Neonatal Neurology 2 Stroke Hemorrhage PVL CHO NICU
- Slides: 46
Neonatal Neurology 2: Stroke, Hemorrhage, PVL CHO NICU Lecture D Durand Revised 10/17/12
Stroke
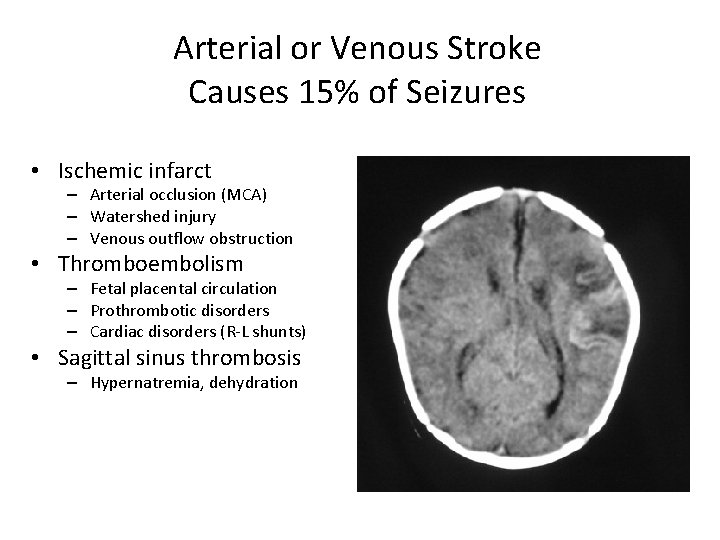
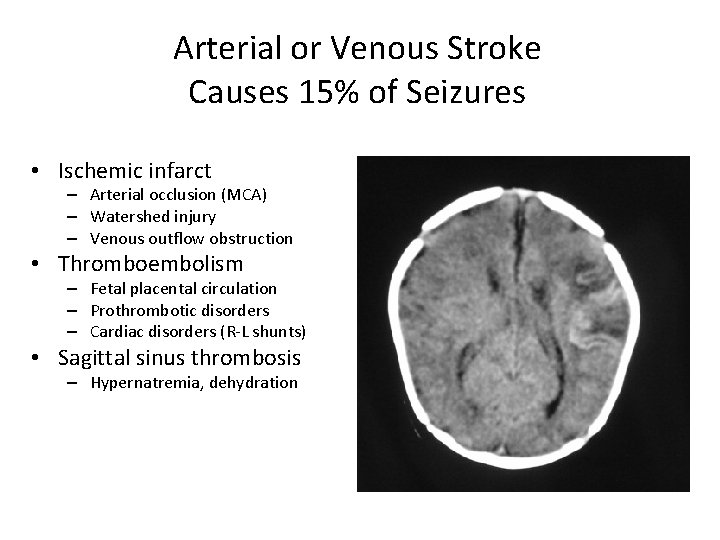
Arterial or Venous Stroke Causes 15% of Seizures • Ischemic infarct – Arterial occlusion (MCA) – Watershed injury – Venous outflow obstruction • Thromboembolism – Fetal placental circulation – Prothrombotic disorders – Cardiac disorders (R-L shunts) • Sagittal sinus thrombosis – Hypernatremia, dehydration
Ischemic Perinatal Stroke • Serious but under-recognized event – Occurring in 1/4000 live births • Definition: – Focal disruption of CBF secondary to arterial or cerebral venous thrombosis or embolization between 20 weeks of fetal life through the 28 th postnatal day – Confirmed by neuroimaging or neuropathology studies.
Ischemic Perinatal Stroke • 85% of IPS occurs in term gestation infants • Low mortality (3 -10%) • Low recurrence rates (3 -5%) • Etiology: – 83% of arterial strokes involve the MCA • • 2/3 involving the left MCA 10% bilateral MCA
Arterial or Venous Stroke • May have few overt signs of encephalopathy • Clues to diagnosis: – Focal, clonic seizures common – Often after 24 hrs – Commonly noted later as asymmetric strength, movement – Lesion contralateral to affected side – Cause of hemiplegic cerebral palsy • Upper extremity, face
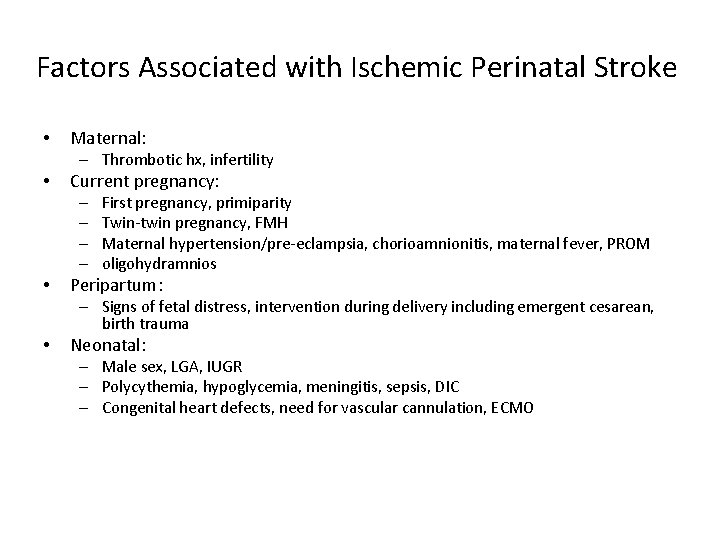
Factors Associated with Ischemic Perinatal Stroke • Maternal: – Thrombotic hx, infertility • Current pregnancy: – – • First pregnancy, primiparity Twin-twin pregnancy, FMH Maternal hypertension/pre-eclampsia, chorioamnionitis, maternal fever, PROM oligohydramnios Peripartum: – Signs of fetal distress, intervention during delivery including emergent cesarean, birth trauma • Neonatal: – Male sex, LGA, IUGR – Polycythemia, hypoglycemia, meningitis, sepsis, DIC – Congenital heart defects, need for vascular cannulation, ECMO
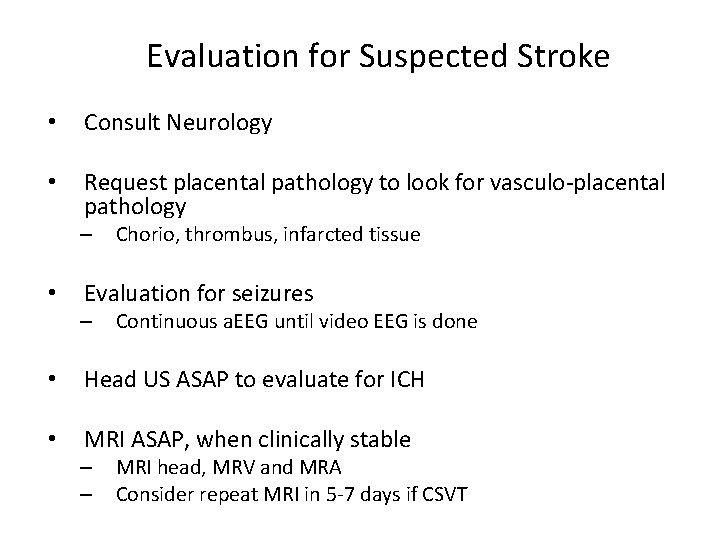
Evaluation for Suspected Stroke • Consult Neurology • Request placental pathology to look for vasculo-placental pathology – • Chorio, thrombus, infarcted tissue Evaluation for seizures – Continuous a. EEG until video EEG is done • Head US ASAP to evaluate for ICH • MRI ASAP, when clinically stable – – MRI head, MRV and MRA Consider repeat MRI in 5 -7 days if CSVT
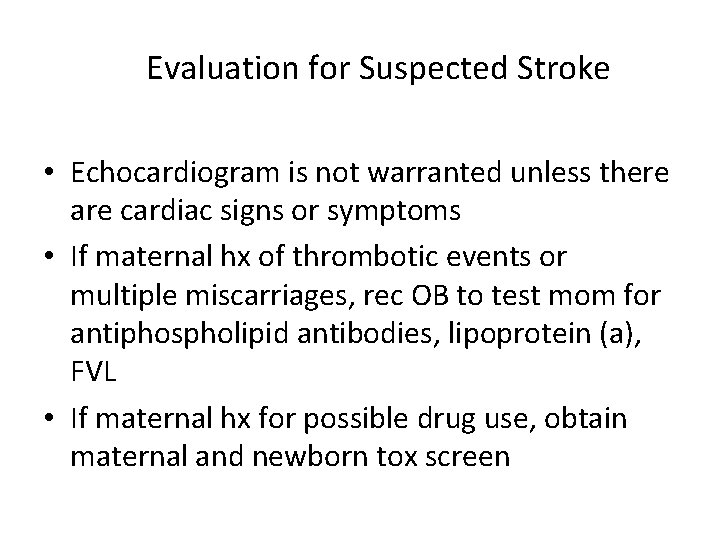
Evaluation for Suspected Stroke • Echocardiogram is not warranted unless there are cardiac signs or symptoms • If maternal hx of thrombotic events or multiple miscarriages, rec OB to test mom for antiphospholipid antibodies, lipoprotein (a), FVL • If maternal hx for possible drug use, obtain maternal and newborn tox screen
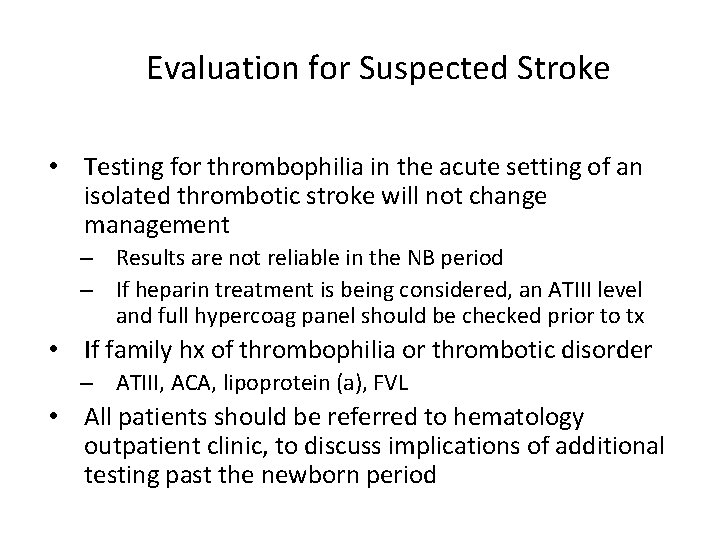
Evaluation for Suspected Stroke • Testing for thrombophilia in the acute setting of an isolated thrombotic stroke will not change management – Results are not reliable in the NB period – If heparin treatment is being considered, an ATIII level and full hypercoag panel should be checked prior to tx • If family hx of thrombophilia or thrombotic disorder – ATIII, ACA, lipoprotein (a), FVL • All patients should be referred to hematology outpatient clinic, to discuss implications of additional testing past the newborn period
Stroke Management • • Avoid dehydration Blood pressure/perfusion – – • Glucose – • Maintain goal Sp. O 2 (89 -94%) Ventilation – • Avoid hyperthermia, aim 36 -37 degrees temp Oxygenation – • Maintain normal serum glucose Temperature – • Maintain cardiac output and normal BP Treat with volume/inotropes/pressors as needed Avoid hyperventilation Treat seizures with anticonvulsant – Phenobarbital, fosphenytoin, keppra
Stroke Management • • In most cases anticoagulation is not indicated Anticoagulation may be considered with progressive ischemic infarction or: – – – • Relative contraindications for anticoagulation: – – – • • Clinical or radiological evidence of propagating CSVT despite supportive therapy Intracardiac or intravascular thrombus considered at risk for embolization Severe thrombophilic disorders Hemorrhagic transformation of the infarct MCA infarct >50% of territory Large cerebellar infarct Consult hematology if considering anticoagulation Check ATIII, coags, and d-dimers prior to starting heparin
Stroke Follow-Up • • Neurology at age 3 months Hematology within the first year High Risk Infant Follow up Refer to local Regional Center or CCS MTU
Stroke Outcome • Remarkably good outcome in many infants with IPS – • Cortical and subcortical plasticity and functional recovery Adverse outcome – – Hemiplegic CP (approx 30%) Visual Impairments (less than 1/3) • – – – • unusual in the absence of hemiplegia Cognitive deficits (approx 15 -25%) Behavioral problems (approx 10 -25%) Recurrence of seizure (approx 25 -50%) Predicting outcome – – If seizures, outcome seems to be worse Background normalization of EEG is good
Intracranial Hemorrhage
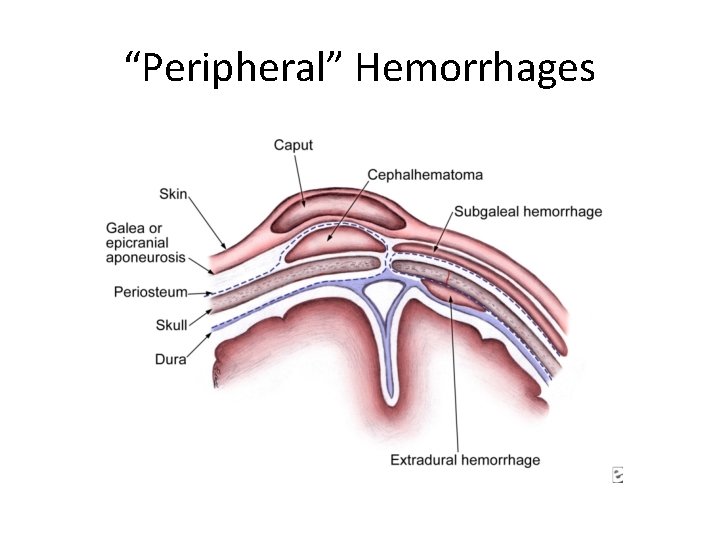
Hemorrhage • “Outside” – Sub-galeal – above periosteum – Cephalohematoma – below periosteum • Extra-axial – Epidural – Sub-arachnoid • Germinal Matrix & Intraventricular – Grade 1 -4
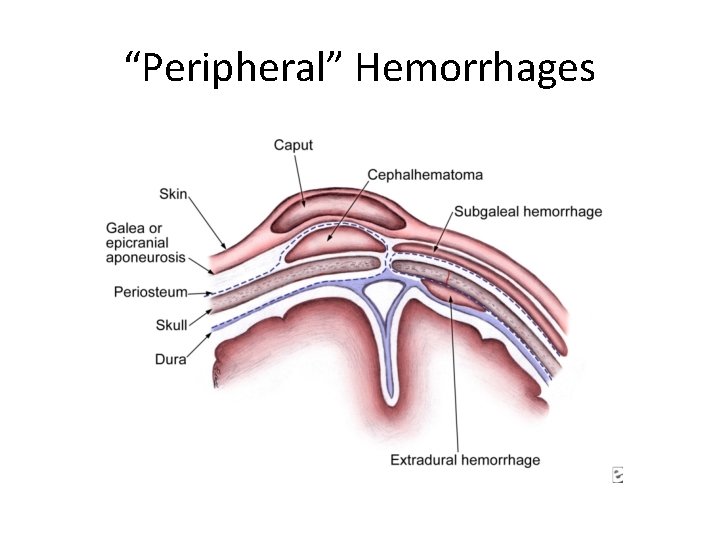
“Peripheral” Hemorrhages
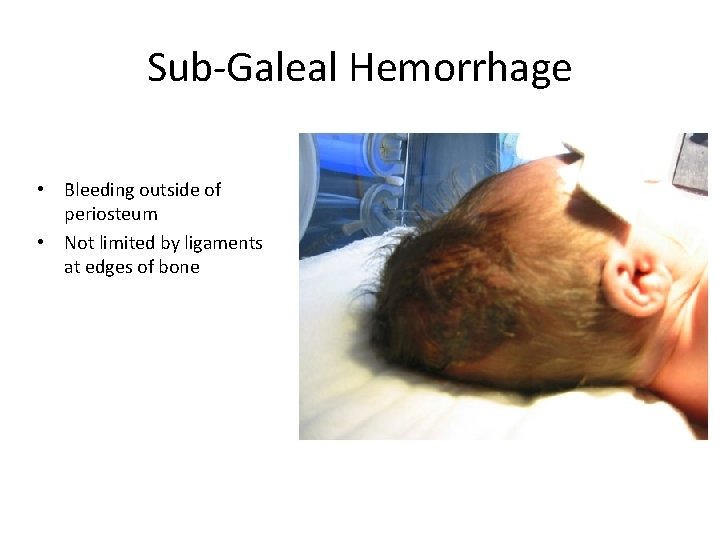
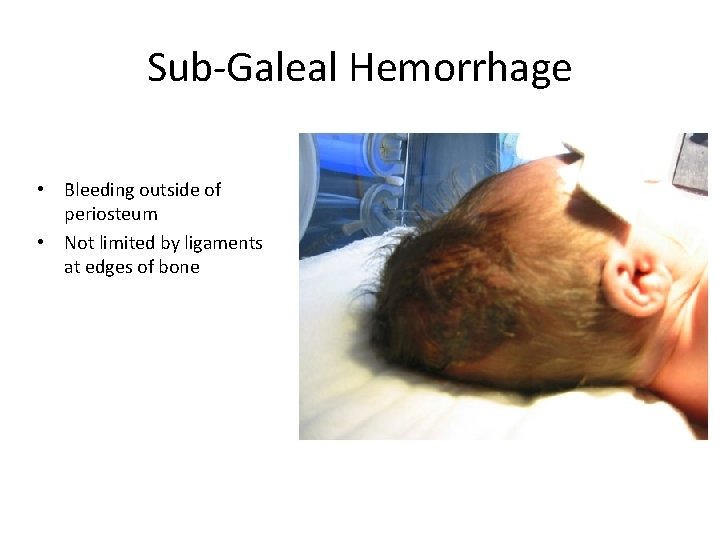
Sub-Galeal Hemorrhage • Bleeding outside of periosteum • Not limited by ligaments at edges of bone
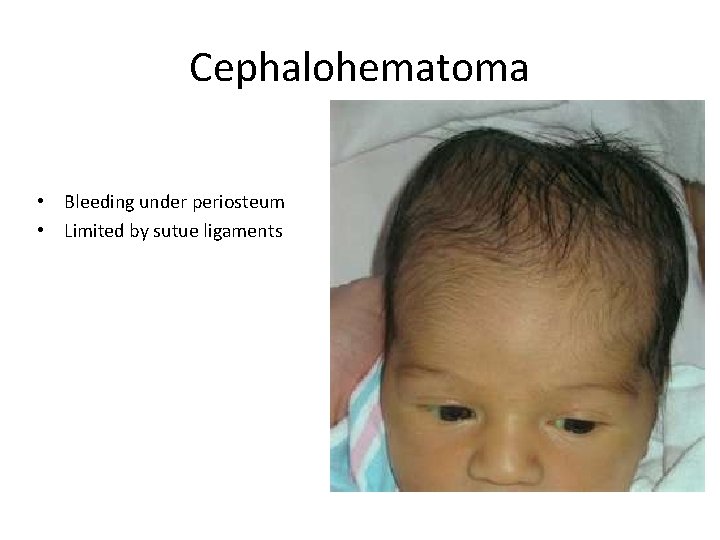
Cephalohematoma • Bleeding under periosteum • Limited by sutue ligaments
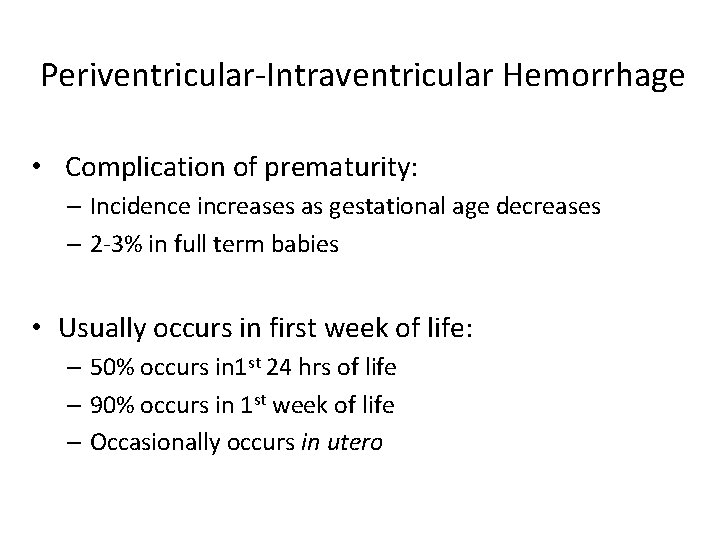
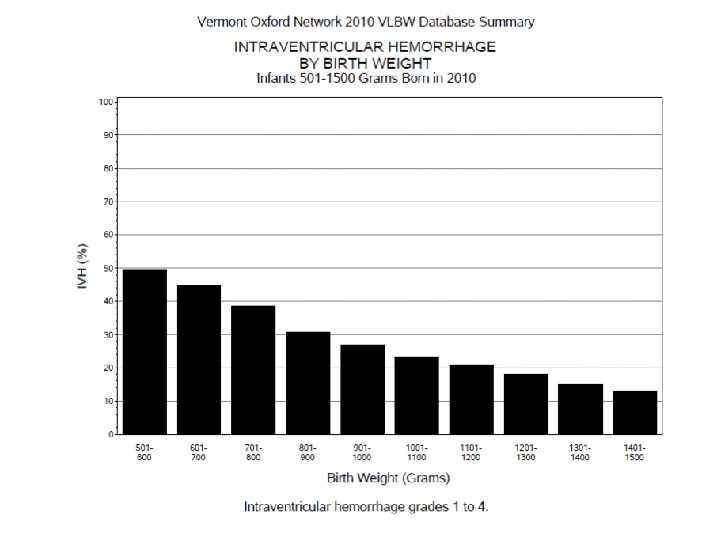
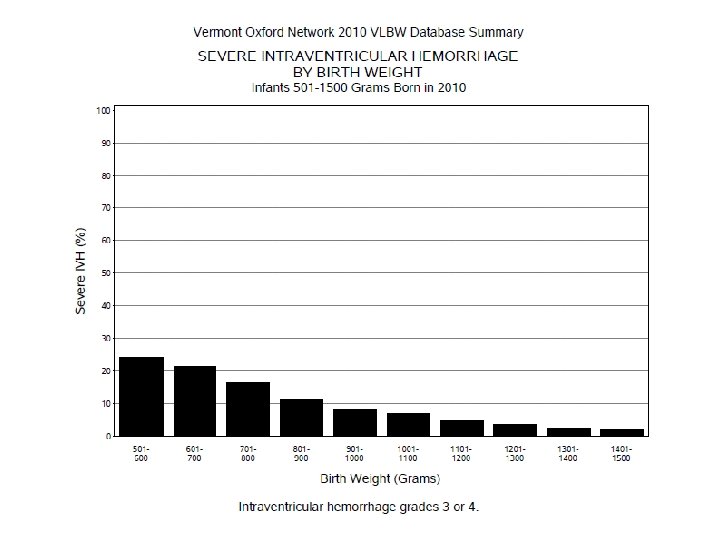
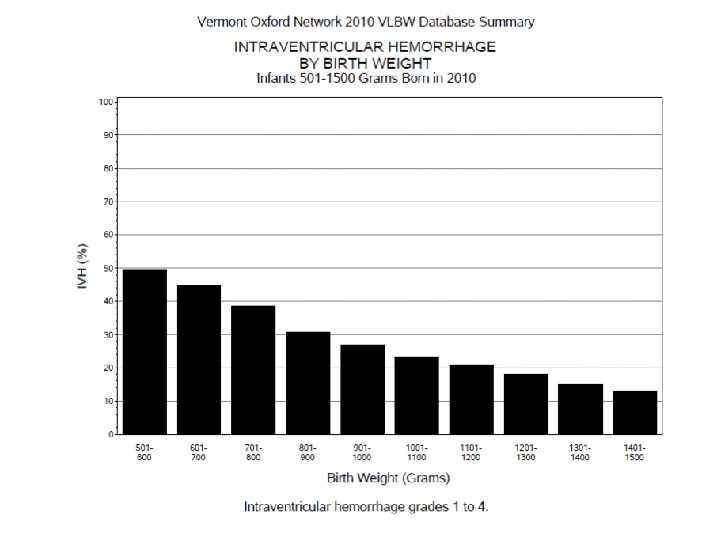
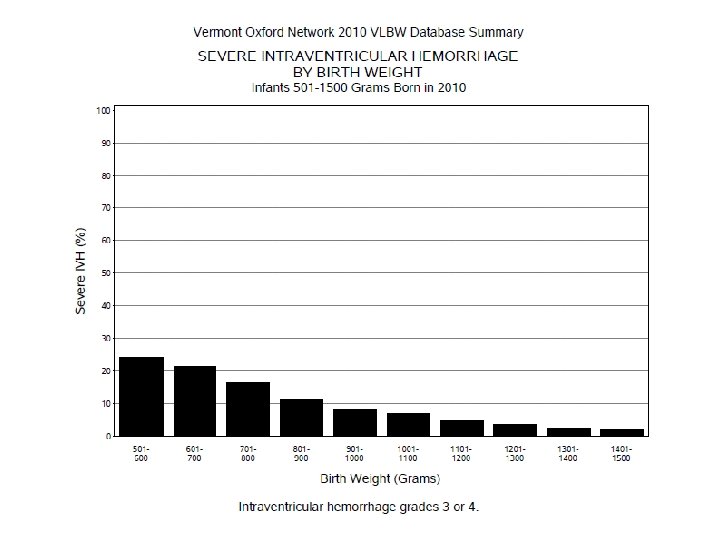
Periventricular-Intraventricular Hemorrhage • Complication of prematurity: – Incidence increases as gestational age decreases – 2 -3% in full term babies • Usually occurs in first week of life: – 50% occurs in 1 st 24 hrs of life – 90% occurs in 1 st week of life – Occasionally occurs in utero
Risk for IVH • Increases risk: – Low gestation – Rapid changes in BP – Rapid changes in intra-thoracic pressure • Decreases risk: – Prenatal steroids – Indomethacin – Delayed cord clamping
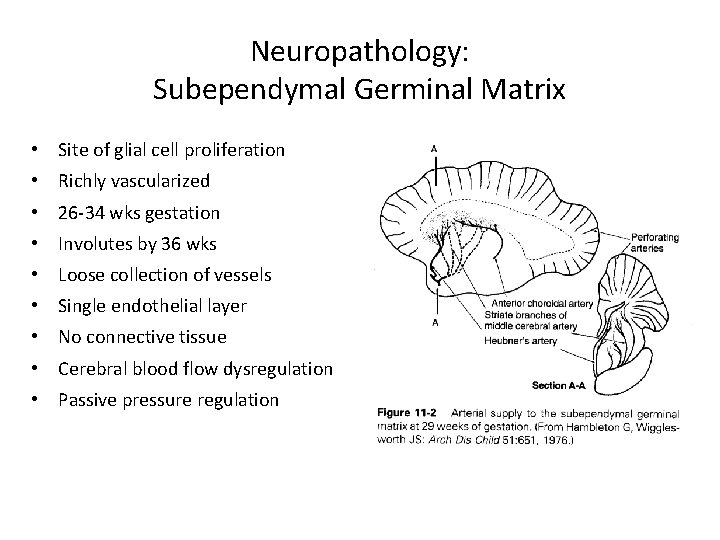
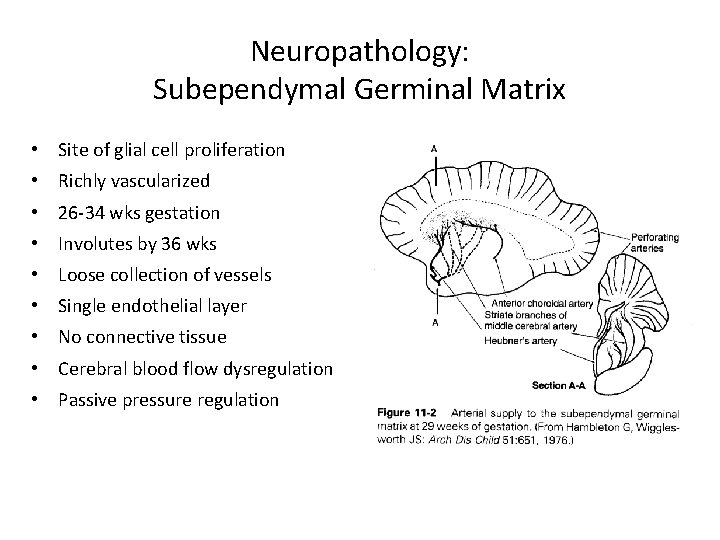
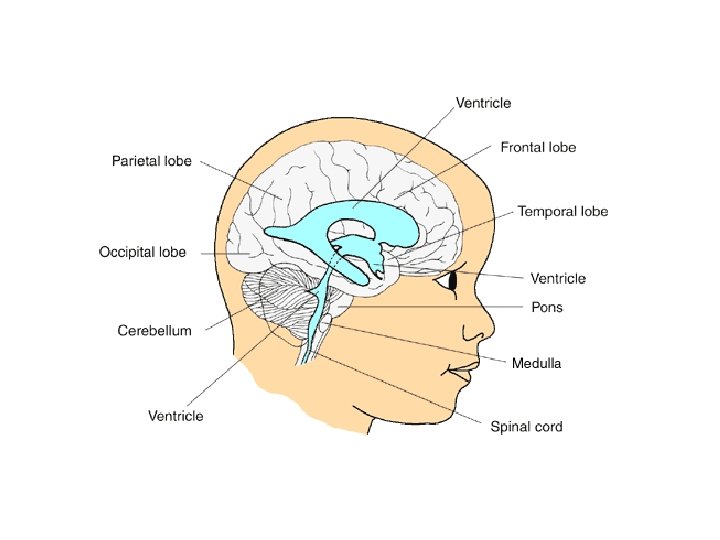
Neuropathology: Subependymal Germinal Matrix • Site of glial cell proliferation • Richly vascularized • 26 -34 wks gestation • Involutes by 36 wks • Loose collection of vessels • Single endothelial layer • No connective tissue • Cerebral blood flow dysregulation • Passive pressure regulation
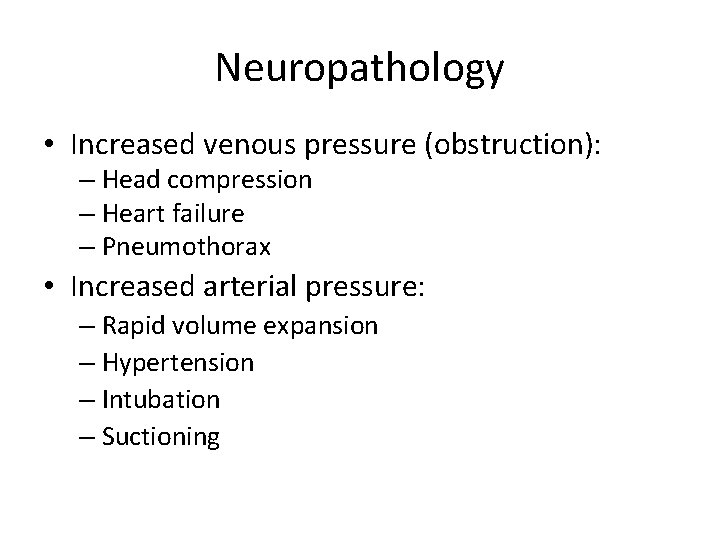
Neuropathology • Increased venous pressure (obstruction): – Head compression – Heart failure – Pneumothorax • Increased arterial pressure: – Rapid volume expansion – Hypertension – Intubation – Suctioning
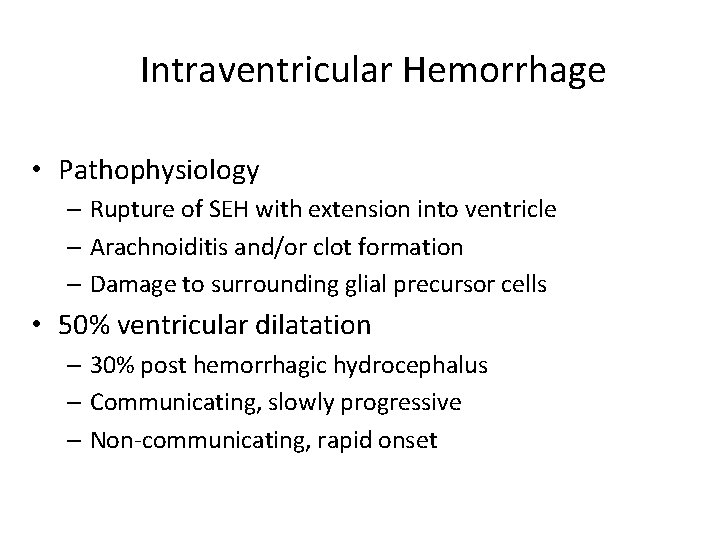
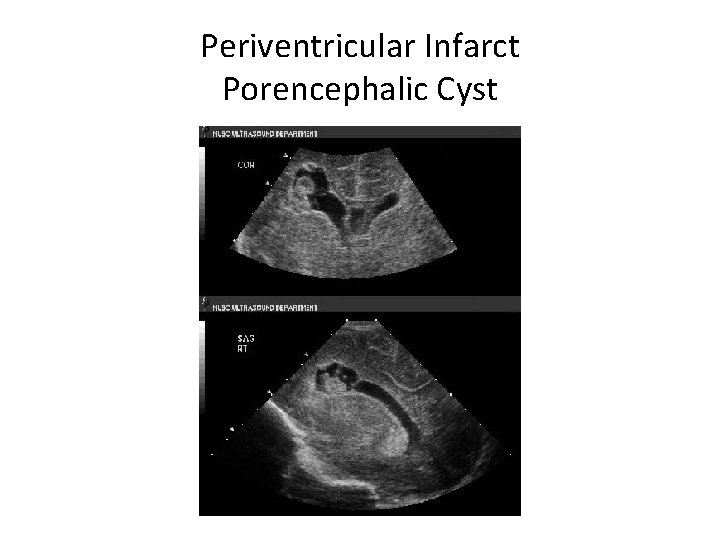
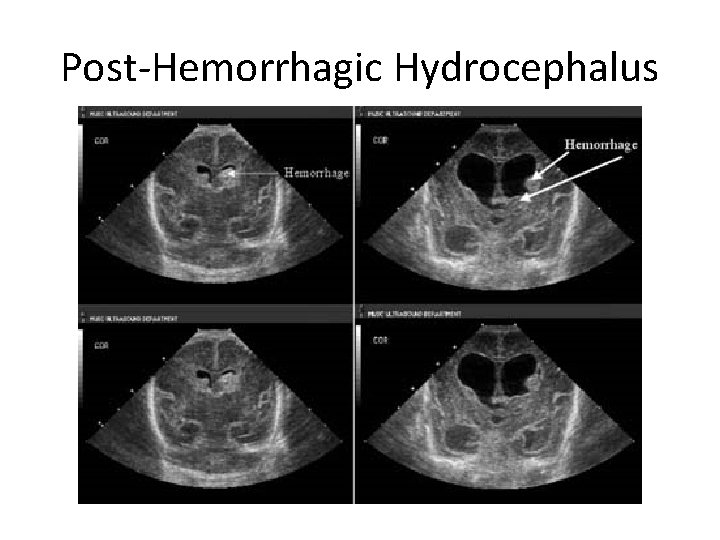
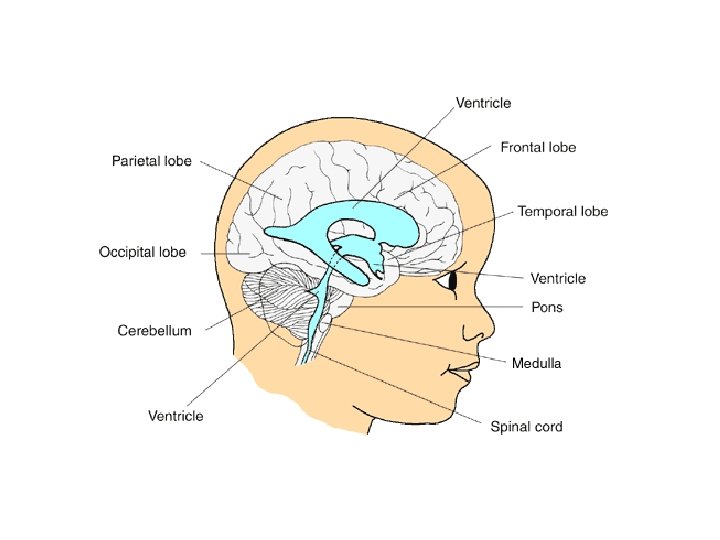
Intraventricular Hemorrhage • Pathophysiology – Rupture of SEH with extension into ventricle – Arachnoiditis and/or clot formation – Damage to surrounding glial precursor cells • 50% ventricular dilatation – 30% post hemorrhagic hydrocephalus – Communicating, slowly progressive – Non-communicating, rapid onset
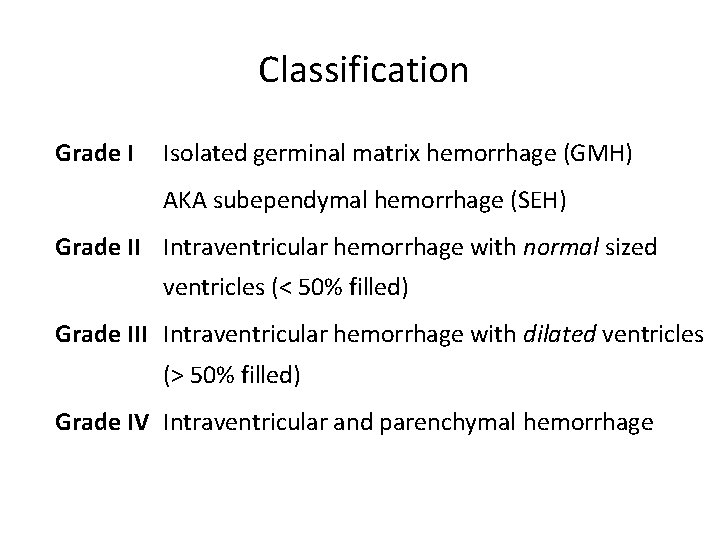
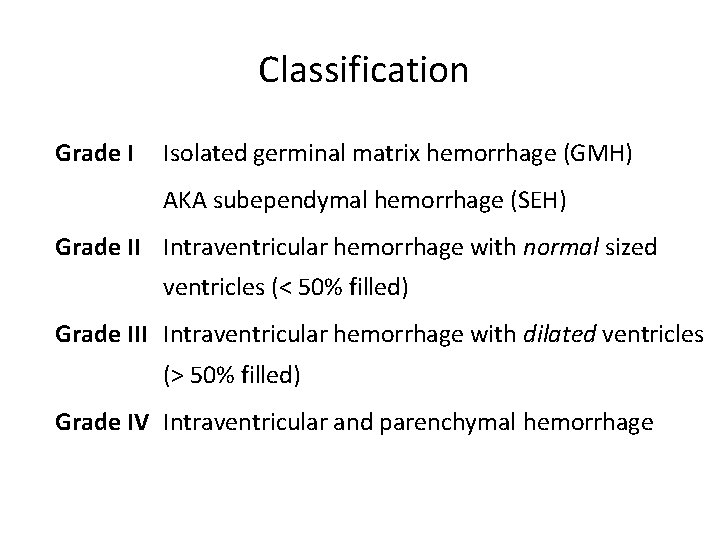
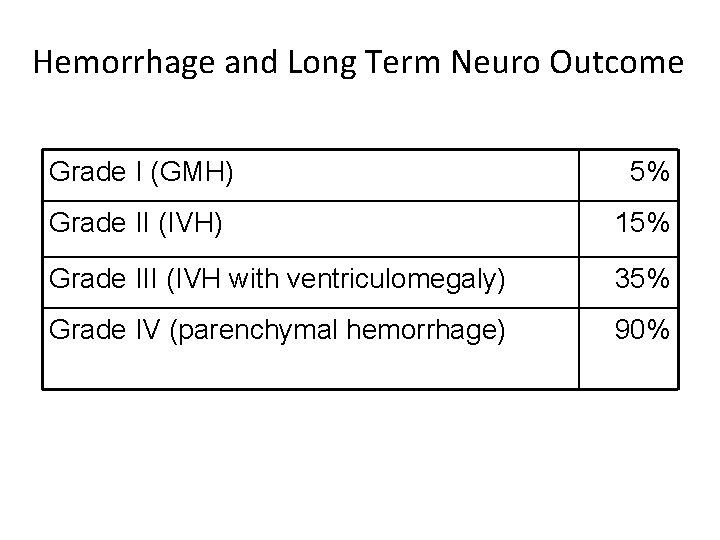
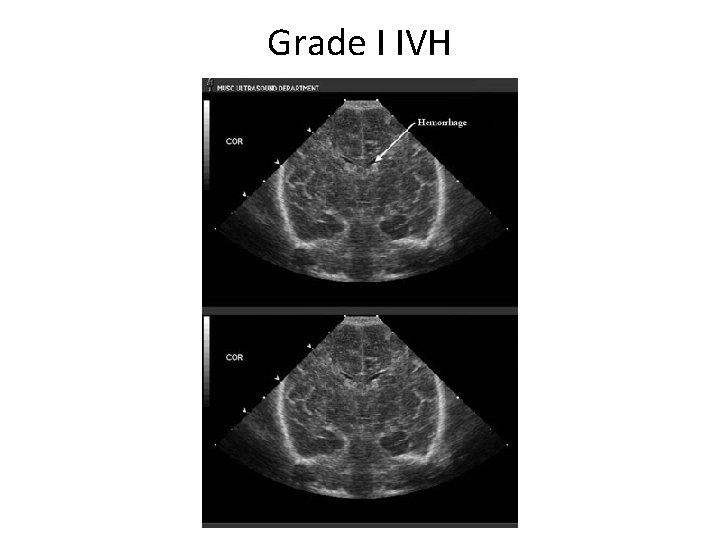
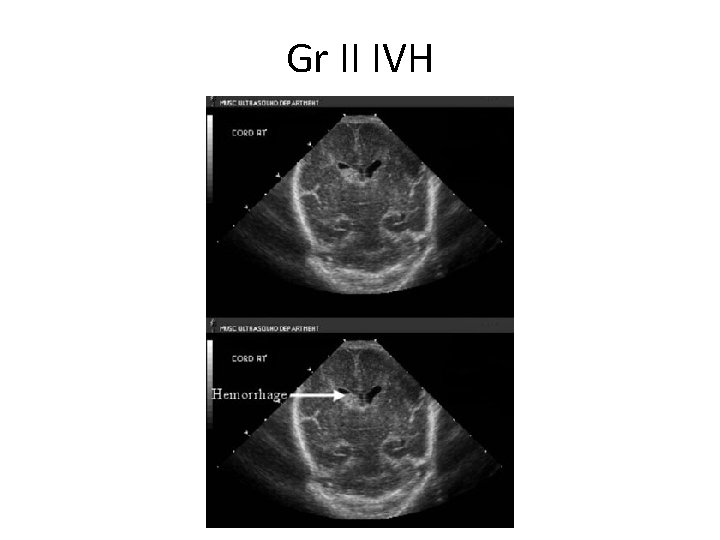
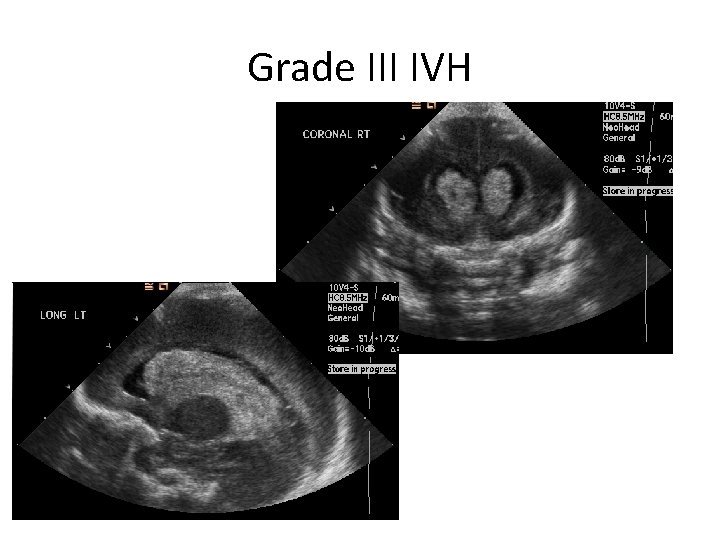
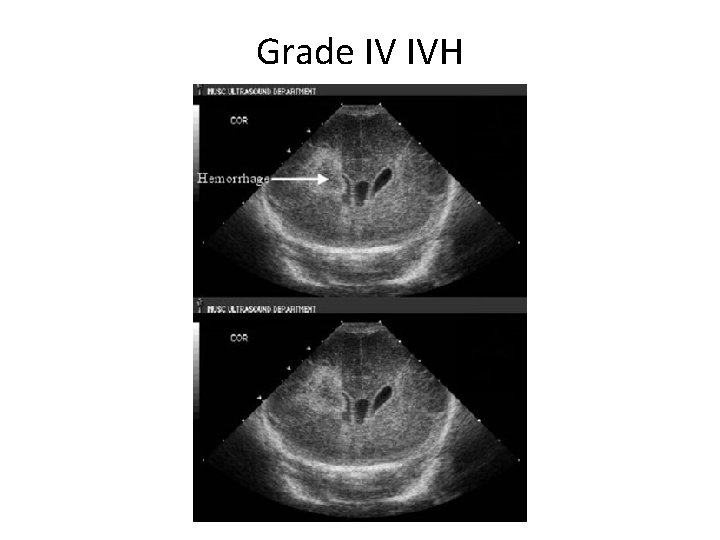
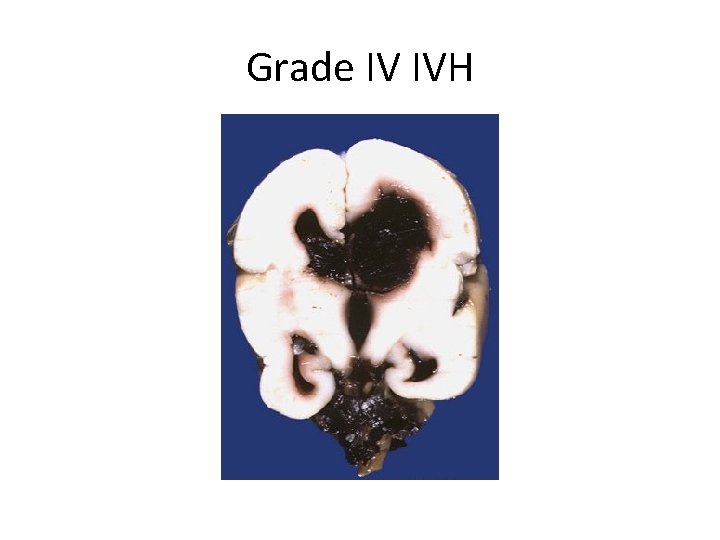
Classification Grade I Isolated germinal matrix hemorrhage (GMH) AKA subependymal hemorrhage (SEH) Grade II Intraventricular hemorrhage with normal sized ventricles (< 50% filled) Grade III Intraventricular hemorrhage with dilated ventricles (> 50% filled) Grade IV Intraventricular and parenchymal hemorrhage
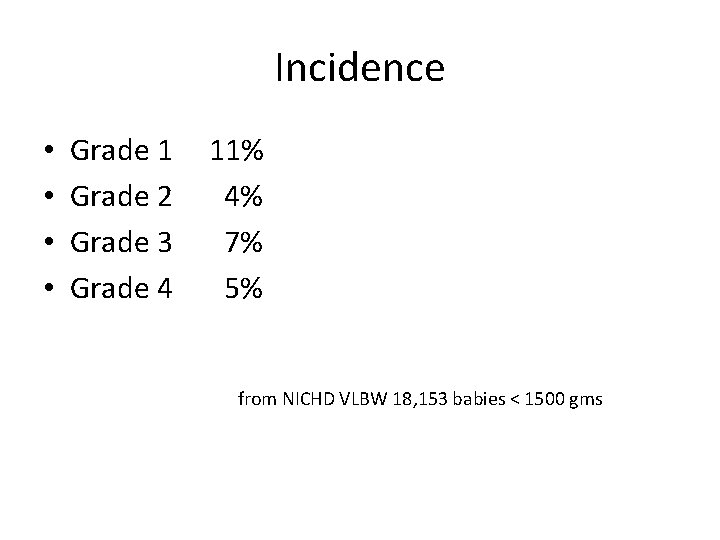
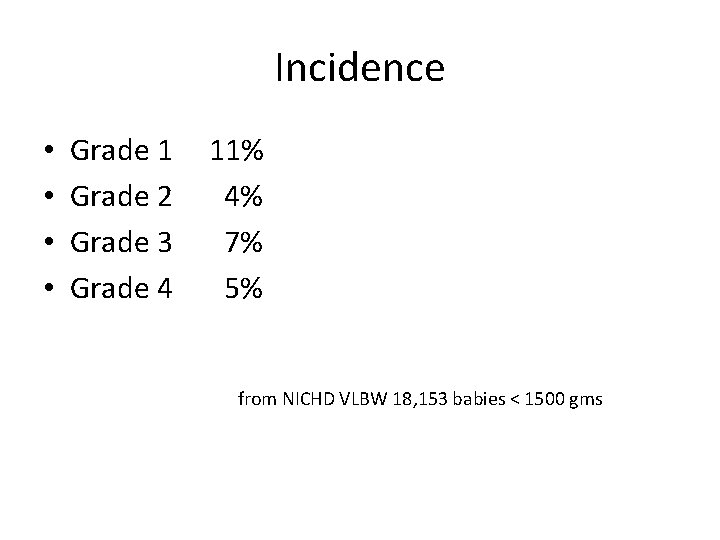
Incidence • • Grade 1 Grade 2 Grade 3 Grade 4 11% 4% 7% 5% from NICHD VLBW 18, 153 babies < 1500 gms
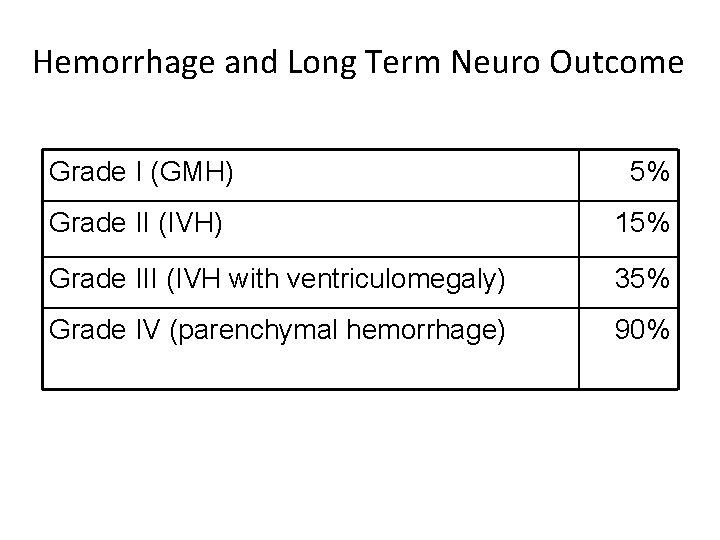
Hemorrhage and Long Term Neuro Outcome Grade I (GMH) 5% Grade II (IVH) 15% Grade III (IVH with ventriculomegaly) 35% Grade IV (parenchymal hemorrhage) 90%
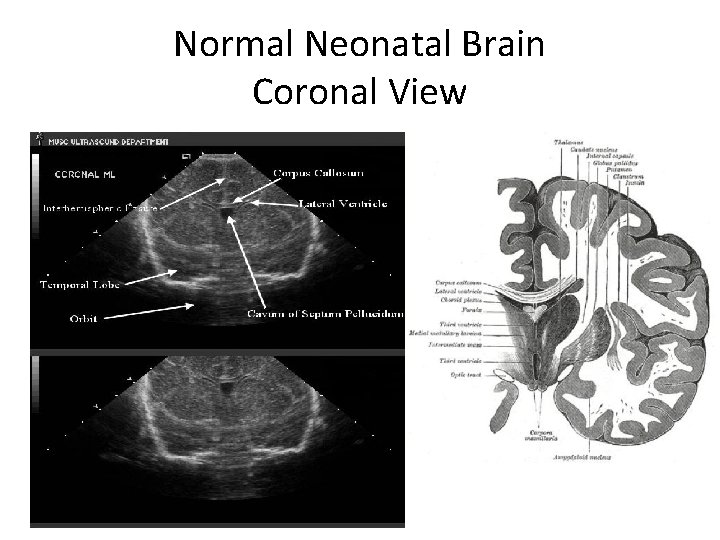
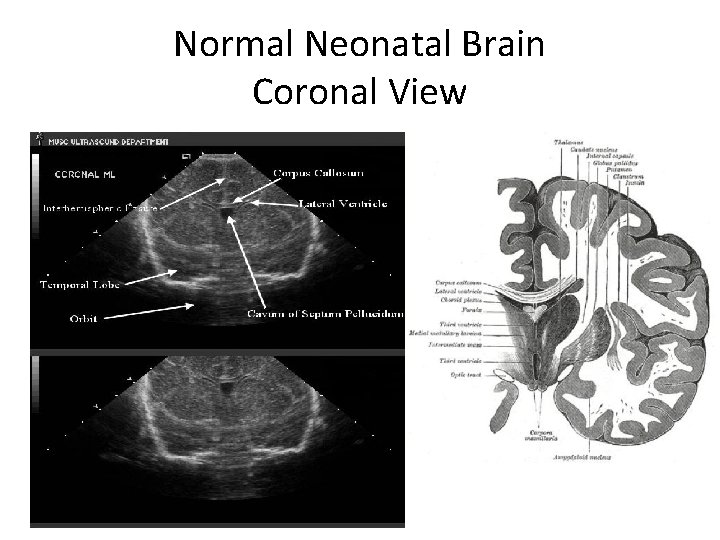
Normal Neonatal Brain Coronal View
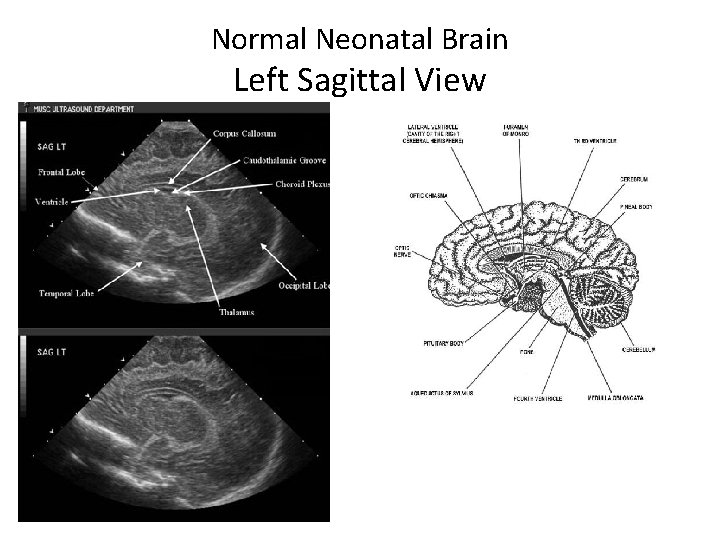
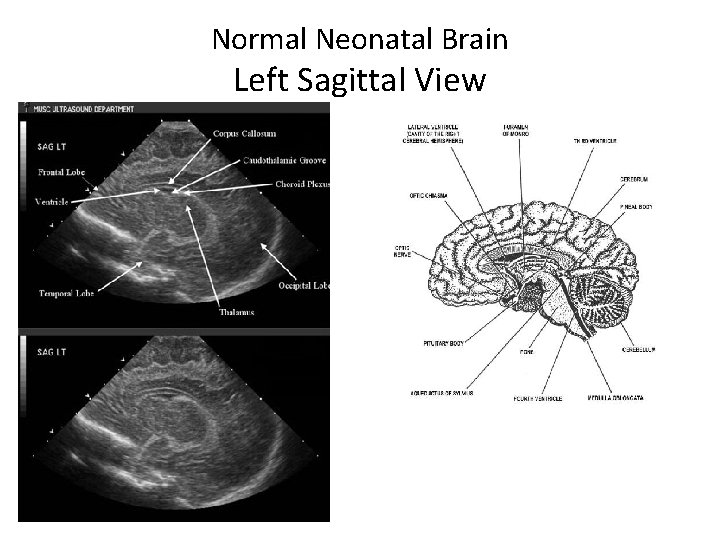
Normal Neonatal Brain Left Sagittal View
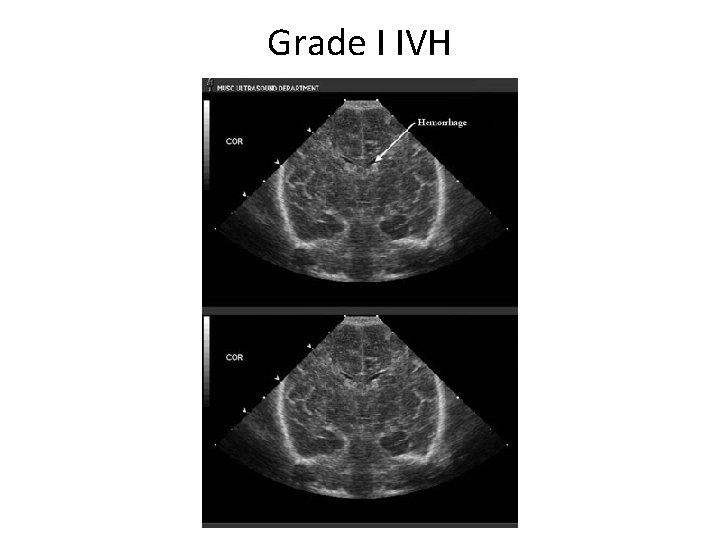
Grade I IVH
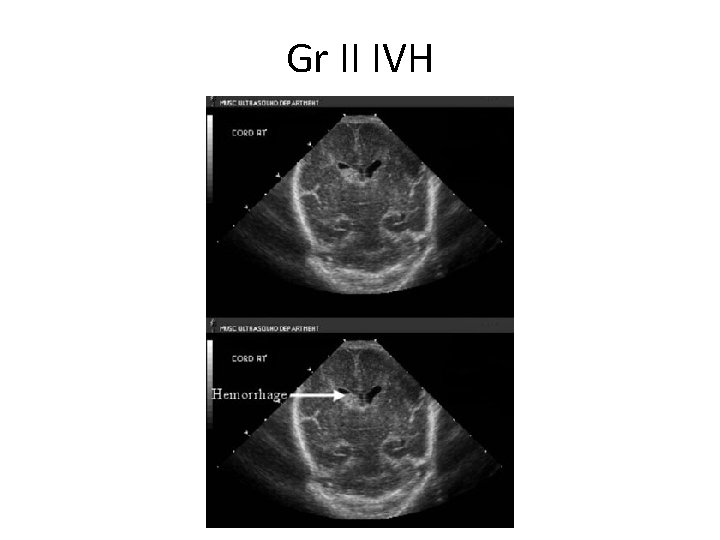
Gr II IVH
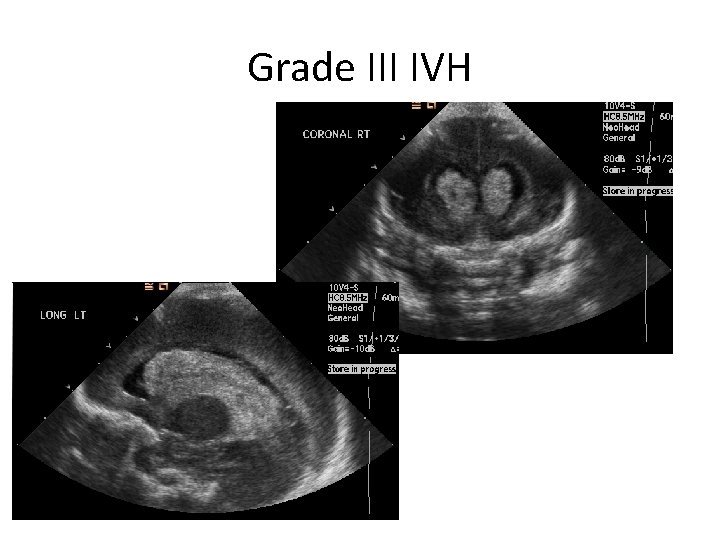
Grade III IVH
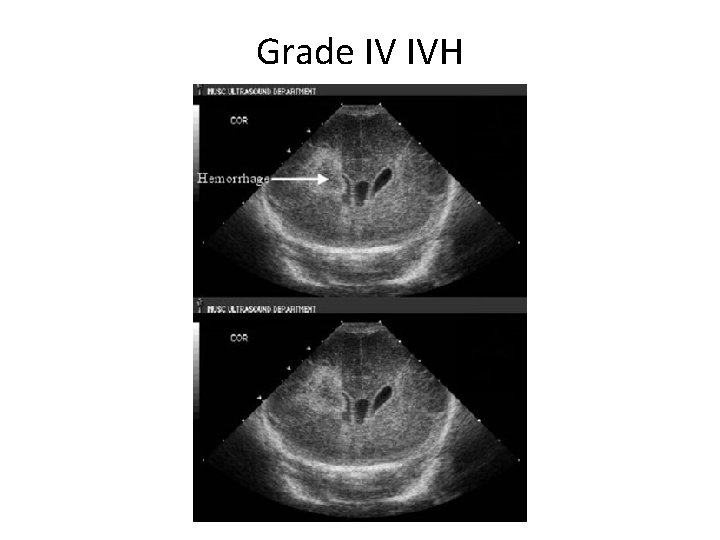
Grade IV IVH
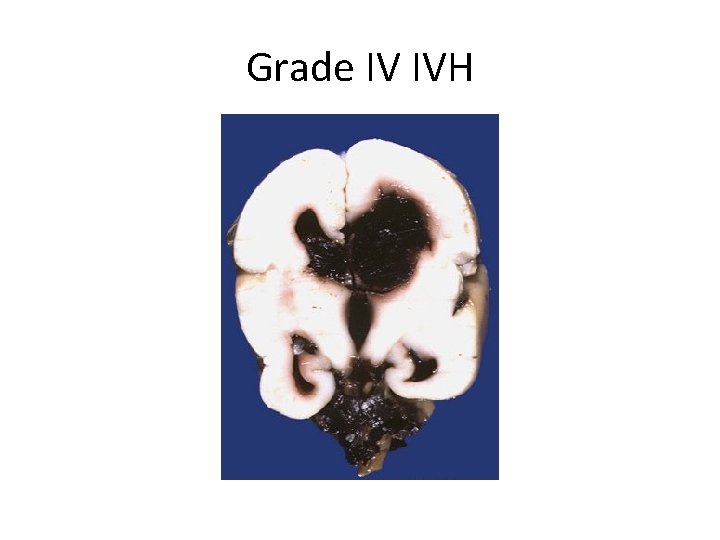
Grade IV IVH
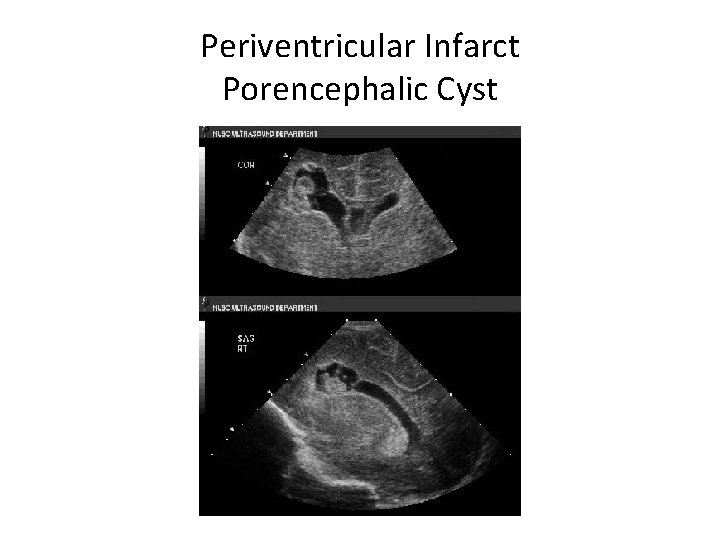
Periventricular Infarct Porencephalic Cyst
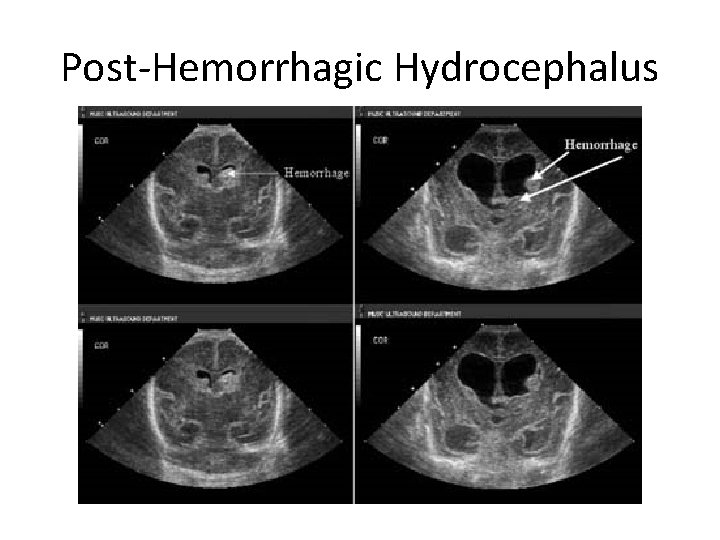
Post-Hemorrhagic Hydrocephalus
Post-Hemorrhagic Hydrocephalus • Occurs in 35% of babies with IVH • Communicating, slowly progressive – – Secondary to decreased CSF absorption by arachnoid villi Spontaneous resolution by 4 wks (65%) Slow progression for 1 st 4 wks, followed by arrest after 4 wks (20%) Progression after 4 wks (10%) • Non-communicating, rapidly evolving – Rapid progression during initial 4 wks (5%)
Rx of Post-Hemorrhagic Hydrocephalus • Medical Rx – not proven to be effective – Serial LPs – effective in old studies – Acetazolamide – not proven to be effective – Diuretics – not proven to be effective • Surgical Rx – Subcutaneous reservoir – External ventricular drain (rarely used) – VP shunt
Periventricular Leukomalacia
Periventricular Leukomalacia • Cystic lesions in the periventricular white matter • 4% of VLBW babies • Detected later in neonatal period • Probably related to: – Severe hypoxic, ischemic, or inflammatory events – in utero or neonatal • Risk factors: – – – Twins IUGR Cocaine Chorioamnionitis Hypocapnia!!!! (decreases CBF)
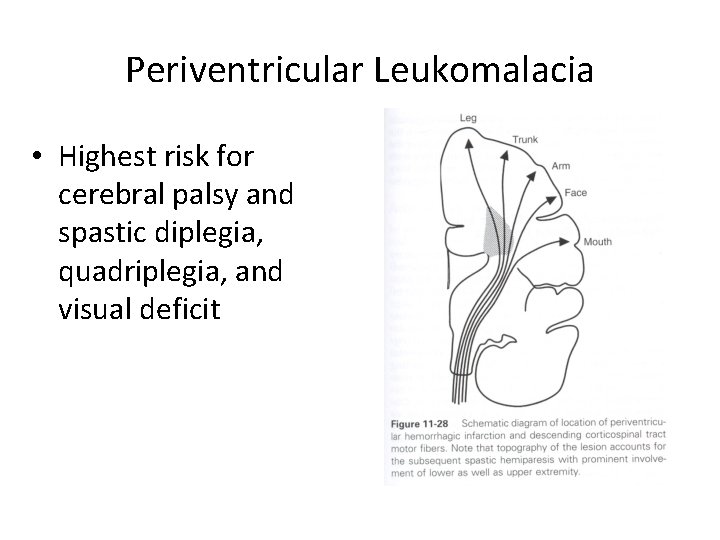
Periventricular Leukomalacia • Diffuse or focal • Bilateral and symmetric • Secondary hydrocephalus • Highest risk for later neurologic abnormalities
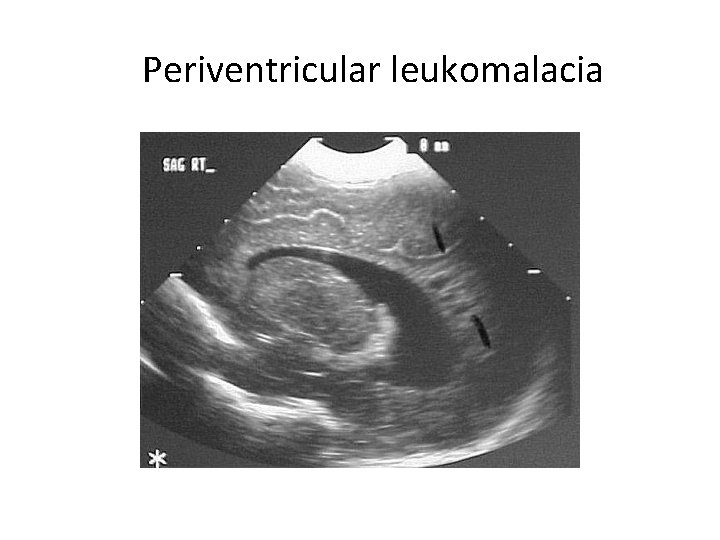
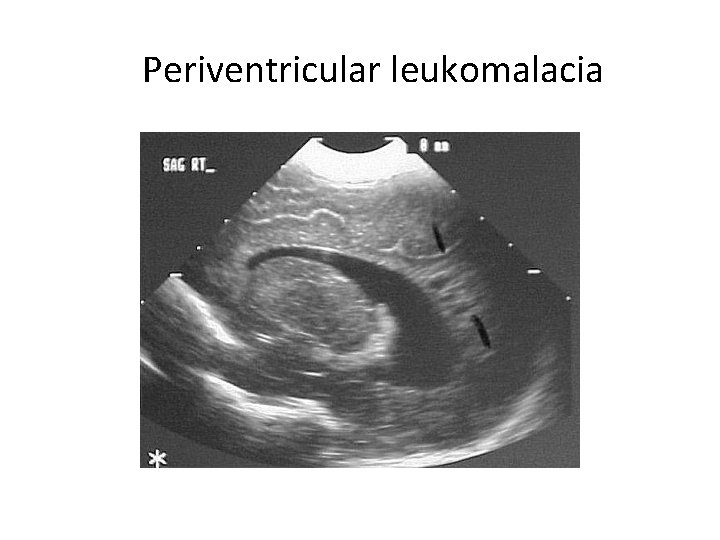
Periventricular leukomalacia
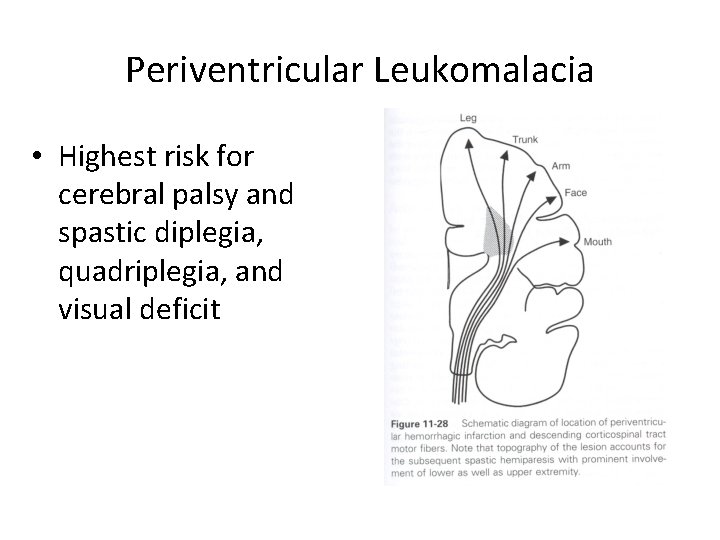
Periventricular Leukomalacia • Highest risk for cerebral palsy and spastic diplegia, quadriplegia, and visual deficit