Neonatal Resuscitation Dr Afkar Ragab Assist Prof Pediatric
Neonatal Resuscitation Dr. Afkar Ragab Assist. Prof. Pediatric Nursing 1/30/2022
Antepartum Risk Factors o Maternal Age >35 Yrs. Or <16 Yrs. o Maternal Diabetes o Maternal Hemorrhage Substance Abuse o Drug Therapy Previous NN Death Lack of Prenatal Care Maternal Hypertension 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Antepartum Risk Factors o o o Anemia Maternal Illness Multiple Fetuses SGA Preterm/Post-term Fetus Premature ROM 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
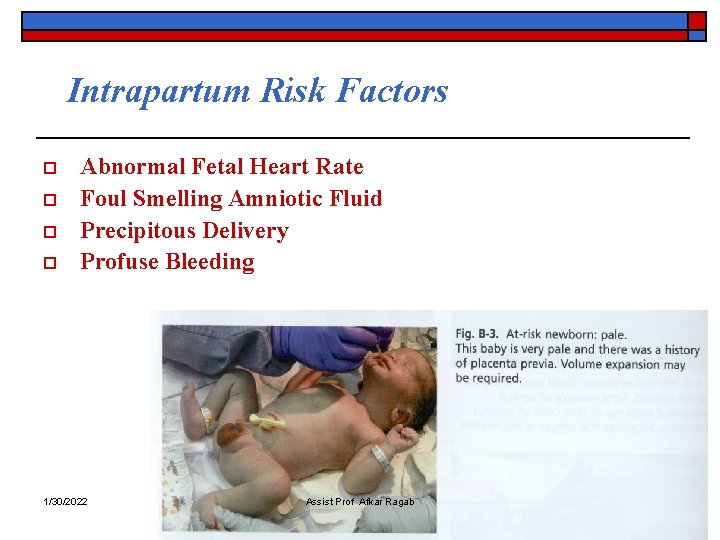
Intrapartum Risk Factors o o Abnormal Fetal Heart Rate Foul Smelling Amniotic Fluid Precipitous Delivery Profuse Bleeding 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Intrapartum Risk Factors o o o o Abnormal Presentation Infection Prolonged Labor Prolonged ROM Prolapsed Cord Maternal Sedation Meconium Stained Amniotic Fluid 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Core Knowledge and Skills o o Air ways- Establish Clear Airway Breathing- Ventilation & Oxygenation Circulation- Adequate Cardiac Output Reduce Heat Loss 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Phases of Resuscitation o o o Preperation Resuscitation Postresuscitaion 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Neutral Thermal Environmental o o o Overhead Warmer Heat Lamps Incubator Warm Towels & Blankets Warm Water Filled Gloves 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Resuscitation Equipment o o o Organized Readily Accessible Easy to Assemble 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Universal Precautions o o o Gloves Goggles Gown 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab

Neonatal Drug Preparations o Precalculated Drugs Sodium Bicarbonate 0. 5 m. Eq/L Epinephrine 1: 10000 o Broselow Tape 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab

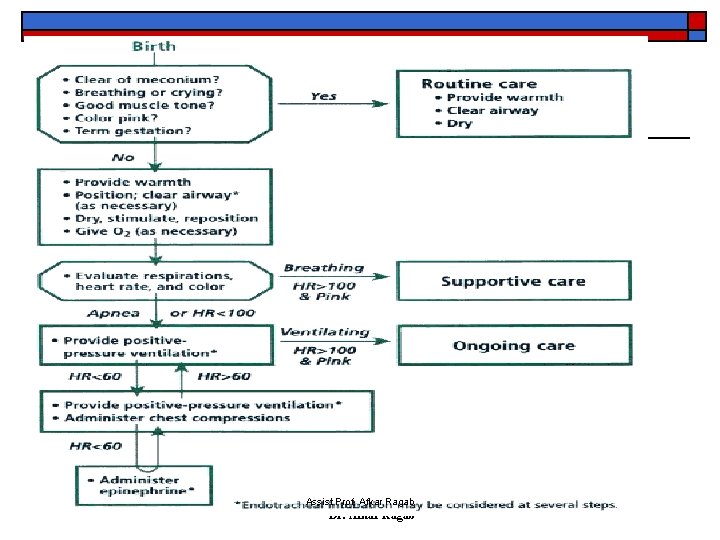
Resuscitation Priorities Drying, Warming, Positioning Suctioning, Stimulation BVM Vent Oxygen Chest Compressions Intubations Bag-Valve-Mask Medication Ventilation 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Resuscitation Priorities • Oxygen • Indications: Dusky, Poor Tone, Breathing Spont. • Route Blow By or Mask if Breathing Spontaneously 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
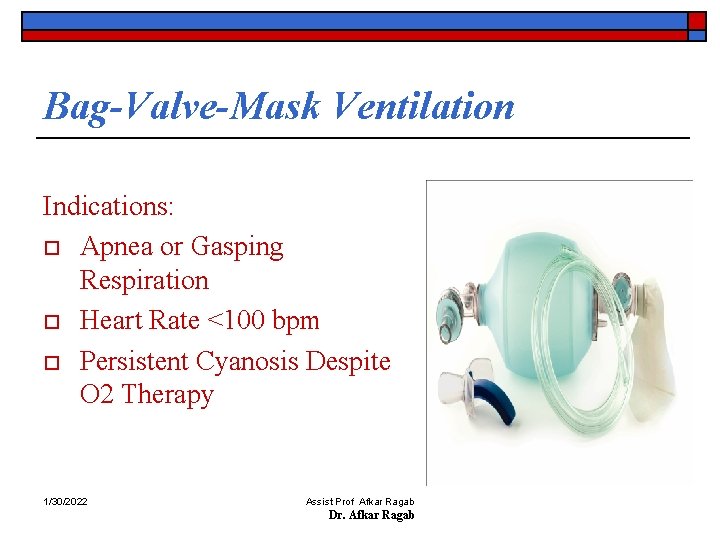
Bag-Valve-Mask Ventilation Indications: o Apnea or Gasping Respiration o Heart Rate <100 bpm o Persistent Cyanosis Despite O 2 Therapy 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Ventilation of the Newborn Assisted rate= 40 to 60 bpm Signs of Adequate Ventilation • Bilateral Chest Expansion • Bilateral Breath Sounds • Adequate Heart Rate & Color 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Indications for Intubation o BVM Ventilation Not Effective o Thick Meconium o Prolonged Positive Press. Vent. 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
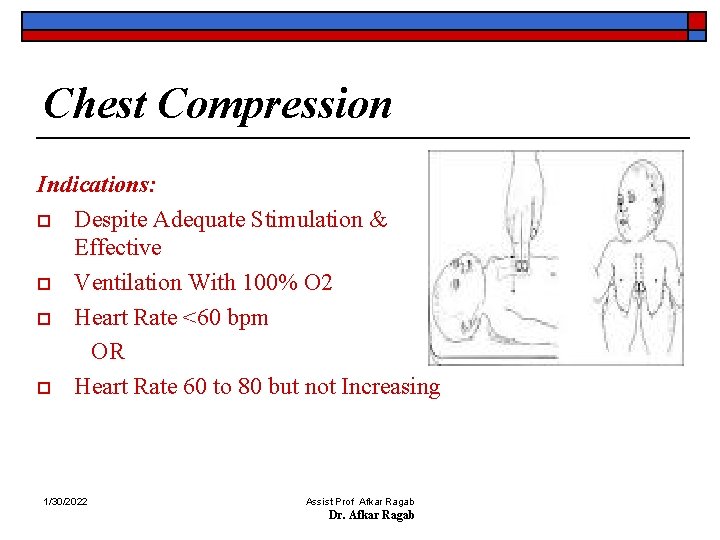
Chest Compression Indications: o Despite Adequate Stimulation & Effective o Ventilation With 100% O 2 o Heart Rate <60 bpm OR o Heart Rate 60 to 80 but not Increasing 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Chest Compressions o o o Rate: 90 per minute, Interposed by Vent. Compression - Ventilation Ratio: 3: 1 Stop Compressions When HR >80 bpm 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
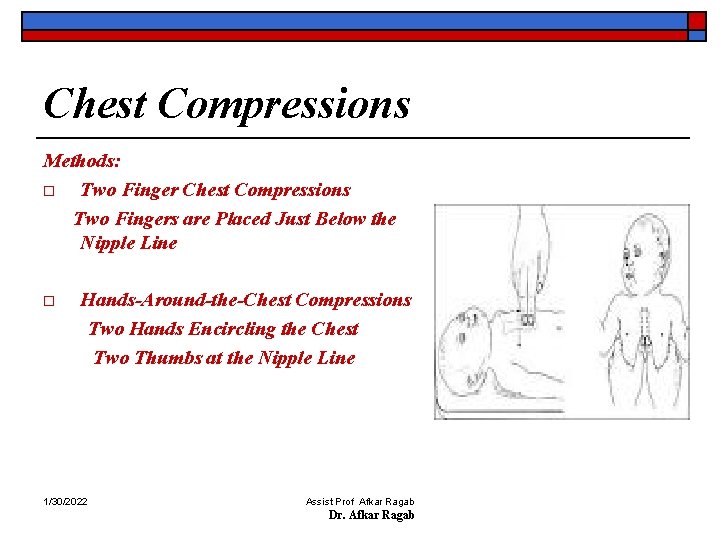
Chest Compressions Methods: o Two Finger Chest Compressions Two Fingers are Placed Just Below the Nipple Line o Hands-Around-the-Chest Compressions Two Hands Encircling the Chest Two Thumbs at the Nipple Line 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Medications “Epinephrine dose” n The recommended epinephrine dose is 0. 1 to 0. 3 m. L/kg of a 1: 10, 000 solution (0. 01 to 0. 03 mg/kg) repeated every 3 to 5 minutes as indicated. n Higher doses have been associated with increased risk of intracranial hemorrhage and myocardial damage. n 1/30/2022 No different dose for premature infants Assist Prof Afkar Ragab Dr. Afkar Ragab
Neonatal Resuscitation Ethics o o o Non-initiation of resuscitation in the delivery room may be appropriate in infants with: confirmed gestation < 23 weeks birthweight < 400 grams anencephaly confirmed trisomy 13 or 18 may be appropriate. Current data support that resuscitation of these newborns is very unlikely to result in survival or survival without severe disability. 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Neonatal Resuscitation Ethics o In cases of uncertain prognosis, including uncertain gestational age, a trial of therapy, non -initiation, or discontinuation of resuscitation remain options following assessment of the baby. o Ongoing evaluation and discussion with the parents and the health care team should guide continuation vs. withdrawal of support. 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Common Post-Resuscitation Airway Complications o o o Displaced ET Tube Pneumothorax Equipment Failure Inadequate Ventilatory Support Gastric Distension 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Post-Resuscitation Evaluation Care o o o Temperature Regulation Acid-Base Status Blood Glucose Laboratory Studies Chest X-Ray 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Documentation Written documentation of o Personal involved o All procedures including drugs o Timing 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
Conclusions o o o Some preparation and teaching in the bottom of successful resuscitation ventilation is the primary goal oxygenation can in most cases be obtained by room air - more studies are needed Chest compression and drugs are rarely needed ethics should carefully be considered All steps should be Documented 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
THANK YOU 1/30/2022 Assist Prof Afkar Ragab Dr. Afkar Ragab
- Slides: 28