Neonatal Opioid Withdrawal Syndrome Definitions Neonatal abstinence syndrome
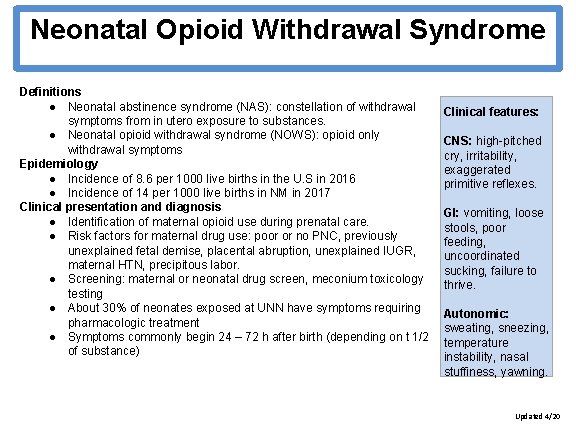
Neonatal Opioid Withdrawal Syndrome Definitions ● Neonatal abstinence syndrome (NAS): constellation of withdrawal symptoms from in utero exposure to substances. ● Neonatal opioid withdrawal syndrome (NOWS): opioid only withdrawal symptoms Epidemiology ● Incidence of 8. 6 per 1000 live births in the U. S in 2016 ● Incidence of 14 per 1000 live births in NM in 2017 Clinical presentation and diagnosis ● Identification of maternal opioid use during prenatal care. ● Risk factors for maternal drug use: poor or no PNC, previously unexplained fetal demise, placental abruption, unexplained IUGR, maternal HTN, precipitous labor. ● Screening: maternal or neonatal drug screen, meconium toxicology testing ● About 30% of neonates exposed at UNN have symptoms requiring pharmacologic treatment ● Symptoms commonly begin 24 – 72 h after birth (depending on t 1/2 of substance) Clinical features: CNS: high-pitched is the cry, What irritability, relative What is risk the exaggerated reduction of primitive reflexes. relative risk statins forof reduction GI: statins vomiting, loose primary for stools, poor prevention primary of feeding, CVD event? prevention of uncoordinated About 30%to CVD event? sucking, failure (an at-best estimate) thrive. About 30% (an at-best estimate) Autonomic: sweating, sneezing, temperature instability, nasal stuffiness, yawning. Updated 4/20
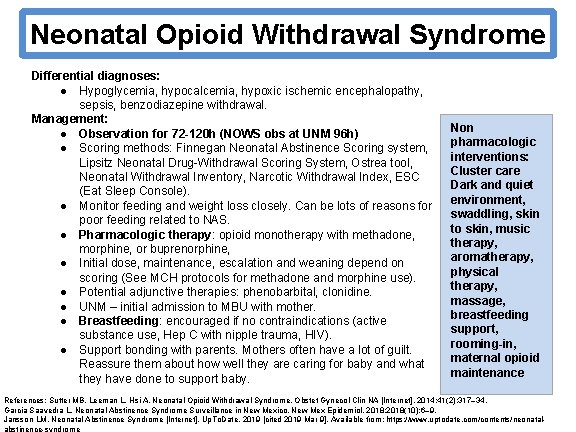
Neonatal Opioid Withdrawal Syndrome Differential diagnoses: ● Hypoglycemia, hypocalcemia, hypoxic ischemic encephalopathy, sepsis, benzodiazepine withdrawal. Management: ● Observation for 72 -120 h (NOWS obs at UNM 96 h) ● Scoring methods: Finnegan Neonatal Abstinence Scoring system, Lipsitz Neonatal Drug-Withdrawal Scoring System, Ostrea tool, Neonatal Withdrawal Inventory, Narcotic Withdrawal Index, ESC (Eat Sleep Console). ● Monitor feeding and weight loss closely. Can be lots of reasons for poor feeding related to NAS. ● Pharmacologic therapy: opioid monotherapy with methadone, morphine, or buprenorphine, ● Initial dose, maintenance, escalation and weaning depend on scoring (See MCH protocols for methadone and morphine use). ● Potential adjunctive therapies: phenobarbital, clonidine. ● UNM – initial admission to MBU with mother. ● Breastfeeding: encouraged if no contraindications (active substance use, Hep C with nipple trauma, HIV). ● Support bonding with parents. Mothers often have a lot of guilt. Reassure them about how well they are caring for baby and what they have done to support baby. Non pharmacologic interventions: What care is the Cluster relative risk Dark and quiet environment, reduction of swaddling, skin statins for to skin, music primary therapy, prevention of aromatherapy, CVD event? physical About 30% therapy, (an at-best estimate) massage, breastfeeding support, rooming-in, maternal opioid maintenance References: Sutter MB, Leeman L, Hsi A. Neonatal Opioid Withdrawal Syndrome. Obstet Gynecol Clin NA [Internet]. 2014; 41(2): 317– 34. Garcia Saavedra L. Neonatal Abstinence Syndrome Surveillance in New Mexico. New Mex Epidemiol. 2018; 2018(10): 6– 9. Jansson LM. Neonatal Abstinence Syndrome [Internet]. Up. To. Date. 2019 [cited 2019 Mar 9]. Available from: https: //www. uptodate. com/contents/neonatalabstinence-syndrome
- Slides: 2