Neonatal Intensive Care Monitoring n Overview Neonatal Blood
Neonatal Intensive Care Monitoring n Overview – Neonatal Blood Gases – Pulse Oximeters – Neonatal Hemodynamic Equipment – Transcutaneous Monitors
Neonatal Blood Gases - Sampling Possibilities n Arterial Gases n Venous Gases n Capillary
Arterial Gases n Radial, Brachial, Temporal Punctures n Radial Artery Line n Umbilical Artery Gases n Umbilical Artery Catheter (UAC) n Preductal placement vs postductal placement
Venous Gases n Drawn from Umbilical Venous Catheter (UVC) n Not desirable but. . .
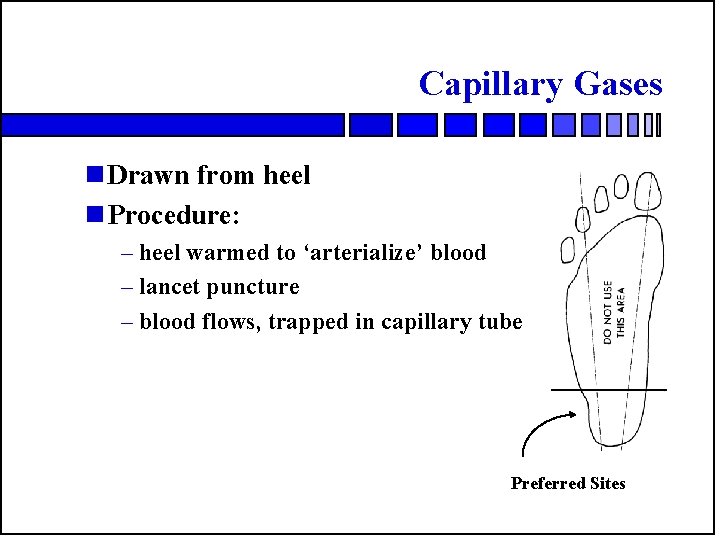
Capillary Gases n Drawn from heel n Procedure: – heel warmed to ‘arterialize’ blood – lancet puncture – blood flows, trapped in capillary tube Preferred Sites
Variability in Cap Gases n Warming time n Amount of contact with air n Squeezing blood n As a result, not desired but. . . .
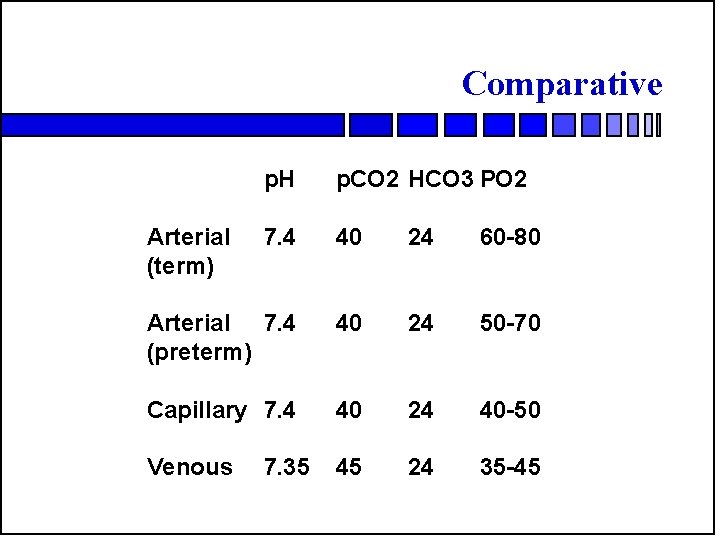
Comparative p. H p. CO 2 HCO 3 PO 2 7. 4 40 24 60 -80 Arterial 7. 4 (preterm) 40 24 50 -70 Capillary 7. 4 40 24 40 -50 Venous 45 24 35 -45 Arterial (term) 7. 35
Pulse Oximeters n Sites of attachment (foot and hand) n Preductal placement in first twelve hours (right hand)
Pulse Oximeters n Reads high – Methemoglobin – Caboxyhemoglobin – Jaundice n Reads low – Medical dyes n Other causes of inaccuracy – Motion – Hypothermia/vasoconstriction – Hypotension – Excessive ambient light on sensor probe
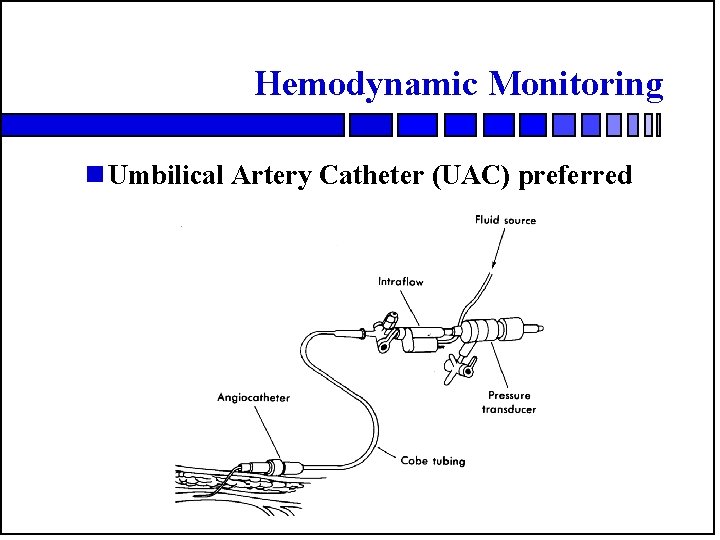
Hemodynamic Monitoring n Umbilical Artery Catheter (UAC) preferred
UAC Insertion Procedure n Insertional position 1/3 length heel to crown n Procedure – sterile field and drape – purse string suture around umbilicus – cut cord and snug – tease umbilical artery open – insert catheter – fix position – follow with CXR
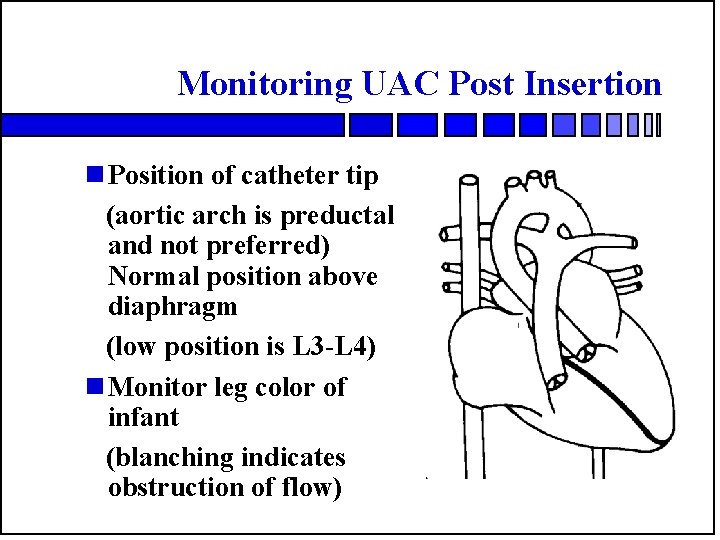
Monitoring UAC Post Insertion n Position of catheter tip (aortic arch is preductal and not preferred) Normal position above diaphragm (low position is L 3 -L 4) n Monitor leg color of infant (blanching indicates obstruction of flow)
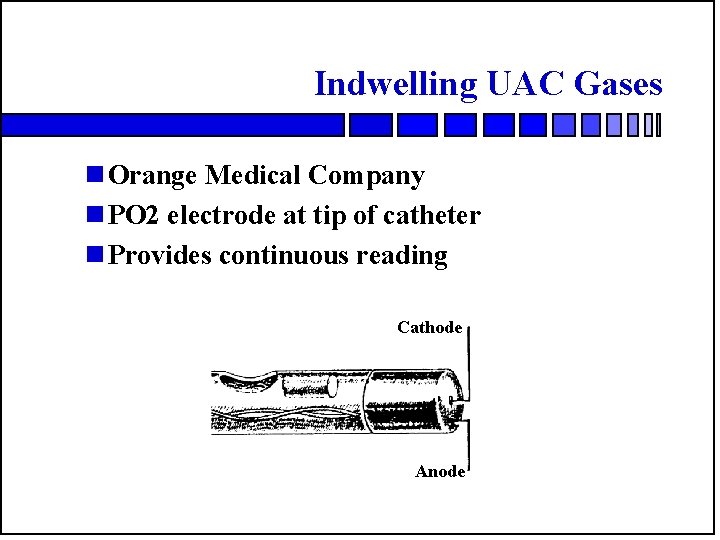
Indwelling UAC Gases n Orange Medical Company n PO 2 electrode at tip of catheter n Provides continuous reading Cathode Anode
Transcutaneous Gas Monitors n Useful as ‘trend’ monitor n Can detect hypoxemia, hyperoxemia n Can detect hypocarbia, hypercarbia n Also responds to changes in blood flow
Types of Transcutaneous Monitors n Single Electrode Models n PO 2 most common
Types of Transcutaneous Monitors n Dual element electrodes n PO 2 and PCO 2 n Called Tc. PO 2 and Tc. PCO 2
Principle of Operation Tc Monitors n Heated electrode placed on skin n Temperature 43 to 45 C n ‘Arterializes’ sample n Gas diffuses through skin
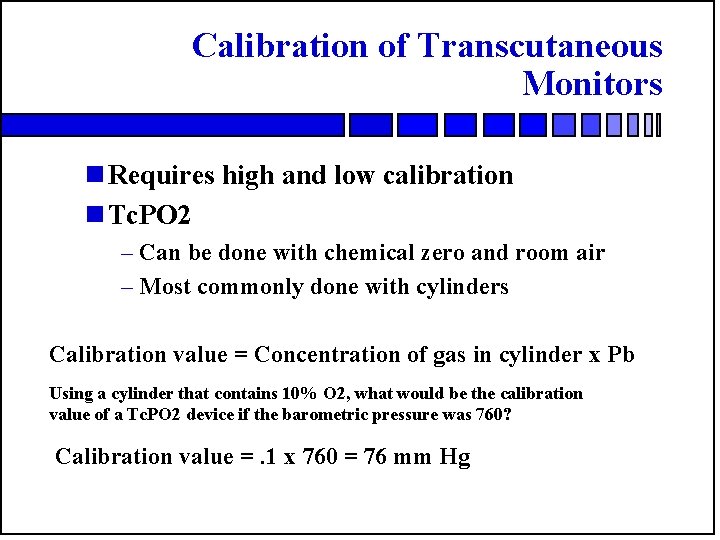
Calibration of Transcutaneous Monitors n Requires high and low calibration n Tc. PO 2 – Can be done with chemical zero and room air – Most commonly done with cylinders Calibration value = Concentration of gas in cylinder x Pb Using a cylinder that contains 10% O 2, what would be the calibration value of a Tc. PO 2 device if the barometric pressure was 760? Calibration value =. 1 x 760 = 76 mm Hg
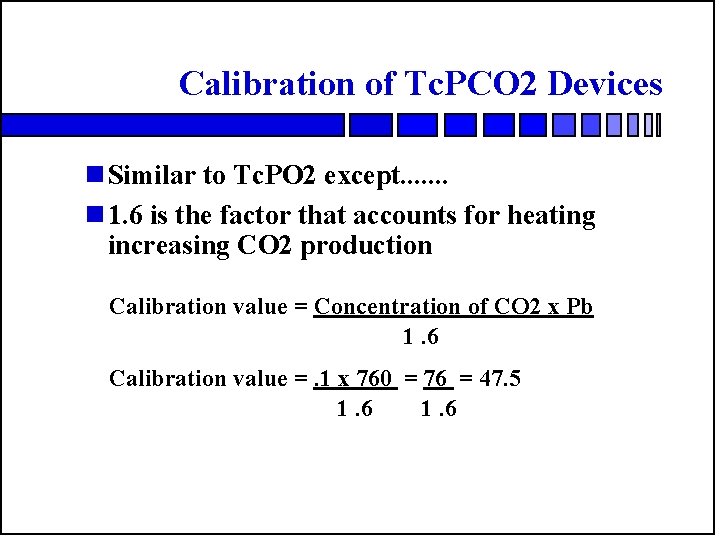
Calibration of Tc. PCO 2 Devices n Similar to Tc. PO 2 except. . . . n 1. 6 is the factor that accounts for heating increasing CO 2 production Calibration value = Concentration of CO 2 x Pb 1. 6 Calibration value =. 1 x 760 = 76 = 47. 5 1. 6
Normal Transcutaneous Gases n Tc. PCO 2 is 35 to 45 torr n Tc. PO 2 is 50 to 70 torr
Advantages of Transcutaneous Monitors n Decreased number of ‘sticks’ – cost reduction – lower infant risk (less invasive) n Trend tool – blood sample provides ‘view’ at one moment – gases values wander (+ 7 torr) – infant reaction to sample varies
Problems with Transcutaneous Monitors n Labor Intensive – Change site every 4 to 6 hours or more – Limited choices for attachment – (site must have perfusion) – Air leak around electrode n Burns – called ‘hookies’ after Huch
Interpretation of Tc Results n Air leak under electrode – Tc. PCO 2 reading near zero – Tc. PO 2 reading near Pb. O 2 n Decreased perfusion under electrode – Tc. PCO 2 will increase – Tc. PO 2 will decrease
- Slides: 23