Neonatal High Flow Nasal Cannula Towards A Clinical



- Slides: 36
Neonatal High Flow Nasal Cannula Towards A Clinical Practice Guideline Bradley A. Yoder, MD Professor of Pediatrics Division of Neonatology University of Utah School of Medicine
Disclosure Statement I have received research and/or travel compensation as a consultant to Drager Medical Fisher & Paykel Vapotherm & Ikaria
Objectives Recognize Detrimental Approaches Suggest Clinical Guidelines Identify Areas for Further Research
Contributing Consultants • Clare Collins, MBCh. B, Ph. D, FRACP. Department of Paediatrics, Mercy Hospital for Women, Melbourne, AU (CCollins@mercy. com. au) • Kevin Ives, MBBChir, , MD, FRCPCH. Dept of Neonatology, John Radcliffe Hospital, Oxford, UK (Kevin. Ives@nhs. net) • Brett Manley, MB BS (Hons. ), Ph. D, FRACP. Consultant Neonatologist Neonatal Services and Newborn Research Centre, Royal Women's Hospital Department of Obstetrics and Gynaecology, The University of Melbourne, AU (Brett. Manley@thewomens. org. au) • Michael Mc. Queen, MD, MBA, FAAP. Neonatology, Banner Health System, Phoenix, AZ, USA (Michael. Mc. Queen@bannerhealth. com) • Bradley A. Yoder, MD, FAAP. Division of Neonatology, University of Utah School of Medicine, SLC, UT, USA (bradley. yoder@hsc. utah. edu)
Why Do We Need Practice Guidelines?
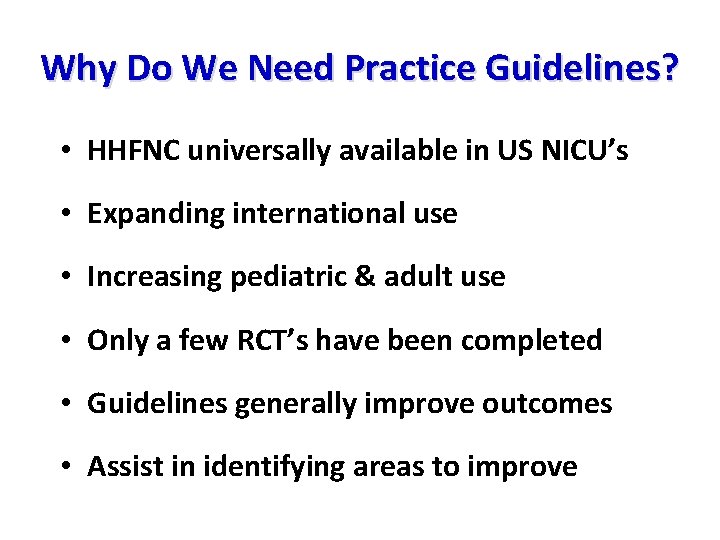
Why Do We Need Practice Guidelines? • HHFNC universally available in US NICU’s • Expanding international use • Increasing pediatric & adult use • Only a few RCT’s have been completed • Guidelines generally improve outcomes • Assist in identifying areas to improve
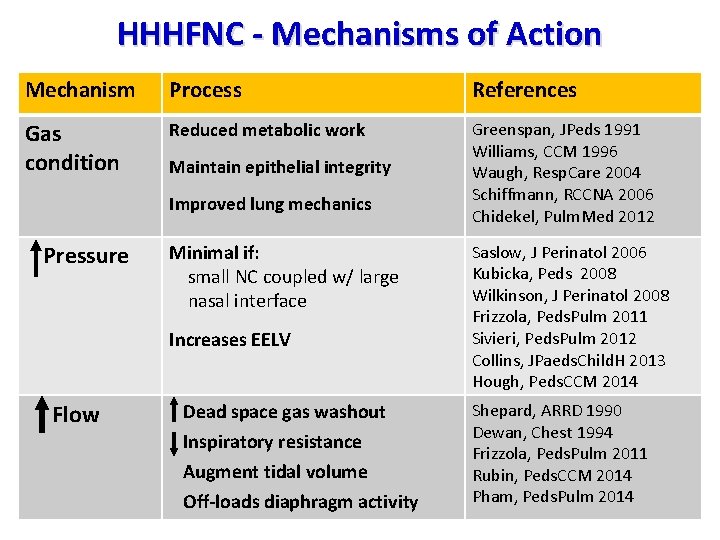
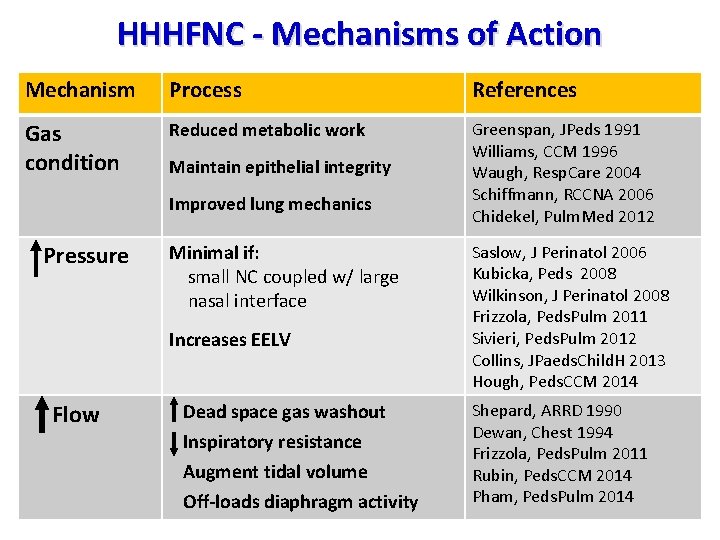
HHHFNC - Mechanisms of Action Mechanism Process References Gas condition Reduced metabolic work Greenspan, JPeds 1991 Williams, CCM 1996 Waugh, Resp. Care 2004 Schiffmann, RCCNA 2006 Chidekel, Pulm. Med 2012 Maintain epithelial integrity Improved lung mechanics Pressure Minimal if: small NC coupled w/ large nasal interface Increases EELV Flow Dead space gas washout Inspiratory resistance Augment tidal volume Off-loads diaphragm activity Saslow, J Perinatol 2006 Kubicka, Peds 2008 Wilkinson, J Perinatol 2008 Frizzola, Peds. Pulm 2011 Sivieri, Peds. Pulm 2012 Collins, JPaeds. Child. H 2013 Hough, Peds. CCM 2014 Shepard, ARRD 1990 Dewan, Chest 1994 Frizzola, Peds. Pulm 2011 Rubin, Peds. CCM 2014 Pham, Peds. Pulm 2014
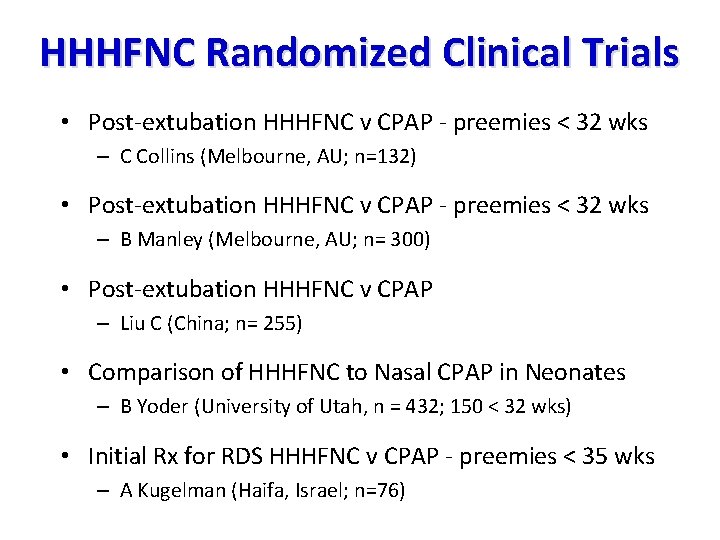
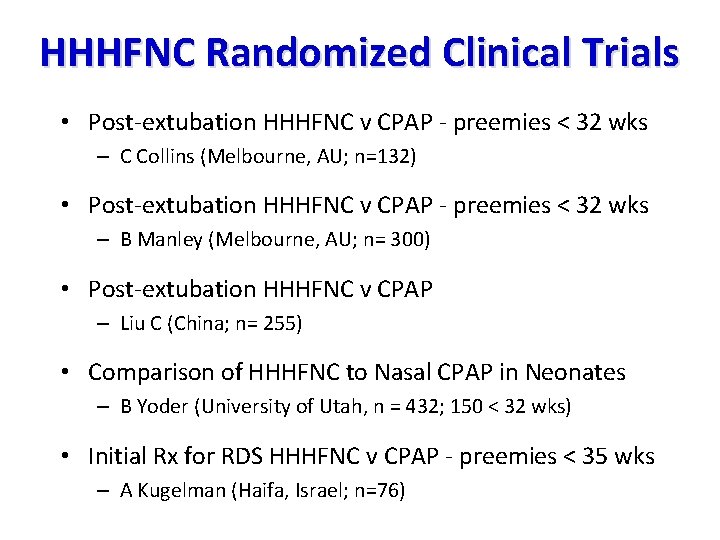
HHHFNC Randomized Clinical Trials • Post-extubation HHHFNC v CPAP - preemies < 32 wks – C Collins (Melbourne, AU; n=132) • Post-extubation HHHFNC v CPAP - preemies < 32 wks – B Manley (Melbourne, AU; n= 300) • Post-extubation HHHFNC v CPAP – Liu C (China; n= 255) • Comparison of HHHFNC to Nasal CPAP in Neonates – B Yoder (University of Utah, n = 432; 150 < 32 wks) • Initial Rx for RDS HHHFNC v CPAP - preemies < 35 wks – A Kugelman (Haifa, Israel; n=76)
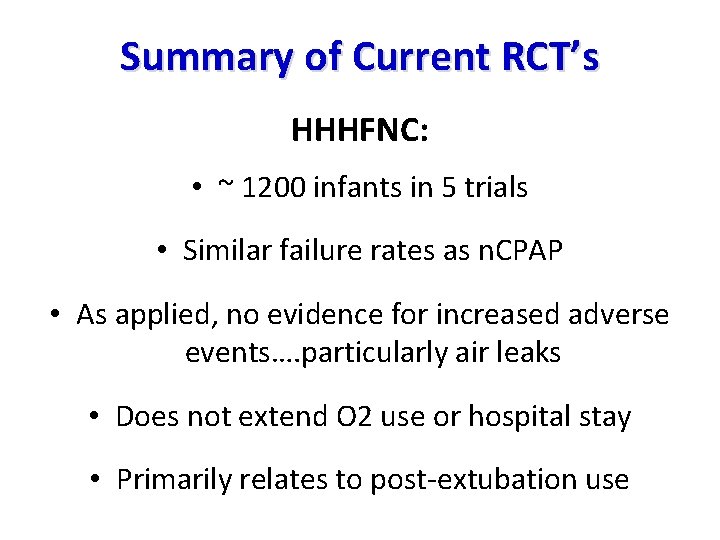
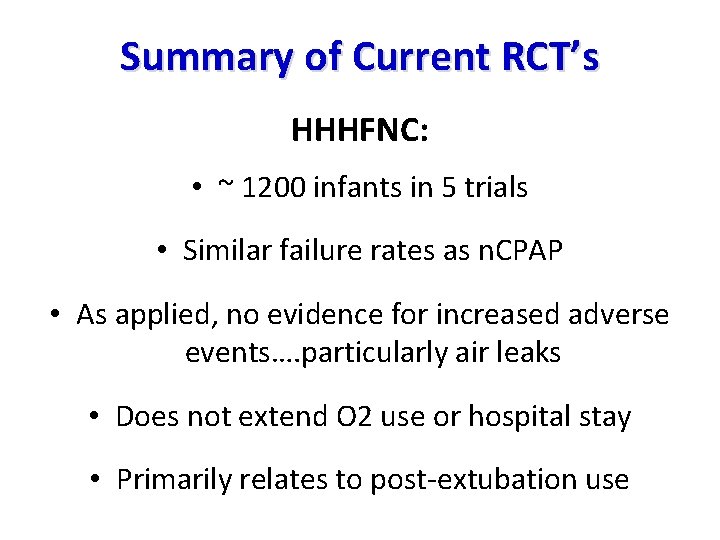
Summary of Current RCT’s HHHFNC: • ~ 1200 infants in 5 trials • Similar failure rates as n. CPAP • As applied, no evidence for increased adverse events…. particularly air leaks • Does not extend O 2 use or hospital stay • Primarily relates to post-extubation use
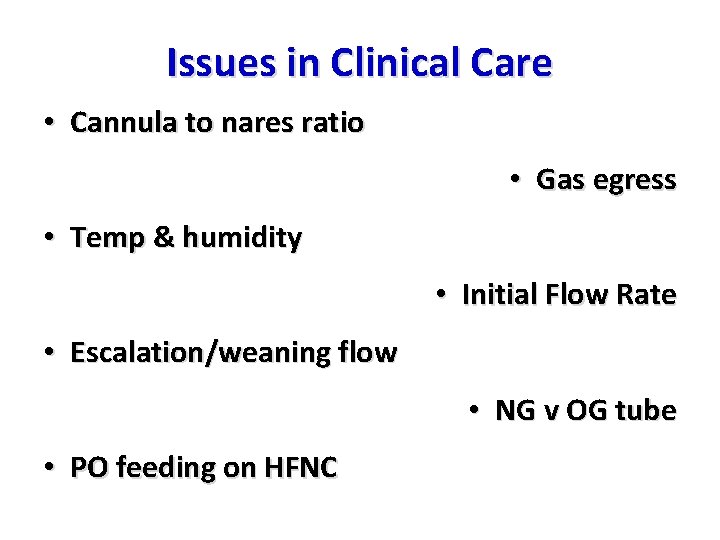
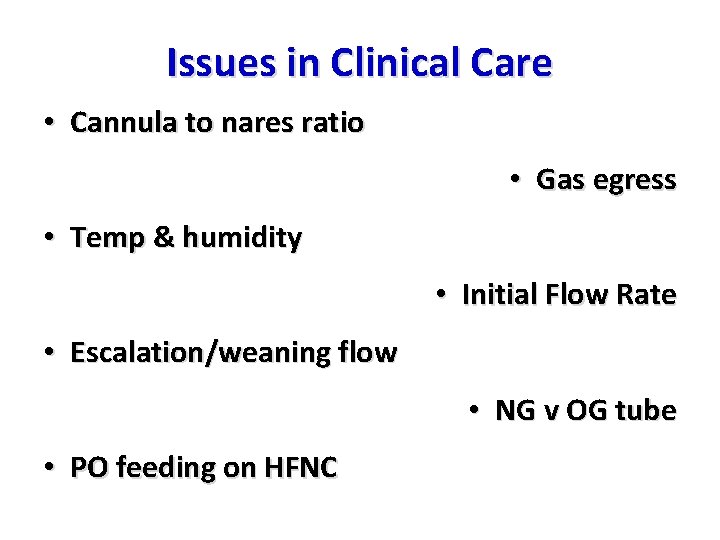
Issues in Clinical Care • Cannula to nares ratio • Gas egress • Temp & humidity • Initial Flow Rate • Escalation/weaning flow • NG v OG tube • PO feeding on HFNC
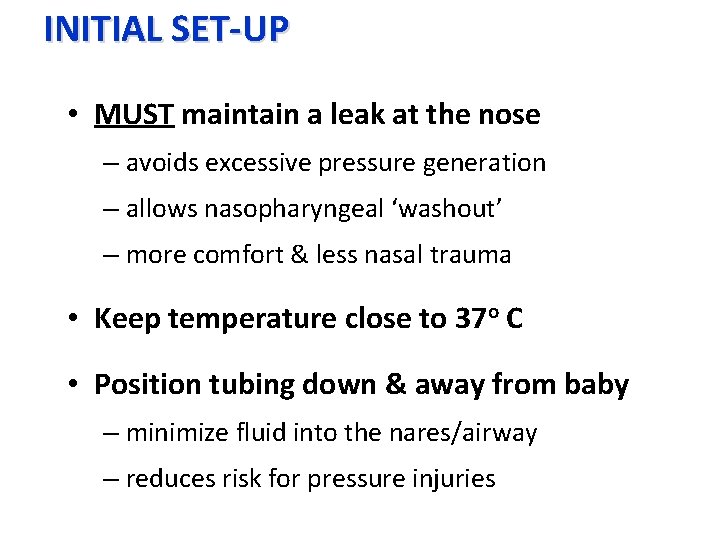
INITIAL SET-UP • MUST maintain a leak at the nose – avoids excessive pressure generation – allows nasopharyngeal ‘washout’ – more comfort & less nasal trauma • Keep temperature close to 37 o C • Position tubing down & away from baby – minimize fluid into the nares/airway – reduces risk for pressure injuries

Occlusive NC Non-occlusive NC
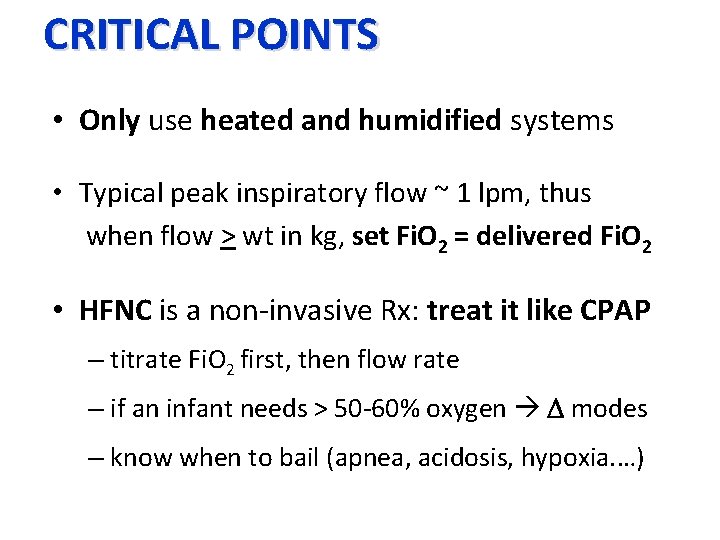
CRITICAL POINTS • Only use heated and humidified systems • Typical peak inspiratory flow ~ 1 lpm, thus when flow > wt in kg, set Fi. O 2 = delivered Fi. O 2 • HFNC is a non-invasive Rx: treat it like CPAP – titrate Fi. O 2 first, then flow rate – if an infant needs > 50 -60% oxygen D modes – know when to bail (apnea, acidosis, hypoxia. …)
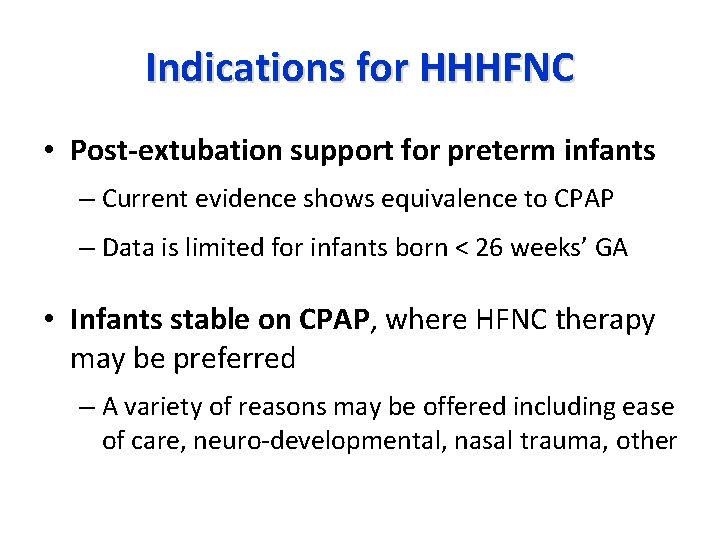
Indications for HHHFNC • Post-extubation support for preterm infants – Current evidence shows equivalence to CPAP – Data is limited for infants born < 26 weeks’ GA • Infants stable on CPAP, where HFNC therapy may be preferred – A variety of reasons may be offered including ease of care, neuro-developmental, nasal trauma, other
Unproven Benefit • As primary support for RDS or other acute neonatal respiratory disorder – Lack of evidence from RCT’s – But empirically used by many centers
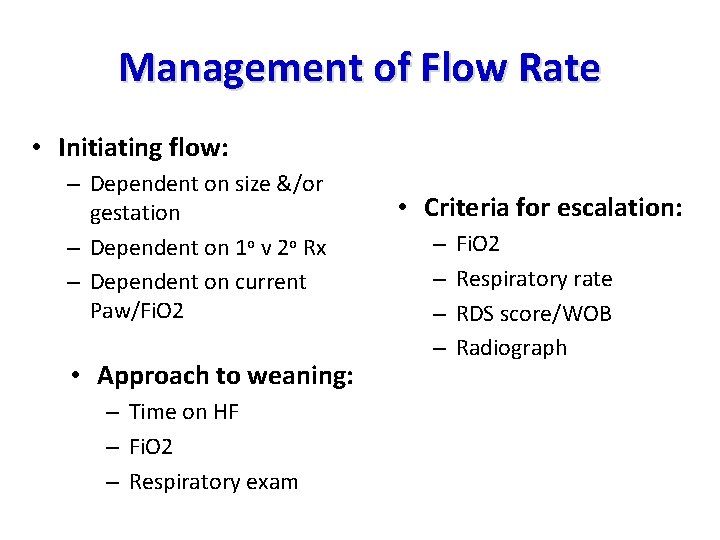
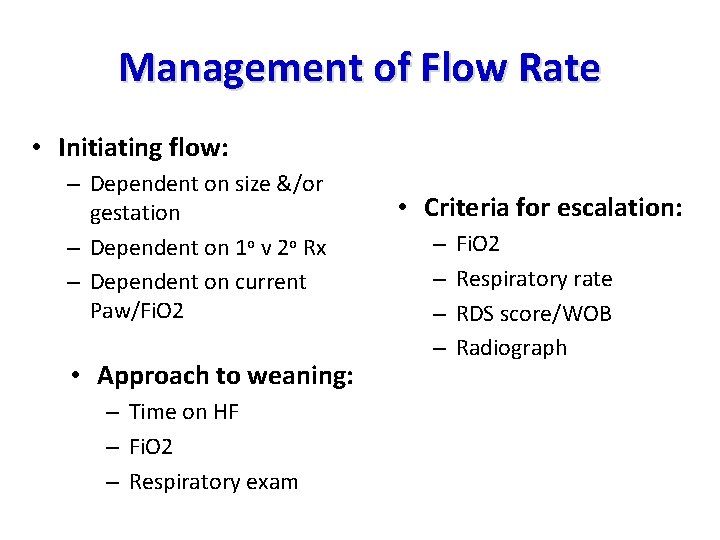
Management of Flow Rate • Initiating flow: – Dependent on size &/or gestation – Dependent on 1 o v 2 o Rx – Dependent on current Paw/Fi. O 2 • Approach to weaning: – Time on HF – Fi. O 2 – Respiratory exam • Criteria for escalation: – – Fi. O 2 Respiratory rate RDS score/WOB Radiograph
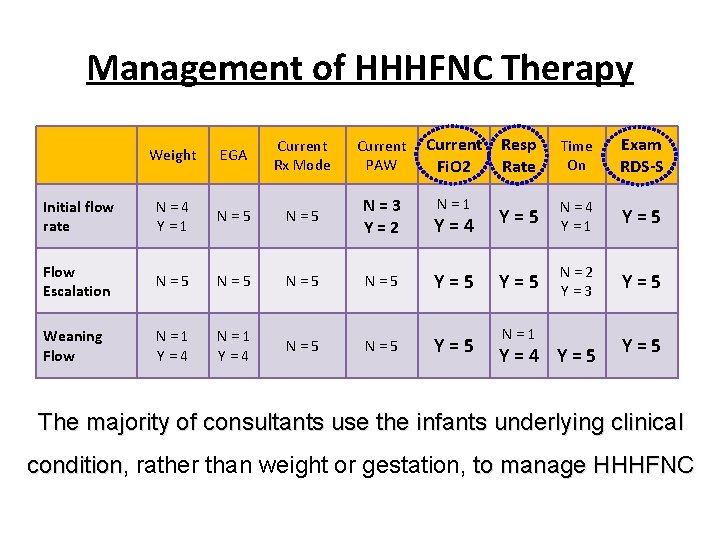
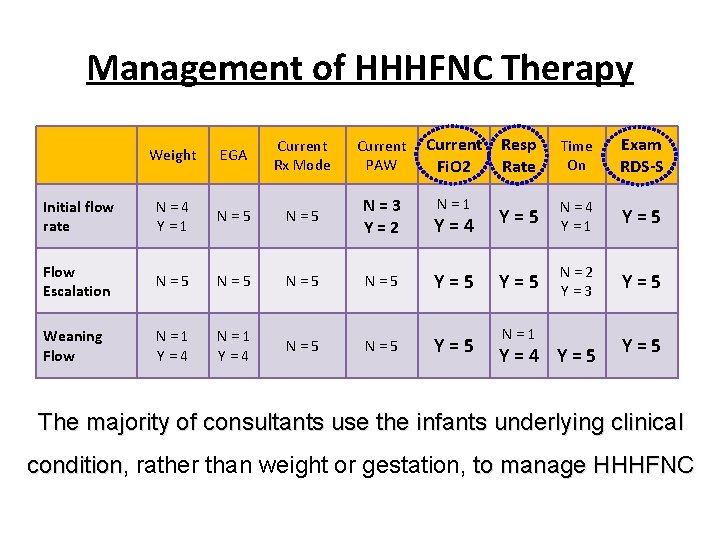
Management of HHHFNC Therapy Weight EGA Current Rx Mode Current PAW Current Fi. O 2 Resp Rate Time On Exam RDS-S Initial flow rate N=4 Y=1 N=5 N=3 Y=2 N=1 Y=4 Y=5 N=4 Y=1 Y=5 Flow Escalation N=5 N=5 Y=5 N=2 Y=3 Y=5 Weaning Flow N=1 Y=4 N=5 Y=5 N=1 Y=4 Y=5 The majority of consultants use the infants underlying clinical condition, condition rather than weight or gestation, to manage HHHFNC
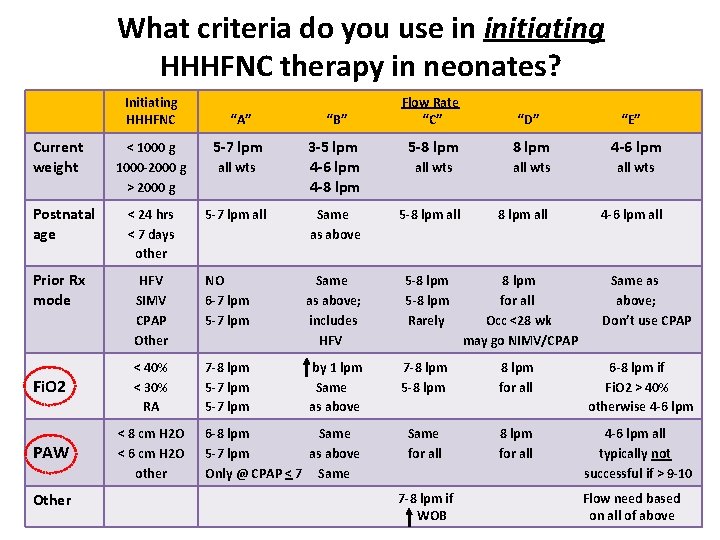
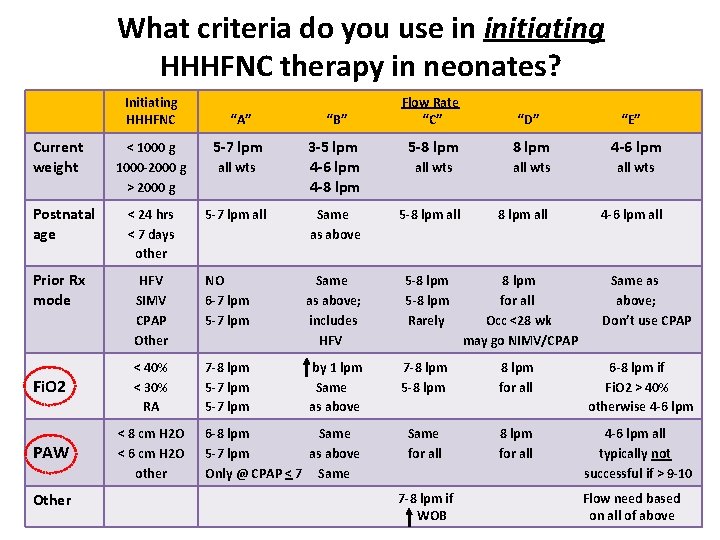
What criteria do you use in initiating HHHFNC therapy in neonates? Initiating HHHFNC Flow Rate “C” “D” “A” “B” < 1000 g 1000 -2000 g > 2000 g 5 -7 lpm 3 -5 lpm 4 -6 lpm 4 -8 lpm 5 -8 lpm 4 -6 lpm all wts < 24 hrs < 7 days other 5 -7 lpm all Same as above 5 -8 lpm all HFV SIMV CPAP Other NO 6 -7 lpm 5 -7 lpm Same as above; includes HFV 5 -8 lpm Rarely 8 lpm for all Occ <28 wk may go NIMV/CPAP Fi. O 2 < 40% < 30% RA 7 -8 lpm 5 -7 lpm by 1 lpm Same as above 7 -8 lpm 5 -8 lpm for all 6 -8 lpm if Fi. O 2 > 40% otherwise 4 -6 lpm PAW < 8 cm H 2 O < 6 cm H 2 O other Same for all 8 lpm for all 4 -6 lpm all typically not successful if > 9 -10 Current weight Postnatal age Prior Rx mode Other all wts 6 -8 lpm Same 5 -7 lpm as above Only @ CPAP < 7 Same 7 -8 lpm if WOB “E” 4 -6 lpm all Same as above; Don’t use CPAP Flow need based on all of above
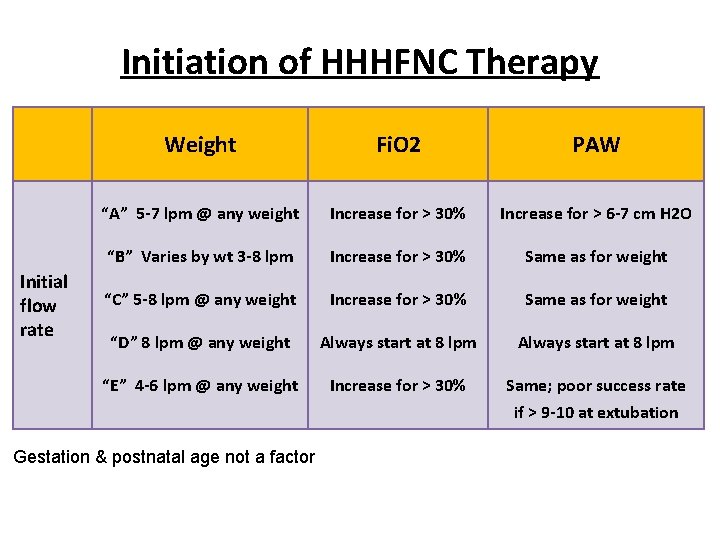
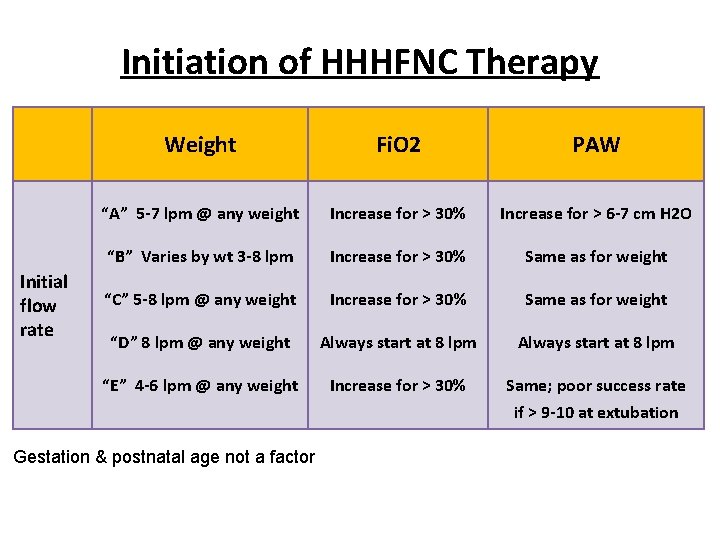
Initiation of HHHFNC Therapy Initial flow rate Weight Fi. O 2 PAW “A” 5 -7 lpm @ any weight Increase for > 30% Increase for > 6 -7 cm H 2 O “B” Varies by wt 3 -8 lpm Increase for > 30% Same as for weight “C” 5 -8 lpm @ any weight Increase for > 30% Same as for weight “D” 8 lpm @ any weight Always start at 8 lpm “E” 4 -6 lpm @ any weight Increase for > 30% Same; poor success rate if > 9 -10 at extubation Gestation & postnatal age not a factor
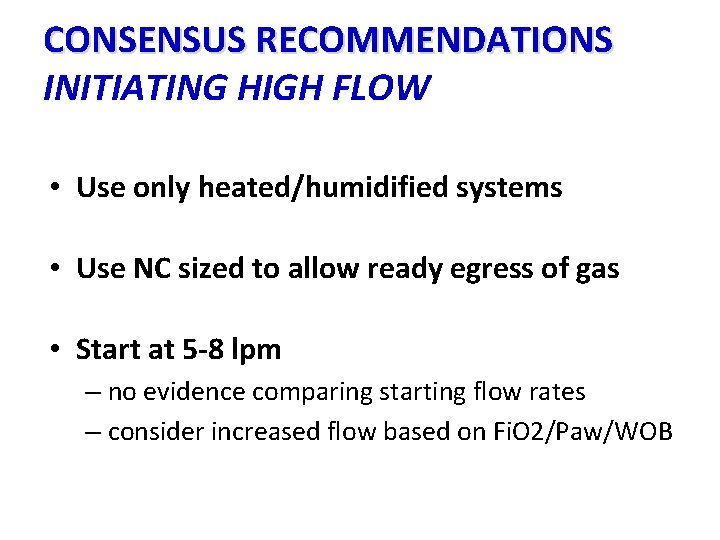
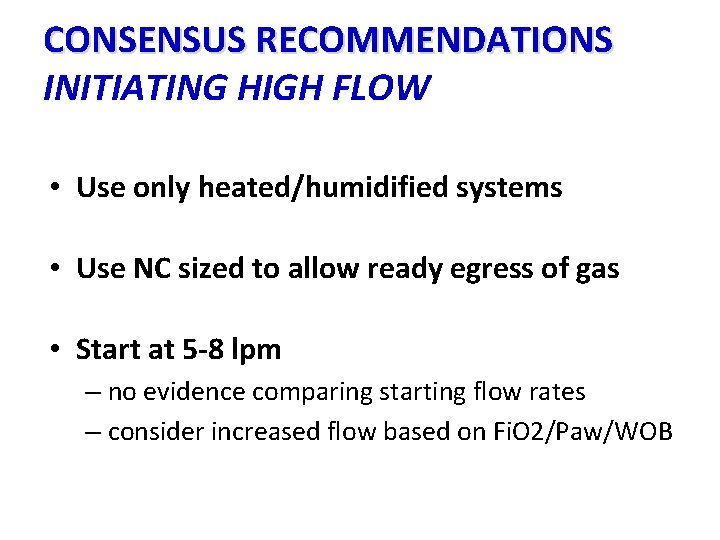
CONSENSUS RECOMMENDATIONS INITIATING HIGH FLOW • Use only heated/humidified systems • Use NC sized to allow ready egress of gas • Start at 5 -8 lpm – no evidence comparing starting flow rates – consider increased flow based on Fi. O 2/Paw/WOB
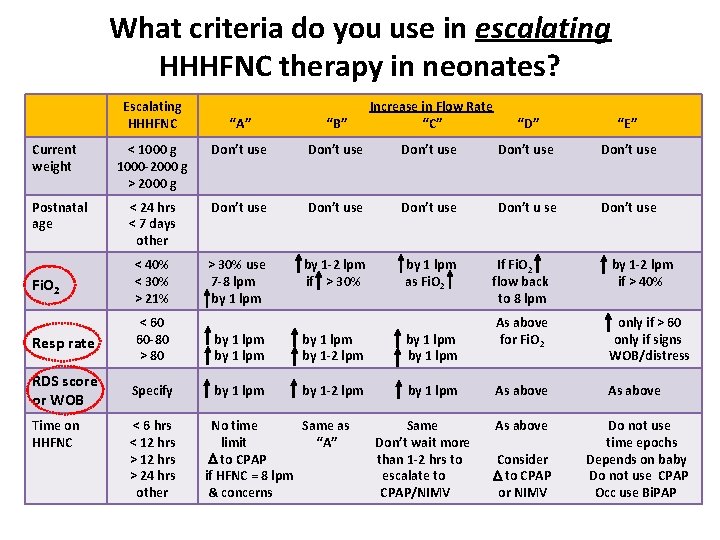
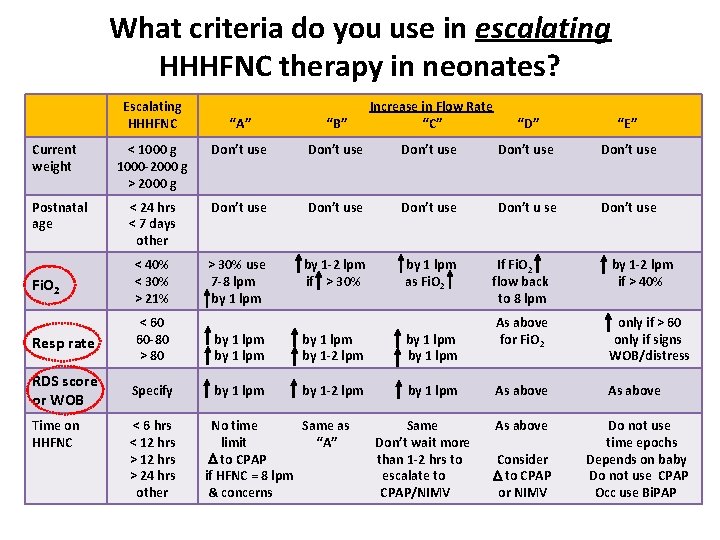
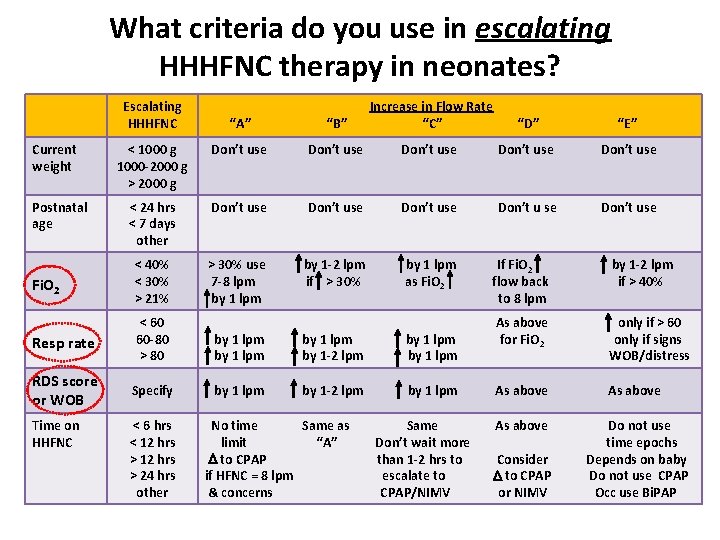
What criteria do you use in escalating HHHFNC therapy in neonates? Escalating HHHFNC “A” “B” Increase in Flow Rate “C” < 1000 g 1000 -2000 g > 2000 g Don’t use Don’t use < 24 hrs < 7 days other Don’t use Don’t u se Don’t use Fi. O 2 < 40% < 30% > 21% > 30% use 7 -8 lpm by 1 -2 lpm if > 30% by 1 lpm as Fi. O 2 Resp rate < 60 60 -80 > 80 by 1 lpm by 1 -2 lpm by 1 lpm RDS score or WOB Specify by 1 lpm by 1 -2 lpm by 1 lpm Current weight Postnatal age Time on HHFNC < 6 hrs < 12 hrs > 24 hrs other No time Same as limit “A” D to CPAP if HFNC = 8 lpm & concerns Same Don’t wait more than 1 -2 hrs to escalate to CPAP/NIMV “D” “E” If Fi. O 2 flow back to 8 lpm by 1 -2 lpm if > 40% As above for Fi. O 2 only if > 60 only if signs WOB/distress As above Do not use time epochs Depends on baby Do not use CPAP Occ use Bi. PAP Consider D to CPAP or NIMV
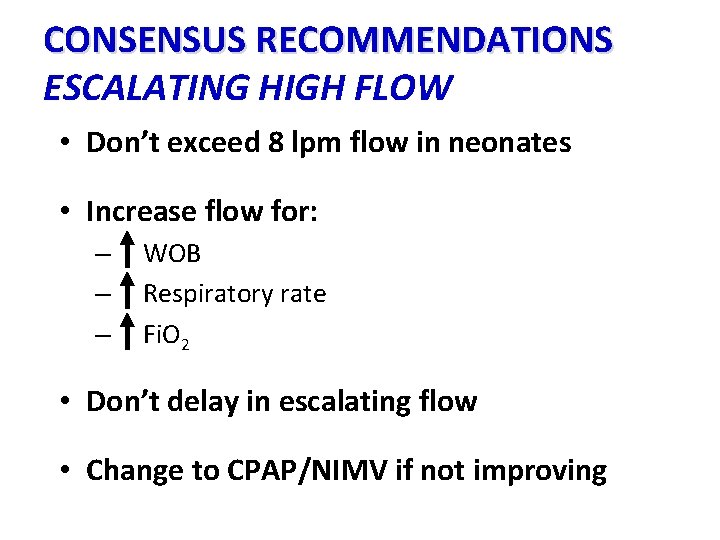
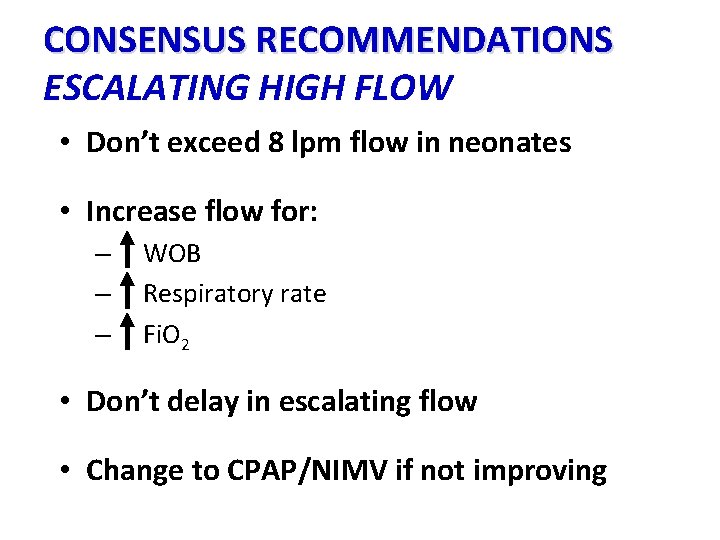
CONSENSUS RECOMMENDATIONS ESCALATING HIGH FLOW • Don’t exceed 8 lpm flow in neonates • Increase flow for: – – – WOB Respiratory rate Fi. O 2 • Don’t delay in escalating flow • Change to CPAP/NIMV if not improving
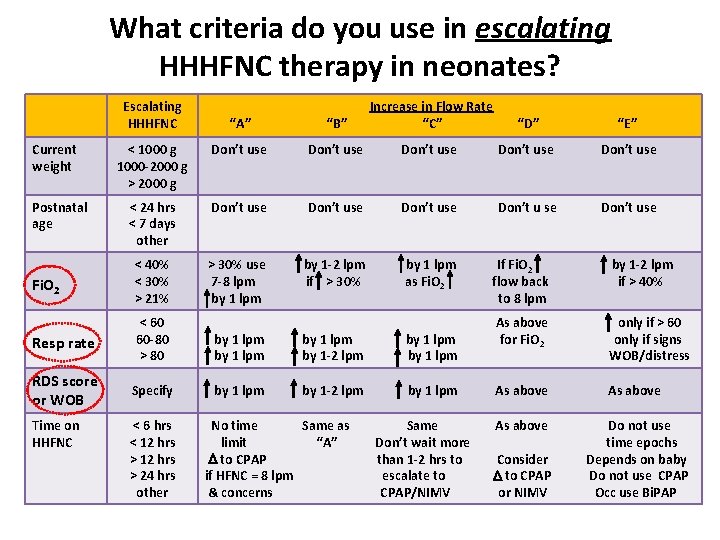
What criteria do you use in escalating HHHFNC therapy in neonates? Escalating HHHFNC “A” “B” Increase in Flow Rate “C” < 1000 g 1000 -2000 g > 2000 g Don’t use Don’t use < 24 hrs < 7 days other Don’t use Don’t u se Don’t use Fi. O 2 < 40% < 30% > 21% > 30% use 7 -8 lpm by 1 -2 lpm if > 30% by 1 lpm as Fi. O 2 Resp rate < 60 60 -80 > 80 by 1 lpm by 1 -2 lpm by 1 lpm RDS score or WOB Specify by 1 lpm by 1 -2 lpm by 1 lpm Current weight Postnatal age Time on HHFNC < 6 hrs < 12 hrs > 24 hrs other No time Same as limit “A” D to CPAP if HFNC = 8 lpm & concerns Same Don’t wait more than 1 -2 hrs to escalate to CPAP/NIMV “D” “E” If Fi. O 2 flow back to 8 lpm by 1 -2 lpm if > 40% As above for Fi. O 2 only if > 60 only if signs WOB/distress As above Do not use time epochs Depends on baby Do not use CPAP Occ use Bi. PAP Consider D to CPAP or NIMV
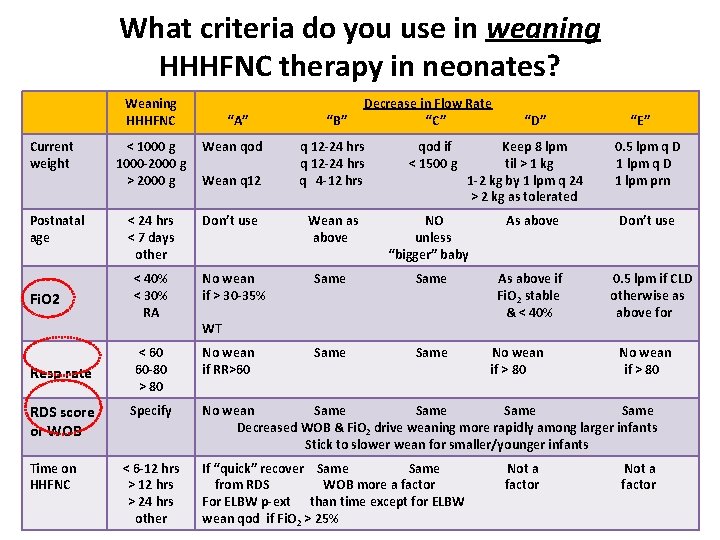
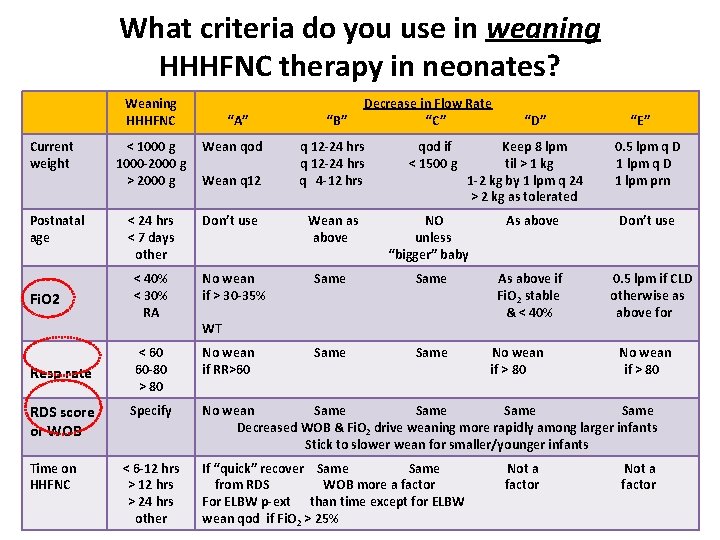
What criteria do you use in weaning HHHFNC therapy in neonates? Weaning HHHFNC Current weight Postnatal age Fi. O 2 Resp rate RDS score or WOB Time on HHFNC “A” < 1000 g 1000 -2000 g > 2000 g Wean qod < 24 hrs < 7 days other Don’t use Wean q 12 < 40% < 30% RA No wean if > 30 -35% < 60 60 -80 > 80 No wean if RR>60 Specify < 6 -12 hrs > 24 hrs other “B” Decrease in Flow Rate “C” q 12 -24 hrs q 4 -12 hrs qod if < 1500 g “D” Keep 8 lpm til > 1 kg 1 -2 kg by 1 lpm q 24 > 2 kg as tolerated “E” 0. 5 lpm q D 1 lpm prn Wean as above NO unless “bigger” baby As above Don’t use Same As above if Fi. O 2 stable & < 40% 0. 5 lpm if CLD otherwise as above for Same WT No wean if > 80 No wean Same Decreased WOB & Fi. O 2 drive weaning more rapidly among larger infants Stick to slower wean for smaller/younger infants If “quick” recover Same from RDS WOB more a factor For ELBW p-ext than time except for ELBW wean qod if Fi. O 2 > 25% Not a factor
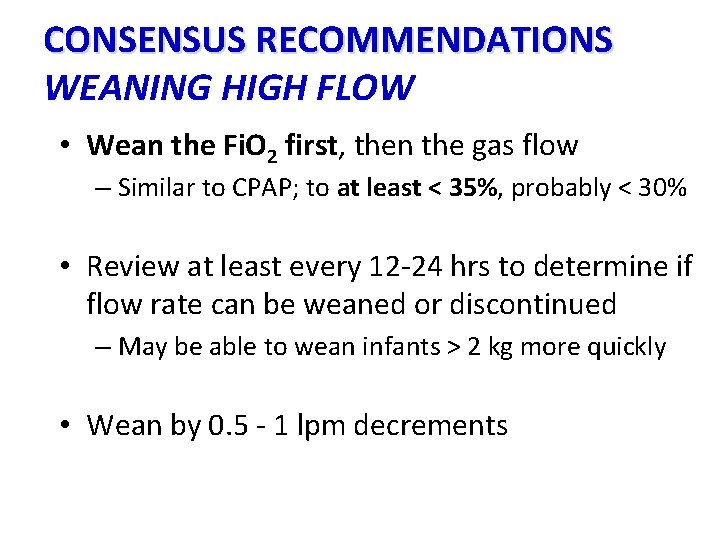
CONSENSUS RECOMMENDATIONS WEANING HIGH FLOW • Wean the Fi. O 2 first, then the gas flow – Similar to CPAP; to at least < 35%, probably < 30% • Review at least every 12 -24 hrs to determine if flow rate can be weaned or discontinued – May be able to wean infants > 2 kg more quickly • Wean by 0. 5 - 1 lpm decrements
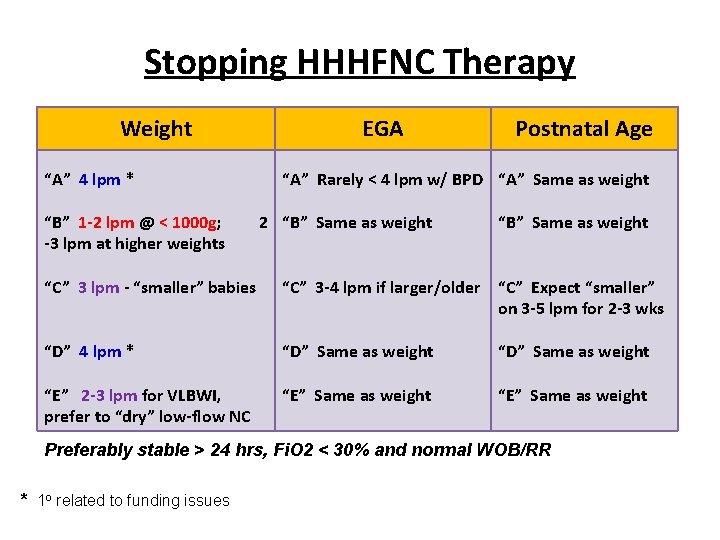
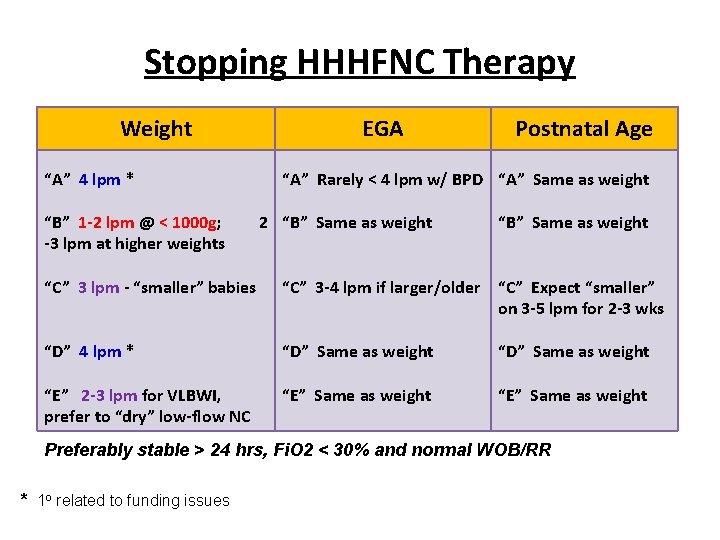
Stopping HHHFNC Therapy Weight “A” 4 lpm * “B” 1 -2 lpm @ < 1000 g; -3 lpm at higher weights EGA Postnatal Age “A” Rarely < 4 lpm w/ BPD “A” Same as weight 2 “B” Same as weight “C” 3 lpm - “smaller” babies “C” 3 -4 lpm if larger/older “C” Expect “smaller” on 3 -5 lpm for 2 -3 wks “D” 4 lpm * “D” Same as weight “E” 2 -3 lpm for VLBWI, prefer to “dry” low-flow NC “E” Same as weight Preferably stable > 24 hrs, Fi. O 2 < 30% and normal WOB/RR * 1 o related to funding issues
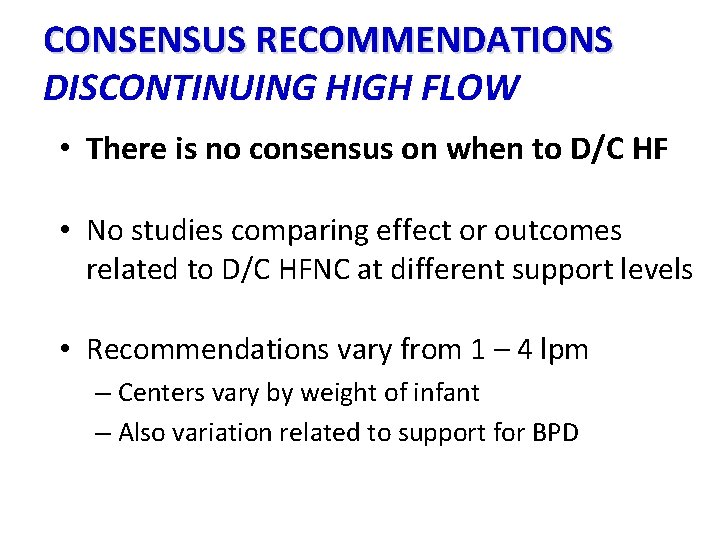
CONSENSUS RECOMMENDATIONS DISCONTINUING HIGH FLOW • There is no consensus on when to D/C HF • No studies comparing effect or outcomes related to D/C HFNC at different support levels • Recommendations vary from 1 – 4 lpm – Centers vary by weight of infant – Also variation related to support for BPD
CONSENSUS ! THIS WOULD WORK A LOT BETTER IF YOU’D JUST AGREE WITH ME
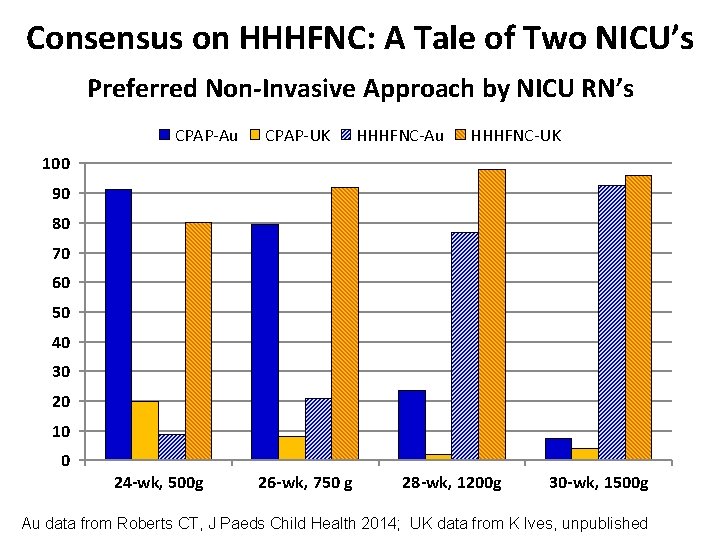
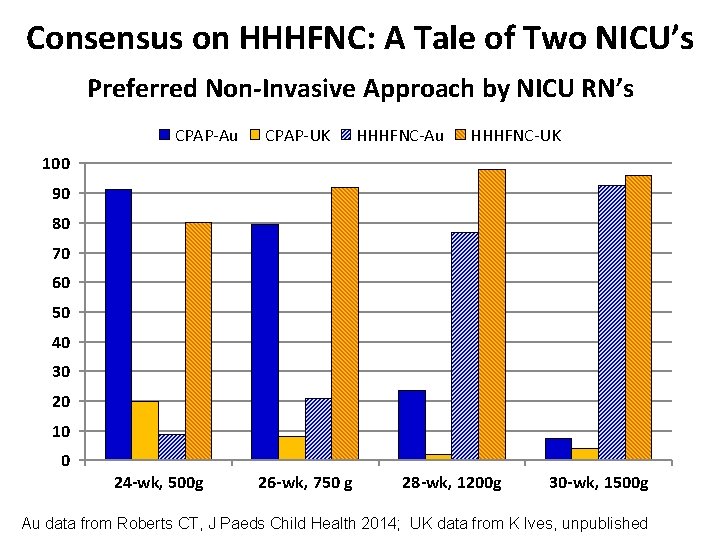
Consensus on HHHFNC: A Tale of Two NICU’s Preferred Non-Invasive Approach by NICU RN’s CPAP-Au CPAP-UK HHHFNC-Au HHHFNC-UK 100 90 80 70 60 50 40 30 20 10 0 24 -wk, 500 g 26 -wk, 750 g 28 -wk, 1200 g 30 -wk, 1500 g Au data from Roberts CT, J Paeds Child Health 2014; UK data from K Ives, unpublished

The Future Challenges are what make life interesting …… …… overcoming them is what makes life meaningful Joshua J. Marine
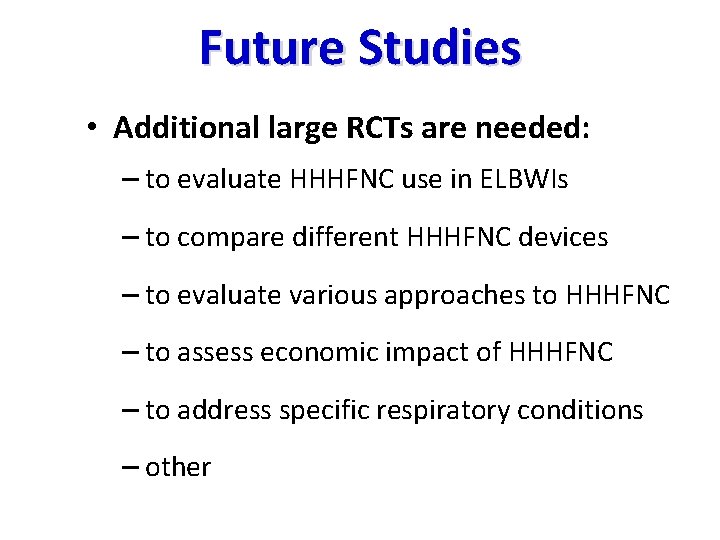
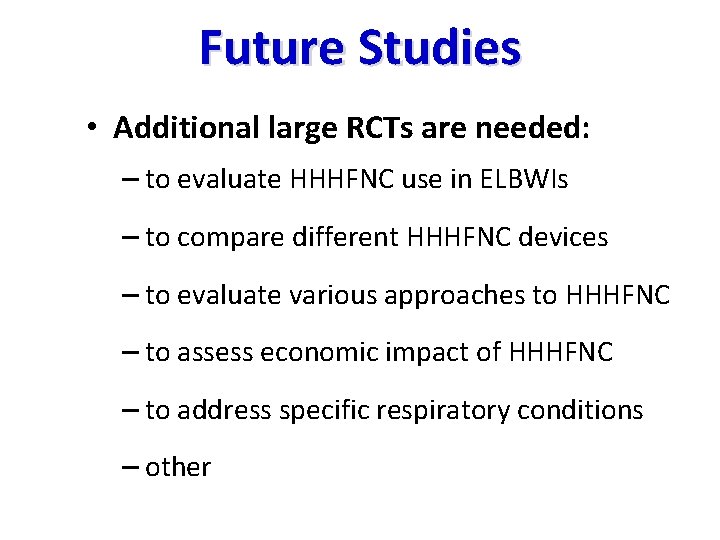
Future Studies • Additional large RCTs are needed: – to evaluate HHHFNC use in ELBWIs – to compare different HHHFNC devices – to evaluate various approaches to HHHFNC – to assess economic impact of HHHFNC – to address specific respiratory conditions – other
VIGILANCE You can’t see it if you don’t stay awake
SUMMARY • HHHFNC is in wide clinical use • RCT’s support HHHFNC as safe, effective alternative to n. CPAP at the time of extubation • Additional RCT’s are needed to study HHHFNC as 1 o therapy & related to flow management • Except for stopping, there is moderate consensus in the management of HHHFNC
Contributing Consultants • Clare Collins, MBCh. B, Ph. D, FRACP. Mercy Hospital for Women, Melbourne, AU • Kevin Ives, MBBChir, , MD, FRCPCH. John Radcliffe Hospital, Oxford, UK • Brett Manley, MB BS (Hons. ), Ph. D, FRACP. The University of Melbourne, AU • Michael Mc. Queen, MD, MBA, FAAP. Banner Health System, Phoenix, AZ, USA
