NEOPLASIAS CANCERS Most common cancers Solid tumors of
- Slides: 68
NEOPLASIAS
CANCERS Most common cancers Solid tumors of the breast, lung, prostate, colon, and rectum Low growth fraction and respond poorly to drugs Rarer cancers Lymphocytic leukemia, Hodgkin’s disease, certain testicular cancers High growth fraction and respond well to drugs
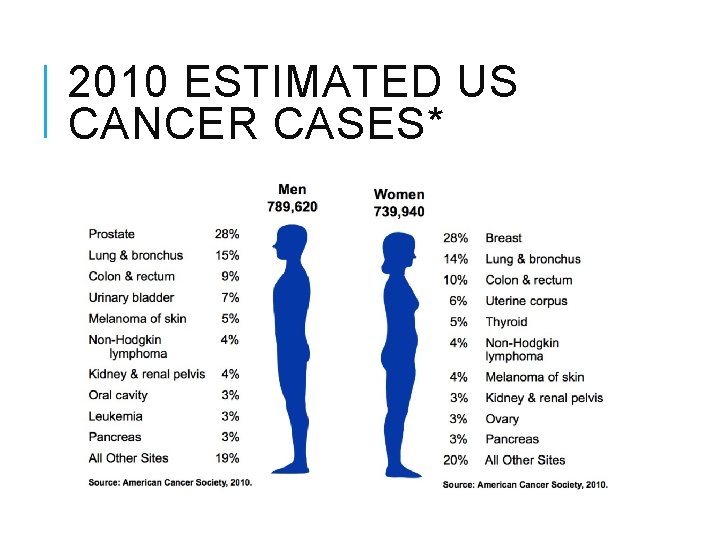
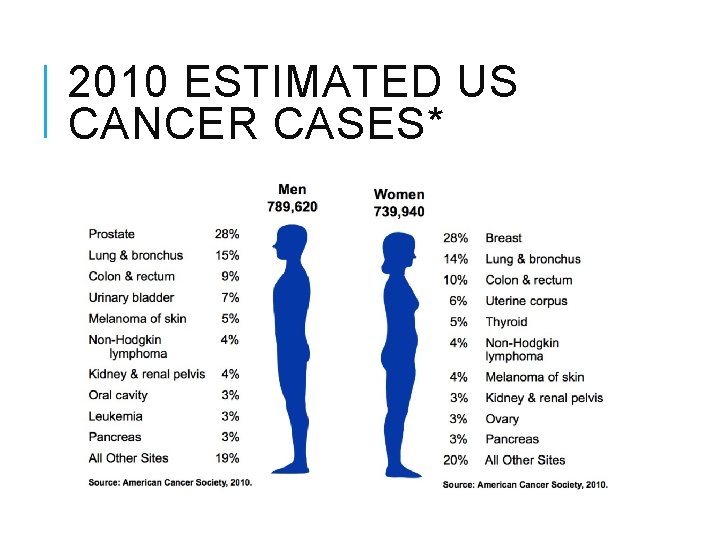
2010 ESTIMATED US CANCER CASES*
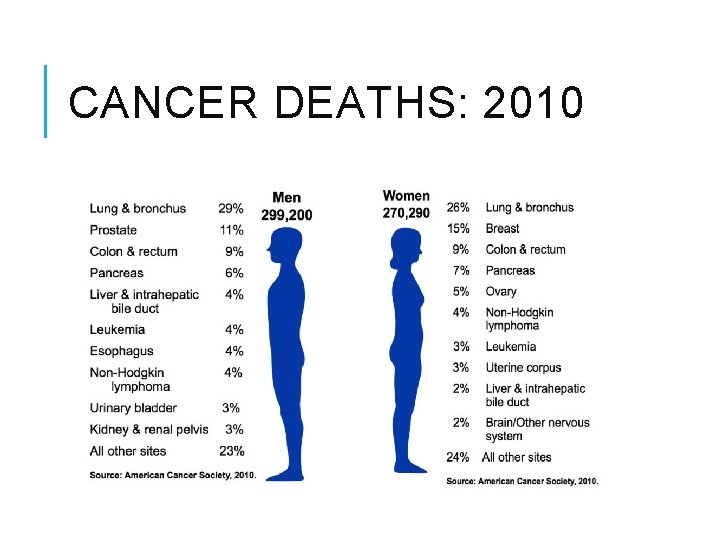
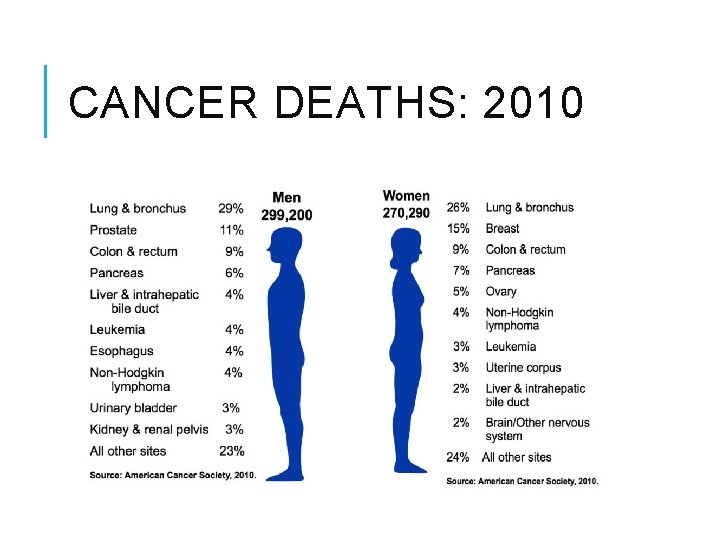
CANCER DEATHS: 2010
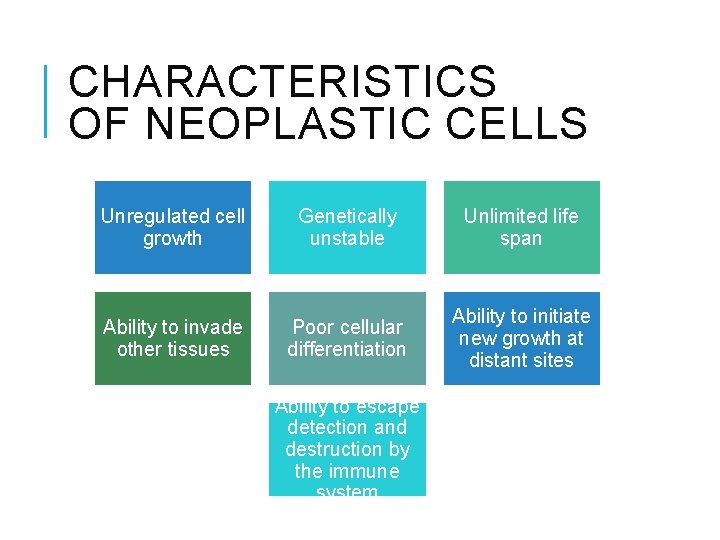
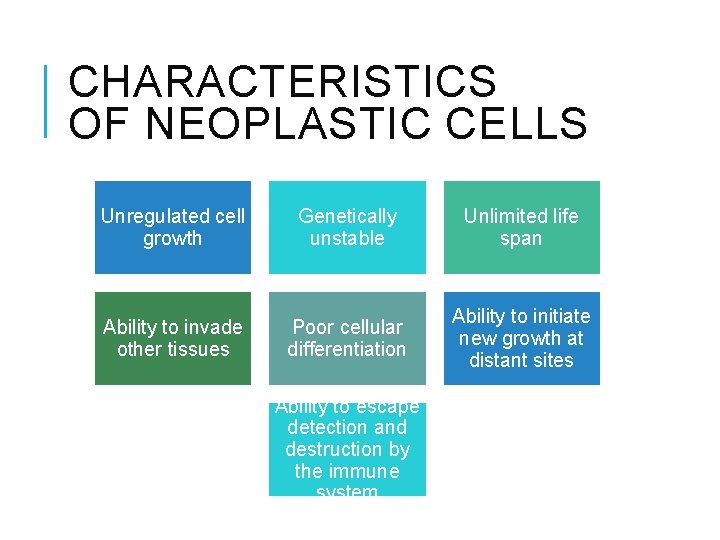
CHARACTERISTICS OF NEOPLASTIC CELLS Unregulated cell growth Genetically unstable Unlimited life span Ability to invade other tissues Poor cellular differentiation Ability to initiate new growth at distant sites Ability to escape detection and destruction by the immune system
CANCER BIOLOGY http: //youtu. be/46 Xh 7 OFkk. CE
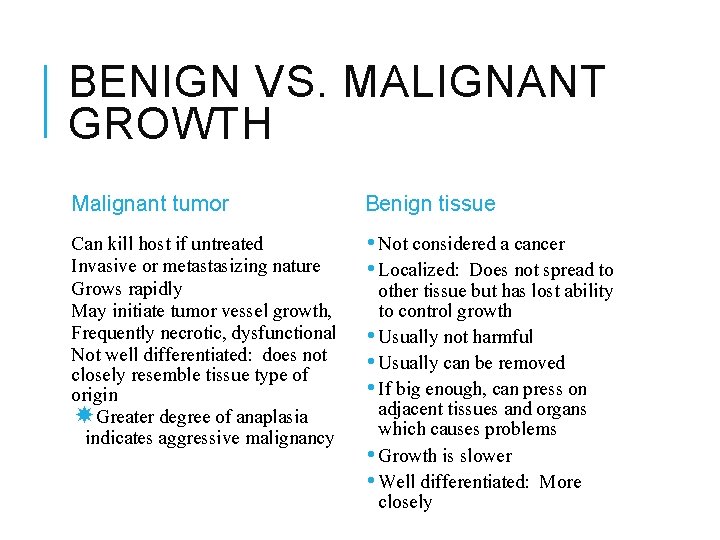
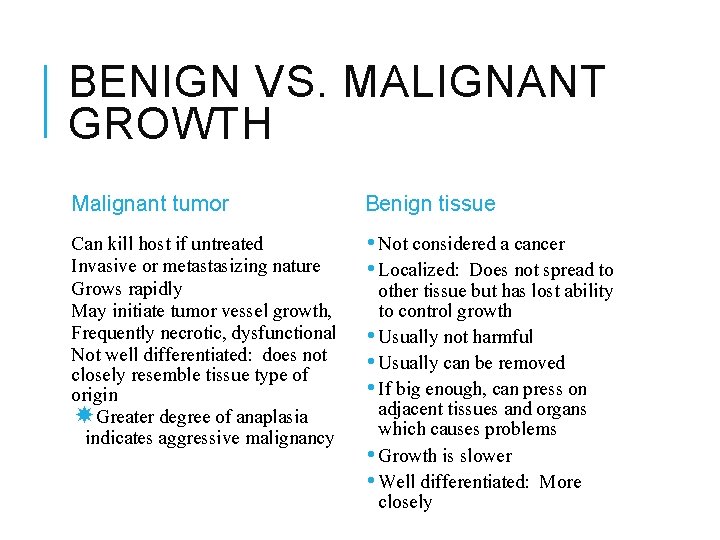
BENIGN VS. MALIGNANT GROWTH Malignant tumor Benign tissue Can kill host if untreated Invasive or metastasizing nature Grows rapidly May initiate tumor vessel growth, Frequently necrotic, dysfunctional Not well differentiated: does not closely resemble tissue type of origin Greater degree of anaplasia indicates aggressive malignancy • Not considered a cancer • Localized: Does not spread to other tissue but has lost ability to control growth • Usually not harmful • Usually can be removed • If big enough, can press on adjacent tissues and organs which causes problems • Growth is slower • Well differentiated: More closely resembles normal tissue
CANCER TERMINOLOGY “-oma” suffix usually indicates benign tumor (adenoma) Exceptions: “lymphoma”, “myeloma”, “melanoma” “-carcinoma, ” and “-sarcoma” indicates malignant tumors “carcinoma” Epithelial origin Example: “adenocarcinoma” (malignant tumor of epithelial origin), basal cell carcinoma “sarcoma” malignant tumor of mesenchymal origin Example: rhabdomyosarcoma, liposarcoma, fibrosarcoma “leukemia” malignant growth of white blood cells
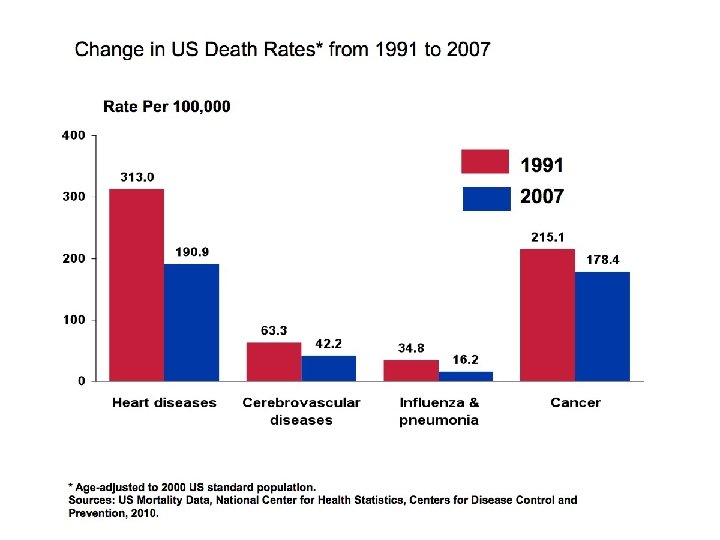
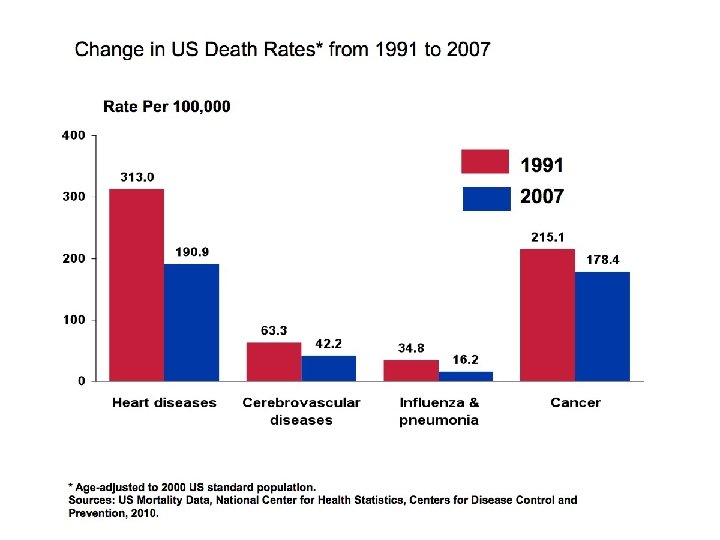
EPIDEMIOLOGY AND CANCER RISK FACTORS Biggest risk factor: age 1/3 of cancer-related deaths may be r/t lifestyle factors Tobacco use Nutrition Obesity Sun exposure (skin cancer) Sexual exposure to HPV (cervical cancer) IMPORTANT: Screening allows for earlier detection Early detection means earlier treatment More positive responses with earlier Tx
TOBACCO USE Death rate from lung cancer has dramatically increased Lung cancer: leading cause of death in men and women worst survival rate Tobacco also linked to: pancreatic kidney bladder mouth throat stomach esophageal cervical cancers
NUTRITIONAL FACTORS Dietary factors believed to be related to cancer risk: ↑Fat: ↑ breast, colon and prostrate ↓Fiber: ↑ colorectal cancer ↑ Alcohol H & N cancers, liver cancer, stomach
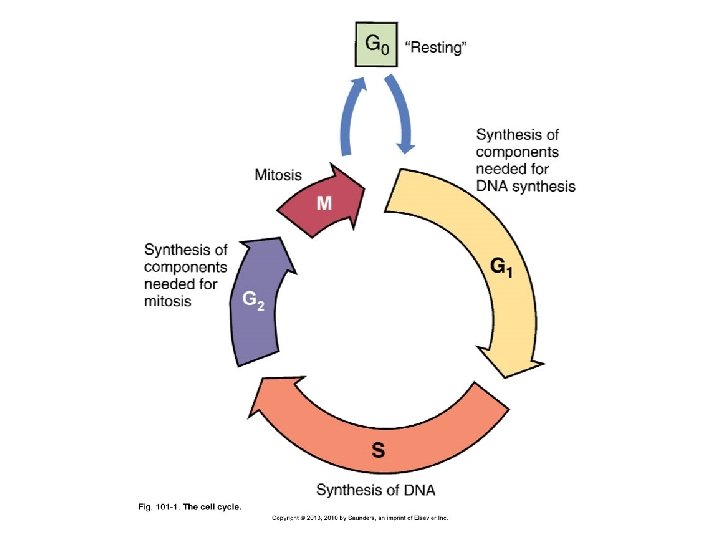
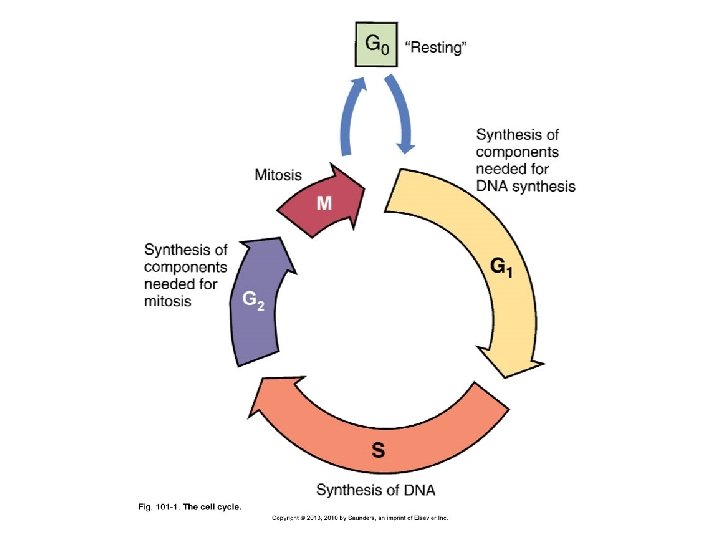
THE GROWTH FRACTION AND ITS RELATIONSHIP TO CHEMOTHERAPY The cell cycle Four major phases The growth fraction Impact of tissue growth fraction on responsiveness to chemotherapy
GENETIC MECHANISMS OF CANCER Carcinogen Potential cancer-causing agent Proto-oncogene Enhances growth producing pathways Oncogene Proto-oncogene in its overactive form Tumor suppressor gene Inhibits cell proliferation Cancers may arise when tumor suppressor gene function is lost or abnormally inhibited
FROM PROTOONCOGENE TO ONCOGENE Proto-oncogenes become activated oncogenes when mutations alter their activity so that proliferation-promoting signals are generated inappropriately Oncogene introduced to host cell by retrovirus Proto-oncogene within cell suffers a mutagenic event DNA sequence may be lost/damaged Error in chromosome replication causes extra copies of proto -oncogene
RETROVIRUS EXAMPLES HIV Kaposi’s sarcoma Epstein-Barr virus Burkitt lymphoma Human T-lymphocyte virus type 1 Adult T-cell leukemia/lymphoma Retroviruses are composed of RNA and contain reverse transcriptase enzyme
TUMOR-SUPPRESSOR GENES Contribute to cancer only when NOT present Both copies of tumor suppressor genes are activated when cancer develops One can inherit a defective copy of tumor suppressor gene At much higher risk for cancer development Mutations cause the gene to not function Epigenetic processes silence the gene
RB GENE Normally “master brake” for the cell cycle Blocks/stops cell division by binding transcription factors An inactivating mutation of the Rb gene removes restraint on cell division Defective Rb genes are common in some cancers
P 53 GENE Most common tumor-suppressor gene defect identified in cancer cells Normally p 53 inhibits cell cycling Mutated or damaged p 53 allows genetically damaged/unstable cells to survive and continue to replicate Cancer cells that lack functional p 53 may be resistant to chemotherapy/radiation
BRCA 1 AND BRCA 2 GENES Tumor suppressor genes Associated with breast cancer Family history and inherited defect in BRCA 1 increases risk of breast cancer
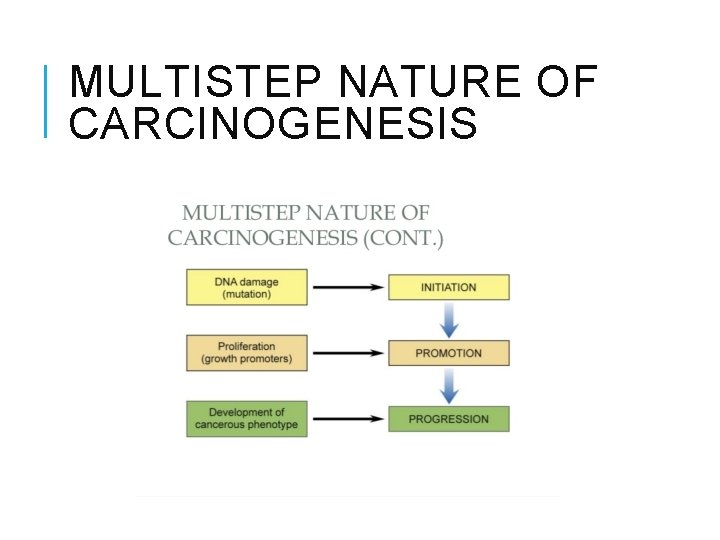
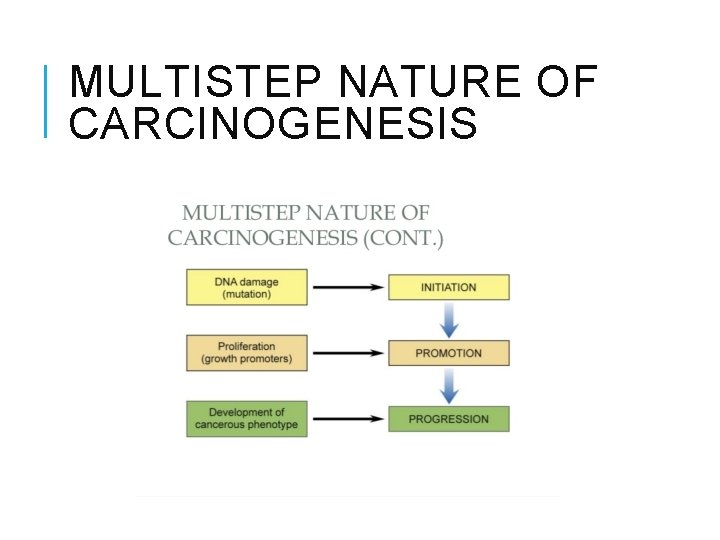
MULTISTEP NATURE OF CARCINOGENESIS
INITATION Initiating events Genetic mutations Proliferation Required for cancer development Each type of cancer has its own combination of mutations that lead to malignancy Carcinogens can be complete or partial
PROMOTION Stage during which mutant cell proliferates Activation of another oncogene Inactivation of tumor suppressor gene Nutritional factors Infection Hormones may be promoters for certain cancers Cancer cells produce telomerase Allows immortality in cancer cells
PROGRESSION Mutant, proliferating cells begin to exhibit malignant behavior Cells whose phenotype gives them a growth advantage proliferate more readily Evolved tumor cells differ significantly from the normal tissue Progress to malignant characteristics
METASTASIS Process of invading other tissues at other sites Requires: Invasion of adjacent tissues Through basement membranes Entrance into nearby vessels (blood or lymph) Invasion of the immune system Reentrance into distant tissue Brain, liver, lung Implantation of malignant cells in new tissue
PATTERNS OF SPREAD Cancer cells generally spread via circulatory or lymphatic systems Tumor markers help identify parent tissue of cancer origin Rely on some retention of parent tumor characteristics Some released into circulation Others identified through biopsy Enzymes/proteins typically used as tumor markers Help track tumor activity
ANGIOGENESIS Process by which cancer tumor forms new blood vessels in order to grow Usually doesn’t develop until later stages Triggers are not well understood Inhibition of angiogenesis is an important therapeutic goal
CANCER DIAGNOSIS Screening ID asymptomatic persons with risk factors Detect occult disease and start treatment Direct clients to genetic counseling when cancer is in family Assessment Physical, health history, diagnostic labs, tumor markers, imaging studies (CT, PET scans, X-rays) Biopsy and cytology of cancer cells Bone marrow aspiration
GRADING AND STAGING OF TUMORS Reasons to grade and stage tumors Determine treatment Estimate prognosis ID appropriate clinical trials Elements of staging Site of tumor Tumor size and number Lymph node involvement Cell type and tumor grade (how closely ca cells resemble normal tissue cells) Presence or absence of metastasis
TNM STAGING SYSTEM: MOST COMMON T = characteristic of the tumor: size, depth of invasion, involvement of surrounding structures N = extent of spread to the lymph nodes M = presence of distant metastasis *a number is added to each letter to indicate the size or extent of the primary tumor and extent of cancer spread
STAGING EXAMPLE Stage I, III or IV Example: Stage I: T 1, N 0, M 0 ( 1 cm, 0 nodes involved, no distant metastasis) Stage II: T 2, N 1, M 0 (2 cm, 1 node, no metastasis) Stage III: Cancer any size and has spread to lymph nodes OR Any size and has spread to breast bone or sticking to other structures Stage IV: metastasis (cancer has spread to other parts of the body)
CAUTION: WARNING SIGNS OF CANCER Change in bowel or bladder habits A sore that does not heal Unusual bleeding or discharge Thickening or lump in breast or elsewhere Indigestion or difficulty swallowing Obvious change in wart or mole Nagging cough or hoarseness
CH↑LDREN: WARNING SIGNS OF CANCER IN CHILDREN Continued, unexplained wt loss Headaches with vomiting in the morning swelling or persistent pain in bones or joints Lump or mass in abdomen, neck, or elsewhere Development of whitish appearance in pupil of the eye Recurrent fevers not caused by infections Excessive bleeding or bruising Noticeable paleness or prolonged tiredness
EFFECTS OF CANCER ON THE BODY: FATIGUE The most commonly reported symptom Factors influencing fatigue Sleep changes and disturbances Decreased activity level Poor nutrition Psychosocial factors such as depression Treatment regimen Biochemical changes Fatigue is generally poorly understood manifestation of cancer
PAIN Pain occurs due to several factors: Pressure or obstruction from tumor Stretching of sensitive structures Tissue destruction Compression of nerve endings Inflammation Infection and necrosis
ANOREXIA, NAUSEA, VOMITING Due to complication of radiation and chemotherapy treatments Kills rapidly proliferating cells of cancer but also affects normal cells lining GI tract Treatment also affects the vomiting center in the hypothalamus
CACHEXIA Malnutrition in cancer Includes: Anorexia - due to pain, treatments or depression Early satiety – due to tumor metabolites or host cell cytokine production Weakness Taste changes Altered protein, lipid and carbohydrate metabolism Nausea and vomiting from treatments Can result in anemia and weight loss One of the most common causes of death in person with cancer
ANEMIA Causes of anemia in cancer include: Chronic bleeding Malnutrition Medical therapies Cancer in blood forming organs Defect in erythropoetin production Shortened life span of RBC Treatment: Administration of erythropoietin Blood transfusions
LEUKOPENIA Deficiency in circulating white blood cells Primary cause Malignant invasion of bone marrow Contributing factors Malnutrition Chemotherapy Opportunistic organisms can infect an immunocompromised host
THROMBOCYTOPENIA Often due to direct invasion of the bone marrow Chemotherapy can be toxic to marrow ↑ risk of bleeding (↓ platelets)
INFECTION One of the most significant complications Factors that increase infections: ↓ in leukocytes Immunosuppresion due to treatment Surgery can also decrease resistance to infection Nosocomial infections
HAIR LOSS AND MUCOSITIS Due to complication of radiation and chemotherapy treatments Kills rapidly proliferating cells of cancer Affects normal cells of epithelia, mucus membranes and hair follicles
PARANEOPLASTIC SYNDROMES 1. 2. 3. Hypercalcemia Increased parathyroid hormone secretion-related protein Cushing syndrome ACTH excess Hyponatremia and water overload SIADH – inappropriate antidiuretic hormone secretion
ONCOLOGICAL EMERGENCIES Cardiac tamponade SIADH Fluid accumulates in pericardial sac ADH released from tumors DIC Hypercalcemia intracranial pressure Malignant pleural effusion Sepsis and septic shock Spinal cord compression Tumor lysis syndrome Hyperkalemia Hyperphosphatemia Hyperuricemia hypocalcemia SVC syndrome
CANCER THERAPY Early detection provides the best prognosis for cure Mainstays of therapy: Surgery Radiation therapy Drug therapy/chemotherapy Emerging therapies: Immunotherapy Targeted molecular therapies Stem cell transplantation
SURGERY Majority of patients with solid tumors are treated surgically Main benefit: removal of tumor with minimal damage to other body cells Commonly accompanied by radiation therapy or chemotherapy
RADIATION THERAPY Kills tumor cells by damaging nuclear DNA Kills cells that are non-resectable due to location, missed by surgery, or undetected May not kill cells directly, but initiates apoptosis Small doses of radiation given over several treatments Some normal cells are also killed during radiation therapy
BASIC PRINCIPLES OF CANCER CHEMOTHERAPY Systemic administration of anticancer chemicals to treat cancers known or suspected to be disseminated in the body Treatment of choice for disseminated cancers (leukemia, disseminated lymphomas, widespread metastases) Most are cytotoxic Not selective for tumor cells (normal cell death may also occur)
BASIC PRINCIPLES OF CHEMOTHERAPY Most effective on rapidly dividing cells Several courses ensure all cancer cells are killed Serious side effect: bone marrow suppression Promising approach is to inhibit angiogenesis by the tumor with anti-angiogenic drugs
BASIC PRINCIPLES OF CHEMOTHERAPY Drug classes Cytotoxic agents Hormones and hormone antagonists Biologic response modifiers Targeted drugs
CYTOTOXIC ANTICANCER DRUGS Largest class of anticancer drugs Acts directly on cancer cells and healthy cells to cause their death About 50% of cytotoxic anticancer drugs are phase-specific Toxic only to cells in a particular phase Must be in the blood continuously over a long time Cell-phase non-specific drugs can act during any phase of the cell cycle
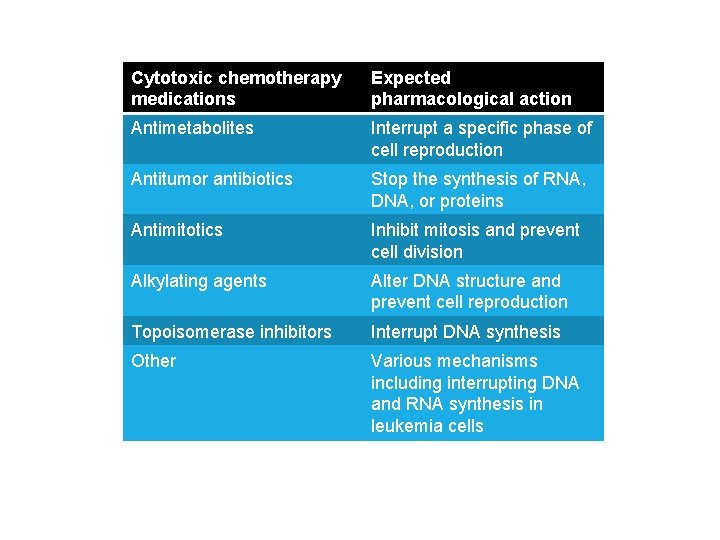
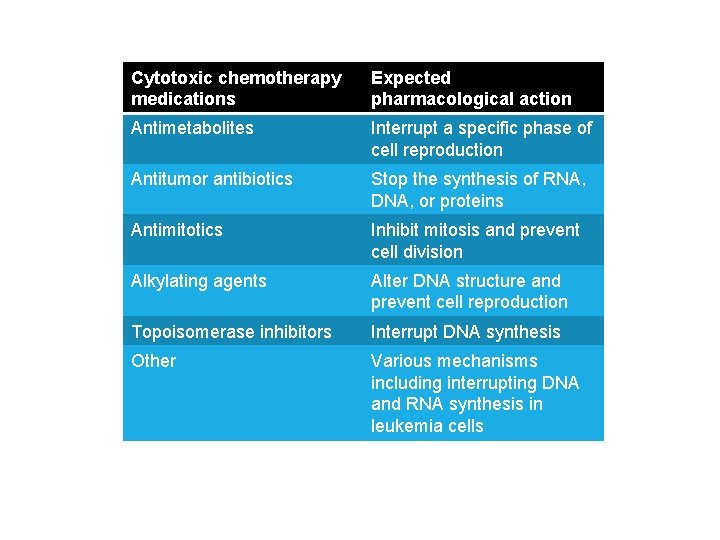
Cytotoxic chemotherapy medications Expected pharmacological action Antimetabolites Interrupt a specific phase of cell reproduction Antitumor antibiotics Stop the synthesis of RNA, DNA, or proteins Antimitotics Inhibit mitosis and prevent cell division Alkylating agents Alter DNA structure and prevent cell reproduction Topoisomerase inhibitors Interrupt DNA synthesis Other Various mechanisms including interrupting DNA and RNA synthesis in leukemia cells
DOSAGE, HANDLING, AND ADMINISTRATION Antineoplastic drugs are often mutagenic, teratogenic, and carcinogenic Direct contact can result in local injury Extravasation of vesicants
NONCYTOTOXIC CHEMOTHERAPY AGENTS Hormonal agents: Effective against tumors that are supported or suppressed by hormones Hormone agonists cause increase in hormone Hormone antagonists block certain hormones Biological response modulators: Act as immunostimulants to enhance the immune response and reduce proliferation of cancer cells Targeted antineoplastic agents: Antibodies or small molecules that attach to specific target sites
TISSUE GROWTH AND CHEMOTHERAPY Chemotherapy drugs are more toxic to tissue with high growth fraction Bone marrow Skin Hair follicles Sperm Gastrointestinal tract
OBSTACLES TO SUCCESSFUL CHEMOTHERAPY Toxicity to normal cells Cure requires 100% cell kill Kinetics of drug-induced cell kill Host defenses contribute little to cell kill When should treatment stop?
OBSTACLES TO SUCCESSFUL CHEMOTHERAPY Absence of truly early detection Solid tumors respond poorly Drug resistance Heterogeneity of tumor cells Limited drug access to tumor cells
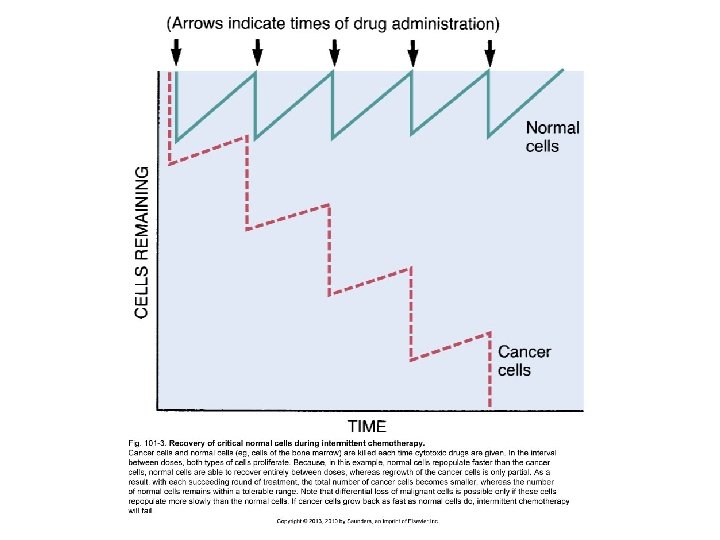
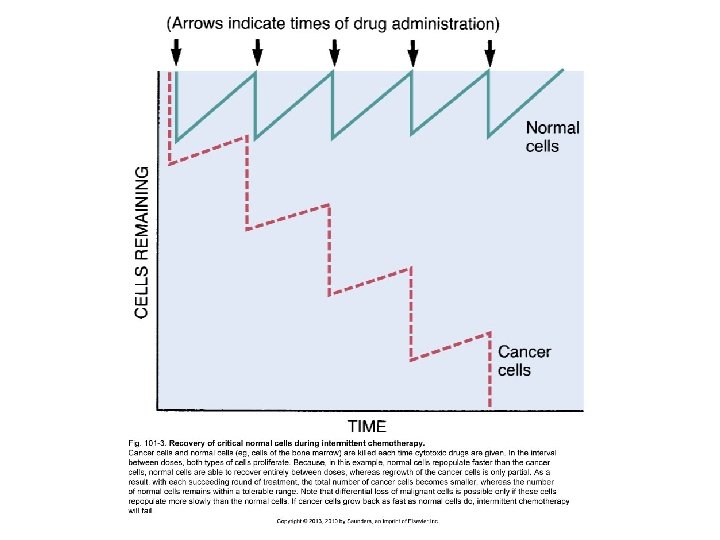
STRATEGIES FOR ACHIEVING MAXIMUM BENEFITS FROM CHEMOTHERAPY Intermittent chemotherapy Combination chemotherapy Benefits of drug combinations Suppression of drug resistance Increased cancer cell kill Reduced injury to normal cells Optimizing dosing schedules
STRATEGIES FOR ACHIEVING MAXIMUM BENEFITS FROM CHEMOTHERAPY Regional drug delivery Intra-arterial Intrathecal Other specialized routes
MAJOR TOXICITIES OF CANCER CHEMOTHERAPY Bone marrow suppression Neutropenia Thrombocytopenia Anemia Digestive tract injury stomatitis Nausea, vomiting, diarrhea
MAJOR TOXICITIES OF CANCER CHEMOTHERAPY Alopecia Hyperuricemia Reproductive toxicity Local injury from extravasation of vesicants Unique toxicities Carcinogenesis
IMMUNOTHERAPY Involves the use of: Interferons: glycoproteins produced by immune cells in response to viral infections Interleukins: peptides produced and secreted by WBCs Lymphokines and cytokines Monoclonal antibodies: antibodies with identical structure that bind with specific target antigens Generally used as adjuncts to surgery, radiation, and chemotherapy
IMMUNOTHERAPY https: //youtu. be/_Au 5 plb. Xm 3 Y
GENE AND MOLECULAR THERAPY May have high therapeutic potential May be used to suppress overactive oncogenes May replenish missing tumor suppressor function Current uses: Genetic alteration of tumor cells to make them more susceptible to cytotoxic agents or immune recognition Genetic alteration of immune cells to make them more efficient killers of tumor cells Enhance the host’s immune system against the cancer
STEM CELL TRANSPLANTATION Used to manage life-threatening disorders in which patient’s bone marrow cannot manufacture white blood cells, red blood cells, or platelets Used in malignant and non-malignant disorders Provides a method to restore bone marrow function after high-dose radiation or chemotherapy Need donor
MAKING THE DECISION TO TREAT Benefits of treatment must outweigh risks Patient must be given some idea of the benefits of proposed therapy One of these three should be possible: Cure, prolongation of life, palliation