NEOPLASMS OF THE GASTROINETESTINAL TRACT Prof Dr Ferenc








- Slides: 57
NEOPLASMS OF THE GASTROINETESTINAL TRACT Prof. Dr. Ferenc Szalay 1 st Department of Semmelweis University Budapest, 2005
Neoplasms of the Gastrointestinal Tract Npls of GI tract continue to be the most common malignant tumors Esophagus Stomach Pancreas Liver Biliary tract Small bowel Colon
ESOPHAGUS Squamous cell cc. Adenocarcinoma INCIDENCE 5/100. 000 black men 4 -5 x more comonly affected mail > femail dramatic regional differences in certain areas of China: incidence 1: 1000 adenocarcinoma in western countries
ESOPHAGUS ETIOLOGY and PATHOGENESIS Cause of squamous cell cc. is unknown Enviromental factors: tobacco alcohol abuse lye ingestion, hot tea radiation long term stasis (achalasia) Adenocarcinoma association with Barrett’s GERD inherited disorder: tylosis
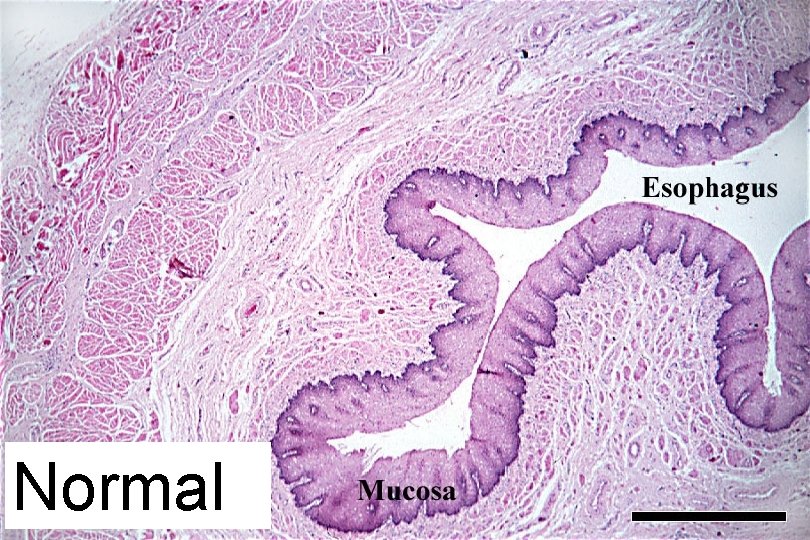
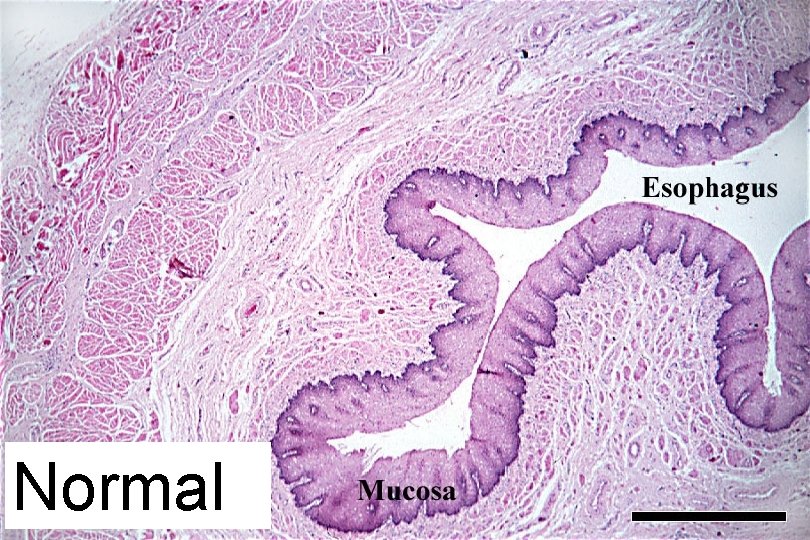
Normal
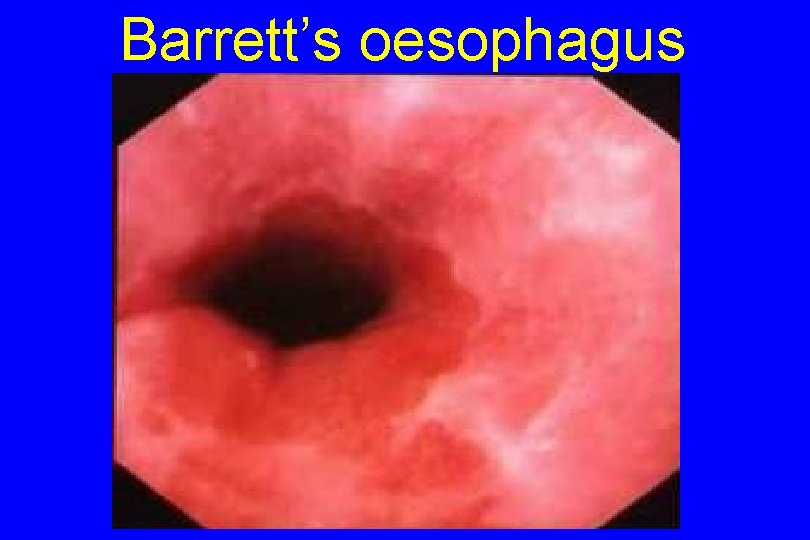
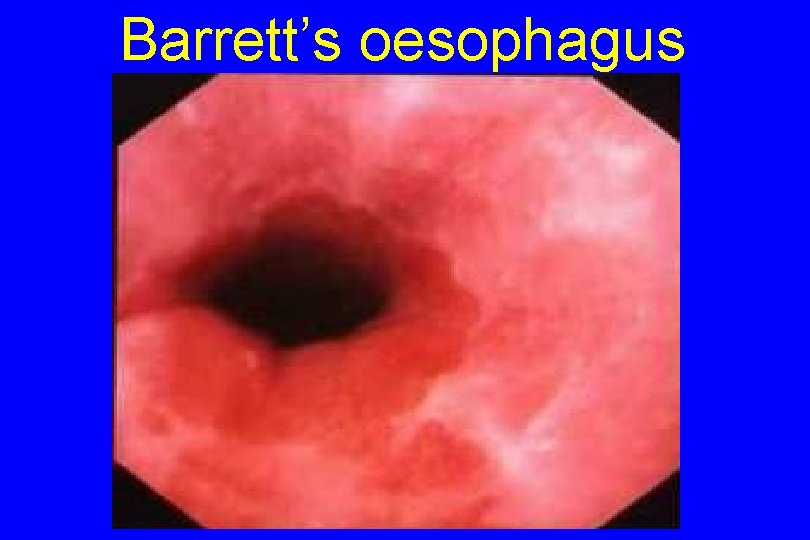
Barrett’s oesophagus
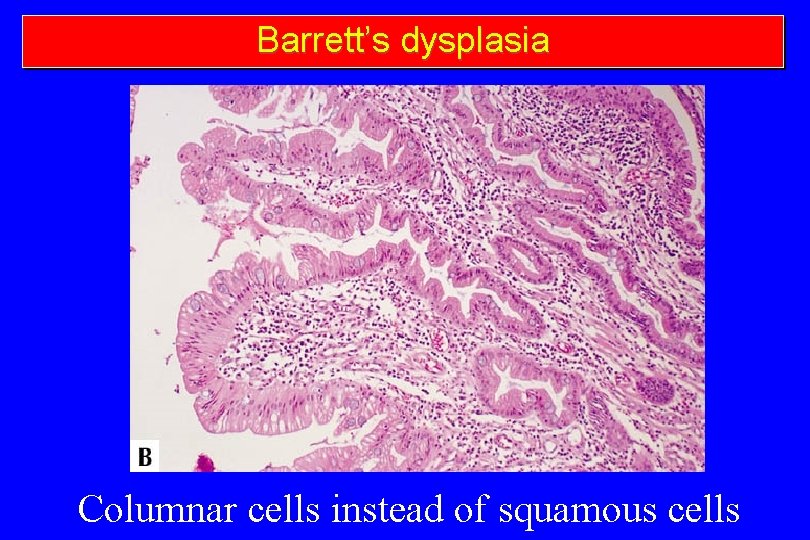
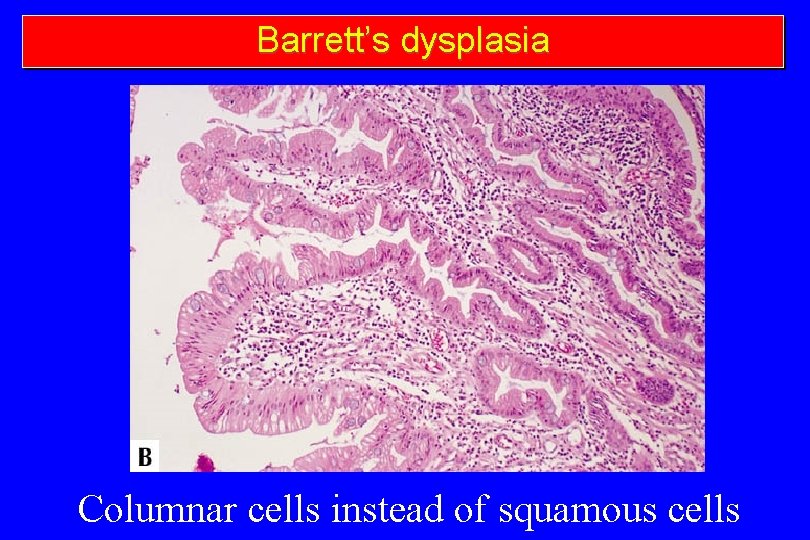
Barrett’s dysplasia Columnar cells instead of squamous cells
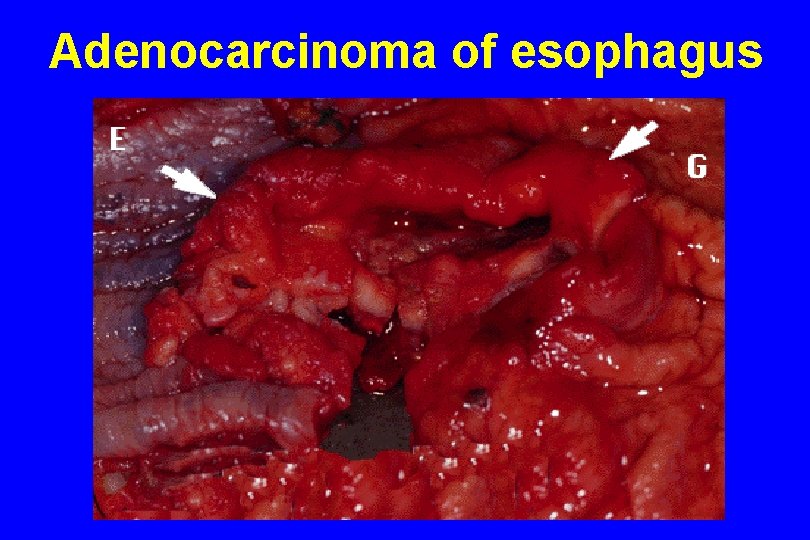
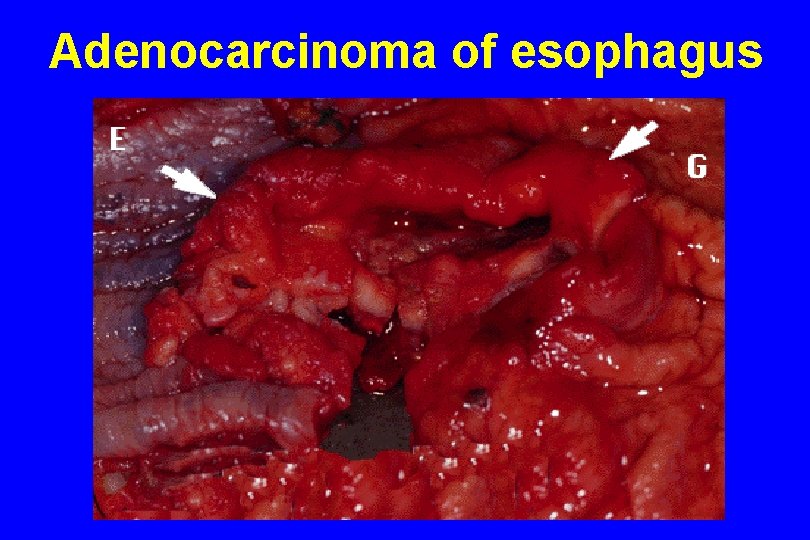
Adenocarcinoma of esophagus
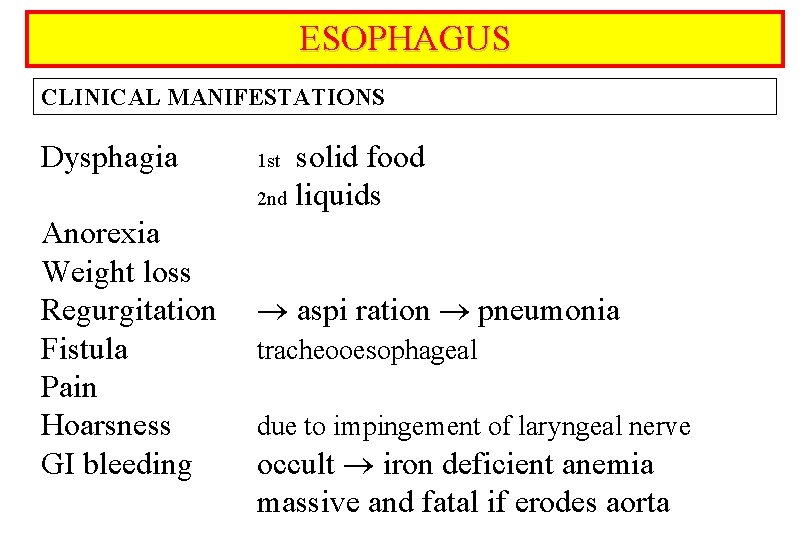
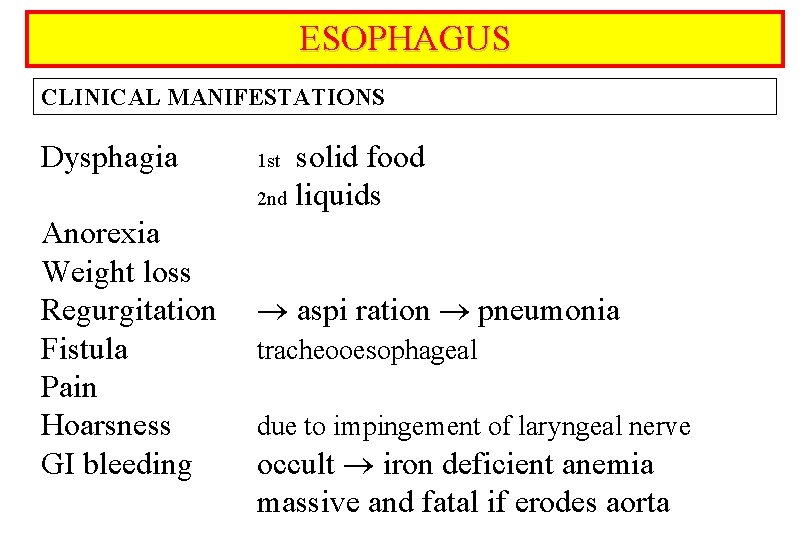
ESOPHAGUS CLINICAL MANIFESTATIONS Dysphagia Anorexia Weight loss Regurgitation Fistula Pain Hoarsness GI bleeding solid food 2 nd liquids 1 st aspi ration pneumonia tracheooesophageal due to impingement of laryngeal nerve occult iron deficient anemia massive and fatal if erodes aorta
ESOPHAGUS COMPLICATIONS Silent Symptomatic Metastatic no serosal lining metastasize early to regional lymph nodes
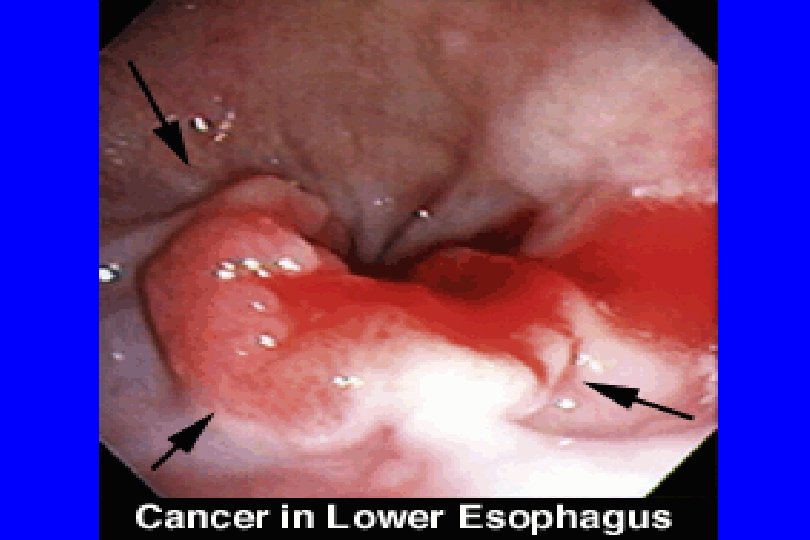
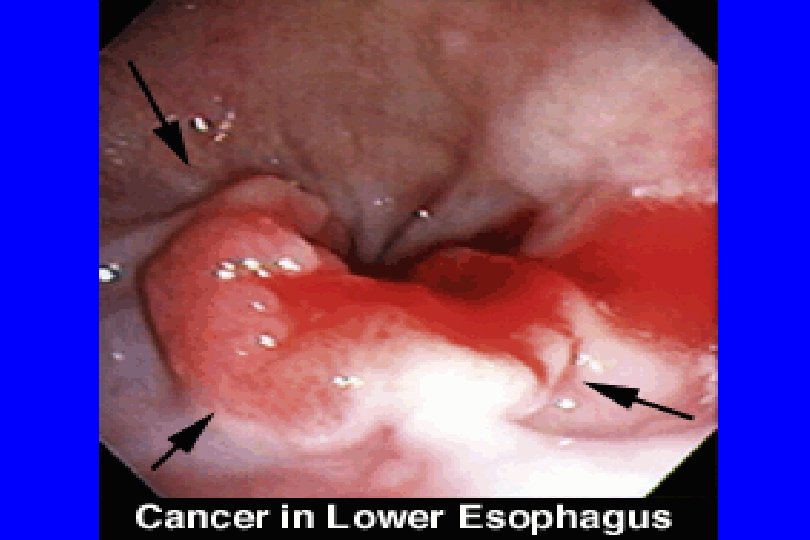
ESOPHAGUS DIAGNOSIS Double contrast barium Endoscopy biopsy - cytology, histology CT Endoscopic ultrasonography
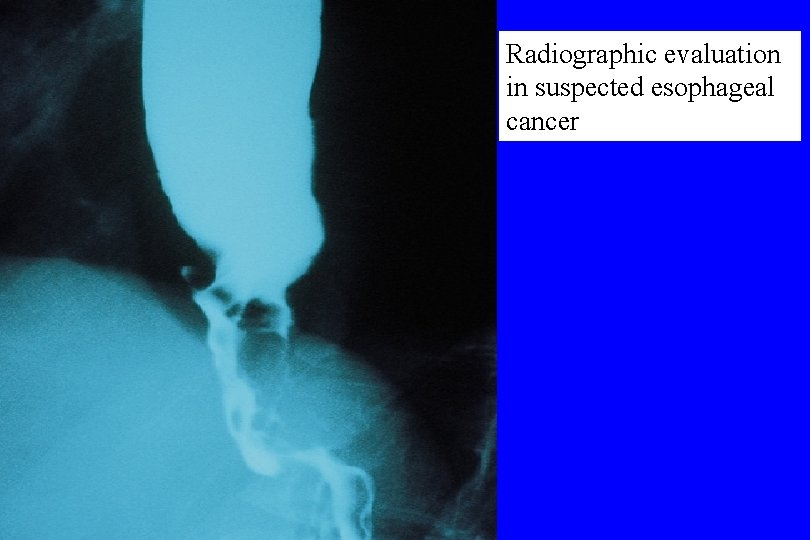
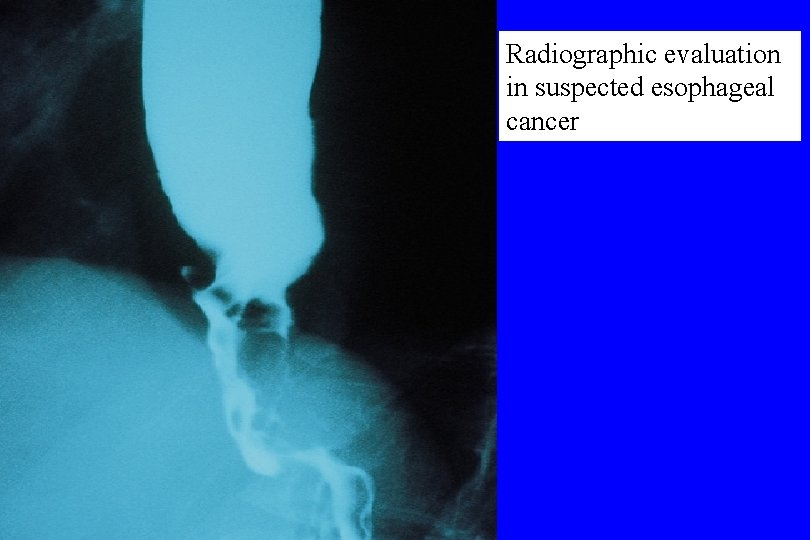
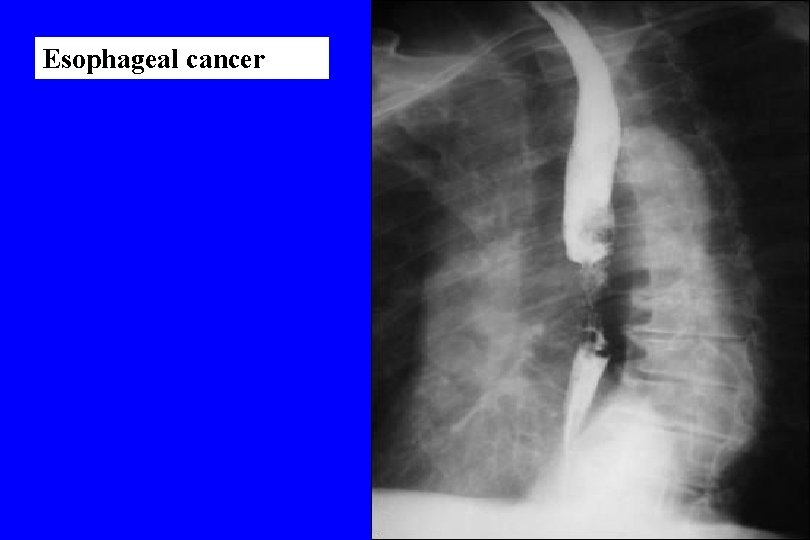
Radiographic evaluation in suspected esophageal cancer
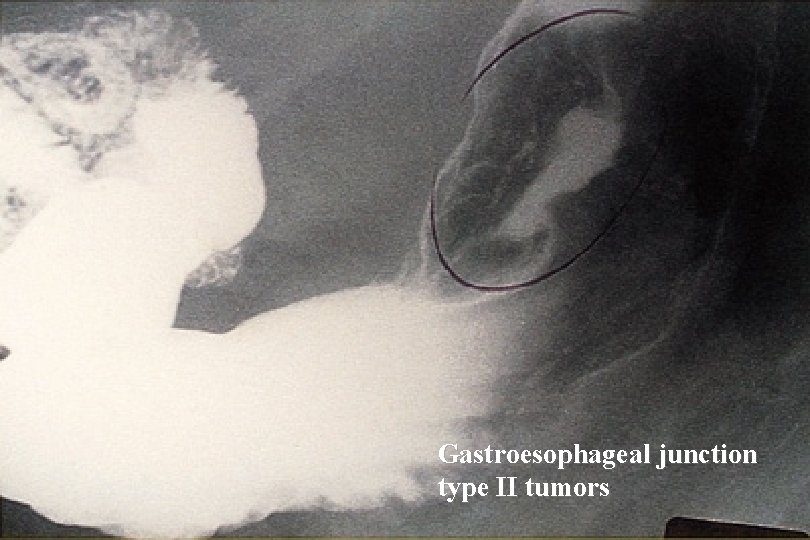
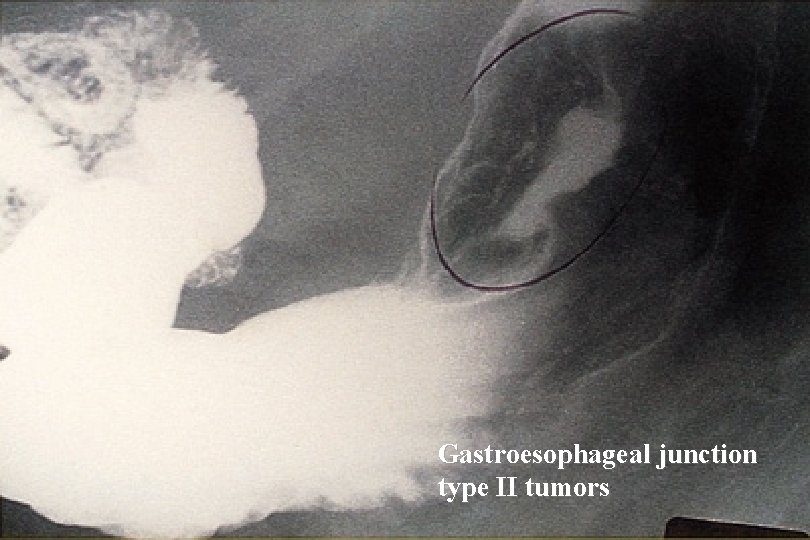
Gastroesophageal junction type II tumors
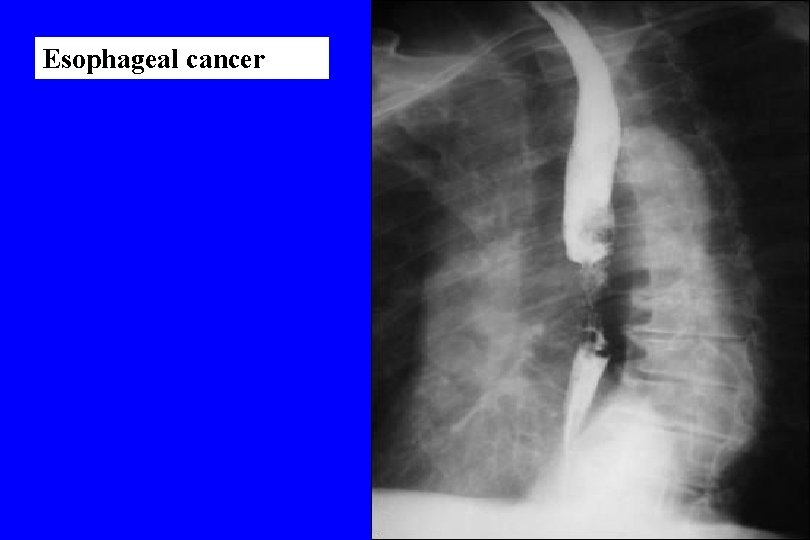
Esophageal cancer
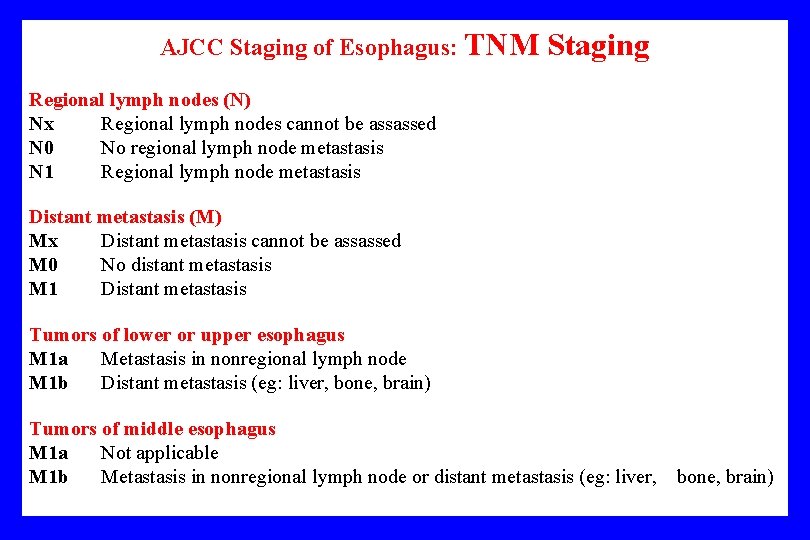
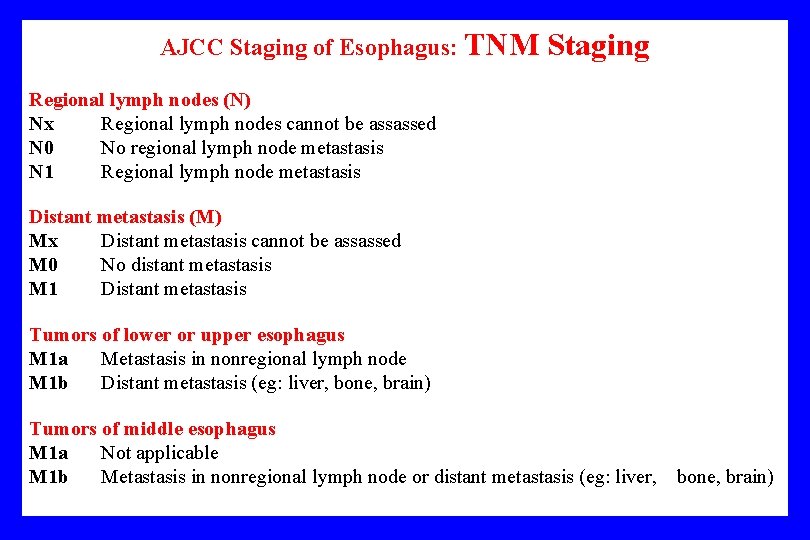
AJCC Staging of Esophagus: TNM Staging Regional lymph nodes (N) Nx Regional lymph nodes cannot be assassed N 0 No regional lymph node metastasis N 1 Regional lymph node metastasis Distant metastasis (M) Mx Distant metastasis cannot be assassed M 0 No distant metastasis M 1 Distant metastasis Tumors of lower or upper esophagus M 1 a Metastasis in nonregional lymph node M 1 b Distant metastasis (eg: liver, bone, brain) Tumors of middle esophagus M 1 a Not applicable M 1 b Metastasis in nonregional lymph node or distant metastasis (eg: liver, bone, brain)
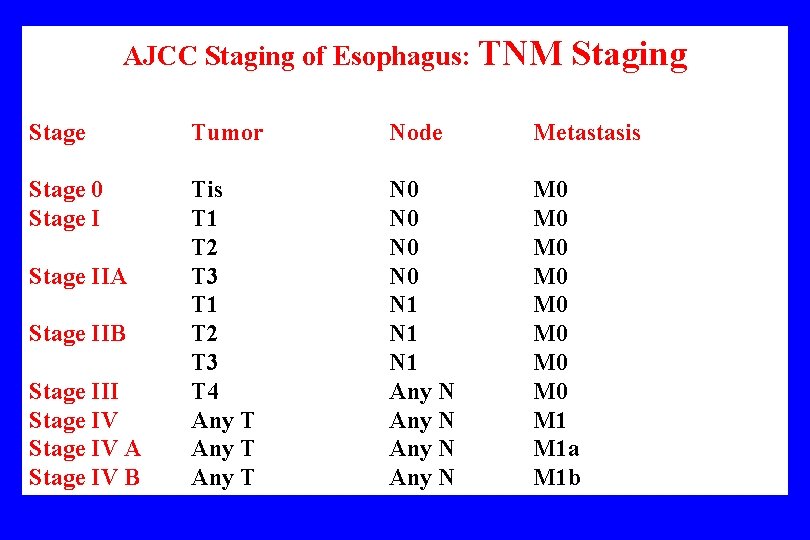
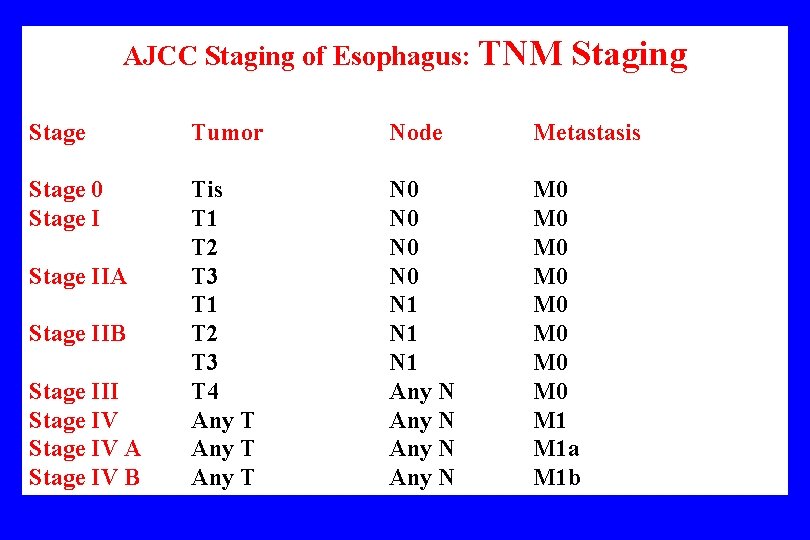
AJCC Staging of Esophagus: TNM Staging Stage Tumor Node Metastasis Stage 0 Stage I Tis T 1 T 2 T 3 T 4 Any T N 0 N 0 N 1 N 1 Any N M 0 M 0 M 1 a M 1 b Stage IIA Stage IIB Stage III Stage IV A Stage IV B
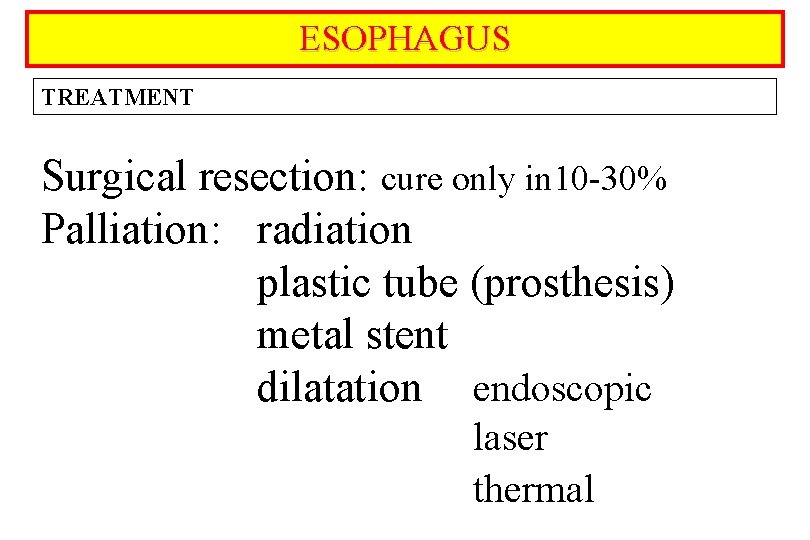
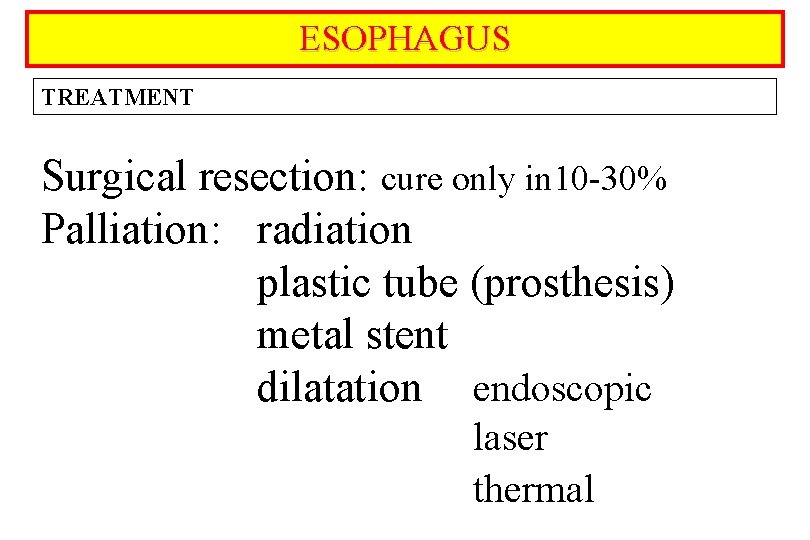
ESOPHAGUS TREATMENT Surgical resection: cure only in 10 -30% Palliation: radiation plastic tube (prosthesis) metal stent dilatation endoscopic laser thermal
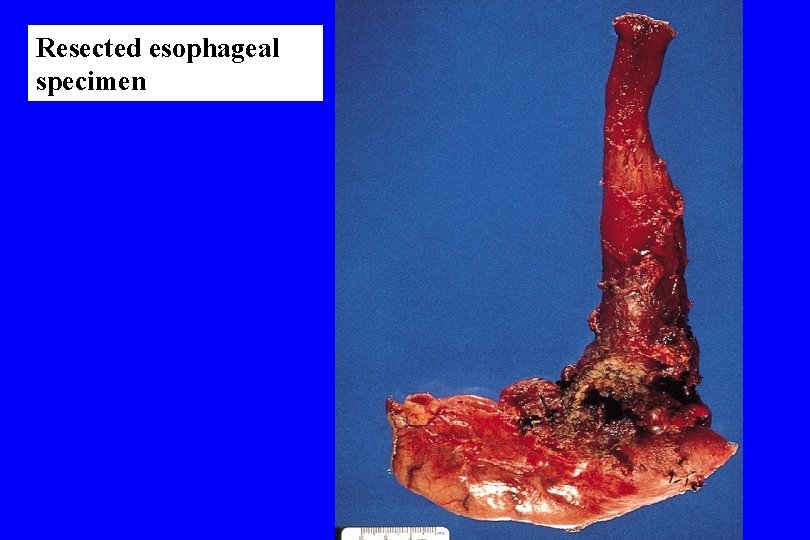
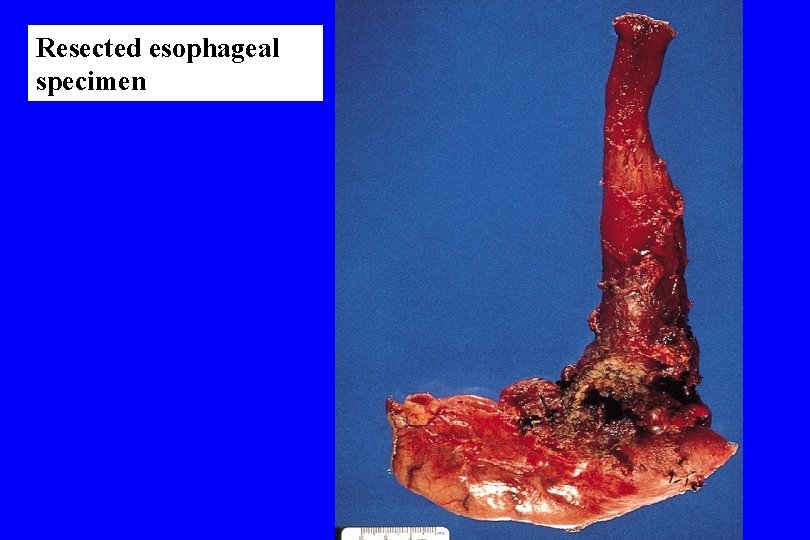
Resected esophageal specimen
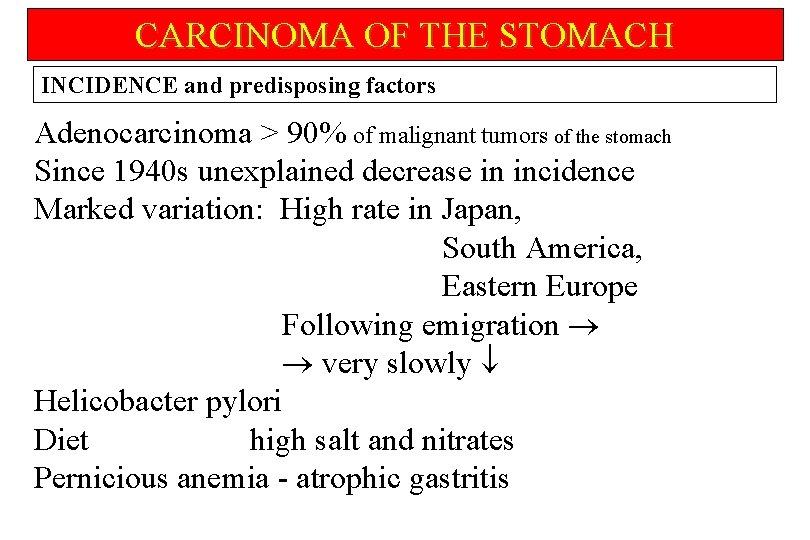
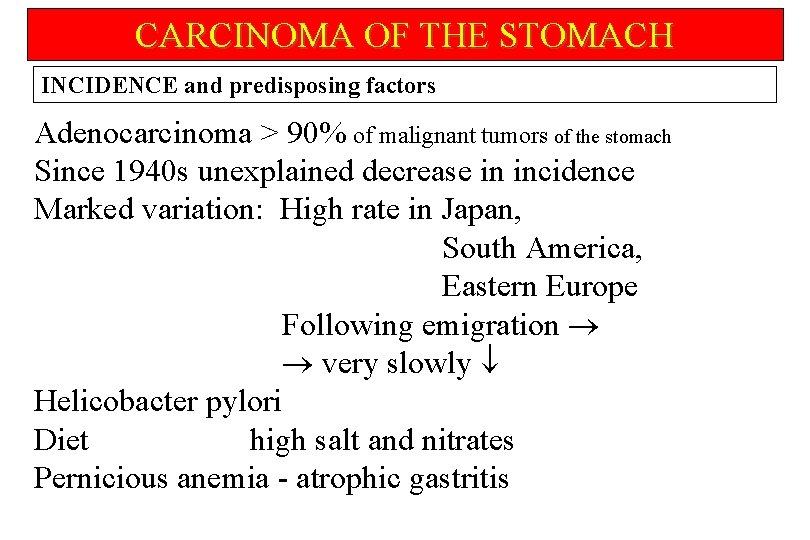
CARCINOMA OF THE STOMACH INCIDENCE and predisposing factors Adenocarcinoma > 90% of malignant tumors of the stomach Since 1940 s unexplained decrease in incidence Marked variation: High rate in Japan, South America, Eastern Europe Following emigration very slowly Helicobacter pylori Diet high salt and nitrates Pernicious anemia - atrophic gastritis

CARCINOMA OF THE STOMACH CLINICAL MANIFESTATIONS Clinical presentation depends on morphologic characteristics: infiltrating or ulcerating size of the tumor presence of gastric outlet obstruction metastatic or nonmetastatic Pain Nausea and vomiting Anorexia Iron deficiency anemia Paraneoplastic signs
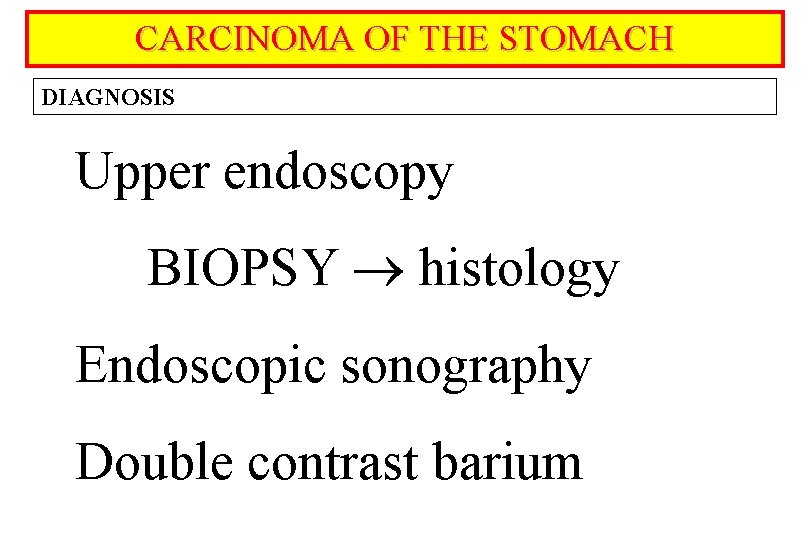
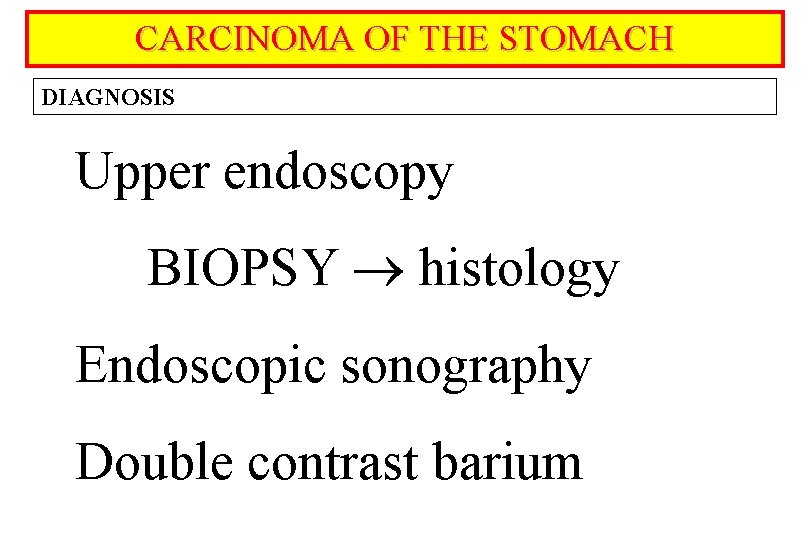
CARCINOMA OF THE STOMACH DIAGNOSIS Upper endoscopy BIOPSY histology Endoscopic sonography Double contrast barium
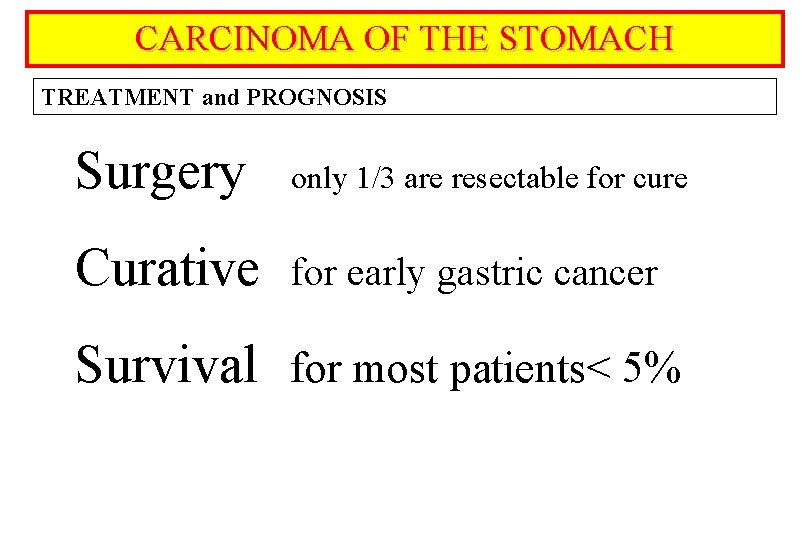
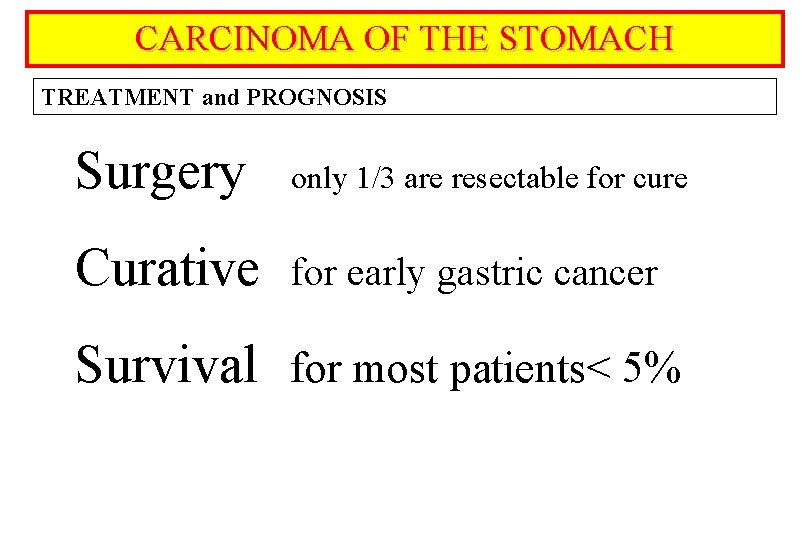
CARCINOMA OF THE STOMACH TREATMENT and PROGNOSIS Surgery only 1/3 are resectable for cure Curative for early gastric cancer Survival for most patients< 5%
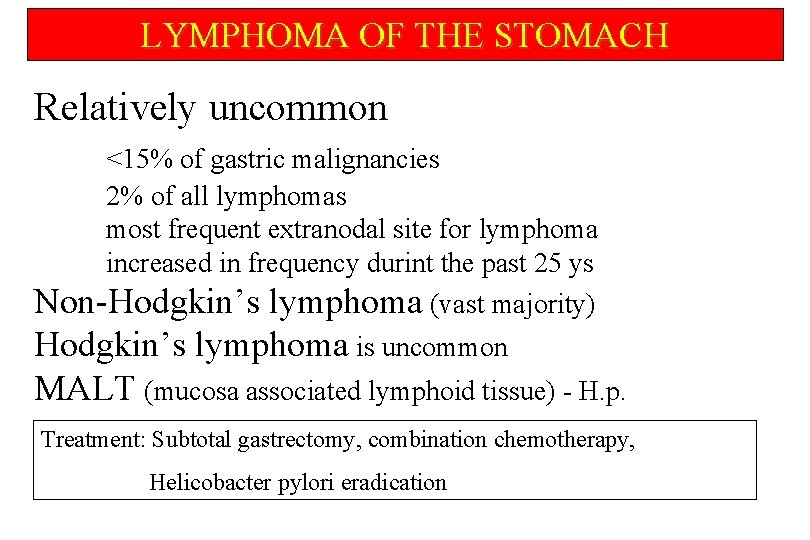
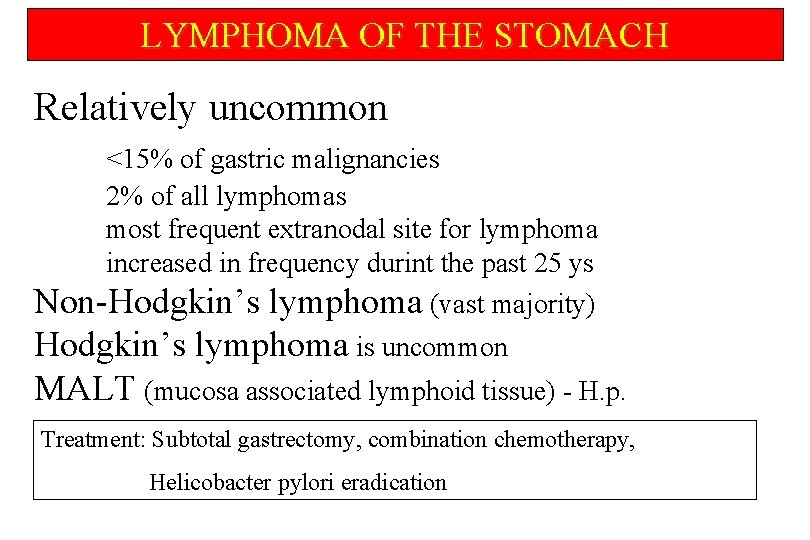
LYMPHOMA OF THE STOMACH Relatively uncommon <15% of gastric malignancies 2% of all lymphomas most frequent extranodal site for lymphoma increased in frequency durint the past 25 ys Non-Hodgkin’s lymphoma (vast majority) Hodgkin’s lymphoma is uncommon MALT (mucosa associated lymphoid tissue) - H. p. Treatment: Subtotal gastrectomy, combination chemotherapy, Helicobacter pylori eradication
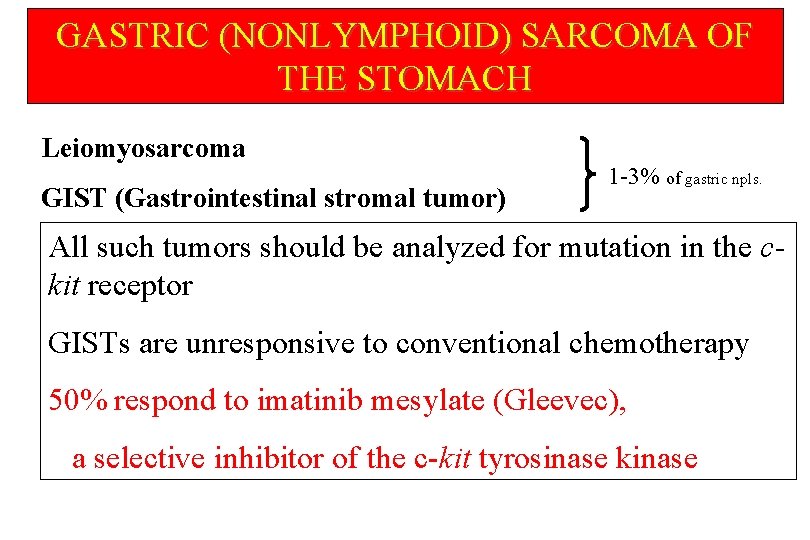
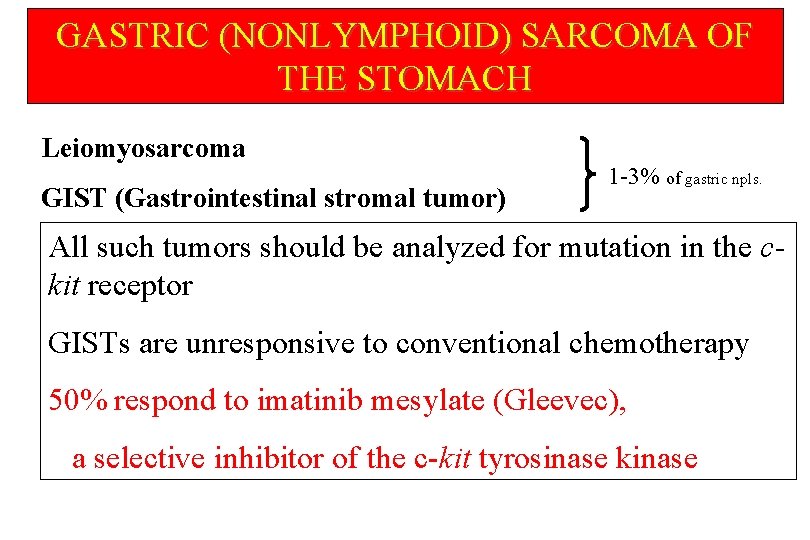
GASTRIC (NONLYMPHOID) SARCOMA OF THE STOMACH Leiomyosarcoma GIST (Gastrointestinal stromal tumor) 1 -3% of gastric npls. All such tumors should be analyzed for mutation in the ckit receptor GISTs are unresponsive to conventional chemotherapy 50% respond to imatinib mesylate (Gleevec), a selective inhibitor of the c-kit tyrosinase kinase

CARCINOMA OF THE COLON INCIDENCE and predisposing factors 3 rd most comon cc. in men, 2 nd in women 3 rd most common cause of cancer death CRC is 15% of all malignant tumors More comon in developed countries Emigrants get the risk characteristic for new enviroment Role of diet Genetic factors
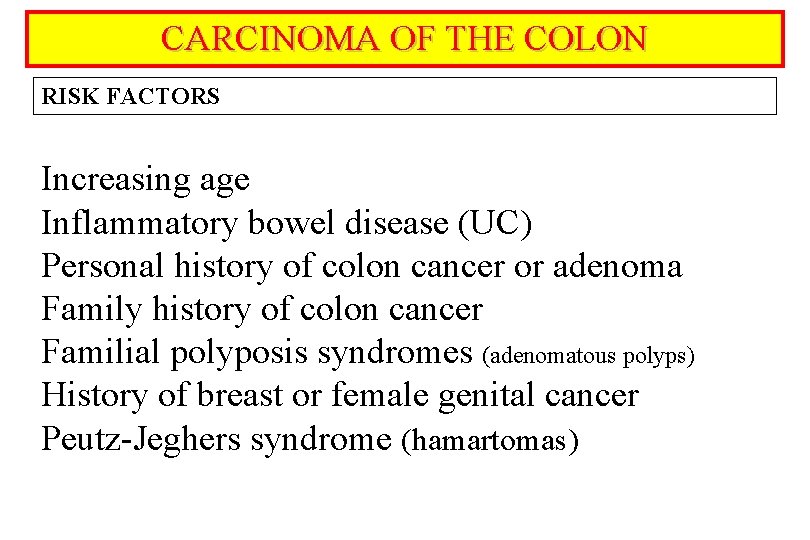
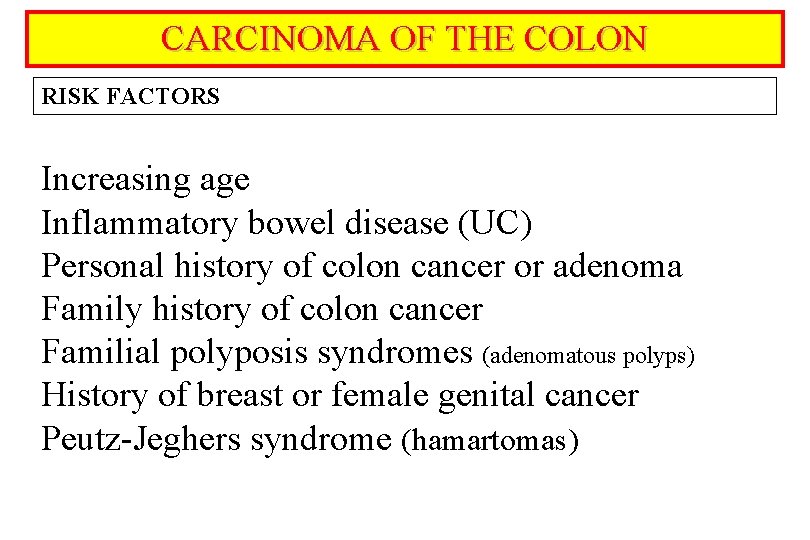
CARCINOMA OF THE COLON RISK FACTORS Increasing age Inflammatory bowel disease (UC) Personal history of colon cancer or adenoma Family history of colon cancer Familial polyposis syndromes (adenomatous polyps) History of breast or female genital cancer Peutz-Jeghers syndrome (hamartomas)
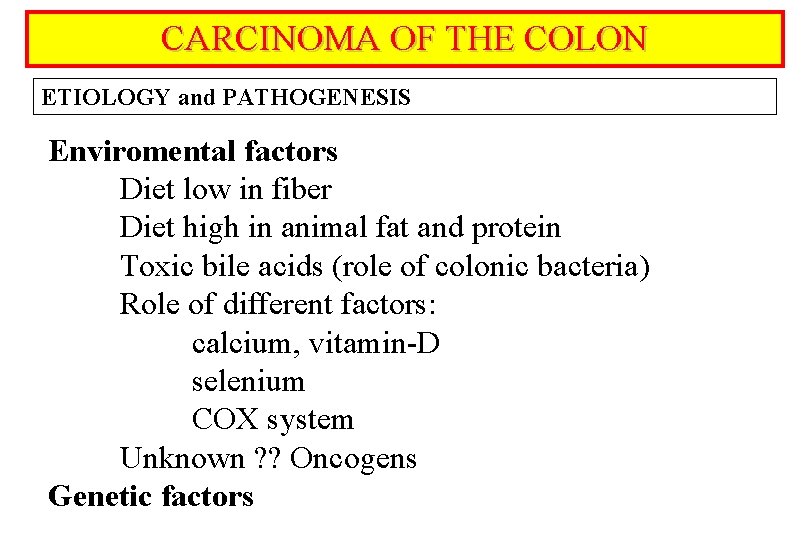
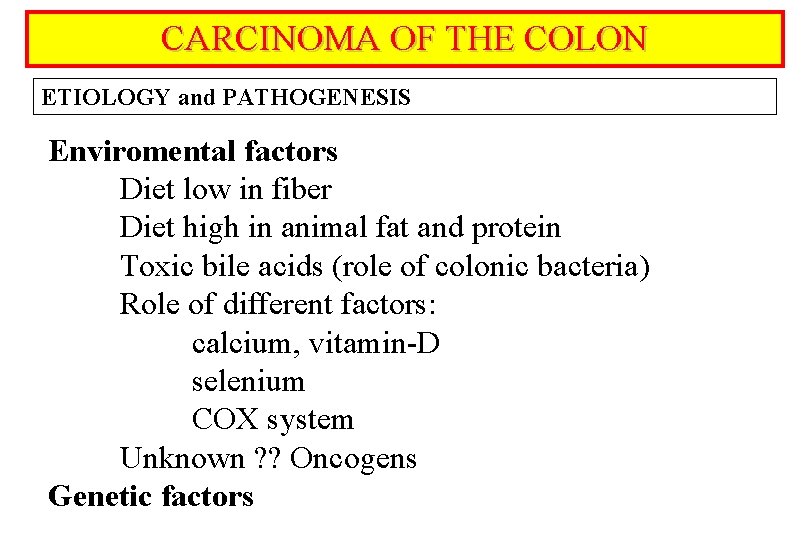
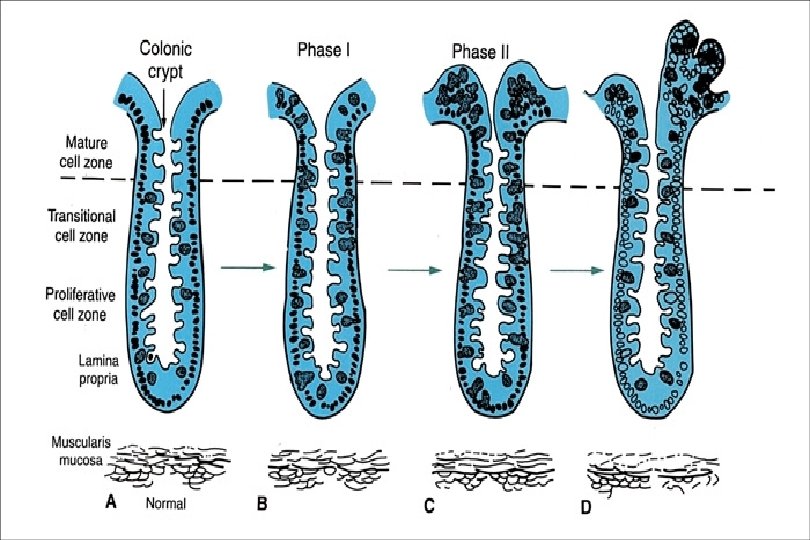
CARCINOMA OF THE COLON ETIOLOGY and PATHOGENESIS Enviromental factors Diet low in fiber Diet high in animal fat and protein Toxic bile acids (role of colonic bacteria) Role of different factors: calcium, vitamin-D selenium COX system Unknown ? ? Oncogens Genetic factors
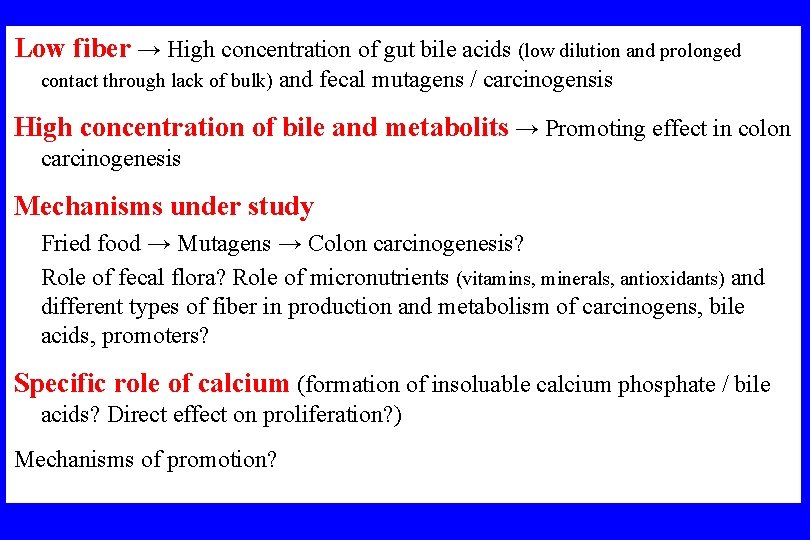
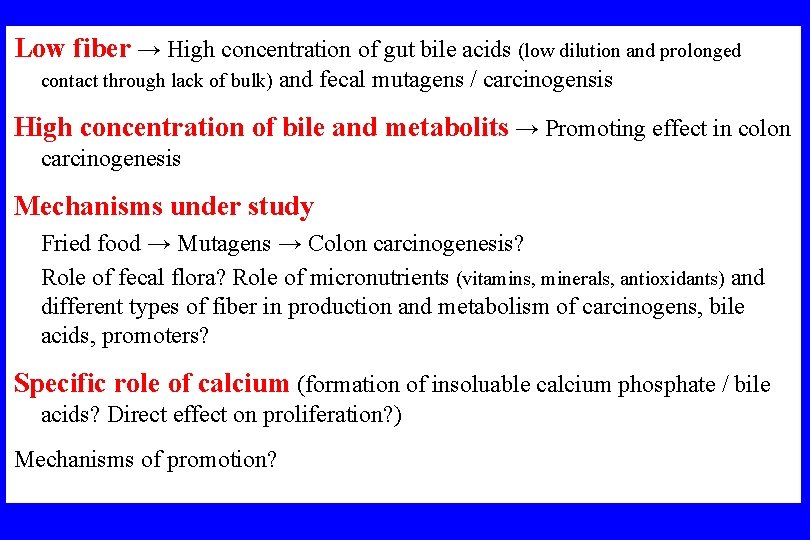
Low fiber → High concentration of gut bile acids (low dilution and prolonged contact through lack of bulk) and fecal mutagens / carcinogensis High concentration of bile and metabolits → Promoting effect in colon carcinogenesis Mechanisms under study Fried food → Mutagens → Colon carcinogenesis? Role of fecal flora? Role of micronutrients (vitamins, minerals, antioxidants) and different types of fiber in production and metabolism of carcinogens, bile acids, promoters? Specific role of calcium (formation of insoluable calcium phosphate / bile acids? Direct effect on proliferation? ) Mechanisms of promotion?
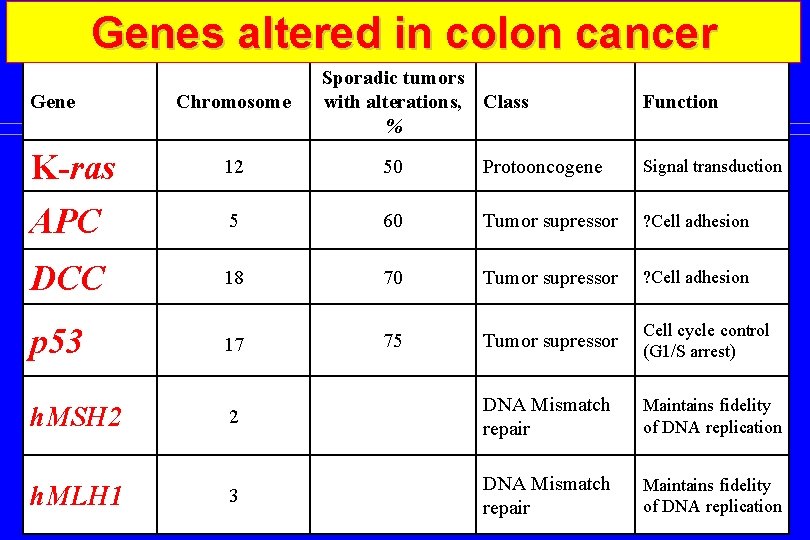
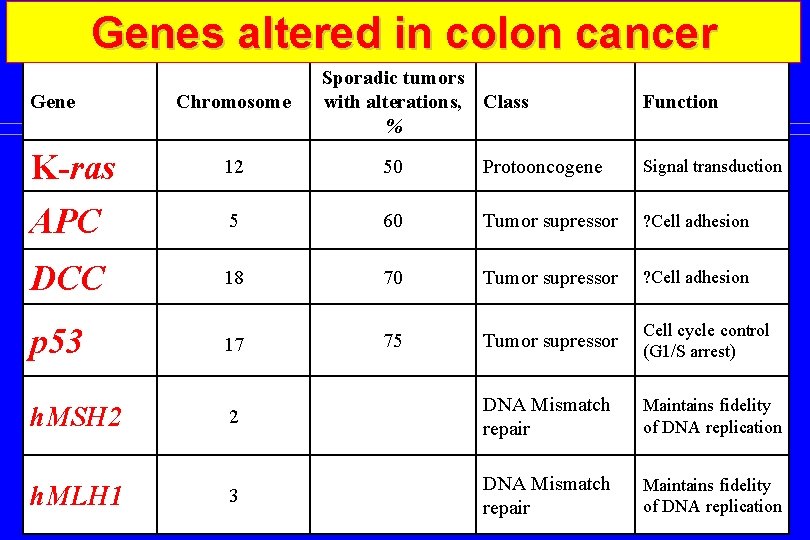
Genes altered in colon cancer Gene Chromosome Sporadic tumors with alterations, Class % Function K-ras 12 50 Protooncogene Signal transduction APC 5 60 Tumor supressor ? Cell adhesion DCC 18 70 Tumor supressor ? Cell adhesion p 53 17 75 Tumor supressor Cell cycle control (G 1/S arrest) h. MSH 2 2 DNA Mismatch repair Maintains fidelity of DNA replication h. MLH 1 3 DNA Mismatch repair Maintains fidelity of DNA replication

CARCINOMA OF THE COLON CLINICAL MANIFESTATIONS Few early warning signs Depend on location, size, bleeding tendency GI blood loss occult blood melaena hematochezia Alteration of bowel habits (left sided or distal tumors) Owerflow diarrhea (severe but incomplete obstruction) Abdominal pain (uncommon, obstuction related) Weight loss, anorexia (nonspecific, appear late) Perforation, malignant ascites, liver metastasis
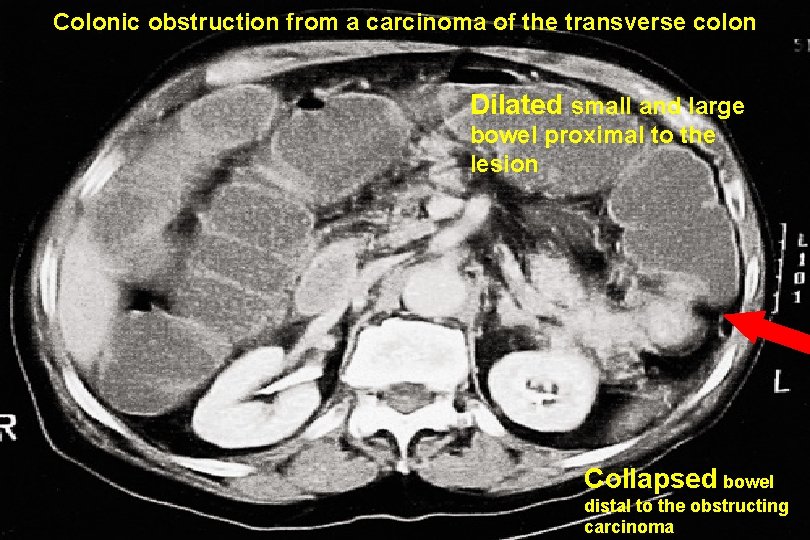
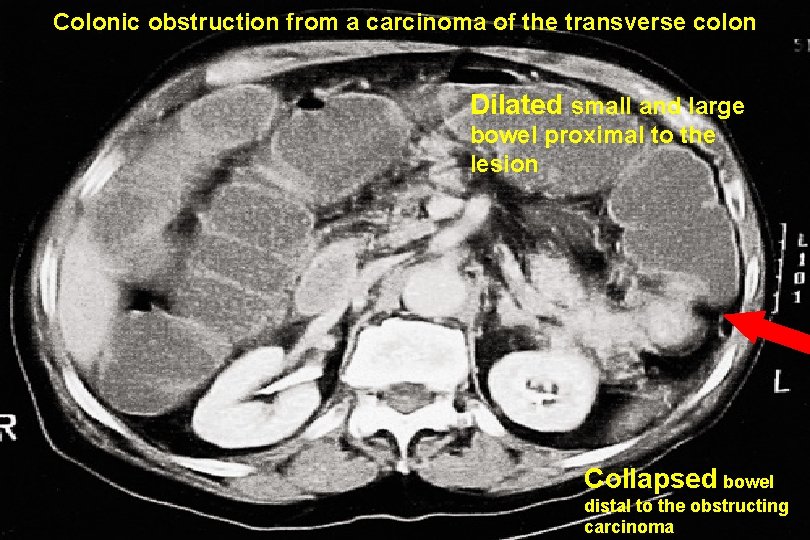
Colonic obstruction from a carcinoma of the transverse colon Dilated small and large bowel proximal to the lesion Collapsed bowel distal to the obstructing carcinoma
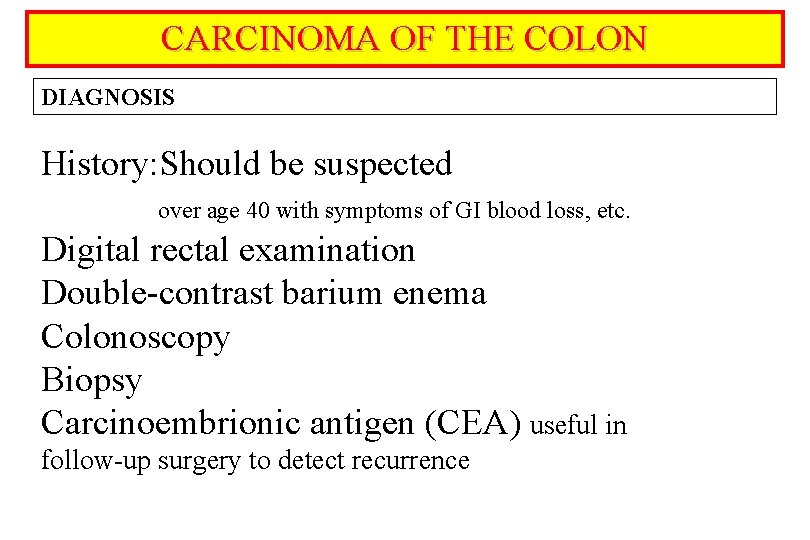
CARCINOMA OF THE COLON DIAGNOSIS History: Should be suspected over age 40 with symptoms of GI blood loss, etc. Digital rectal examination Double-contrast barium enema Colonoscopy Biopsy Carcinoembrionic antigen (CEA) useful in follow-up surgery to detect recurrence
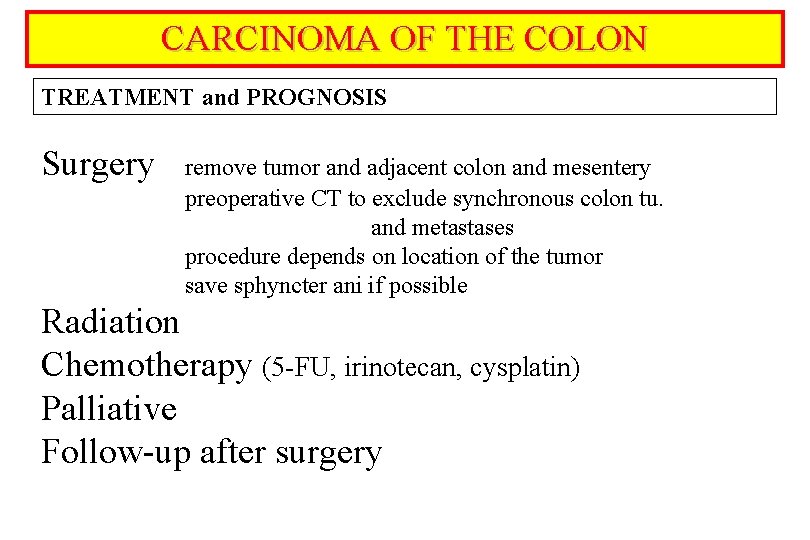
CARCINOMA OF THE COLON TREATMENT and PROGNOSIS Surgery remove tumor and adjacent colon and mesentery preoperative CT to exclude synchronous colon tu. and metastases procedure depends on location of the tumor save sphyncter ani if possible Radiation Chemotherapy (5 -FU, irinotecan, cysplatin) Palliative Follow-up after surgery
CARCINOMA OF THE COLON SCREENING AND PREVENTION Link between adenomatous polyps and cancer ! Testing for occult fecal blood over age 40 -50 y Colonoscopy over age 50 y Colonoscopy in high risk population Diet
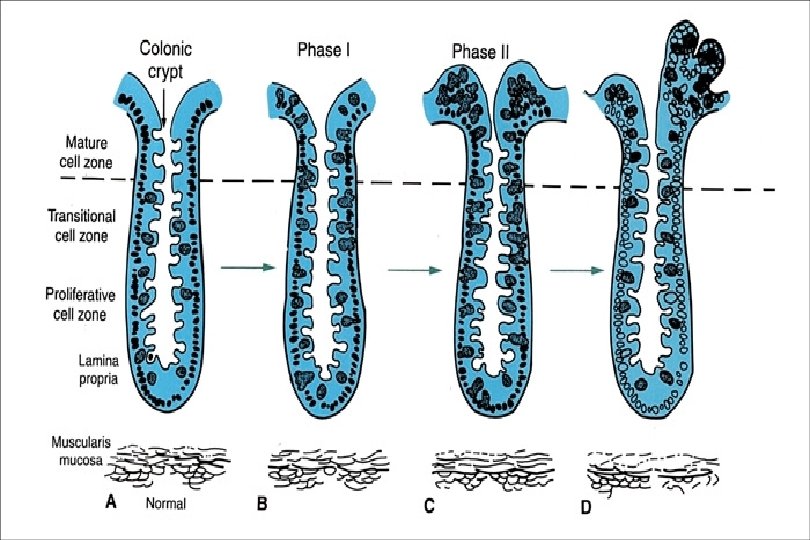
POLYPS OF THE GASTROINTESTINAL TRACT Overgrowth of tissue, usually of epithelial cells, that arises from the mucosal surface and extends into the lumen of the GI tract single or sporadic or pedunculated (stalk) or neoplastic or benign or multiple familial sessile (flat base) non-neoplastic malignant May occure enywhere throughout the GI tract
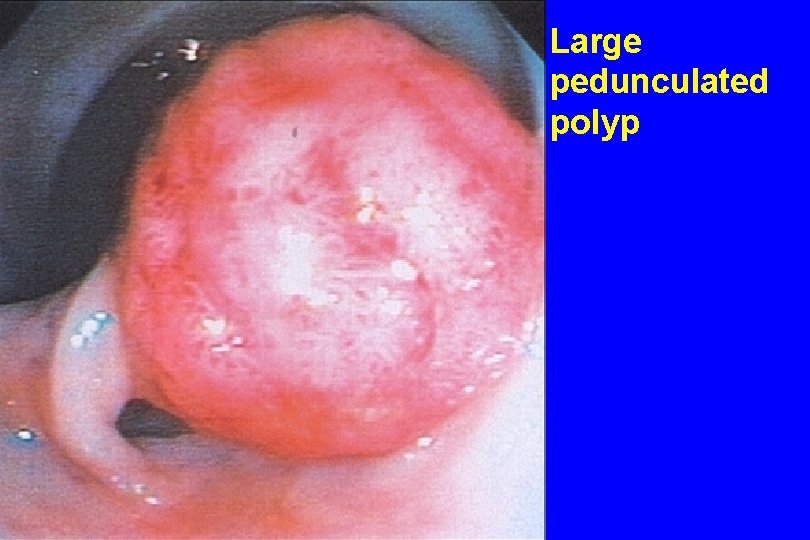
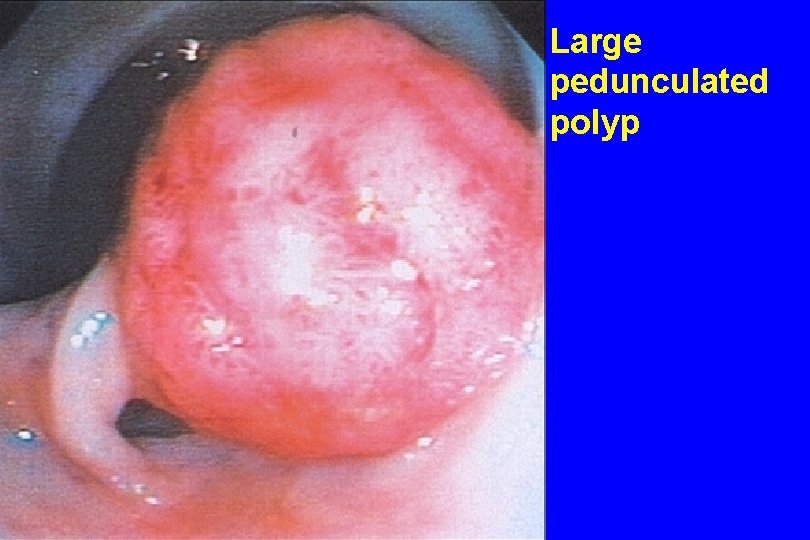
Large pedunculated polyp
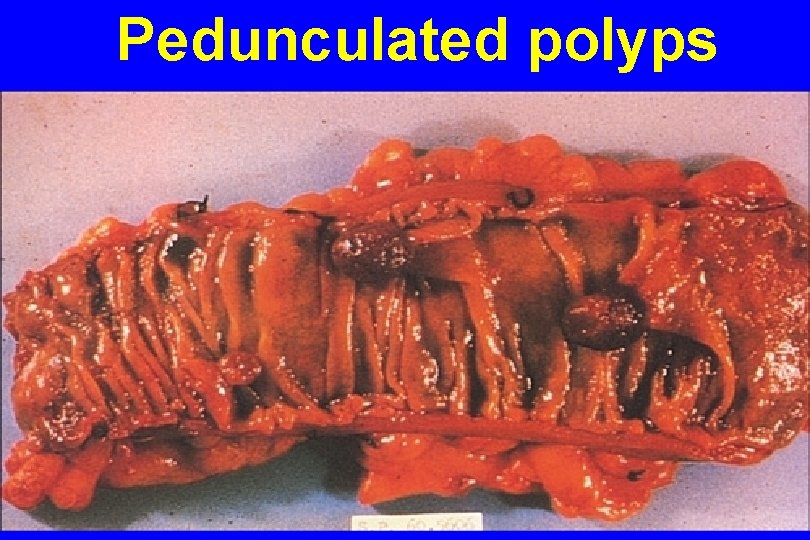
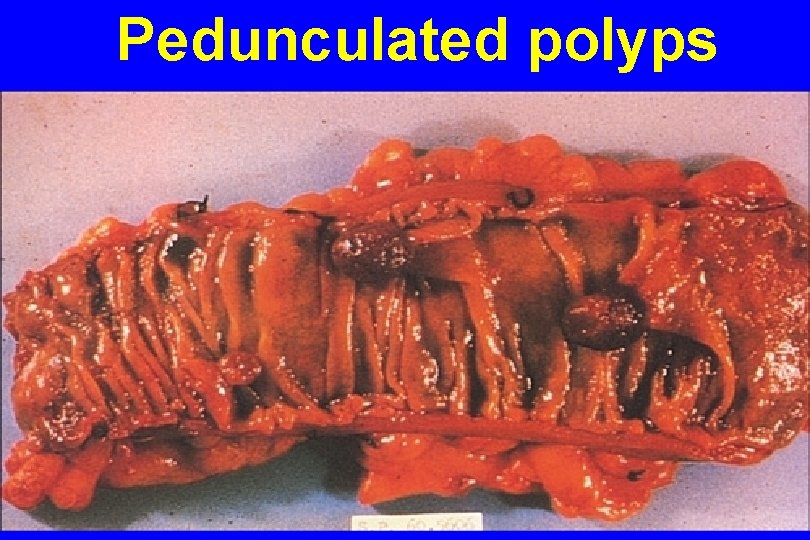
Pedunculated polyps
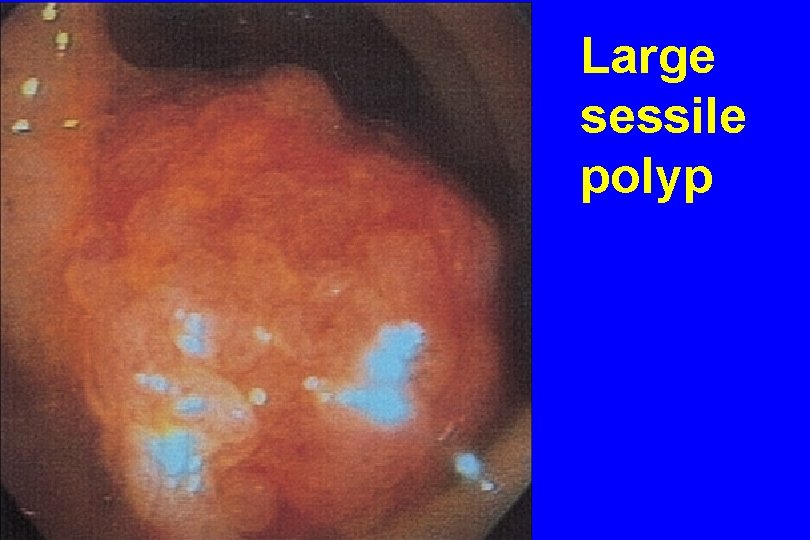
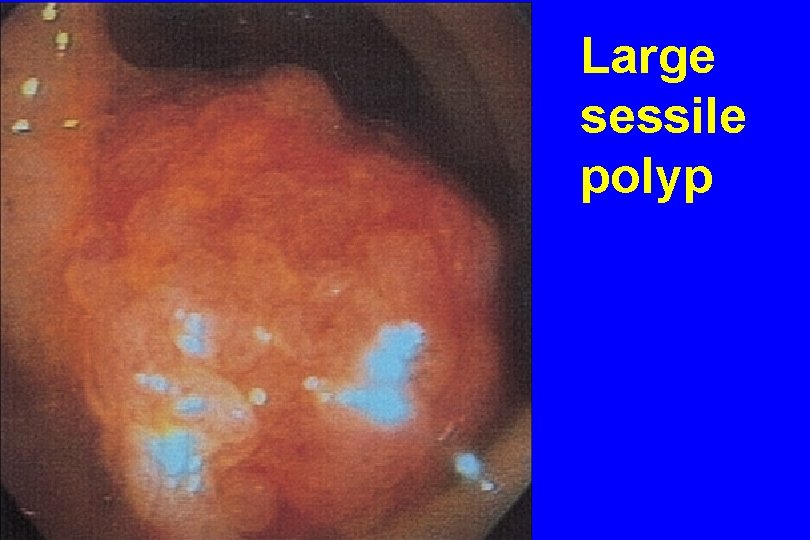
Large sessile polyp
POLYPS OF THE GASTROINTESTINAL TRACT INCIDENCE Adenomatous colonic polyps are very comon Increase with age 50 year-old 20% chance 70 year-old 40% chance Patients with one polyp have higher frequency of synchronous P. greater potential for additional P. over time
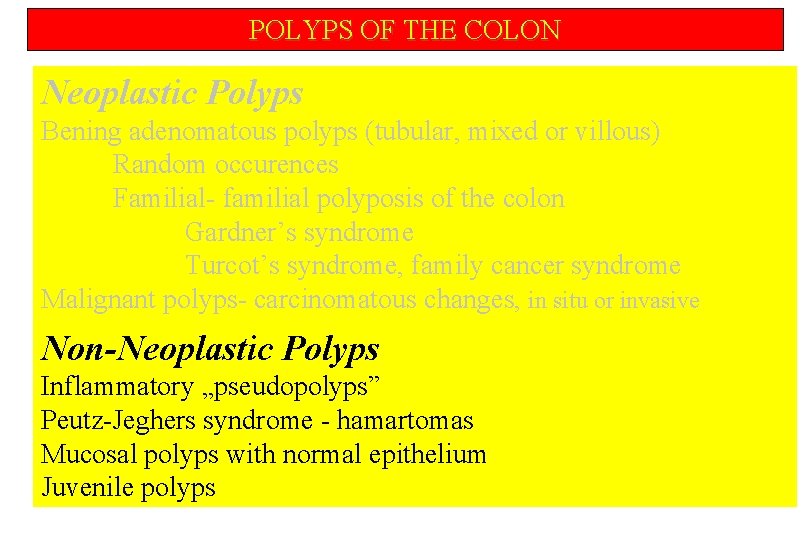
POLYPS OF THE COLON Neoplastic Polyps Bening adenomatous polyps (tubular, mixed or villous) Random occurences Familial- familial polyposis of the colon Gardner’s syndrome Turcot’s syndrome, family cancer syndrome Malignant polyps- carcinomatous changes, in situ or invasive
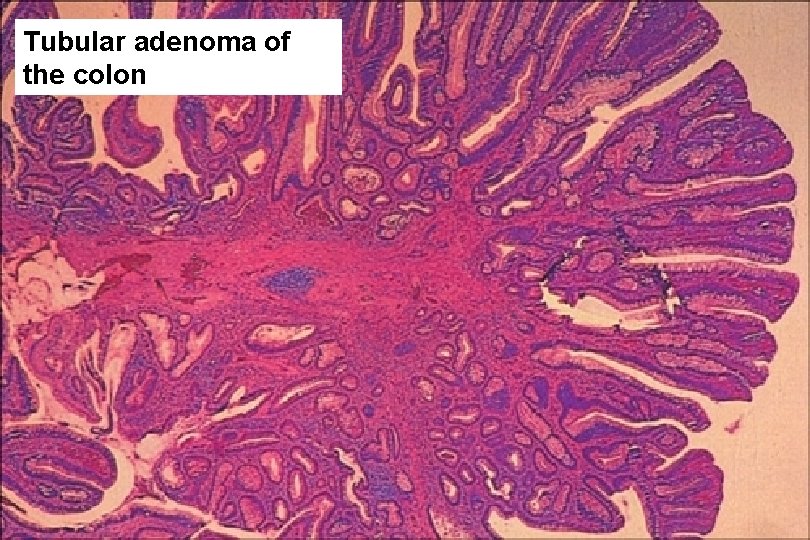
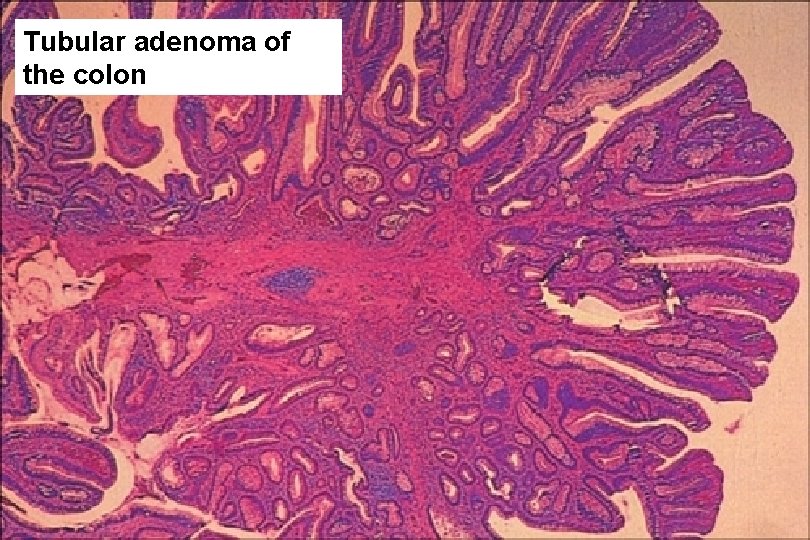
Tubular adenoma of the colon
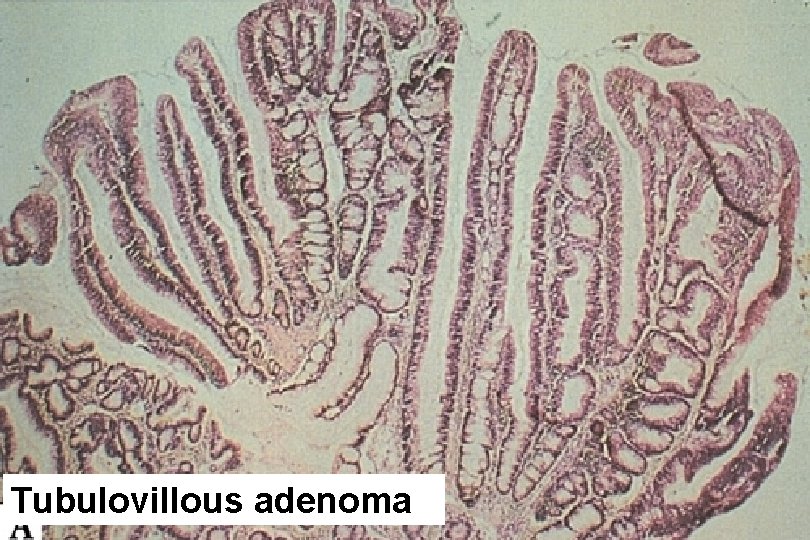
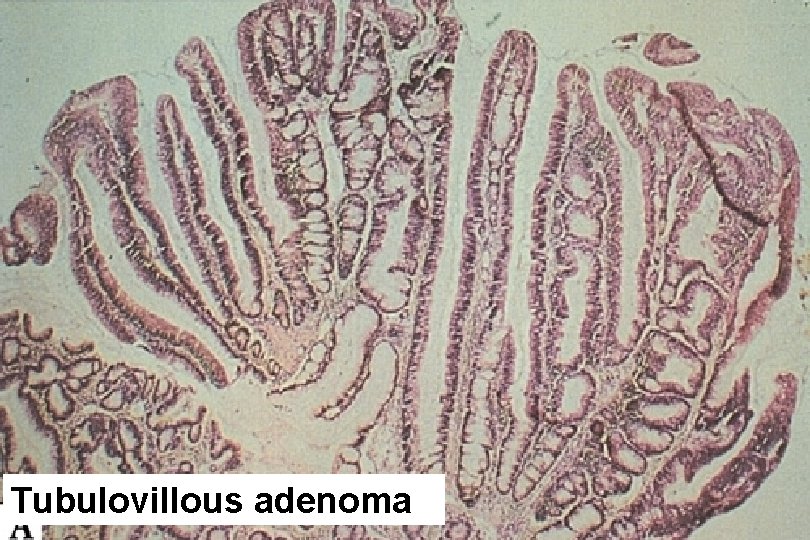
Tubulovillous adenoma

Tubulovillous adenoma

Percent of adenomas containing invasive cancer Adenoma size, cm
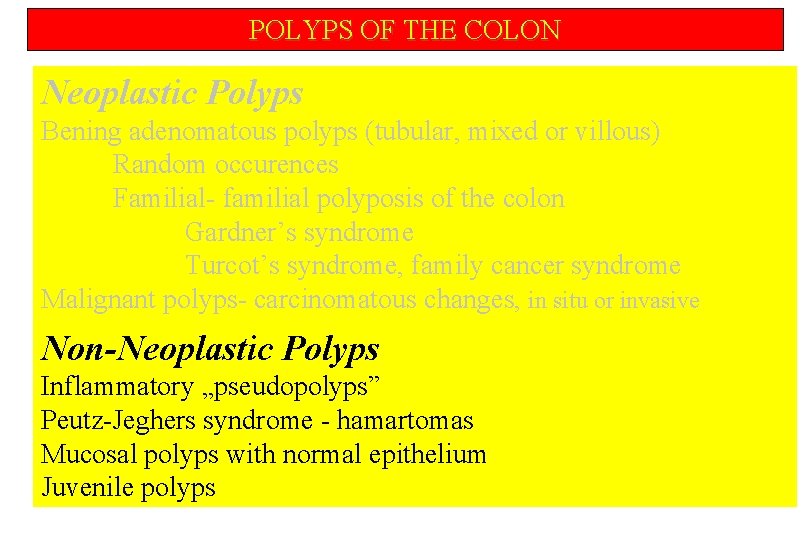
POLYPS OF THE COLON Neoplastic Polyps Bening adenomatous polyps (tubular, mixed or villous) Random occurences Familial- familial polyposis of the colon Gardner’s syndrome Turcot’s syndrome, family cancer syndrome Malignant polyps- carcinomatous changes, in situ or invasive Non-Neoplastic Polyps Inflammatory „pseudopolyps” Peutz-Jeghers syndrome - hamartomas Mucosal polyps with normal epithelium Juvenile polyps
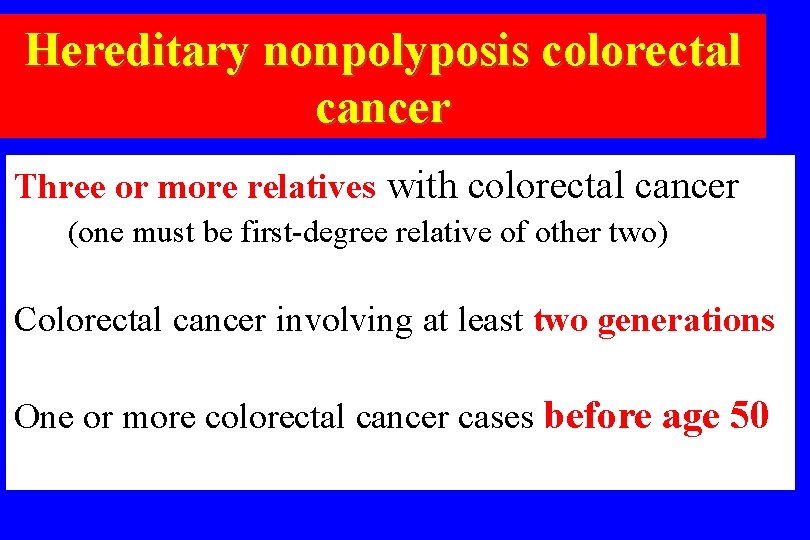
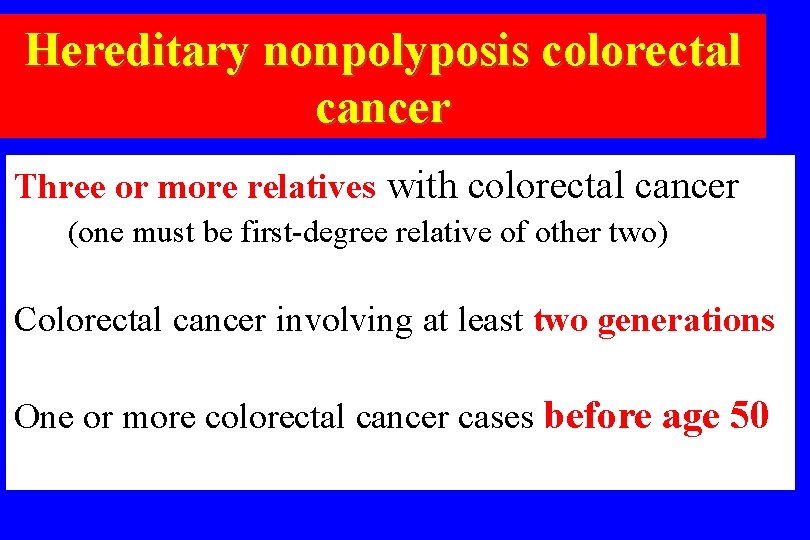
Hereditary nonpolyposis colorectal cancer Three or more relatives with colorectal cancer (one must be first-degree relative of other two) Colorectal cancer involving at least two generations One or more colorectal cancer cases before age 50
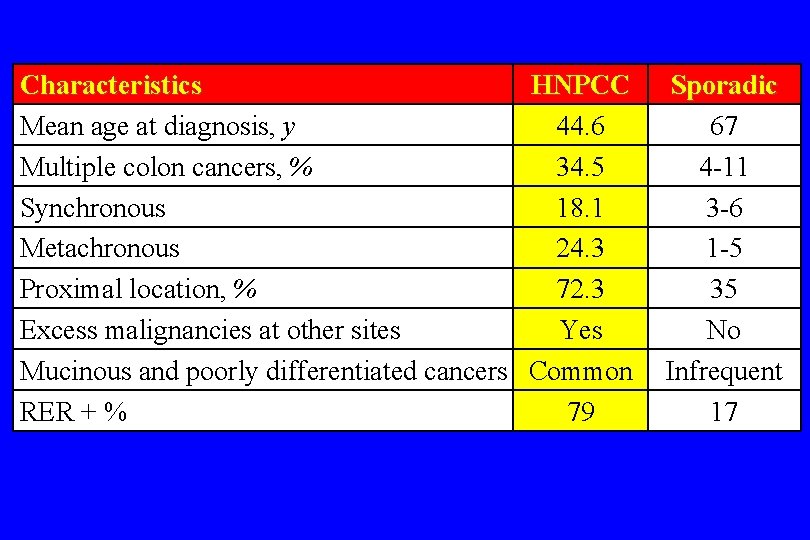
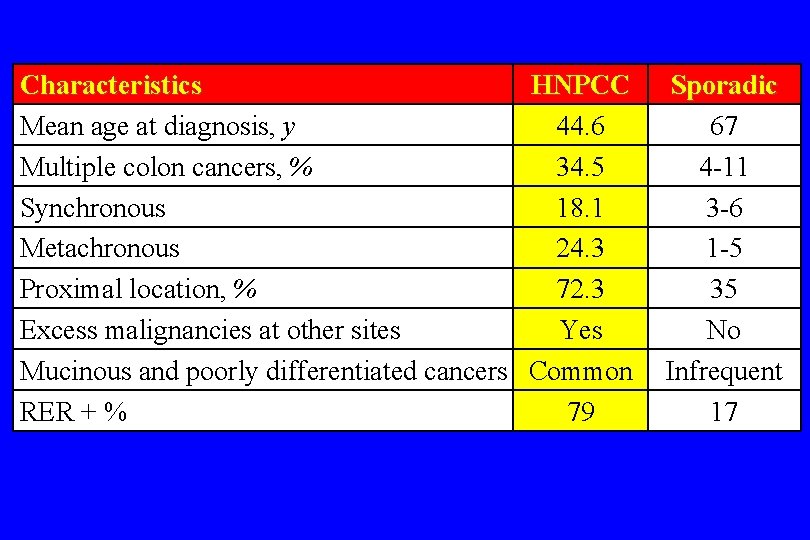
Characteristics HNPCC Mean age at diagnosis, y 44. 6 Multiple colon cancers, % 34. 5 Synchronous 18. 1 Metachronous 24. 3 Proximal location, % 72. 3 Excess malignancies at other sites Yes Mucinous and poorly differentiated cancers Common RER + % 79 Sporadic 67 4 -11 3 -6 1 -5 35 No Infrequent 17
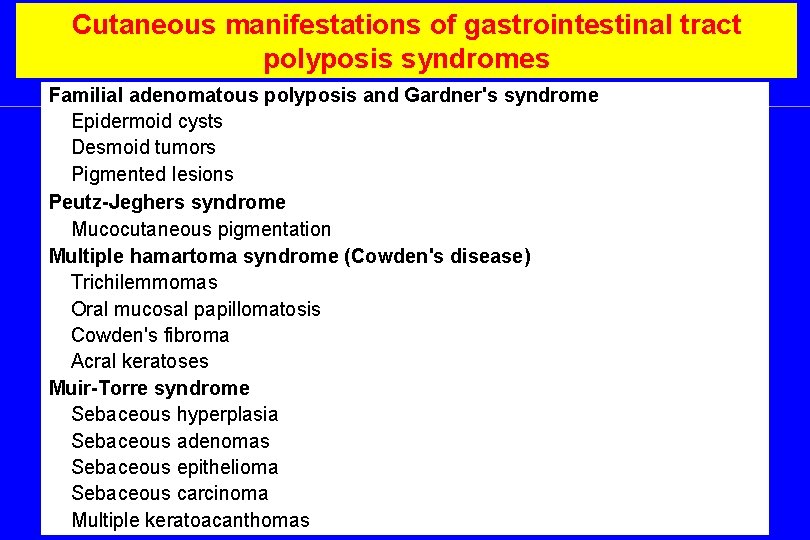
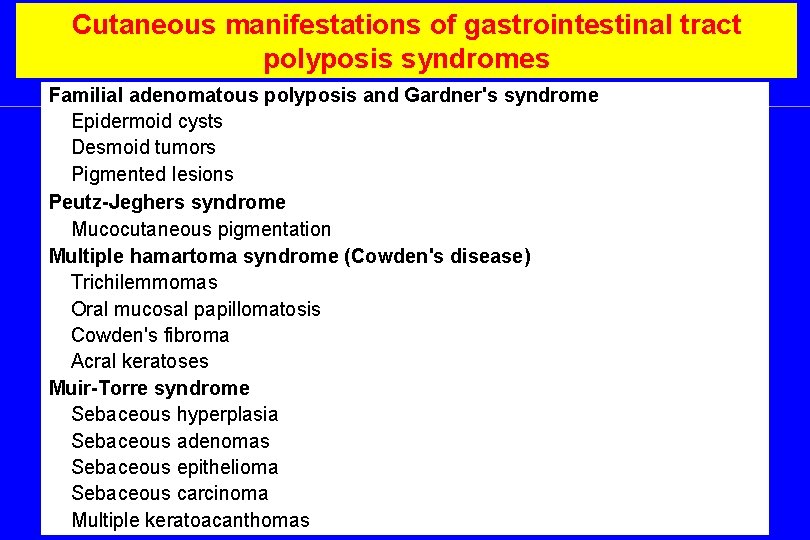
Cutaneous manifestations of gastrointestinal tract polyposis syndromes Familial adenomatous polyposis and Gardner's syndrome Epidermoid cysts Desmoid tumors Pigmented lesions Peutz-Jeghers syndrome Mucocutaneous pigmentation Multiple hamartoma syndrome (Cowden's disease) Trichilemmomas Oral mucosal papillomatosis Cowden's fibroma Acral keratoses Muir-Torre syndrome Sebaceous hyperplasia Sebaceous adenomas Sebaceous epithelioma Sebaceous carcinoma Multiple keratoacanthomas

TUMORS OF THE LIVER Benign Tumor-like Malignant Metastatic

TUMORS OF THE LIVER Benign Hemangioma Hepatocellular adenoma Focal nodular hyperplasia (FNH) Biliary truct adenoma Intrahepatic cytadenoma
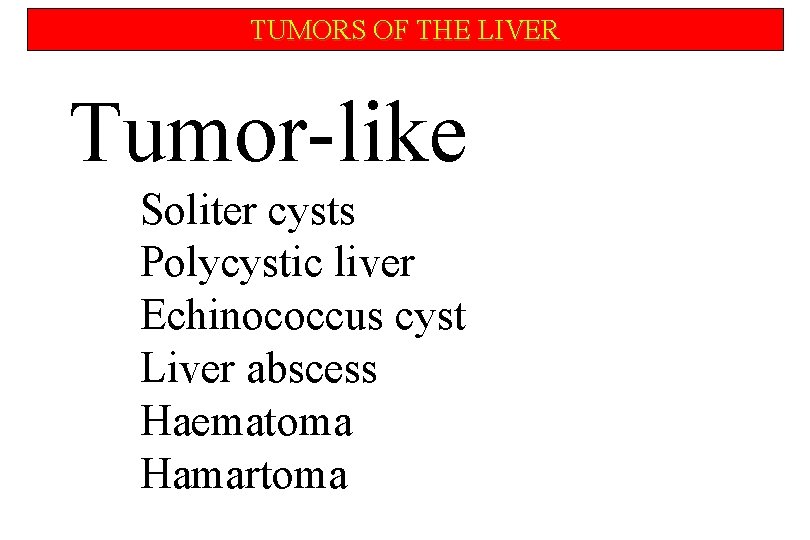
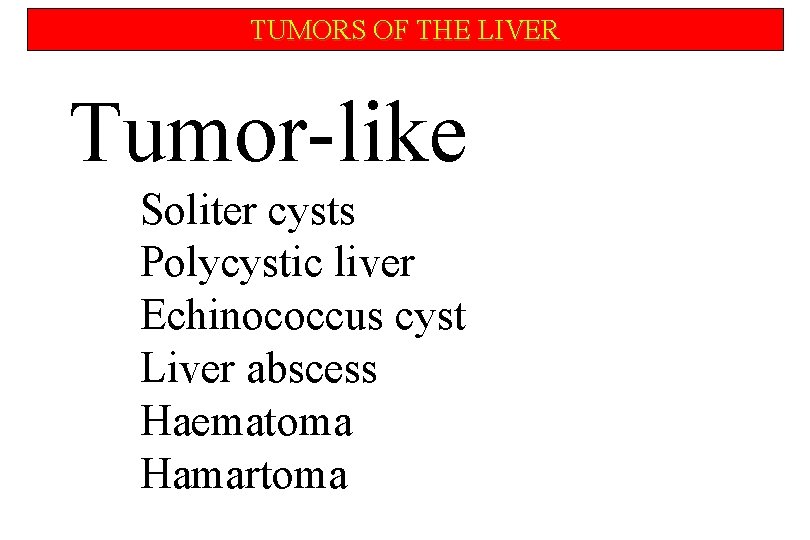
TUMORS OF THE LIVER Tumor-like Soliter cysts Polycystic liver Echinococcus cyst Liver abscess Haematoma Hamartoma
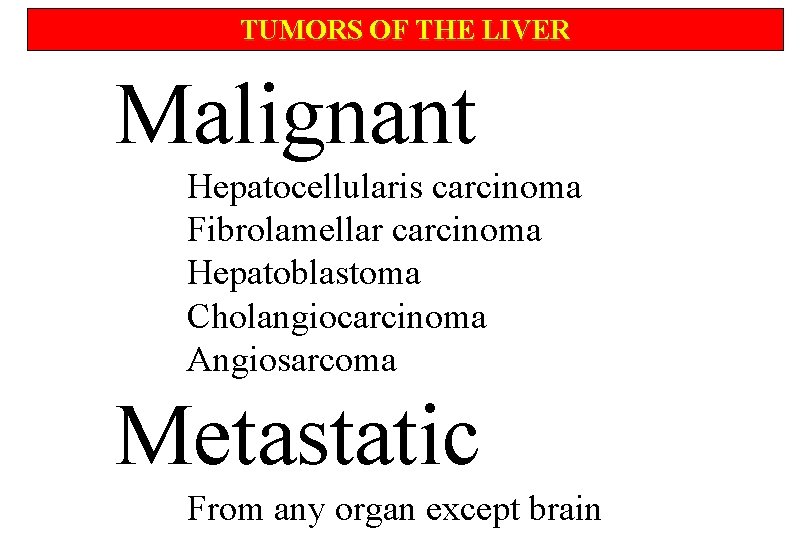
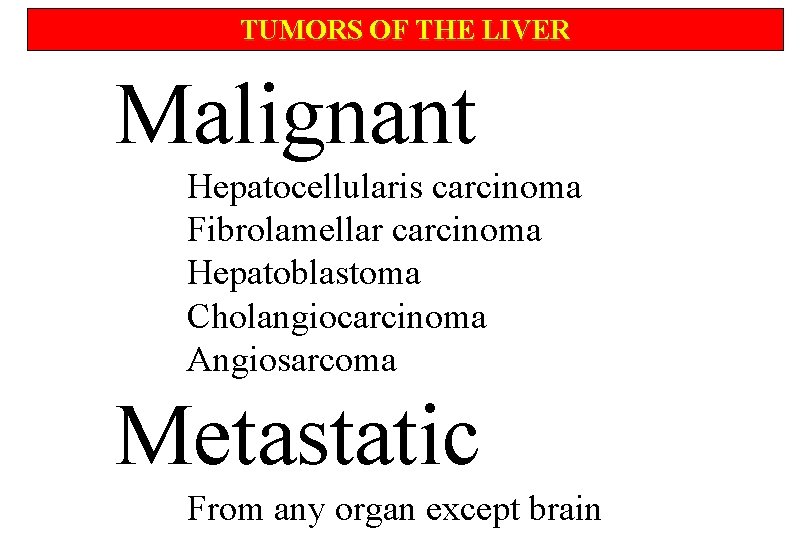
TUMORS OF THE LIVER Malignant Hepatocellularis carcinoma Fibrolamellar carcinoma Hepatoblastoma Cholangiocarcinoma Angiosarcoma Metastatic From any organ except brain
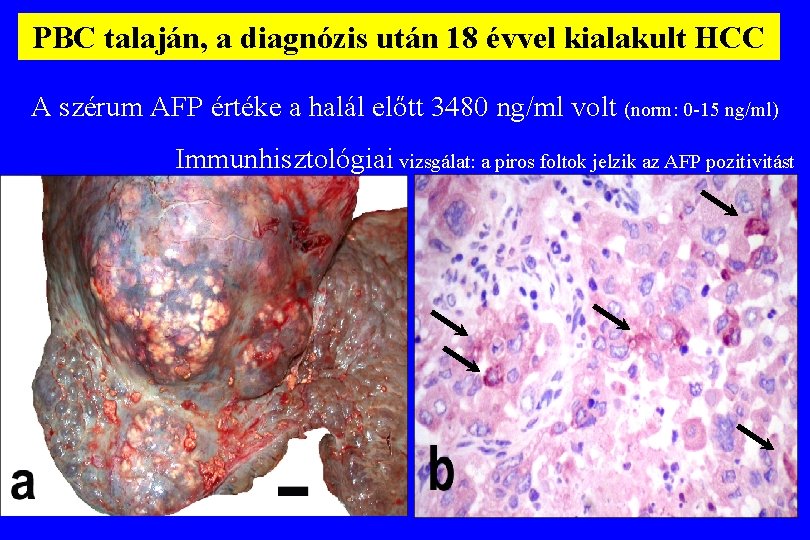
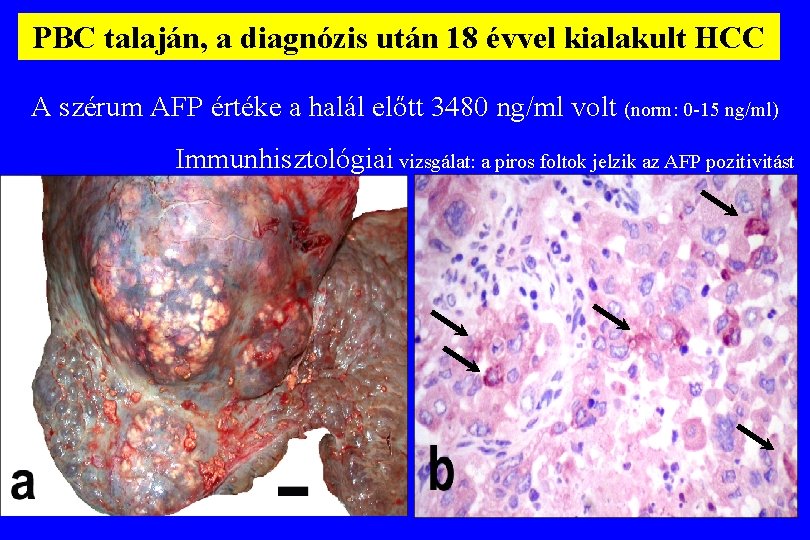
PBC talaján, a diagnózis után 18 évvel kialakult HCC A szérum AFP értéke a halál előtt 3480 ng/ml volt (norm: 0 -15 ng/ml) Immunhisztológiai vizsgálat: a piros foltok jelzik az AFP pozitivitást

Polycystás máj 1 cm
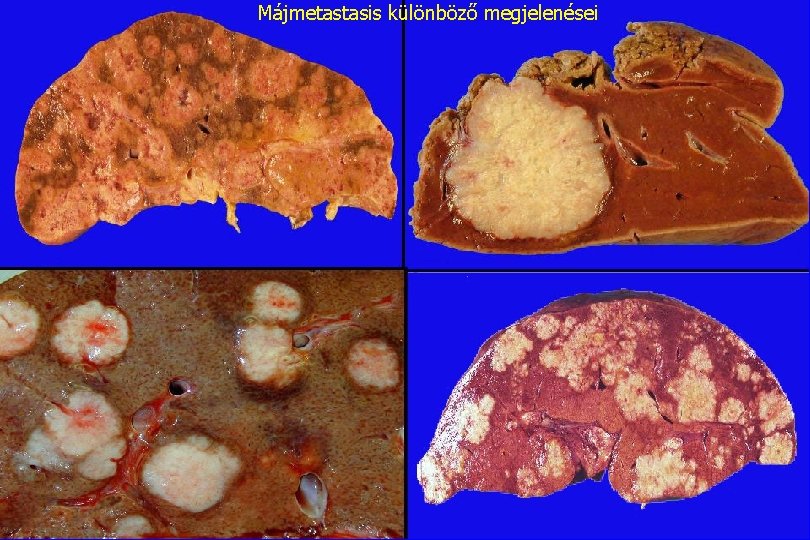
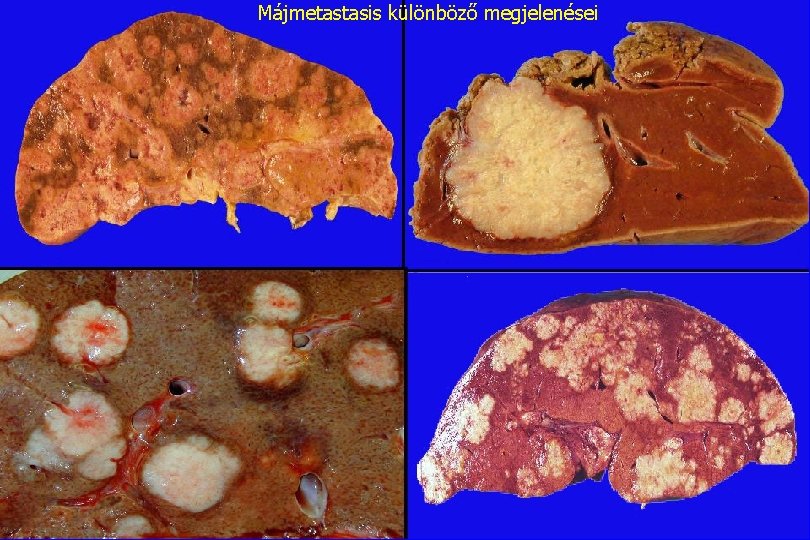
Májmetastasis különböző megjelenései
 Dr kiran bidari
Dr kiran bidari Pyramidal tract vs extrapyramidal tract
Pyramidal tract vs extrapyramidal tract Olivospinal tract vs tectospinal tract
Olivospinal tract vs tectospinal tract Leitold ferenc
Leitold ferenc Dr bauer ferenc
Dr bauer ferenc Adrian ferenc
Adrian ferenc Oktoberi diploma
Oktoberi diploma Ferenc puskás
Ferenc puskás Forgalmi vizsga minosito lappal lehet vezetni
Forgalmi vizsga minosito lappal lehet vezetni Nagyvárad románul
Nagyvárad románul Prandtl szám
Prandtl szám Vissi ferenc
Vissi ferenc Ferenc nádasdy
Ferenc nádasdy Tokaji ferenc gimnázium
Tokaji ferenc gimnázium Szlivka ferenc
Szlivka ferenc Szociometria kérdőív
Szociometria kérdőív Bencs ferenc
Bencs ferenc Kölcsey ferenc vaksága
Kölcsey ferenc vaksága Csik ferenc általános iskola és gimnázium
Csik ferenc általános iskola és gimnázium Ii. rákóczi ferenc leopold györgy rákóczi
Ii. rákóczi ferenc leopold györgy rákóczi Somogyi ferenc felszámoló
Somogyi ferenc felszámoló Mustafa burak doğu
Mustafa burak doğu Oberfrank ferenc
Oberfrank ferenc Szlivka ferenc
Szlivka ferenc Dr kuti ferenc
Dr kuti ferenc Impulzus megmaradásának tétele
Impulzus megmaradásának tétele Otto körfolyamat
Otto körfolyamat Janka ferenc
Janka ferenc Humana ferenc krt
Humana ferenc krt Kölcsey ferenc
Kölcsey ferenc Chłopcy z placu broni dlaczego warto przeczytać
Chłopcy z placu broni dlaczego warto przeczytać Mi a klasszicizmus
Mi a klasszicizmus Szlivka ferenc
Szlivka ferenc Ferenczy istván kölcsey ferenc szobra
Ferenczy istván kölcsey ferenc szobra Szlivka ferenc
Szlivka ferenc Ferenc józsef
Ferenc józsef Giczi ferenc
Giczi ferenc Himnusz fokozás
Himnusz fokozás Rafael pavlus ferenc
Rafael pavlus ferenc Szlivka ferenc
Szlivka ferenc Lődíj
Lődíj Habsburg–lotaringiai ferenc károly főherceg
Habsburg–lotaringiai ferenc károly főherceg Szlivka ferenc
Szlivka ferenc Dr suba ferenc
Dr suba ferenc Vasúti vizsgabiztosi névjegyzék
Vasúti vizsgabiztosi névjegyzék Szlivka ferenc
Szlivka ferenc Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Tư thế ngồi viết
Tư thế ngồi viết Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ