NEOPLASMS OF THE THYROID PATHOLOGY OF PARATHYROID GLANDS
- Slides: 27
NEOPLASMS OF THE THYROID PATHOLOGY OF PARATHYROID GLANDS BY: Shifaa’ Qa’qa’
Neoplasmas of the thyroid • thyroid nodules Neoplastic ---- benign, malignant Non neoplastic
• Solitary nodules ----- neoplastic • Nodules in younger patients ----- neoplastic • Nodules in males ---- neoplastic • history of radiation treatment to the head and neck------ malignancy • hot nodules ------ benign
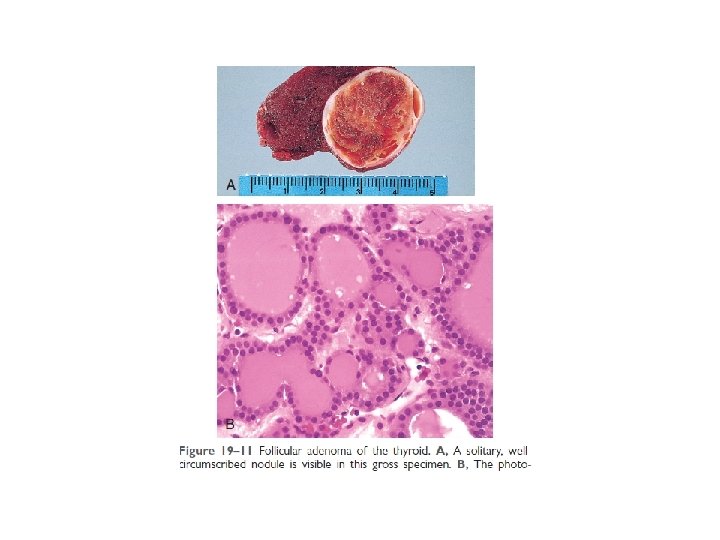
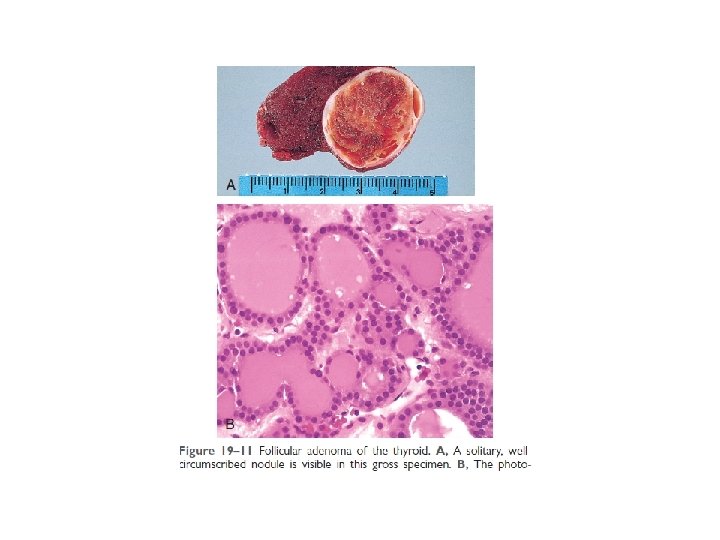
Adenomas • Follicular adenomas • Solitary • Nonfunctional---- M. C--- RAS, PAX 8/PPARG fusion gene • toxic adenomas---- TSHR, α-subunit of Gs (GNAS)--- autonomy---- thyrotoxicosis • Carcinoma ? ?
• well-defined, intact capsule Adenoma----- no invasion Carcinoma----- invasion Multinodular goiter---- no capsule • Uniform follicles
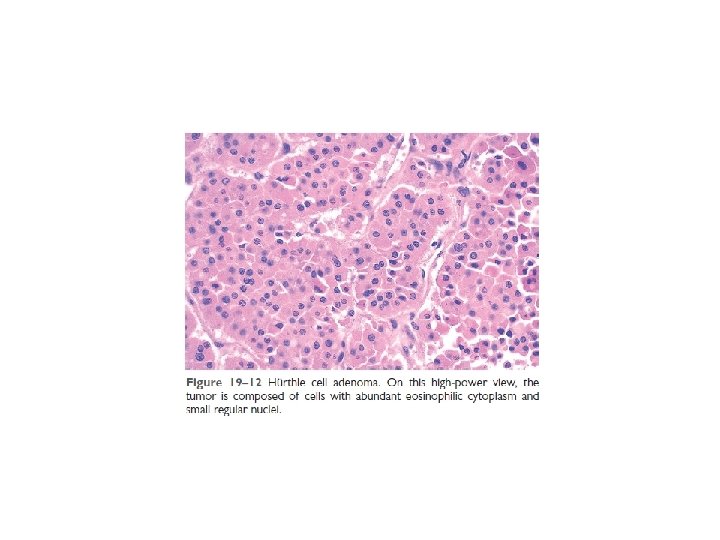
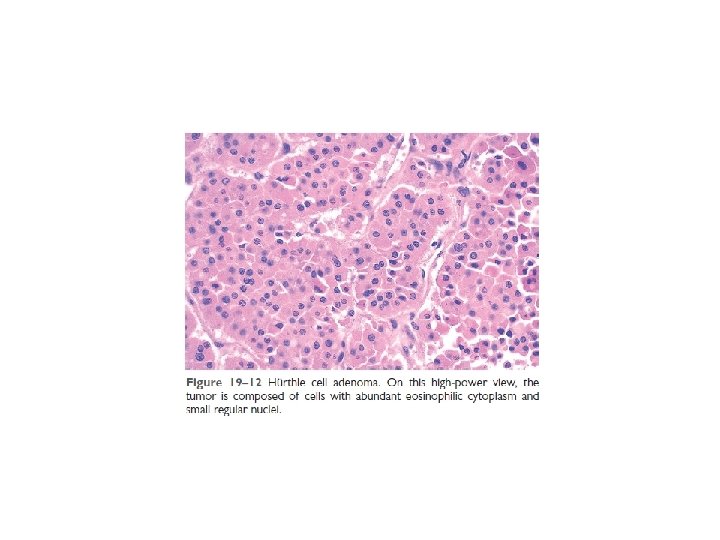
• Hürthle cell adenoma ? ? ? • endocrine atypia ? ?
• cold nodules---10% of cold nodules eventually prove to be malignant. • hot nodules---- malignancy is rare---- toxic adenoma • ultrasonography • fine needle aspiration biopsy (FNA) • Because of the need for evaluating capsular integrity, the definitive diagnosis of thyroid adenoma can be made only after careful histologic examination of the resected specimen.
Carcinomas • Papillary carcinoma (85% of cases) • Follicular carcinoma (5% to 15% of cases) • Anaplastic (undifferentiated) carcinoma (less than 5% of cases) • Medullary carcinoma (5% of cases)
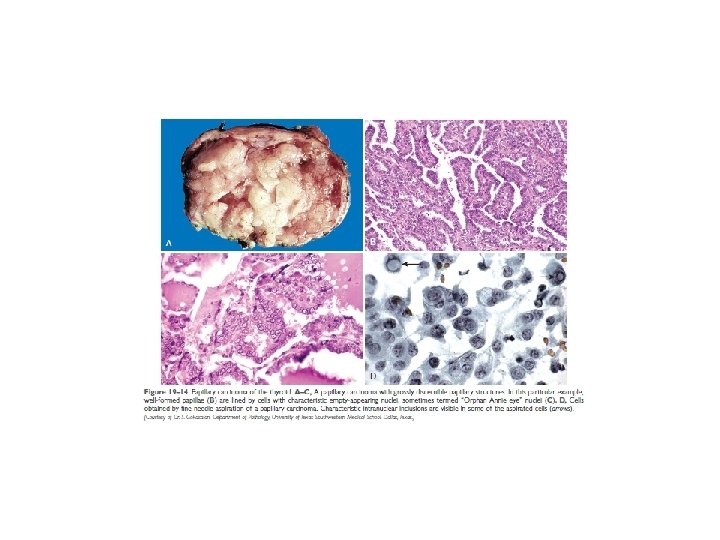
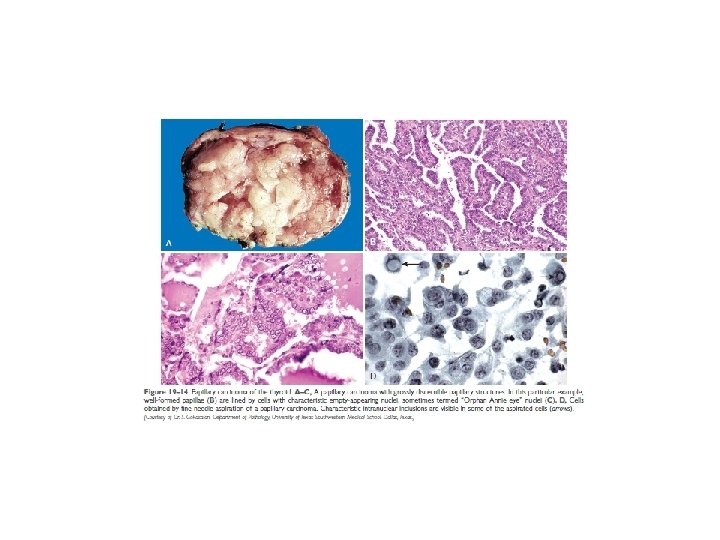
• - Papillary thyroid carcinomas: m. c ionizing radiation nonfunctional tumors - Activation of the MAP kinase pathway: Rearrangements of RET (RET/PTC) BRAF - nuclear features ? ? ? Papillae ? ? lymphatic permeation, LN - indolent lesions, with 10 -year survival rates in excess of 95%.
• - Follicular thyroid carcinomas: older age than that typical for papillary carcinoma iodine deficiency Solitary cold thyroid nodules - mutations in the PI-3 K/AKT signaling pathway: RAS and PIK 3 CA PTEN PAX 8/PPARG fusion genes - widely invasive minimally invasive - hematogenous dissemination surgical excision, radioactive iodine
• Anaplastic Carcinoma: - undifferentiated - Mortality rate approaching 100% (mets, local effect) - mean age of 65 years - giant cells - Spindle cells
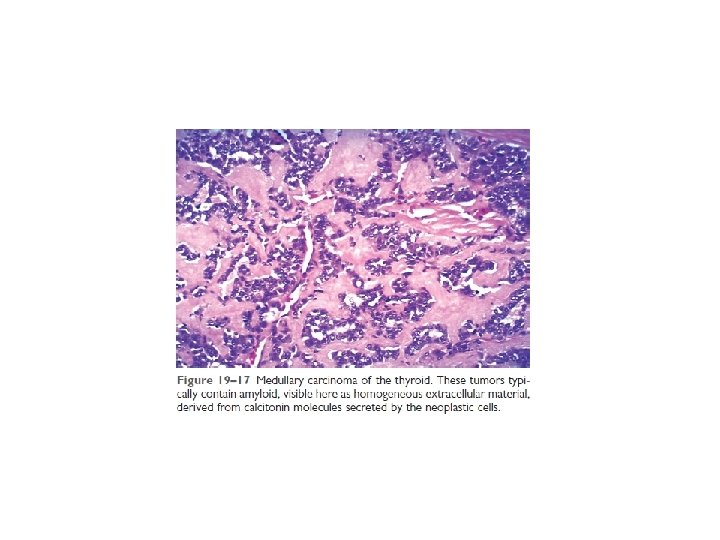
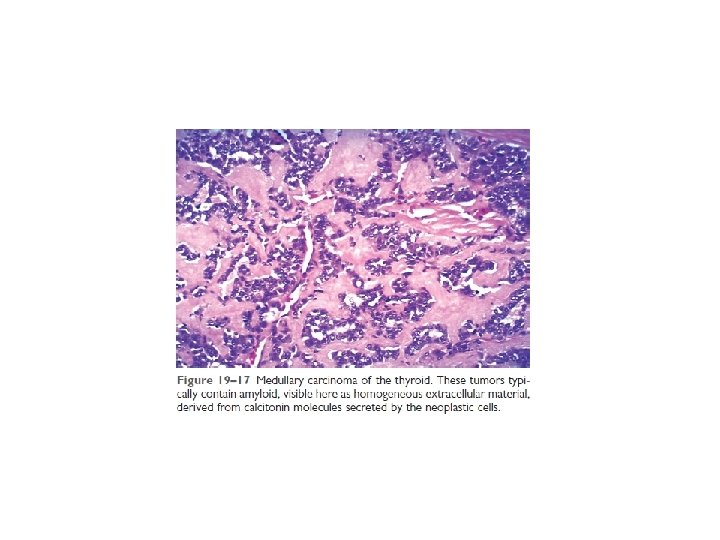
• Medullary Carcinoma: - parafollicular cells, or C cells----neuroendocrine neoplasms - Sporadically familial cases (30%)---- MEN syndrome 2 A, 2 B, familial medullary thyroid carcinoma - RET mutations Multicentricity? ? multicentric C cell hyperplasia? ? - Mass peptide hormone
PARATHYROID GLANDS • free (ionized) calcium
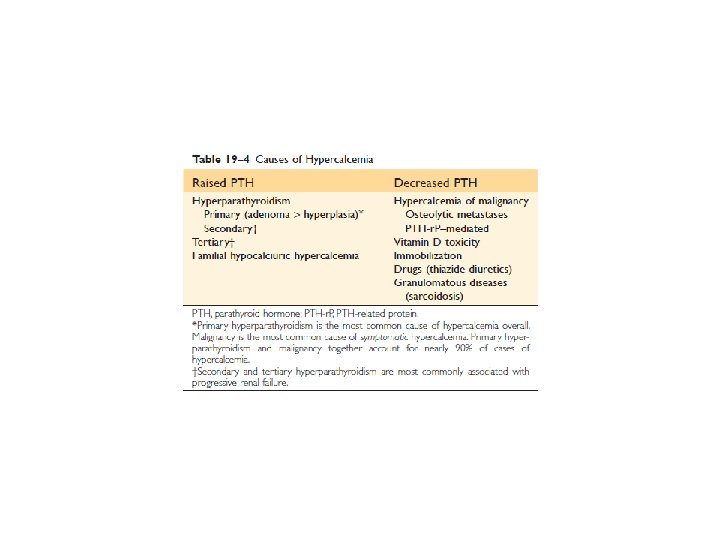
HYPERPARATHYROIDISM • primary • Secondary • tertiary
• Primary Hyperparathyroidism: - Adenoma— 85% to 95% - Primary hyperplasia (diffuse or nodular)— 5% to 10% - Parathyroid carcinoma— 1% - Sporadic----- m. c---- Cyclin D 1, MEN 1 - Familial ------ MEN 1, MEN 2 A, Familial hypocalciuric hypercalcemia - hypercalcemia
parathyroid adenomas: • By definition, parathyroid adenomas are almost invariably confined to single glands • 0. 5 - 5 g. • dipose tissue is inconspicuous within adenomas • rim of compressed, non-neoplastic parathyroid tissue, generally separated by a fibrous capsule
Parathyroid hyperplasia: Multiglandular process weight of all glands rarely exceeds 1. 0 g Parathyroid carcinomas: exceed 10 g in weight invasion of surrounding tissues and metastasis
• Morphologic changes in other organs: osteitis fibrosa cystica brown tumors Nephrolithiasis Nephrocalcinosis Metastatic calcification
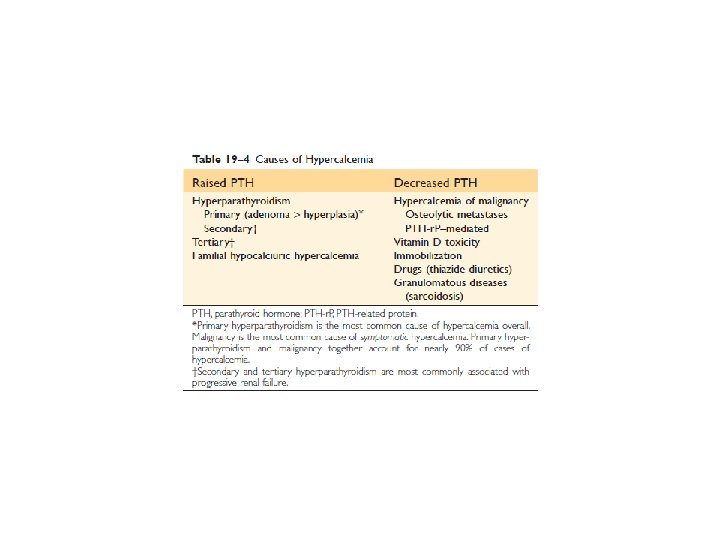
• The most common manifestation of primary hyperparathyroidism is an increase in serum ionized calcium • primary hyperparathyroidism is the most common cause of clinically silent hypercalcemia--- PTH is high, hypophosphatemia • The most common cause of clinically apparent hypercalcemia in adults is paraneoplastic syndromes associated with malignancy and bone metastases
• “painful bones (fractures), renal stones, abdominal groans, and psychic moans. ” • Gastrointestinal disturbances: constipation, nausea, peptic ulcers, pancreatitis, and gallstones • Central nervous system alterations: depression, lethargy, and seizures • Neuromuscular abnormalities: weakness and hypotonia • Polyuria and secondary polydipsia
Secondary Hyperparathyroidism • Renal failure is by far the most common cause of secondary hyperparathyroidism • RF: hyperphosphatemia, hypocalcemia----- Serum calcium remains near normal • The parathyroid glands in secondary hyperparathyroidism are hyperplastic • tertiary hyperparathyroidism
HYPOPARATHYROIDISM • Surgically induced hypoparathyroidism (hyroidectomy) • Congenital absence ? ? ? • Autoimmune hypoparathyroidism • Hypocalcemia: - increased neuromuscular irritability (tingling, muscle spasms, facial grimacing, and sustained carpopedal spasm or tetany), - Cardiac arrhythmias, - increased intracranial pressures and seizures