NEISSERIA l Gram negative diplococci l Aerobic Catalase
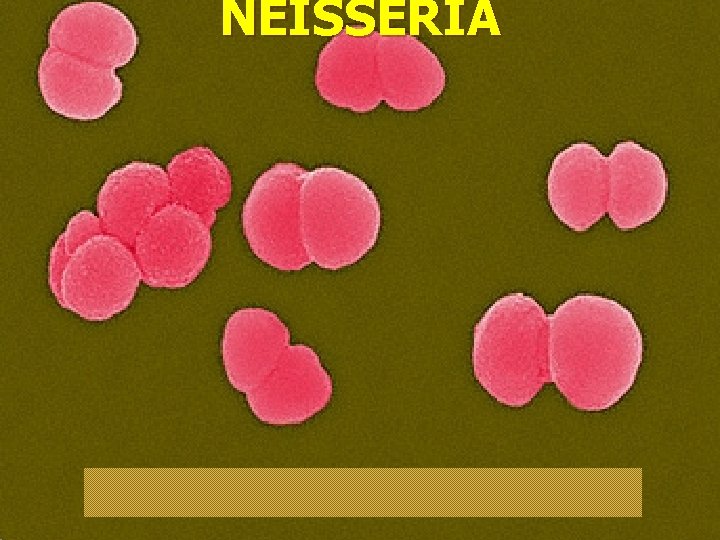
NEISSERIA
l Gram negative diplococci l Aerobic, Catalase –ve, Oxidase +ve l Pathogenic – N. meningitidis, N. gonorrhoeae l Non-pathogenic – commensals in oral cavity ; N. flavescens, N. sicca
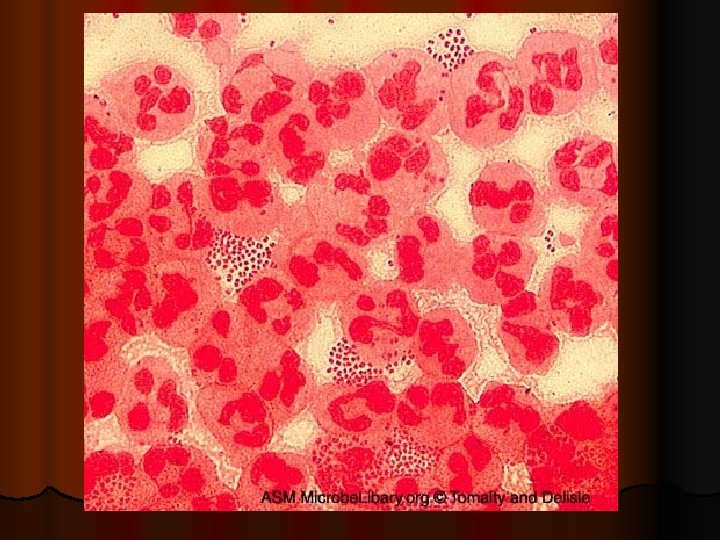
NEISSERIA MENINGITIDIS l Intracellular l Culture diplococci; Gram negative – l Blood agar, Chocolate agar, l Thayer Martin medium with Vancomycin, colistin, nystatin & trimethoprim l Obligate aerobes; 5 -10% CO 2 l Gluocse & maltose fermented with acid only l Oxidase test – 1% tetramethyl paraphenylene diamine hydrochloride

+ve - ve
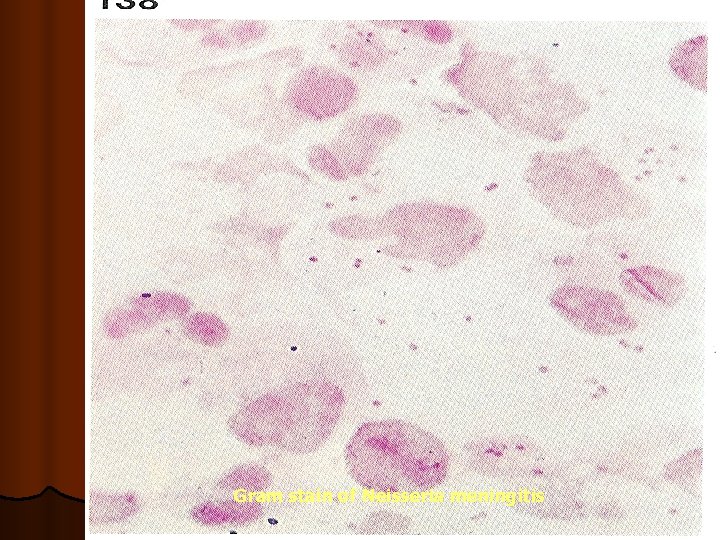
Gram stain of Neisseria meningitis

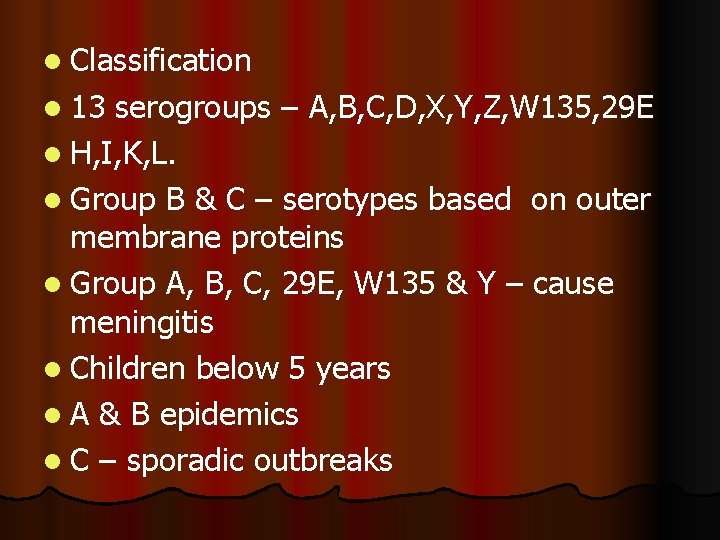
l Classification l 13 serogroups – A, B, C, D, X, Y, Z, W 135, 29 E l H, I, K, L. l Group B & C – serotypes based on outer membrane proteins l Group A, B, C, 29 E, W 135 & Y – cause meningitis l Children below 5 years l A & B epidemics l C – sporadic outbreaks
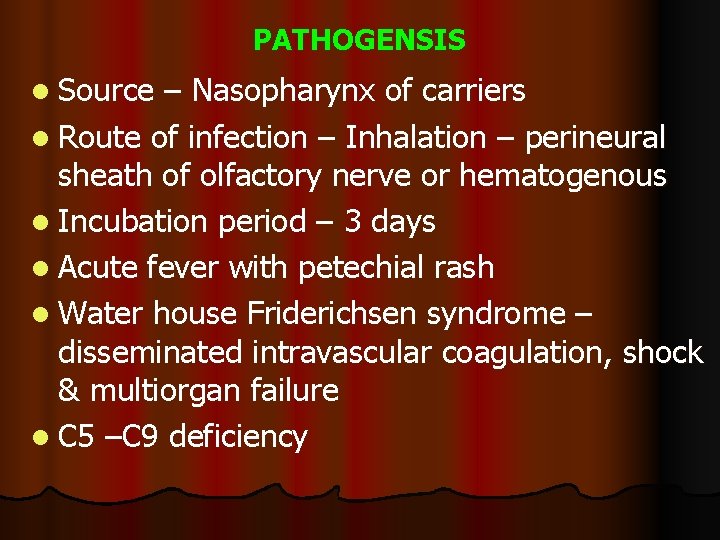
PATHOGENSIS l Source – Nasopharynx of carriers l Route of infection – Inhalation – perineural sheath of olfactory nerve or hematogenous l Incubation period – 3 days l Acute fever with petechial rash l Water house Friderichsen syndrome – disseminated intravascular coagulation, shock & multiorgan failure l C 5 –C 9 deficiency

Haemorrhagic rash
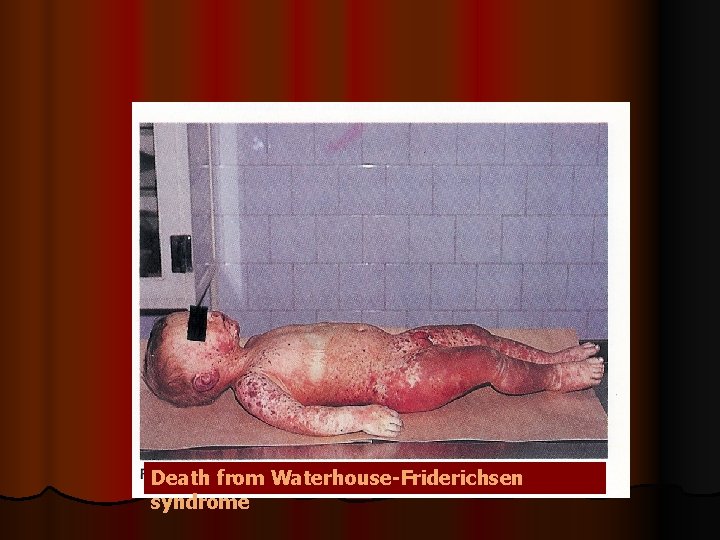
Death from Waterhouse-Friderichsen syndrome
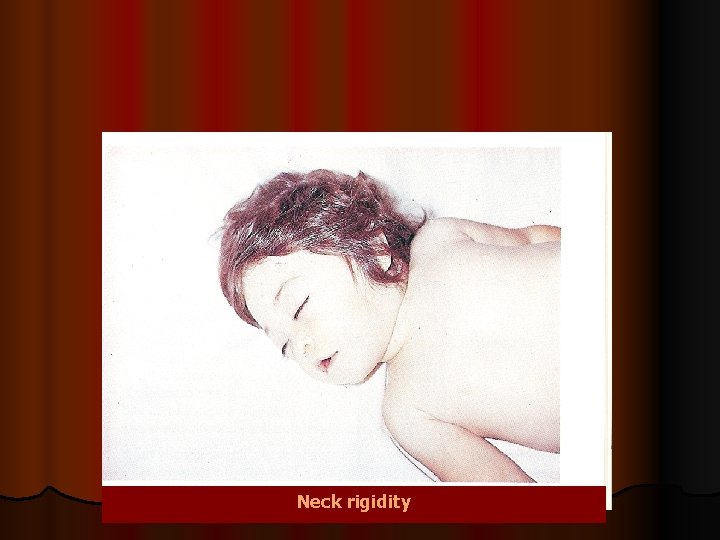
Neck rigidity

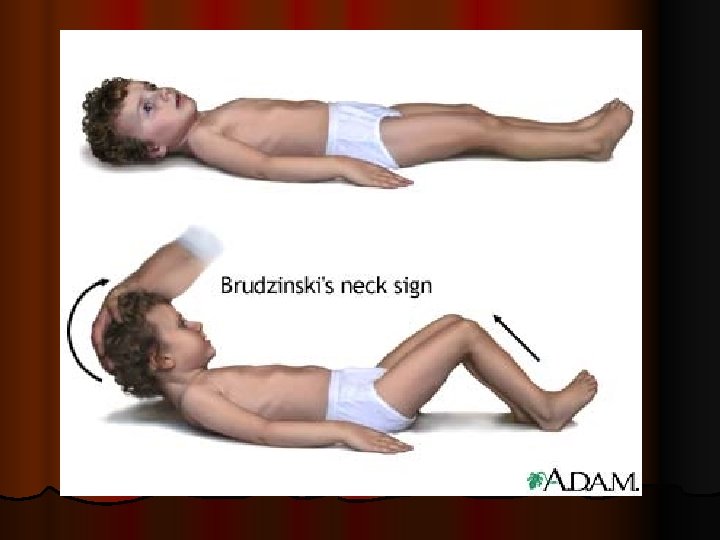
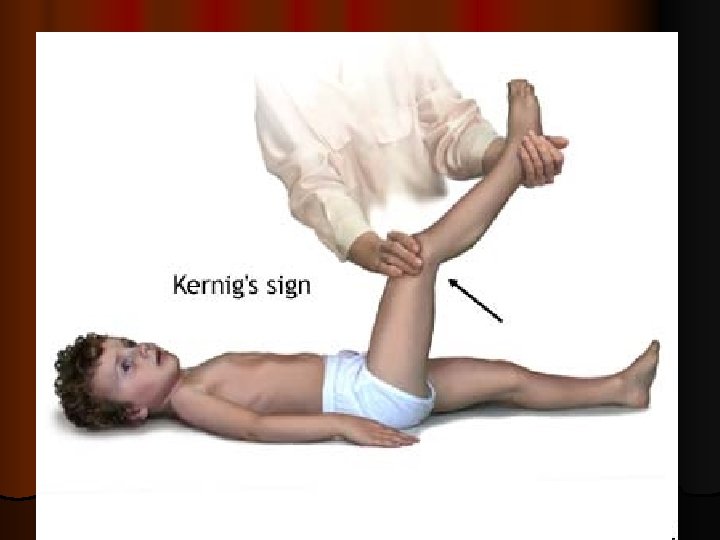

Lab diagnosis l Specimen – CSF, Blood, swabs from petechial lesions, nasopharyngeal sawbs l Stuart’s transport media l Microscopy - Gram negative diplococci within polymorphs l Capsular polysaccharide Antigen detection by latex agglutination l Culture – BA, CA, Glucose broth, Bile broth
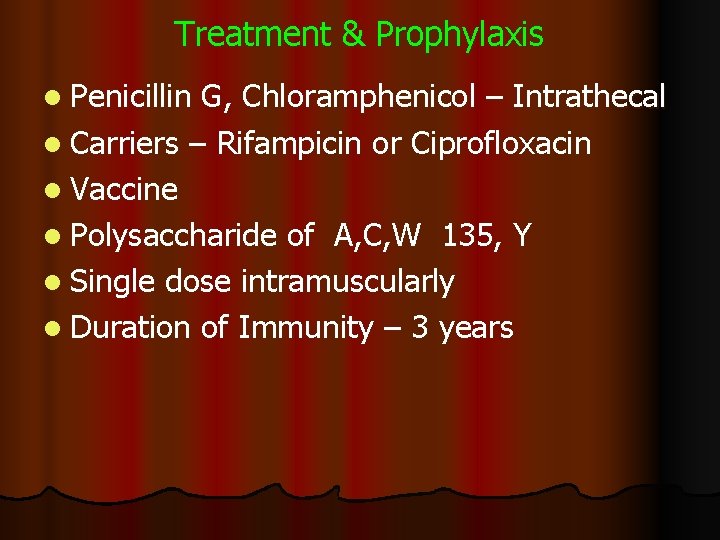
Treatment & Prophylaxis l Penicillin G, Chloramphenicol – Intrathecal l Carriers – Rifampicin or Ciprofloxacin l Vaccine l Polysaccharide of A, C, W 135, Y l Single dose intramuscularly l Duration of Immunity – 3 years
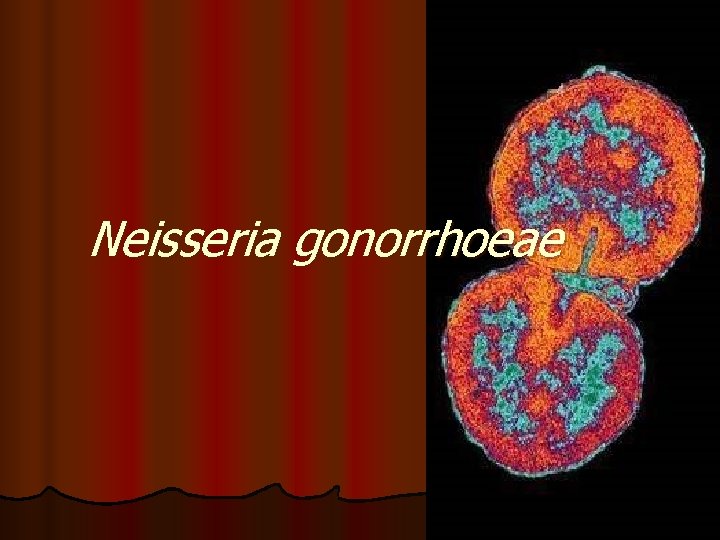
Neisseria gonorrhoeae
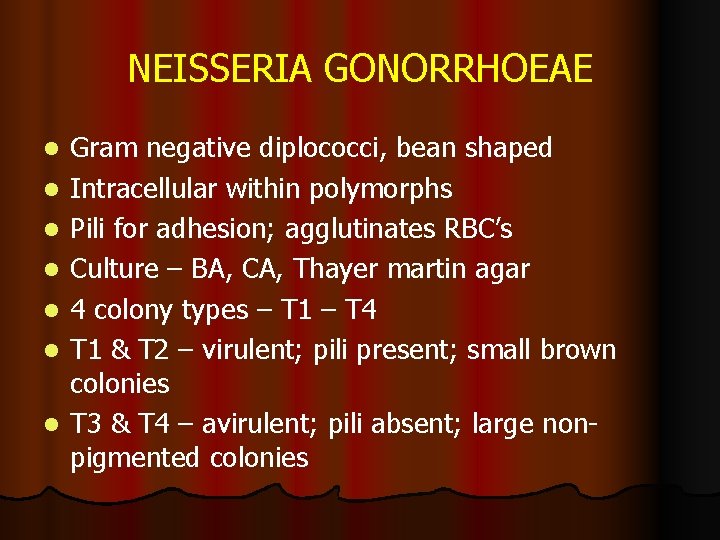
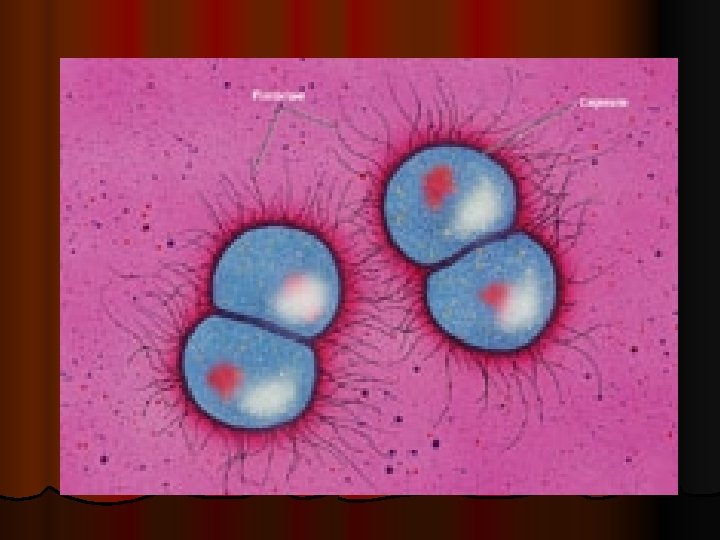
NEISSERIA GONORRHOEAE l l l l Gram negative diplococci, bean shaped Intracellular within polymorphs Pili for adhesion; agglutinates RBC’s Culture – BA, CA, Thayer martin agar 4 colony types – T 1 – T 4 T 1 & T 2 – virulent; pili present; small brown colonies T 3 & T 4 – avirulent; pili absent; large nonpigmented colonies
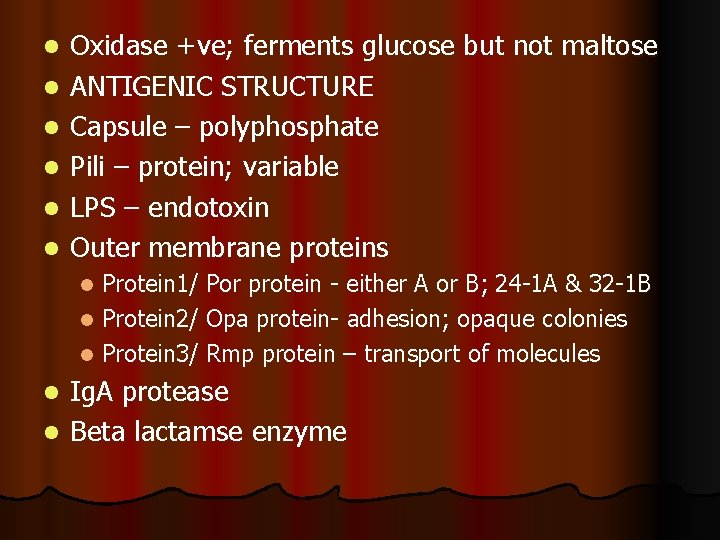
l l l Oxidase +ve; ferments glucose but not maltose ANTIGENIC STRUCTURE Capsule – polyphosphate Pili – protein; variable LPS – endotoxin Outer membrane proteins Protein 1/ Por protein - either A or B; 24 -1 A & 32 -1 B l Protein 2/ Opa protein- adhesion; opaque colonies l Protein 3/ Rmp protein – transport of molecules l Ig. A protease l Beta lactamse enzyme l
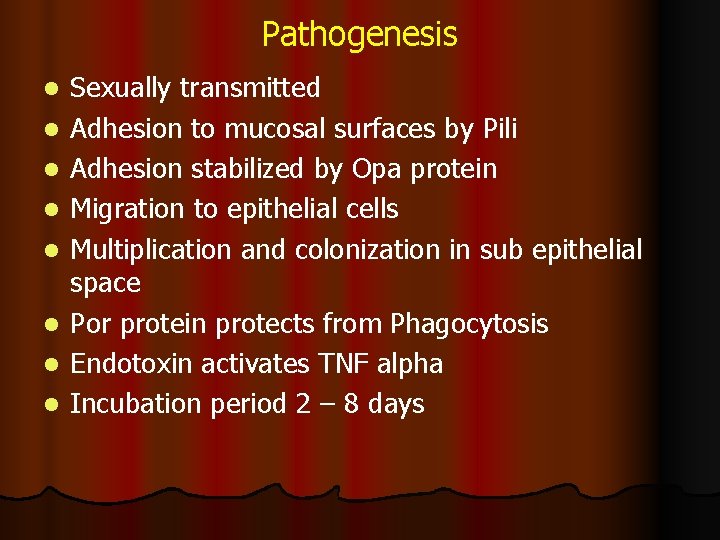
Pathogenesis l l l l Sexually transmitted Adhesion to mucosal surfaces by Pili Adhesion stabilized by Opa protein Migration to epithelial cells Multiplication and colonization in sub epithelial space Por protein protects from Phagocytosis Endotoxin activates TNF alpha Incubation period 2 – 8 days
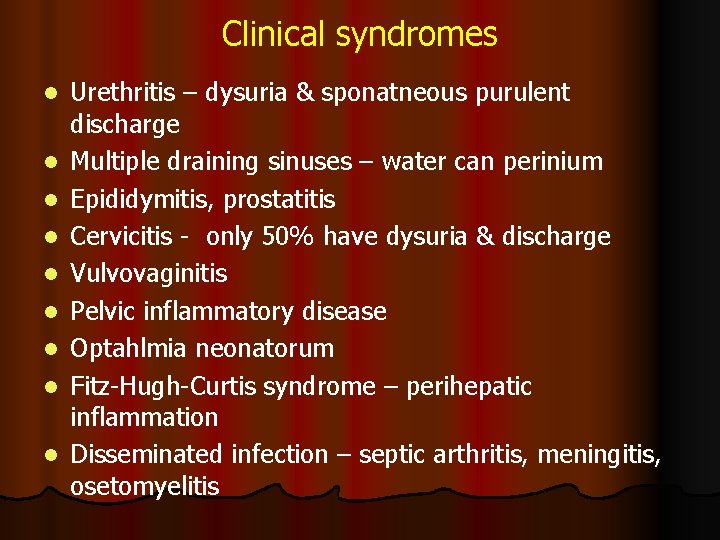
Clinical syndromes l l l l l Urethritis – dysuria & sponatneous purulent discharge Multiple draining sinuses – water can perinium Epididymitis, prostatitis Cervicitis - only 50% have dysuria & discharge Vulvovaginitis Pelvic inflammatory disease Optahlmia neonatorum Fitz-Hugh-Curtis syndrome – perihepatic inflammation Disseminated infection – septic arthritis, meningitis, osetomyelitis
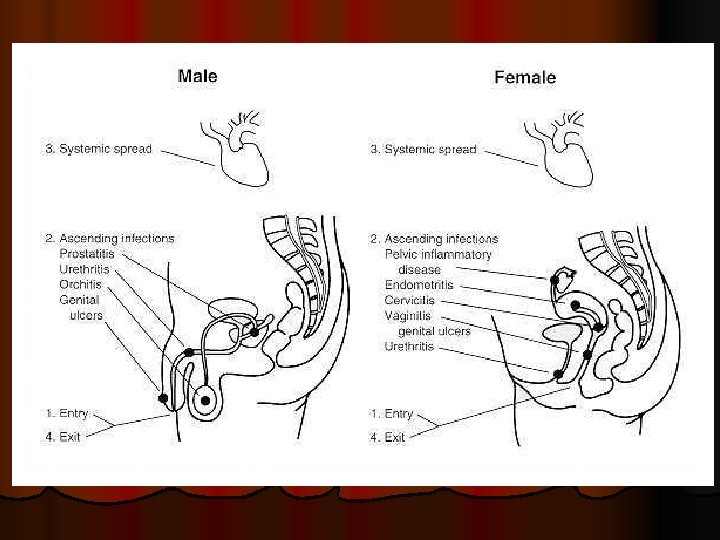


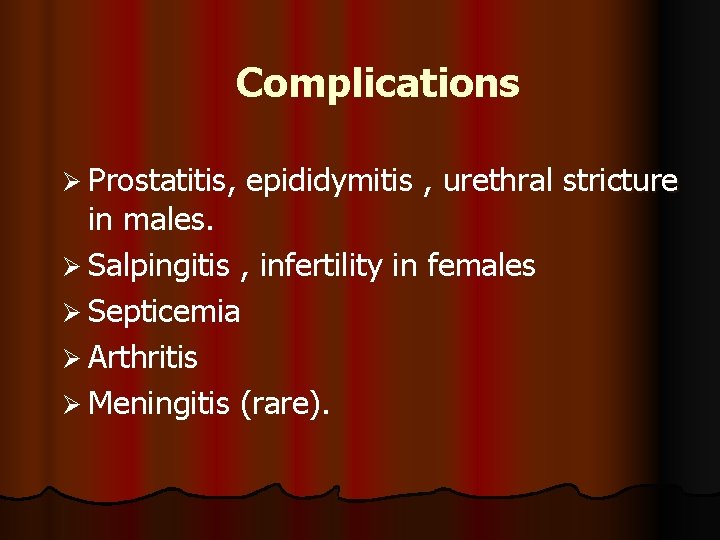
Complications Ø Prostatitis, epididymitis , urethral stricture in males. Ø Salpingitis , infertility in females Ø Septicemia Ø Arthritis Ø Meningitis (rare).
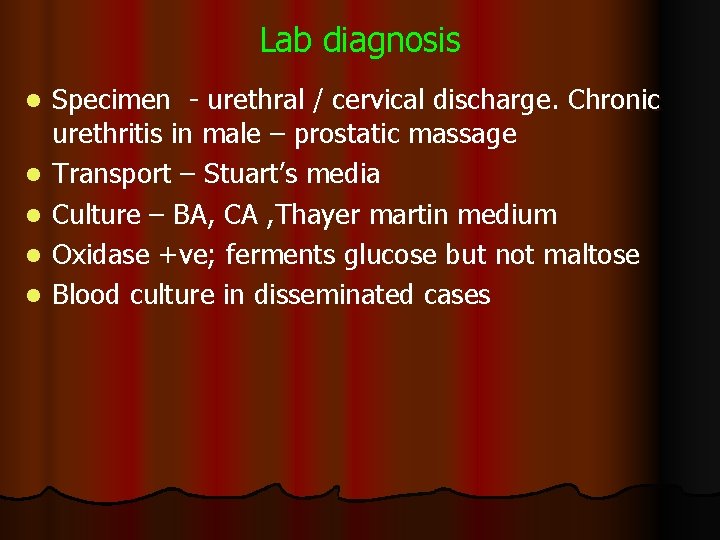
Lab diagnosis l l l Specimen - urethral / cervical discharge. Chronic urethritis in male – prostatic massage Transport – Stuart’s media Culture – BA, CA , Thayer martin medium Oxidase +ve; ferments glucose but not maltose Blood culture in disseminated cases
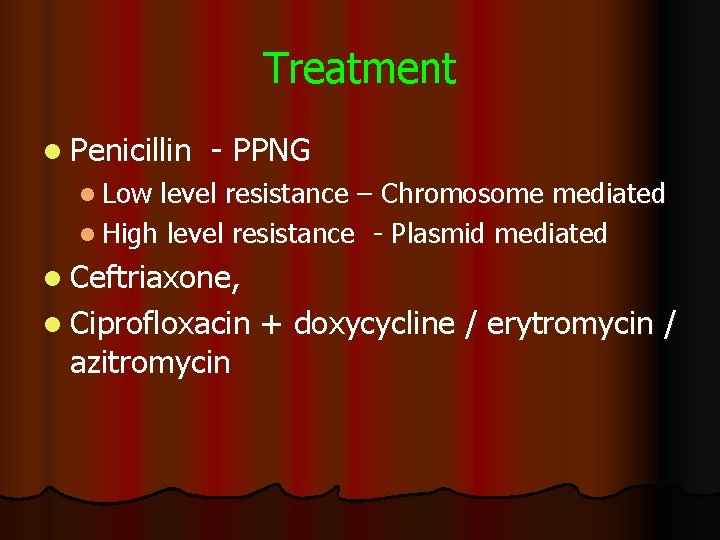
Treatment l Penicillin - PPNG l Low level resistance – Chromosome mediated l High level resistance - Plasmid mediated l Ceftriaxone, l Ciprofloxacin azitromycin + doxycycline / erytromycin /
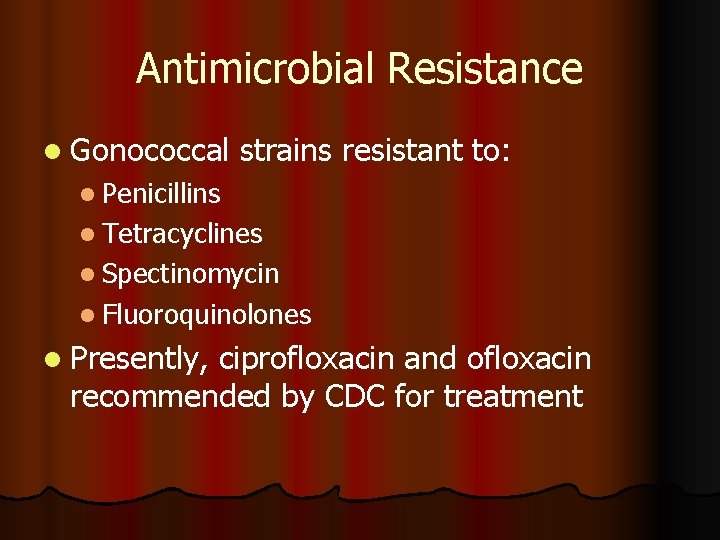
Antimicrobial Resistance l Gonococcal strains resistant to: l Penicillins l Tetracyclines l Spectinomycin l Fluoroquinolones l Presently, ciprofloxacin and ofloxacin recommended by CDC for treatment
Commensal Neisseriae N. pharyngis, N. flava, N. sicca, . . Ø In mucous mem. Of mouth, nose, pharynx, less common in genital tract. Ø Differ. From pathogenic one: Ø § § grow in ordinary media( no CO 2) at room temp. rough, pigmented acid from a number of CHOs
- Slides: 31