Nephrotic Syndrome Dr Shahzad Ahmad Learning Objectives Understand

Nephrotic Syndrome Dr Shahzad Ahmad
Learning Objectives Understand define nephrotic and nephritic syndromes. Describe the initial investigations and management of nephrotic and nephritic syndromes. Describe the complications of nephrotic and nephritic syndromes.
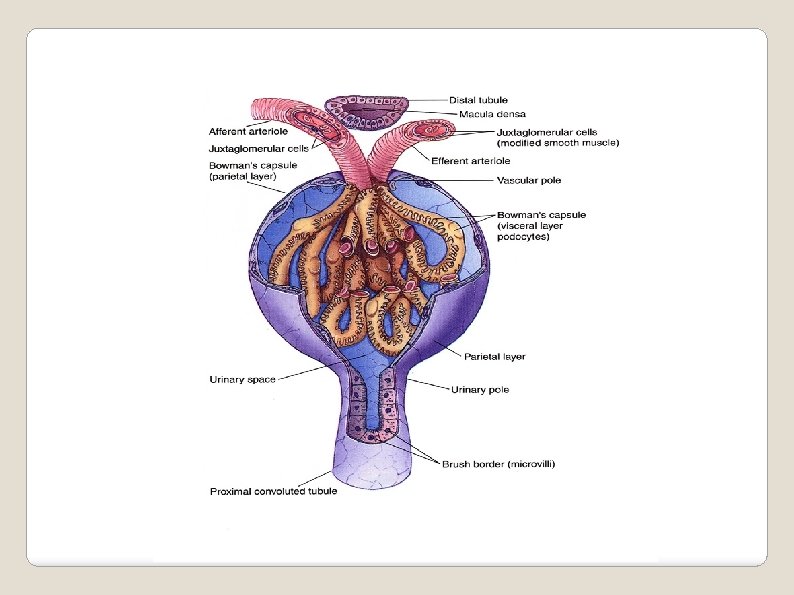
Glomerulus – capillary loop with basement membrane which allows passage of specific molecules into the nephron Glomerulus
Draw a Glomerulus!
Glomerulonephritis – inflammation/damage of the glomerular basement membrane resulting in altered function. Can present as nephrotic and/or nephritic syndrome. (Syndrome- a complex of signs and symptoms resulting from a common cause. ) Glomerulonephritis
What is nephrotic syndrome? Increased permeability of the glomerulus leading to loss of proteins into the tubules.
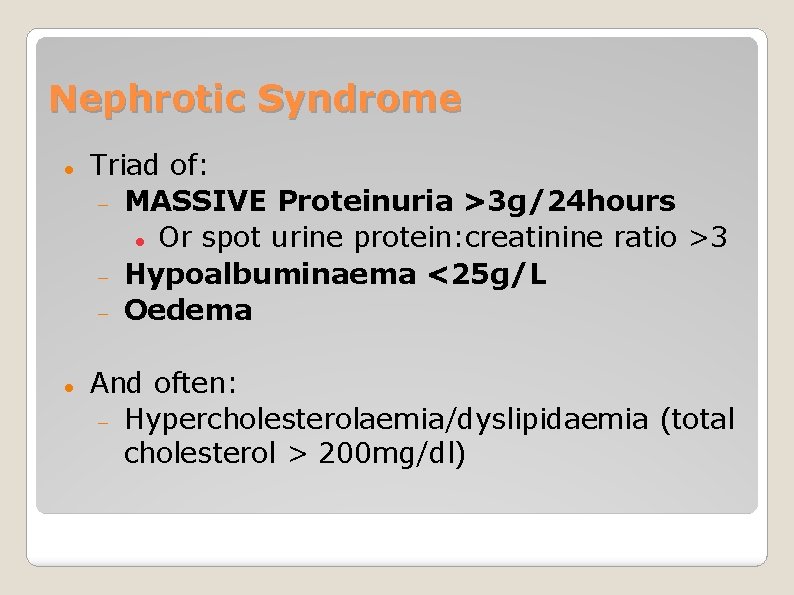
Nephrotic Syndrome Triad of: MASSIVE Proteinuria >3 g/24 hours Or spot urine protein: creatinine ratio >3 Hypoalbuminaema <25 g/L Oedema And often: Hypercholesterolaemia/dyslipidaemia (total cholesterol > 200 mg/dl)
Proteinuria can be caused by glomerular dysfunction, tubular dysfunction, or systemic overproduction. It is important to identify patients in whom the proteinuria is a manifestation of substantial glomerular disease. Proteinuria
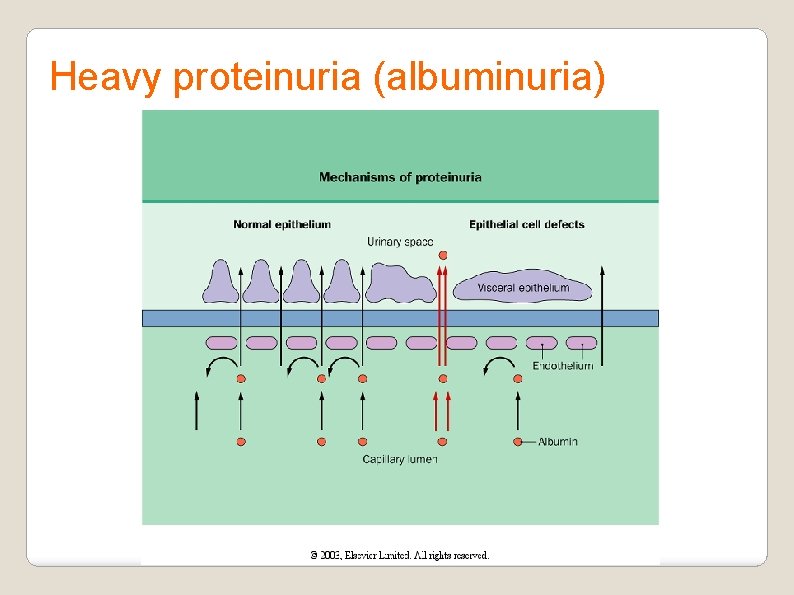
Heavy proteinuria (albuminuria)
Hypoalbuminemia is in part a consequences of urinary protein loss. It is also due to the catabolism of filtered albumin by the proximal tubule as well as to redistribution of albumin within the body.
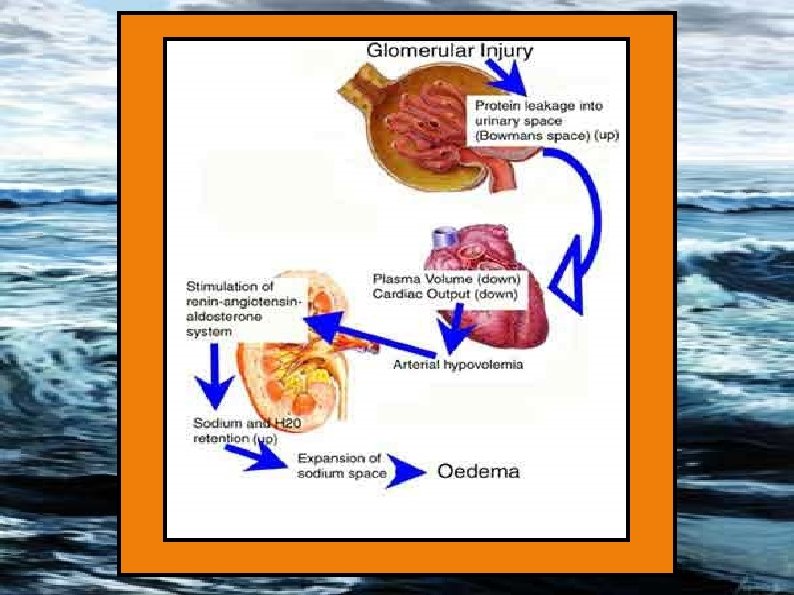
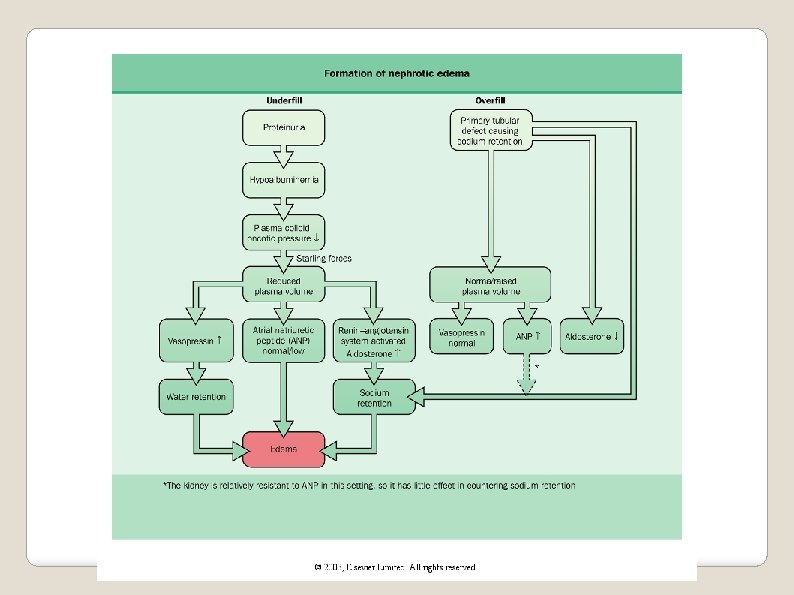
Edema The salt and volume retention in the NS may occur through at least two different major mechanisms.
In the classic theory, proteinuria leads to hypoalbuminemia, a low plasma oncotic pressure, and intravascular volume depletion. Subequent underperfusion of the kidney stimulates the sodium-retentive hormonal systems such as the RAS axis, causing increased renal sodium and volume retention, In the peripheral capillaries with normal hydrostatic pressures and decreased oncotic pressure, lead to transcapillary fluid leakage and edema. Edema
• In some patients, however, the intravascular volume found to be increased along with suppression of the RAS axis resulting in renal sodium retention at a distal nephron site, perhaps due to altered responsiveness to hormones such as atrial natriuretic factor. Edema
Hyperlipidemia Most nephrotic patients have elevated levels of total and low-density lipoprotein (LDL) cholesterol with low or normal high-density lipoprotein (HDL) cholesterol. Nephrotic patients often have a hypercoagulable state and are predisposed to deep vein thrombophlebitis, pulmonary emboli, and renal vein thrombosis.
Frothy /Foamy urine Generalised symptoms – lethargy fatigue reduced appetite Swollen abdomen/ facial swelling Unintentional weight gain Decreased urine output Clinical Manifestations
Further possible presentations. . . Oedema, mainly located around the eyes & extremities; especially around the feet & ankles. BP normal/raised Breathlessness: Pleural effusion, fluid overload, AKI DVT/PE/MI
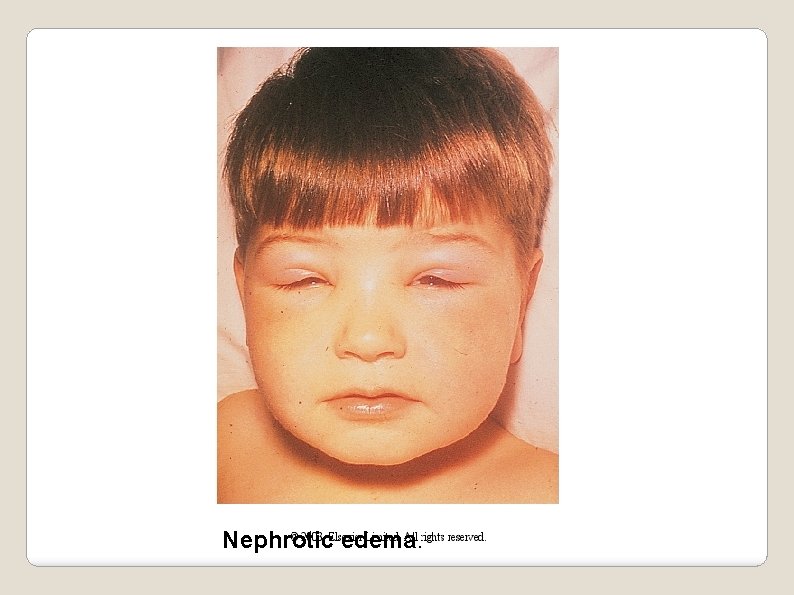
Nephrotic edema.

Nephrotic edema.
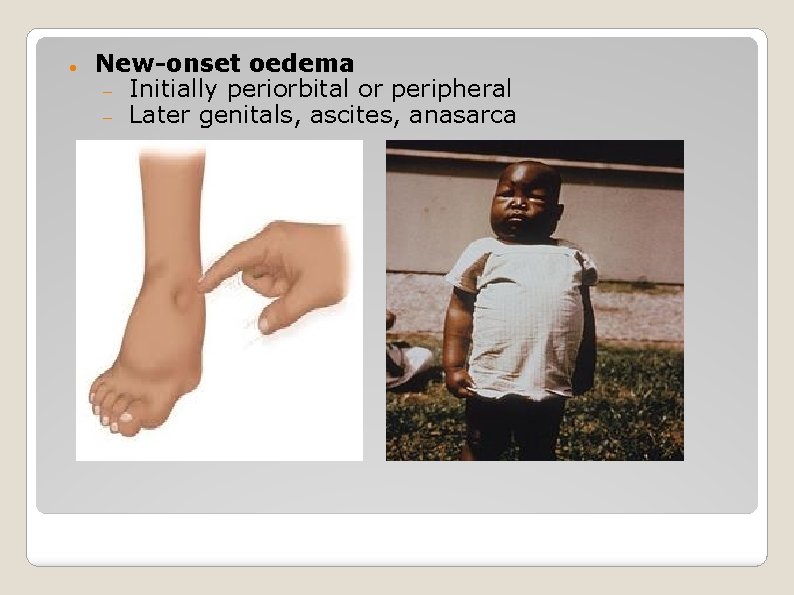
New-onset oedema Initially periorbital or peripheral Later genitals, ascites, anasarca
Causes of Nephrotic Syndrome Primary glomerulonephritis Minimal change disease (80% paeds cases) Focal segmental glomerulosclerosis (most common cause in adults) Membranous glomerulonephritis
Systemic Causes Secondary glomerulonephritis Diabetic nephropathy Sarcoidosis Autoimmune: SLE, Sjogrens Infection: Syphilis, hepatitis B, HIV Amyloidosis Multiple myeloma Vasculitis Cancer Drugs: gold, penicillamine, captopril, NSAIDs
You are a GP with the following patients. . . Young, fit 24 year old male complaining of frothy urine. 10 year old boy with puffy eyes. 74 year old female with multiple comorbidities and swollen ankles.
Differential Diagnosis for Oedema Congestive Cardiac Failure Liver disease Raised JVP, pulmonary oedema, mild proteinuria Hypoalbuminaemia, ascites/oedema What investigations can you do to find a renal cause?
Initial evaluation of the nephrotic patient includes laboratory tests to define whether the patient has primary, idiopathic nephrotic syndrome or a secondary cause related to a systemic disease.
Investigations Urine dipstick and send to lab Urine microscopy Bloods – the usual ones, plus renal screen Immunoglobulins, electrophoresis (myeloma screen), complement (C 3, C 4) autoantibodies (ANA, ANCA, anti-ds. DNA, anti-GBM) Renal ultrasound Renal biopsy (all adults) Children generally trial of steroids first
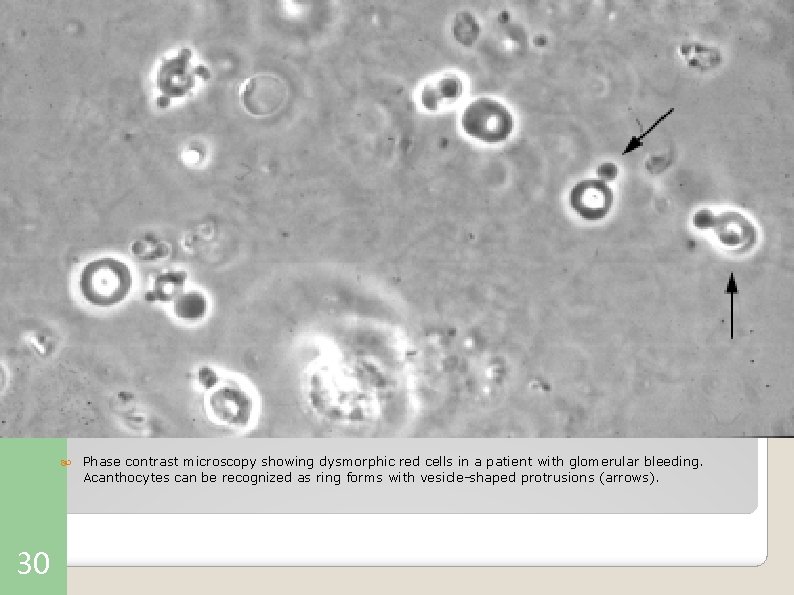
30 Phase contrast microscopy showing dysmorphic red cells in a patient with glomerular bleeding. Acanthocytes can be recognized as ring forms with vesicle-shaped protrusions (arrows).
Treatment 1. General treatment 2. Symptomatic treatment (e. g. diuresis to relieve edema, treating dyslipidemias, anticoagulate treatment, etc. ) 3. Immunosupressive treatment
Monitor I&O, weight, measure abdominal girth, BP Bed rest if pt has extreme edema Assess for electrolyte imbalance Skin care/ gradual increase of activity as edema resolves Sodium restriction General Measures
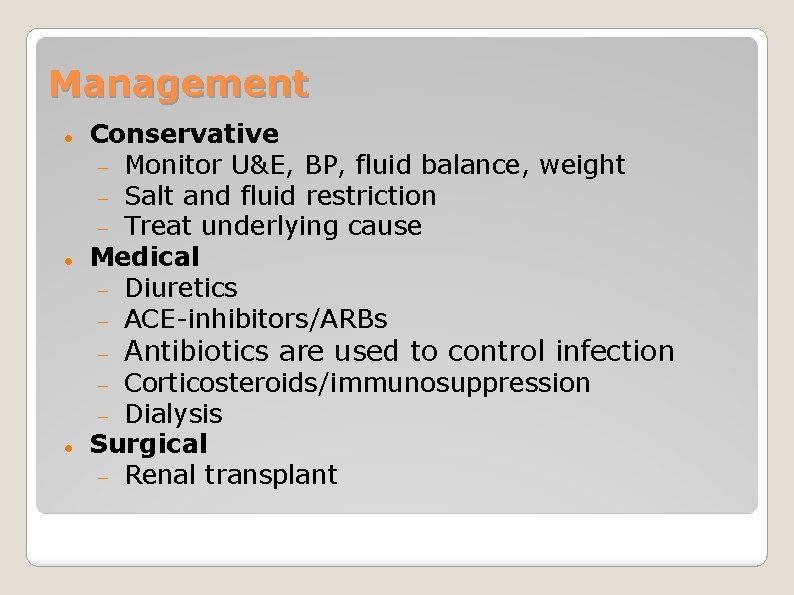
Management Conservative Monitor U&E, BP, fluid balance, weight Salt and fluid restriction Treat underlying cause Medical Diuretics ACE-inhibitors/ARBs Corticosteroids/immunosuppression Dialysis Surgical Renal transplant Antibiotics are used to control infection
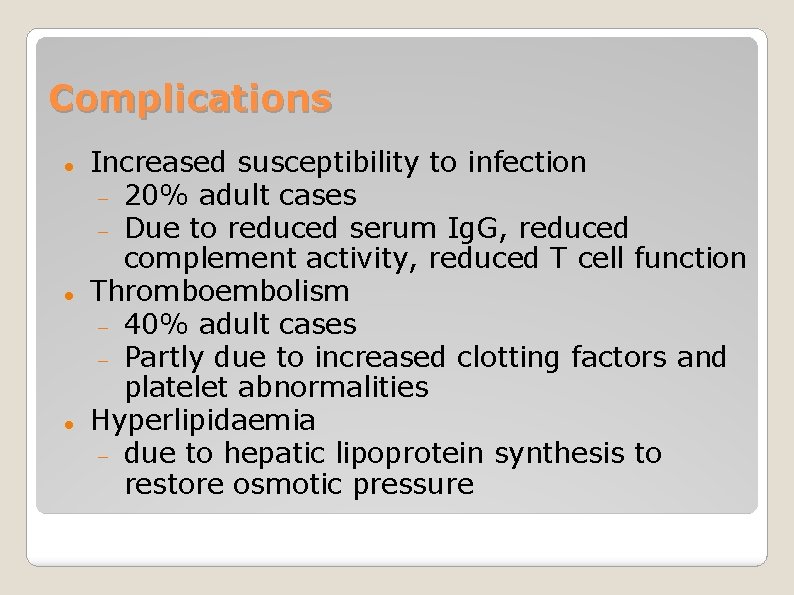
Complications Increased susceptibility to infection 20% adult cases Due to reduced serum Ig. G, reduced complement activity, reduced T cell function Thromboembolism 40% adult cases Partly due to increased clotting factors and platelet abnormalities Hyperlipidaemia due to hepatic lipoprotein synthesis to restore osmotic pressure
Complications It leads to other consequences, such as Protein malnutrition & dyslipidemia In general, the diseases associated with NS cause chronic kidney dysfunction, but rarely they can cause AKI may be seen with minimal change disease, and bilateral renal vein thrombosis.
Medication regimen- type, dosage, side effects, the need to take meds as prescribed Nutrition- low sodium Self-assessment of fluid status- monitor weight, presence of edema Signs/ symptoms indicating need for medical attention (edema, fatigue, headache, infection) Need for follow-up care Patient Teaching
Prognosis Varies With treatment, generally good prognosis Especially minimal change disease (1% progress to ESRF) Without treatment, very poor prognosis Children under 5 or adults older than 30 = worse prognosis

Thank you
- Slides: 39