Neonatal End of Life Care Pathway Background to
Neonatal End of Life Care Pathway
Background to project Neonatal Toolkit (DOH, 2009) Principle 3: Care of the baby & family experience Principle 5: Professional competence, Education & Training
Benchmarks Benchmark tool adapted with permission of the Northwest Regional Benchmarking Group Best practice statement‘Members of the MDT are enabled to support families and facilitate individualised Palliative and Bereavement Care. ’
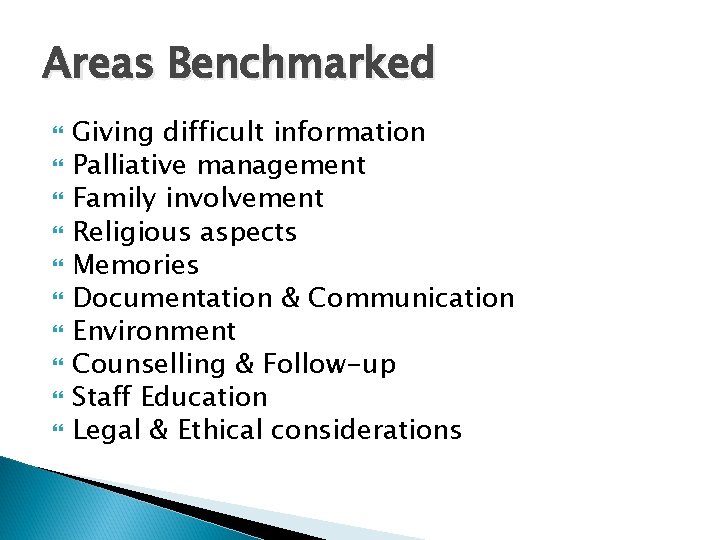
Areas Benchmarked Giving difficult information Palliative management Family involvement Religious aspects Memories Documentation & Communication Environment Counselling & Follow-up Staff Education Legal & Ethical considerations
Areas of concern MDT Communication between other Hospitals/NNU’s Follow-up Appointments Staff Education & Support
Action plan Improve Staff Education & Support across the Network Improve Documentation & Communication by Developing a Neonatal End of Life Care Pathway Repeat Benchmark
Staff Bereavement Training Staff Induction Alder Centre To date each NNU has had greater than 40% staff attend Bereavement training at the Alder Centre
Unit Based Actions - BVH Timely De-briefing sessions Individual MDT Case Reviews Clinical Supervision Improved Staff Education Programme Improved Facilities for Families Development of Pathway
Development of Pathway – Aims Greater Involvement of Parents in decision making Improved Documentation & Communication between members of MDT & other NNU’s Reduction in paperwork; more time spent supporting & caring for family Aid to guide & support staff caring for babies & families throughout end of life period
- Slides: 9