Necrotizing Soft Tissue Infections SIS 35 th Annual

- Slides: 23
Necrotizing Soft Tissue Infections SIS 35 th Annual Meeting Four Seasons Westlake Village, CA Addison K. May, MD, FACS, FCCM Professor of Surgery and Anesthesiology Division of Trauma and Surgical Critical Care Vanderbilt University Medical Center
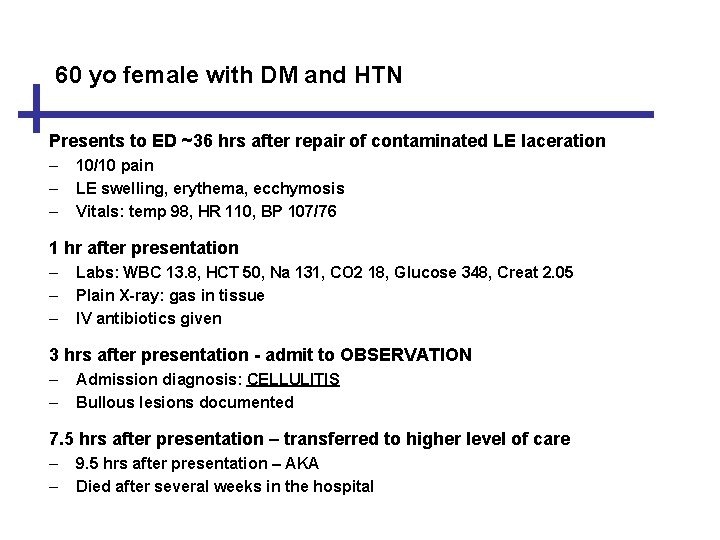
60 yo female with DM and HTN Presents to ED ~36 hrs after repair of contaminated LE laceration – – – 10/10 pain LE swelling, erythema, ecchymosis Vitals: temp 98, HR 110, BP 107/76 1 hr after presentation – – – Labs: WBC 13. 8, HCT 50, Na 131, CO 2 18, Glucose 348, Creat 2. 05 Plain X-ray: gas in tissue IV antibiotics given 3 hrs after presentation - admit to OBSERVATION – – Admission diagnosis: CELLULITIS Bullous lesions documented 7. 5 hrs after presentation – transferred to higher level of care – – 9. 5 hrs after presentation – AKA Died after several weeks in the hospital
Disclosures Research funding: • Fresenius Kabi • Bayer Health. Care Pharmaceuticals Inc • Cubist Pharmaceuticals, Inc • BHR Pharma, LLC Consultant: • Atox Bio, Ltd.
What’s New in NSTI? • Ovid: 2005 – 2015 for NSTI, NF, Fournier’s, Gas Gangrene – English language, human: 1508 – English, human, review articles: 215 – Prospective studies: 36 – 25 NSTI/NF/Fournier’s (2 hyperbaric) – 7 Streptococcal/Vibrio epidemiology – 4 total hyperbaric – Randomized trials: 0 • 1 RTC in NSTI: Bulger, EM. JAMA Surg. 2014; 149: 528 -536.
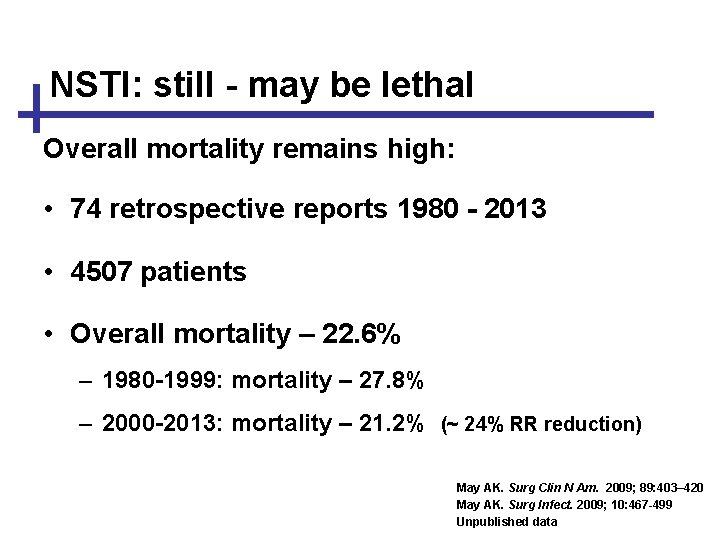
NSTI: still - may be lethal Overall mortality remains high: • 74 retrospective reports 1980 - 2013 • 4507 patients • Overall mortality – 22. 6% – 1980 -1999: mortality – 27. 8% – 2000 -2013: mortality – 21. 2% (~ 24% RR reduction) May AK. Surg Clin N Am. 2009; 89: 403– 420 May AK. Surg Infect. 2009; 10: 467 -499 Unpublished data
Today’s focus 1. Importance of nomenclature and implications of pathophysiology 2. Establishing the diagnosis 3. Important components of therapy
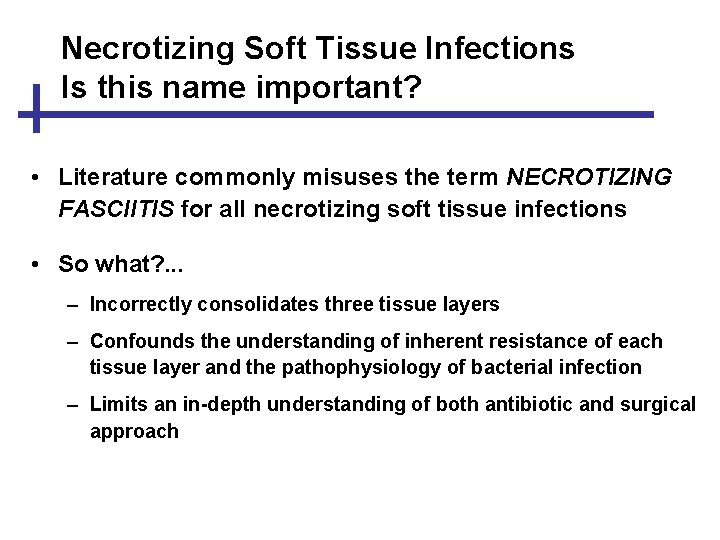
Necrotizing Soft Tissue Infections Is this name important? • Literature commonly misuses the term NECROTIZING FASCIITIS for all necrotizing soft tissue infections • So what? . . . – Incorrectly consolidates three tissue layers – Confounds the understanding of inherent resistance of each tissue layer and the pathophysiology of bacterial infection – Limits an in-depth understanding of both antibiotic and surgical approach
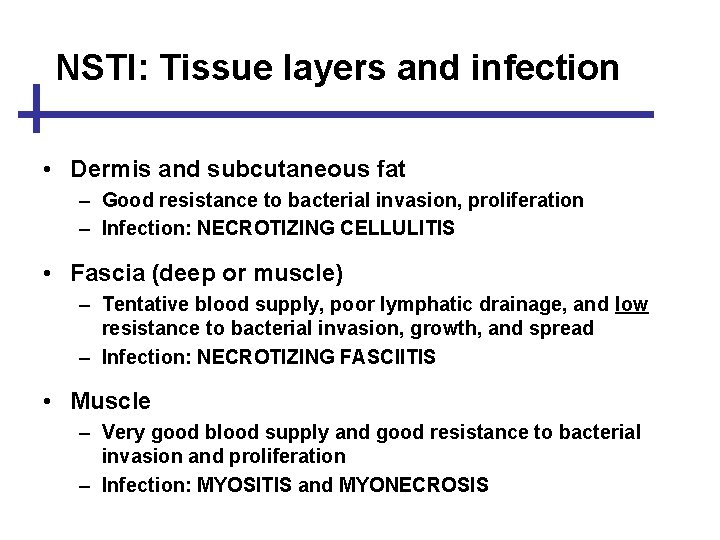
NSTI: Tissue layers and infection • Dermis and subcutaneous fat – Good resistance to bacterial invasion, proliferation – Infection: NECROTIZING CELLULITIS • Fascia (deep or muscle) – Tentative blood supply, poor lymphatic drainage, and low resistance to bacterial invasion, growth, and spread – Infection: NECROTIZING FASCIITIS • Muscle – Very good blood supply and good resistance to bacterial invasion and proliferation – Infection: MYOSITIS and MYONECROSIS
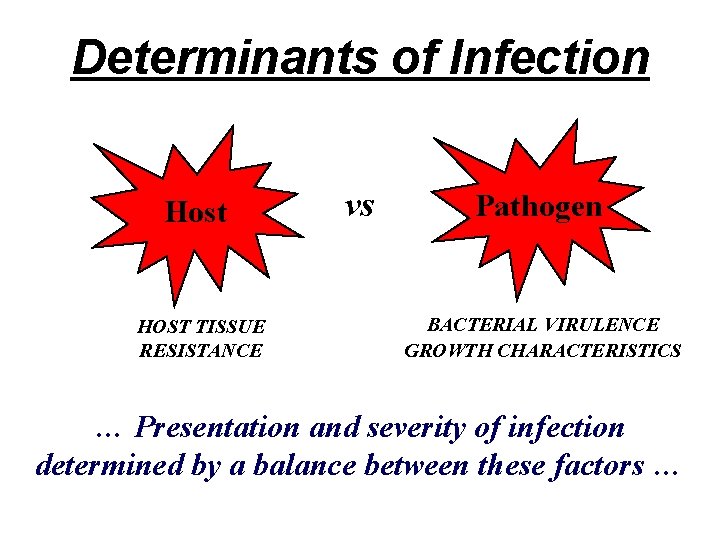
Determinants of Infection Host HOST TISSUE RESISTANCE vs Pathogen BACTERIAL VIRULENCE GROWTH CHARACTERISTICS … Presentation and severity of infection determined by a balance between these factors …
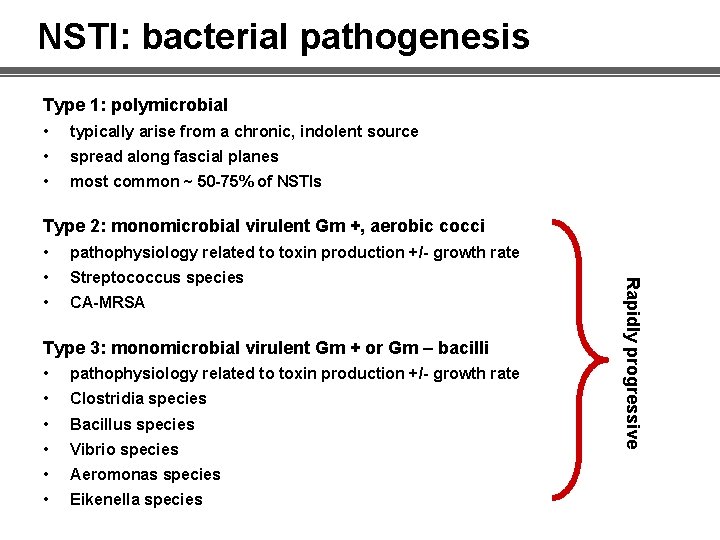
NSTI: bacterial pathogenesis Type 1: polymicrobial • typically arise from a chronic, indolent source • spread along fascial planes • most common ~ 50 -75% of NSTIs Type 2: monomicrobial virulent Gm +, aerobic cocci pathophysiology related to toxin production +/- growth rate • Streptococcus species • CA-MRSA Type 3: monomicrobial virulent Gm + or Gm – bacilli • pathophysiology related to toxin production +/- growth rate • Clostridia species • Bacillus species • Vibrio species • Aeromonas species • Eikenella species Rapidly progressive •
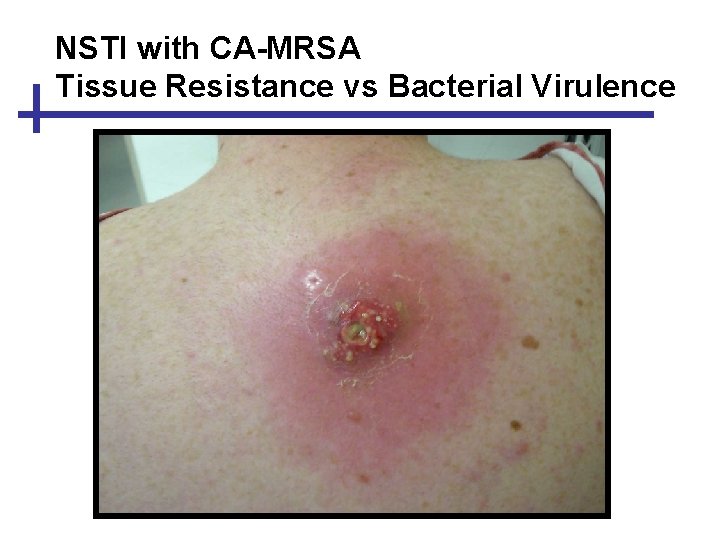
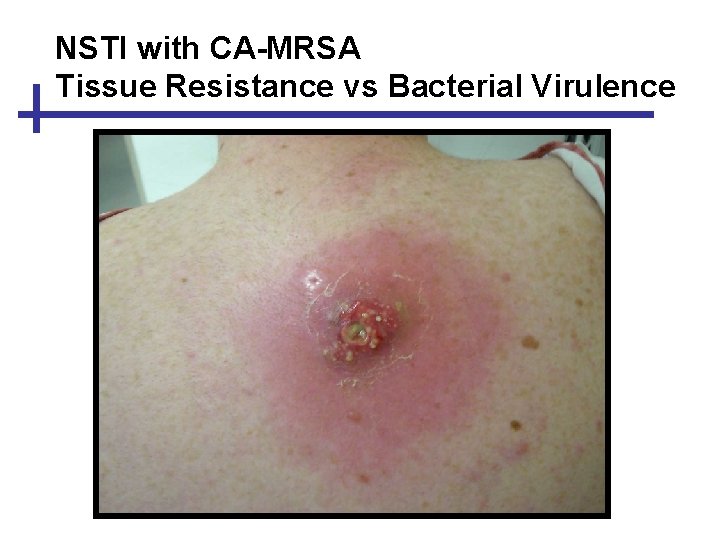
NSTI with CA-MRSA Tissue Resistance vs Bacterial Virulence
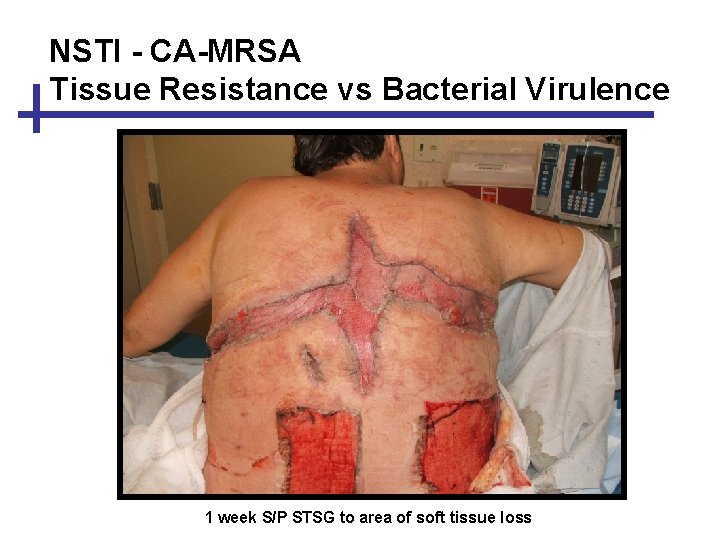
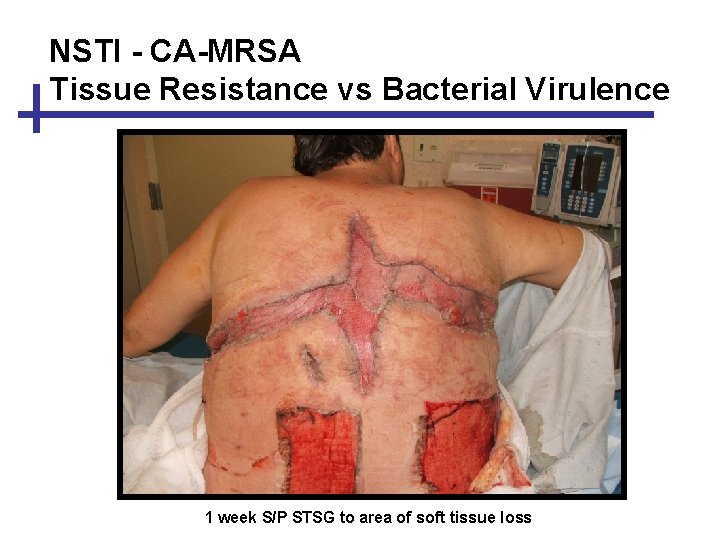
NSTI - CA-MRSA Tissue Resistance vs Bacterial Virulence 1 week S/P STSG to area of soft tissue loss
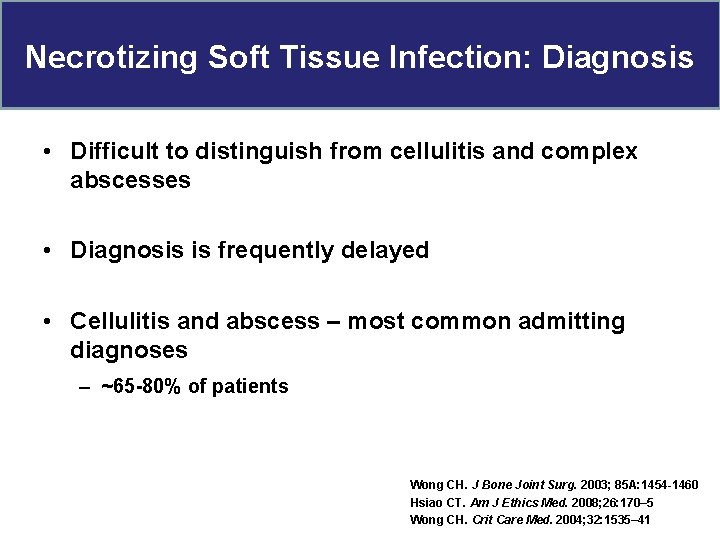
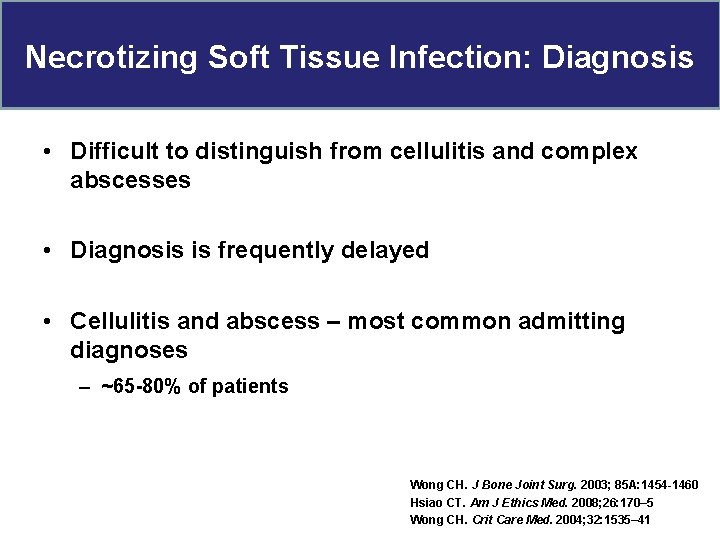
Necrotizing Soft Tissue Infection: Diagnosis • Difficult to distinguish from cellulitis and complex abscesses • Diagnosis is frequently delayed • Cellulitis and abscess – most common admitting diagnoses – ~65 -80% of patients Wong CH. J Bone Joint Surg. 2003; 85 A: 1454 -1460 Hsiao CT. Am J Ethics Med. 2008; 26: 170– 5 Wong CH. Crit Care Med. 2004; 32: 1535– 41
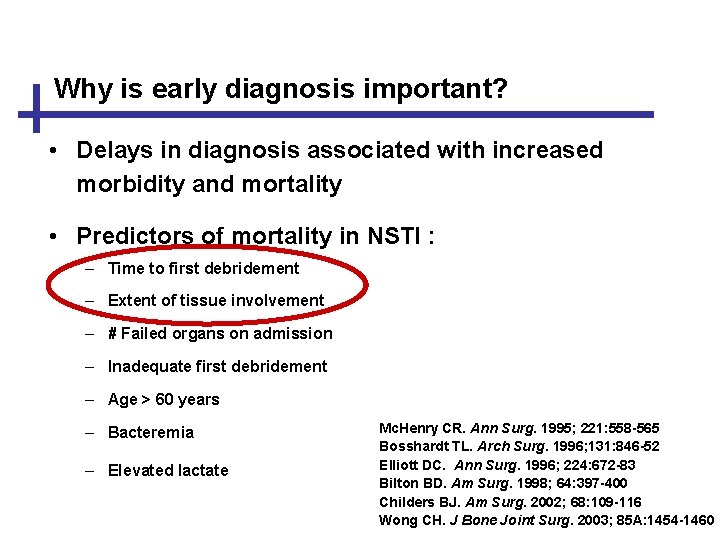
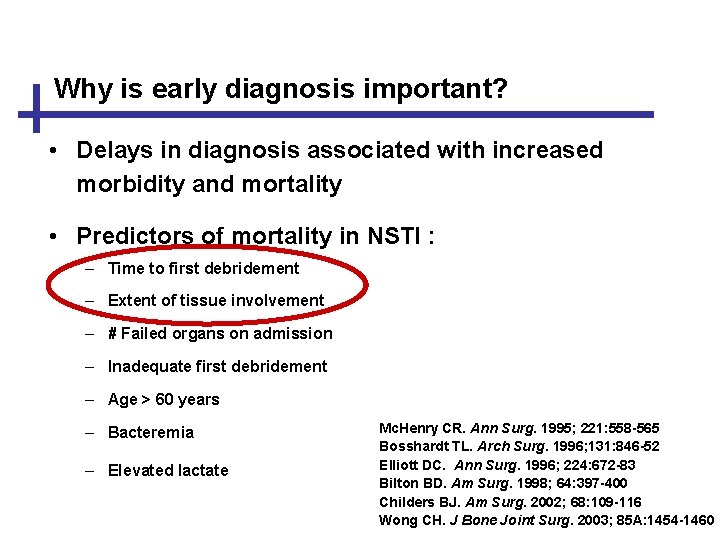
Why is early diagnosis important? • Delays in diagnosis associated with increased morbidity and mortality • Predictors of mortality in NSTI : – Time to first debridement – Extent of tissue involvement – # Failed organs on admission – Inadequate first debridement – Age > 60 years – Bacteremia – Elevated lactate Mc. Henry CR. Ann Surg. 1995; 221: 558 -565 Bosshardt TL. Arch Surg. 1996; 131: 846 -52 Elliott DC. Ann Surg. 1996; 224: 672 -83 Bilton BD. Am Surg. 1998; 64: 397 -400 Childers BJ. Am Surg. 2002; 68: 109 -116 Wong CH. J Bone Joint Surg. 2003; 85 A: 1454 -1460
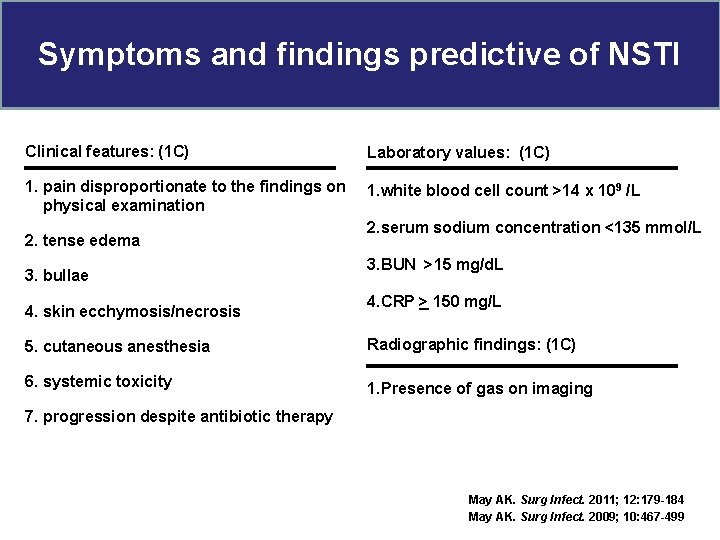
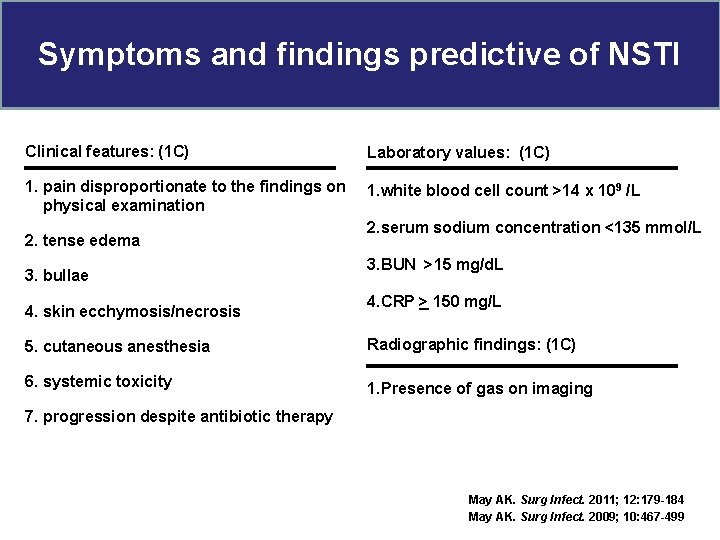
Symptoms and findings predictive of NSTI Clinical features: (1 C) Laboratory values: (1 C) 1. pain disproportionate to the findings on physical examination 1. white blood cell count >14 x 109 /L 2. tense edema 3. bullae 4. skin ecchymosis/necrosis 2. serum sodium concentration <135 mmol/L 3. BUN >15 mg/d. L 4. CRP > 150 mg/L 5. cutaneous anesthesia Radiographic findings: (1 C) 6. systemic toxicity 1. Presence of gas on imaging 7. progression despite antibiotic therapy May AK. Surg Infect. 2011; 12: 179 -184 May AK. Surg Infect. 2009; 10: 467 -499
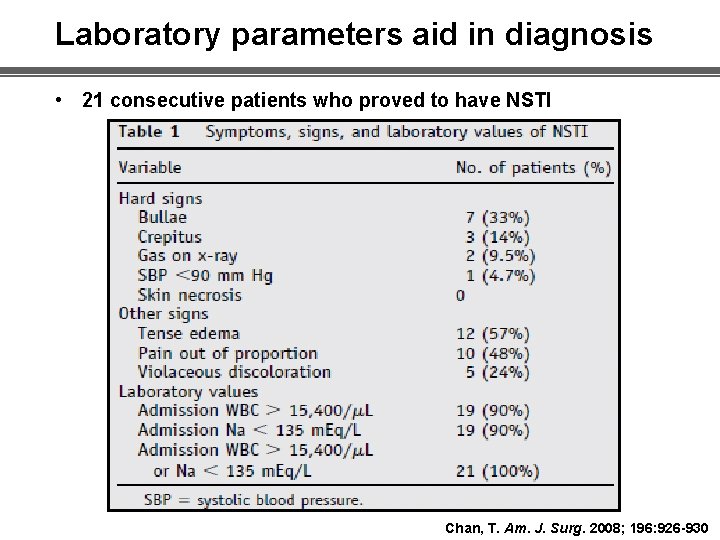
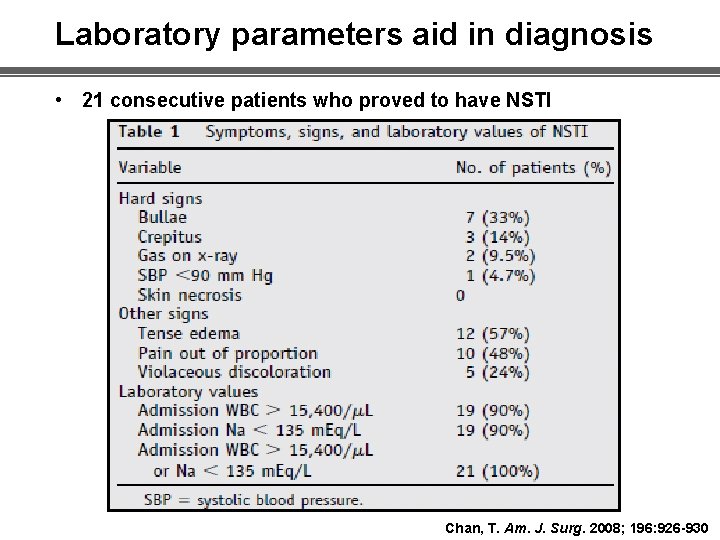
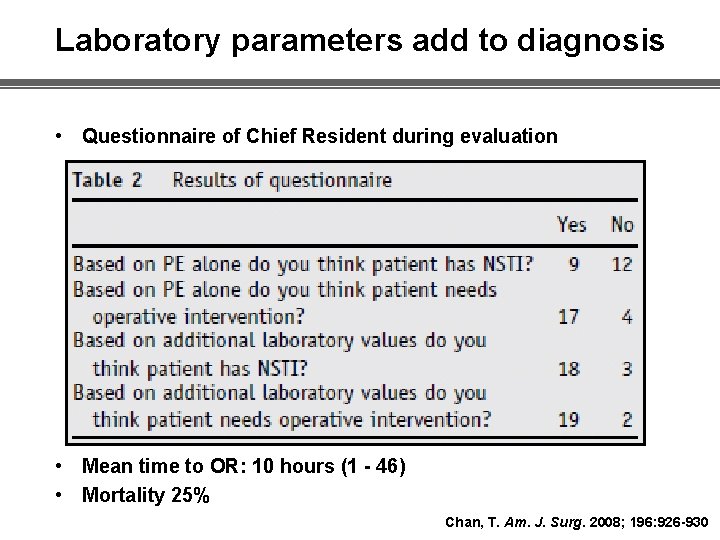
Laboratory parameters aid in diagnosis • 21 consecutive patients who proved to have NSTI Chan, T. Am. J. Surg. 2008; 196: 926 -930
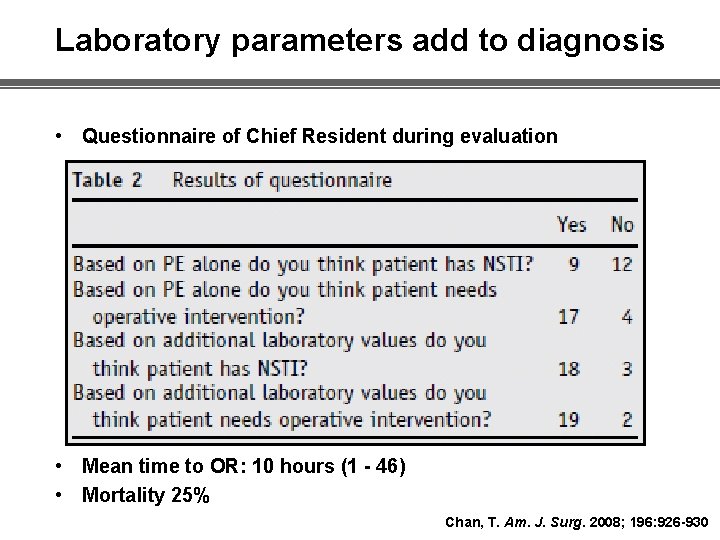
Laboratory parameters add to diagnosis • Questionnaire of Chief Resident during evaluation • Mean time to OR: 10 hours (1 - 46) • Mortality 25% Chan, T. Am. J. Surg. 2008; 196: 926 -930
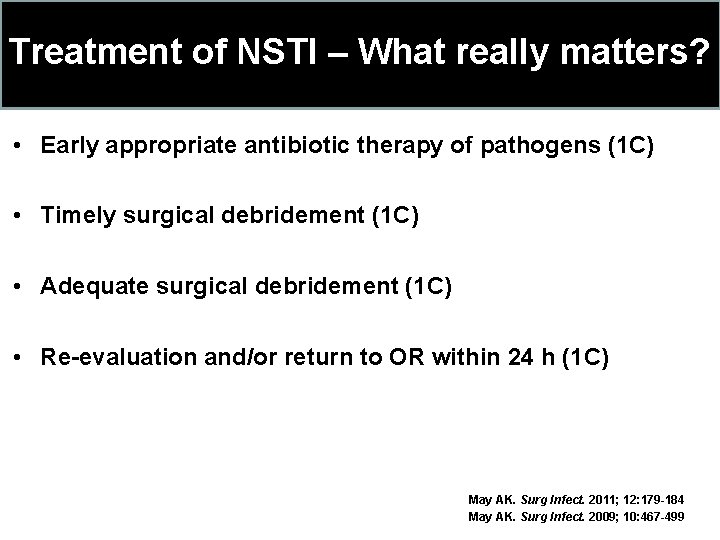
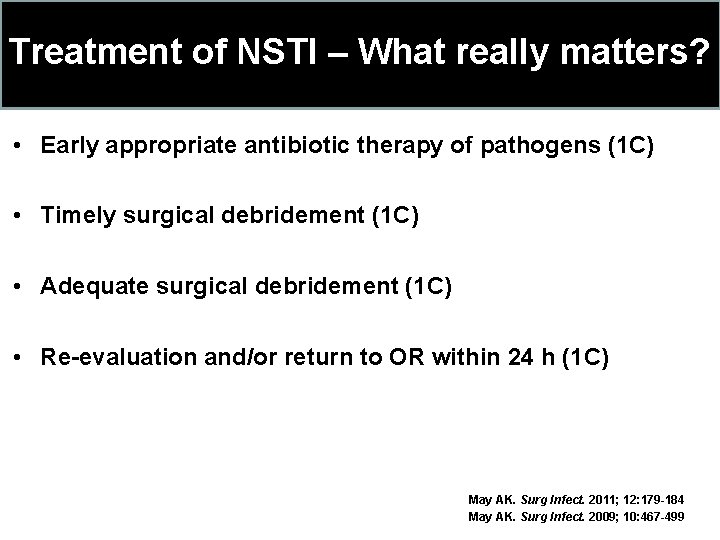
Treatment of NSTI – What really matters? • Early appropriate antibiotic therapy of pathogens (1 C) • Timely surgical debridement (1 C) • Adequate surgical debridement (1 C) • Re-evaluation and/or return to OR within 24 h (1 C) May AK. Surg Infect. 2011; 12: 179 -184 May AK. Surg Infect. 2009; 10: 467 -499
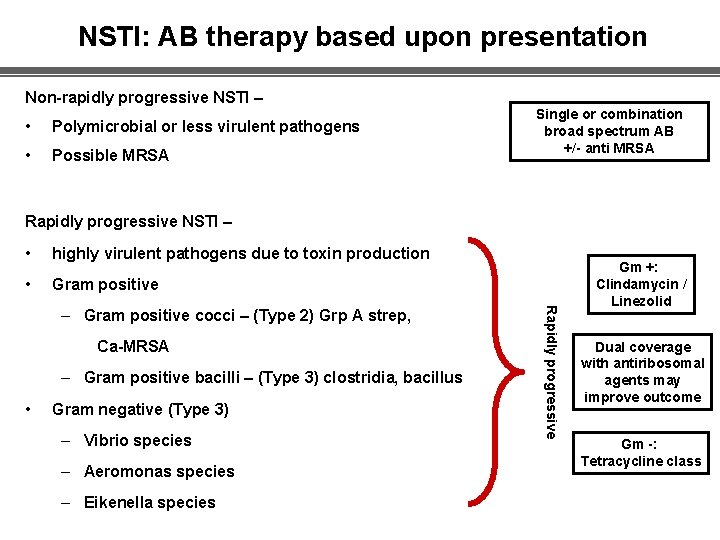
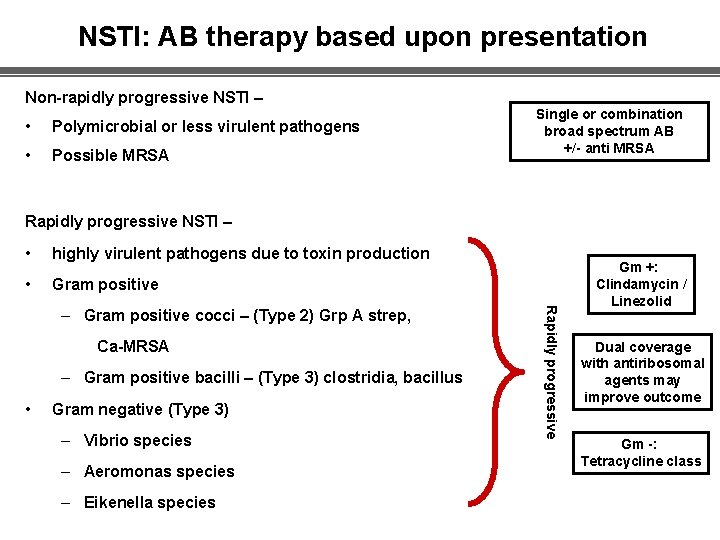
NSTI: AB therapy based upon presentation Non-rapidly progressive NSTI – • Polymicrobial or less virulent pathogens • Possible MRSA Single or combination broad spectrum AB +/- anti MRSA Rapidly progressive NSTI – • highly virulent pathogens due to toxin production • Gram positive Ca-MRSA – Gram positive bacilli – (Type 3) clostridia, bacillus • Gram negative (Type 3) – Vibrio species – Aeromonas species – Eikenella species Rapidly progressive – Gram positive cocci – (Type 2) Grp A strep, Gm +: Clindamycin / Linezolid Dual coverage with antiribosomal agents may improve outcome Gm -: Tetracycline class
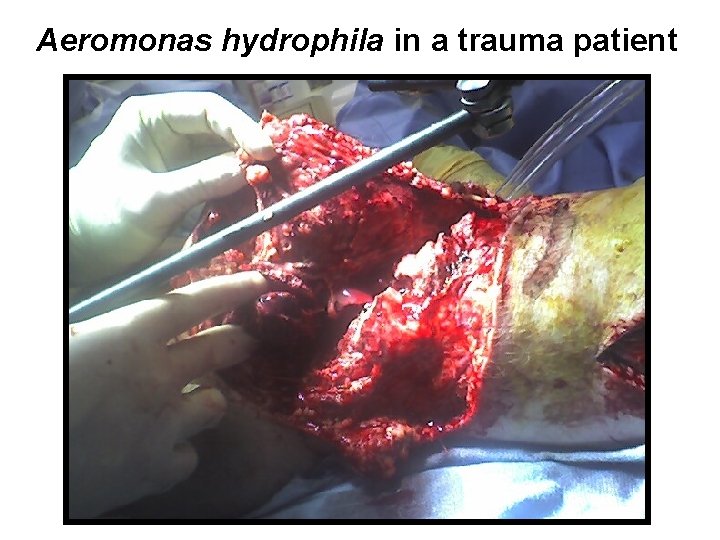
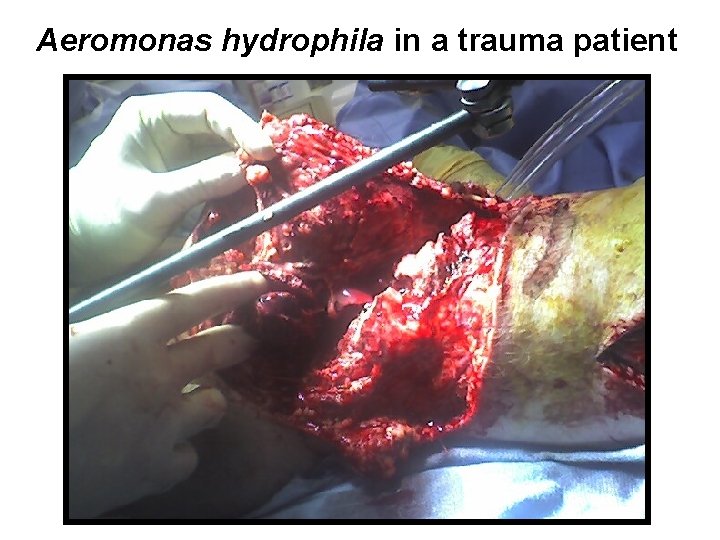
Aeromonas hydrophila in a trauma patient
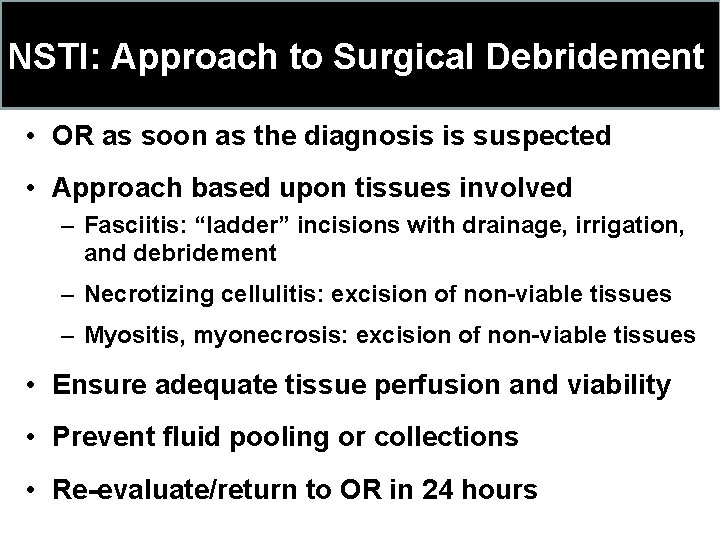
NSTI: Approach to Surgical Debridement • OR as soon as the diagnosis is suspected • Approach based upon tissues involved – Fasciitis: “ladder” incisions with drainage, irrigation, and debridement – Necrotizing cellulitis: excision of non-viable tissues – Myositis, myonecrosis: excision of non-viable tissues • Ensure adequate tissue perfusion and viability • Prevent fluid pooling or collections • Re-evaluate/return to OR in 24 hours
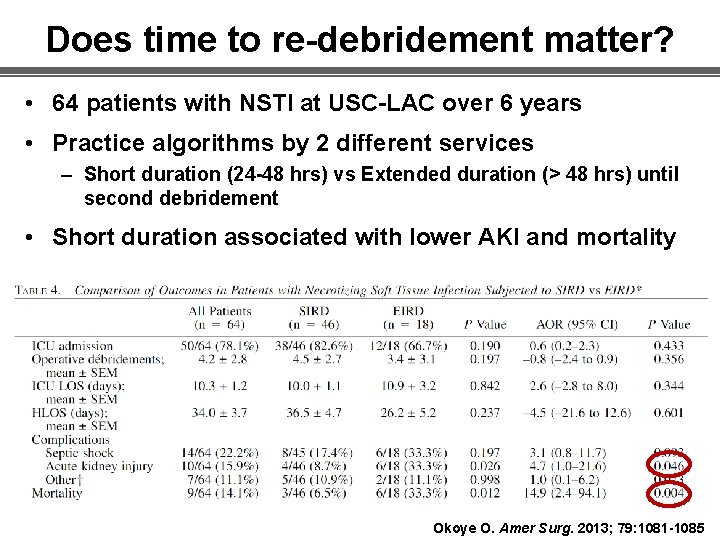
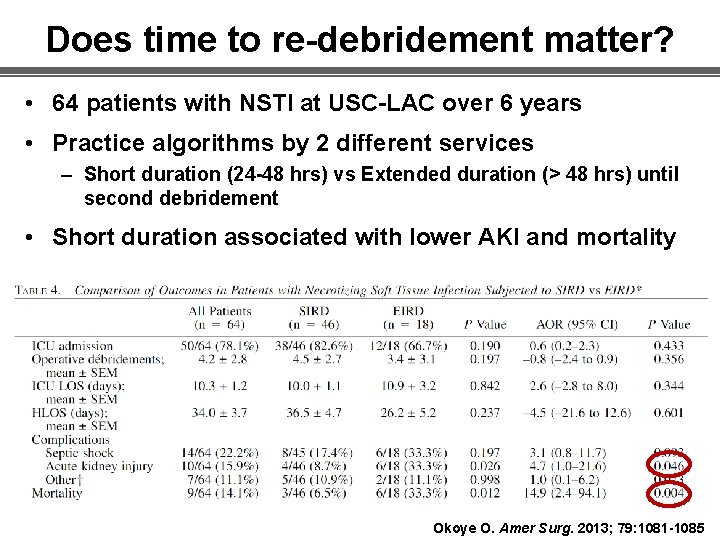
Does time to re-debridement matter? • 64 patients with NSTI at USC-LAC over 6 years • Practice algorithms by 2 different services – Short duration (24 -48 hrs) vs Extended duration (> 48 hrs) until second debridement • Short duration associated with lower AKI and mortality Okoye O. Amer Surg. 2013; 79: 1081 -1085

Necrotizing Soft Tissue Infections SIS 35 th Annual Meeting Four Seasons Westlake Village, CA Thank you for your attention