NECROTIZING PANCREATITIS A CASE STUDY PRESENTATION BY MIKE
NECROTIZING PANCREATITIS A CASE STUDY PRESENTATION BY MIKE MELTON
CASE STUDY OBJECTIVES • • • Introduction to the Problem Introduction to the Subject Patient History Nutrition Diagnosis and PES Statement Interventions Proposed Outcomes to Monitor and Evaluate Conclusion Resources Questions and (hopefully) Answers
INTRODUCTION TO THE PROBLEM • The Anatomy and Function of the Pancreas • Chronic vs Acute • Atlanta Classifications of Acute Pancreatitis(1992)¹ • Inflammation of parenchyma and peripancreatic tissues • Inflammation plus necrosis • Mild, Moderately Severe, or Severe. • No organ failure with local complications • Transient organ failure with or without complications • Organ failure > 48 hrs involving one or multiple organs.
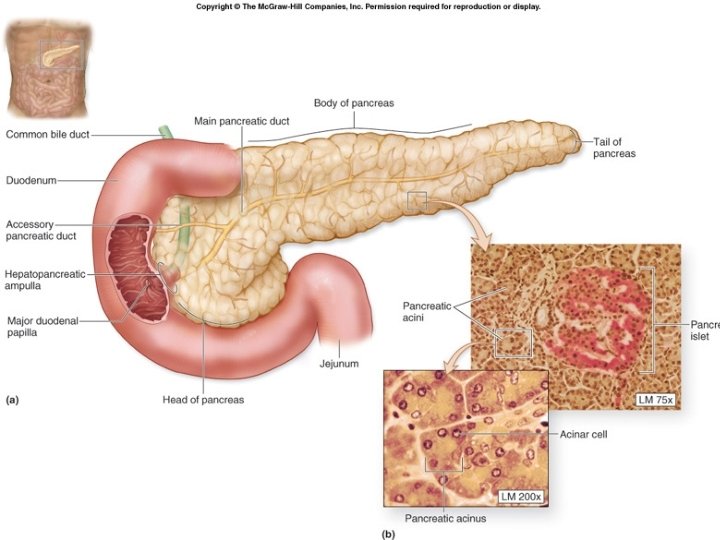
INTRODUCTION TO THE PROBLEM • The Anatomy and Function of the Pancreas • Chronic vs Acute • Atlanta Classifications of Acute Pancreatitis(1992)¹ • Inflammation of parenchyma and peripancreatic tissues • Inflammation plus necrosis • Mild, Moderately Severe, or Severe. • No organ failure with local complications • Transient organ failure with or without complications • Organ failure > 48 hrs involving one or multiple organs.
INTRODUCTION TO THE PROBLEM • Predictors of Severity² • • • Age > 75 years old Alcohol abuse Short time onset of Symptoms Obesity (BMI > 30) Organ Failure (esp. . Cardiovascular, Respiratory, Renal) APACHE (Acute Physiology and Chronic Health Examination) II score > 8 within 24 hrs • Ranson’s score >3 • Persistent SIRS (Systemic Inflammatory Response Syndrome) • Elevated hematocrit (>44 percent), blood urea nitrogen (BUN) (>20 mg/d. L), or creatinine (>1. 8 mg/d. L)
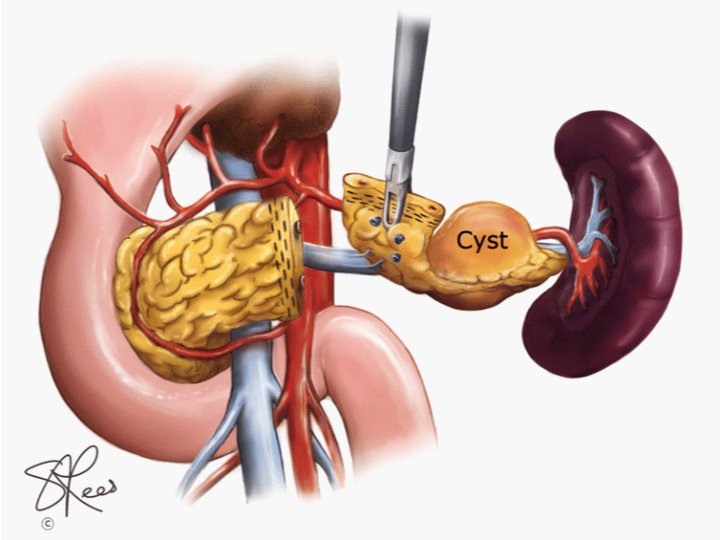
INTRODUCTION TO THE PROBLEM • Local Complications³ • • Acute Peripancreatic Fluid Collection (usually < 10 days) Pancreatic Pseudocyst (usually >4 weeks) Acute Necrotic Collection vs Walled off Necrosis Sterile vs Infected Necrosis Splanchnic Venous Thrombosis Pseudoaneurism Abdominal Compartment Syndrome Exacerbation of Comorbidities
INTRODUCTION TO THE PROBLEM • Causes • • • Gallstones (35 -40%) Alcohol Abuse Biliary Sludge and Microlithiasis Smoking Genetic Mutations Hypertriglyceridemia • Medical Treatment • Aggressive fluid replacement if not contraindicated at 5 -10 ml/Kg per hour of normal saline or lactated ringers. • Pain management • Removal of necrotic tissue
PATIENT HISTORY: DS • • White, Male, Age 28 at first admission, 31 now Married, no kids, dog 5’ 10” 234 lb (106. 5 kg) first admit, 160 lb (73 kg) now Hx alcohol and tobacco use- denies significant intake Hx depression and anxiety. Married with a dog Presented initially to Community Anderson with abdominal pain, nausea, and vomiting.
PATIENT HISTORY: DS • Initial dx acute gallstone pancreatitis (3 Ranson criteria, mild), acute respiratory failure (hypoventilation r/t excessive sedation and abdominal distention), mild acute renal failure, tachycardia r/t severe dehydration, hypovolemic shock. Intubates, ventilated, and sedated. • 4 weeks later, s/p first laparotomy his condition called acute necrotizing biliary pancreatitis. + necrosed neck with large disconnected remnant, pseudocyst with abdominal compartment syndrome, ascites, small clot in portal vein w/o thrombosis. Transfer to CHN 7/15/14.
PATIENT HISTORY: DS • Physical exam at CHN: • • + anasarca, pitting edema lower extremities and abdominal wall + tachycardic + distended and tense abdomen + scrotal and penile edema • Pancreatic debridement and drainage by the Dr. Howard, 7/16/14. • Second exploratory laparotomy 7/22/14 and abdomen left open with vicryl mesh.
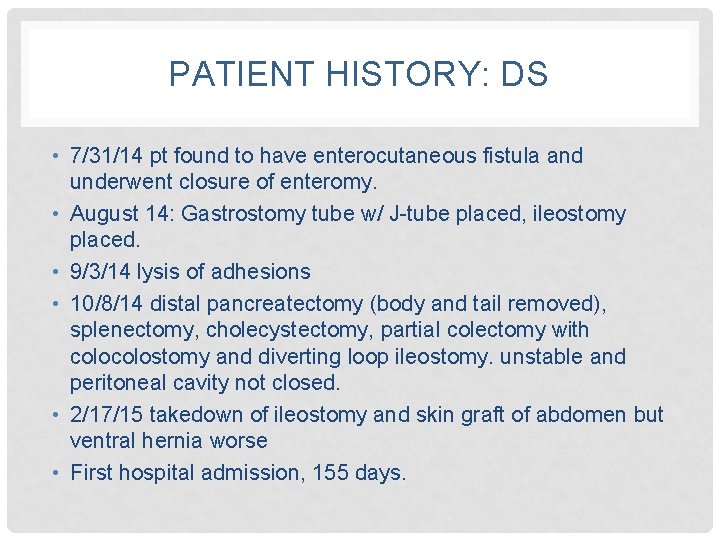
PATIENT HISTORY: DS • 7/31/14 pt found to have enterocutaneous fistula and underwent closure of enteromy. • August 14: Gastrostomy tube w/ J-tube placed, ileostomy placed. • 9/3/14 lysis of adhesions • 10/8/14 distal pancreatectomy (body and tail removed), splenectomy, cholecystectomy, partial colectomy with colostomy and diverting loop ileostomy. unstable and peritoneal cavity not closed. • 2/17/15 takedown of ileostomy and skin graft of abdomen but ventral hernia worse • First hospital admission, 155 days.
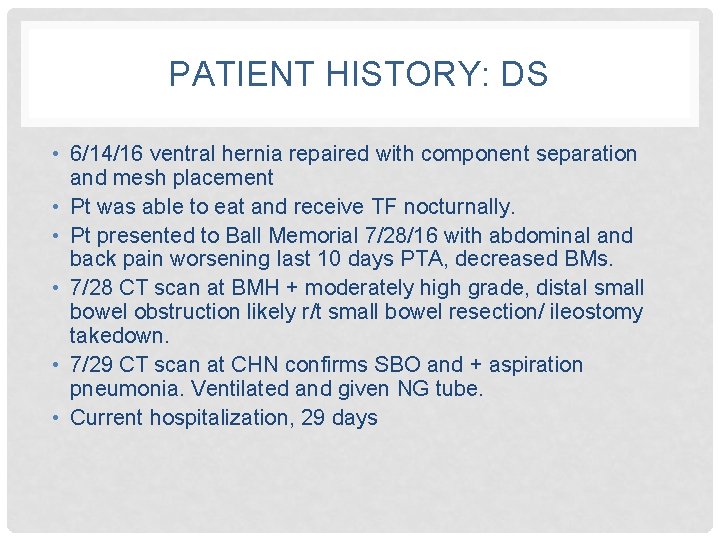
PATIENT HISTORY: DS • 6/14/16 ventral hernia repaired with component separation and mesh placement • Pt was able to eat and receive TF nocturnally. • Pt presented to Ball Memorial 7/28/16 with abdominal and back pain worsening last 10 days PTA, decreased BMs. • 7/28 CT scan at BMH + moderately high grade, distal small bowel obstruction likely r/t small bowel resection/ ileostomy takedown. • 7/29 CT scan at CHN confirms SBO and + aspiration pneumonia. Ventilated and given NG tube. • Current hospitalization, 29 days
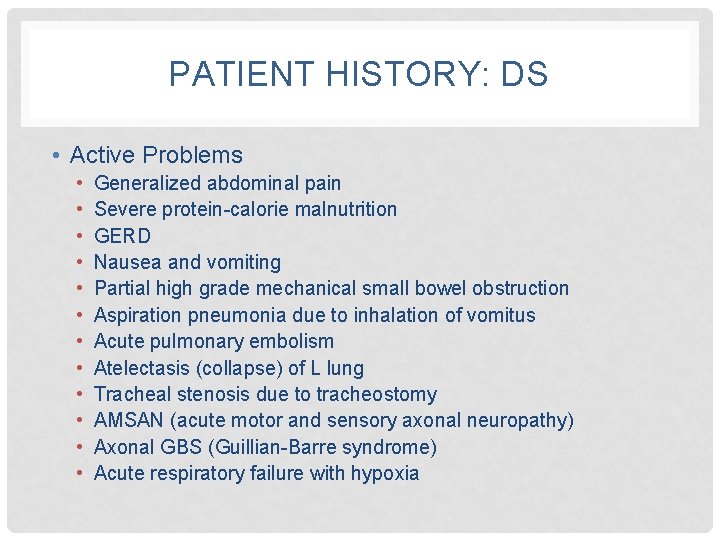
PATIENT HISTORY: DS • Active Problems • • • Generalized abdominal pain Severe protein-calorie malnutrition GERD Nausea and vomiting Partial high grade mechanical small bowel obstruction Aspiration pneumonia due to inhalation of vomitus Acute pulmonary embolism Atelectasis (collapse) of L lung Tracheal stenosis due to tracheostomy AMSAN (acute motor and sensory axonal neuropathy) Axonal GBS (Guillian-Barre syndrome) Acute respiratory failure with hypoxia
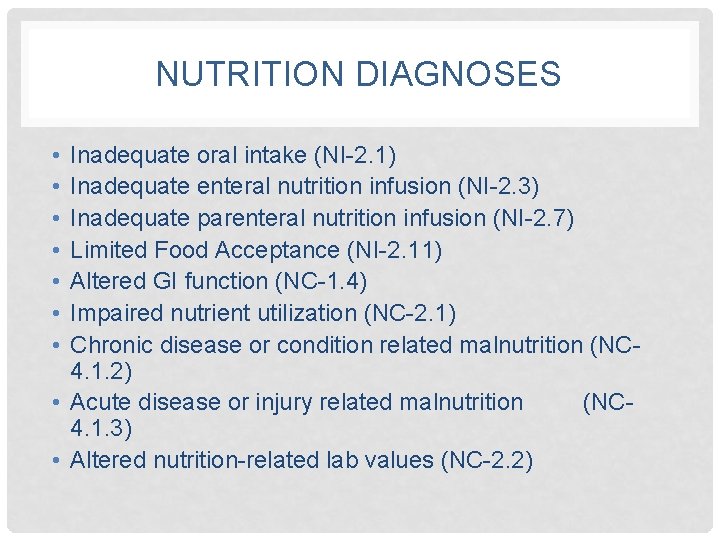
NUTRITION DIAGNOSES • • Inadequate oral intake (NI-2. 1) Inadequate enteral nutrition infusion (NI-2. 3) Inadequate parenteral nutrition infusion (NI-2. 7) Limited Food Acceptance (NI-2. 11) Altered GI function (NC-1. 4) Impaired nutrient utilization (NC-2. 1) Chronic disease or condition related malnutrition (NC 4. 1. 2) • Acute disease or injury related malnutrition (NC 4. 1. 3) • Altered nutrition-related lab values (NC-2. 2)
PES STATEMENTS • Altered GI function r/t changes in GI tract motility AEB pancreatitis, po & gastric TF intolerance. • Inadequate oral intake r/t inability to consume sufficient energy AEB small bowel obstruction, ventilation, and recent weight loss (74 lb, 33. 5 kg, 31. 6% x last 2 years).
INTERVENTIONS • Early (within 48 hrs of admission) enteral nutrition better outcomes than NPO to allow pancreas to rest and better outcomes than TPN with severe pancreatitis. 4 • Enteral feeding should be peptide-based, with medium chain triglycerides. TF should provide 25 -35 kcal/ kg body weight; 1. 2 -1. 5 gm protein/kg body weight. 5 • Supplement with thiamin and folic acid (esp. . alcoholics) • When ready for po, encourage low-fat diet therapy using teach-back!
MONITOR AND EVALUATE • • EN/PN nutrition intake tolerance/residuals with EN Weight/ Weight Changes Labs • Potassium, Magnesium, Phosphorous with risk for Refeeding Syndrome esp. . after several days NPO. • TG, liver function tests, and prealbumin weekly (esp. TPN) • BMP, Magnesium, Phosphorous daily (esp. TPN) • GI function and BM • Plan of Care
CONCLUSION • Pancreatitis is inflammation of the pancreas. It can be mild to severe, acute or chronic. • Introduction to the Subject • Patient History • Nutrition Diagnosis and PES Statement • Interventions
REFERENCES 1. Bradley E. A clinically based classification-system for acute pancreatitis: Summary of the international symposium on acute-pancreatitis, Atlanta, GA, September 11 Through 13, 1992. Archives of Surgery. 1993; 128: 586 -590. 2. Wu, B. U. , & Banks, P. A. (2013). Clinical Management of Patients With Acute Pancreatitis. GASTROENTEROLOGY, 144(6), 1272 -1281. doi: 10. 1053/j. gastro. 2013. 01. 075
REFERENCES 3. Anand N, Park J, Wu B. Modern Management of Acute Pancreatitis. Gastroenterology Clinics of North America. 2012; 41: 1 -1. 4. Mc. Clave SA, Martindale RG, Vanek VW, Mc. Carthy M, Roberts P, Taylor B, Ochoa JB, Napolitano L, Cresci G; ASPEN Board of Directors; American College of Critical Care Medicine; Society of Critical Care Medicine. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN). JPEN J Parenter Enteral Nutr. 2009; 33(3): 277 -316
REFERENCES 5. Mirtallo J, Forbes A, Mc. Clave S, Jensen G, Waitzberg D, Davies A. International consensus guidelines for nutrition therapy in pancreatitis. JPEN J Parenter Enteral Nutr. 2012; 36(3): 284 -291 5. Pancreatitis. Nutrition Care Manual Web Site. https: //www. nutritioncaremanual. org/topic. cfm? ncm_categor y_id=1&lv 1=5522&lv 2=19869&ncm_toc_id=19869&ncm_he ading=& Date Published unknown. Accessed August 14, 2016. 6. Management of Acute Pancreatitis. Up to Date Web site. http: //www. uptodate. com/contents/ management-of-acutepancreatitis Updated November 19, 2015. Accessed August 14, 2016.
QUESTIONS AND ANSWERS • Why did the chicken cross the road? • How much wood would a woodchuck if a woodchuck could chuck wood? • What is the air speed velocity of an unladen swallow? • Rhode Island is neither a road nor an island. Discuss amongst yourself. • Why can’t you hear a pterodactyl going to the restroom?
- Slides: 24