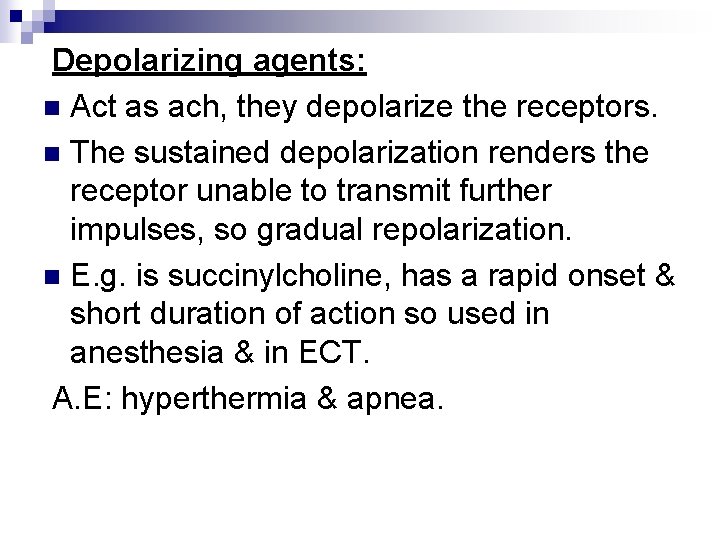
Nervous system Peripheral NS Efferent division Autonomic NS

- Slides: 22
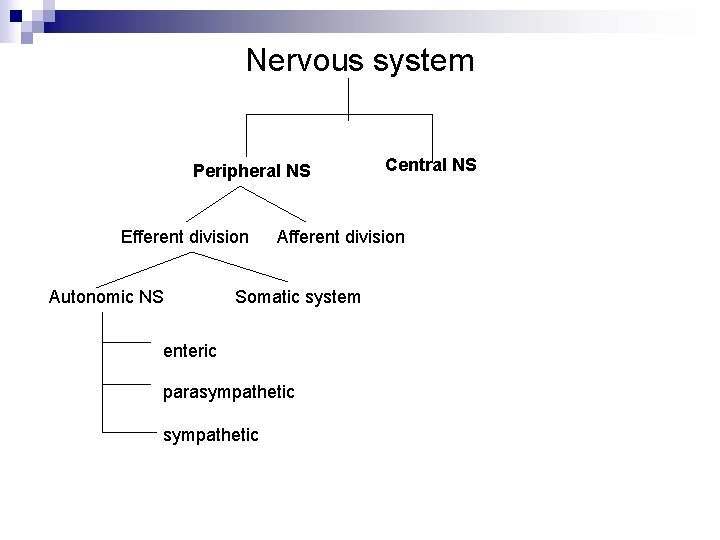
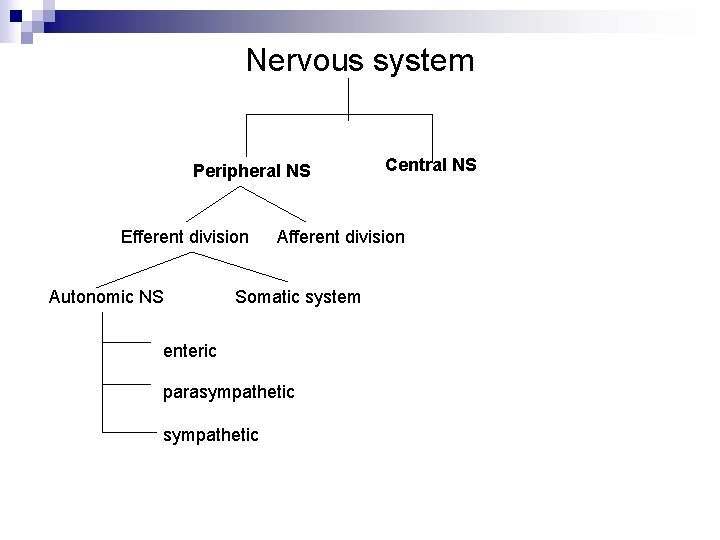
Nervous system Peripheral NS Efferent division Autonomic NS Afferent division Somatic system enteric parasympathetic Central NS
Anatomy of the ANS: n Efferent neurons. n Afferent neurons.
Cholinergic Agonist Ach transmission has 6 steps: n Synthesis, storage, release, binding, degradation & choline recycling. n
n Cholinergic agonist: 1. Direct-acting cholinergic agonist. 2. Indirect-acting cholinergic agonist. (anticholinestrase).
Direct-acting cholinergic agonist: n Binds directly to cholinoceptors. n Synthetic esters of choline or natural alkaloids. n Longer action than Ach. Acetylcholine: n Has no therapeutic importance due to the multiplicity of action & the rapid inactivation. n Has both muscarinic & nicotinic activity. n
Action: n the heart rate, COP & the BP. n the GIT secretions & motility. n the bronchial secretion. n the tone of detrosur muscle. n leads to ciliary muscle contraction & pupilary constriction. Bethanechol: n Related structurally to ACH. n It has no nicotinic action but a strong muscarinic one.
Action: 1. In the GIT, it increases motility & tone. 2. In the bladder, it stimulates the detruser muscle causing urine expulsion ( used for PO atonic bladder). A. E: n As generalized cholinergic stimulation. Carbachol: n Muscarinic & nicotinic action.
Action: 1. On the CVS. 2. On the GIT. 3. Epinephrine release from the adrenal medulla (nicotinic action). 4. In the eye it causes miosis & spasm of accommodation. n is used as a miotic agent to treat glaucoma (pupilary constriction & the IOP).
pilocaroine: n Less potent than Ach & it’s derivatives. n Has muscarinic activity. n Used in the eye to produce miosis & accommodation spasm. n The drug of choice in emergency lowering of the IOP. A. E: n CNS disturbances. n Profuse sweating & salivation.
Reversible -anticholinestrase They inhibit Ach-esterase so prolong the action of Ach. n Act on all cholinoceptors in the body (nicotinic & muscarinic). n
Physostigmine: n A tertiary amine. n intestinal & bladder motility so is used in atony. n Used in glaucoma. n To treat overdose of anti-cholinergic action as atropine. A. E: 1. Convulsions. 2. Bradycardia & COP. 3. Skeletal muscle paralysis (rare with therapeutic dose).
Neostigmine: n A quaternary amine. n Stronger action than physo. On skeletal muscles (contraction then paralysis). n Used to stimulate the bladder & GIT, myasthenia gravis (edrophonium for Δ). A. E: n generalized cholinergic stimulation.
Irreversible anticholinesterase Are synthetic organophosphorus compound. n Extremely toxic (as pesticides). Isoflurophate: n Generalized cholinergic stimulation. n Paralysis of motor function (breathing difficulties). n Convulsions. n Intense miosis (topically to treat open-angle glaucoma) ecothiophate replace it. n Pralidoxime is an antidote (except for the CNS). n
Cholinergic antagonists 1 -Antimuscarinic They block the muscarinic receptors inhibiting their function. Atropine: n Binds competitively. n Acts centrally & peripherally. Action: n In the eye it causes persistent mydriasis & cycloplegia. n GIT : it’s an antispasmodic. n
Urinary system: it decrease the bladder motility. n CVS: In low dose bradycardia (blocks M 1 in the inhibitory prejunctional neurons. In higher doses HR (blocks M 2 in SA node). n It blocks the salivary, lacrimal & sweat glands (as antiscretory prior to surgery). n Used as an antidote for cholinergic agonist. n
A. E: n Tachycardia, dry mouth, constipation, blurred vision, restlessness, confusion hallucinations & glaucoma precipitation. Scopalamine: n It has greater CNS action, longer duration, antimotion sickness, sedation & blocks short term memory. Ipratropium: n Quaternary derivative of atropine & is positively charged. n As an inhaler in asthma & COPD.
Ganglionic Blockers Work on the nicotinic receptors in the autonomic ganglia. n Are non-depolarizing competitive blockers. n Has no selectivity for sympathetic or parasympathetic ganglia (so rarely used therapeutically only experimentally). Nicotine: n Stimulation & then paralysis of all the ganglia. n It causes transmitter release. n It BP, HR, secretions & peristalsis. n At higher doses the opposite happens due to ganglionic block. n
Trimethophan short acting, used as an alternative drug to lower the BP in emergency situations. Neuromuscular blocking drugs: n Either antagonist (non-depolarizing), or agonist (depolarizing). Non-depolarizing (competitive) blockers: n At low dose they compete with Ach & prevent muscle contraction (action is overcomed by e. g. cholinesterase inhibitors). n
n n n 1. 2. 3. 4. At high doses, they can block the ion-channels so further weakening the NMJ transmission. Used in surgery for muscle relaxation. They don’t cross the BBB. A. E: release of histamine, BP& HR, malignant hyperthermia, hyperkalemia. Drug interactions: Cholinesterase inhibitors overcome the action. Halothane stabilizes their action. Aminoglycosides antibiotics enhance the blockade by inhibiting Ach release. Calcium -channel blockers may enhance their action.
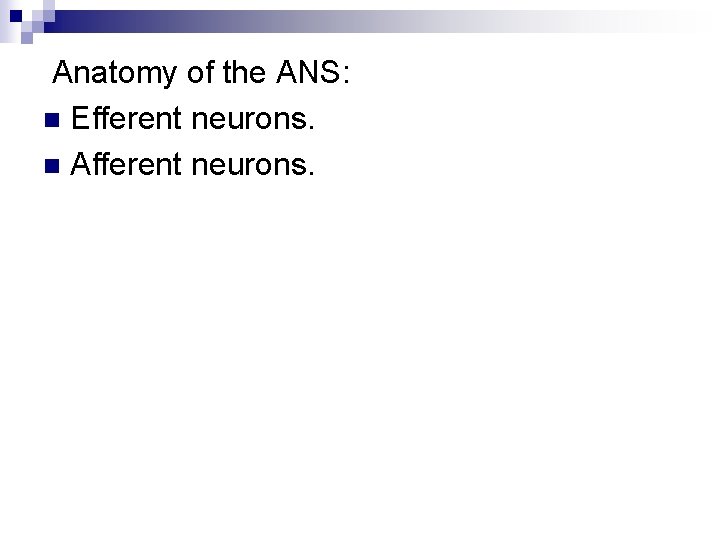
Depolarizing agents: n Act as ach, they depolarize the receptors. n The sustained depolarization renders the receptor unable to transmit further impulses, so gradual repolarization. n E. g. is succinylcholine, has a rapid onset & short duration of action so used in anesthesia & in ECT. A. E: hyperthermia & apnea.
