Neonatology The State of the Unit Melinda J









































- Slides: 77
Neonatology: The State of the Unit Melinda J Elliott, M. D. Pediatric Grand Rounds March 16, 2010
Objectives • Sinai Demographics • Vermont-Oxford Network Data – Perinatal Trends – Morbidities and PI • • Necrotizing Enterocolitis Infections Chronic Lung Disease Retinopathy of Prematurity Intraventricular Hemorrhage Hypothermia Breast Milk Usage in the NICU – Mortality Data
Sinai NICU Admissions 2000 -2008 Total =249

Sinai NICU Patient Days 5382 in 2008

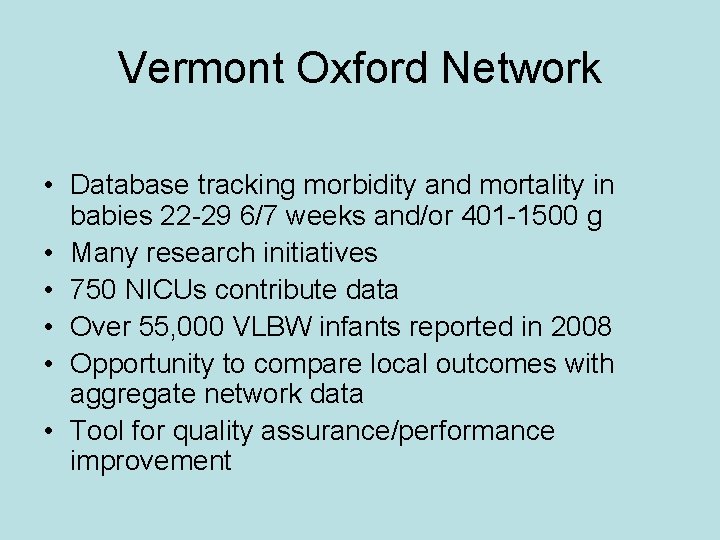
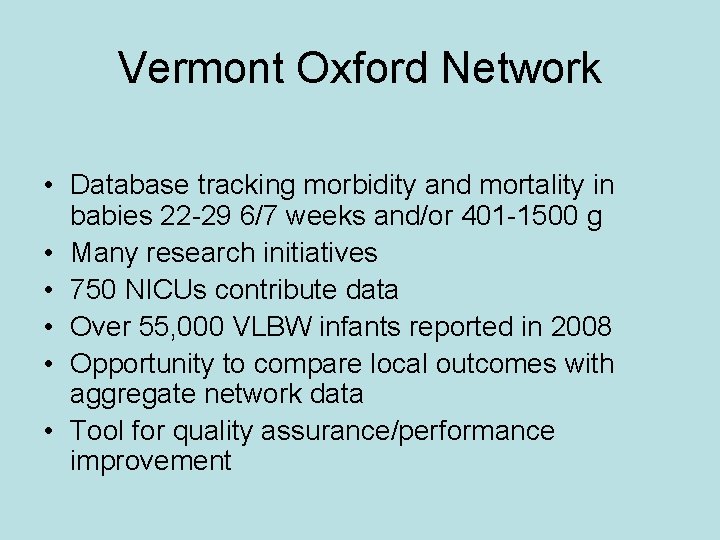
Vermont Oxford Network • Database tracking morbidity and mortality in babies 22 -29 6/7 weeks and/or 401 -1500 g • Many research initiatives • 750 NICUs contribute data • Over 55, 000 VLBW infants reported in 2008 • Opportunity to compare local outcomes with aggregate network data • Tool for quality assurance/performance improvement
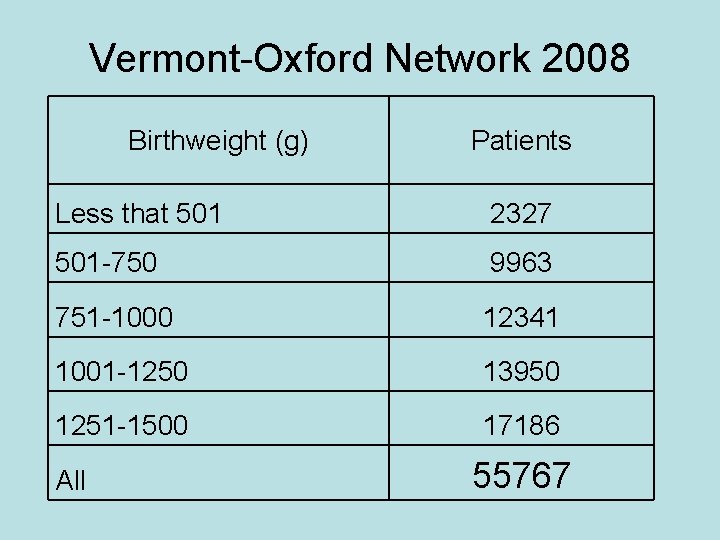
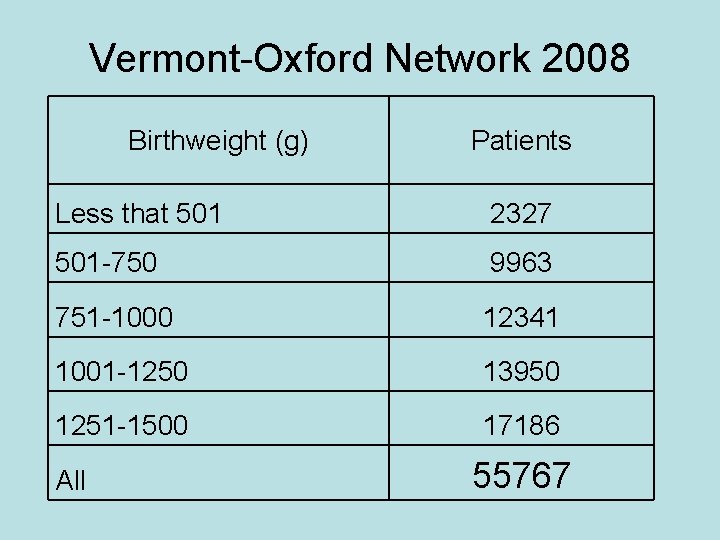
Vermont-Oxford Network 2008 Birthweight (g) Patients Less that 501 2327 501 -750 9963 751 -1000 12341 1001 -1250 13950 1251 -1500 17186 All 55767




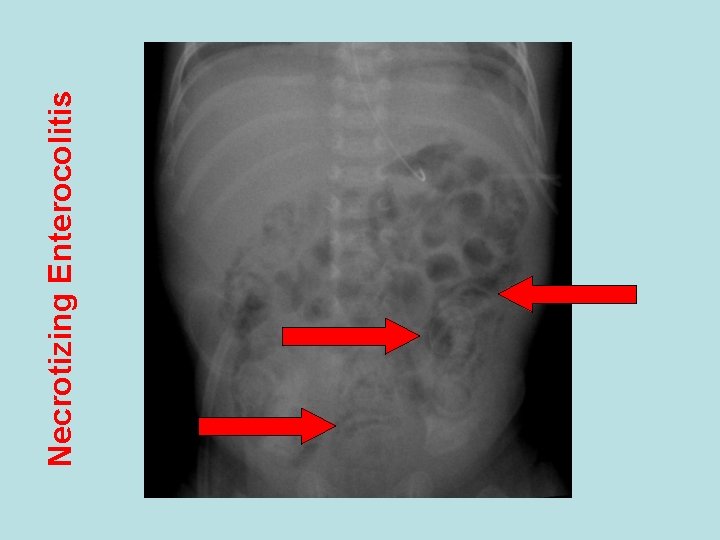
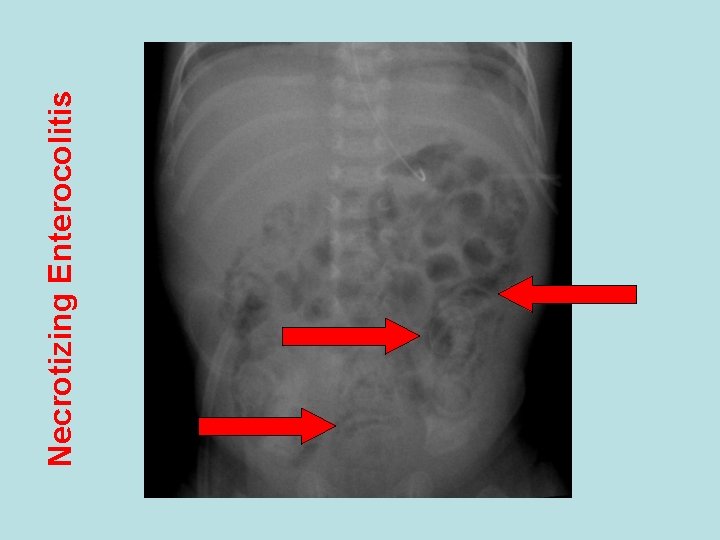
Necrotizing Enterocolitis

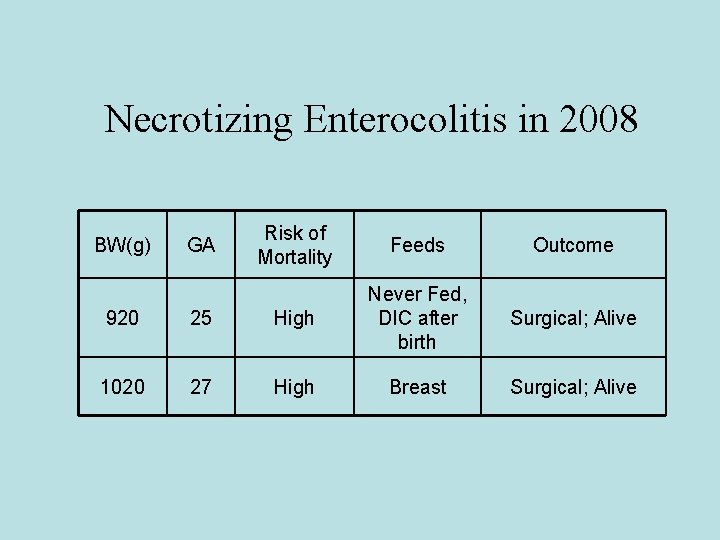
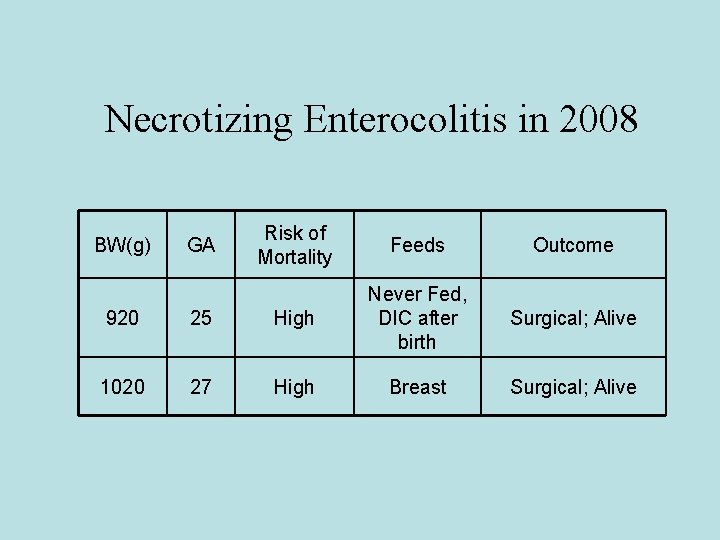
Necrotizing Enterocolitis in 2008 BW(g) GA Risk of Mortality Feeds Outcome Surgical; Alive 920 25 High Never Fed, DIC after birth 1020 27 High Breast
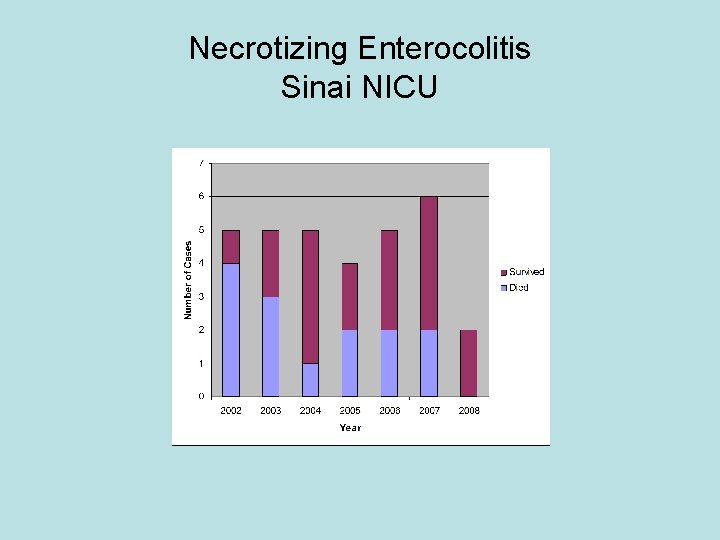
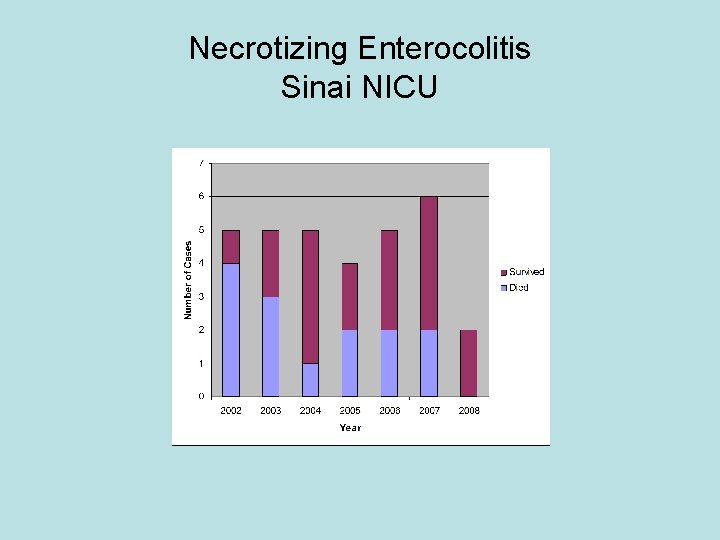
Necrotizing Enterocolitis Sinai NICU

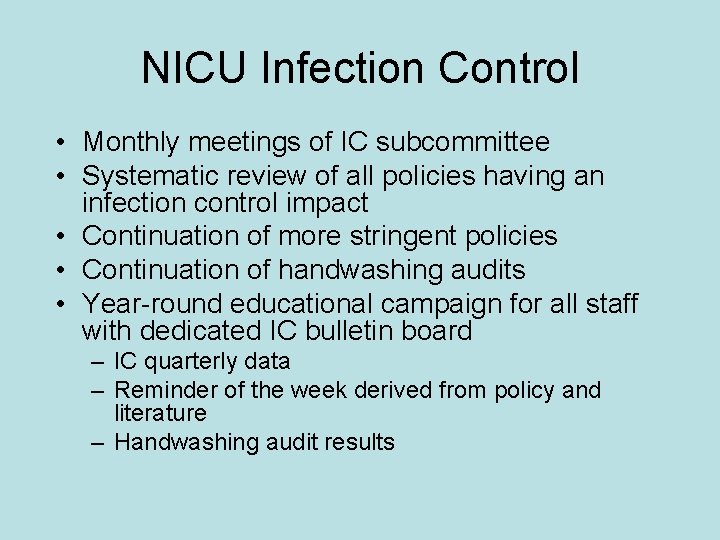
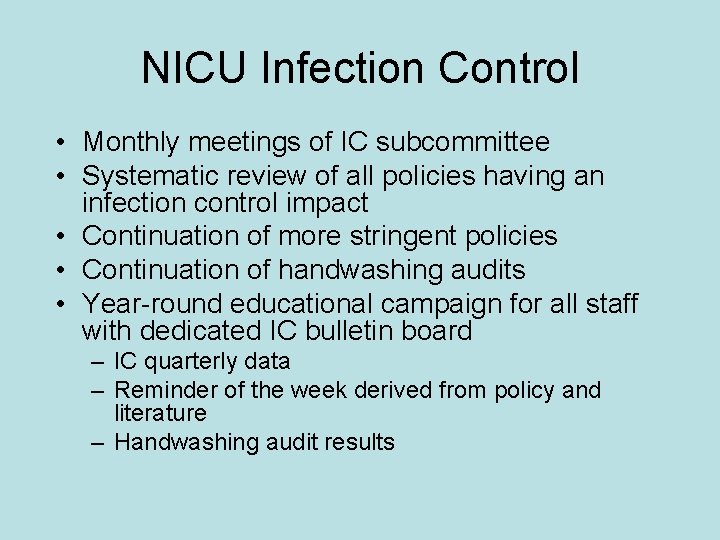
NICU Infection Control • Monthly meetings of IC subcommittee • Systematic review of all policies having an infection control impact • Continuation of more stringent policies • Continuation of handwashing audits • Year-round educational campaign for all staff with dedicated IC bulletin board – IC quarterly data – Reminder of the week derived from policy and literature – Handwashing audit results







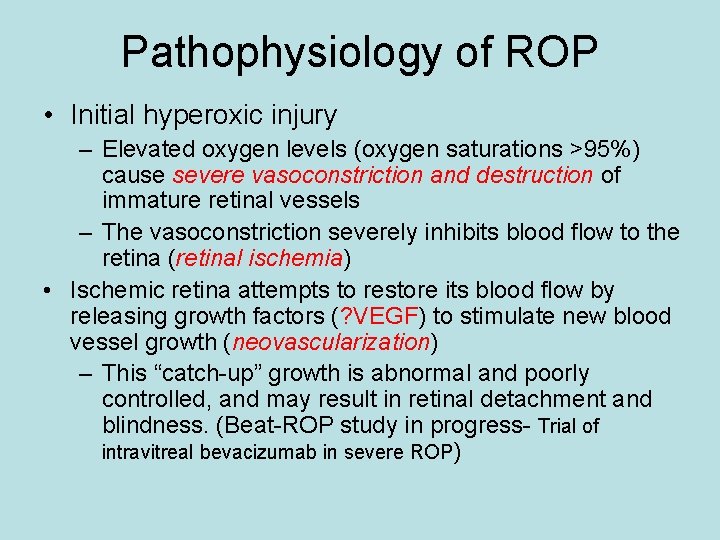
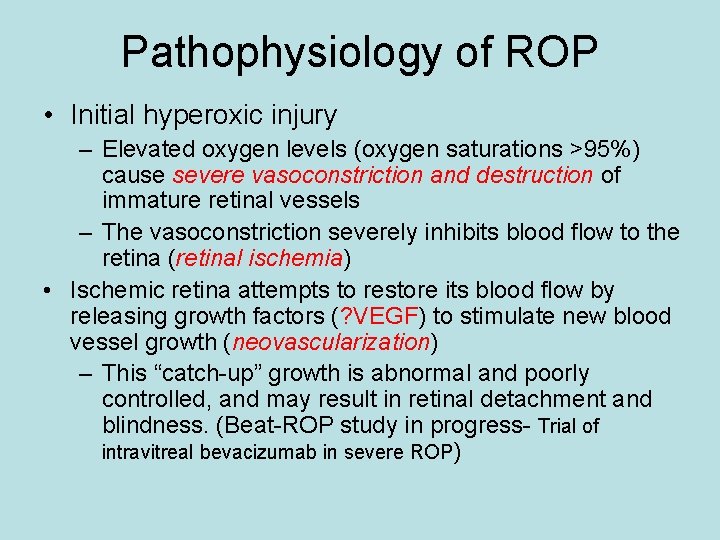
Pathophysiology of ROP • Initial hyperoxic injury – Elevated oxygen levels (oxygen saturations >95%) cause severe vasoconstriction and destruction of immature retinal vessels – The vasoconstriction severely inhibits blood flow to the retina (retinal ischemia) • Ischemic retina attempts to restore its blood flow by releasing growth factors (? VEGF) to stimulate new blood vessel growth (neovascularization) – This “catch-up” growth is abnormal and poorly controlled, and may result in retinal detachment and blindness. (Beat-ROP study in progress- Trial of intravitreal bevacizumab in severe ROP)
ROP-Prevention • For premature babies on oxygen therapy – Avoid hyperoxia – Avoid wide fluctuations in oxygen saturations – Keep oxygen saturations well controlled within set limits depending on postmenstrual age
ROP Subcommittee • Technology currently in use: – Massimo pulse oximetry – O 2 blenders • Bedside • Transporters • Delivery rooms
ROP Subcommittee • Staff Education – Multiple educational seminars completed • Oxygen Targeting Protocol – Developed in tandem with ROP initiative in Pediatrix Medical Group – Officially implemented December 2007 – Ongoing compliance audits
Hidden Oxygen Use Seen With: • Large rather than small incremental changes in O 2 for desaturations • Correctly identify and treat the underlying cause for the desaturation (apnea) • Not responding quickly enough to high alarms • Placing the infant back on O 2 targeting protocol when going from RA back on O 2 • Pre-oxygenating for procedures or suctioning

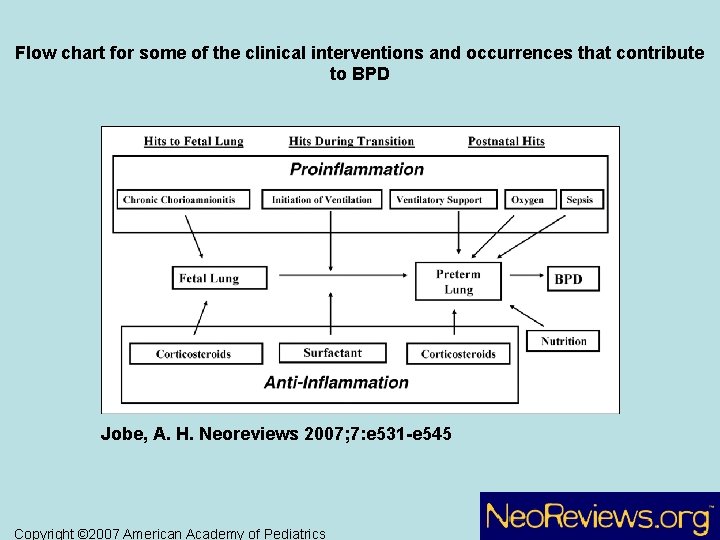
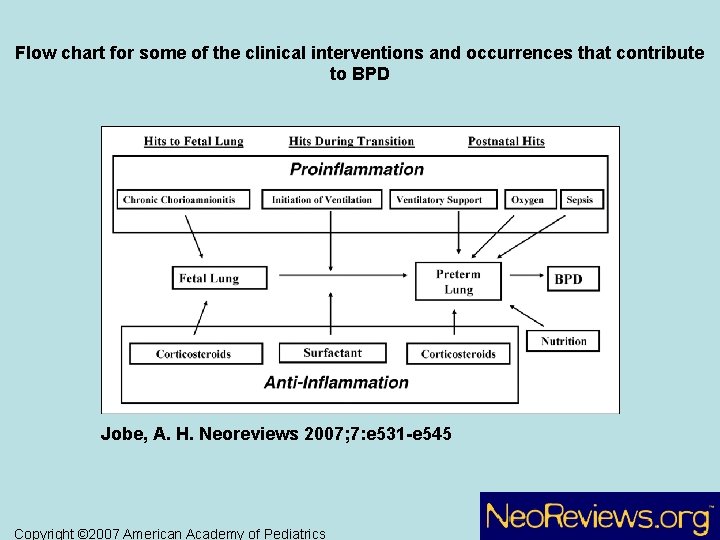
Flow chart for some of the clinical interventions and occurrences that contribute to BPD Jobe, A. H. Neoreviews 2007; 7: e 531 -e 545 Copyright © 2007 American Academy of Pediatrics






Chronic Lung Disease (CLD) Algorithm • If the infant is hospitalized at 36 weeks, CLD is based on whether the infant was on oxygen at 36 weeks, as answered on the Discharge Form. • If the infant is discharged between 34 and 36 weeks CGA, CLD is coded YES if the infant was on oxygen at the time of discharge and is coded NO if the infant was not on oxygen at the time of discharge. • If the infant is discharged home or transferred before 34 weeks CGA and the infant was not on oxygen at the time of discharge, CLD is coded NO. • If the infant’s gestational age is unknown, or if the infant is discharged home or transferred before 34 weeks CGA and the infant was on oxygen at the time of discharge, CLD is coded as unknown and the case is not considered in calculating CLD rates. • If the infant dies in the delivery room or prior to 36 weeks CGA, or if the infant’s gestational age is greater than 36 weeks, CLD is coded as not applicable and the case is not considered in calculating CLD rates.
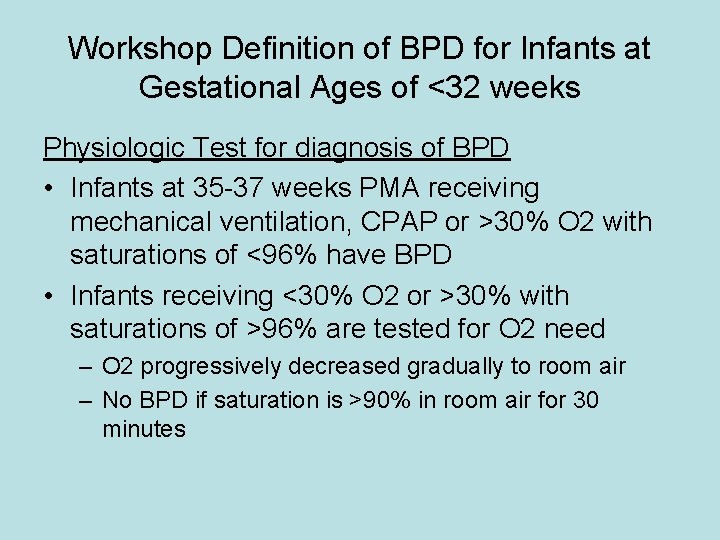
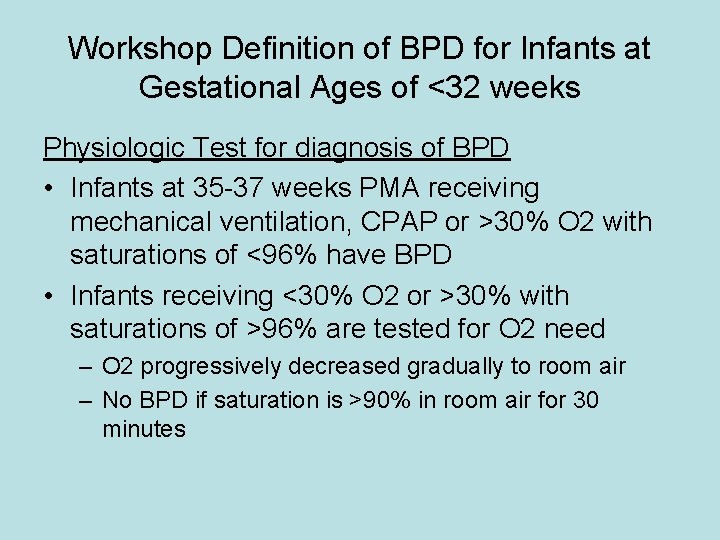
Workshop Definition of BPD for Infants at Gestational Ages of <32 weeks Physiologic Test for diagnosis of BPD • Infants at 35 -37 weeks PMA receiving mechanical ventilation, CPAP or >30% O 2 with saturations of <96% have BPD • Infants receiving <30% O 2 or >30% with saturations of >96% are tested for O 2 need – O 2 progressively decreased gradually to room air – No BPD if saturation is >90% in room air for 30 minutes






Prevention of Hypothermia in the Preterm Infant

World Health Organization (WHO) classification of hypothermia • Core temperatures – Mild 36 -36. 4 degree C – Moderate 32 -35. 9 degree C – Severe < 32 degree C
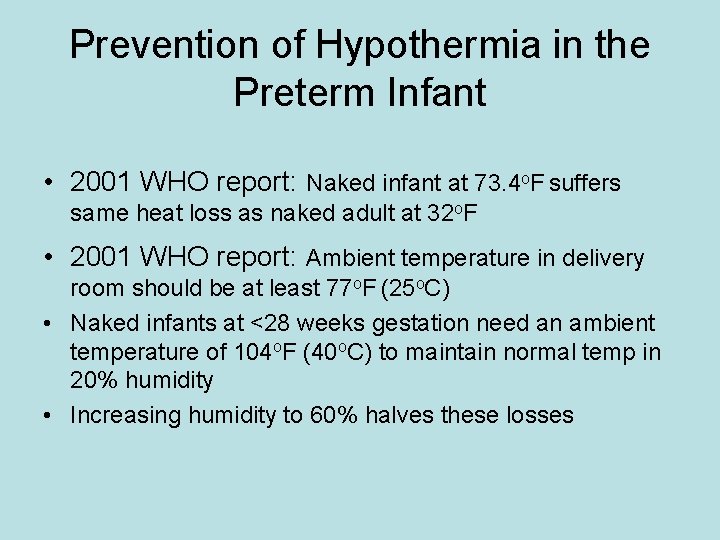
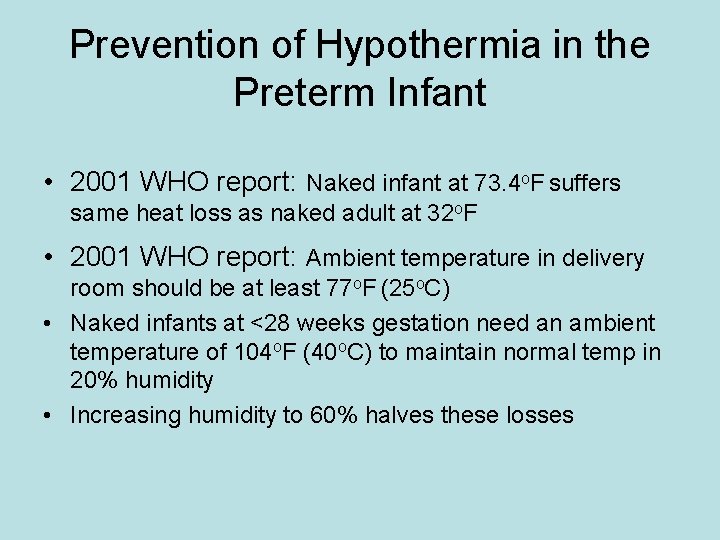
Prevention of Hypothermia in the Preterm Infant • 2001 WHO report: Naked infant at 73. 4 o. F suffers same heat loss as naked adult at 32 o. F • 2001 WHO report: Ambient temperature in delivery room should be at least 77 o. F (25 o. C) • Naked infants at <28 weeks gestation need an ambient temperature of 104 o. F (40 o. C) to maintain normal temp in 20% humidity • Increasing humidity to 60% halves these losses
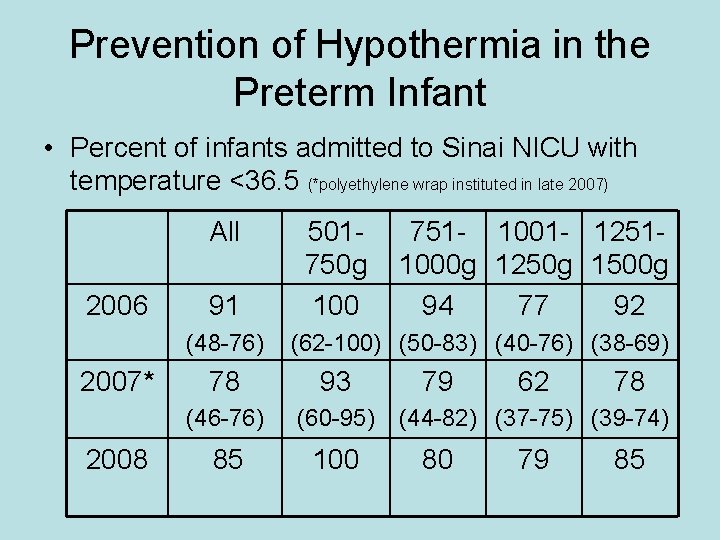
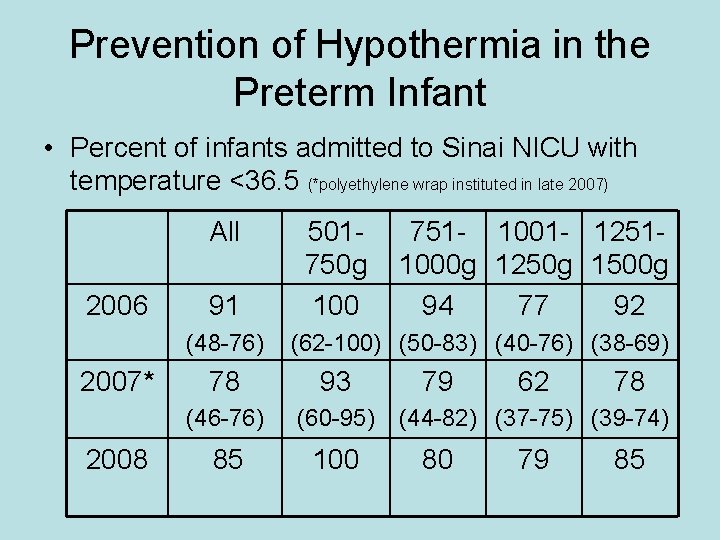
Prevention of Hypothermia in the Preterm Infant • Percent of infants admitted to Sinai NICU with temperature <36. 5 (*polyethylene wrap instituted in late 2007) All 2006 91 (48 -76) 2007* 2008 501750 g 100 751 - 1001 - 12511000 g 1250 g 1500 g 94 77 92 (62 -100) (50 -83) (40 -76) (38 -69) 78 93 (46 -76) (60 -95) 85 100 79 62 78 (44 -82) (37 -75) (39 -74) 80 79 85
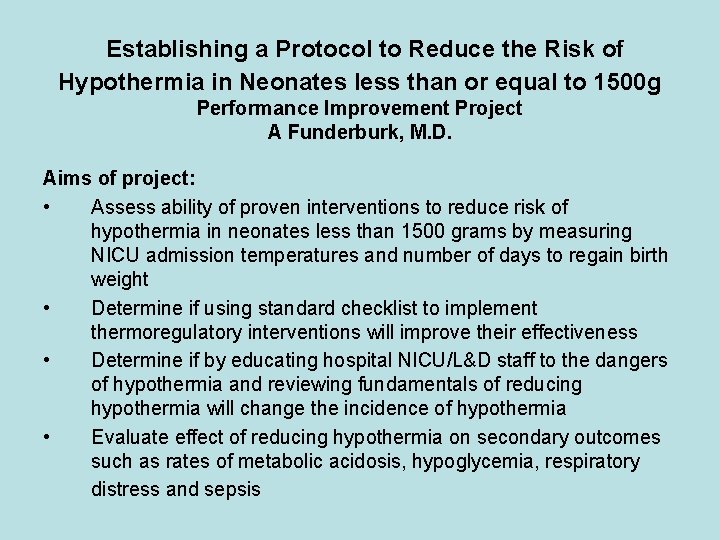
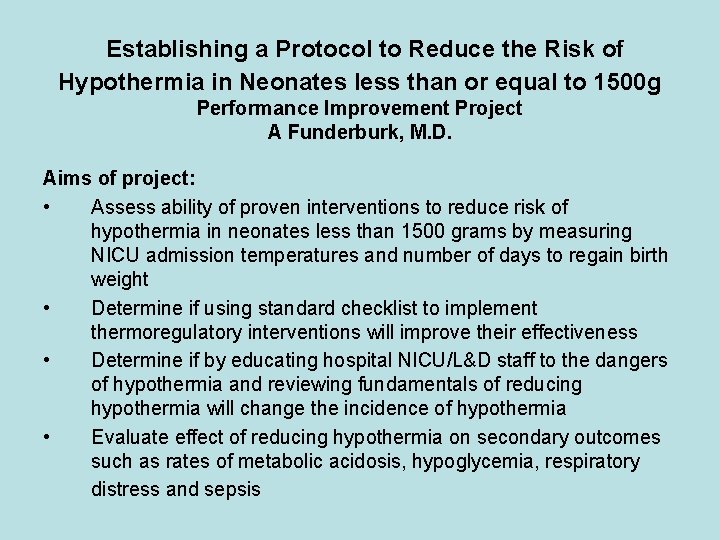
Establishing a Protocol to Reduce the Risk of Hypothermia in Neonates less than or equal to 1500 g Performance Improvement Project A Funderburk, M. D. Aims of project: • Assess ability of proven interventions to reduce risk of hypothermia in neonates less than 1500 grams by measuring NICU admission temperatures and number of days to regain birth weight • Determine if using standard checklist to implement thermoregulatory interventions will improve their effectiveness • Determine if by educating hospital NICU/L&D staff to the dangers of hypothermia and reviewing fundamentals of reducing hypothermia will change the incidence of hypothermia • Evaluate effect of reducing hypothermia on secondary outcomes such as rates of metabolic acidosis, hypoglycemia, respiratory distress and sepsis

Establishing a Protocol to Reduce the Risk of Hypothermia in Neonates less than or equal to 1500 g Performance Improvement Project A Funderburk, M. D. • Established protocol for delivery room temp, use of polyethylene wrap, pre-warming radiant heaters, etc, now in place • Data collection complete and results being analyzed now for admission and subsequent temps, and secondary outcomes such as metabolic acidosis, hypoglycemia, IVH, LOS, etc • Preliminary data show significant increase in admission temps for 2009. Final results next year
Breast Milk in the NICU Why is it important?
Benefits of Human Milk: Infectious Diseases Strong evidence exists that human milk feedings decrease the incidence and/or severity of a wide range of infectious diseases: • Late-onset sepsis in preterm infants • Necrotizing enterocolitis • Bacterial meningitis • Bacteremia • Respiratory tract infection • Urinary tract infection • Otitis media • Diarrhea Pediatrics. 2005 Feb; 115(2): 496 -506

Benefits of Human Milk: Mortality Post-neonatal infant mortality rates in the United States are reduced by 21% in breastfed infants Pediatrics. 2005 Feb; 115(2): 496 -506
Benefits of Human Milk: Other Health Outcomes Studies suggest decreased rates of: • Sudden infant death syndrome • Insulin-dependent (type 1) diabetes mellitus • Non–insulin-dependent (type 2) diabetes mellitus • Asthma • Lymphoma • Leukemia • Hodgkin disease • Obesity • Hypercholesterolemia Pediatrics. 2005 Feb; 115(2): 496 -506
Benefits of Human Milk: Neurodevelopment • Breastfeeding has been associated with slightly enhanced performance on tests of cognitive development • Breastfeeding during a painful procedure such as a heel-stick for newborn screening provides analgesia to infants Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. NICHD, Pediatrics. 2006 Jul; 118(1): e 115 -23 – Every 10 m. L/kg per day breast milk contributed 0. 53 points to the Bayley Mental Development Index; therefore, the impact of breast milk ingestion during the hospitalization for infants in the highest quintile (110 m. L/kg per day) on the Bayley Mental Development Index would be 10 x 0. 53, or 5. 3 points. – The potential long-term benefit of receiving breast milk in the NICU for extremely low birth weight infants may be to optimize cognitive potential and reduce the need for early intervention and Pediatrics. 2005 Feb; 115(2): 496 -506 special education services

Benefits of Human Milk: Maternal Health Benefits Important health benefits of breastfeeding and lactation are also described for mothers: • Decreased postpartum bleeding and more rapid uterine involution attributable to increased concentrations of oxytocin • Decreased menstrual blood loss and increased child spacing attributable to lactational amenorrhea • Earlier return to prepregnancy weight • Decreased risk of breast cancer • Decreased risk of ovarian cancer • Possibly decreased risk of hip fractures and osteoporosis in the postmenopausal period Pediatrics. 2005 Feb; 115(2): 496 -506
Benefits of Human Milk: Community Benefits • Potential for decreased annual health care costs of $3. 6 billion in the United States • Decreased costs for public health programs such as the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) • Decreased parental employee absenteeism and associated loss of family income • More time for attention to siblings and other family matters as a result of decreased infant illness • Decreased environmental burden for disposal of formula cans and bottles • Decreased energy demands for production and transport of artificial feeding products Pediatrics. 2005 Feb; 115(2): 496 -506
Benefits of Human Milk: Summary • Human milk is the recommended source of nutrition for preterm and term newborns • Human milk has a large number of health benefits for babies, mothers, and society Human milk is an extremely important MEDICATION that should be used in every newborn!!!
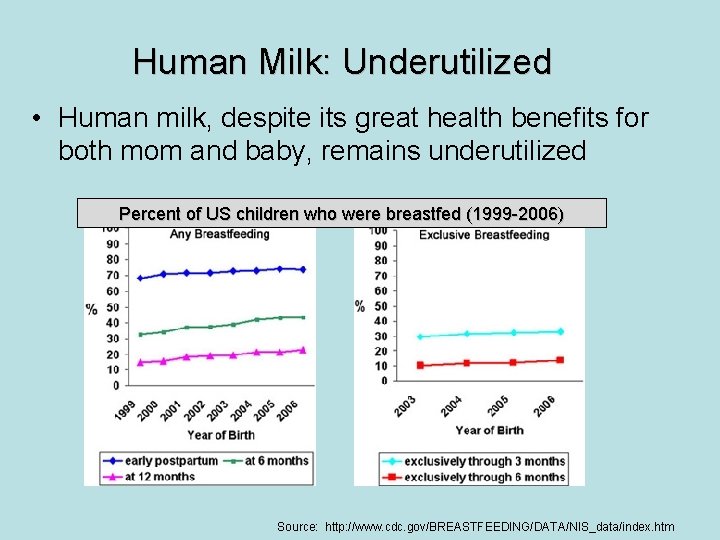
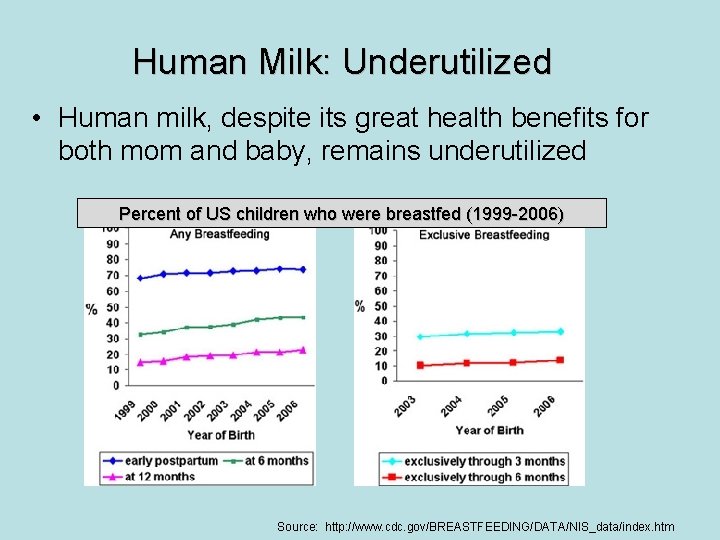
Human Milk: Underutilized • Human milk, despite its great health benefits for both mom and baby, remains underutilized Percent of US children who were breastfed (1999 -2006) Source: http: //www. cdc. gov/BREASTFEEDING/DATA/NIS_data/index. htm
Human Milk: Underutilized in NICU Babies • Human milk utilization is even worse in the NICU population • Breast milk use at discharge is only ~40% for babies born 501 -1500 grams • Utilization for larger NICU babies is slightly higher, but still lower than term babies Despite NICU babies being at higher risk for NEC, infection, ROP, neurodevelopmental impairment, etc – they have the lowest rates of human milk utilization. The babies that need human milk the most are the group least likely to receive it!! Source: Pediatrix Clinical Data Warehouse
WHY? ?
Highly suggested reading for the entire NICU staff J Obstet Gynecol Neonatal Nurs. 2005; 34: 109
Two questions, two barriers Maternity and neonatal nurses have raised several questions about talking with women about lactation for their infants, but two are the most common: 1. “Does it really matter? ” — or — “Is there a clinically significant difference between formula and mothers’ milk for infants? ” 2. “Won’t I make these women feel guilty or pressured if I promote lactation, because infant feeding method should be a personal choice? ” J Obstet Gynecol Neonatal Nurs. 2005; 34: 109
Does it really matter? YES, IT REALLY DOES!! • Review the first half of the presentation again – there are multiple very real advantages to providing human milk (for both mom and baby) • Hundreds of scientific papers have been published on this topic • Human milk is superior to formula • Formula is inferior to human milk
What if I make mom feel guilty? • Contrary to common assumptions, several studies show that women want evidence-based knowledge about formula and mothers’ milk feedings to make an informed choice for themselves and their infants. • In one study, moms were asked about their initial feeding intent, they indicated that they initially planned to formula feed primarily because they “did not know anyone who had ever breastfed” or because they felt that lactation would involve discomfort and lifestyle changes. • All mothers reported that the major reason they changed the initial decision was hearing from a health care provider that their milk was best for their infant. Moms want what is best for their babies – it is our responsibility to make sure that they clearly understand that human milk is the best choice. J Obstet Gynecol Neonatal Nurs. 2005; 34: 109

What if I make mom feel guilty? • Consider this: What if a mom decides to not provide human milk, and no staff member discusses this with her further, out of fear of making her feel guilty. • What if her baby gets NEC, and she reads somewhere that breast milk use is associated with a lower incidence of NEC? Do you think she will feel guilty then? This is not about “making someone feel guilty” – this is about providing important information to families so they can make the best decisions possible for their baby. J Obstet Gynecol Neonatal Nurs. 2005; 34: 109
Please counsel all your patients about the benefits of breast feeding, particularly those with premature infants. Continue this discussion with every interaction you have with them!



NICU Mortality 2008 Birthweight (g) Gest. Age Cause of Death 650 241 Acute air embolus, pneumopericardium 570 234 Twin B, Respiratory failure 2100 280 Hypoplastic lungs, Hydrops, Died at < 12 Hours of life 580 231 Twin A, Grade IV ICH, Removed from life support 500 231 Twin B, Grade IV ICH, Removed from life support 600 241 Respiratory failure, severe pulmonary hemorrhage, grade III ICH

Delivery Room Deaths 2008 Birthweight (g) Gest. Age (weeks) 545 216 526 215 478 223


Survival to Discharge Without Known Morbidity*** Infants 501 -1500 grams Sinai NICU 2008 ***None of the following morbidities at discharge: Severe IVH, CLD, NEC, pneumothorax, any nosocomial infection, PVL, Extreme LOS


 Neonatology lectures
Neonatology lectures History of neonatology
History of neonatology Oecd meaning
Oecd meaning Alexis reich burke ramsey
Alexis reich burke ramsey Melinda and danny
Melinda and danny Speak tree project
Speak tree project Melinda haley
Melinda haley Melinda starr
Melinda starr Melinda kellogg
Melinda kellogg Signing naturally 5:4
Signing naturally 5:4 Who are stephanie and iva talking about
Who are stephanie and iva talking about Melinda marquis
Melinda marquis Vanderbilt isfaa form
Vanderbilt isfaa form Melinda sawyer
Melinda sawyer Melinda orta nwea
Melinda orta nwea Fazekas vivien gyereke
Fazekas vivien gyereke Melinda trask
Melinda trask The elevator incident by melinda
The elevator incident by melinda The elevator incident by melinda answers
The elevator incident by melinda answers Forgó melinda
Forgó melinda Hidvéghy melinda
Hidvéghy melinda Melinda butler
Melinda butler Melinda marquis
Melinda marquis The bill melinda gates
The bill melinda gates Melinda jaco
Melinda jaco Melinda haley
Melinda haley Flyslides
Flyslides Melinda haley
Melinda haley Aszeptikus csomagolás
Aszeptikus csomagolás Melinda haley
Melinda haley Melinda haley
Melinda haley Unit 6 review questions
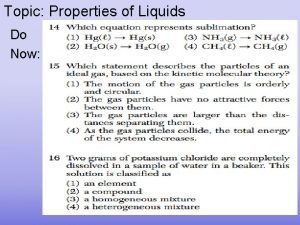
Unit 6 review questions Properties of liquid in matter
Properties of liquid in matter State to state regionalism
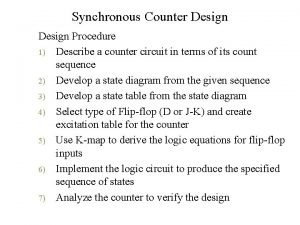
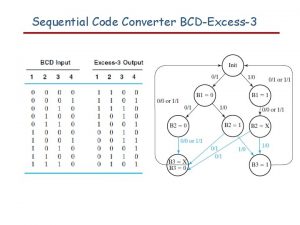
State to state regionalism Excitation table
Excitation table Good and bad state graphs
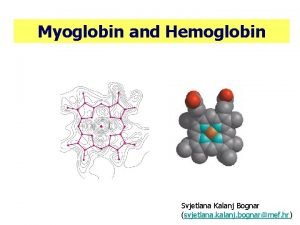
Good and bad state graphs Svjetlana kalanj bognar
Svjetlana kalanj bognar What is the difference between an orbital and a shell
What is the difference between an orbital and a shell T and r state of hemoglobin
T and r state of hemoglobin Absorptive state vs postabsorptive state
Absorptive state vs postabsorptive state Pka glycogen
Pka glycogen Age of consent state by state
Age of consent state by state Current state vs future state slide
Current state vs future state slide Equivalent state
Equivalent state New state drink
New state drink State state graphs and transition testing
State state graphs and transition testing What is initial state + goal state in search terminology?
What is initial state + goal state in search terminology? Tasscc state of the state
Tasscc state of the state Submachine state in state diagram
Submachine state in state diagram Connecticut comptroller
Connecticut comptroller Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế worms-breton
Tư thế worms-breton Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế