, less dense block (typically) than spinal SPINAL • Injection into intrathecal space, with medication directly bathing spinal cord performed below the termination of the spinal cord, in lumbar region • Usually for lower extremity, lower abdominal, or perineal surgery • Very small volumes = big results • Usually faster and less uncomfortable than epidural placement • Denser sensory and motor block than epidural
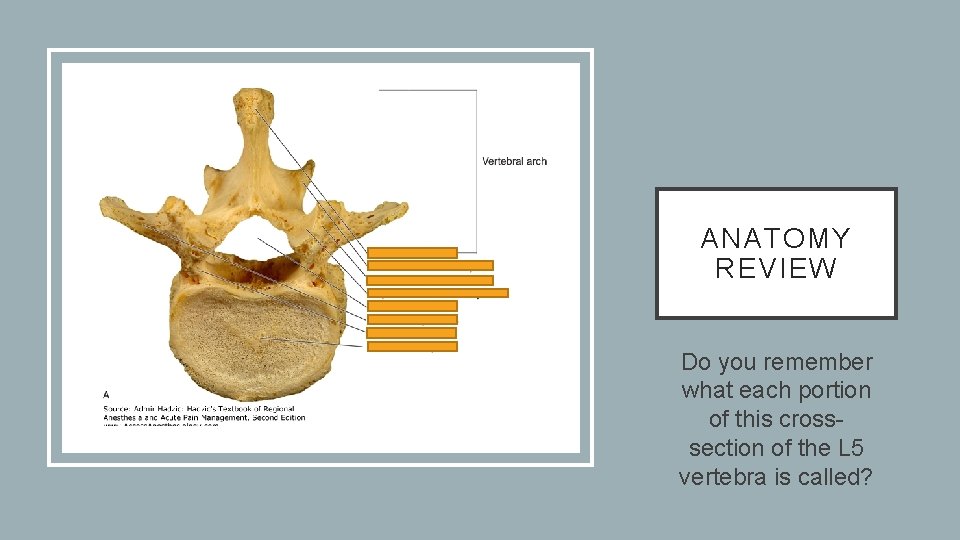
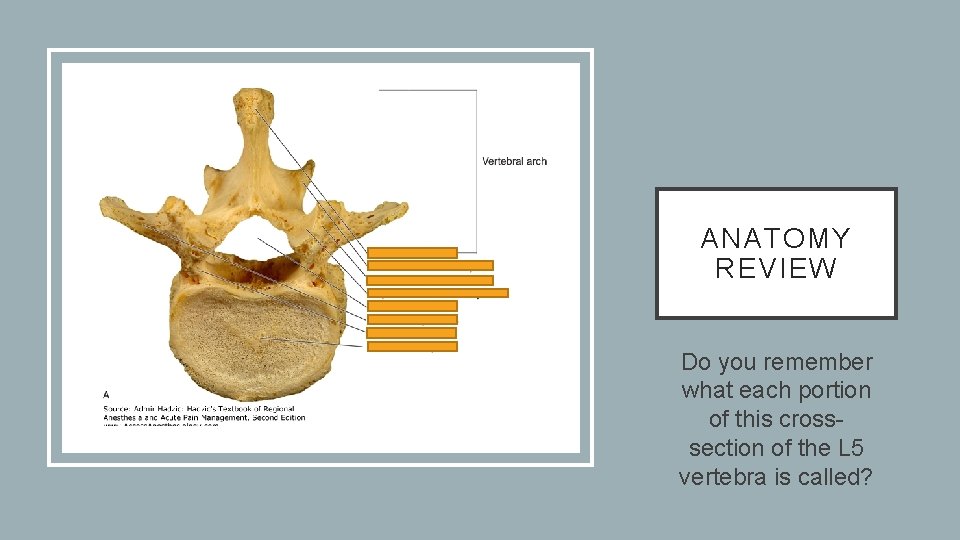
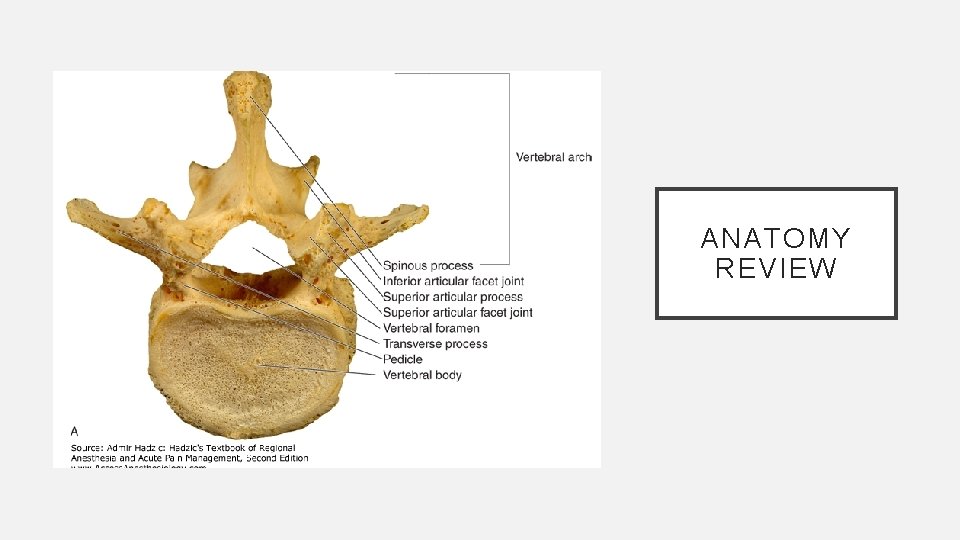
ANATOMY REVIEW Do you remember what each portion of this crosssection of the L 5 vertebra is called?
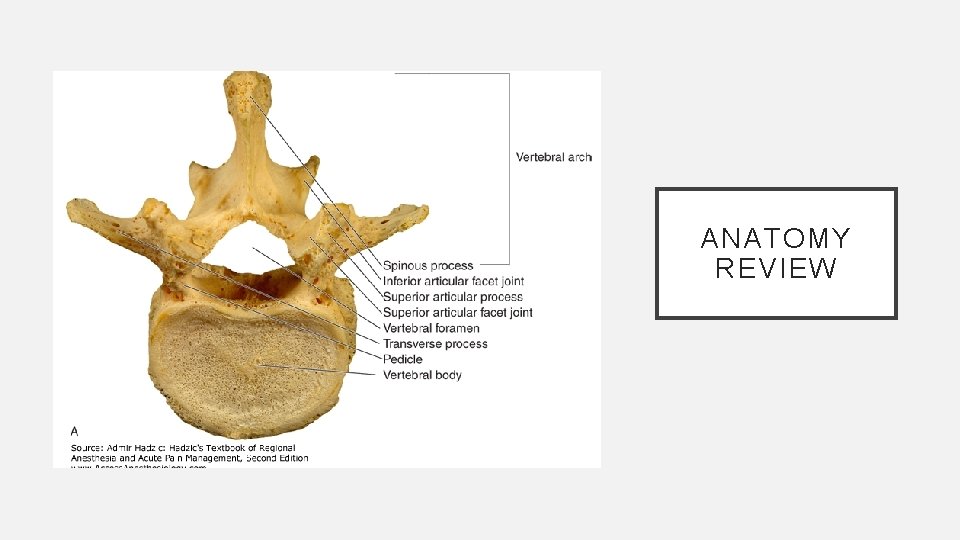
ANATOMY REVIEW
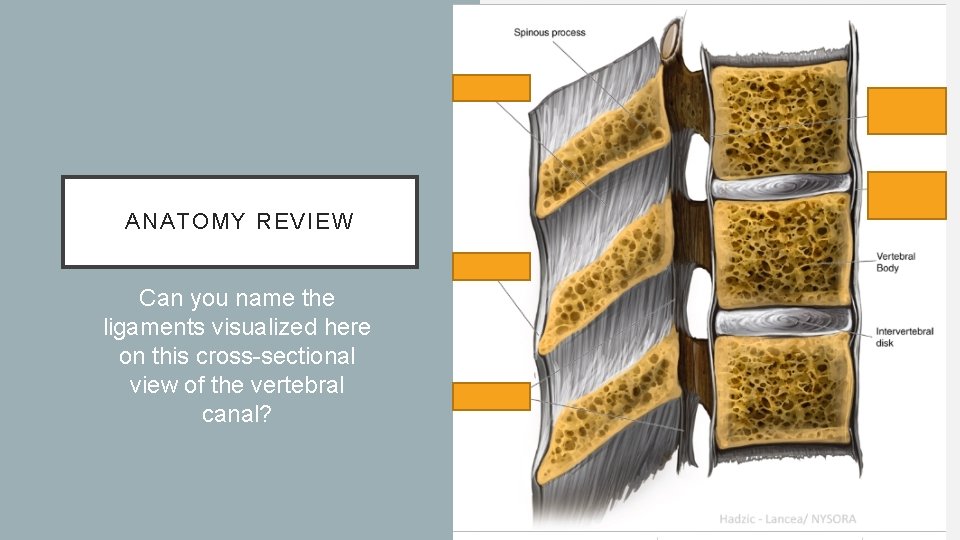
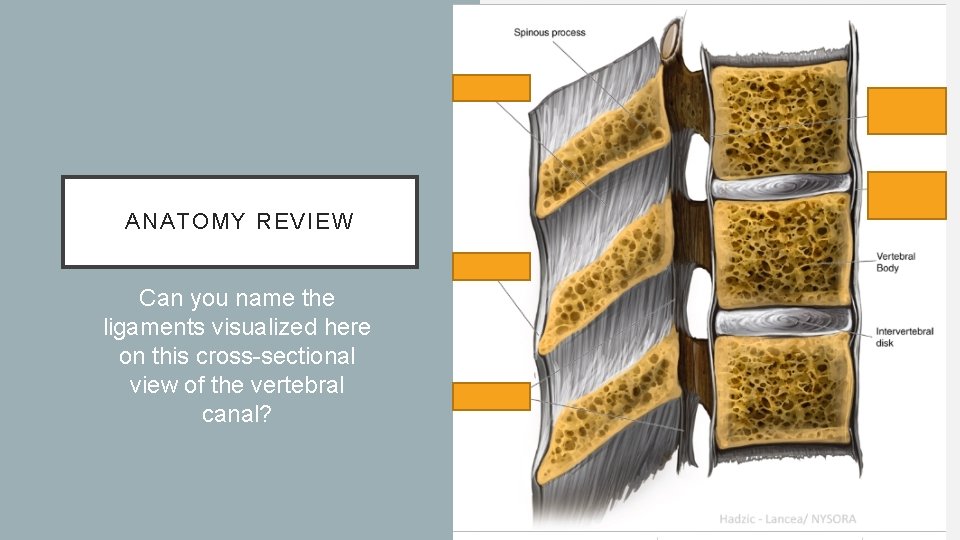
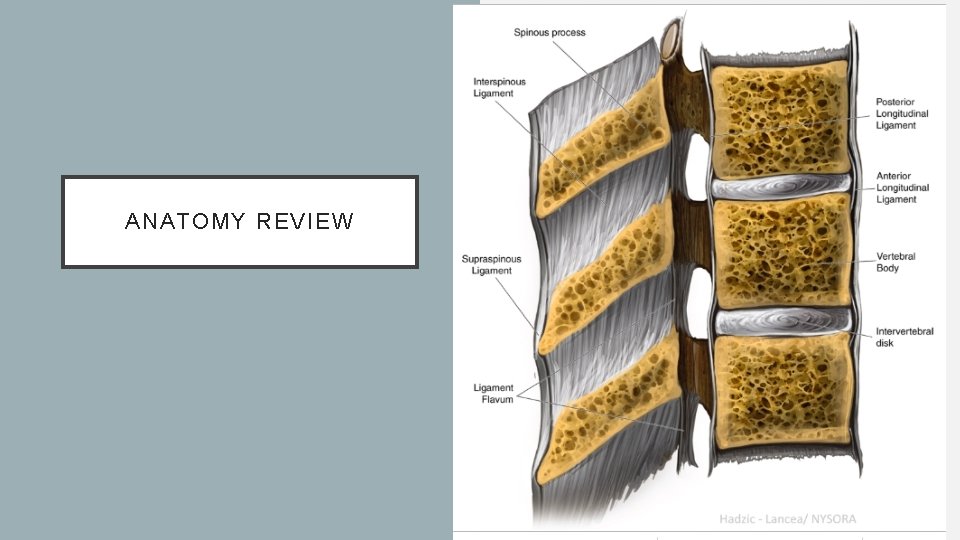
ANATOMY REVIEW Can you name the ligaments visualized here on this cross-sectional view of the vertebral canal?
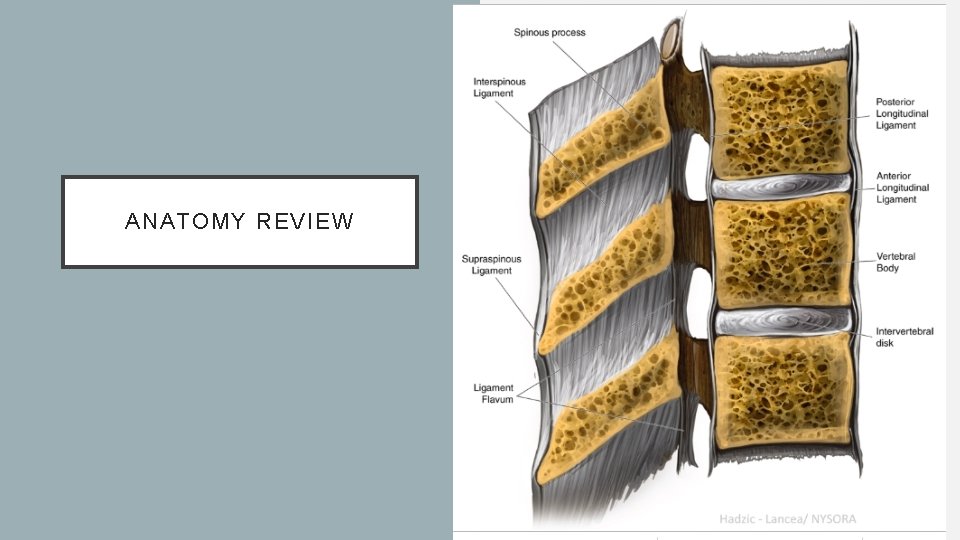
ANATOMY REVIEW
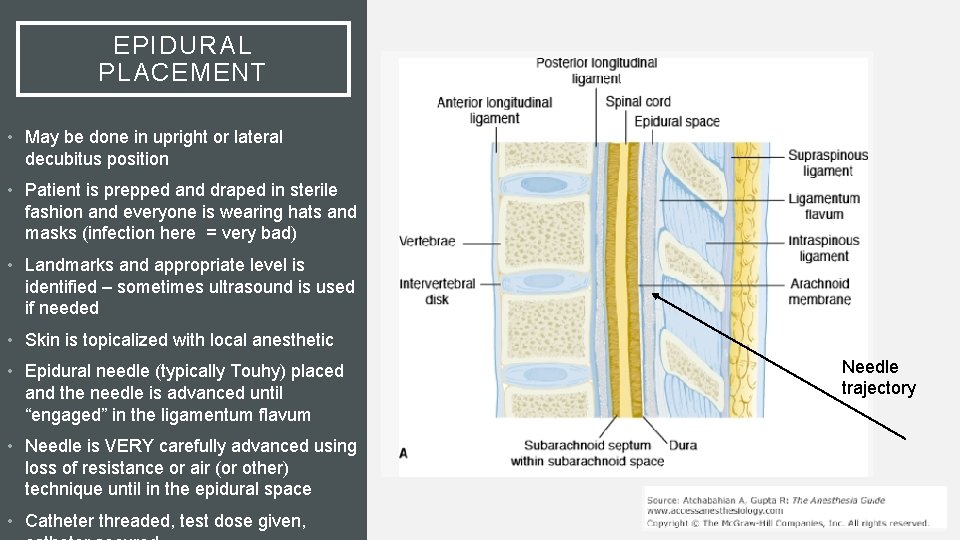
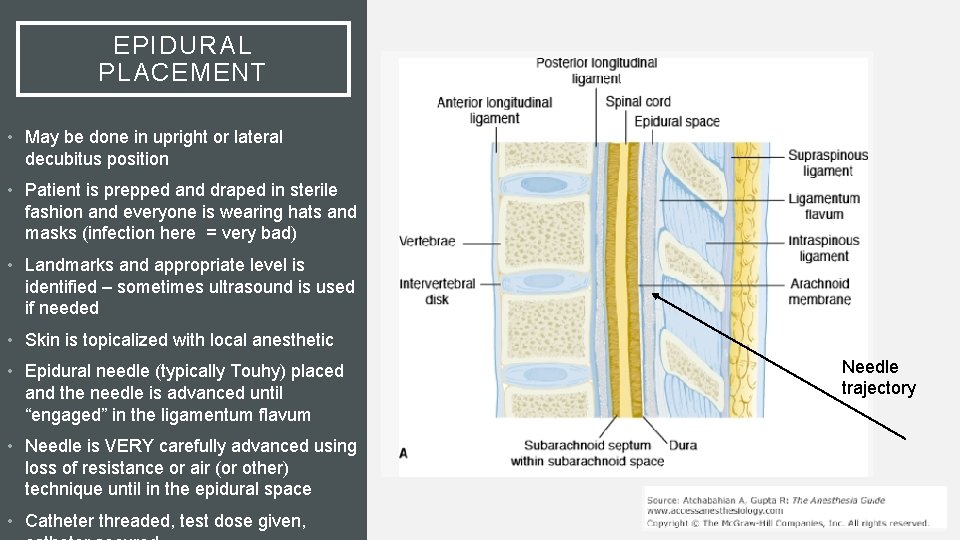
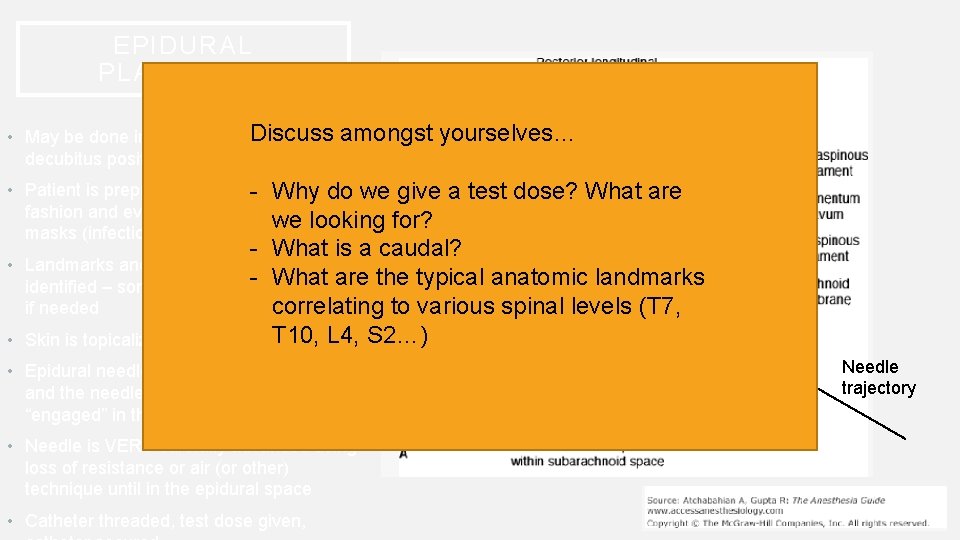
EPIDURAL PLACEMENT • May be done in upright or lateral decubitus position • Patient is prepped and draped in sterile fashion and everyone is wearing hats and masks (infection here = very bad) • Landmarks and appropriate level is identified – sometimes ultrasound is used if needed • Skin is topicalized with local anesthetic • Epidural needle (typically Touhy) placed and the needle is advanced until “engaged” in the ligamentum flavum • Needle is VERY carefully advanced using loss of resistance or air (or other) technique until in the epidural space • Catheter threaded, test dose given, Needle trajectory
EPIDURAL PLACEMENT Discuss • May be done in upright or lateral decubitus position amongst yourselves… • Patient is prepped and draped sterile - in Why do we give fashion and everyone is wearing hats and we looking for? masks (infection here = very bad) a test dose? What are - What is a caudal? • Landmarks and appropriate level is - What are the typical anatomic landmarks identified – sometimes ultrasound is used correlating to various spinal levels (T 7, if needed T 10, L 4, • Skin is topicalized with local anesthetic • Epidural needle (typically Touhy) placed and the needle is advanced until “engaged” in the ligamentum flavum • Needle is VERY carefully advanced using loss of resistance or air (or other) technique until in the epidural space • Catheter threaded, test dose given, S 2…) Needle trajectory
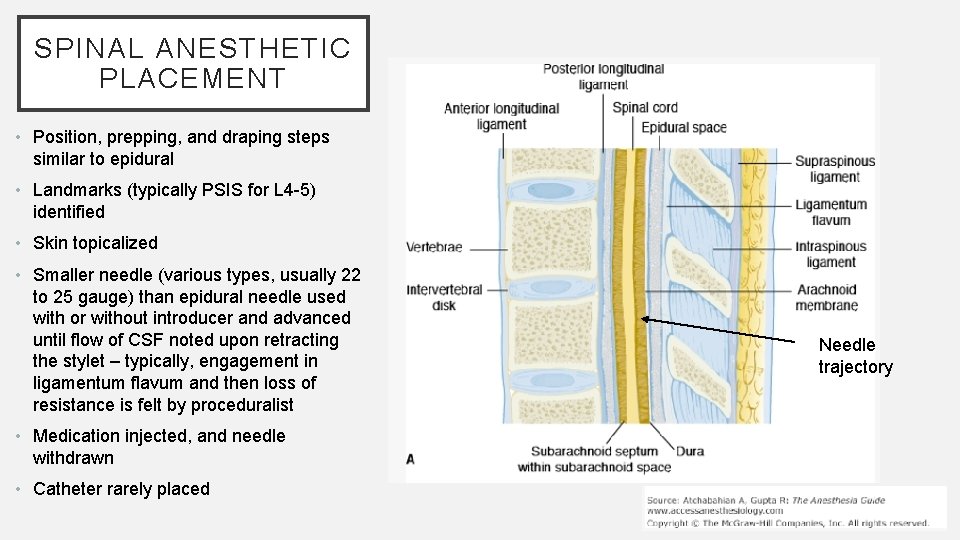
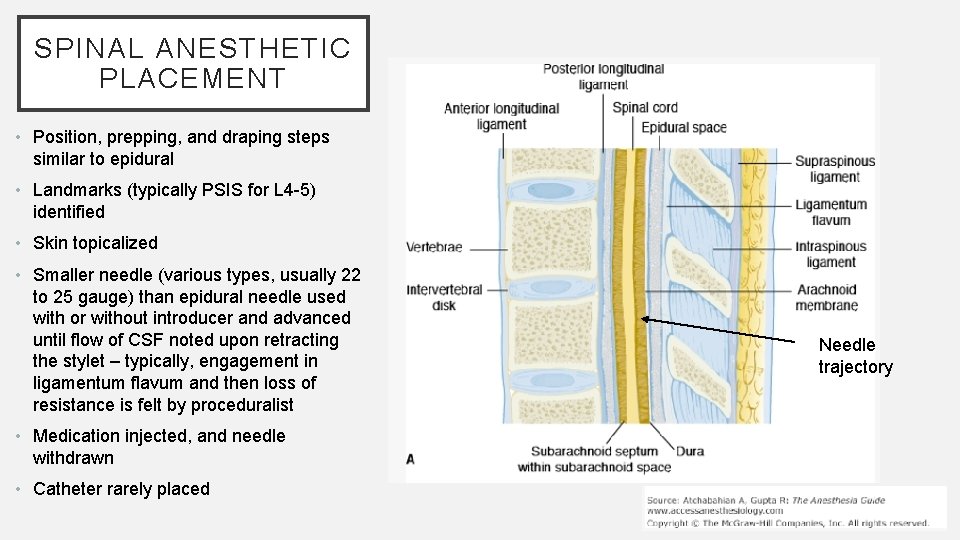
SPINAL ANESTHETIC PLACEMENT • Position, prepping, and draping steps similar to epidural • Landmarks (typically PSIS for L 4 -5) identified • Skin topicalized • Smaller needle (various types, usually 22 to 25 gauge) than epidural needle used with or without introducer and advanced until flow of CSF noted upon retracting the stylet – typically, engagement in ligamentum flavum and then loss of resistance is felt by proceduralist • Medication injected, and needle withdrawn • Catheter rarely placed Needle trajectory
WHAT ARE CONTRAINDICATIONS TO SPINAL AND EPIDURAL PLACEMENT? • Guess, please.
WHAT ARE CONTRAINDICATIONS TO SPINAL AND EPIDURAL PLACEMENT? • Absolute • Patient refusal • Infection at site • Elevated ICP • Bleeding diathesis • Relative • Bacteremia • Pre-existing neurologic deficits (ex. MS, etc) • Significant cardiac pathology that doesn’t tolerate abrupt decreases in SVR (caution with critical aortic stenosis, hypertrophic subaortic stenosis, etc)
SIDE EFFECTS AND COMPLICATIONS • Neurologic complications – rare, but can be caused by direct trauma or compression from abscess, epidural hematoma, etc. • Hypotension (expected to a certain degree) • Bradycardia and asystole – especially if T 1 -4 cardioaccelerator fibers affected • Post-dural puncture headache – typically with unintended dural puncture with epidural (larger) needle • High spinal anesthesia • Nausea • Urinary retention • Back pain
IS NEURAXIAL ANESTHESIA WORTH THE RISKS? • What is the alternative? • What do you think?
REFERENCES • Atchabahian, A. , & Gupta, R. (2013). The anesthesia guide. New York: Mc. Graw-Hill Medical. • Miller, R. D. , Pardo, M. , & Stoelting, R. K. (2011). Basics of anesthesia (6 th ed. ). Philadelphia, PA: Elsevier/Saunders. • New York School of Regional Anesthesia. , & Hadzic, A. (2007). Textbook of regional anesthesia and acute pain management. New York: Mc. Graw-Hill, Medical Pub. Division.