Neonatal fever General data Name Gender male 1
- Slides: 29
Neonatal fever 新生兒發燒
General data Name: 黃ㄨ瑩之子 Gender: male / 1 -day-old Hx: 2791668 Ward: PICU-CN 02 Admission Date: 2014/10/24 Time of birth: 2014/10/24 22: 05 GA: 39 1/7 weeks, BBW: 3458 gm
Chief complaint Fever 38. 3℃(Anal temperature) after birth.
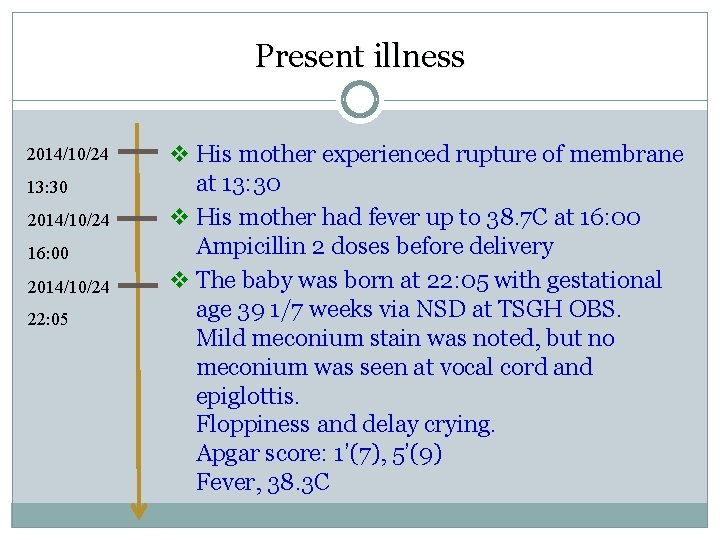
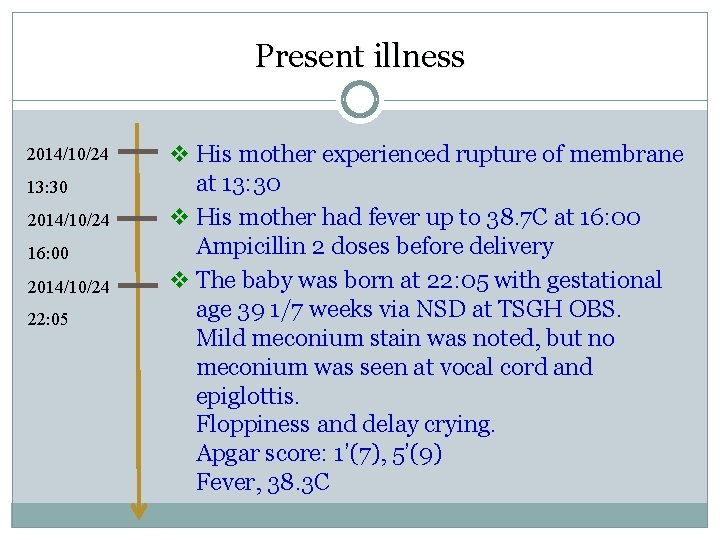
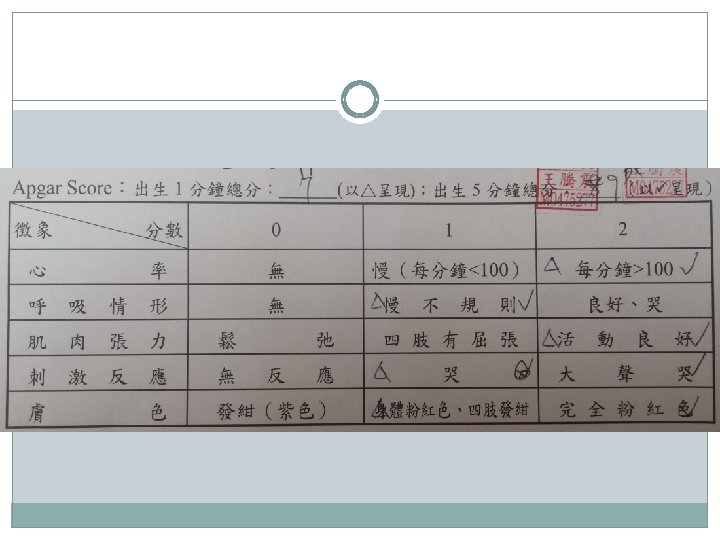
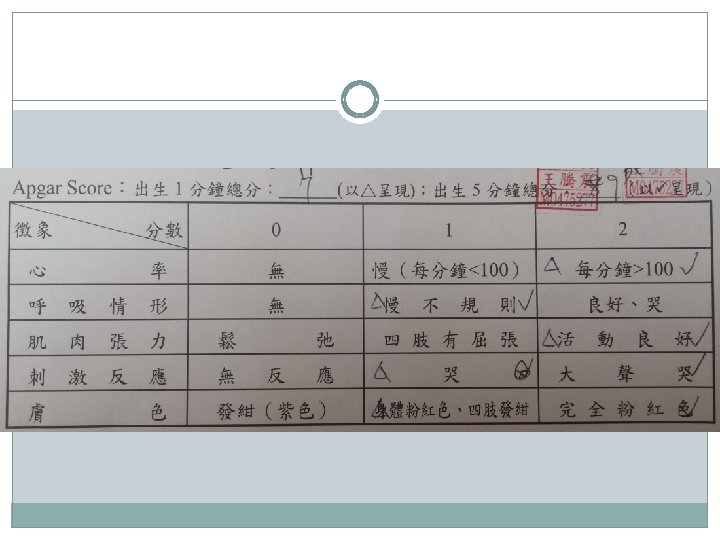
Present illness 2014/10/24 13: 30 2014/10/24 16: 00 2014/10/24 22: 05 v His mother experienced rupture of membrane at 13: 30 v His mother had fever up to 38. 7 C at 16: 00 Ampicillin 2 doses before delivery v The baby was born at 22: 05 with gestational age 39 1/7 weeks via NSD at TSGH OBS. Mild meconium stain was noted, but no meconium was seen at vocal cord and epiglottis. Floppiness and delay crying. Apgar score: 1’(7), 5’(9) Fever, 38. 3 C
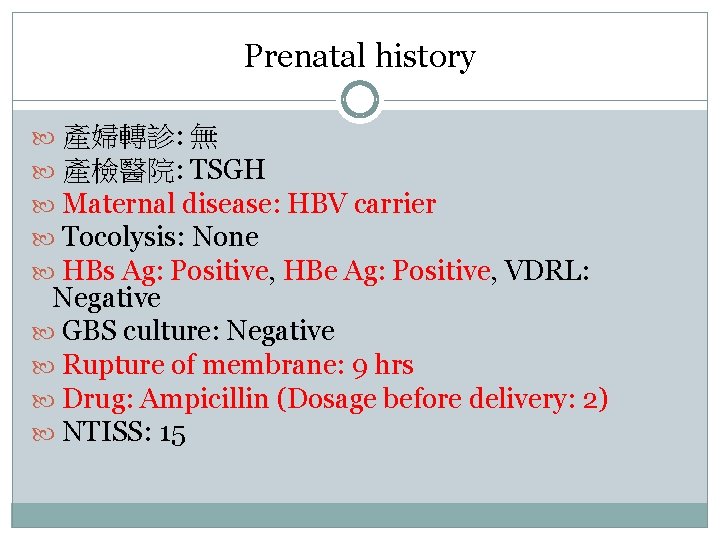
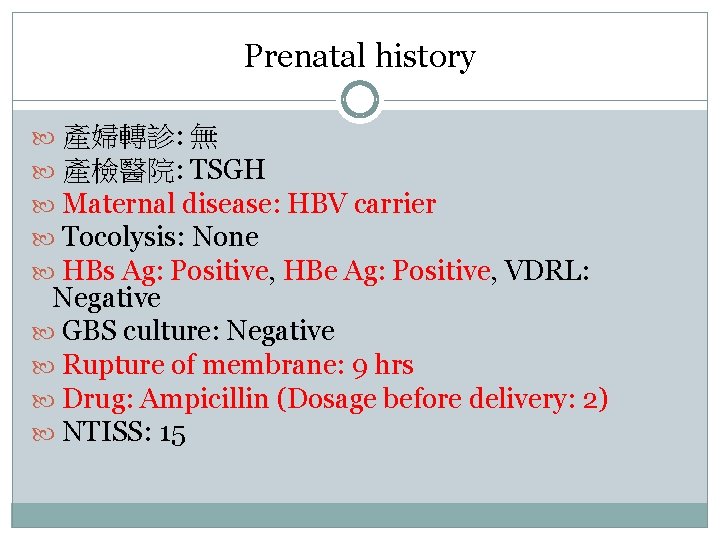
Prenatal history 產婦轉診: 無 產檢醫院: TSGH Maternal disease: HBV carrier Tocolysis: None HBs Ag: Positive, HBe Ag: Positive, VDRL: Negative GBS culture: Negative Rupture of membrane: 9 hrs Drug: Ampicillin (Dosage before delivery: 2) NTISS: 15
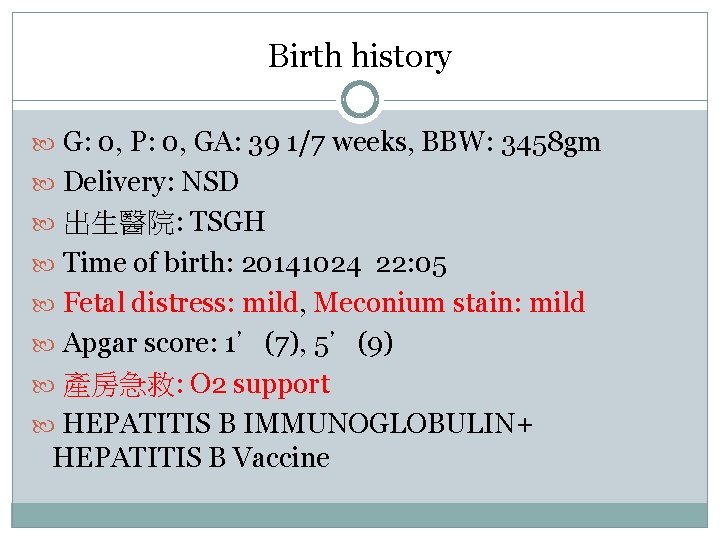
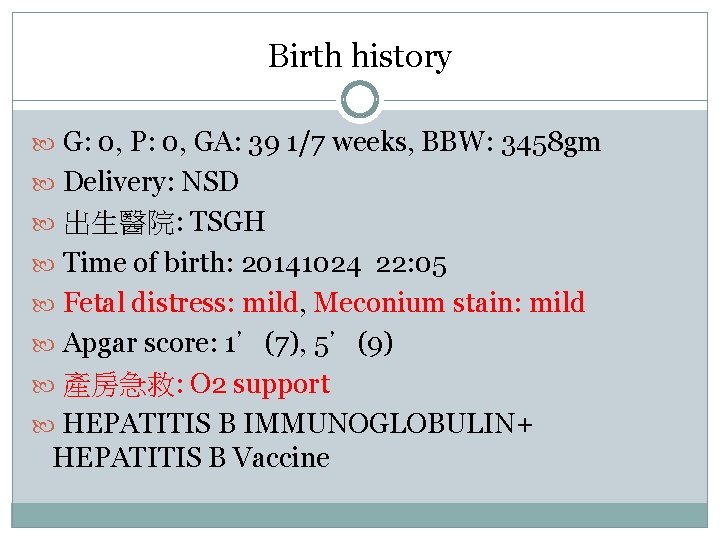
Birth history G: 0, P: 0, GA: 39 1/7 weeks, BBW: 3458 gm Delivery: NSD 出生醫院: TSGH Time of birth: 20141024 22: 05 Fetal distress: mild, Meconium stain: mild Apgar score: 1’(7), 5’(9) 產房急救: O 2 support HEPATITIS B IMMUNOGLOBULIN+ HEPATITIS B Vaccine
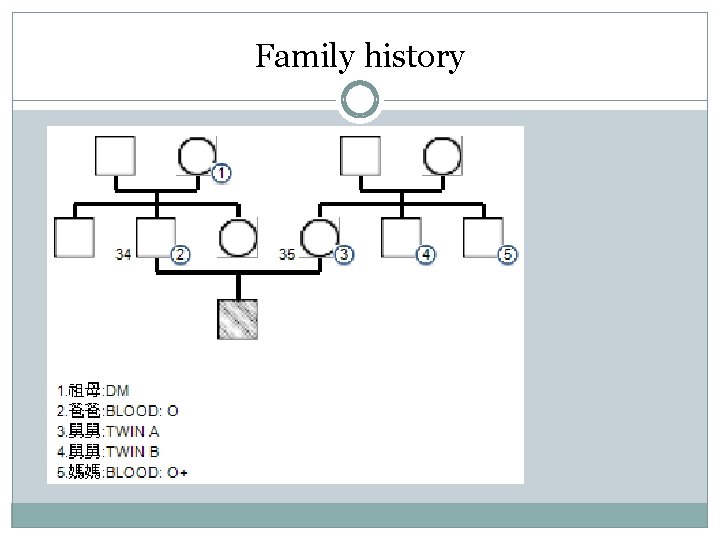
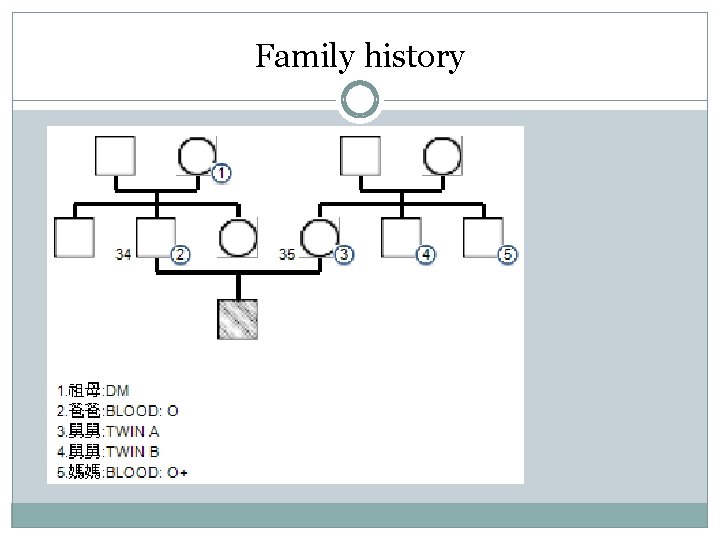
Family history
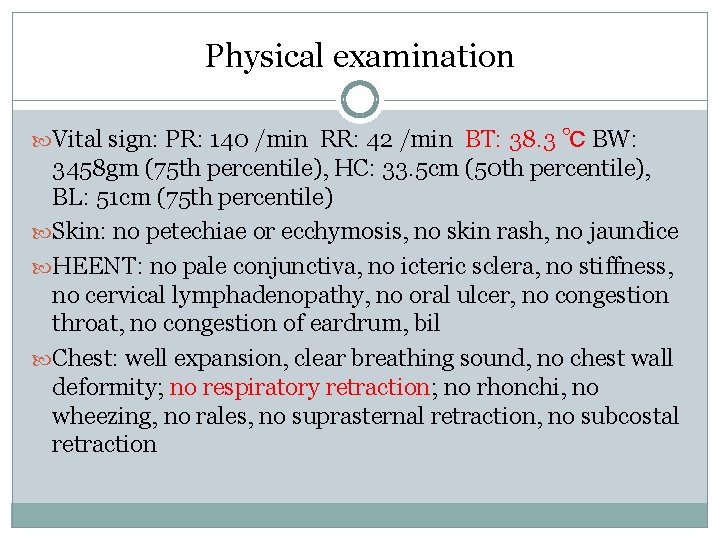
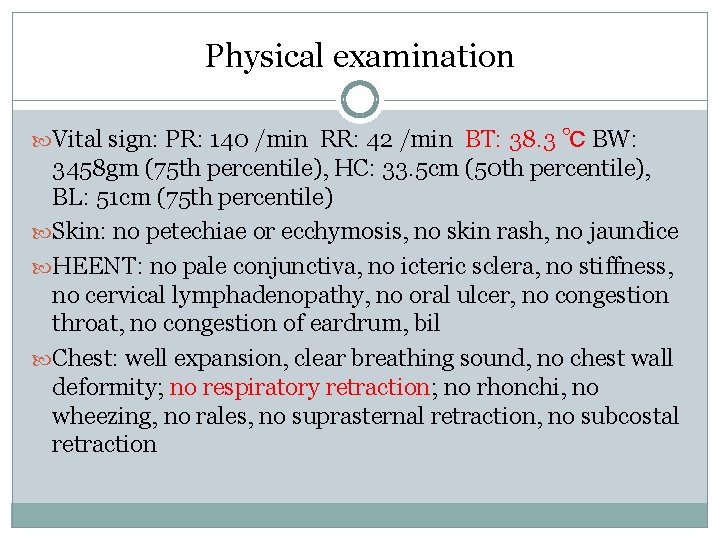
Physical examination Vital sign: PR: 140 /min RR: 42 /min BT: 38. 3 ℃ BW: 3458 gm (75 th percentile), HC: 33. 5 cm (50 th percentile), BL: 51 cm (75 th percentile) Skin: no petechiae or ecchymosis, no skin rash, no jaundice HEENT: no pale conjunctiva, no icteric sclera, no stiffness, no cervical lymphadenopathy, no oral ulcer, no congestion throat, no congestion of eardrum, bil Chest: well expansion, clear breathing sound, no chest wall deformity; no respiratory retraction; no rhonchi, no wheezing, no rales, no suprasternal retraction, no subcostal retraction
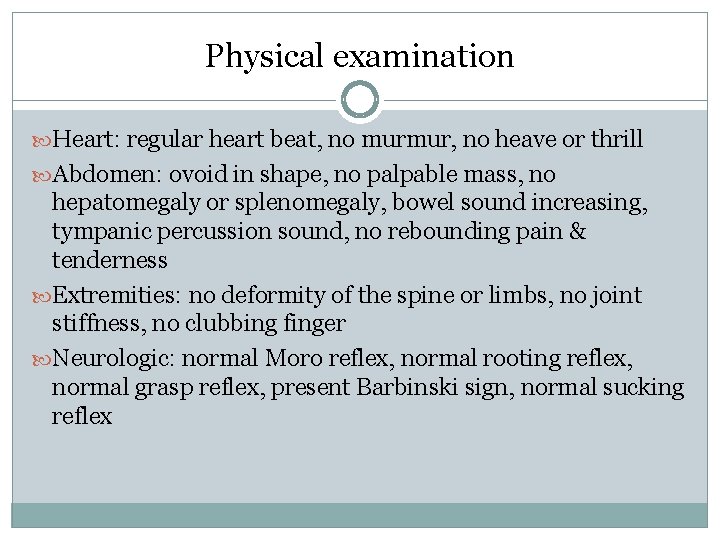
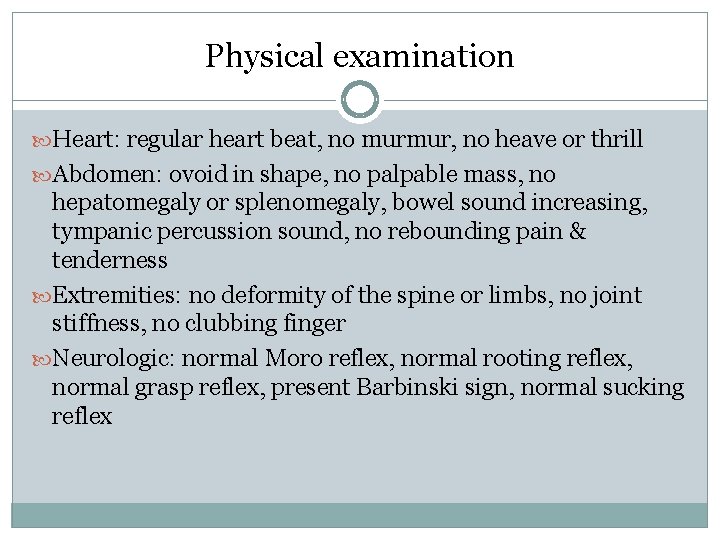
Physical examination Heart: regular heart beat, no murmur, no heave or thrill Abdomen: ovoid in shape, no palpable mass, no hepatomegaly or splenomegaly, bowel sound increasing, tympanic percussion sound, no rebounding pain & tenderness Extremities: no deformity of the spine or limbs, no joint stiffness, no clubbing finger Neurologic: normal Moro reflex, normal rooting reflex, normal grasp reflex, present Barbinski sign, normal sucking reflex
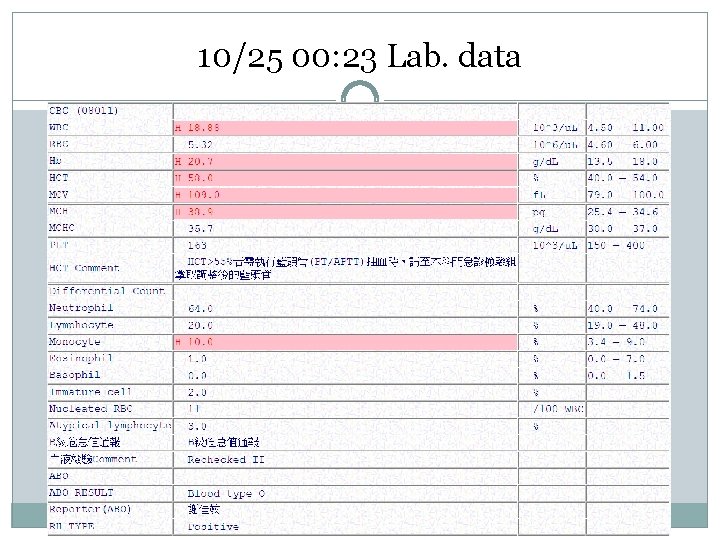
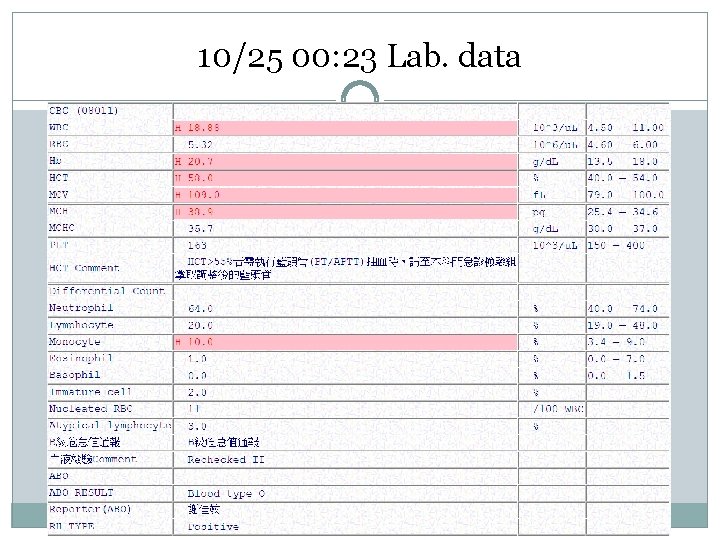
10/25 00: 23 Lab. data
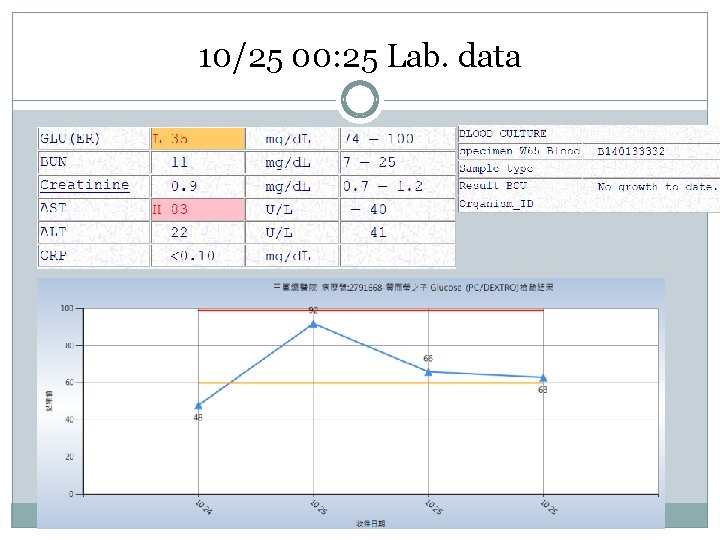
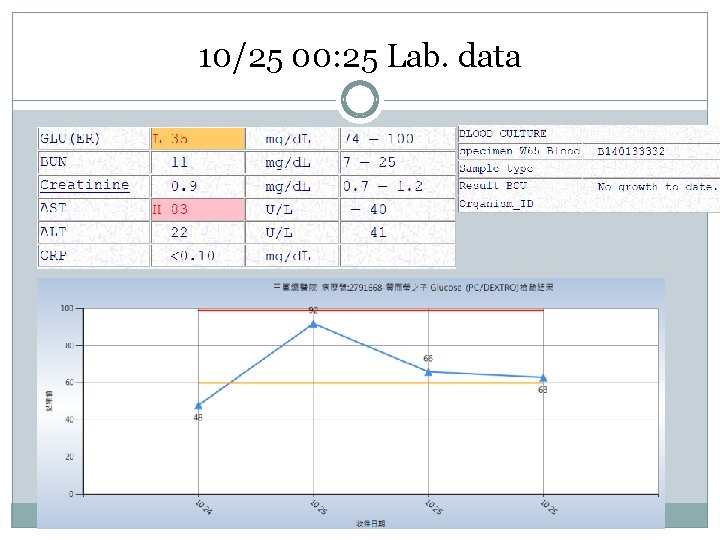
10/25 00: 25 Lab. data
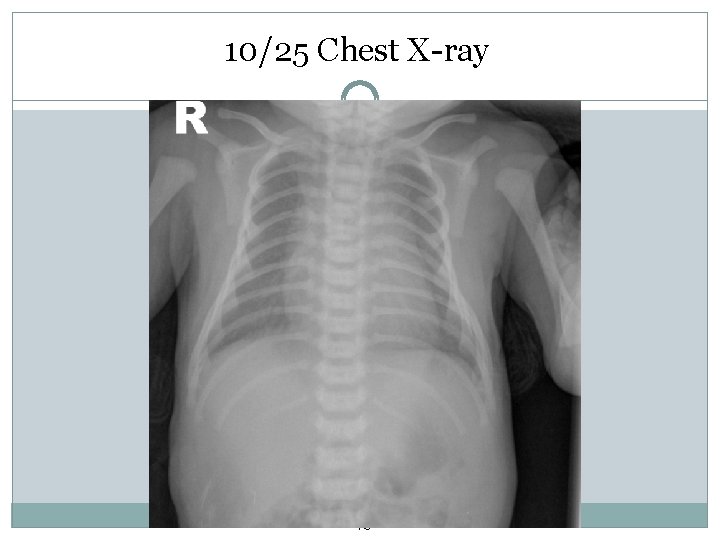
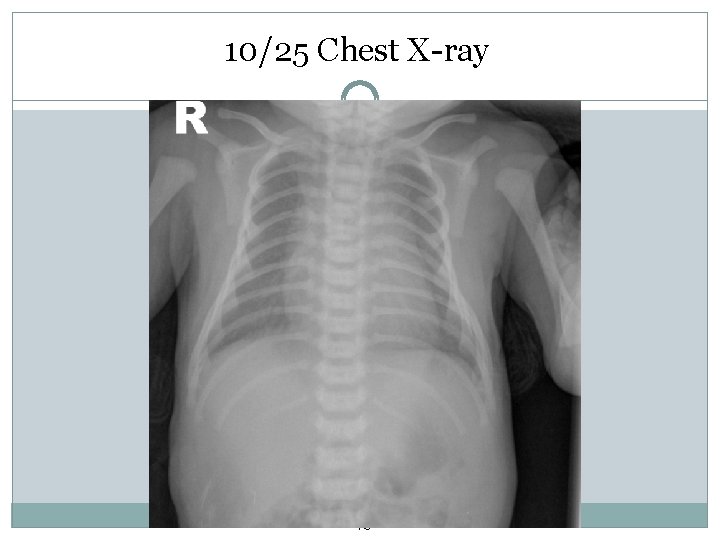
10/25 Chest X-ray 13
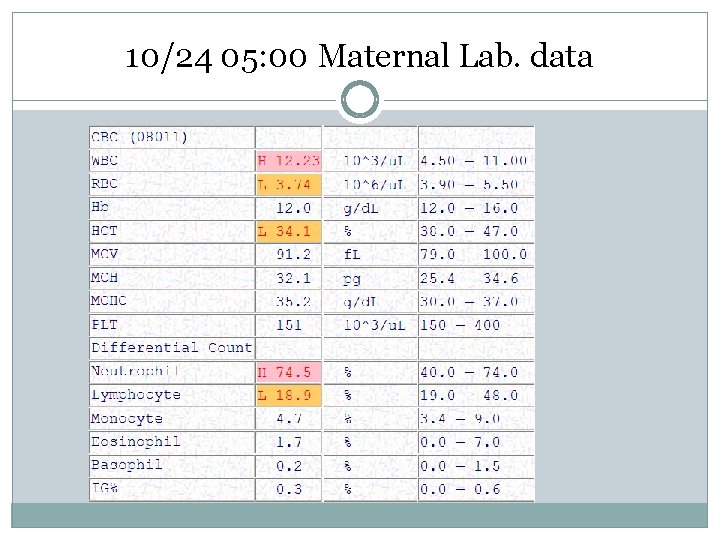
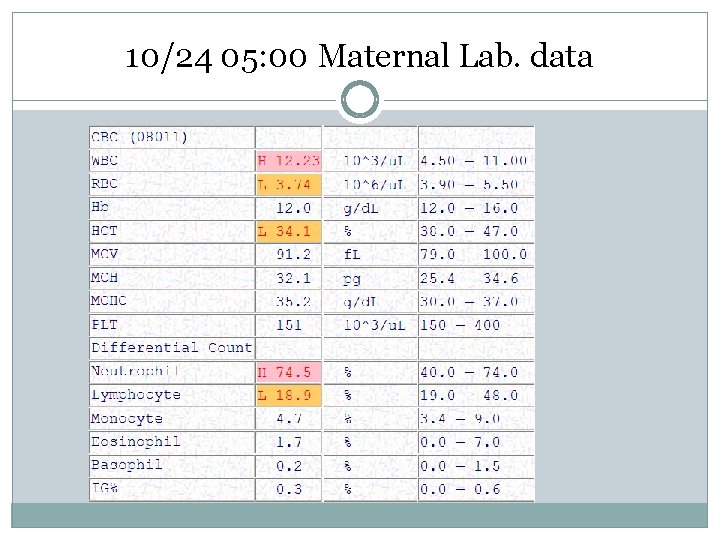
10/24 05: 00 Maternal Lab. data
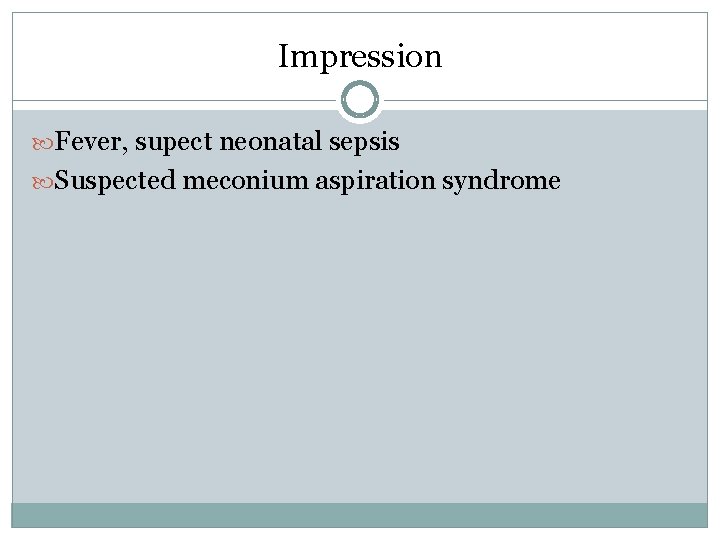
Impression Fever, supect neonatal sepsis Suspected meconium aspiration syndrome
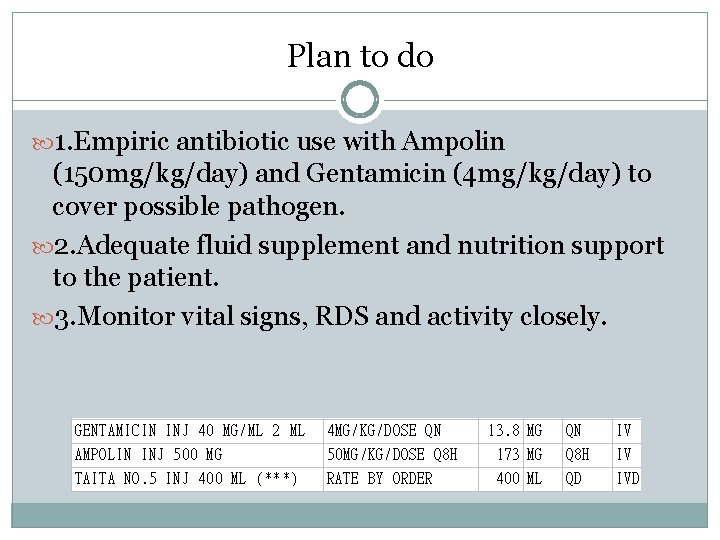
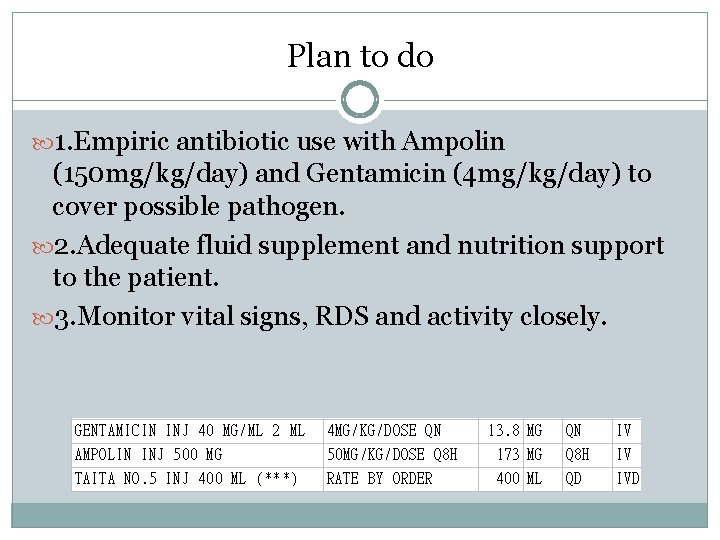
Plan to do 1. Empiric antibiotic use with Ampolin (150 mg/kg/day) and Gentamicin (4 mg/kg/day) to cover possible pathogen. 2. Adequate fluid supplement and nutrition support to the patient. 3. Monitor vital signs, RDS and activity closely.
Definition rectal temperature ≥ 38ºC (100. 4ºF) 2. Vaccinations and bundling may affect body temperature ~~ a fever >38. 5ºC (101ºF) should not be attributed to bundling regardless of the manner taken 1.
Immunity Immunologic competence improves steadily in the first 3 months of life more susceptible to serious bacterial infection (Pneumococcus and Hemophilus influenza type b)
Etiology-virus Viral infection : the most common cause 1. vertical transmission 2. family members and hospital personnel Pathogens 1. Herpes simplex 2. Varicella 3. Enteroviruses 4. Influenza virus 5. Adenoviruses 6. Respiratory syncytial virus
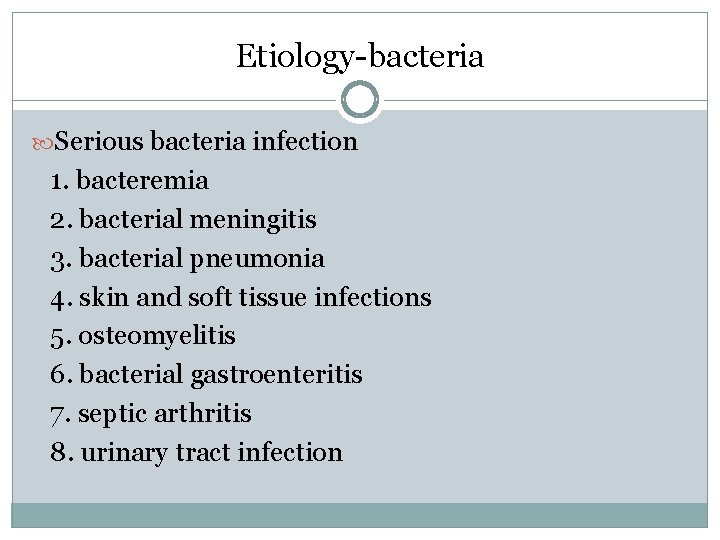
Etiology-bacteria Serious bacteria infection 1. bacteremia 2. bacterial meningitis 3. bacterial pneumonia 4. skin and soft tissue infections 5. osteomyelitis 6. bacterial gastroenteritis 7. septic arthritis 8. urinary tract infection
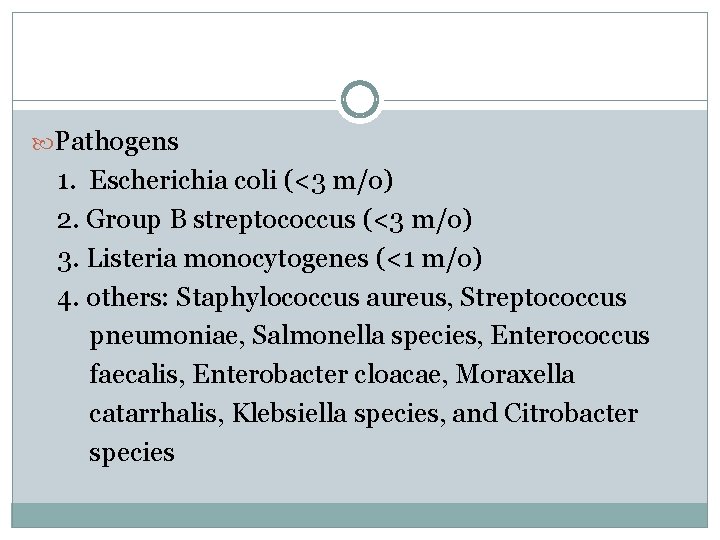
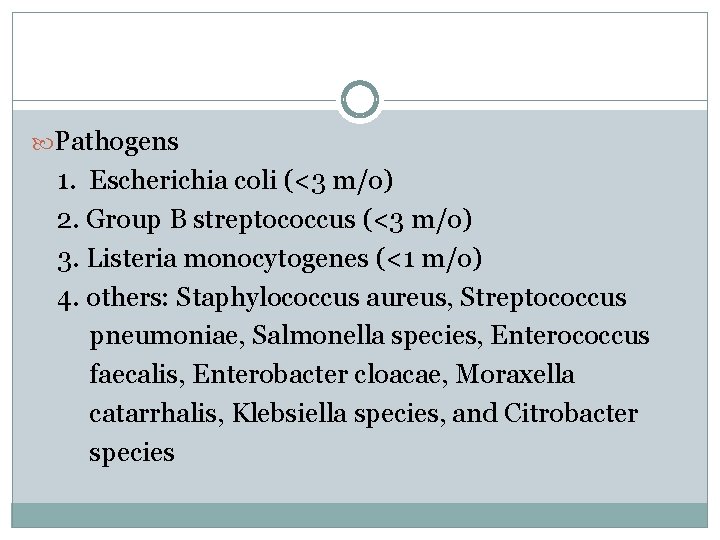
Pathogens 1. Escherichia coli (<3 m/o) 2. Group B streptococcus (<3 m/o) 3. Listeria monocytogenes (<1 m/o) 4. others: Staphylococcus aureus, Streptococcus pneumoniae, Salmonella species, Enterococcus faecalis, Enterobacter cloacae, Moraxella catarrhalis, Klebsiella species, and Citrobacter species
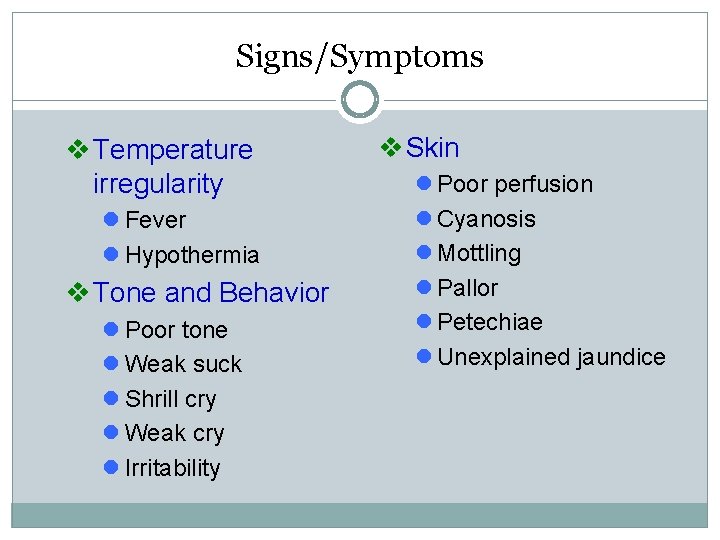
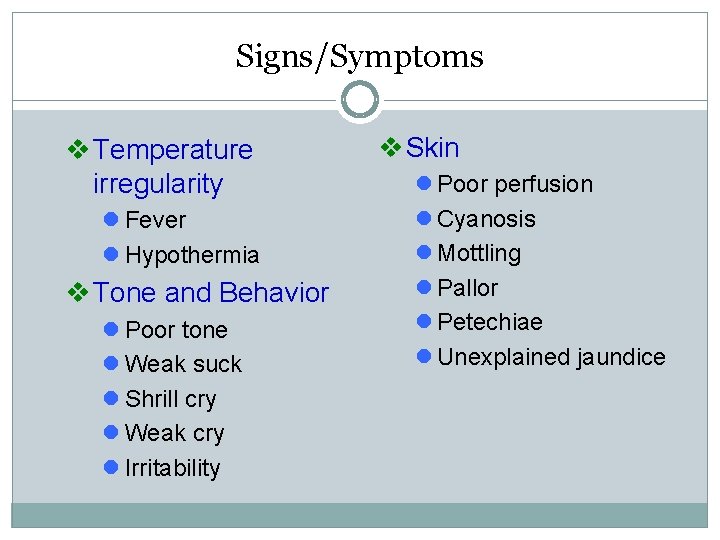
Signs/Symptoms v Temperature irregularity l Fever l Hypothermia v Tone and Behavior l Poor tone l Weak suck l Shrill cry l Weak cry l Irritability v Skin l Poor perfusion l Cyanosis l Mottling l Pallor l Petechiae l Unexplained jaundice
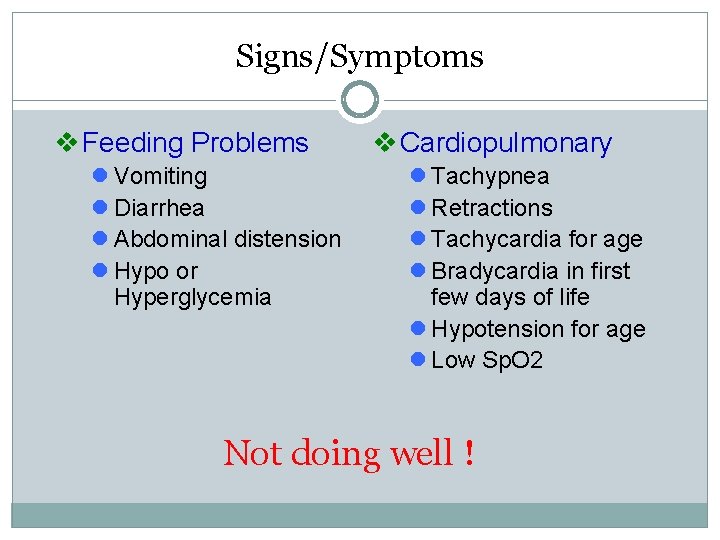
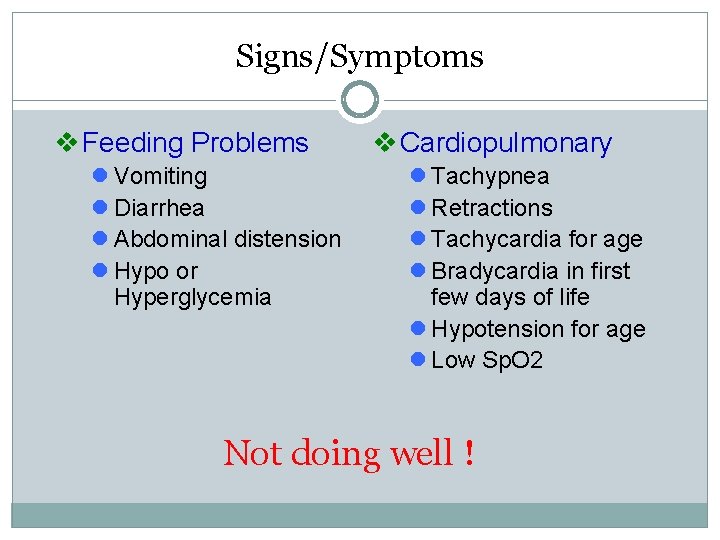
Signs/Symptoms v Feeding Problems l Vomiting l Diarrhea l Abdominal distension l Hypo or Hyperglycemia v Cardiopulmonary l Tachypnea l Retractions l Tachycardia for age l Bradycardia in first few days of life l Hypotension for age l Low Sp. O 2 Not doing well !
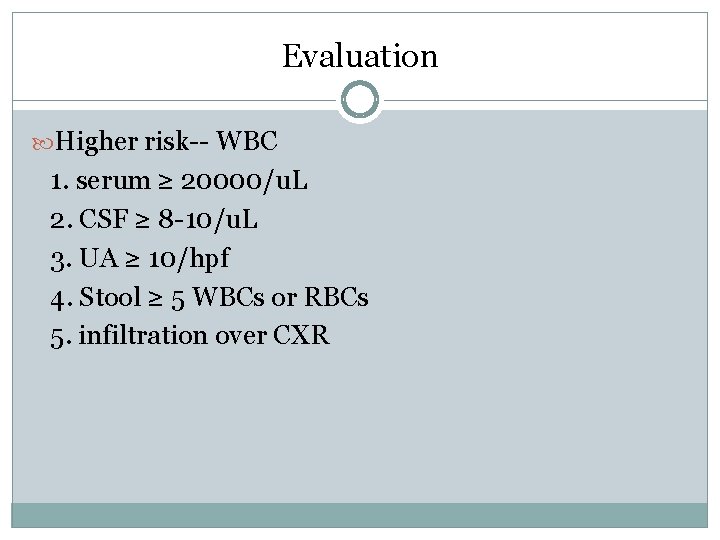
Evaluation Higher risk-- WBC 1. serum ≥ 20000/u. L 2. CSF ≥ 8 -10/u. L 3. UA ≥ 10/hpf 4. Stool ≥ 5 WBCs or RBCs 5. infiltration over CXR
Sepsis Work-Up Blood cultures Confirms sepsis Urine cultures Don’t need in infants <24 hours old because UTIs are exceedingly rare in this age group Lumbar puncture Suspect Meningitis Others: Tracheal aspirates, tapping for pleural effusion/ascites, …. etc.
Other studies CBC/DCs CRP CXR Obtain in infants with respiratory symptoms Renal ultrasound or VCUG in infants with accompanying UTI
Maternal Studies Examination of placenta and fetal membranes for evidence of chorioamnionitis
Management Neonates should be considered high risk! -> a complete sepsis evaluation with hospital admission are warranted regardless of clinical picture and laboratory results Antibiotics 1. ampicillin and gentamicin 2. ampicillin and cefotaxin (meningitis) 3. vancomycin and gentamicin/cefotaxin (nosocominal infection)
Thanks for your attention!