NECK MASSES Neck masses Introduction Common in children
- Slides: 24
NECK MASSES
Neck masses - Introduction Ø Common in children Lymphadenopathy – response to infection Ø Less common in adults Malignant until proven otherwise
Neck masses - Children Ø Larger lymphoid mass Ø Brisk lymphoreticular response Ø Present with lymphadenopathy after minor infections Ø Nodes may continue to enlarge after initiation of treatment and resolution of infection
Neck masses - Children Ø Causes - benign 80% - bacterial - viral - TB - HIV (Drainage from throat, nose, ear, scalp) - malignant 20% - lymphoma
Neck masses - Causes Ø Congenital (present at birth) Ø Developmental Ø Neck space infections Ø Salivary glands Ø Thyroid
Causes - Congenital Ø Lymphangiomata : Simple and cavernous Cystic hygroma Ø Dermoids : Epidermoid True dermoid Teratoid Ø Thyroglossal cysts : along tract of thyroglossal duct 90% midline may be only functioning thyroid tissue
Causes - Developmental Ø Branchial cysts - various theories - can become infected - treat with aspiration and antibiotics - excision when infection settled
Causes – Neck space infections Ø Parapharyngeal abscesses : - tonsillitis, quinsy, lower 3 rd molar abscess - swelling posterior to sternomastoid - stridor Ø Prevertebral / retropharyngeal abscess - acute suppurative otitis media
Causes – Salivary gland, Thyroid Ø Salivary gland : - mumps - recurrent parotitis of childhood - HIV Ø Thyroid - pubertal goitre :
Management Ø Clinical history and examination Ø Masses requiring investigation : - clinically suspicious - not responding after appropriate treatment (4 – 6 weeks) Ø Fine Needle Aspiration
Neck masses - Adults Ø Always presents as a pathological condition Ø History and clinical evaluation will lead to disease diagnosis in most cases Ø Neck masses usually related to diseases of the lymph nodes (80 % malignant) Ø Incidence of neoplasia increases with age
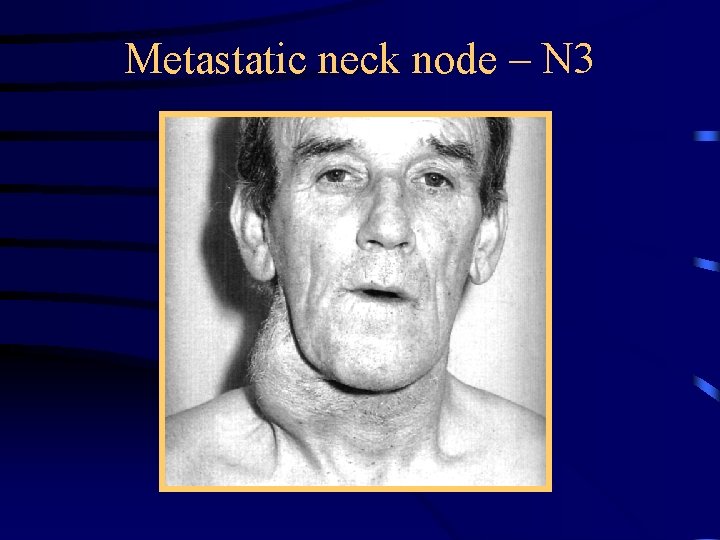
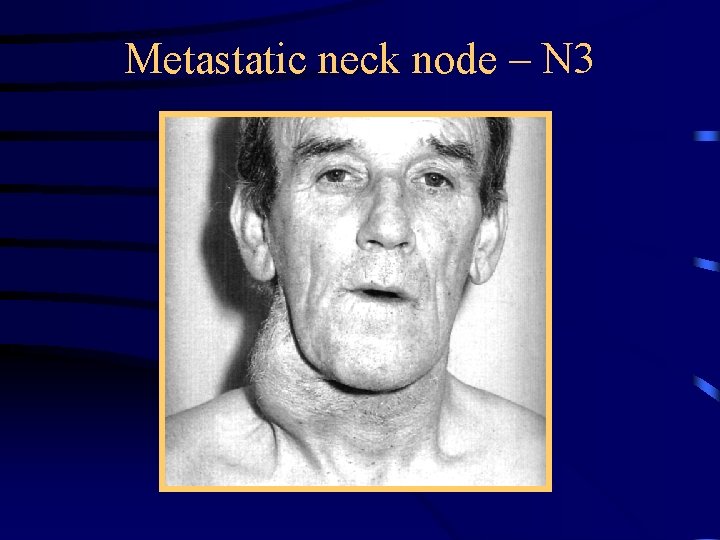
Metastatic neck node – N 3
Neck masses - Epidemiology Ø Heavy smoking and alcohol abuse Ø Adult male population ( > 40 years ) Ø Painless, slow growing mass ( level II/III ) Ø Radiation exposure in the past Ø Curative treatment in the distant past for other malignancy
Neck masses – History taking Ø Otalgia Ø Blocked nose Ø Epistaxis Ø Unilateral hearing loss Ø Dysphagia / Odynophagia Ø ( Hoarseness / Dysphonia, Stridor )
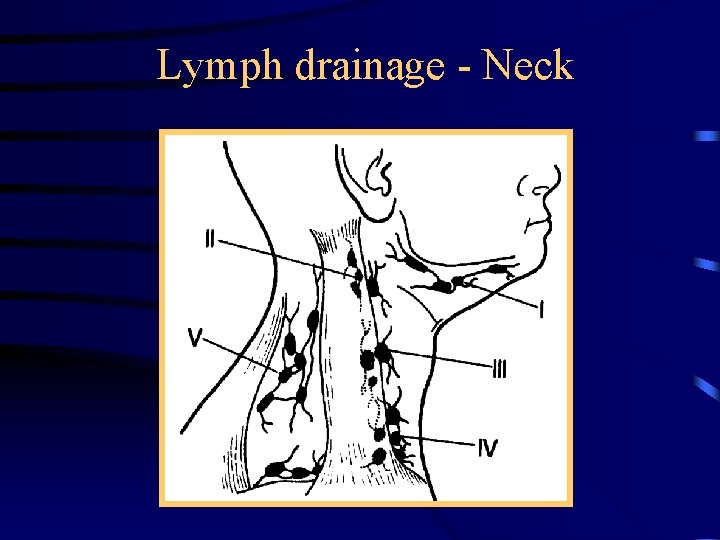
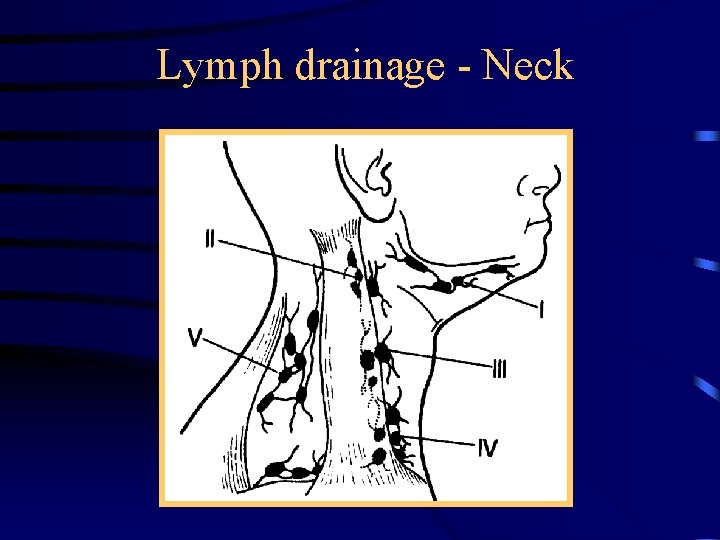
Lymph drainage - Neck
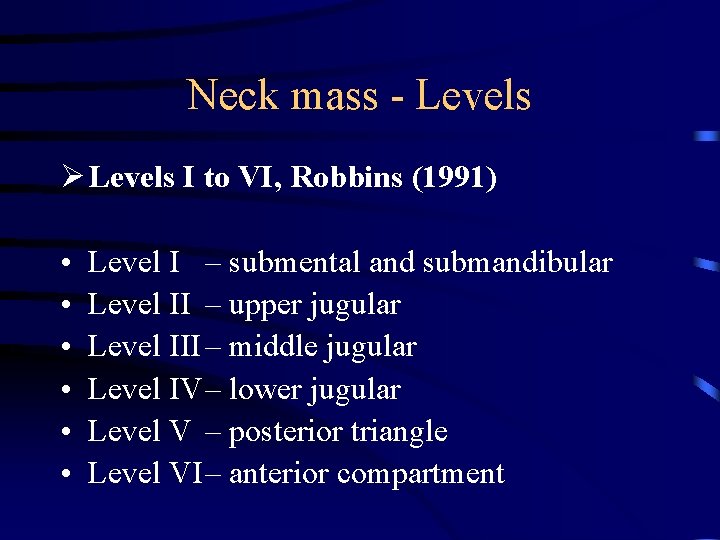
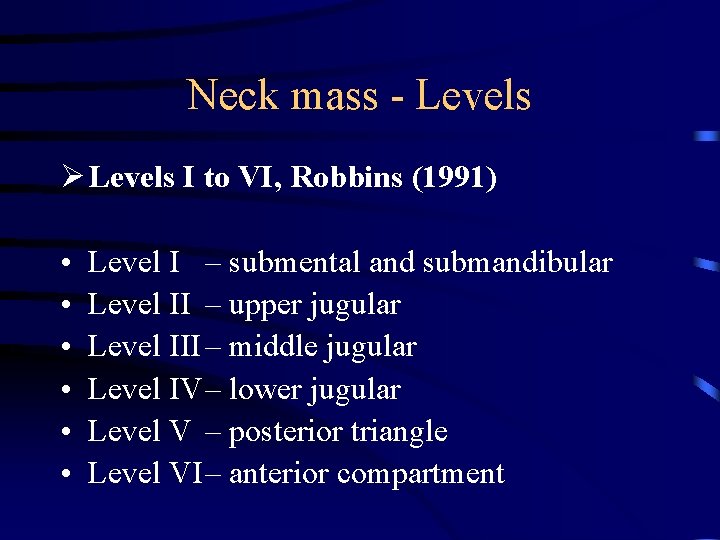
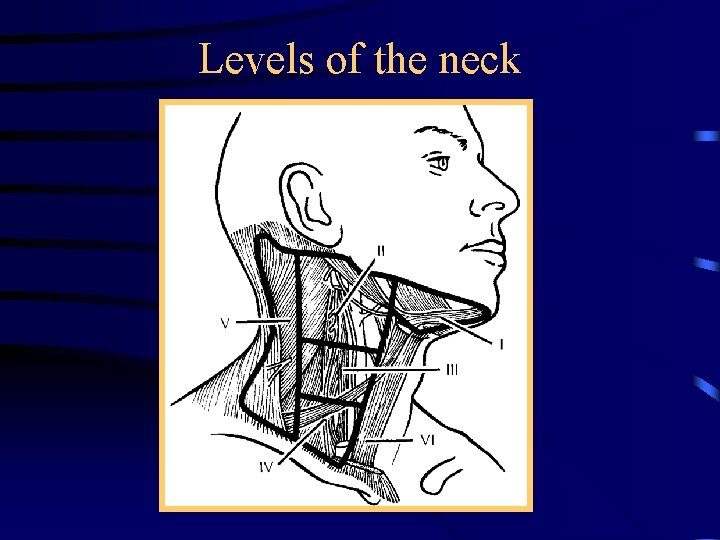
Neck mass - Levels Ø Levels I to VI, Robbins (1991) • • • Level I – submental and submandibular Level II – upper jugular Level III – middle jugular Level IV– lower jugular Level V – posterior triangle Level VI– anterior compartment
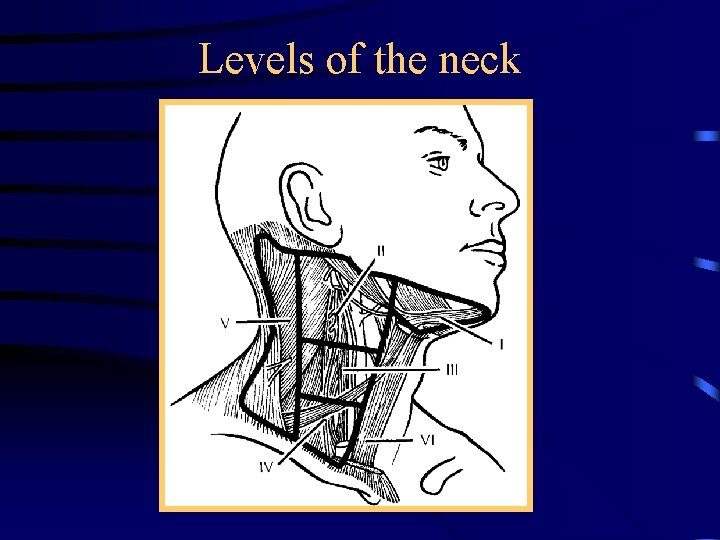
Levels of the neck
Neck masses - Causes Ø 80 % of neck masses in adults (>40) are malignant Ø Of those, 80% will be squamous cell carcinoma Ø Of those, in 80% the primary will be found Ø Of those, 80% will be in the head and neck region
Neck mass – work-up Ø Careful head and neck examination Ø In majority of cases a primary will be found Ø Examination should include the following areas : oral cavity, nasopharynx, oropharynx, larynx, hypopharynx Ø Examination under anaesthetic Ø Examine skin, thyroid, salivary glands
THE MOST ACCEPTABLE TEST TO ESTABLISH THE DIAGNOSIS IS FINE NEEDLE ASPIRATION CYTOLOGY
Neck masses - Cytology 1. Squamous cell carcinoma undifferentiated carcinoma : ENT examination EUA CT scan MRI
Neck masses - Cytology 1. Adenocarcinoma : ENT examination EUA CT scan, MRI (including abdomen) thyroid / kidneys /adrenals lungs examination of breast, prostate, endometrium
Neck mass – Cytology (cont) 1. Non-Hodgkin’s lymphoma : ENT examination, EUA with guided biopsies, CT scan thorax and abdomen, bone marrow biopsy, excision of single node for histological examination 1. Melanoma : ENT examination, dermatological and ophthalmological examination, CT/ MRI head and neck
Neck masses - Summary Ø Commonest cause in children is infective Ø Give 4 – 6 weeks to resolve Ø Commonest cause in adults is malignant Ø FNA Cytology the only diagnostic tool