Neonatal Assessment Resuscitation Michael Rieker DNP CRNA Director



















































- Slides: 62

Neonatal Assessment, Resuscitation Michael Rieker, DNP, CRNA Director, Wake Forest University Baptist Medical Center Nurse Anesthesia Program

Neonatal challenges after birth • CV system changes to adult state • Pulmonary system: expand lungs • Thermal regulation: non-shivering thermogenesis
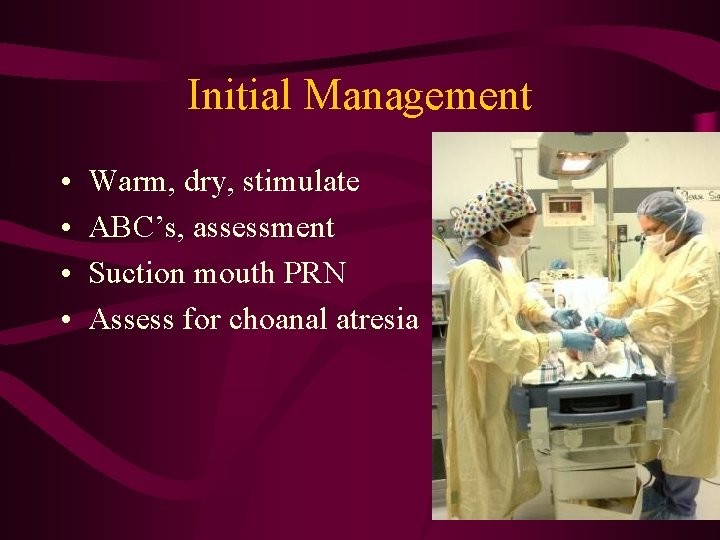
Initial Management • • Warm, dry, stimulate ABC’s, assessment Suction mouth PRN Assess for choanal atresia
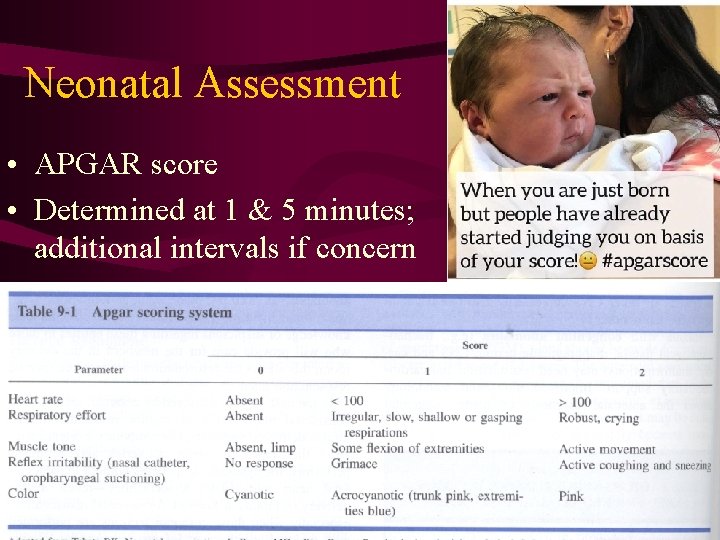
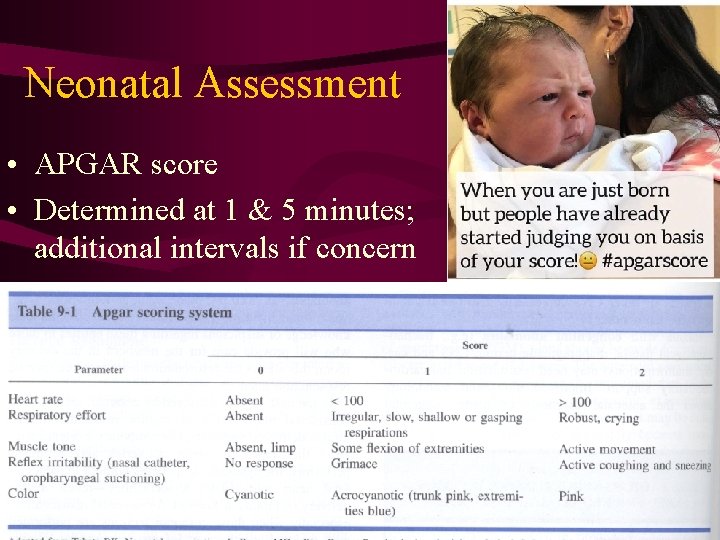
Neonatal Assessment • APGAR score • Determined at 1 & 5 minutes; additional intervals if concern


Apnea • Primary • Secondary

Hemodynamics • HR 120 -160 • B/P
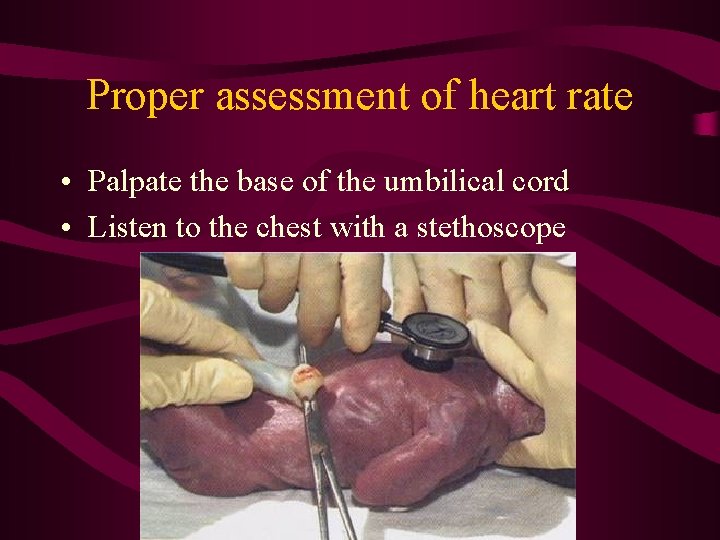
Proper assessment of heart rate • Palpate the base of the umbilical cord • Listen to the chest with a stethoscope
Umbilical Cord Blood • Used as an indicator of fetal acidosis • Presence of fixed (metabolic) acids indicate significant anaerobic metabolism • 7. 2 considered low end of normal

Delivery of pre-term fetus • Watch for uterine hypotonia after tocolytic therapy. • ? c/s <what gestational age?

Neonatal Resuscitation

10 -15% of newborns require some resuscitation • Maternal: AMA, HTN, DM, substance abuse, previous fetal loss • Fetus: preemie, post-date, CHD, multiple gestation • Placenta: previa, abruptio, oligohydramnios, chorio • Delivery: abnormal lie, meconium, FHR abnormalities, instrumented delivery, maternal opioid admin.

• 5% of malpractice claims R/T neonatal resuscitation • Hospital needs clear policies re: personnel responsibilities • Anesthetist often asked to help with resuscitation • First priority is the mother

Immediate Care • • • Suction mouth and nose Dry/warmer Lateral/slight T-berg to facilitate drainage Tactile stimulation Assess HR; treat with oxygen & PPV – – – Have pop-off or manometer Breathe 40 -60/min at < 20 -30 cm H 2 O Assess efficacy via heart rate, not skin color If continues < 60, chest compressions 90 compressions/minute. 3: 1 ratio

A word about oxygen



Neonatal Airway Management Age Weight ETT Preemie <1. 0 kg 2. 5 Preemie 1. 0 - 2. 5 kg 3. 0 Term 2. 5 - 3. 5 kg 3. 0 Term 3. 5 -5. 0 kg 3. 5

Pharmacological Support 1. 2. 3. 4. Oxygen and ventilation Epinephrine 10 mcg/kg (to 30 mcg/kg) Naloxone 10 mcg/kg Bicarb- only if specifically indicated 12 m. Eq/kg (rate of 1 m. Eq/kg/min) 5. Fluid/blood 10 -20 ml/kg

Pharmacological Support Drug Purpose Route Epinephrine Increase rate and strength of cardiac contractions IV (ETT if IV not est. ) Naloxone (Narcan) Continued respiratory depression after PPV Reverse maternal narcotic administration IV (IM acceptable) No evidence that ETT administration of this drug is beneficial. Sodium Bicarbonate Correct severe metabolic acidosis (ongoing resuscitation) IV only (large vein) Volume Expanders Fluid replacement for hypovolemia (NS) IV (UVC preferred)

Drug Access 1. UV line 2. Intraosseous 3. ETT



Special Problems

Meconium Aspiration Syndrome • • Respiratory distress Can be severe and require ECMO or NO An intrauterine event Suction before delivery of shoulders is no longer recommended After delivery, if non-vigorous, suction via ETT repeatedly up to 2 minutes until clear Proceed with normal resuscitation High Fi. O 2 Pass NG or OG tube once stable



Antepartum and Postpartum Hemorrhage

Causes of obstetric hemorrhage • • Abortion Ectopic pregnancy Placenta previa Placental abruption • Placenta accreta • Uterine rupture • Uterine atony • Cervical/vaginal laceration • Retained placenta • Uterine inversion • Coagulopathy

4 T’s of OB hemorrhage • Tone • Trauma • Tissue • Thrombin

At term, the uterus receives 700 -900 ml blood/min

Hemorrhage is underestimated • Normal pregnancy changes mimic or mask signs of blood loss (tachy, low B/P) • Increased renin, ADH & catecholamines • 35 -40% increase in blood volume – 500 ml “autotransfusion” at delivery

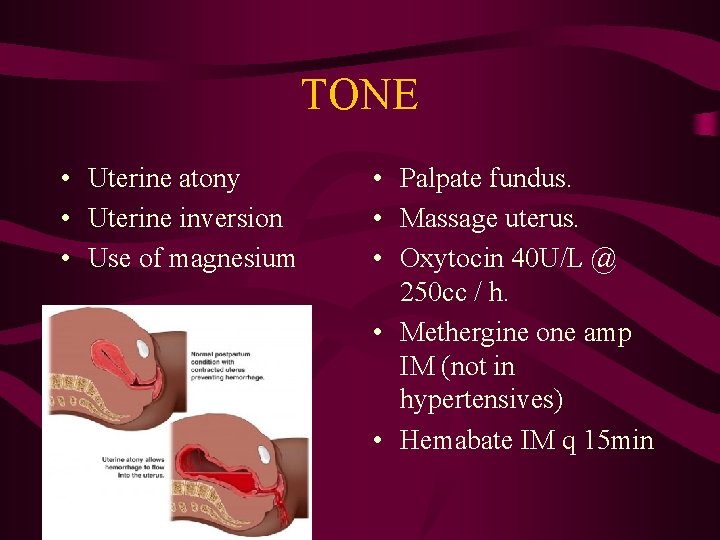
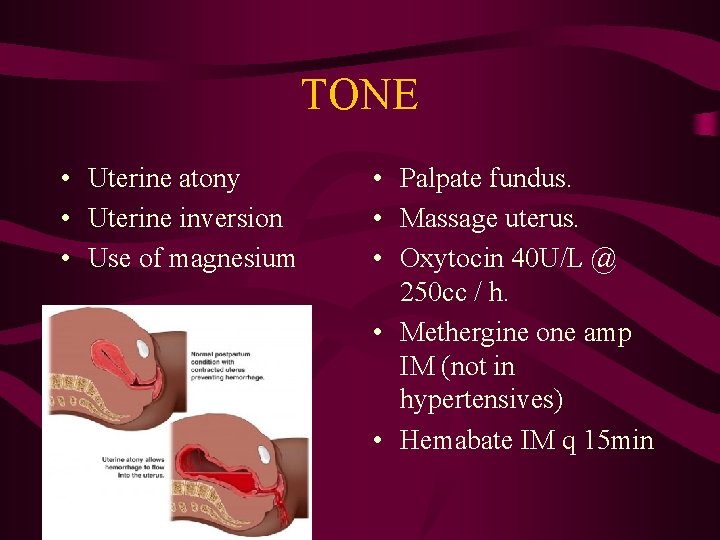
TONE • Uterine atony • Uterine inversion • Use of magnesium • Palpate fundus. • Massage uterus. • Oxytocin 40 U/L @ 250 cc / h. • Methergine one amp IM (not in hypertensives) • Hemabate IM q 15 min

Postpartum Hemorrhage Uterine Atony Most common cause of postpartum hemorrhage • • Presentation: painless vaginal bleeding, a rising fundus, soon or hours following delivery • Risk factors: multiparity, multiple gestation, macrosomia, prolonged labor, oxytocin in labor, chorioamnionitis, retained placenta, volatile anesthetics • Treatment: IV fluid, uterine massage, pharmacologic tx, surgery

Postpartum Hemorrhage: • Retained POC vs. Atony

TRAUMA • R/O cervical or vaginal lacerations. • Uterine rupture • Birth canal trauma • Episiotomy • Hematoma • Uterine inversion • Obtain good exposure. • Inspect cervix and vagina. • Worry about slow bleeders. • Treat hematomas.
Uterine Inversion • • 1: 2000 vaginal births Hold pitocin until uterus is replaced Nitroglycerin 10 -50 ug trial x 2 General anesthesia for profound analgesia and uterine relaxation • Massive blood loss - SHOCK
Vasa Previa • 50 -75% fetal mortality • Variable decels may predict • AROM may lead to compression or tear of UC • Fetus has only 250 ml blood
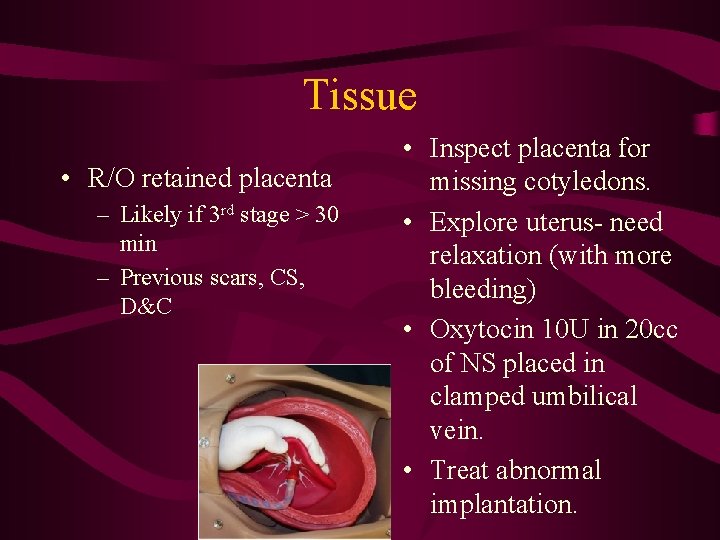
Tissue • R/O retained placenta – Likely if 3 rd stage > 30 min – Previous scars, CS, D&C • Inspect placenta for missing cotyledons. • Explore uterus- need relaxation (with more bleeding) • Oxytocin 10 U in 20 cc of NS placed in clamped umbilical vein. • Treat abnormal implantation.

Placenta Previa • Placenta implants in advance of fetal presenting part • 1: 200. Previous uterine trauma encourages • Causes 25 -40% of perinatal mortality • Types of previa: – Marginal – Partial – Total


Placenta Previa • • • Painless vaginal bleeding pre-term Lack of abdominal pain or contractions Diagnosed via ultrasound Vaginal exams contraindicated May be complicated by preterm labor or abruptio
Placenta Previa Management • Double set-up for SVE • Expect bleeding – Abruptio – Cut into placenta with C/S – Ineffective contraction of lower segment – Accreta • IVs and blood • Ketamine
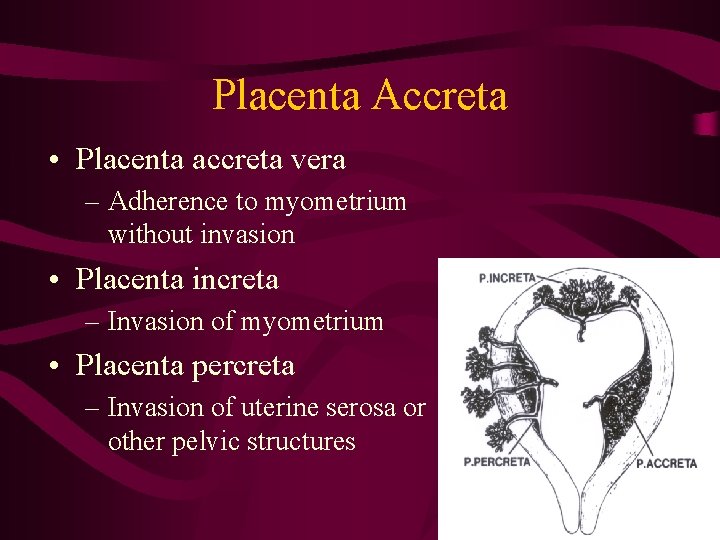
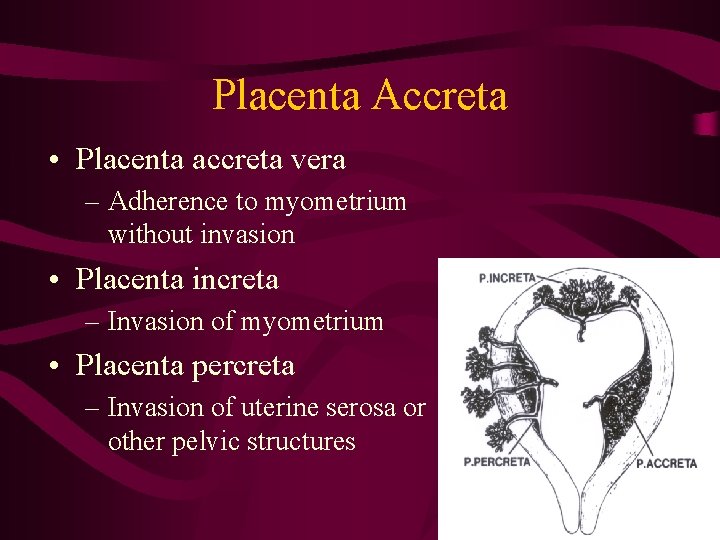
Placenta Accreta • Placenta accreta vera – Adherence to myometrium without invasion • Placenta increta – Invasion of myometrium • Placenta percreta – Invasion of uterine serosa or other pelvic structures


Abruptio Placentae • Separation of placenta from decidua basalis • Assoc. with HTN, smoking, cocaine, trauma, PROM • Abdominal pain and vaginal bleeding • May be > 2000 ml occult blood • 10% risk of DIC • Fetal death 20%

Abruption

Abruptio video

Signs of abruption Palmer pg 142

Abruptio Placentae • Large IV • Signs of hypovolemia? Ketamine, fluids, blood • May deliver vaginally if stable • Careful with epidural- hypotension

Anesthetic Management of Abruption Palmer pg 143

Surgical Intervention • Delivery • Hypogastric or uterine artery ligation • Hysterectomy

Thrombin- DIC • Most common in OB with severe placenta abruptio, fetal demise or embolotic event • Eliminate trigger • Maintain volume • Administration of appropriate clotting factors

Oxytocin (Pitocin) • Uterine smooth muscle constrictor • Vascular dilatation (increases renal, coronary & cerebral blood flow) • Antidiuretic effect-potential pulmonary edema • Plasma half-life 3 -5 minutes • Dose: 10 -20 U per 1000 cc Extreme circumstances-up to 80 U/1000

Methylergonovine (Methergine) • Treats hemorrhage refractory to Oxytocin • Constricts uterine and vascular smooth muscle • IM or oral administration • 0. 2 mg IM, q. 2 -5 hours • Peak effect 3 -5 minutes

Prostaglandin F 2 alpha (Hemabate) • Induce second trimester abortion • Control severe postpartum hemorrhage • Constricts uterine, GI, brochial and vascular smooth muscle • Extreme caution in asthmatics & HTN • . 25 mg IM or interuterine q. 90 min. to 2. 0 mg • nb. Severe transient V/Q mismatch can occur with interuterine injection requiring ventilatory support

Other prostaglandins • Misoprostol (Cytotec) PGE 1 - Orally, vaginal, sublingual, rectal • Dinoprostone (Prepidil-gel, Cervidil-insert) PGE 2 - vaginal, rectal • Used for labor induction/cervical ripening

Anesthetic Care • MAC: cervical and vaginal lacerations • Regional: controversial • GET: for uncontrolled hemorrhage with hypovolemia

Rapid fluid replacement is key to preventing shock and preserving a good outcome

10 Flags for Bleeding • Blood loss is usually underestimated in OB • Volume is more important than H/H • Rapid fluid is more important than type of fluid • Type specific is better than O-neg • FFP, cryo or platelets should not be give prophylactically • NO IV Methergine or Hemabate • Do not delay for lab in severe bleeding • Previa+previous C/S=acreta • C-hyst can have regional, prepare for bleeding • Call for help