Nephrotic Syndrome NS PREPARED BY MOHAMMAD ALI ALSHEHRI
Nephrotic Syndrome. . …(NS) PREPARED BY: MOHAMMAD ALI AL-SHEHRI …. . SUPERVISED BY : DR.
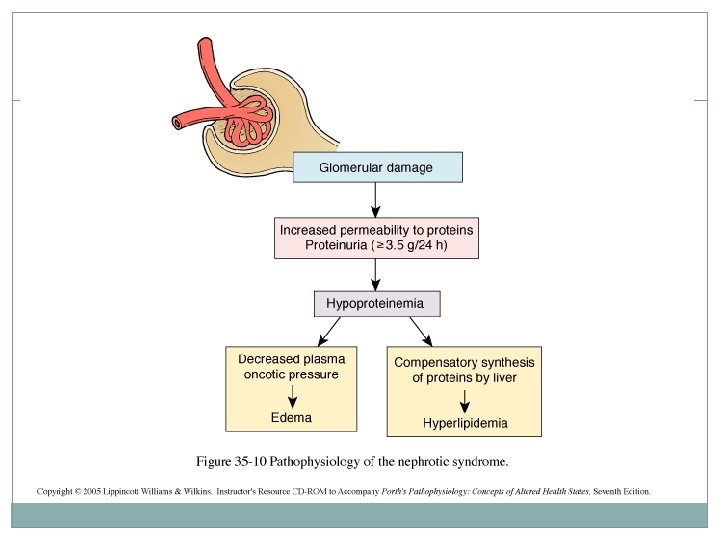
Nephrotic syndrome (NS) results from increased permeability of Glomeulrar basement membrane (GBM) to plasma protein. It is clinical and laboratory syndrome characterized by massive proteinuria, which lead to hypoproteinemia ( hypo-albuminemia), hyperlipidemia and pitting edema. (4 -increase, 1 -decrease).
Nephrotic Criteria: *Massive proteinuria: qualitative proteinuria: 3+ or 4+, quantitative proteinuria : more than 40 mg/m 2/hr in children (selective). *Hypo-proteinemia : total plasma proteins < 5. 5 g/dl and serum albumin : < 2. 5 g/dl. *Hyperlipidemia: serum cholesterol : > 5. 7 mmol/L *Edema: pitting edema in different degree
Nephritic Criteria -Hematuria: RBC in urine (gross hematuria) -Hypertension: ≥ 130/90 mm. Hg in school-age children ≥ 120/80 mm. Hg in preschool-age children ≥ 110/70 mm. Hg in infant and toddler’s children -Azotemia(renal insufficiency): Increased level of serum BUN 、Cr -Hypo-complementemia: Decreased level of serum c 3
Classification: A-Primary Idiopathic NS (INS): majority The cause is still unclear up to now. Recent 10 years , increasing evidence has suggested that INS may result from a primary disorder of T– cell function. Accounting for 90% of NS in child. mainly discussed. B-Secondary NS: NS resulted from systemic diseases, such as anaphylactoid purpura , systemic lupus erythematosus, HBV infection. C-Congenital NS: rare *1 st 3 monthe of life , only treatment renal transplantation
Secondary NS Drug, Toxic, Allegy: mercury, snake venom, vaccine, pellicillamine, Heroin, gold, NSAID, captopril, probenecid, volatile hydrocarbons Infection: APSGN, HBV, HIV, shunt nephropathy, reflux nephropathy, leprosy, syphilis, Schistosomiasis, hydatid disease Autoimmune or collagen-vascular diseases: SLE, Hashimoto’s thyroiditis, , HSP, Vasculitis Metabolic disease: Diabetes mellitus Neoplasma: Hodgkin’s disease, carcinoma ( renal cell, lung, neuroblastoma, breast, and etc) Genetic Disease: Alport syn, Sickle cell disease, Amyloidosis, Congenital nephropathy Others: Chronic transplant rejection, congenital nephrosclerosis
Idiopathic NS (INS): Pathology: Minimal Change Nephropathy (MCN): >80% The glomeruli appear normal basically Under Light microscopy, and Under Immunofluorescence *under Electron microscopy – fusion of the foot processes of the podocytes (2) Non—MCN: < 20% *Mesangial proliferative glomerulonephritis (Ms. PGN): about 10% *Focal segmental glomerulosclerosis (FSGS): 5% *Membranous Nephropathy (MN) : 2% *Membrane proliferative glomerulonephritis (MPGN) : 1% *Others: rare, Cresent glomerulonephritis
NB: *Nephrotic syndrome is 15 times more common in children than in adults. *Most cases of primary nephrotic syndrome are in children and are due to minimal-change disease. The age at onset varies with the type of nephrotic syndrome.
Pathophysiology: The Main Trigger Of primary Nephrotic Syndrome and Fundamental and highly important change of pathophysiology : Proteinuria
Pathogenesis of Proteinuria: Increase glomerular permeability for proteins due to loss of negative charged glycoprotein Degree of protineuria: Mild less than 0. 5 g/m 2/day Moderate 0. 5 – 2 g/m 2/day Sever more than 2 g/m 2/day Type of proteinuria: A-Selective proteinuria: where proteins of low molecular weight. such as albumin, are excreted more readily than protein of HMW B-Non selective : LMW+HMW are lost in urine
pathogenesis of hypoalbuminemia *Due to hyperproteinuria----- Loss of plasma protein in urine mainly the albumin. *Increased catabolism of protein during acute phase.
pathogenesis of hyperlipidemia: *Response to Hypoalbuminemia → reflex to liver --→ synthesis of generalize protein ( including lipoprotein ) and lipid in the liver , the lipoprotein high molecular weight no loss in urine → hyperlipidemia *Diminished catabolism of lipoprotein
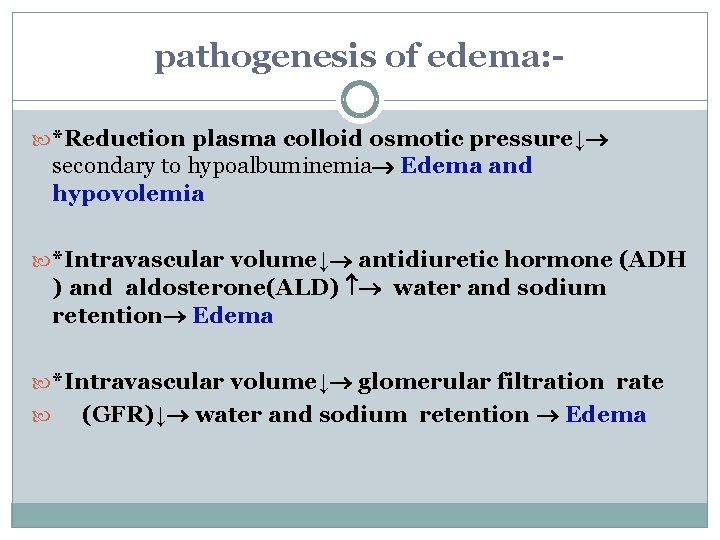
pathogenesis of edema: *Reduction plasma colloid osmotic pressure↓ secondary to hypoalbuminemia Edema and hypovolemia *Intravascular volume↓ antidiuretic hormone (ADH ) and aldosterone(ALD) water and sodium retention Edema *Intravascular volume↓ glomerular filtration rate (GFR)↓ water and sodium retention Edema
How many pathological types causes nephrotic syndrome?
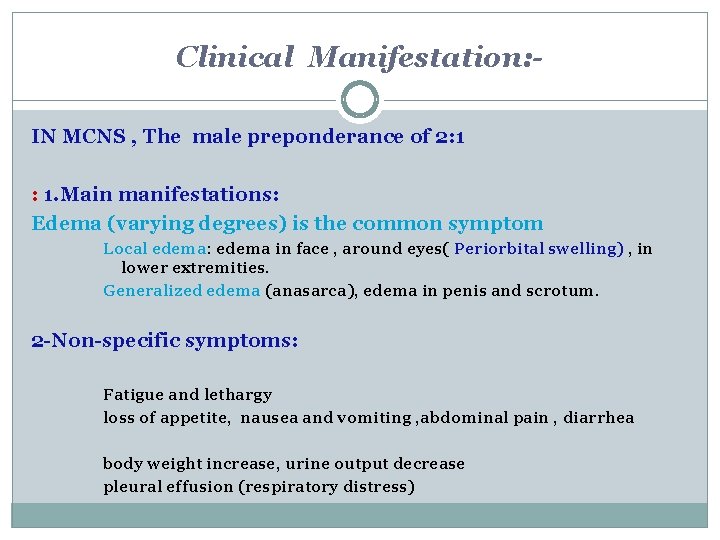
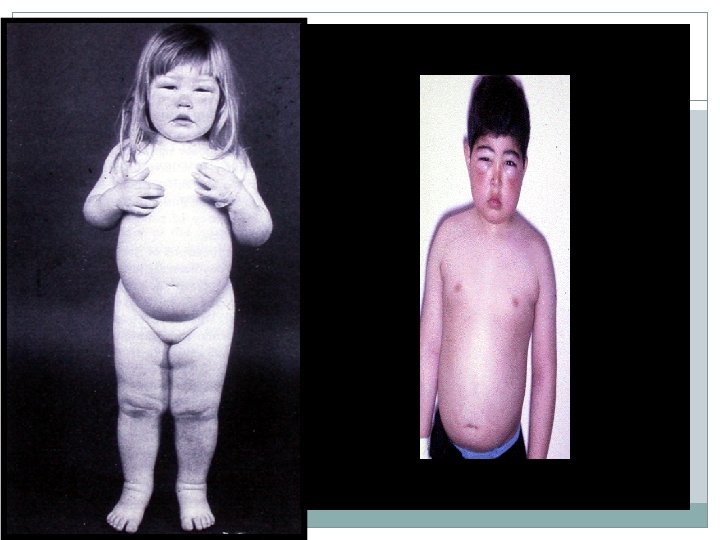
Clinical Manifestation: IN MCNS , The male preponderance of 2: 1 : 1. Main manifestations: Edema (varying degrees) is the common symptom Local edema: edema in face , around eyes( Periorbital swelling) , in lower extremities. Generalized edema (anasarca), edema in penis and scrotum. 2 -Non-specific symptoms: Fatigue and lethargy loss of appetite, nausea and vomiting , abdominal pain , diarrhea body weight increase, urine output decrease pleural effusion (respiratory distress)
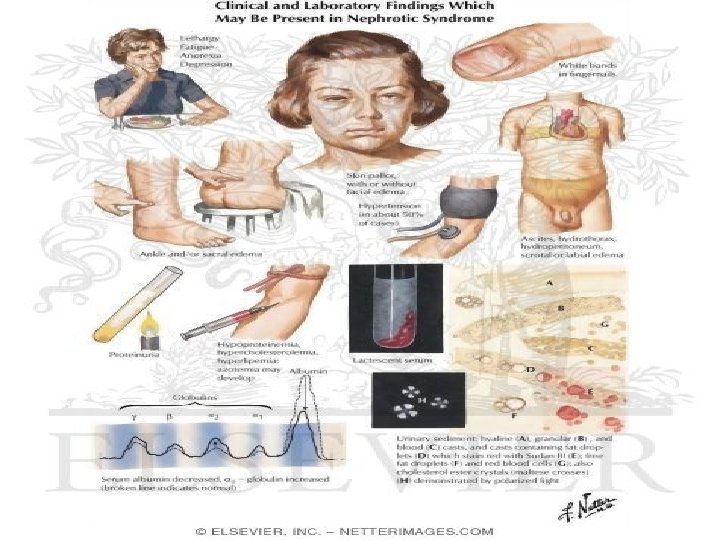
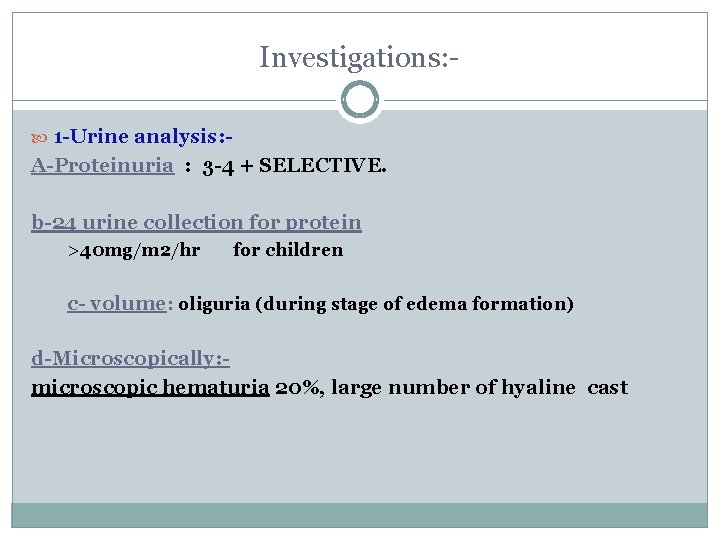
Investigations: 1 -Urine analysis: - A-Proteinuria : 3 -4 + SELECTIVE. b-24 urine collection for protein >40 mg/m 2/hr for children c- volume: oliguria (during stage of edema formation) d-Microscopically: microscopic hematuria 20%, large number of hyaline cast
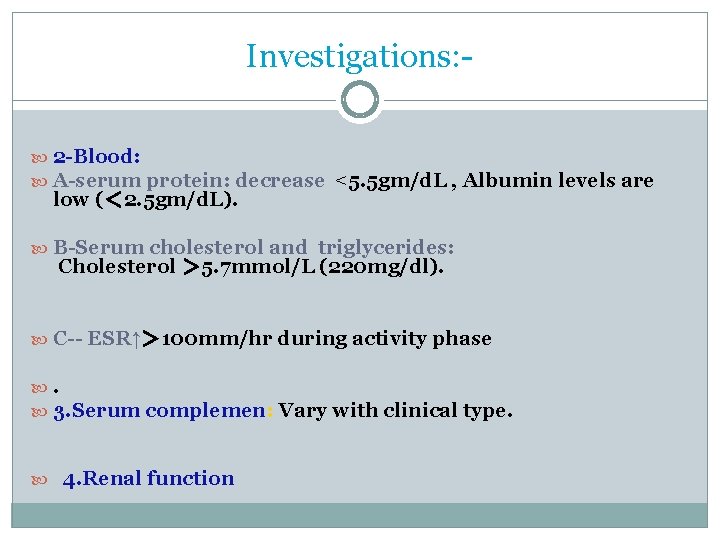
Investigations: 2 -Blood: A-serum protein: decrease <5. 5 gm/d. L , Albumin levels are low (< 2. 5 gm/d. L). B-Serum cholesterol and triglycerides: Cholesterol > 5. 7 mmol/L (220 mg/dl). C-- ESR↑> 100 mm/hr during activity phase . 3. Serum complemen: Vary with clinical type. 4. Renal function
Kidney Biopsy: - Considered in: 1 -Secondary N. S 2 -Frequent relapsing N. S 3 -Steroid resistant N. S 4 - Hematuria 5 -Hypertension 6 - Low GFR
Differential Diagnosis of NS: D. D of generalized edema: 1 -Protein –losing enteropathy 2 -Hepatic Failure. 3 -HF 4 -Protein energy malnutrition 5 -Acute and chronic GN 6 -urticaria? Angio edema
Complications of NS: 1 -Infections: Infections is a major complication in children with NS. It frequently trigger relapses. Nephrotic pt are liable to infection because : A-loss of immunoglobins in urine. B-the edema fluid act as a culture medium. C-use immunosuppressive agents. D- malnutrition The common infection : URI, peritonitis, cellulitis and UTI may be seen. Organisms: encapsulated (Pneumococci, H. influenzae), Gram negative (e. g E. coli
Complication … Vaccines in NS; polyvalent pneumococcal vaccine (if not previously immunized) when the child is in remission and off daily prednisone therapy. Children with a negative varicella titer should be given varicella vaccine.
Complication…. . 2 -Hypercoagulability (Thrombosis). Hypercoagulability of the blood leading to venous or arterial thrombosis: Hypercoagulability in Nephrotic syndrome caused by: 1 -Higher concentration of I, II, V, VIII, X and fibrinogen 2 - Lower level of anticoagulant substance: antithrombin III 3 -decrease fibrinolysis. 4 -Higher blood viscosity 5 - Increased platelet aggregation 6 - Overaggressive diuresis
3 -ARF: pre-renal and renal 4 - cardiovascular disease : -Hyperlipidemia, may be a risk factor for cardiovascular disease. 5 -Hypovolemic shock 6 -Others: growth retardation, malnutrition, adrenal cortical insufficiency

Management of NS: General (non-specific ) *Corticosteroid therapy
General therapy: Hospitalization: - for initial work-up and evaluation of treatment. Activity: usually no restriction , except massive edema, heavy hypertension and infection. Diet Hypertension and edema: Low salt diet (<2 g. Na/ day) only during period of edema or salt-free diet. Severe edema: Restricting fluid intake Avoiding infection: very important. Diuresis: Hydrochlorothiazide (HCT) : 2 mg/kg. d Antisterone : 2~ 4 mg/kg. d Dextran : 10~ 15 ml/kg , after 30~ 60 m, followed by Furosemide (Lasix) at 2 mg/kg.
Induction use of albumin: Albumin + Lasix (20 % salt poor) 1 -Severe edema 2 -Ascites 3 -Pleural effusion 4 -Genital edema 5 -Low serum albumin
Corticosteroid—prednisone therapy: - Prednisone tablets at a dose of 60 mg/m 2/day (maximum daily dose, 80 mg divided into 2 -3 doses) for at least 4 consecutive weeks. After complete absence of proteinuria, prednisone dose should be tapered to 40 mg/m 2/day given every other day as a single morning dose. The alternate-day dose is then slowly tapered and discontinued over the next 2 -3 mo.
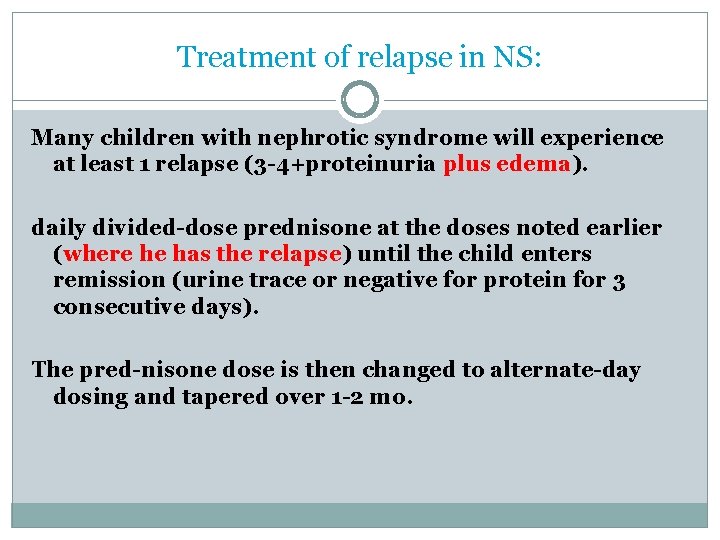
Treatment of relapse in NS: Many children with nephrotic syndrome will experience at least 1 relapse (3 -4+proteinuria plus edema). daily divided-dose prednisone at the doses noted earlier (where he has the relapse) until the child enters remission (urine trace or negative for protein for 3 consecutive days). The pred-nisone dose is then changed to alternate-day dosing and tapered over 1 -2 mo.
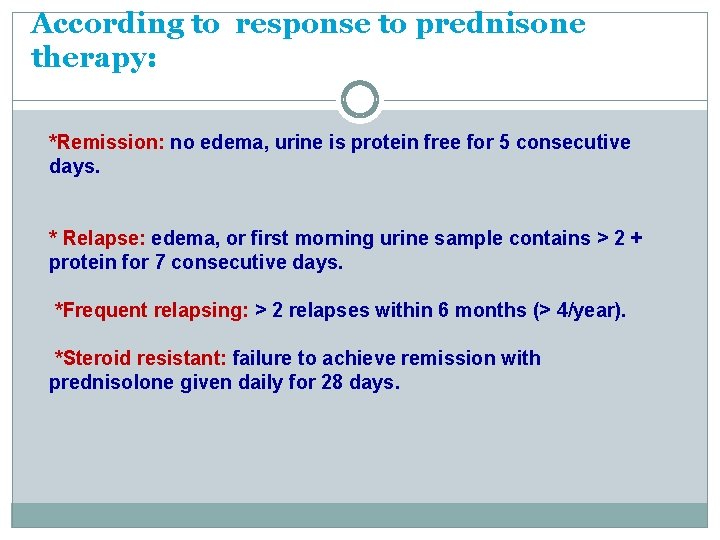
According to response to prednisone therapy: *Remission: no edema, urine is protein free for 5 consecutive days. * Relapse: edema, or first morning urine sample contains > 2 + protein for 7 consecutive days. *Frequent relapsing: > 2 relapses within 6 months (> 4/year). *Steroid resistant: failure to achieve remission with prednisolone given daily for 28 days.
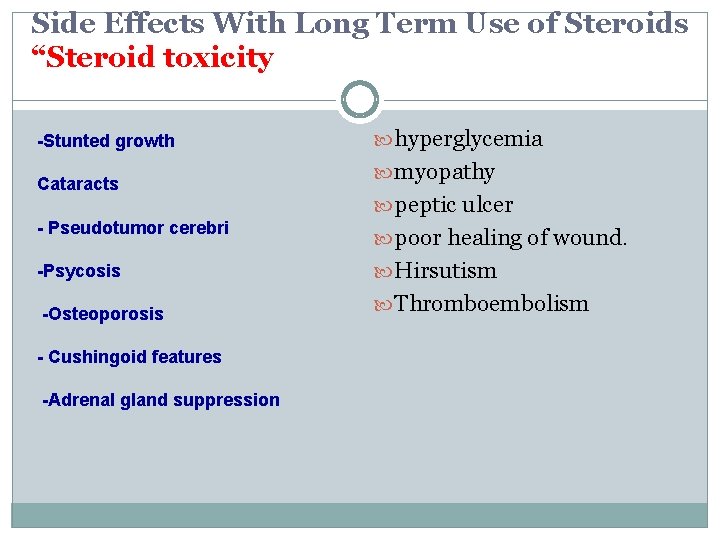
Side Effects With Long Term Use of Steroids “Steroid toxicity -Stunted growth Cataracts hyperglycemia myopathy peptic ulcer - Pseudotumor cerebri poor healing of wound. -Psycosis Hirsutism -Osteoporosis Thromboembolism - Cushingoid features -Adrenal gland suppression
Alternative agent: When can be used: Steroid-dependent patients, frequent relapsers, and steroid- resistant patients. Cyclophosphamide Pulse steroids Cyclosporin A Tacrolimus Microphenolate
THE END…. THANK YOU….
- Slides: 34