Neonatal Jaundice Ruben Bromiker Department of Neonatology Shaare
Neonatal Jaundice Ruben Bromiker Department of Neonatology Shaare Zedek Medical Center
Physiologic Jaundice Healthy infants up to 12 mg% in 3 rd day; in premature, 5 th day. No hemolysis or bleedings No underlying metabolic disease
Mechanism Production: Volemia, RBC span (90 days) Ineffective erythropoyesis Turnover of non Hb heme proteins
Mechanism Enterohepatic recirculation: Glucuronidase Bilirubin monoglucuronide Intestinal bacteria Intestinal motility and stooling
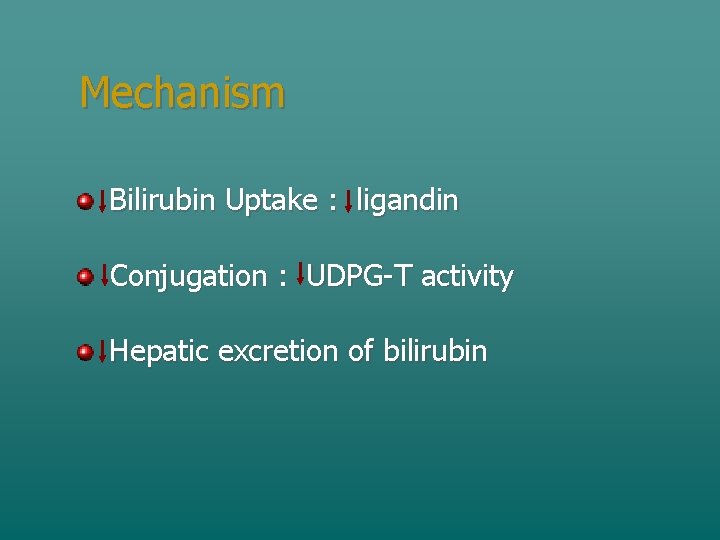
Mechanism Bilirubin Uptake : ligandin Conjugation : UDPG-T activity Hepatic excretion of bilirubin
Neonatal Hyperbilirubinemia Visible jaundice: Adults: >2 mg% Newborns: >6 mg Up to 50% of all newborns may develop jaundice
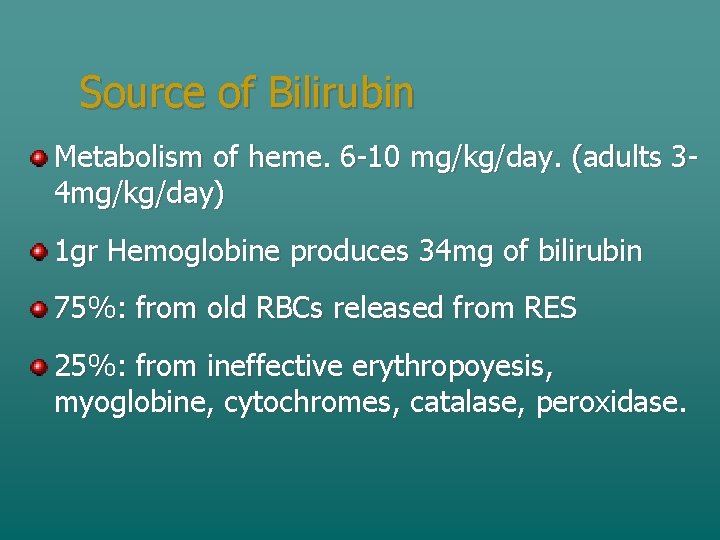
Source of Bilirubin Metabolism of heme. 6 -10 mg/kg/day. (adults 34 mg/kg/day) 1 gr Hemoglobine produces 34 mg of bilirubin 75%: from old RBCs released from RES 25%: from ineffective erythropoyesis, myoglobine, cytochromes, catalase, peroxidase.
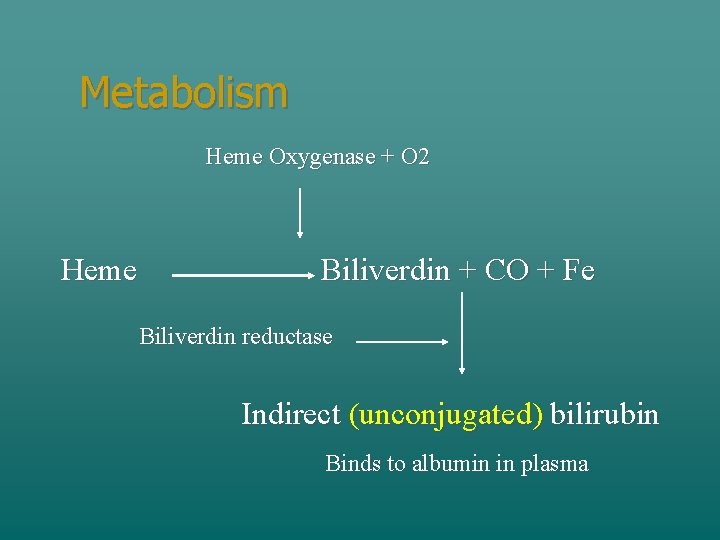
Metabolism Heme Oxygenase + O 2 Heme Biliverdin + CO + Fe Biliverdin reductase Indirect (unconjugated) bilirubin Binds to albumin in plasma
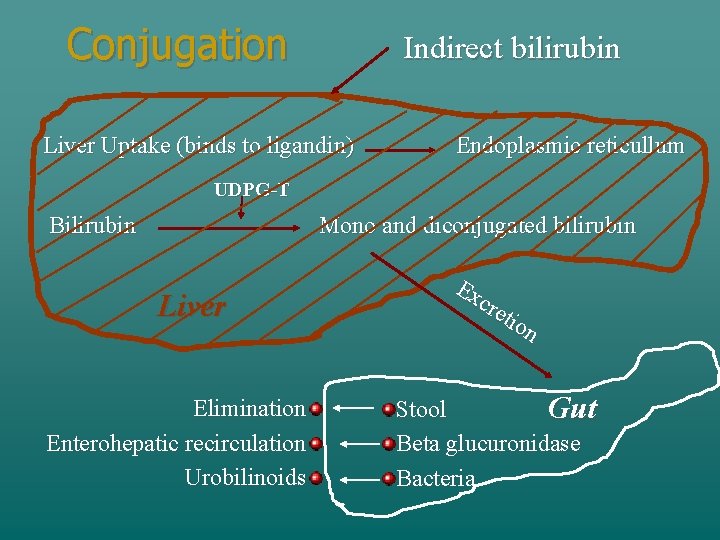
Conjugation Indirect bilirubin Liver Uptake (binds to ligandin) Endoplasmic reticullum UDPG-T Bilirubin Mono and diconjugated bilirubin Liver Elimination Enterohepatic recirculation Urobilinoids Ex cre tio n Stool Gut Beta glucuronidase Bacteria
Jaundice: Physical examination Blanch skin with a finger Jaundice Significant when appears at palms or below knees. Transcutaneous bilirubinometer Bruising, cephalohematoma, others. Organomegaly
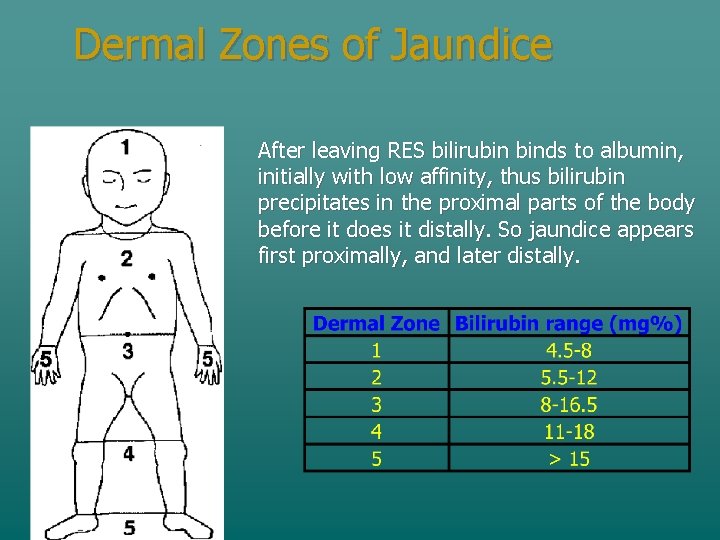
Dermal Zones of Jaundice After leaving RES bilirubin binds to albumin, initially with low affinity, thus bilirubin precipitates in the proximal parts of the body before it does it distally. So jaundice appears first proximally, and later distally.
Jaundice: Laboratory Total serum bilirubin Blood type, Rh, Coombs infant and mother Smear (morphology and reticulocytes) Hematocrit
Jaundice: Laboratory Antibody identification Direct bilirubin: When more than 2 weeks old or signs of cholestasis If prolonged: LFT, TORCH, sepsis work-up, metabolic, thyroid G 6 PD
Non Physiologic Jaundice Onset at < 24 hs Bilirubin over levels for phototherapy Bilirubin rise > 0. 5 mg%/hr Signs of underlying illness Vomiting, lethargy, poor feeding, weight Age > 8 days in term or 15 days in premature
Non Physiologic Jaundice: Anamnesis Familial: G 6 PD, spherocytosis, metabolic, enzymes. Siblings: Immune, breast milk. Pregnancy: Infections, drugs, diabetes. Delivery: Trauma, cord clumping, asphyxia.
Bilirubin toxicity: Cerebral Penetration: As free indirect bilirubin or bound when disrupted BBB Disrupted BB barrier Hyperosmolarity Anoxia Hypercarbia Prematurity
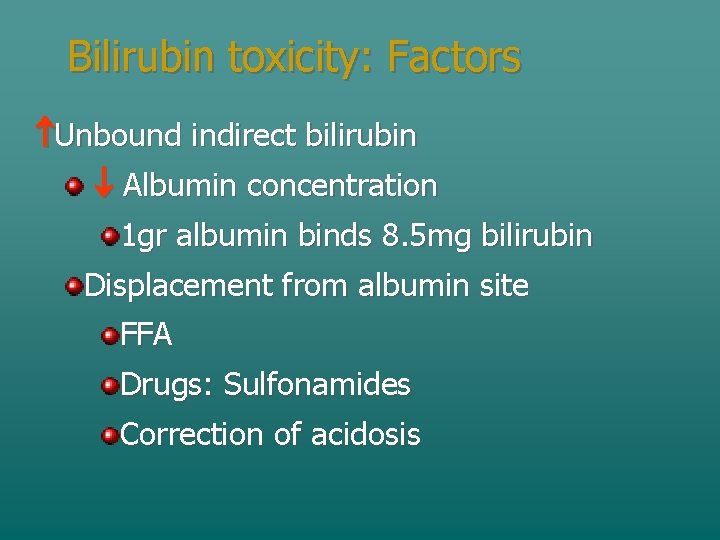
Bilirubin toxicity: Factors Unbound indirect bilirubin Albumin concentration 1 gr albumin binds 8. 5 mg bilirubin Displacement from albumin site FFA Drugs: Sulfonamides Correction of acidosis
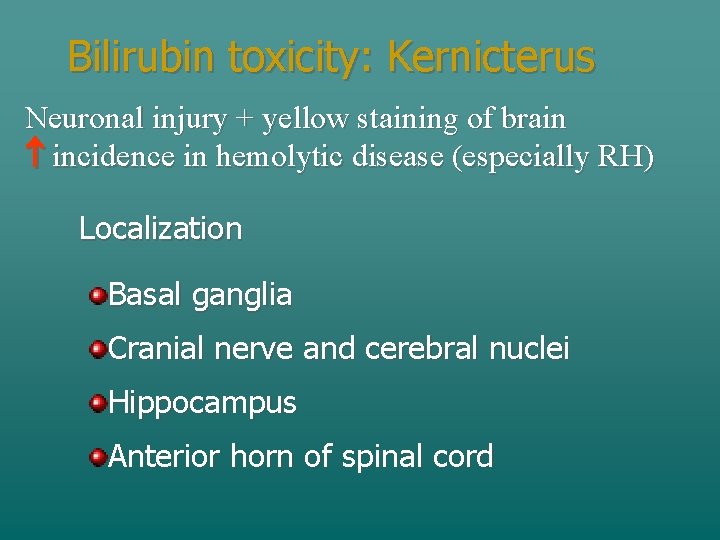
Bilirubin toxicity: Kernicterus Neuronal injury + yellow staining of brain incidence in hemolytic disease (especially RH) Localization Basal ganglia Cranial nerve and cerebral nuclei Hippocampus Anterior horn of spinal cord
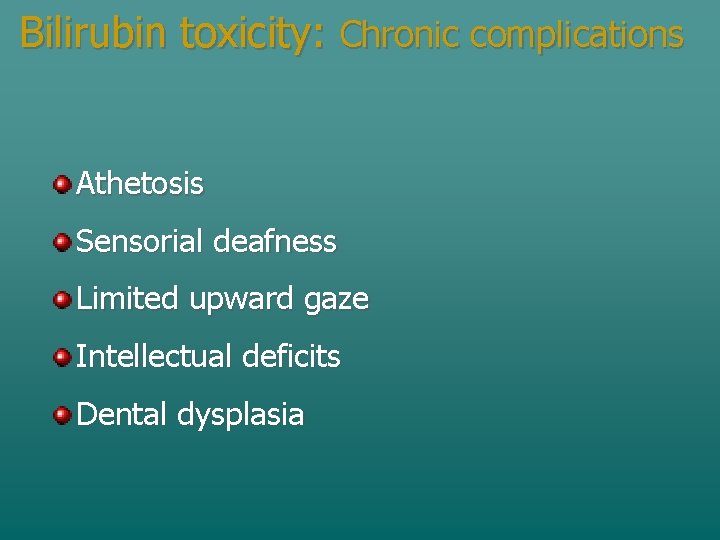
Bilirubin toxicity: Chronic complications Athetosis Sensorial deafness Limited upward gaze Intellectual deficits Dental dysplasia
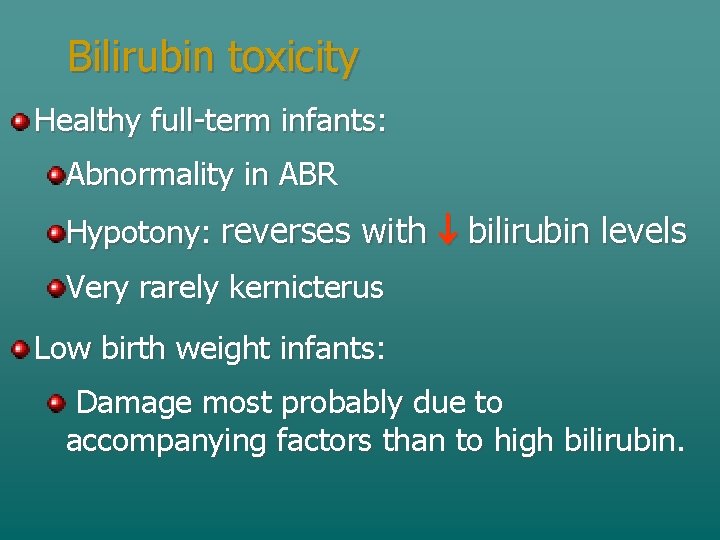
Bilirubin toxicity Healthy full-term infants: Abnormality in ABR Hypotony: reverses with bilirubin levels Very rarely kernicterus Low birth weight infants: Damage most probably due to accompanying factors than to high bilirubin.
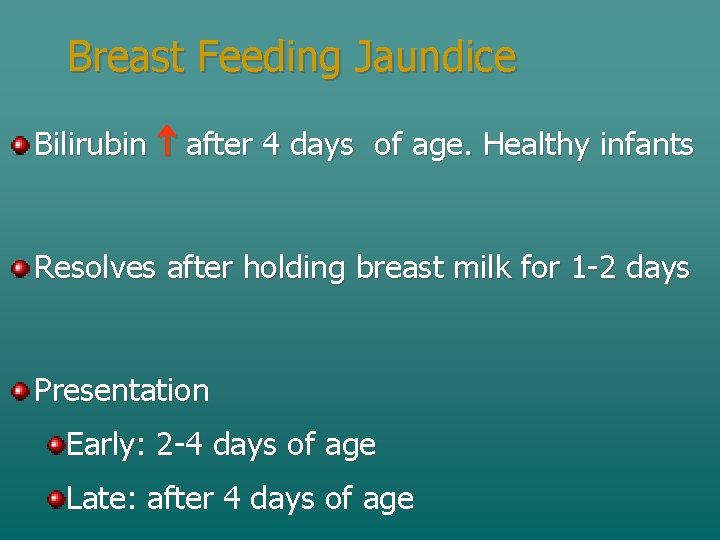
Breast Feeding Jaundice Bilirubin after 4 days of age. Healthy infants Resolves after holding breast milk for 1 -2 days Presentation Early: 2 -4 days of age Late: after 4 days of age
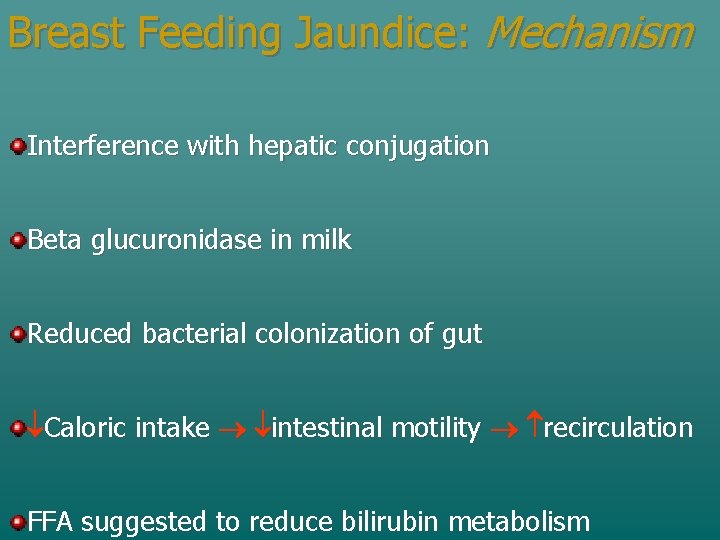
Breast Feeding Jaundice: Mechanism Interference with hepatic conjugation Beta glucuronidase in milk Reduced bacterial colonization of gut Caloric intake intestinal motility recirculation FFA suggested to reduce bilirubin metabolism
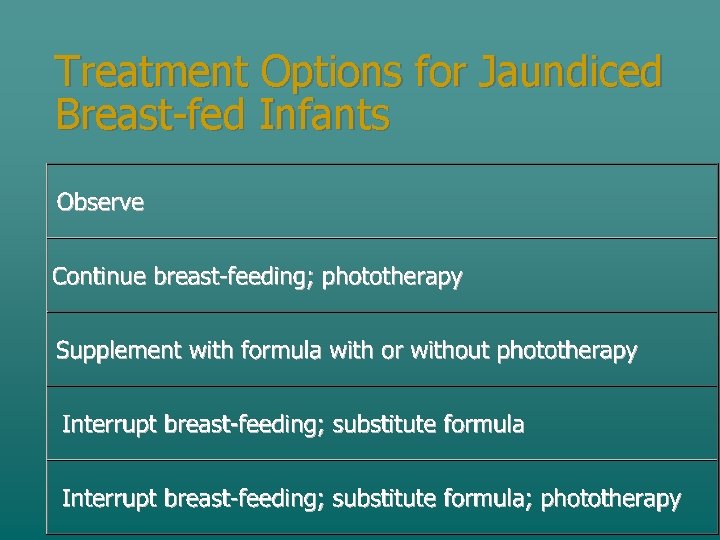
Treatment Options for Jaundiced Breast-fed Infants
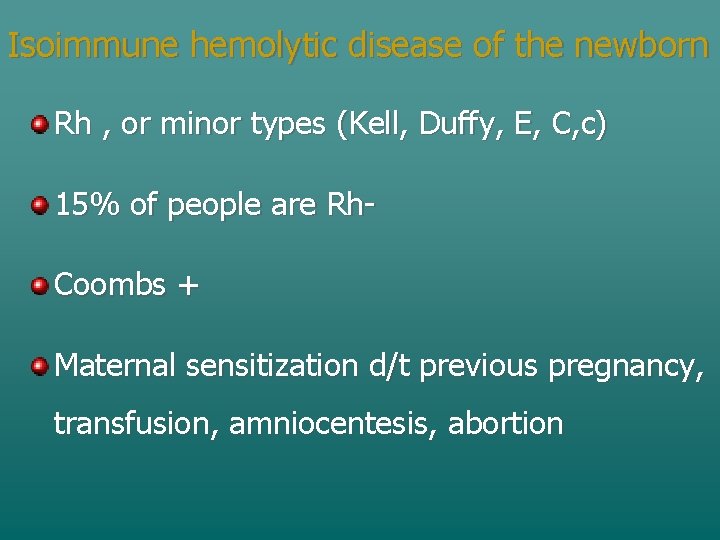
Isoimmune hemolytic disease of the newborn Rh , or minor types (Kell, Duffy, E, C, c) 15% of people are Rh. Coombs + Maternal sensitization d/t previous pregnancy, transfusion, amniocentesis, abortion
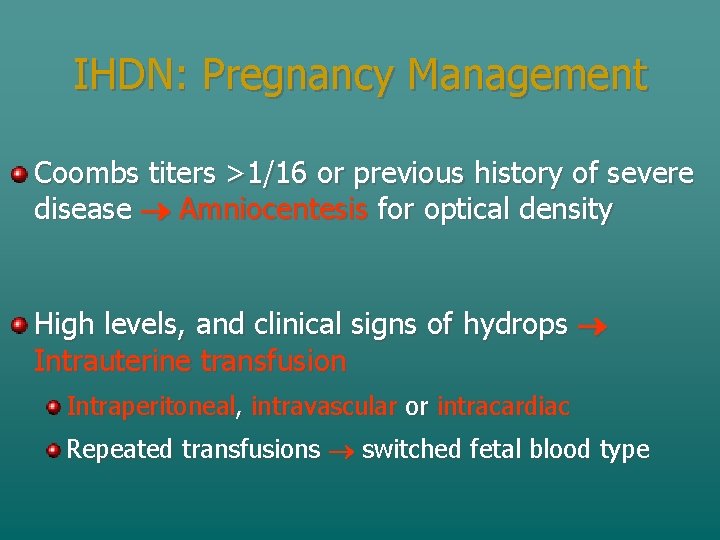
IHDN: Pregnancy Management Coombs titers >1/16 or previous history of severe disease Amniocentesis for optical density High levels, and clinical signs of hydrops Intrauterine transfusion Intraperitoneal, intravascular or intracardiac Repeated transfusions switched fetal blood type
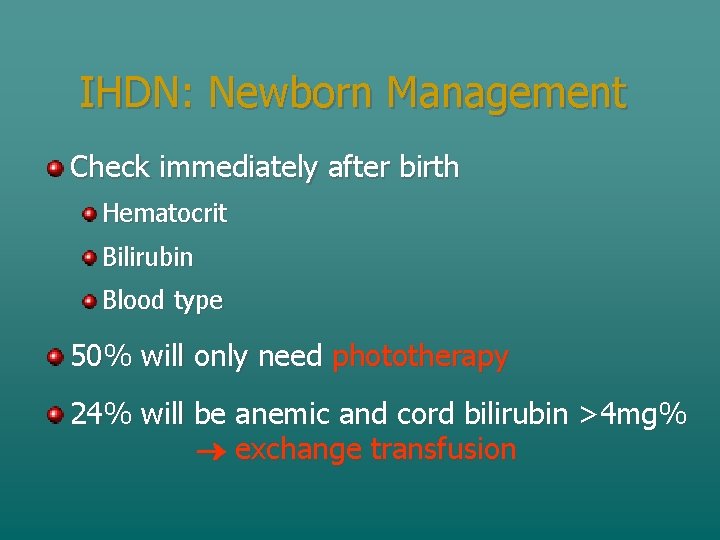
IHDN: Newborn Management Check immediately after birth Hematocrit Bilirubin Blood type 50% will only need phototherapy 24% will be anemic and cord bilirubin >4 mg% exchange transfusion
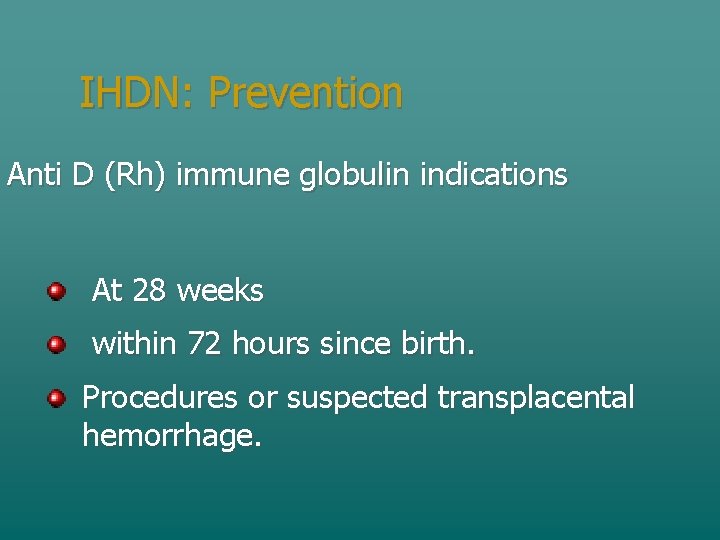
IHDN: Prevention Anti D (Rh) immune globulin indications At 28 weeks within 72 hours since birth. Procedures or suspected transplacental hemorrhage.
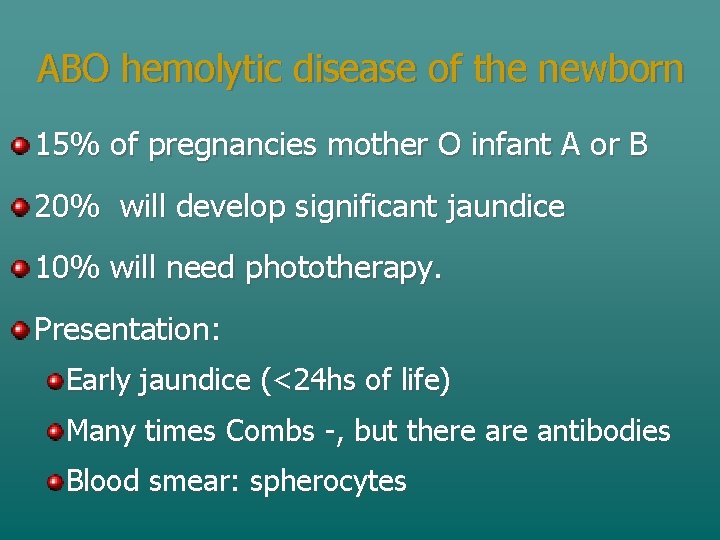
ABO hemolytic disease of the newborn 15% of pregnancies mother O infant A or B 20% will develop significant jaundice 10% will need phototherapy. Presentation: Early jaundice (<24 hs of life) Many times Combs -, but there antibodies Blood smear: spherocytes
Treatment: Phototherapy Bilirubin best absorbs light at 450 hm. The best is to provide it with blue light. White range: 380 -700 hm also adequate. Irradiation generates photochemical reaction in the extravascular space of the skin A higher illuminated area increases effectiveness
Treatment: Phototherapy Mechanism Photoisomerization: Natural Isomer 4 Z, 15 Z 4 Z, 15 E hydrosoluble blood biliar secretion (unconjugated) Slow excretion and fast reisomerization reabsorbed. Photooxydation: Small polar products. Slow
Treatment: Phototherapy mechanism Structural isomerization: Ciclization to lumirubin (irreversible) bile and urine Fast excretion not reabsorption. Related to dose of phototherapy (intensity of light)
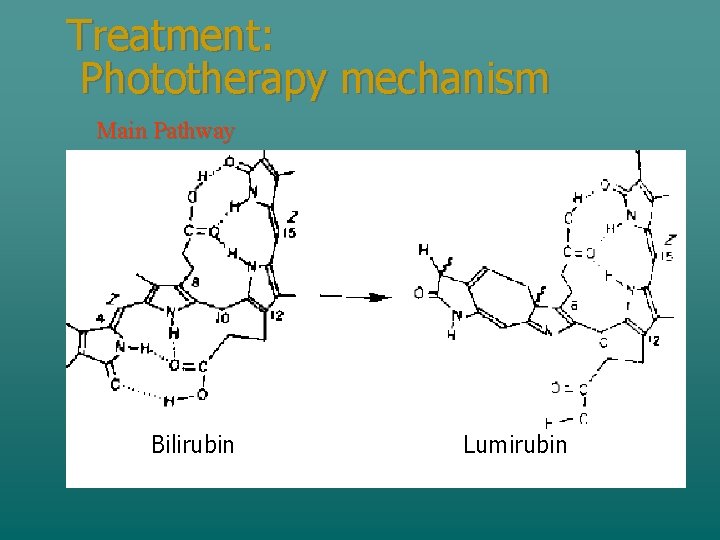
Treatment: Phototherapy mechanism Main Pathway Bilirubin Lumirubin
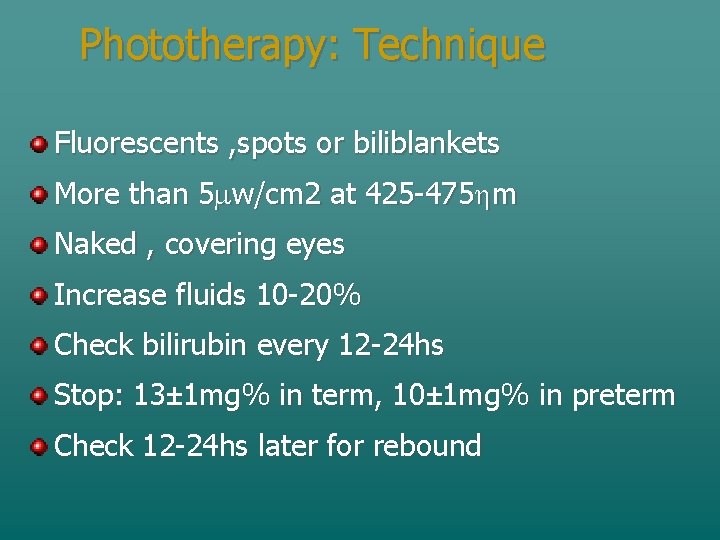
Phototherapy: Technique Fluorescents , spots or biliblankets More than 5 mw/cm 2 at 425 -475 hm Naked , covering eyes Increase fluids 10 -20% Check bilirubin every 12 -24 hs Stop: 13± 1 mg% in term, 10± 1 mg% in preterm Check 12 -24 hs later for rebound
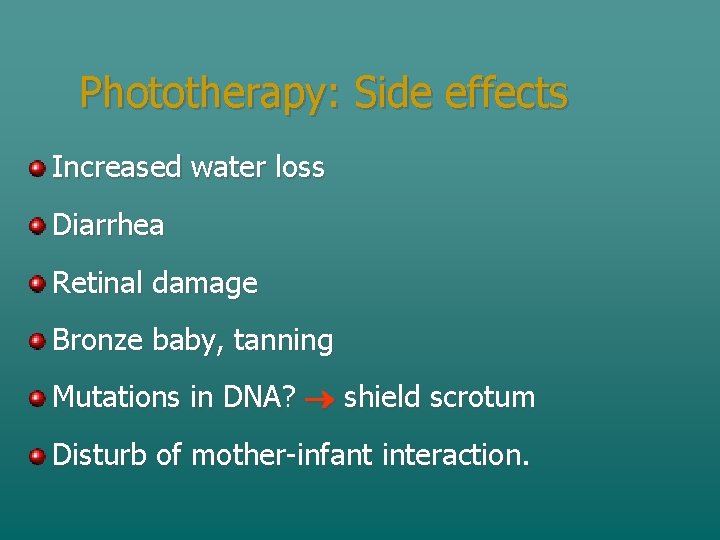
Phototherapy: Side effects Increased water loss Diarrhea Retinal damage Bronze baby, tanning Mutations in DNA? shield scrotum Disturb of mother-infant interaction.
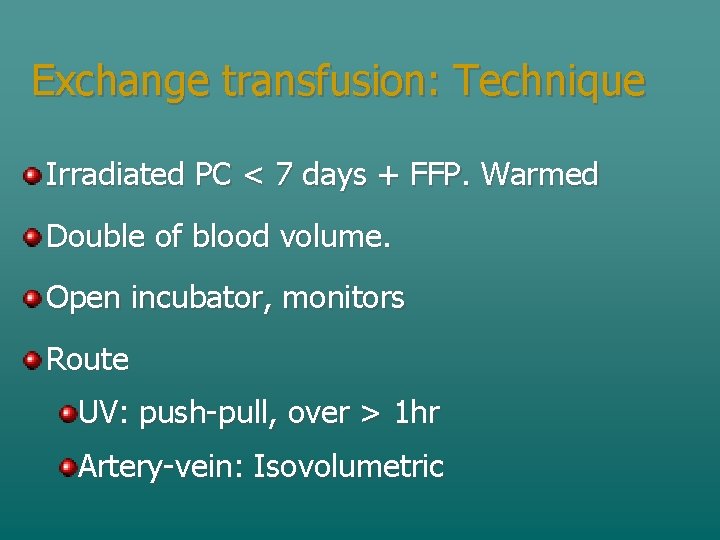
Exchange transfusion: Technique Irradiated PC < 7 days + FFP. Warmed Double of blood volume. Open incubator, monitors Route UV: push-pull, over > 1 hr Artery-vein: Isovolumetric
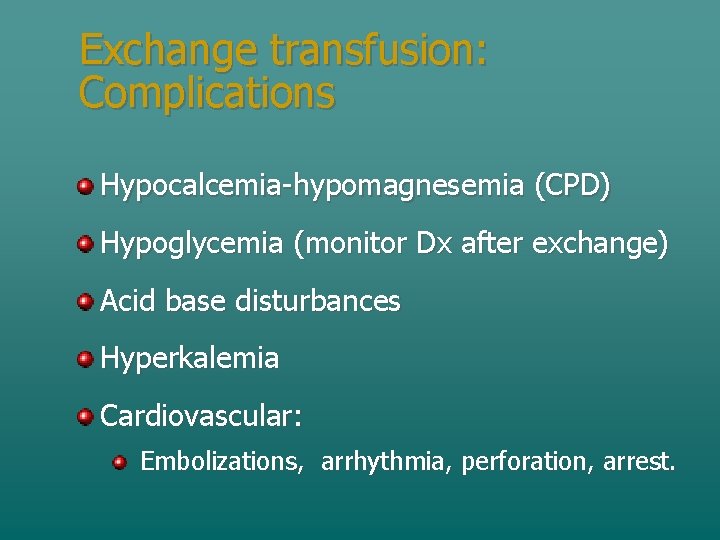
Exchange transfusion: Complications Hypocalcemia-hypomagnesemia (CPD) Hypoglycemia (monitor Dx after exchange) Acid base disturbances Hyperkalemia Cardiovascular: Embolizations, arrhythmia, perforation, arrest.
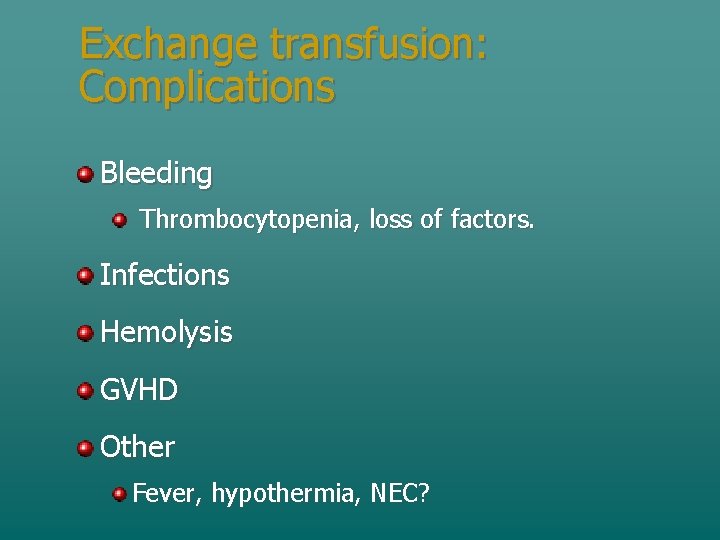
Exchange transfusion: Complications Bleeding Thrombocytopenia, loss of factors. Infections Hemolysis GVHD Other Fever, hypothermia, NEC?
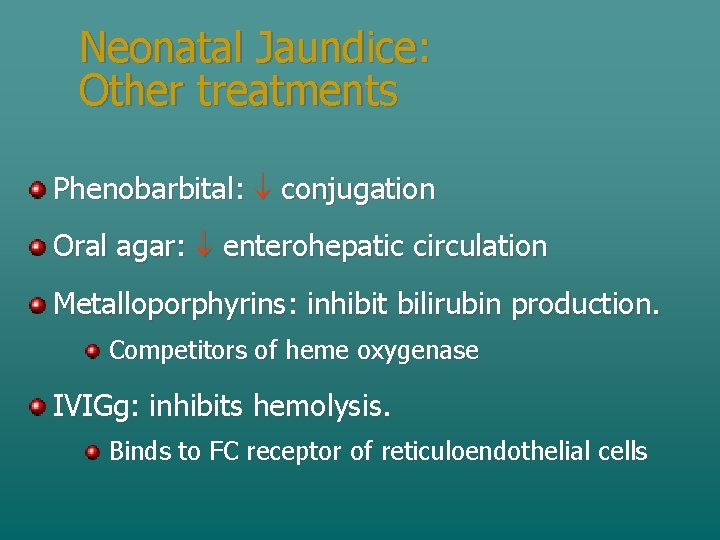
Neonatal Jaundice: Other treatments Phenobarbital: conjugation Oral agar: enterohepatic circulation Metalloporphyrins: inhibit bilirubin production. Competitors of heme oxygenase IVIGg: inhibits hemolysis. Binds to FC receptor of reticuloendothelial cells
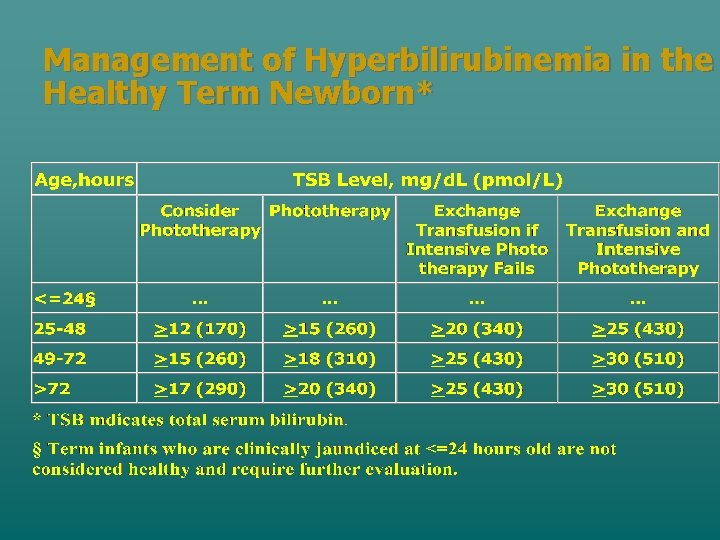
Management of Hyperbilirubinemia in the Healthy Term Newborn*
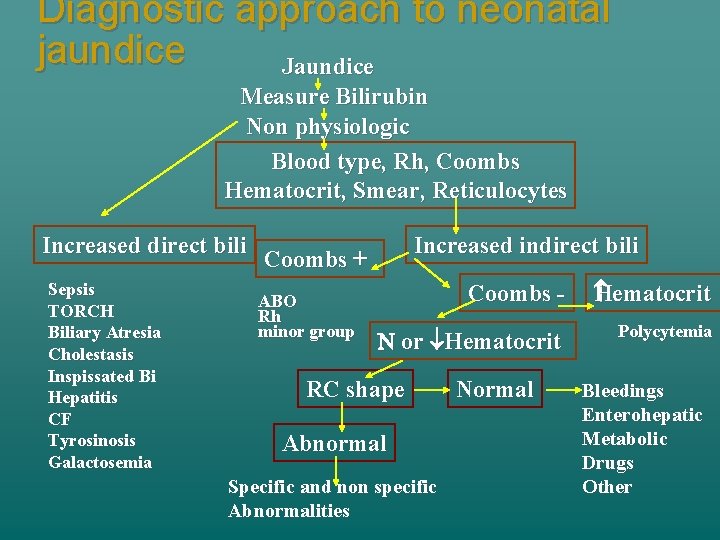
Diagnostic approach to neonatal jaundice Jaundice Measure Bilirubin Non physiologic Blood type, Rh, Coombs Hematocrit, Smear, Reticulocytes Increased direct bili Sepsis TORCH Biliary Atresia Cholestasis Inspissated Bi Hepatitis CF Tyrosinosis Galactosemia Increased indirect bili Coombs + ABO Rh minor group Coombs - Hematocrit N or Hematocrit Polycytemia RC shape Abnormal Specific and non specific Abnormalities Normal Bleedings Enterohepatic Metabolic Drugs Other
- Slides: 40