Neonatal Cyanosis and respiratory disorders 1 Neonatal cyanosis





- Slides: 56
Neonatal Cyanosis and respiratory disorders 1
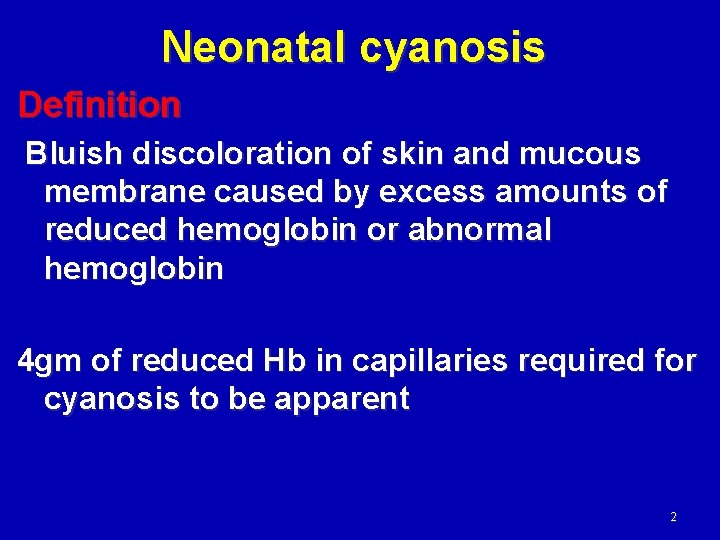
Neonatal cyanosis Definition Bluish discoloration of skin and mucous membrane caused by excess amounts of reduced hemoglobin or abnormal hemoglobin 4 gm of reduced Hb in capillaries required for cyanosis to be apparent 2
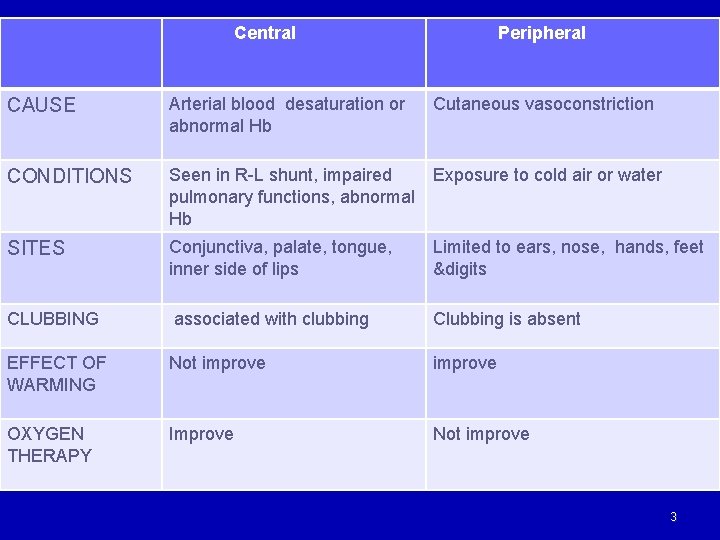
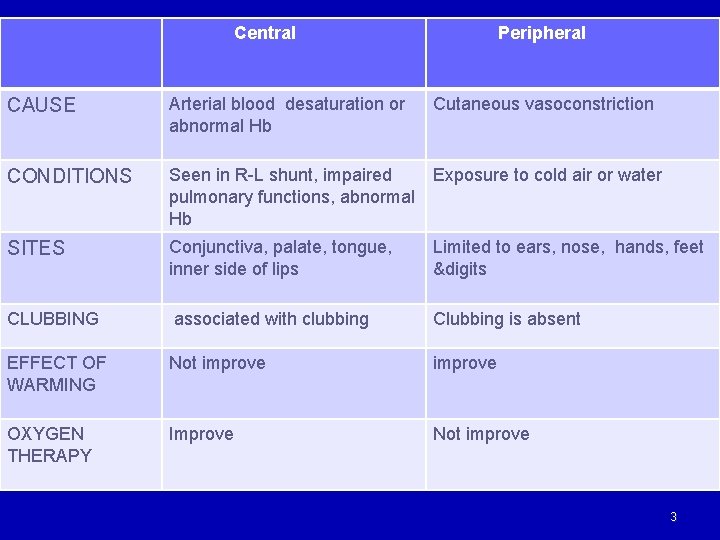
Central Peripheral CAUSE Arterial blood desaturation or abnormal Hb Cutaneous vasoconstriction CONDITIONS Seen in R-L shunt, impaired Exposure to cold air or water pulmonary functions, abnormal Hb SITES Conjunctiva, palate, tongue, inner side of lips Limited to ears, nose, hands, feet &digits CLUBBING associated with clubbing Clubbing is absent EFFECT OF WARMING Not improve OXYGEN THERAPY Improve Not improve 3
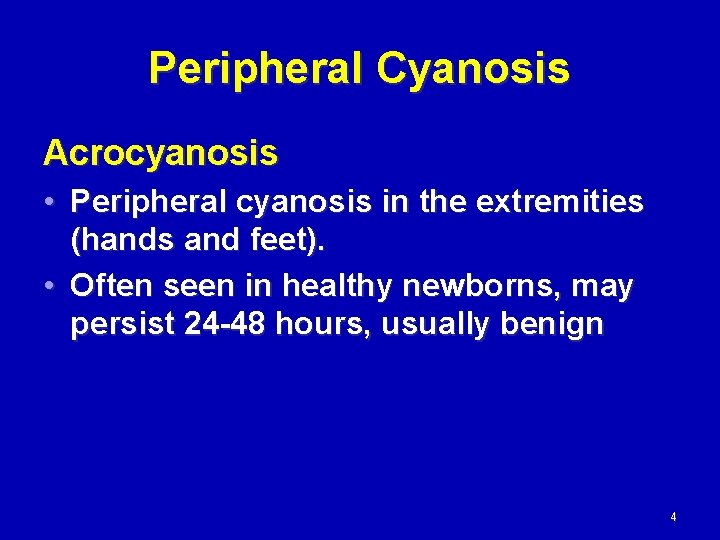
Peripheral Cyanosis Acrocyanosis • Peripheral cyanosis in the extremities (hands and feet). • Often seen in healthy newborns, may persist 24 -48 hours, usually benign 4
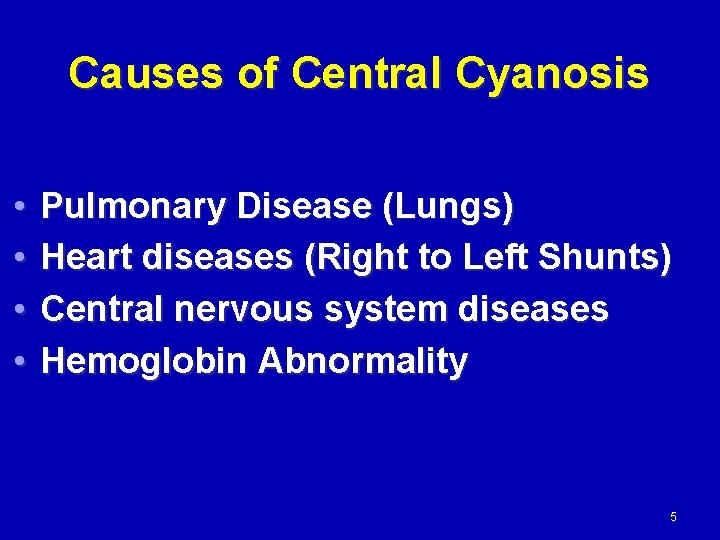
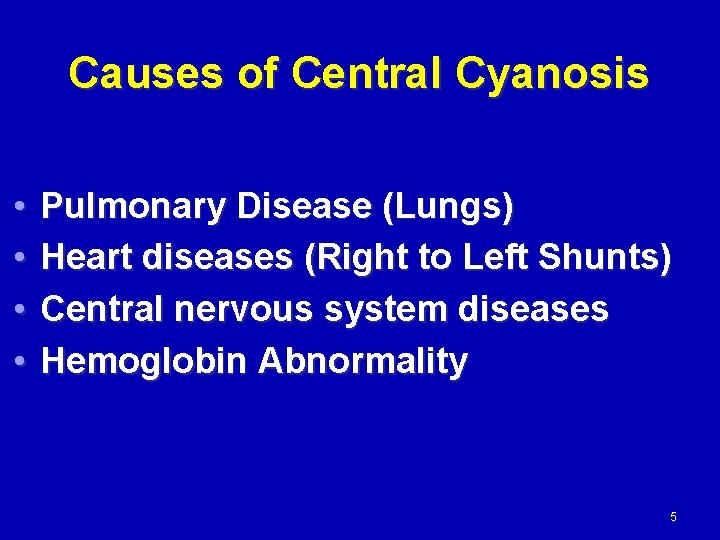
Causes of Central Cyanosis • • Pulmonary Disease (Lungs) Heart diseases (Right to Left Shunts) Central nervous system diseases Hemoglobin Abnormality 5
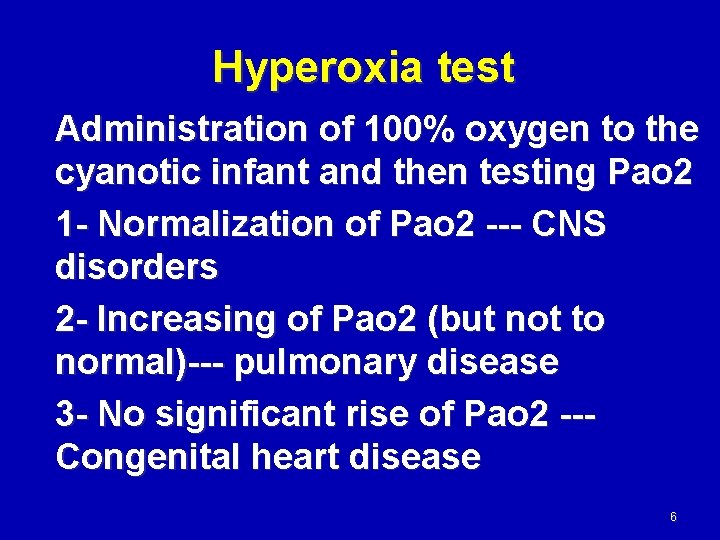
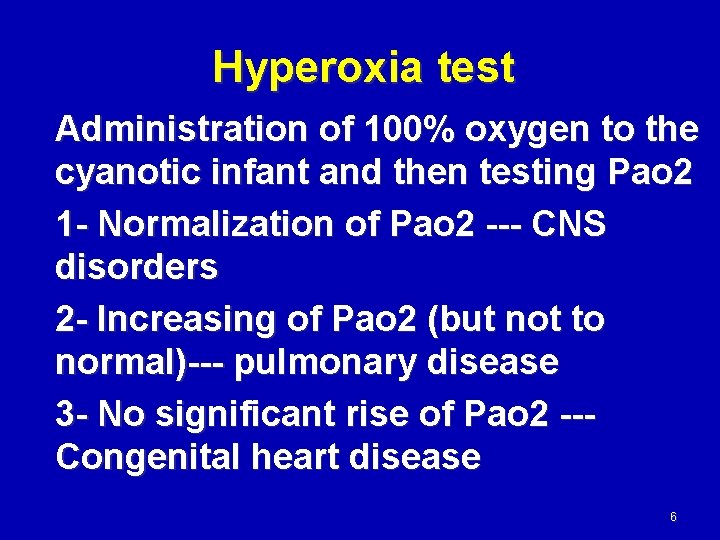
Hyperoxia test Administration of 100% oxygen to the cyanotic infant and then testing Pao 2 1 - Normalization of Pao 2 --- CNS disorders 2 - Increasing of Pao 2 (but not to normal)--- pulmonary disease 3 - No significant rise of Pao 2 --Congenital heart disease 6

7
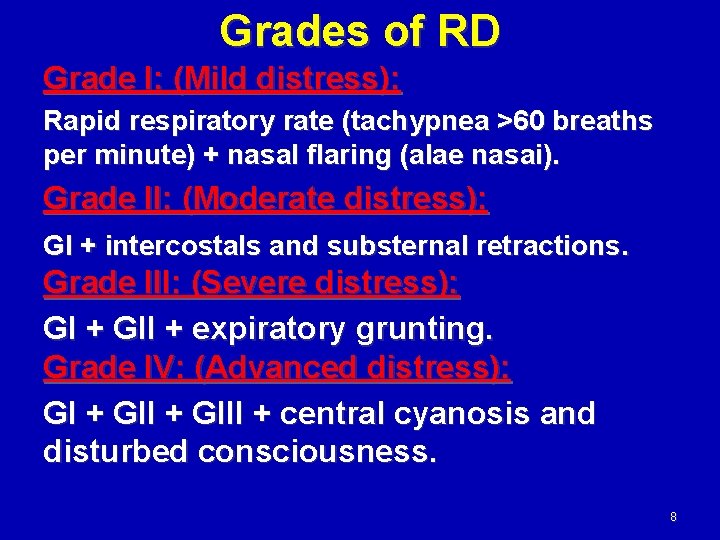
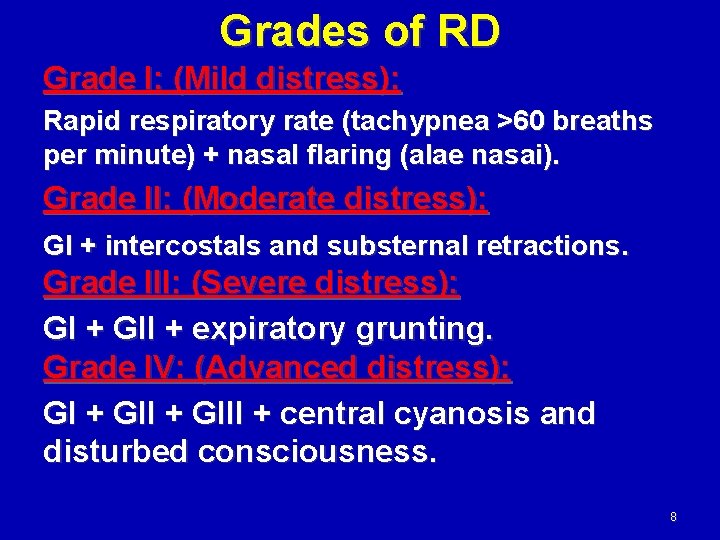
Grades of RD Grade I: (Mild distress): Rapid respiratory rate (tachypnea >60 breaths per minute) + nasal flaring (alae nasai). Grade II: (Moderate distress): GI + intercostals and substernal retractions. Grade III: (Severe distress): GI + GII + expiratory grunting. Grade IV: (Advanced distress): GI + GIII + central cyanosis and disturbed consciousness. 8
9
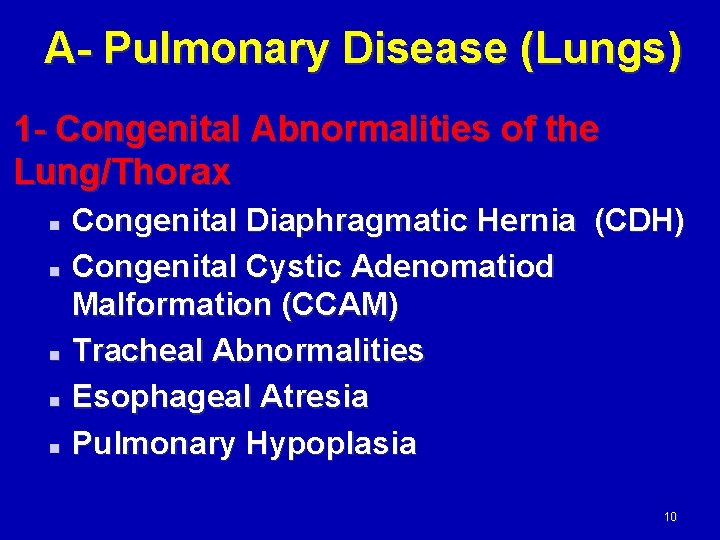
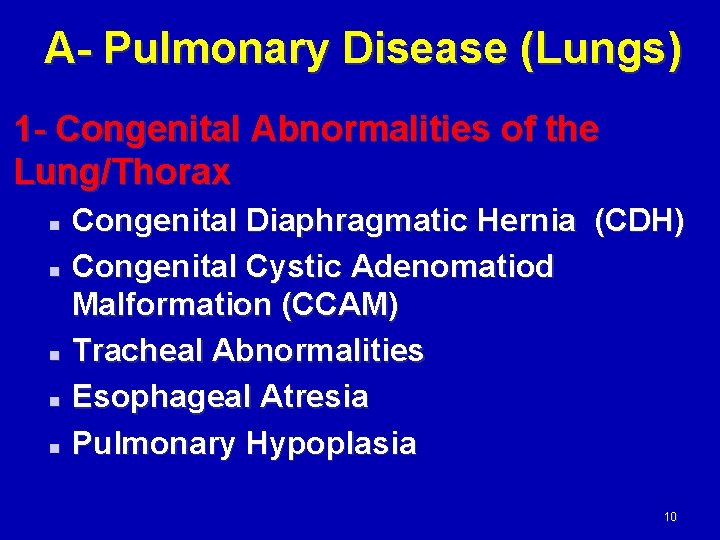
A- Pulmonary Disease (Lungs) 1 - Congenital Abnormalities of the Lung/Thorax Congenital Diaphragmatic Hernia (CDH) n Congenital Cystic Adenomatiod Malformation (CCAM) n Tracheal Abnormalities n Esophageal Atresia n Pulmonary Hypoplasia n 10
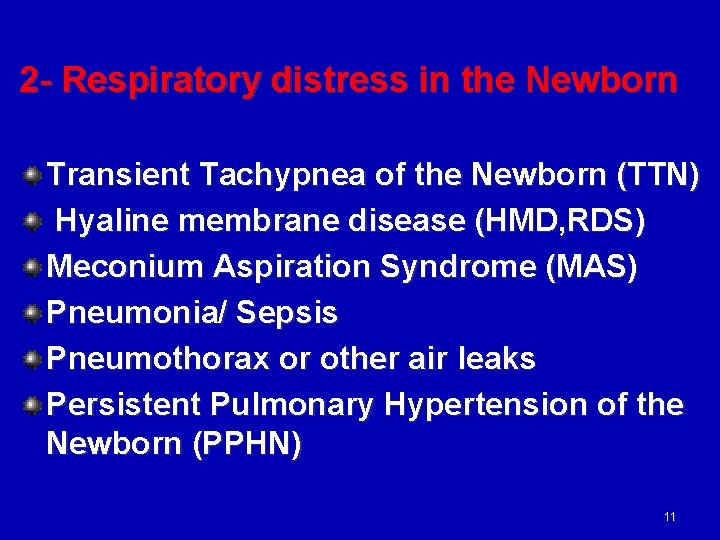
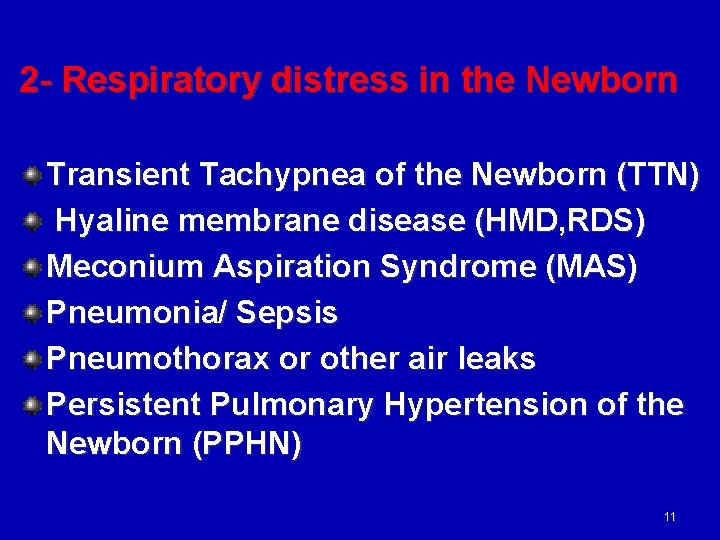
2 - Respiratory distress in the Newborn Transient Tachypnea of the Newborn (TTN) Hyaline membrane disease (HMD, RDS) Meconium Aspiration Syndrome (MAS) Pneumonia/ Sepsis Pneumothorax or other air leaks Persistent Pulmonary Hypertension of the Newborn (PPHN) 11
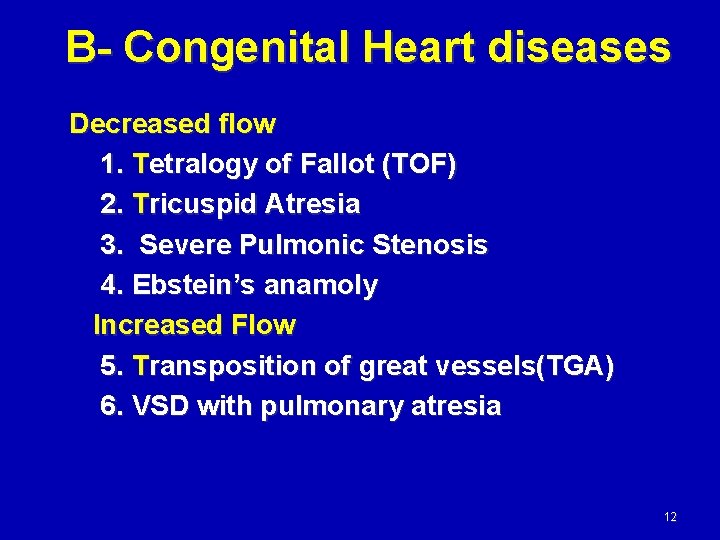
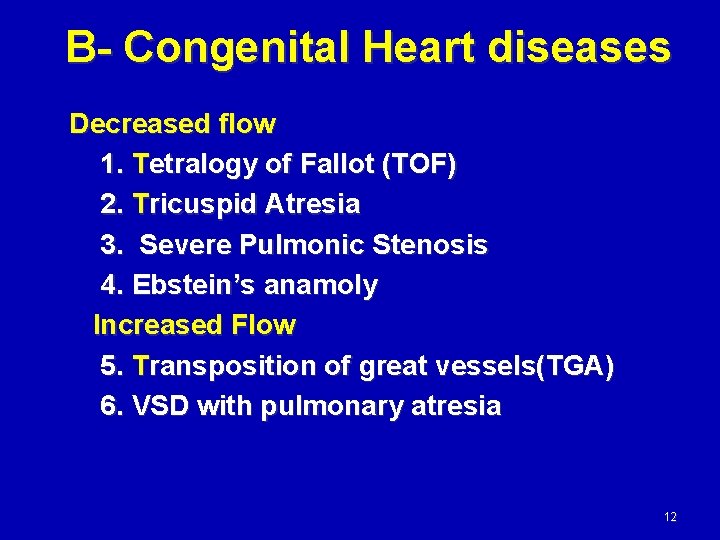
B- Congenital Heart diseases Decreased flow 1. Tetralogy of Fallot (TOF) 2. Tricuspid Atresia 3. Severe Pulmonic Stenosis 4. Ebstein’s anamoly Increased Flow 5. Transposition of great vessels(TGA) 6. VSD with pulmonary atresia 12
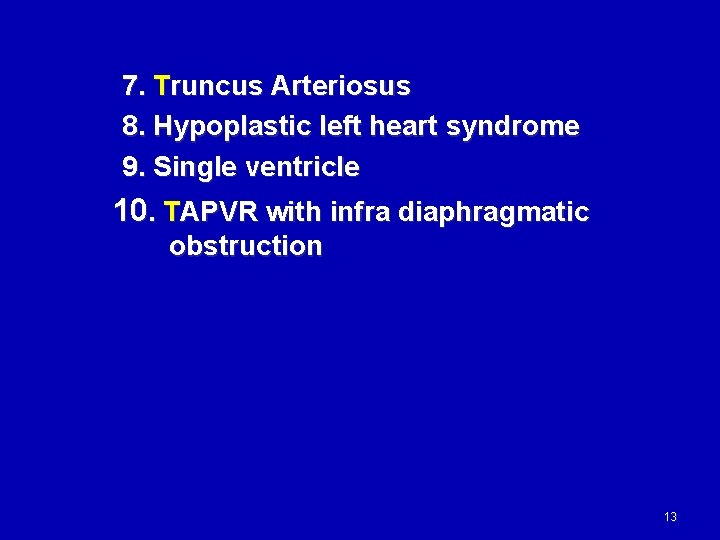
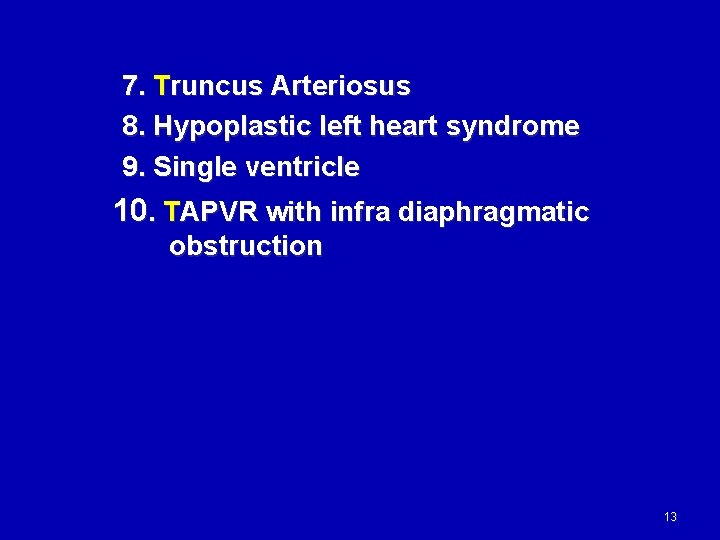
7. Truncus Arteriosus 8. Hypoplastic left heart syndrome 9. Single ventricle 10. TAPVR with infra diaphragmatic obstruction 13
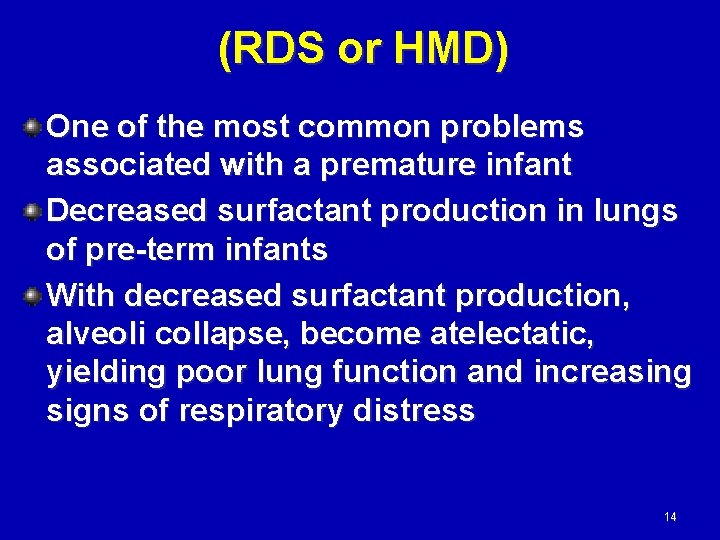
(RDS or HMD) One of the most common problems associated with a premature infant Decreased surfactant production in lungs of pre-term infants With decreased surfactant production, alveoli collapse, become atelectatic, yielding poor lung function and increasing signs of respiratory distress 14
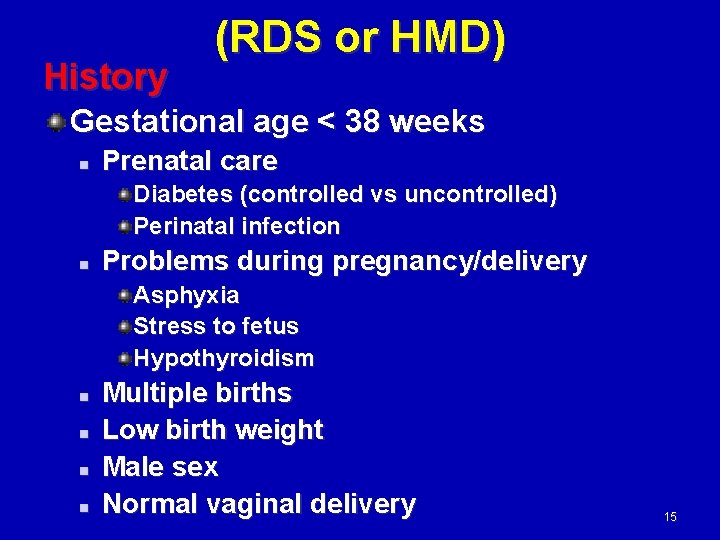
History (RDS or HMD) Gestational age < 38 weeks n Prenatal care Diabetes (controlled vs uncontrolled) Perinatal infection n Problems during pregnancy/delivery Asphyxia Stress to fetus Hypothyroidism n n Multiple births Low birth weight Male sex Normal vaginal delivery 15
(RDS or HMD) Symptoms usually appear 2 -6 hours after birth Disease peaks at 48 -72 hours Recovery usually occurs 5 -7 days after birth 16
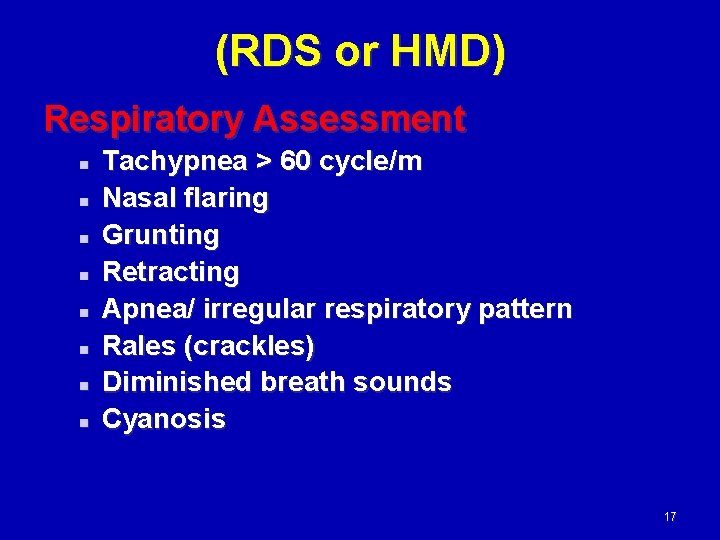
(RDS or HMD) Respiratory Assessment n n n n Tachypnea > 60 cycle/m Nasal flaring Grunting Retracting Apnea/ irregular respiratory pattern Rales (crackles) Diminished breath sounds Cyanosis 17
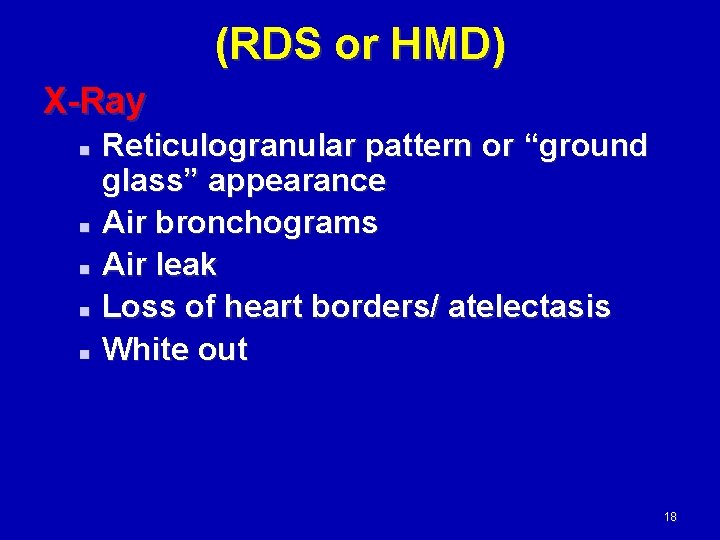
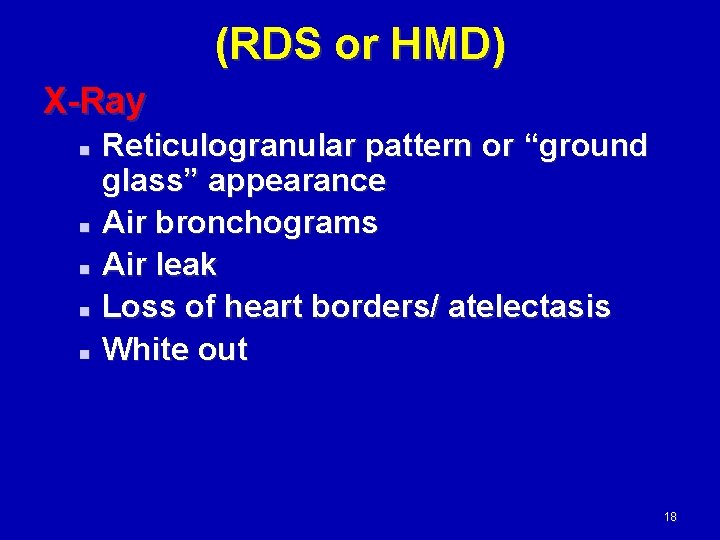
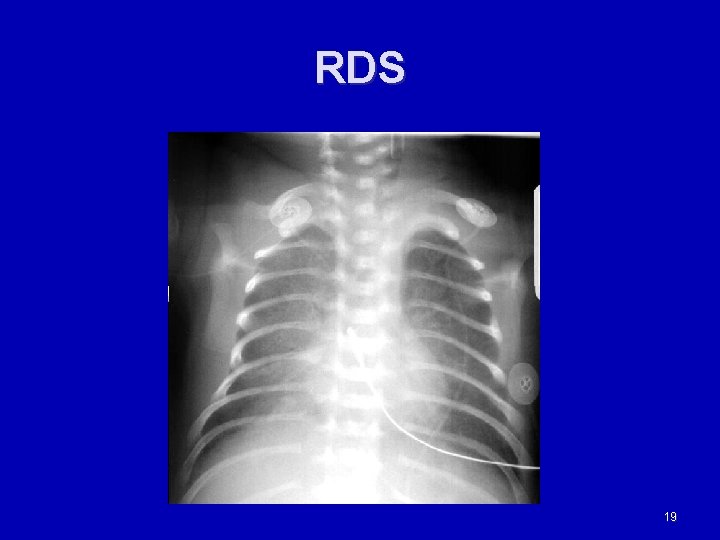
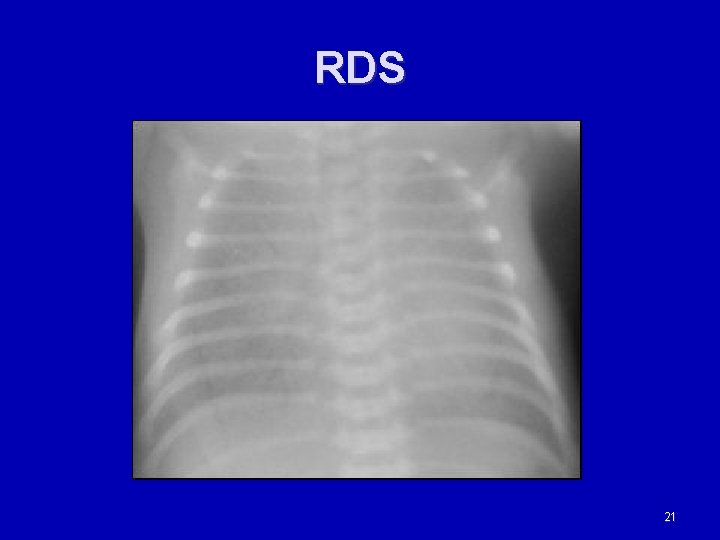
(RDS or HMD) X-Ray Reticulogranular pattern or “ground glass” appearance n Air bronchograms n Air leak n Loss of heart borders/ atelectasis n White out n 18
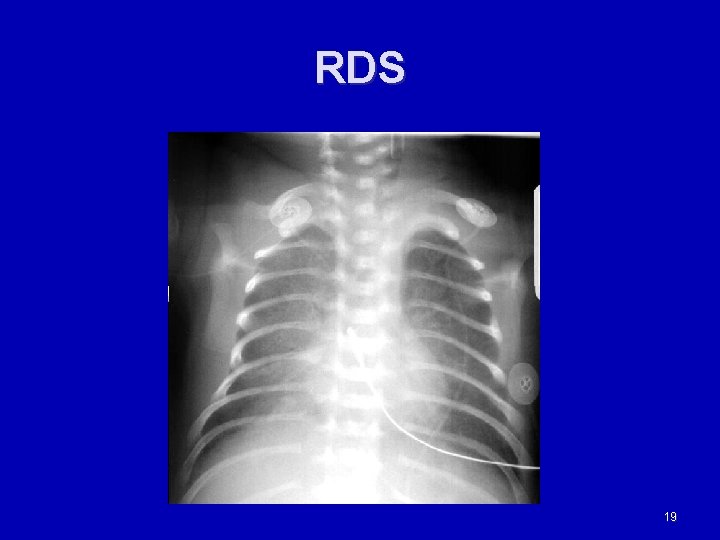
RDS 19

20
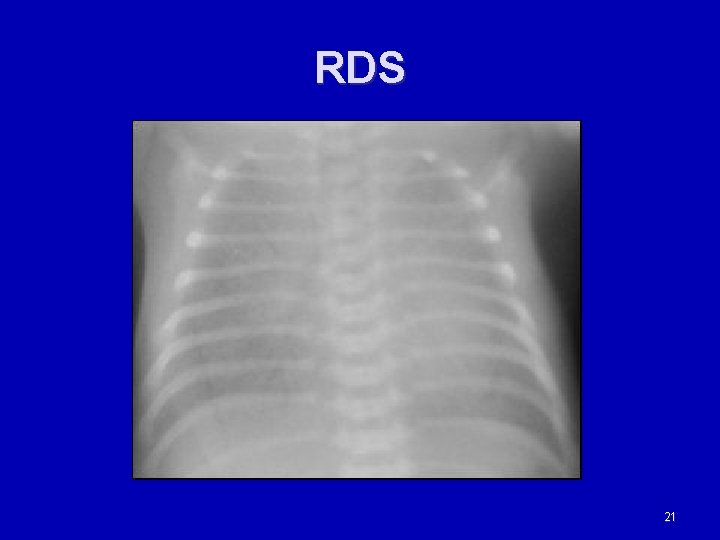
RDS 21
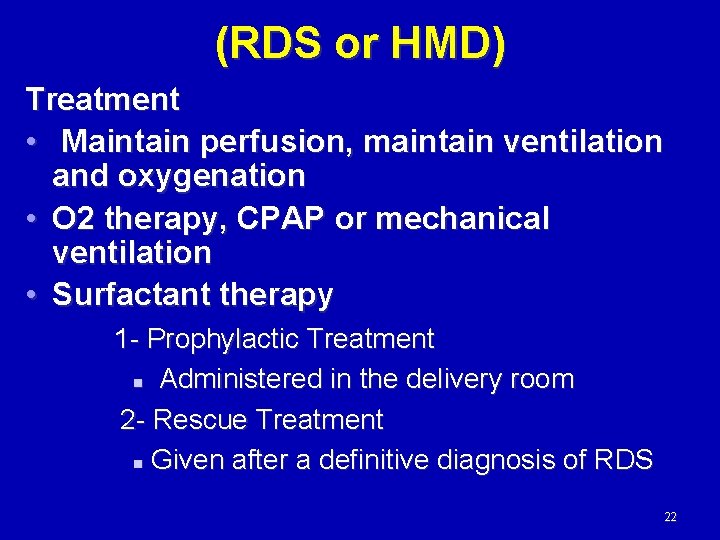
(RDS or HMD) Treatment • Maintain perfusion, maintain ventilation and oxygenation • O 2 therapy, CPAP or mechanical ventilation • Surfactant therapy 1 - Prophylactic Treatment n Administered in the delivery room 2 - Rescue Treatment n Given after a definitive diagnosis of RDS 22
(RDS or HMD) Prognosis is good once infant makes it past the peak (48 -72 hours) Complications possible are: Intracranial Bleeding BPD (Broncho pulmonary Dysplasia) PDA (Patent Ductus Arteriosus) 23
Transient Tachypnea of the Newborn (TTN) • Most common diagnosis of respiratory distress in the newborn • Common in full term infants • Due to delaying in reabsorption of fetal lung fluid which eventually will clear over several hours to days • Most often seen at birth or shortly afterbirth • Common with C-Section delivery • Maternal anesthesia during labor • Maternal fluid administration 24
Clinical picture of TTN Respiratory Assessment Tachypnea > 60 n Nasal flaring n Grunting n Retracting n Fine Rales n Cyanotic n 25
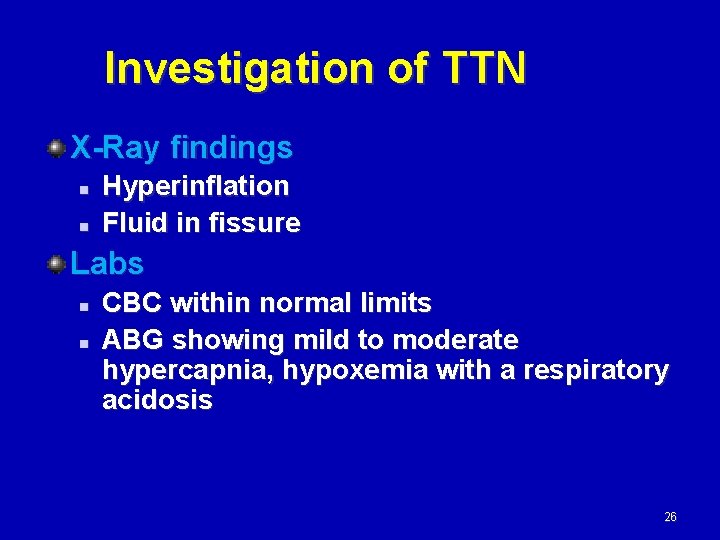
Investigation of TTN X-Ray findings n n Hyperinflation Fluid in fissure Labs n n CBC within normal limits ABG showing mild to moderate hypercapnia, hypoxemia with a respiratory acidosis 26

TTN 27
Treatment of TTN 1 -Supportive with IV fluids 2 - Oxygen therapy (nasal pronge or CPAP ) 3 - Nutritional support 28
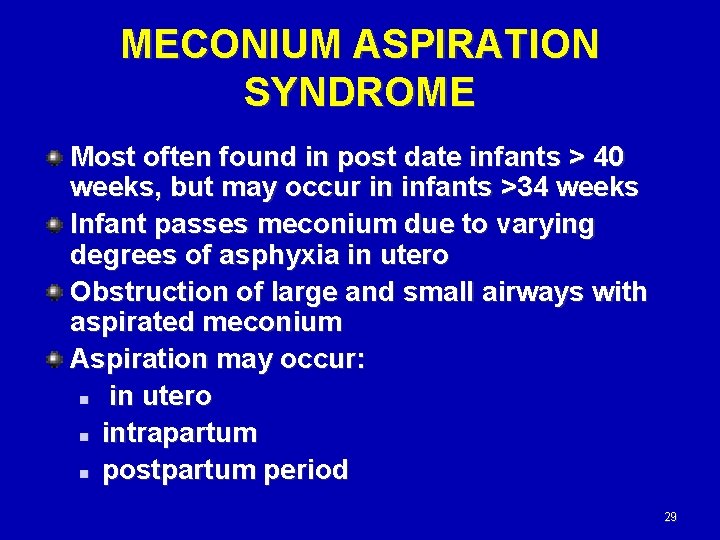
MECONIUM ASPIRATION SYNDROME Most often found in post date infants > 40 weeks, but may occur in infants >34 weeks Infant passes meconium due to varying degrees of asphyxia in utero Obstruction of large and small airways with aspirated meconium Aspiration may occur: n in utero n intrapartum n postpartum period 29
Clinical picture of MAS Respiratory Assessment n n n n Tachypnea Nasal flaring Grunting Retracting Apnea/ irregular respiratory pattern Decreased breath sounds/ wet/ rhonchi Cyanosis 30
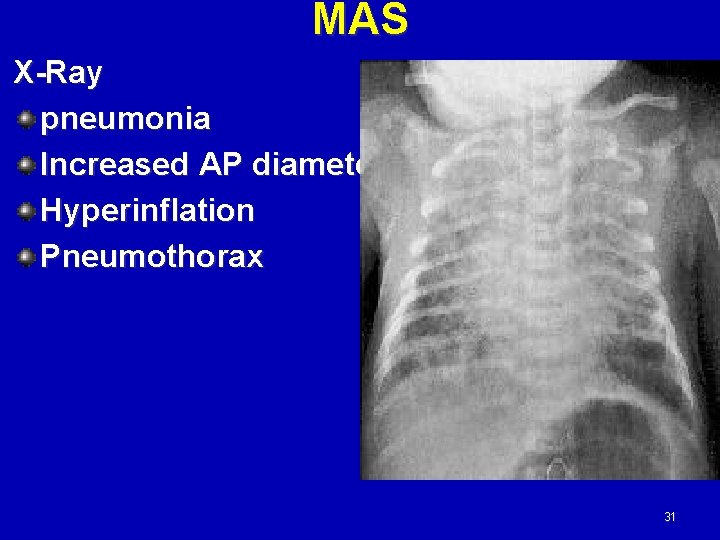
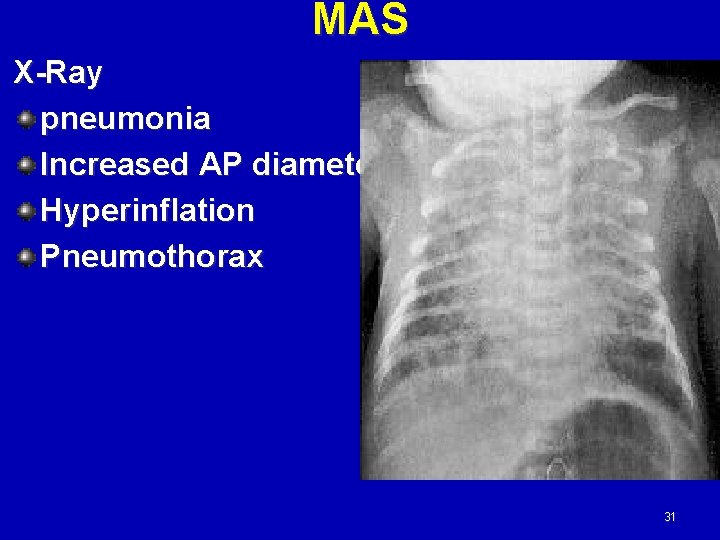
MAS X-Ray pneumonia Increased AP diameter Hyperinflation Pneumothorax 31
Treatment of MAS 1 - Good suctioning and physiotherapy 2 - Oxygen therapy --- no positive pressure by ambo bag for induced pneumothorax 3 - IV fluids 4 - Antibiotics for chemical pneumonitis 5 - Treatment of PPH 32
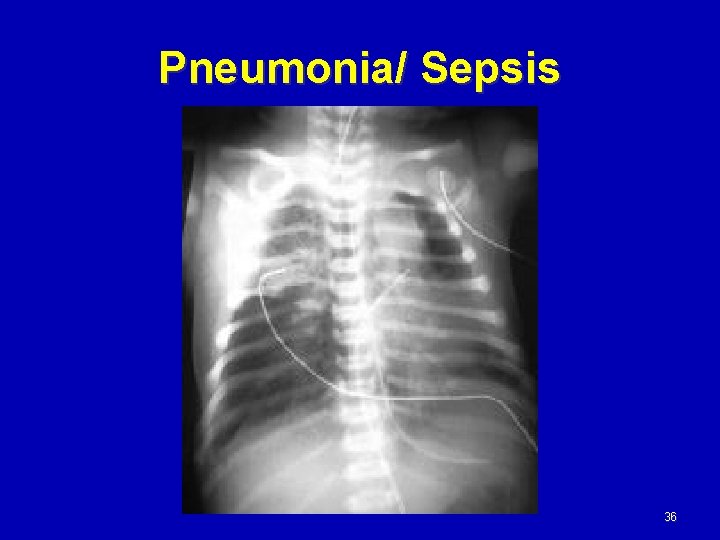
Pneumonia/ Sepsis Occurs frequently in newborns 3 types n Congenital Pneumonia n Intrapartum Pneumonia n Postnatal Pneumonia Most often seen with chorioamnionitis, prematurity and meconium aspiration 33
Causes of pneumonia Prematurity Prolonged rupture of membranes >18 hours Maternal temp > 38 C Foul smelling amniotic fluid Meconium aspiration 34
Clinical picture of pneumonia Tachypnea Apnea, irregular breathing pattern Grunting Retractions Nasal flaring Colorful secretions Rales, rhonchi Cyanosis 35
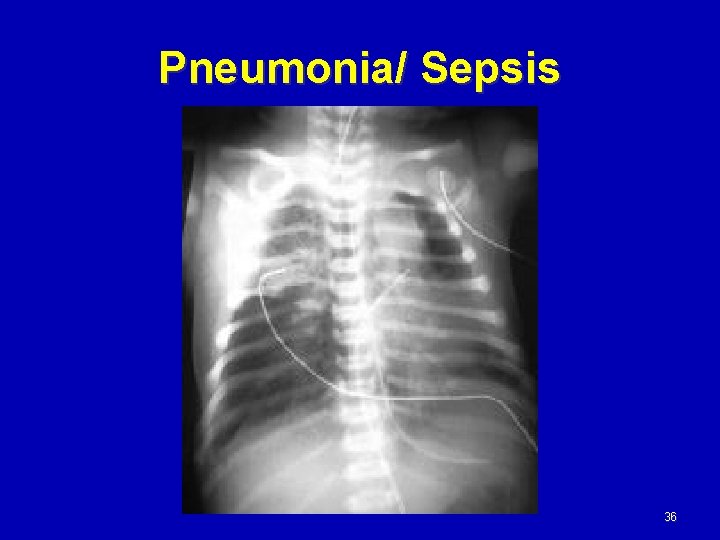
Pneumonia/ Sepsis 36
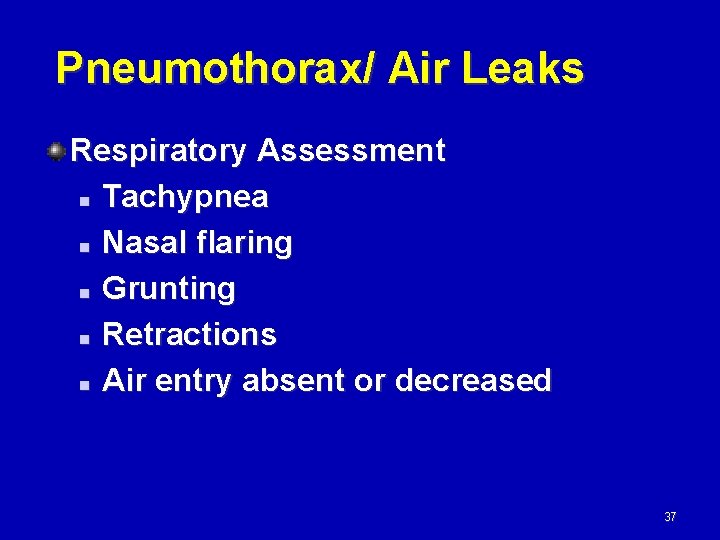
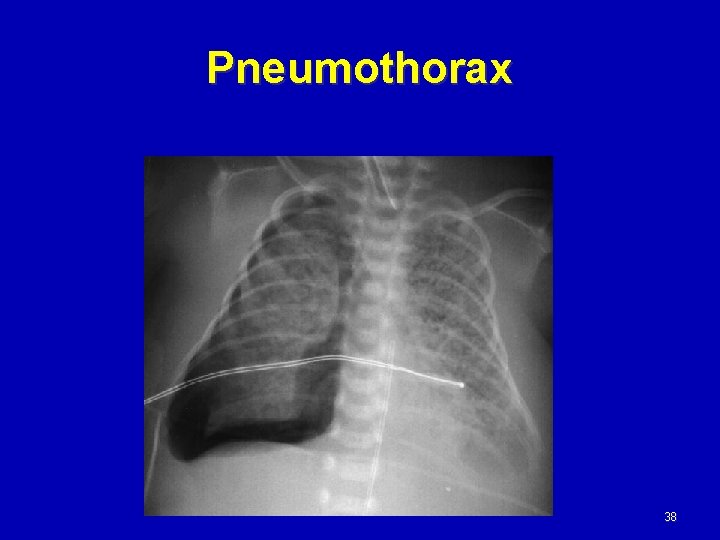
Pneumothorax/ Air Leaks Respiratory Assessment n Tachypnea n Nasal flaring n Grunting n Retractions n Air entry absent or decreased 37
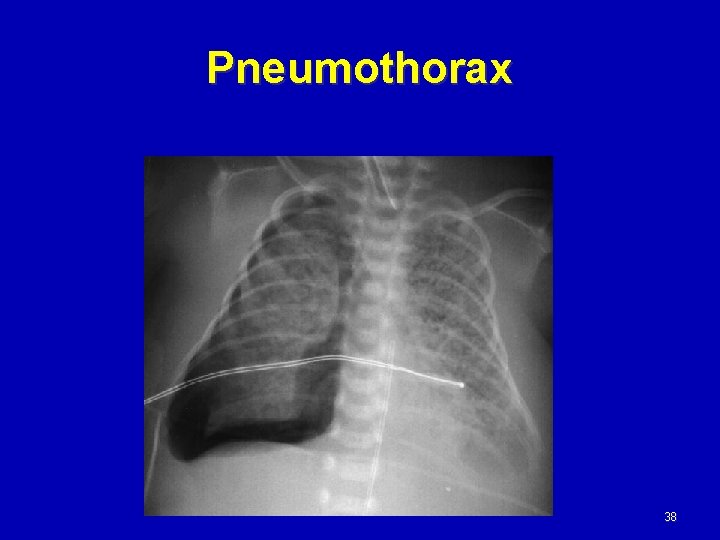
Pneumothorax 38
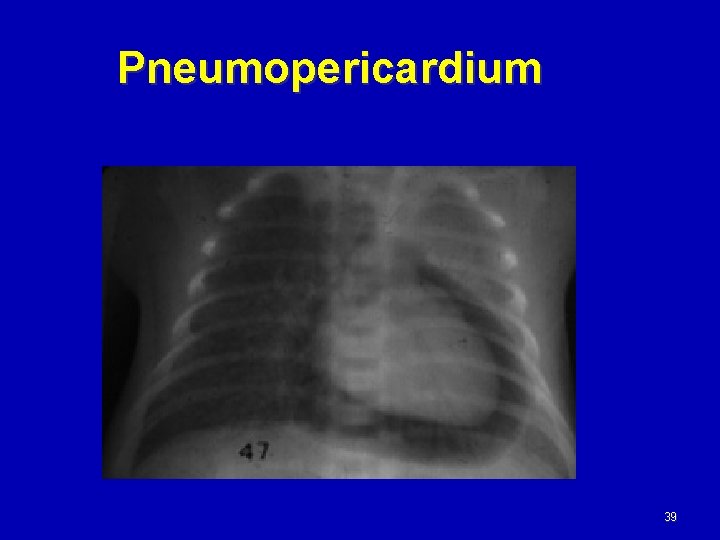
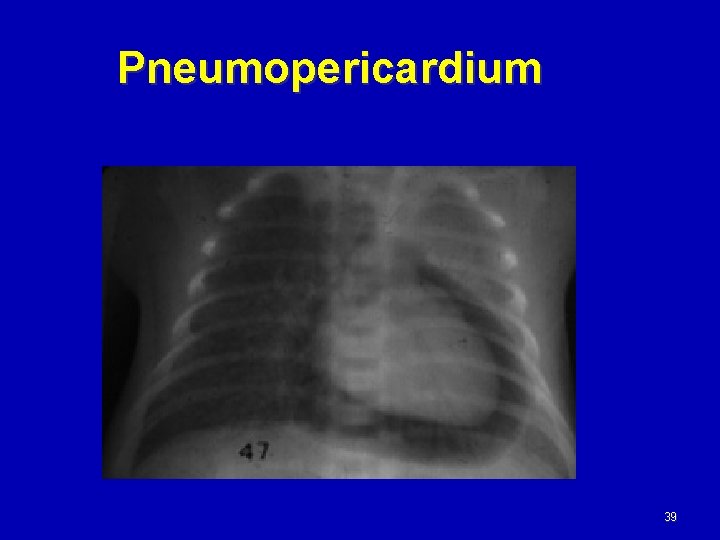
Pneumopericardium 39
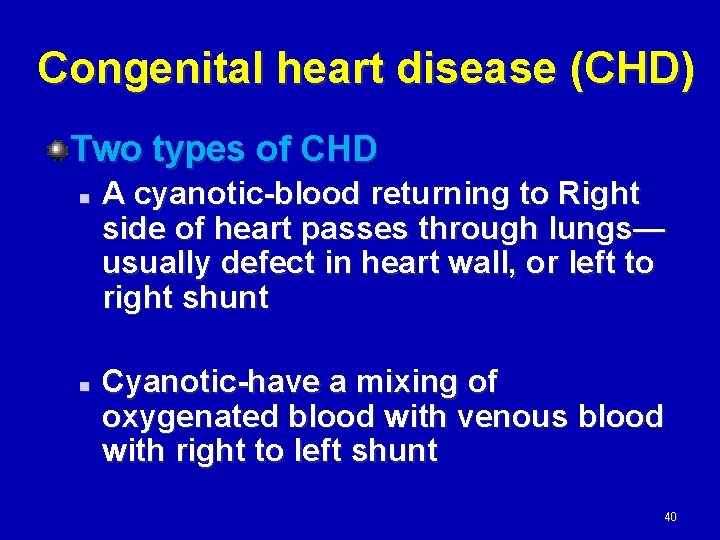
Congenital heart disease (CHD) Two types of CHD n n A cyanotic-blood returning to Right side of heart passes through lungs— usually defect in heart wall, or left to right shunt Cyanotic-have a mixing of oxygenated blood with venous blood with right to left shunt 40
CHD Clinical Assessment n HR Slow, fast, variable murmur n BP Check in all 4 extremities n n Pulses in all extremities Color Acyanotic -pink Cyanotic-blue 41
CHD Labs and Tests n n ABGs—dependent upon defect Lactic Acid Chest X-Ray n n Heart shape and size Pulmonary blood flow Echocardiogram n Best to aid in diagnosis Cardiac Cath for possible intervention 42
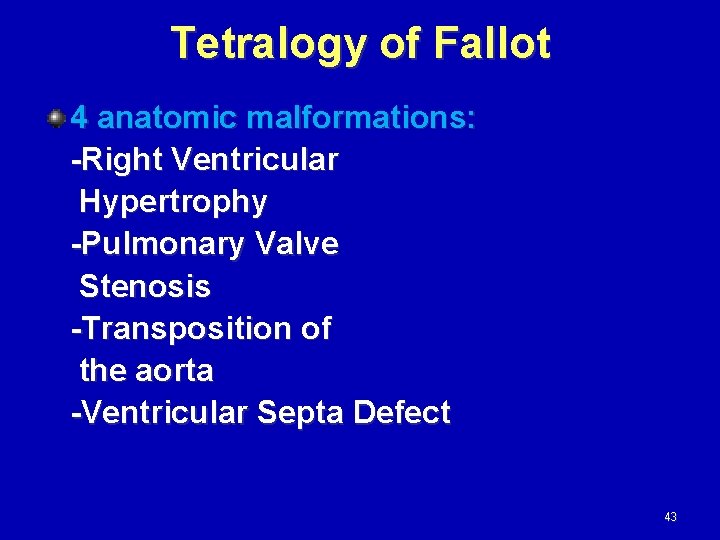
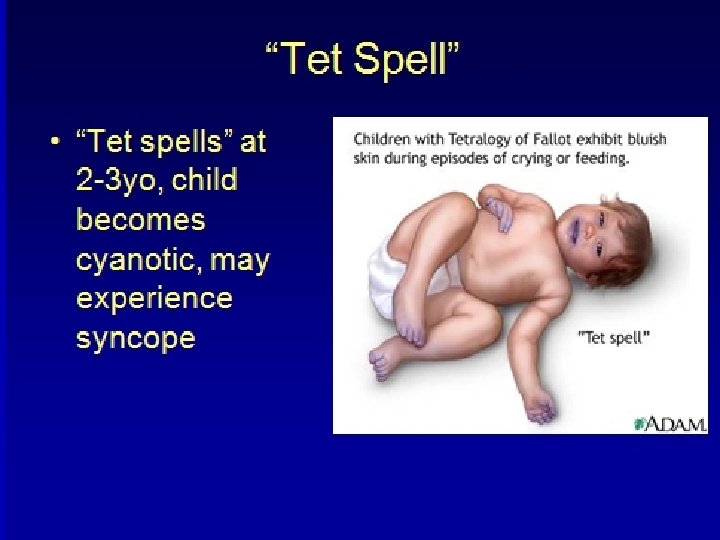
Tetralogy of Fallot 4 anatomic malformations: -Right Ventricular Hypertrophy -Pulmonary Valve Stenosis -Transposition of the aorta -Ventricular Septa Defect 43
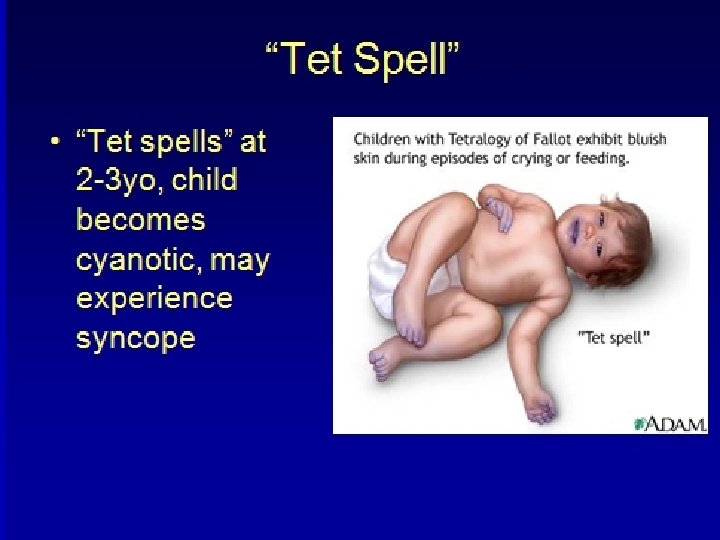
Tetralogy of Fallot Clinical presentation is directly related to the degree of pulmonary stenosis. Severe stenosis results in immediate cyanosis following birth. Mild stenosis will not present until later. Growth is retarded – insufficient oxygen and nutrients 44

45
46
47
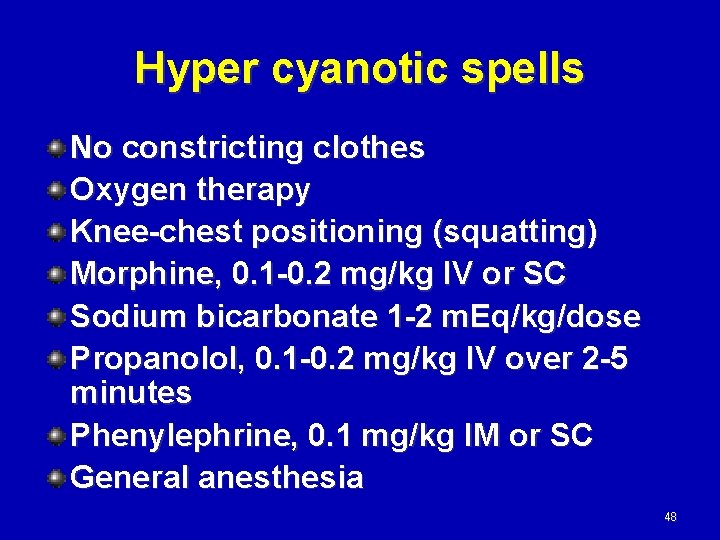
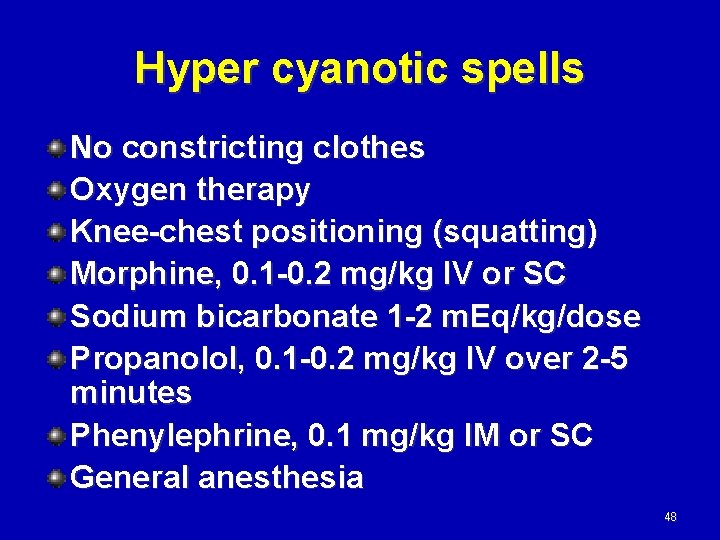
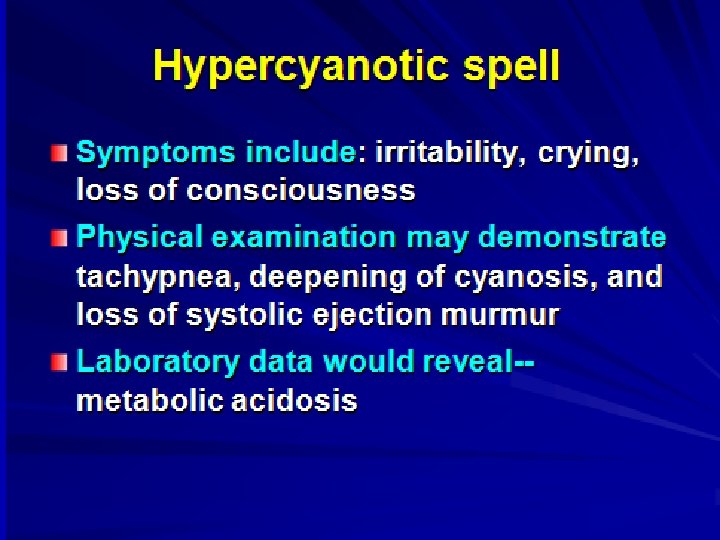
Hyper cyanotic spells No constricting clothes Oxygen therapy Knee-chest positioning (squatting) Morphine, 0. 1 -0. 2 mg/kg IV or SC Sodium bicarbonate 1 -2 m. Eq/kg/dose Propanolol, 0. 1 -0. 2 mg/kg IV over 2 -5 minutes Phenylephrine, 0. 1 mg/kg IM or SC General anesthesia 48
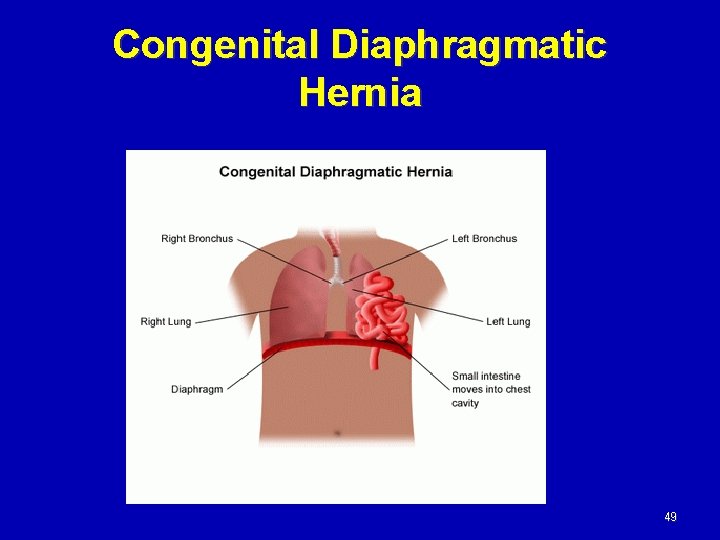
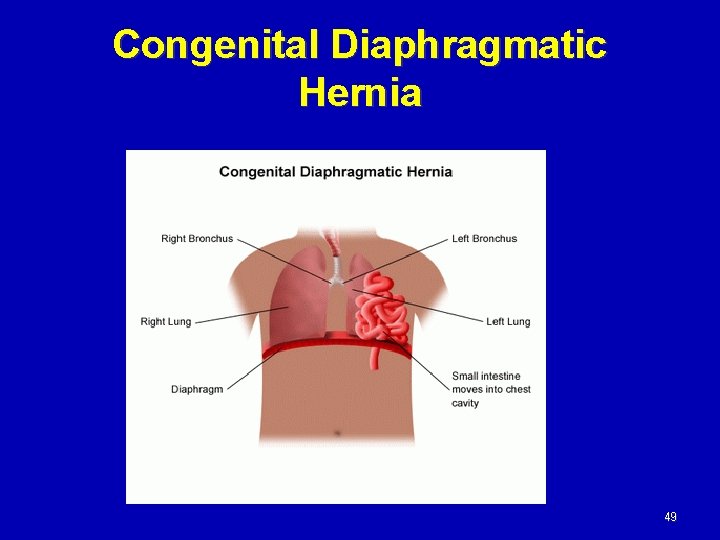
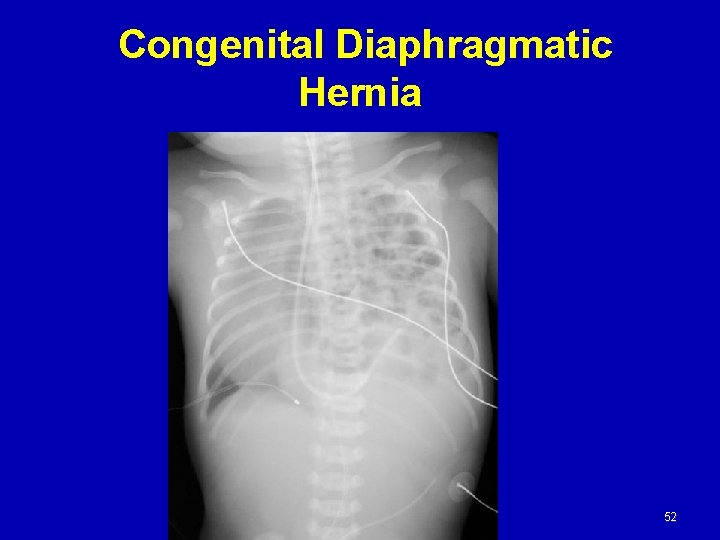
Congenital Diaphragmatic Hernia 49
CDH Respiratory Assessment n n n Tachypneic Retractions Nasal flaring Grunting Breath Sounds Decreased on the affected side May hear bowel sounds in chest with CDH 50
CDH Clinical Assessment Clin n n n Scaphoid Abdomen- classic sign Color Cyanotic Heart Rate Fast, slow or normal Perfusion Depends upon the severity X-Ray— Best diagnostic tool Bowel, stomach, liver in chest ABGs Acidosis, hypoxemia and hypercarbia 51
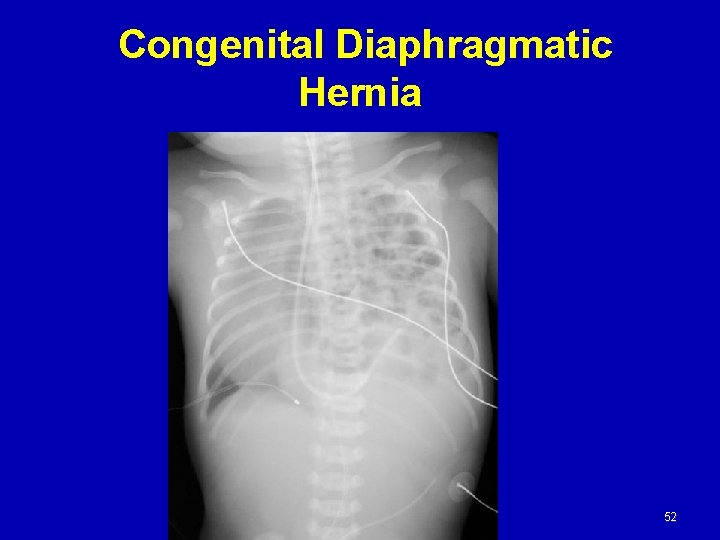
Congenital Diaphragmatic Hernia 52
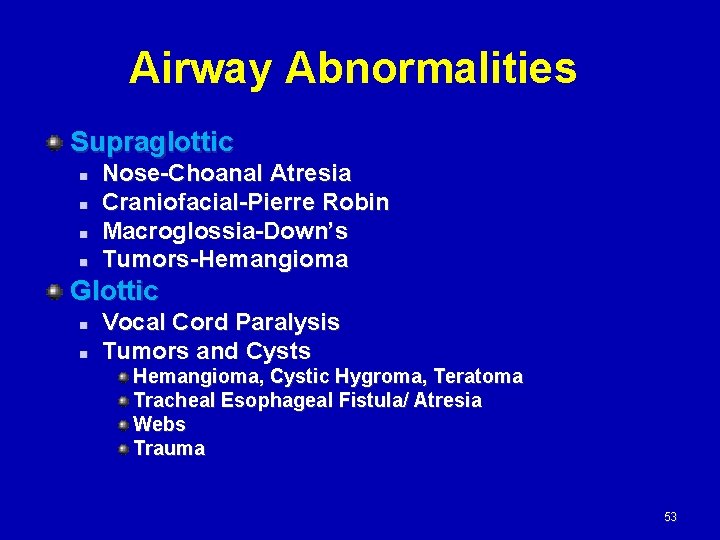
Airway Abnormalities Supraglottic n n Nose-Choanal Atresia Craniofacial-Pierre Robin Macroglossia-Down’s Tumors-Hemangioma Glottic n n Vocal Cord Paralysis Tumors and Cysts Hemangioma, Cystic Hygroma, Teratoma Tracheal Esophageal Fistula/ Atresia Webs Trauma 53
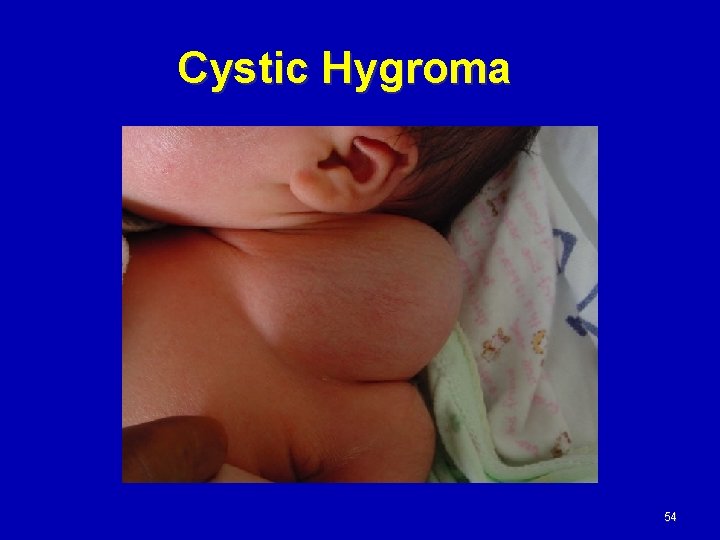
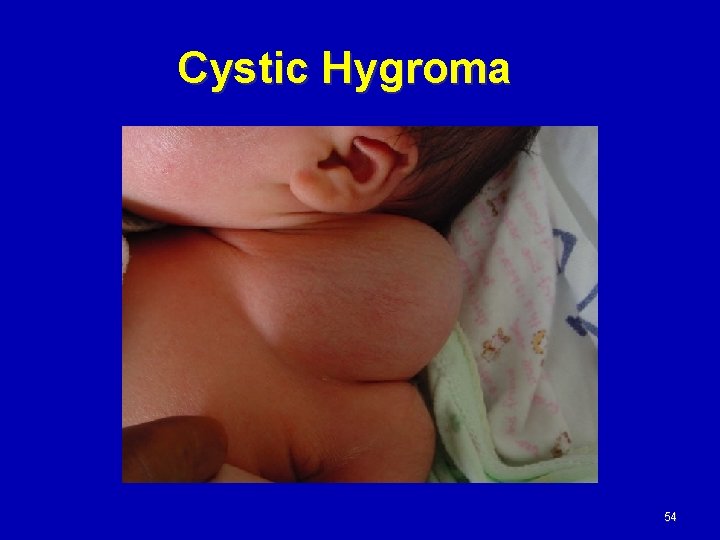
Cystic Hygroma 54
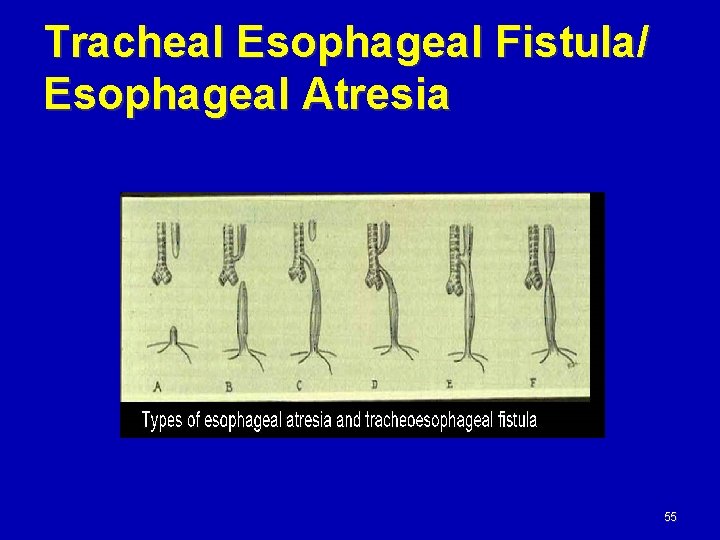
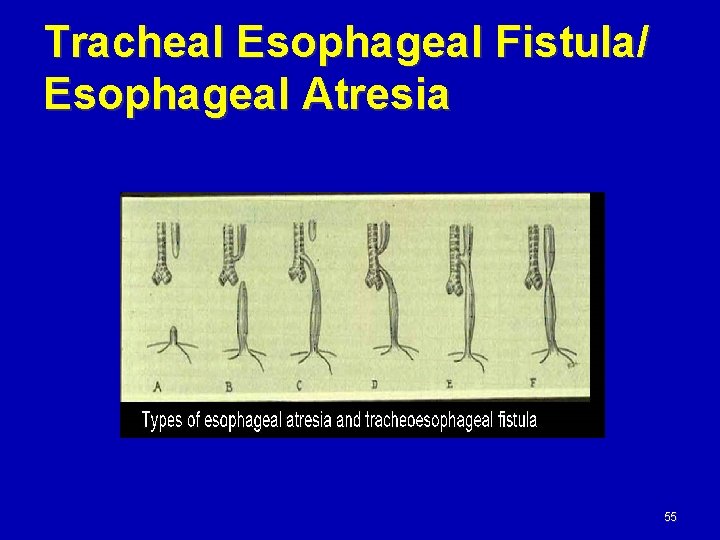
Tracheal Esophageal Fistula/ Esophageal Atresia 55

THANK YOU 56