Neonatal cardiac disorders 1 2 3 Abnormal finding
Neonatal cardiac disorders 1
2
3

Abnormal finding l Delayed capillary refill (>3 seconds) suggests poor perfusion (low cardiac output state : Shock-CHF) l DD: Sepsis 4
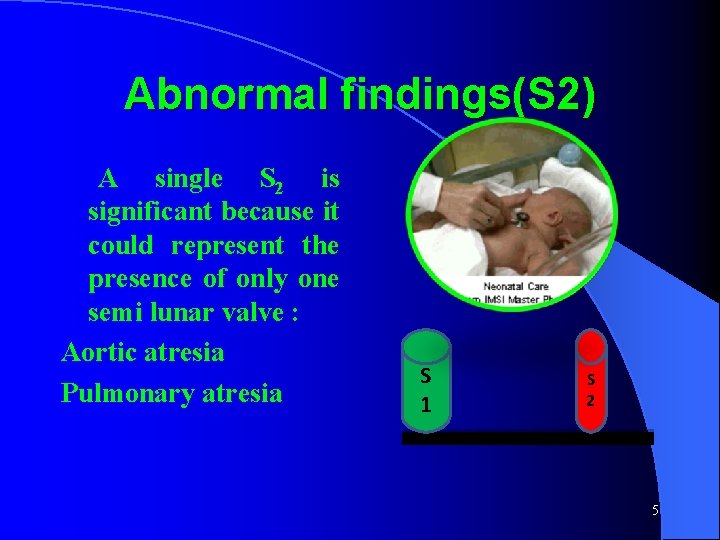
Abnormal findings(S 2) A single S 2 is significant because it could represent the presence of only one semi lunar valve : Aortic atresia Pulmonary atresia S 1 S 2 5

Abnormal findings(murmur) Murmurs often indicate CHD. However, many serious lesions do not present with a murmur (TGA, COA) 6
Decompansation (Liver Eaxam. ) l Palpate the lower border of the liver in Right MCL. l Liver is normally palpable up to 3 cm blew RCM. l Enlarged liver usually denotes CHF l DD: Cong. infection 7
1)Congenital Heart Disease: l PINK Shunts ( L to R) : l ASD l VSD l PDA Stenosis: l AS l PS l BLUE TOF l TGA l 8
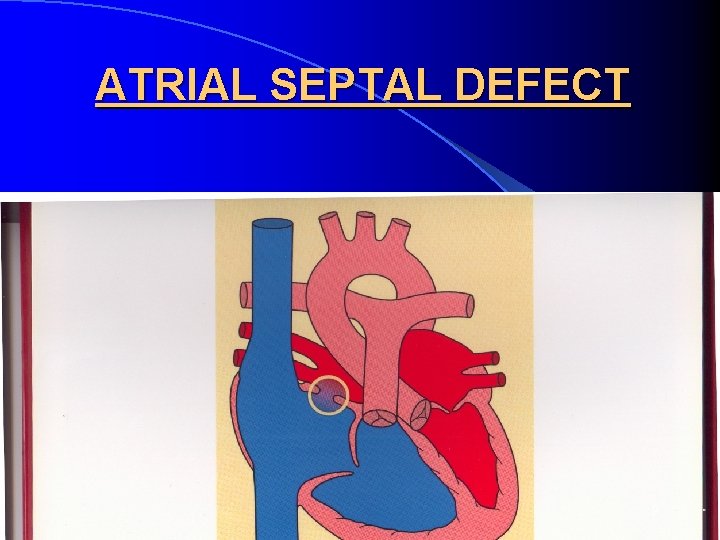
ATRIAL SEPTAL DEFECT 9
ATRIAL SEPTAL DEFECTS (ASD) l Three types exist : primum (lower in position & is a form of AVSD), secundum (arises from an enlarged foramen ovale)and sinus venosus(located at the junction of the superior vena cava and the right atrium) l The most common is the secundum type l Symptoms: None in childhood, arrhythmias in the 3 rd decade 10
ASD - cont. . . l ECHO: Diagnostic l c/p: asymptomatic , arrhythmias l Treatment : Surgical vs. transcatheter closure(Closure is performed electively between ages 2 & 5 yrs to avoid late complications) 11
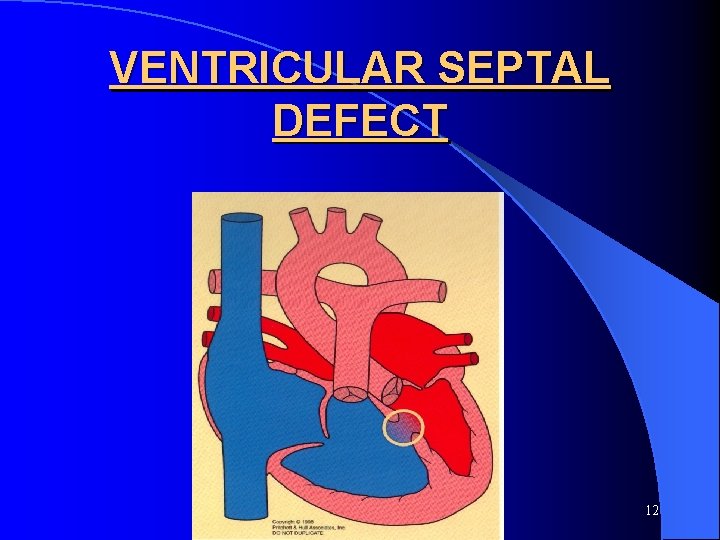
VENTRICULAR SEPTAL DEFECT 12
VENTRICULAR SEPTAL DEFECTS ( VSD) l This is the most common form of CHD l The VSDs are subdivided according to the part of the septum they occur in : Muscular, membranous l A large VSD causes left ventricular enlargement l With a small VSD there is normal growth and development 13
l With VSD - cont…. . a large defect there may be CHF(due to pulmonary congestion with Lt to Rt shunt), pulmonary infections and delayed growth l Murmur: harsh holosystolic or pansystolic murmur at 3 rd, 4 th intercostal spaces at parasternal area l ECHO: Diagnostic 14
l Fate VSD -cont. . . &treatment : Small VSDs close spontaneously depending on the site. Large defects may lead to Eisenmenger’s syndrome(Rt to Lt shunt with cyanosis due to pulmonary hypertension(due to untreated pulmonary congestion from large VSD) l Large VSDs are closed surgically usually at about 4 - 6 months of age. l Diuretics, digoxin and afterload reducing agents are used prior to surgery 15
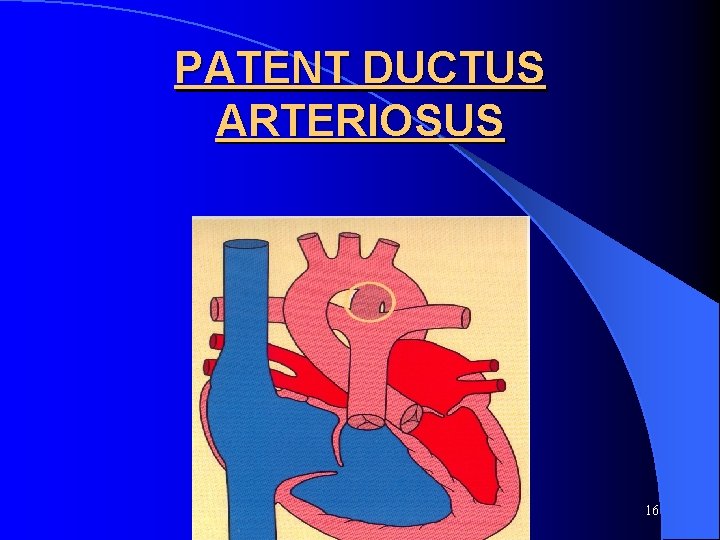
PATENT DUCTUS ARTERIOSUS 16
PATENT DUCTUS ARTERIOSUS ( PDA) l It is a connection between the aorta and the pulmonary artery. l Very common in preterm babies. l Usually closes in the first 2 weeks of life. 17
PDA - cont…. . l Symptoms : a) None if small b) If large can cause CHF in a term infant c) In a preterm baby respiratory distress(tachypnea, retraction, grunting , cyanosis in sever cases) and CHF usually occurs after day 3 of life. 18
PDA l Signs: continuous “machinary” murmur later. Best heard below the left clavicle. l A large PDA causes LA and LV enlargement. l Treatment : Preterm vs. term baby. 19
PDA - cont. . . l In a preterm it can be closed medically using indomethacin, ibuprofen, diuretics l In a term baby if still open at 3 months of age then closure by cardiac catherization is the method of choice. 20
Duct-dependent lesion l l Types: A)Duct-dependent systemic blood flow: 1) aortic stenosis l 3) interrupted aortic arch l l l 2) coarctation of aorta 4) hypoplastic heart syndrome B)Duct-dependent pulmonary blood flow: 1) pulmonary stenosis 3) tricusped atresia 2) pulmonary atresia 4) tetralogy of fallot Treatment of duct dependent lesions: PGE 1 continuous intravenous infusion to keep the ductus arteriosus patent l Surgical repair according to each lesion l 21
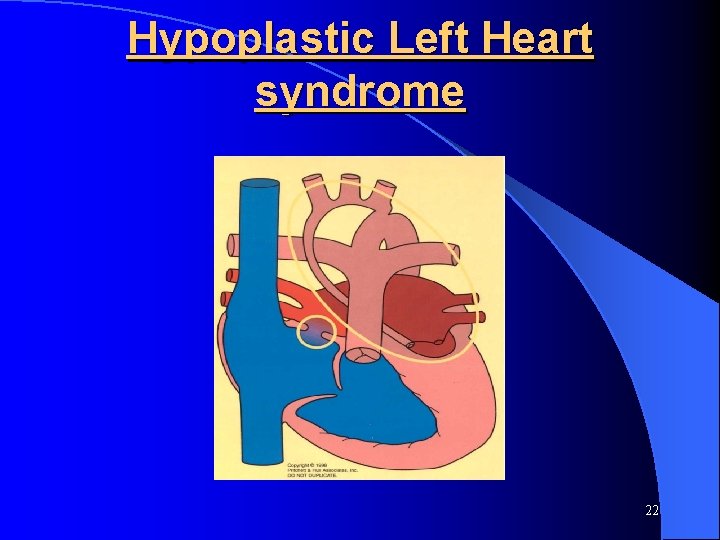
Hypoplastic Left Heart syndrome 22
Hypoplastic Left Heart Syndrome Varying degrees of left heart hypoplasia at multiple levels l Babies present in cardiogenic SHOCK once the ductus closes. l Immediate treatment is PGE 1 intravenously as an infusion. l Surgical repair after PGE 1. l 23
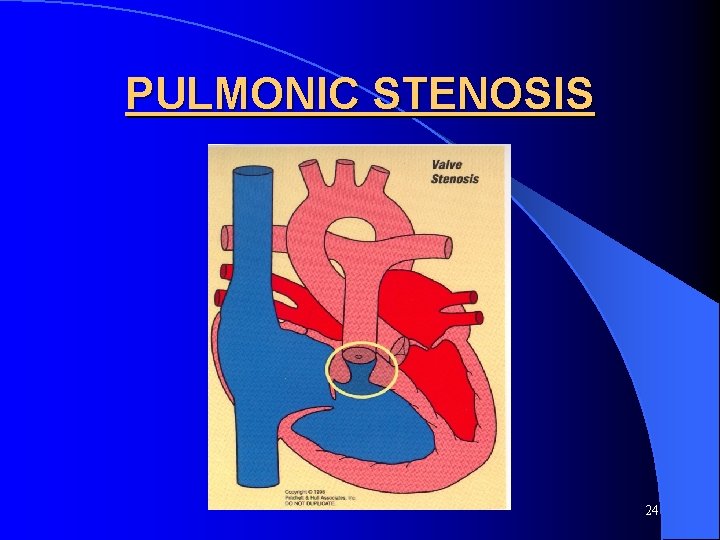
PULMONIC STENOSIS 24
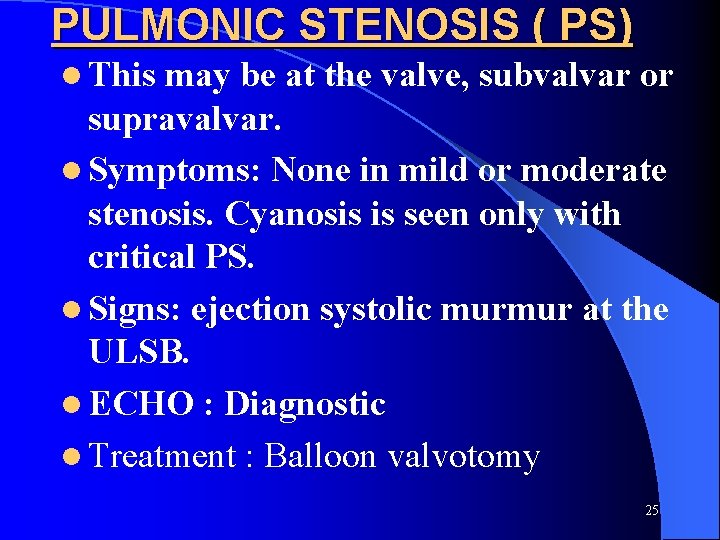
PULMONIC STENOSIS ( PS) l This may be at the valve, subvalvar or supravalvar. l Symptoms: None in mild or moderate stenosis. Cyanosis is seen only with critical PS. l Signs: ejection systolic murmur at the ULSB. l ECHO : Diagnostic l Treatment : Balloon valvotomy 25
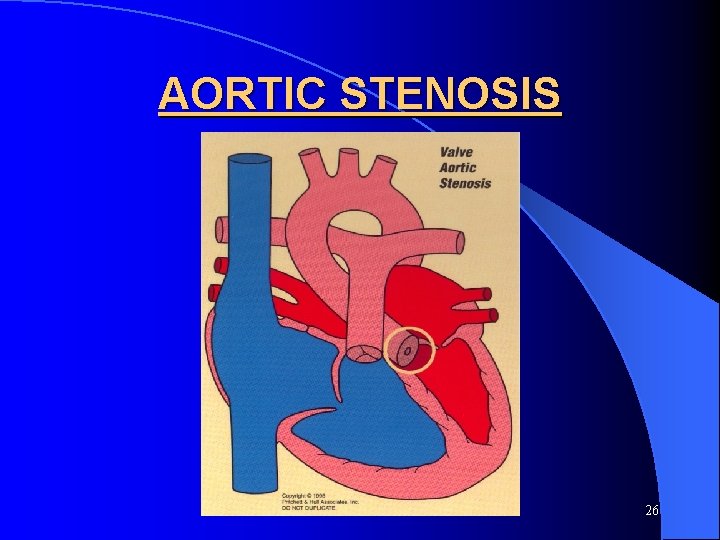
AORTIC STENOSIS 26
AS Stenosis possible at the valve, subvalvar or supravalvar. l Symptoms: Mild : None Moderate to severe: c/p of low cardiac output(chest pain, poor perfusion, fatigability, syncope). l 27

BLUE LESIONS 28
There has to be a RIGHT to LEFT shunt to cause cyanosis 29
30
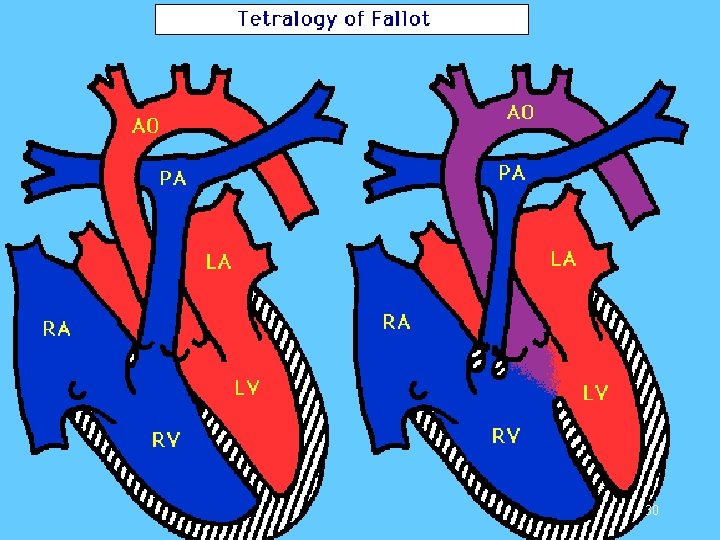
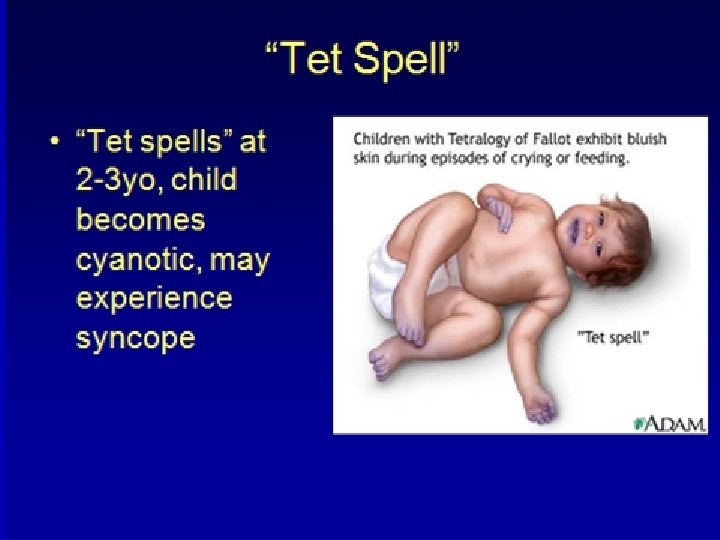
l Most Tetralogy of Fallot common cyanotic heart disease. l The four abnormalities include: – VSD - Overriding Aorta - RVH - PS l C/P: RD, cyanotic spells, rare CHF except in mild degree of RV outflow obstruction l Murmur: systolic(turbulence of blood over RV outflow tract) at Lt 3 rd, 4 th spaces l Chest x-ray: oligemic lung, boot shaped heart (elevated cardiac apex) due to RV hypertrophy 31
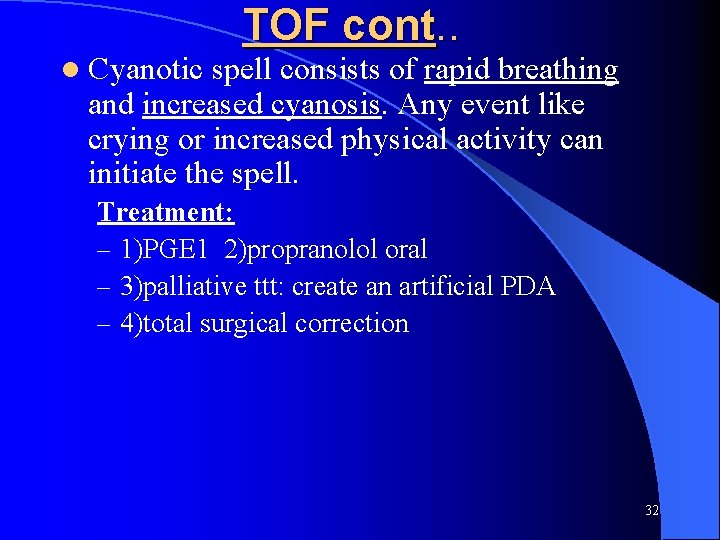
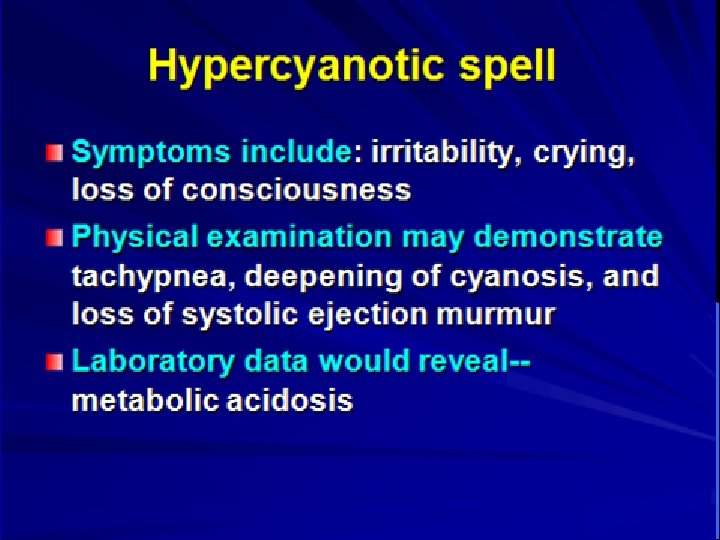
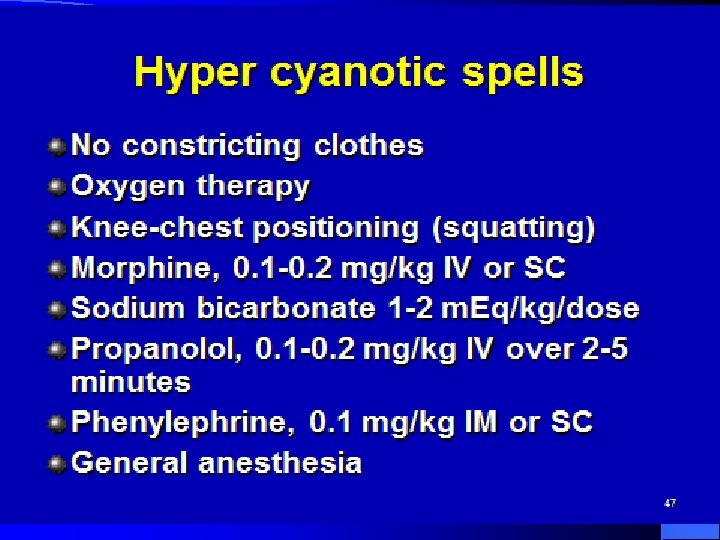
l Cyanotic TOF cont. . spell consists of rapid breathing and increased cyanosis. Any event like crying or increased physical activity can initiate the spell. Treatment: – 1)PGE 1 2)propranolol oral – 3)palliative ttt: create an artificial PDA – 4)total surgical correction 32

33
34
35
36
TRANSPOSITION OF THE GREAT ARTERIES 37
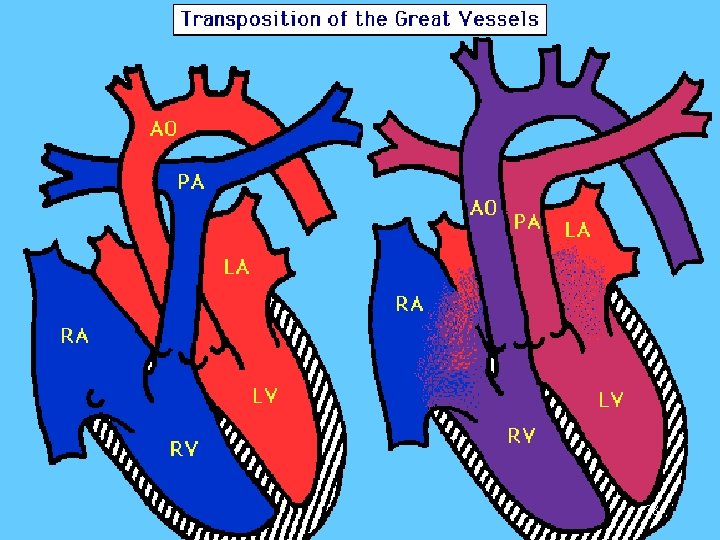
38
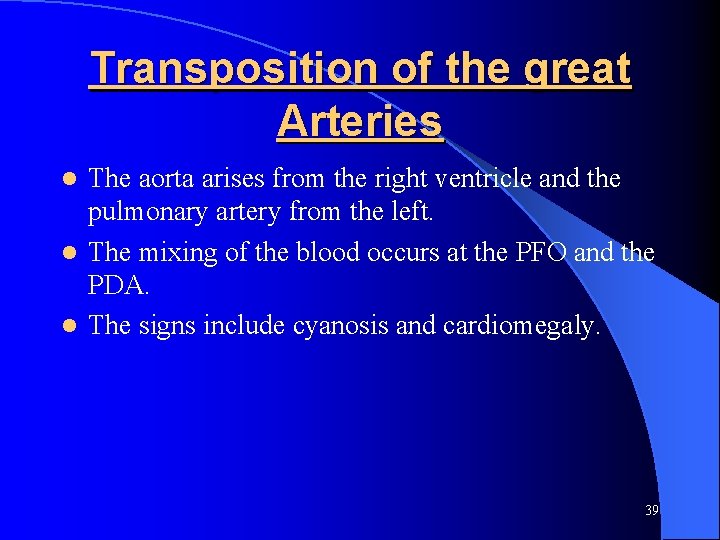
Transposition of the great Arteries The aorta arises from the right ventricle and the pulmonary artery from the left. l The mixing of the blood occurs at the PFO and the PDA. l The signs include cyanosis and cardiomegaly. l 39
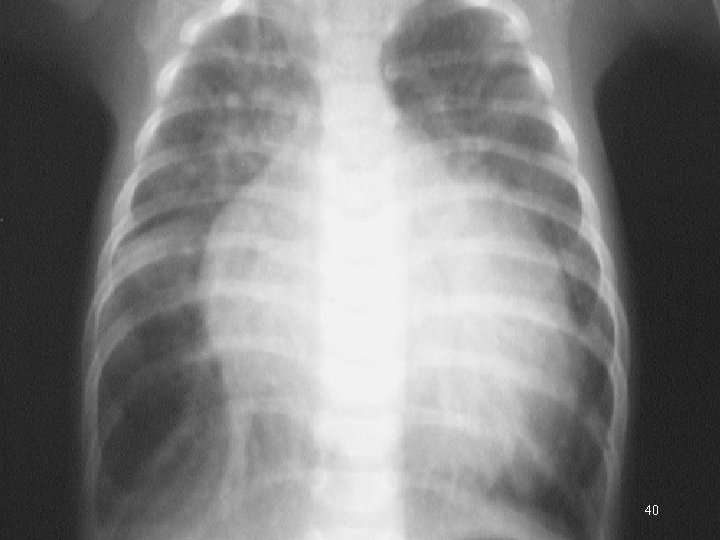
40

41
- Slides: 41