NCS Acute Traumatic Brain Injury Nursing SelfPaced Case

NCS Acute Traumatic Brain Injury Nursing Self-Paced Case Study DEBORA ARGETSINGER, MS, AGACNP-BC, CCRN HONEY BEDDINGFIELD, BSN, RN, CCRN, CNRN KAREN MARCH, MN, RN, CNRN, CCRNalumnus BILL LOMBARDI, DNP, RN, AGACNP-BC YANA SERONDO, RN, NVRN-BC CYNTHIA BAUTISTA, PHD, APRN, FNCS Begin
Introduction Welcome to the Neurocritical Care Society’s Self-Learning Module on Acute Severe Traumatic Brain Injury! The target audience for this module is experienced neurocritical care nurses and APRNs, although the information provided may also be helpful to newer nurses and to other professionals. Because the module allows the learner to tailor the information reviewed, the time required for completion varies from 30 minutes to several hours. To move through the module, use the arrow buttons on your keyboard or select Next and Back buttons within presentation. There a number of interactive hyperlinks throughout the module that allow the learner to review additional information and test knowledge. ◦ Click on the underlined item to follow the links. ◦ After reviewing information using one of the interactive features, click the “return” button to return to the presentation. If you have questions or comments about this module, please email Cynthia Bautista, Ph. D, APRN, FNCS at cabbrain@aol. com Next
Objectives At the completion of this self-paced case study, the learner will be able to: 1. Identify the primary and secondary injuries that can occur with an acute severe traumatic brain injury. 2. List the subjective and objective assessments needed for an acute severe traumatic brain injured patient. 3. Summarize the many nursing interventions needed in monitoring and caring for an acute traumatic brain injured patient. Next
Case Study #1 An 85 year old female patient status post ground level fall is brought into the ED on a non-rebreather via Emergency Medical Services. She has a known history of diabetes, chronic kidney disease, hypertension, hypothyroidism and congestive heart failure. Upon initial exam you find that the patient has a small laceration over her right eye, but no obvious signs of skull fracture or penetrating injuries. Next
Epidemiology Fifty million people suffer from a traumatic brain injury (TBI) worldwide every year (https: //intbir. nih. gov) The global incidence rate of TBIs is estimated at 200/100, 000 people per year. (www. internationalbrain. org) In the United States 153 people die each day from injuries related to TBIs (www. cdc. gov) In 2013 there were 2. 5 million emergency department visits related to TBI is the leading cause of death related to trauma ◦ It is responsible for 30% of all injury related deaths Next
Epidemiology The leading causes of TBI ◦ Falls ◦ Being struck ◦ Motor vehicle crash Certain groups of individuals are at risk for TBI ◦ Individuals partaking in high risk behavior(s) ◦ Alcohol use, drug use, team sports, not using seat belts ◦ Men > women ◦ Very young (<10 years) and very old (>74 years) (Hickey, 2014) Next
Mechanism of Injury Blunt ◦ Motor vehicle crash ◦ Falls ◦ Intentional assaults ◦ Recreational and sport injuries Penetrating ◦ Firearm use ◦ Knife injuries/stabbings Blast ◦ Explosives (Bader, et al. , 2016) Next
Check Point - Test your Understanding Based on this presentation the information presented on the patient and traumatic brain injuries…. What type of mechanism of injury does she have? A. Blunt B. Penetrating Next
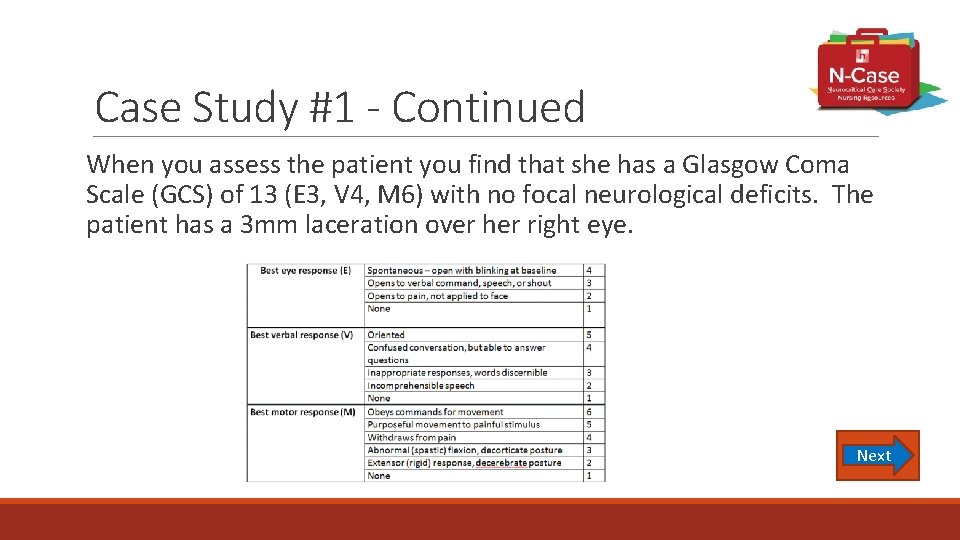
Case Study #1 - Continued When you assess the patient you find that she has a Glasgow Coma Scale (GCS) of 13 (E 3, V 4, M 6) with no focal neurological deficits. The patient has a 3 mm laceration over her right eye. Next
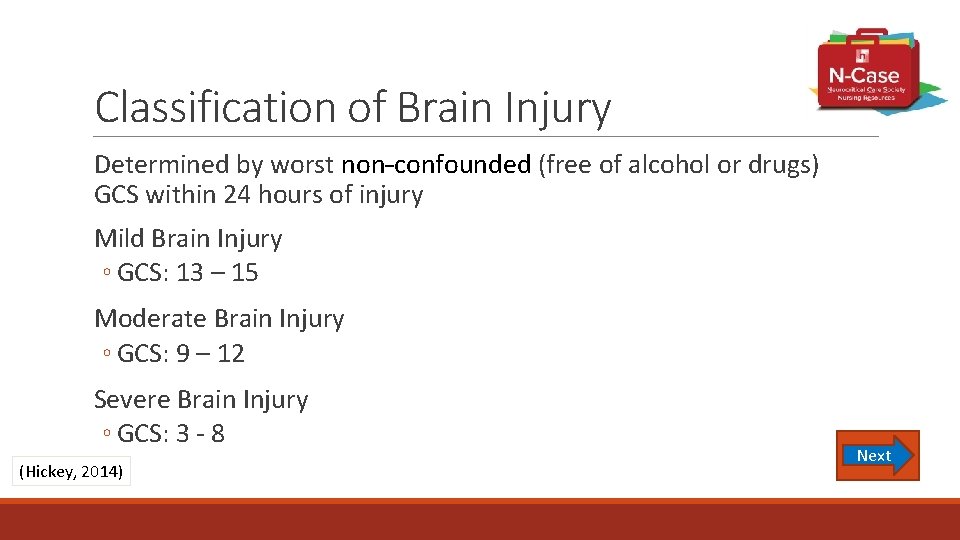
Classification of Brain Injury Determined by worst non-confounded (free of alcohol or drugs) GCS within 24 hours of injury Mild Brain Injury ◦ GCS: 13 – 15 Moderate Brain Injury ◦ GCS: 9 – 12 Severe Brain Injury ◦ GCS: 3 - 8 (Hickey, 2014) Next
Check Point - Test your Understanding She has a Glasgow Coma Scale (GCS) of 13 (E 3, V 4, M 6) with no focal neurological deficits. Which classification of brain injury does she have? A. Mild B. Moderate C. Severe Back Next
Case Study #1 - Continued The patient is now complaining of a headache and is impulsive, attempting to get out of bed despite being told multiple times that she needs to have someone assist her when getting out of bed because of her risk of falling. She is oriented to person and place, but not to time or situation continuing to ask to get up to let her dog out and complains that it, “smells like rubbing alcohol in here”. When you ask her to please sit down she smiles and gets back in bed. Next
Primary Brain Injury
Scalp Wound Highly vascular Bleeds briskly Assess for skull fracture Assess for shock (due to blood loss) Apply direct pressure Suture or staple wound Appropriate dressing (Hickey, 2014) Next
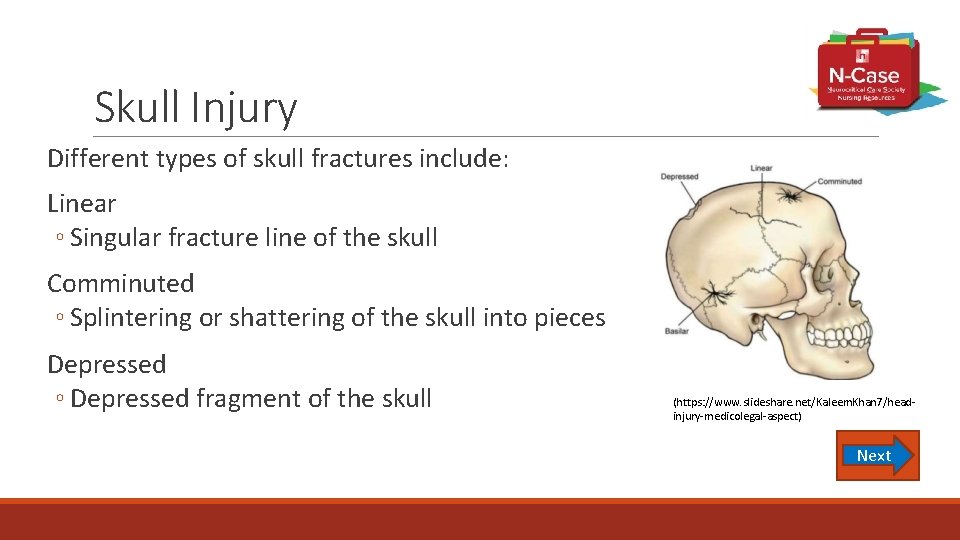
Skull Injury Different types of skull fractures include: Linear ◦ Singular fracture line of the skull Comminuted ◦ Splintering or shattering of the skull into pieces Depressed ◦ Depressed fragment of the skull (https: //www. slideshare. net/Kaleem. Khan 7/headinjury-medicolegal-aspect) Next
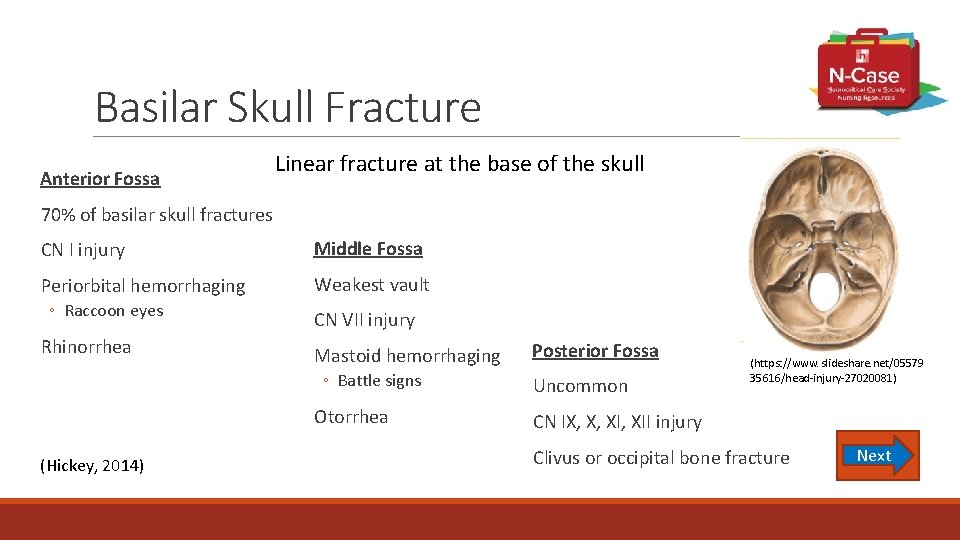
Basilar Skull Fracture Anterior Fossa Linear fracture at the base of the skull 70% of basilar skull fractures CN I injury Periorbital hemorrhaging ◦ Raccoon eyes Rhinorrhea Middle Fossa Weakest vault CN VII injury Mastoid hemorrhaging ◦ Battle signs Otorrhea (Hickey, 2014) Posterior Fossa Uncommon (https: //www. slideshare. net/05579 35616/head-injury-27020081) CN IX, X, XII injury Clivus or occipital bone fracture Next
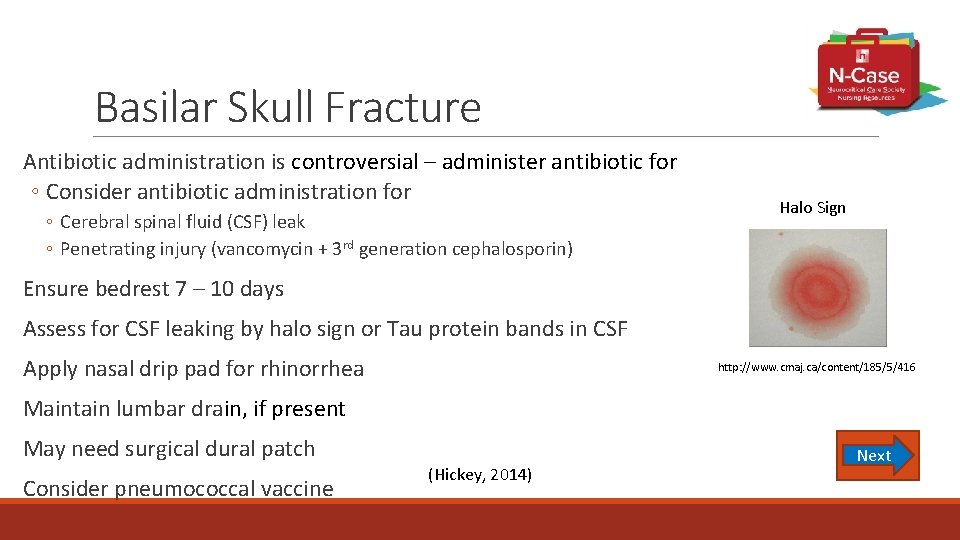
Basilar Skull Fracture Antibiotic administration is controversial – administer antibiotic for ◦ Consider antibiotic administration for ◦ Cerebral spinal fluid (CSF) leak ◦ Penetrating injury (vancomycin + 3 rd generation cephalosporin) Halo Sign Ensure bedrest 7 – 10 days Assess for CSF leaking by halo sign or Tau protein bands in CSF Apply nasal drip pad for rhinorrhea http: //www. cmaj. ca/content/185/5/416 Maintain lumbar drain, if present May need surgical dural patch Consider pneumococcal vaccine (Hickey, 2014) Next
Check Point - Test your Understanding Your patient has a GCS of 13 and an inability to stick out her tongue. What is the most likely basilar skull fracture associated with this deficit? A. Anterior B. Middle C. Posterior Next
Primary Brain Injury Focal Brain Injury
Contusion Bruising of brain tissue Most common area of injury is frontal or temporal lobe Injury at site of impact is called “Coup” injury Injury at the opposite of impact is called “Contracoup” injury Next
What’s the Challenge? Contusion Altered Level of Consciousness ◦ Conscious, stuporous, or comatose ◦ Are they confused or agitated? ◦ Do they need airway management? Bruising – Peri-contusional Edema – Mass effect ◦ Administer osmotic diuretics and/or hypertonic saline Bleeding into contusion ◦ Monitor/treat for increased intracranial pressure Seizures ◦ Clinical or subclinical ◦ Provide continuous electroencephalography (EEG) monitoring Next
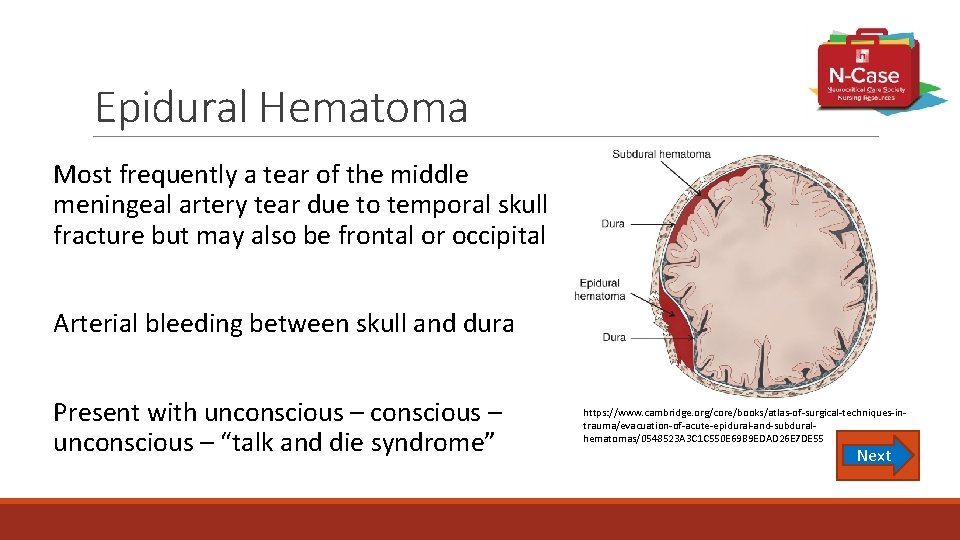
Epidural Hematoma Most frequently a tear of the middle meningeal artery tear due to temporal skull fracture but may also be frontal or occipital Arterial bleeding between skull and dura Present with unconscious – “talk and die syndrome” https: //www. cambridge. org/core/books/atlas-of-surgical-techniques-intrauma/evacuation-of-acute-epidural-and-subduralhematomas/0548523 A 3 C 1 C 550 E 69 B 9 EDAD 26 E 7 DE 55 Next
What’s the Challenge? Epidural Hematoma Prevent Uncal Herniation ◦ Assess for ipsilateral dilated fixed pupil, decreased level of consciousness, contralateral paralysis ◦ Consult Neurosurgery to determine need to drain hematoma Presence of arterial bleeding ◦ Neurosurgery to perform evacuation and repair to prevent/treat herniation Next
Subdural Hematoma Is a venous bleed (superior sagittal sinus, bridging veins) Bleeding is between the dura and arachnoid Acute subdural hematoma ◦ Symptoms occurs < 48 hours post injury ◦ Subacute subdural hematoma ◦ Symptoms occur up to 2 weeks post injury ◦ Chronic subdural hematoma ◦ Symptoms occur after 2 weeks post injury ◦ Occurs in elderly and alcoholics Next
What’s the Challenge? Subdural Hematoma Click on each of the links below to learn more. Monitor Level of Consciousness Surgical Evacuation and Drain Position of Head of bed Next
Traumatic Hemorrhage Intracerebral ◦ Traumatic bleeding into the cerebral tissue Intraventricular ◦ Traumatic bleeding into the ventricles Subarachnoid ◦ Traumatic bleeding into the subarachnoid space Next
Penetrating Injury Most lethal brain injury High mortality rate Due to ◦ Use of a handgun, rifle, and/or shotgun ◦ Objects such as knives, scissors, or nails Next (Hickey, 2014)
Predictors of Penetrating Head Injury Outcomes Presenting Neuro Status ◦ Awake = likely to survive ◦ Comatose = death more likely Path of Bullet ◦ Single hemisphere = likely to survive ◦ Bilateral hemispheres = death more likely Caliber & Velocity of Bullet ◦ Small & slow = likely to survive ◦ Large & fast = death more likely (Van Wyck, 2015) Next
Predictors of Penetrating Head Injury Outcomes (con’t) Time to Treatment ◦ Quick arrival to Emergency Department = survive ◦ Delay in arrival to Emergency Department = death Nature of Shooting ◦ Assault = survive ◦ Suicide = death (Van Wyck, 2015) Next
What’s the Challenge? Penetrating Head Injury Maintain airway, perfusion, intracranial pressure monitoring Legal Aspects ◦ Document injuries sustained ◦ Description of wounds ◦ Preservation of evidence ◦ Do not disrupt bullet holes in clothing ◦ Send clothing to medical examiner, if patient expires Surgical Intervention ◦ Irrigation, removal of fragments, debride tissue, antibiotic administration Next
Check Point - Test your Understanding Which of the following patients is most likely to survive a penetrating head injury? A. An 85 year old female was at the park walking her dog and was stabbed several times in multiple areas of her head. She was found four hours later lethargic with unequal pupils and minimal movement. B. A 26 year old male suffered a self inflicted gunshot wound to the face last night and was found by his family this morning breathing, but not opening his eyes despite aggressive attempts to awaken him. C. A 42 year old man about 1 hour ago, had a witnessed ground level fall landing on a steel rake that penetrated the left side of his head. He is awake and following commands. Next
Primary Brain Injury Diffuse Brain Injury Next
Mild Head Injury - Concussion Violent shaking of the brain Shearing stress on reticular formation Shaking disrupts brain’s normal chemical balance No focal neurologic deficits or CT findings Assess for Post Concussion Symptoms ◦ Symptoms include the following ◦ Confusion, forgets things, loses temper, impulsive, difficulty with new learning, problems at work/school, personality change Next
Diffuse Axonal Injury Mechanism of injury is an angular acceleration and deceleration Causes stress at gray-white mater interface MRI is preferred diagnostic test, it can play a role in predicting length of coma CT scan results show no intracranial lesion ◦ May show petechial hemorrhage of corpus callosum, periventricular, & rostral brainstem Provide supportive care Recovery depends on amount of axonal injury ◦ Grade 1 – brief loss of consciousness, recovery possible ◦ Grade 2 – coma of duration, unclear recovery process ◦ Grade 3 – immediate coma, posturing, incomplete recovery (Bay, et al. , 2007) Next
Case Study #2 The patient presents as a 35 year old female in the Neuro Intensive Care Unit status post motor vehicle crash. She suffers from the following injuries: traumatic right temporal intracerebral hemorrhage, a traumatic subarachnoid hemorrhage, right 36 rib fractures, and a right radial fracture that has been reduced and splinted. Your patient’s vital signs this morning are as follows: Temp 98°F, heart rate 116 beats/minute, blood pressure 88/54 mm. Hg, respiratory rate 18 breaths/minute, Pulse oxygenation 97% on 2 Liters nasal cannula. The patient has no past medical history and is on no medications at home. Their CBC demonstrates a hemoglobin at 10 mg/dl and hematocrit 30% and their chemistry panel is within defined limits. Her last narcotic was given at 11 pm last night. The patient’s pain is a 5/10. Next
Secondary Brain Injury Next
Hypoxia Any degree of respiratory failure is particularly hazardous for the TBI patient. Loss of consciousness following a TBI may be accompanied by decreased respirations and can lead to severe hypoxia. Any hypoxia will aggravate cerebral ischemia and increases cerebral blood flow and cerebral blood volume, thus increasing intracranial pressure. Next
Hypotension The level of systolic blood pressure (SBP) plays a critical role in secondary brain injury. Hypotension has been shown to correlate with diffuse brain swelling. If autoregulation remains intact, a drop in SBP triggers an autoregulatory vasodilation in an attempt to maintain adequate brain perfusion. This results in increased cerebral blood volume, which in turn elevates intracranial pressure. If autoregulation is not intact, there is dependency on SBP to prevent cerebral ischemia, which has been ascribed to be the single most important secondary insult. (Carney, et al. , 2016) Next
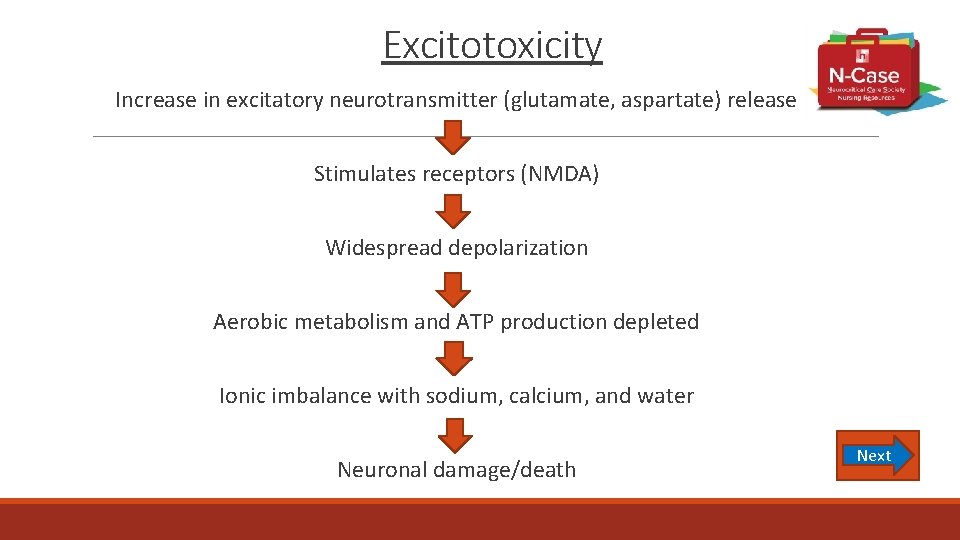
Excitotoxicity Increase in excitatory neurotransmitter (glutamate, aspartate) release Stimulates receptors (NMDA) Widespread depolarization Aerobic metabolism and ATP production depleted Ionic imbalance with sodium, calcium, and water Neuronal damage/death Next
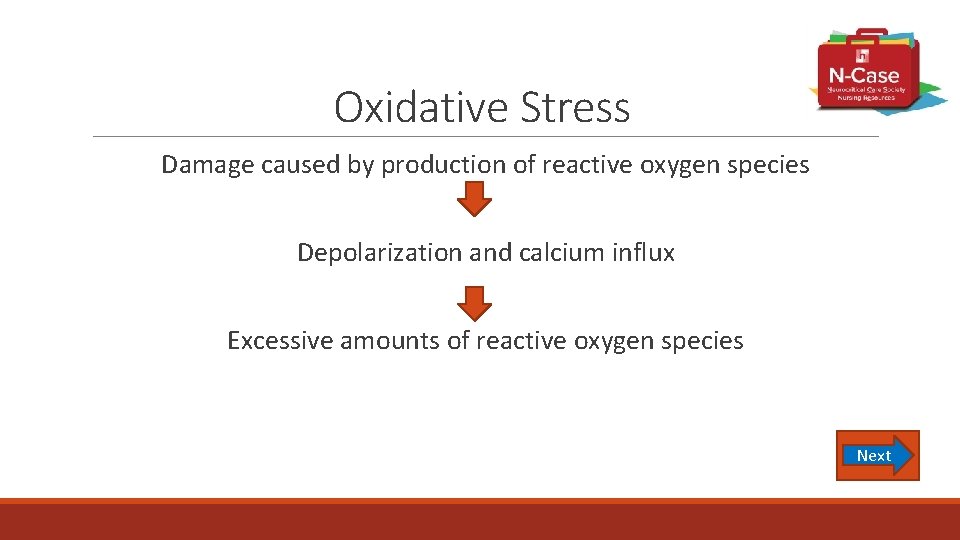
Oxidative Stress Damage caused by production of reactive oxygen species Depolarization and calcium influx Excessive amounts of reactive oxygen species Next
Cerebral Edema Caused by aquaporin dysfunction ◦ Aquaporin are proteins that create water channels ◦ Transports water in and out of cells Cerebral edema can have multiple peaks ◦ First is at 1 -2 days ◦ Lasts 5 -6 days ◦ May have a late peak Next
Mitochondrial Dysfunction Excessive calcium accumulation Release of cytochrome C Swelling and cell death Next
Check Point - Test your Understanding Your patient’s vital signs this morning are as follows: Temp 98°F, heart rate 116 beats/minute, blood pressure 88/54 mm. Hg, respiratory rate 18 breaths/minute, Pulse oxygenation 97% on 2 Liters nasal cannula. Her last narcotic was given at 11 pm last night. The patient’s pain is a 5/10. You walk in to assess your patient and notice that they are difficult to awaken. The most likely reason for this change in mental status is: A. Wrist pain B. Hypotension C. Narcotic overdose Next
Case Study #3 An 80 year old female patient is status post motor vehicle crash and brought in to the Emergency Department (ED) via Emergency Medical Services. She was not conscious and on supplemental oxygen via non-rebreather on route to the hospital. In the ED, she is attached to cardiac monitoring with continuous pulse oximetry and a full set of vital signs is taken. 12 -lead electrocardiogram and lab work are quickly obtained. Then, nursing performs their head-to-toe assessment of the patient, including a full neurologic examination. Due to the patient’s decreased level of consciousness, the patient is unable to participate in some aspects of the exam, so it is modified to still obtain as much information as possible. Subjective history is limited at this time due to the patient’s mental status, and will be obtained once family is available for interview. Next
Assessment Next
Subjective History ◦ Patient identification ◦ Government-issued identification found on the patient ◦ Will be confirmed by family when available ◦ Pertinent past medical history ◦ Include all acute and chronic medical conditions that will affect the patient’s treatment plan for their trauma ◦ Exclude medical history that has no pertinence, such as childhood illnesses without chronic sequelae ◦ Include list of patient’s current home medications when available ◦ Include any known allergies that the patient has ◦ Pertinent social history ◦ Include use of tobacco, alcohol, and recreational drug use ◦ Behaviors known to modify injury risk, such as seat belt usage Next
Subjective ◦ All known information leading up to the trauma, including the mechanism of injury and any causative factors ◦ Was the trauma accidental versus intentional? ◦ Intentional can be harm caused by others or self-inflicted harm ◦ Was the patient engaged in high-risk behavior or under the influence of alcohol or drugs, either prescribed or recreational? ◦ What was the mechanism of injury? ◦ Blunt versus penetrating trauma ◦ Was there peri-trauma loss of consciousness? ◦ Prehospital treatment ◦ How did EMS find the patient upon arrival? ◦ Interventions performs and medications administered? ◦ Changes in patient condition in route to the hospital Next
Case Study #3 - Subjective Findings The patient’s outpatient care is provided by physicians associated with the hospital and many aspects of her medical history can be found in the electronic medical record. The patient’s pertinent medical history includes the following: ◦ ◦ Chronic systolic heart failure with most recent ejection fraction of 35 -40% Chronic kidney disease, stage 3 (GFR 45 -59) Diabetes Mellitus, type II with recent Hgb A 1 C of 7. 8 Chronic atrial fibrillation The patient has no known drug allergies. Her home medication list includes: ◦ ◦ ◦ Metoprolol 25 mg BID Lisinopril 10 mg daily Warfarin 5 mg daily (think about rapid reversal of anticoagulation) Furosemide 20 mg daily Metformin 500 mg BID Glipizide 5 mg daily Next
Case Study #3 - Subjective Findings EMS provides the following report: “Arrived on scene to 2 vehicle collision. Patient’s car appears to have struck the other car from behind. The patient was found in the driver’s seat without seat belt engaged. The patient’s eyes were open and she was responsive to team. She was mumbling incomprehensible words when questioned and following commands in all four extremities. Visible contusions on front of forehead where it likely struck the steering wheel. The patient was removed from the vehicle and placed in the ambulance. Initial vitals HR 114, BP 134/90, RR 24, Sp. O 2 88% on room air. Patient placed on nasal cannula. Patient became less responsive en route to hospital and Sp. O 2 continued to fall, so patient placed on nonrebreather mask and Sp. O 2 stabilized at 94%. Blood glucose 210. Patient only opening eyes to repeated stimulation and intermittently following commands. Arrived to ED and handoff of care completed. ” When family arrives, they state she is a former 0. 5 pack per day smoker who quit 40 years ago. Next She does not drink alcohol or use recreational drugs.
Check Point – Test your Understanding Based upon the patient’s past medical history, for what potential complications should the nurse be vigilant in monitoring initially? (Select all that apply) A - Acute pulmonary edema B - Bradycardia C - Venous thrombosis D - Acute kidney injury Next
Check Point – Test your Understanding What type of injury did this patient experience? A - Blunt injury with no change in level of consciousness B - Blunt injury with change in level of consciousness C - Penetrating injury with no change in level of consciousness D - Penetrating injury with change in level of consciousness Next
Objective Primary survey - The A, B, C’s (Airway – Breathing – Circulation) Identify and treat life threatening injuries first (click on each item below) ◦ Airway – “A” ◦ Breathing – “B” ◦ Circulation – “C” Next
Objective Vital Signs ◦ Continuous monitoring Obtain 12 -lead Electrocardiogram ◦ Assess for arrhythmia and signs of ischemia ◦ New arrhythmia may be sign of electrolyte abnormality or hemodynamic compromise Next
Objective Labs ◦ CBC - monitor for bleeding and anemia ◦ Type and screen - patient may require transfusion ◦ Comprehensive metabolic panel ◦ Mg, and PO 4 - assess for kidney or liver injury and correct electrolytes ◦ a. PTT and PT/INR - ascertain bleeding risk and potentially reverse anticoagulation ◦ ABG - monitor oxygenation and ventilation, can help decide if intubation necessary ◦ Blood glucose - hypoglycemia can cause altered mental status ◦ Toxicology screen – assess use of drugs that can impair level of consciousness Next ◦ Other labs may be necessary based on patient history, such as BNP or TSH
Objective Secondary assessment ◦ Head ◦ Assess for ecchymosis, edema, lacerations, and discharge from orifices ◦ Raccoon’s eyes and Battle’s sign are sign of basilar skull fracture ◦ Use gauze to check discharge for halo sign to see if it is cerebral spinal fluid ◦ Send beta 2 -transferrin for confirmation ◦ Neck ◦ Assess for ecchymosis, tenderness, and impaired range of motion ◦ Cardiac ◦ Assess heart sounds, regularity of rhythm, peripheral pulses ◦ Tachycardia with reduced pulses and cyanosis are signs of potential bleeding and shock ◦ Pulmonary/Thorax ◦ Assess breath sounds, work of breathing, regularity of respirations Next ◦ Check thorax for tenderness, ecchymosis, abnormal chest movement with respiration
Objective ◦ Abdomen/Gastrointestinal ◦ Assess bowel sounds, tenderness, palpable masses ◦ Tenderness or rigidity can be sign of internal hemorrhage or perforation ◦ Nasogastric tube may be needed to drain gastric secretions ◦ May be necessary later for medication administration and nutrition ◦ Genitourinary ◦ Assess for ecchymosis, tenderness, and discharge ◦ Consider placement of indwelling urinary catheter for accurate intake and output ◦ Integumentary/Musculoskeletal ◦ Full body assessment for laceration, ecchymosis, and tenderness ◦ Assess for deformity in extremities ◦ Assess range of motion in each extremity Next
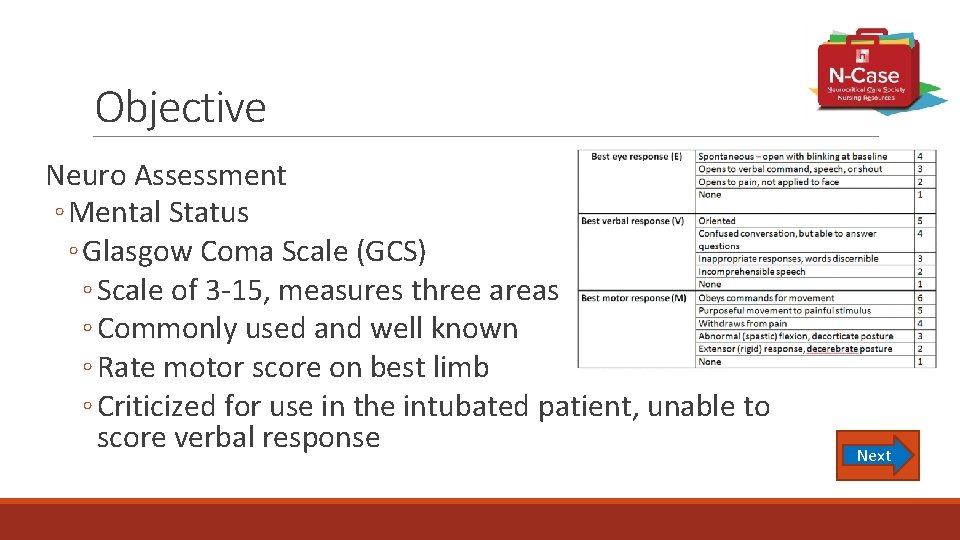
Objective Neuro Assessment ◦ Mental Status ◦ Glasgow Coma Scale (GCS) ◦ Scale of 3 -15, measures three areas ◦ Commonly used and well known ◦ Rate motor score on best limb ◦ Criticized for use in the intubated patient, unable to score verbal response Next
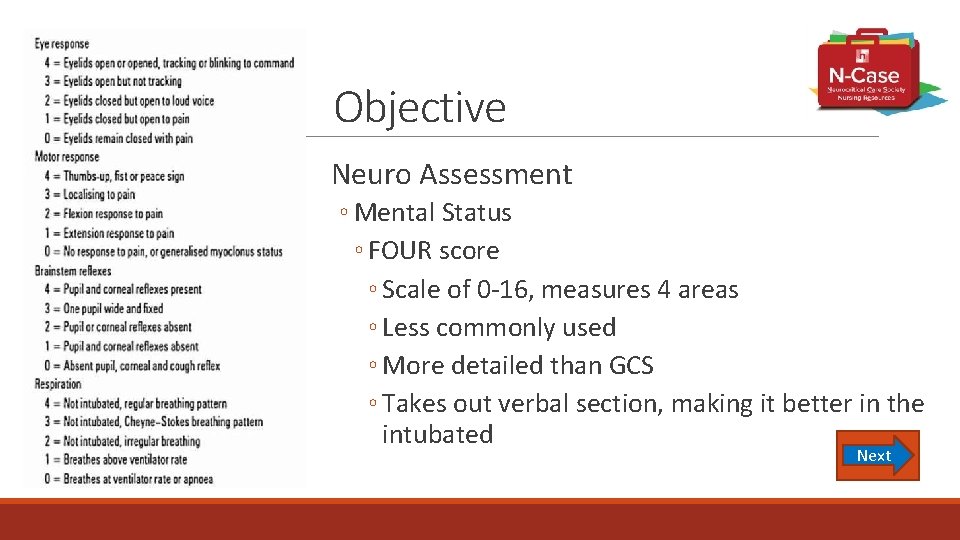
Objective Neuro Assessment ◦ Mental Status ◦ FOUR score ◦ Scale of 0 -16, measures 4 areas ◦ Less commonly used ◦ More detailed than GCS ◦ Takes out verbal section, making it better in the intubated Next
Objective Concussion Assessment ◦ Acute Concussion Evaluation(ACE) for the Emergency Department or the Clinician’s Office ◦ Tools available online through the Center of Disease Control ◦ Helps define the cause and presentation, as well as lists symptoms since injury ◦ Can be used to plan further care needs of the patient Next
Acute Concussion Evaluation (ACE) Select this link to see the Acute Concussion Evaluation form Next
Objective – Concussion Assessment Post Concussion Symptom Scale ◦ Initially designed for athletes as a way to see when they could return to sports ◦ Lists 22 concussion symptoms that patient rates on scale of 0 -6 ◦ Symptoms can be tracked over time to see improvement or worsening Sports Concussion Assessment Tool, 3 rd Edition (SCAT 3) ◦ Evaluation tool to assess concussion in athletes ◦ Combination of symptoms, cognitive assessment, and physical exam Next
Post Concussion Symptom Scale Select this link to view the Post Concussion Symptom Scale Next
Objective ◦ Cranial Nerves ◦ Full exam of CN II-XII ◦ CN II - Visual fields and acuity; blink to threat in unconscious patient ◦ CN II & III - Pupillary reaction ◦ Pupillometry is useful to detect subtle changes ◦ CN III, IV, & VI - Extra-ocular movements; vestibulo-ocular reflex (VOR) ◦ CN V - Facial sensation in forehead, cheek, & chin bilaterally; corneal reflex ◦ CN VII - Facial movement (check symmetry) ◦ CN VIII - Whisper test ◦ CN IX & X - Palate elevation; gag reflex ◦ CN XI - Shoulder shrug and turning head ◦ CN XII - Tongue protrusion and deviation Next
Objective ◦ Motor Examination ◦ Strength and range of motion in all extremities ◦ Check for symmetry ◦ Strength is rated on a 0 -5 scale ◦ Is movement to command, spontaneous, or to stimuli? ◦ Sensory Examination ◦ Start with light touch and work to noxious stimuli if no initial reaction ◦ Can check sharp versus dull sensation ◦ Cerebellar Examination ◦ Romberg test, finger-to-nose, limb ataxia, proprioception ◦ Reflexes ◦ Hyper and hypo reflexia may indicate spinal cord injury Next
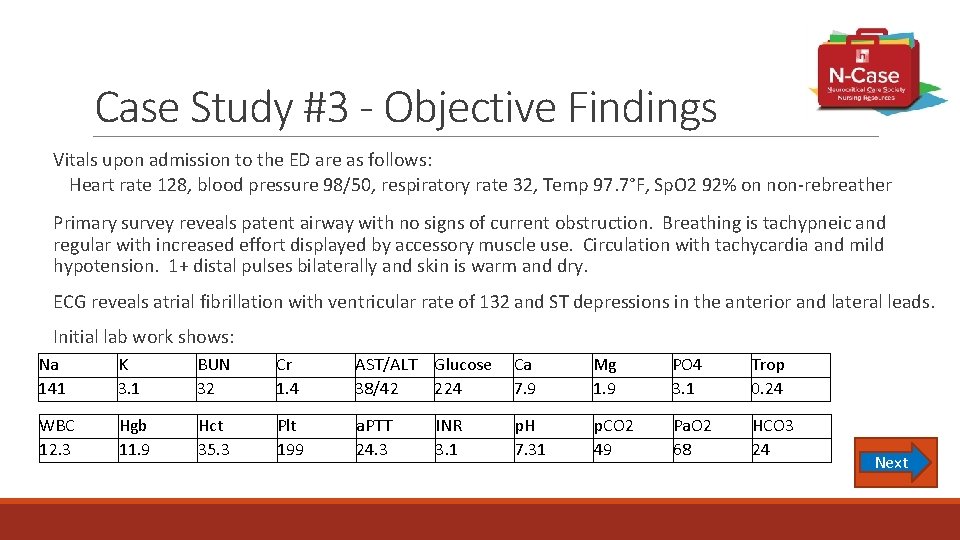
Case Study #3 - Objective Findings Vitals upon admission to the ED are as follows: Heart rate 128, blood pressure 98/50, respiratory rate 32, Temp 97. 7°F, Sp. O 2 92% on non-rebreather Primary survey reveals patent airway with no signs of current obstruction. Breathing is tachypneic and regular with increased effort displayed by accessory muscle use. Circulation with tachycardia and mild hypotension. 1+ distal pulses bilaterally and skin is warm and dry. ECG reveals atrial fibrillation with ventricular rate of 132 and ST depressions in the anterior and lateral leads. Initial lab work shows: Na 141 K 3. 1 BUN 32 Cr 1. 4 AST/ALT 38/42 Glucose 224 Ca 7. 9 Mg 1. 9 PO 4 3. 1 Trop 0. 24 WBC 12. 3 Hgb 11. 9 Hct 35. 3 Plt 199 a. PTT 24. 3 INR 3. 1 p. H 7. 31 p. CO 2 49 Pa. O 2 68 HCO 3 24 Next
Case Study #3 - Objective Findings Physical Exam is performed with the following pertinent findings: ◦ Head: Hematoma on forehead without laceration; no drainage noted ◦ Neck: Unable to state pain, no grimace to palpation; no overt signs of trauma ◦ Cardiac: Irregular rhythm with no extra heart sounds; 1+ pulses, brisk capillary refill ◦ Pulmonary/Thorax: Fine crackles at bilateral bases; increased work of breathing ◦ GI: soft, non-tender, not distended abdomen; active bowel sounds throughout ◦ GU: no signs of trauma; no discharge or lesion present Next
Case Study #3 - Objective Findings Physical Exam is performed with the following pertinent findings: ◦ Integumentary: Scattered ecchymosis on limbs and trunk; no open wounds ◦ Neurologic: Eyes open to noxious stimuli, no verbal response, withdraws to pain in upper extremities and flexes to pain in lower extremities ◦ CN: Pupils equal and brisk, corneal reflex and VOR intact, grimace to pain equal bilaterally, gag intact ◦ Motor: withdraws to pain in upper/lower extremities ◦ Sensory: Responds to painful stimuli in all four extremities ◦ Cerebellar: Patient unable to cooperate with exam ◦ Reflexes: normal reflexes in all four extremities Next
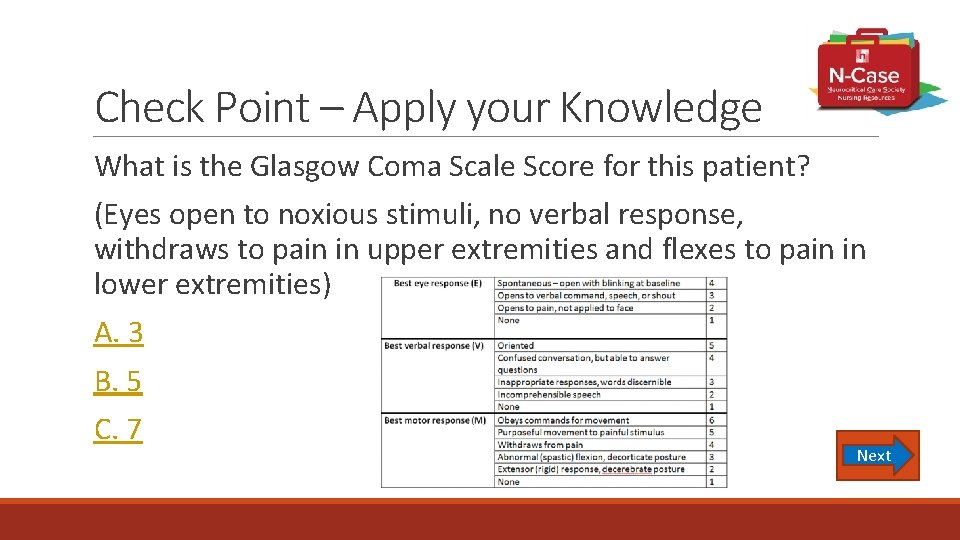
Check Point – Apply your Knowledge What is the Glasgow Coma Scale Score for this patient? (Eyes open to noxious stimuli, no verbal response, withdraws to pain in upper extremities and flexes to pain in lower extremities) A. 3 B. 5 C. 7 Next
Check Point – Apply your Knowledge Based upon the objective findings, which statement is FALSE regarding this patient? A- The patient’s rapid atrial fibrillation could be exacerbated by hypokalemia B - The patient is showing no signs of heart failure exacerbation C - The patient is showing signs of cardiac ischemia D - The patients respiratory status is compromised Next
Case Study #3 - Continued After your assessment is completed, that patient develops generalized convulsive activity concerning for a generalized tonic-clonic seizure. The provider orders 4 mg of lorazepam and 1000 mg of levetiracetam. The patient’s airway is at risk during the seizure and the patient is emergently intubated by the provider. Because the seizure activity is not completely ceased by the initial medications, a propofol infusion is started. Visible seizure activity ceases after initiation. A CT scan is ordered by the provider to assess the type of injury sustained in the motor vehicle crash and different advanced neurologic monitoring modalities are being considered. Next
Imaging ◦ CT Scan ◦ Good for overview of structures, very good for identifying hemorrhage ◦ Does not immediately show early ischemia or anoxia ◦ Quick to obtain, but does expose patient to radiation ◦ Good to identify boney injury ◦ CT Angiogram ◦ Can identify thrombosis in major vessels or vascular malformations, like aneurysm ◦ “Spot sign” shows contrast extravasation into hematoma showing active bleed ◦ Iodinated contrast can cause allergic reaction and kidney injury Next
Advanced Neuromonitoring Multiple Modalities – select links below to learn more ◦ ICP Monitoring ◦ Intraventricular ◦ Intraparenchymal ◦ Transcranial cerebral oximetry ◦ Brain tissue oxygenation monitoring ◦ Cerebral blood flow monitoring ◦ Cerebral Microdialysis https: //pbrainmd. wordpress. com/2015/12/13/multimo ◦ Continuous EEG dality-monitoring-in-neurocritical-care/ (Lee, 2012) Next
Case Study #3 - Advanced Monitoring The CT scan is completed and the patient is accepted by the Neuro ICU team. The patient is brought up to the ICU and a handoff of care is given at bedside between the ED and ICU nurses. The radiology report states a right frontal intraparenchymal hemorrhage (IPH) with posterior occipital contusion. Vasogenic edema and midline shift is seen. The patient is started on hypertonic saline for the edema. The decision is made with the medical team to place a ventriculostomy for ICP monitoring and CSF drainage. Due to her INR of 3. 1 she was reversed prior to placement of ventriculostomy. After placement of the drain, continuous EEG is placed. Next
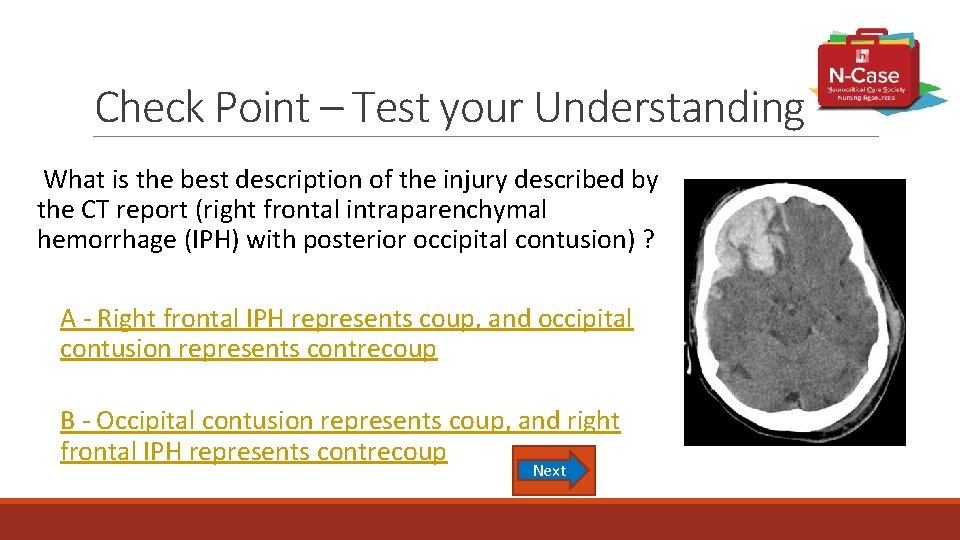
Check Point – Test your Understanding What is the best description of the injury described by the CT report (right frontal intraparenchymal hemorrhage (IPH) with posterior occipital contusion) ? A - Right frontal IPH represents coup, and occipital contusion represents contrecoup B - Occipital contusion represents coup, and right frontal IPH represents contrecoup Next
Check Point – Test your Understanding What is the purpose of implementing continuous EEG monitoring for this patient? A. Monitor for cerebral edema B. Capture electrical impulses from neuroglial cells C. Assess for subclinical seizures D. Monitor vital signs Next
Check Point – Test your Understanding The ICP recorded on the monitor for the EVD has been 18. While suctioning, the ICP increases to 26 while coughing. The ICP returns to 18 two minutes after coughing completed. What is the best nursing intervention? A - Drain extra CSF to prevent further ICP spikes B - Notify the MD for need for mannitol to rapidly decrease ICP C - Nothing, these transient increases in ICP are normal Next
Nursing Management Next
Airway, Oxygen, and Ventilation Monitor airway protection in non-intubated patients ◦ Monitor for signs of respiratory failure ◦ Hypoxia - Pa. O 2 <60 mm. Hg, hypoxia lasting 10 -20 mins occurs in one third of all TBI patients (Hypoxia may result in cytotoxic edema) ◦ Hypercarbia ◦ Anxiety/ restlessness ◦ Confusion ◦ Airway obstruction such as the tongue Provide airway protection for patient with Glasgow Coma Score (GCS) ≤ 8 ◦ Insert an oral gastric tube (OG) to help prevent aspiration Next
Airway, Oxygen, and Ventilation Maintain adequate oxygenation ◦ Maintain O 2 saturation ≥ 90%, Pa. O 2 > 100 mm. Hg ◦ Control p. H & Pa. CO 2 ◦ Keep Pa. CO 2 35 – 45 mm. Hg ◦ Avoid hyperventilation unless signs of herniation are present –abnormal posturing with unilateral or bilateral dilated & non reactive pupils (4 th edition of TBI Guidelines) ◦ Prolonged prophylactic hyperventilation with partial pressure of carbon dioxide in arterial blood (Pa. CO 2) of 25 mm Hg or less is not recommended (4 th edition TBI Guidelines) ◦ Provide sedation & analgesia as needed Next
Airway, Oxygen, and Ventilation Assisted Ventilation ◦ Positive End Expiratory Pressure (PEEP) – may mildly or slightly increase ICP that may or may not be a concern ◦ Suctioning ◦ ICP often increases but decreases after cessation of stimulus ◦ If it does not, pre-medicate with a sedative and/or IV push lidocaine ◦ Hyperoxygenate pre & post suctioning ◦ Avoid saline instillation ◦ Limit time to 10 seconds of suctioning at each pass ◦ Chest Physical Therapy (CPT) is safe Next
Airway, Oxygen, and Ventilation Early Tracheostomy o Reduces mechanical ventilation days when the benefit is felt to outweigh the complications associated with such a procedure o No evidence that early tracheostomy reduces mortality or the rate of nosocomial pneumonia (4 th edition TBI Guidelines) Ventilator Associated Pneumonia (VAP) Protocol ◦ Providone-iodine oral care is not recommended to reduce VAP & may cause an increased risk of acute respiratory distress syndrome (4 th edition TBI Guidelines) Next
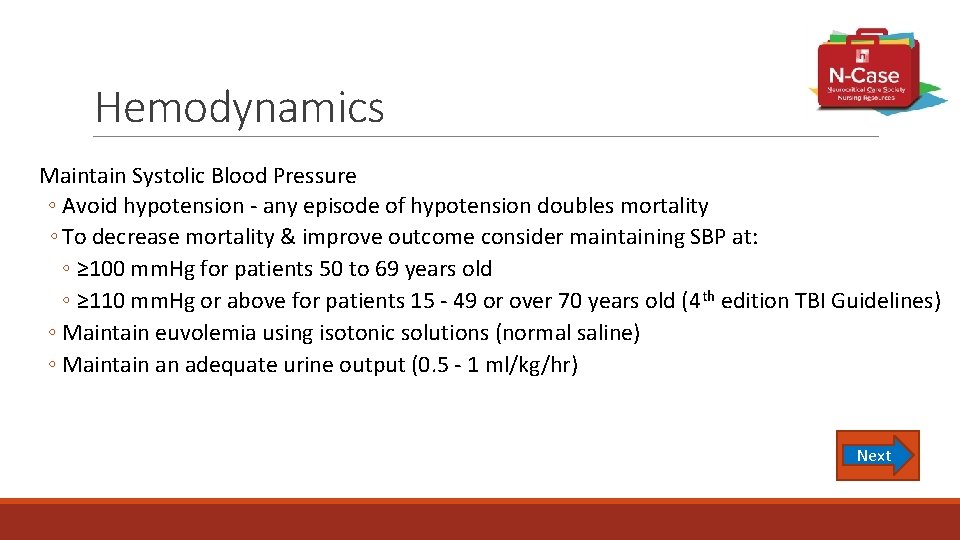
Hemodynamics Maintain Systolic Blood Pressure ◦ Avoid hypotension - any episode of hypotension doubles mortality ◦ To decrease mortality & improve outcome consider maintaining SBP at: ◦ ≥ 100 mm. Hg for patients 50 to 69 years old ◦ ≥ 110 mm. Hg or above for patients 15 - 49 or over 70 years old (4 th edition TBI Guidelines) ◦ Maintain euvolemia using isotonic solutions (normal saline) ◦ Maintain an adequate urine output (0. 5 - 1 ml/kg/hr) Next
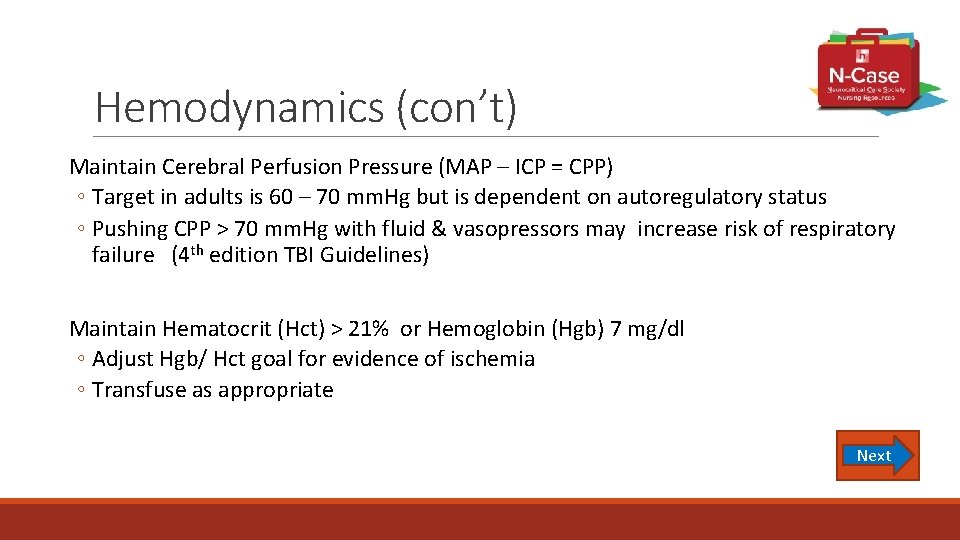
Hemodynamics (con’t) Maintain Cerebral Perfusion Pressure (MAP – ICP = CPP) ◦ Target in adults is 60 – 70 mm. Hg but is dependent on autoregulatory status ◦ Pushing CPP > 70 mm. Hg with fluid & vasopressors may increase risk of respiratory failure (4 th edition TBI Guidelines) Maintain Hematocrit (Hct) > 21% or Hemoglobin (Hgb) 7 mg/dl ◦ Adjust Hgb/ Hct goal for evidence of ischemia ◦ Transfuse as appropriate Next
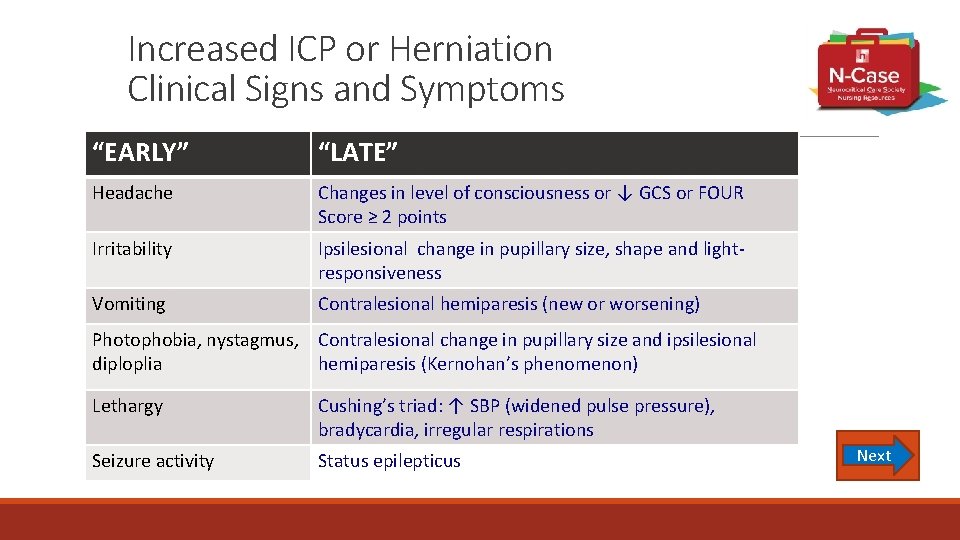
Increased ICP or Herniation Clinical Signs and Symptoms “EARLY” “LATE” Headache Changes in level of consciousness or ↓ GCS or FOUR Score ≥ 2 points Irritability Ipsilesional change in pupillary size, shape and lightresponsiveness Vomiting Contralesional hemiparesis (new or worsening) Photophobia, nystagmus, Contralesional change in pupillary size and ipsilesional diploplia hemiparesis (Kernohan’s phenomenon) Lethargy Cushing’s triad: ↑ SBP (widened pulse pressure), bradycardia, irregular respirations Seizure activity Status epilepticus Next
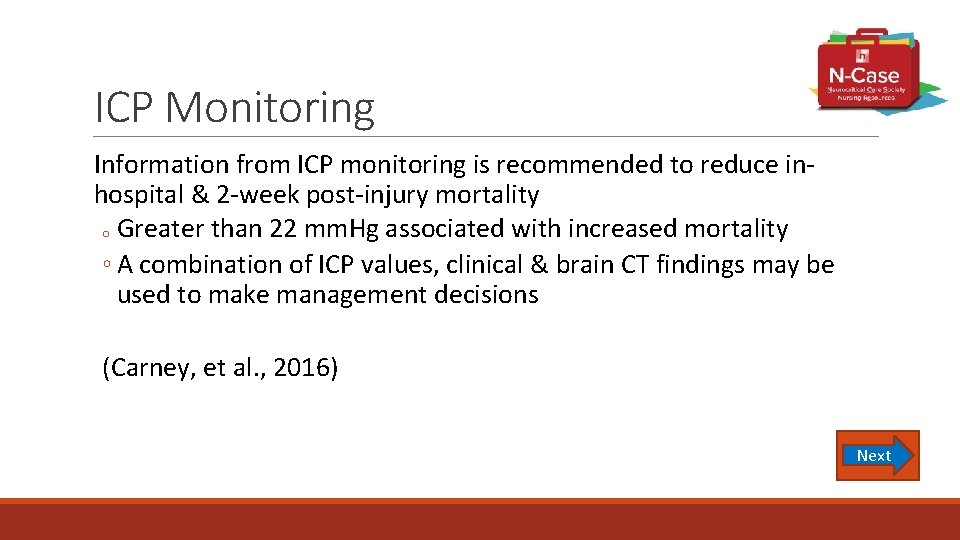
ICP Monitoring Information from ICP monitoring is recommended to reduce inhospital & 2 -week post-injury mortality o Greater than 22 mm. Hg associated with increased mortality ◦ A combination of ICP values, clinical & brain CT findings may be used to make management decisions (Carney, et al. , 2016) Next
ICP Monitoring Nursing Management of ventriculostomy ◦ Adhere to strict aseptic technique ◦ Use only normal saline to flush tubing in patient with external ventricular drain (EVD) system with an external transducer ◦ Level EVD at tragus of ear, which correlates with foramen of Monroe ◦ Head of bed should be at 30 degrees ◦ The system should be leveled during and when: ◦ Positioning the patient ◦ Bed transfers ◦ The height of bed is changed ◦ Ensure that all connections are tightly closed ◦ Monitor for CSF leak (Bader, et al. , 2016) Next
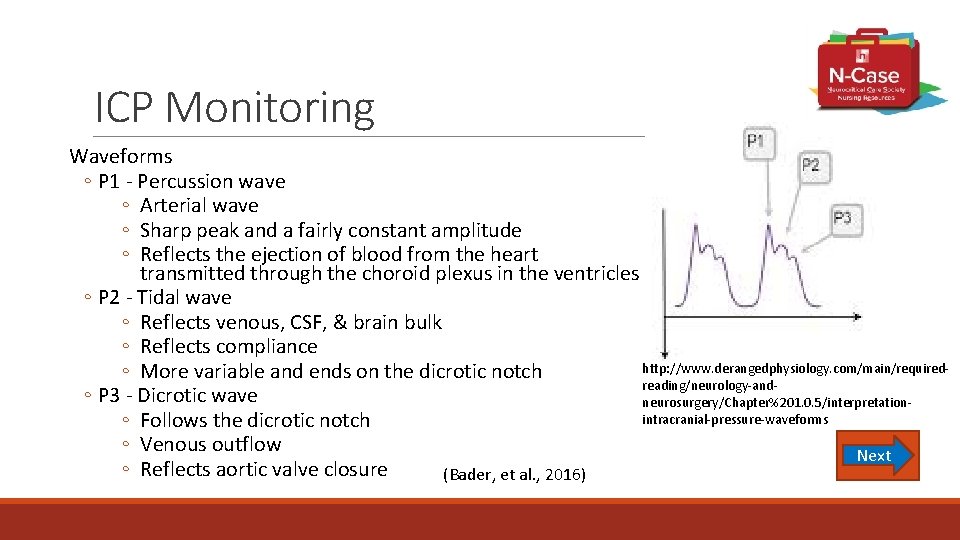
ICP Monitoring Waveforms ◦ P 1 - Percussion wave ◦ Arterial wave ◦ Sharp peak and a fairly constant amplitude ◦ Reflects the ejection of blood from the heart transmitted through the choroid plexus in the ventricles ◦ P 2 - Tidal wave ◦ Reflects venous, CSF, & brain bulk ◦ Reflects compliance http: //www. derangedphysiology. com/main/required◦ More variable and ends on the dicrotic notch reading/neurology-and◦ P 3 - Dicrotic wave neurosurgery/Chapter%201. 0. 5/interpretationintracranial-pressure-waveforms ◦ Follows the dicrotic notch ◦ Venous outflow Next ◦ Reflects aortic valve closure (Bader, et al. , 2016)
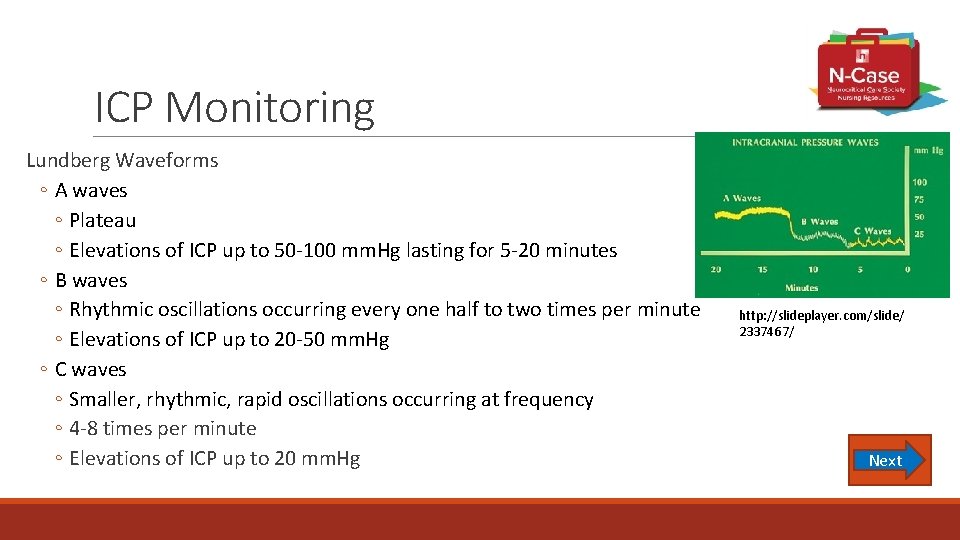
ICP Monitoring Lundberg Waveforms ◦ A waves ◦ Plateau ◦ Elevations of ICP up to 50 -100 mm. Hg lasting for 5 -20 minutes ◦ B waves ◦ Rhythmic oscillations occurring every one half to two times per minute ◦ Elevations of ICP up to 20 -50 mm. Hg ◦ C waves ◦ Smaller, rhythmic, rapid oscillations occurring at frequency ◦ 4 -8 times per minute ◦ Elevations of ICP up to 20 mm. Hg http: //slideplayer. com/slide/ 2337467/ Next
ICP Management Identify Patient Factors that INCREASE ICP ◦ Pain (Bader, et al. , 2016) ◦ Assess presence of pain & if analgesia is adequate ◦ Add or titrate analgesia as ordered ◦ Seizure activity ◦ Monitor and treat seizure activity ◦ Hypotension – Ischemia – Cerebral Edema ◦ Maintain SBP ≥ 100 mm. Hg (age 50 -69) SBP ≥ 110 mm. Hg (age 15 -49) ◦ Fever ◦ Maintain normothermia (temp 36. 5°C – 37. 5°C) ◦ Use of acetaminophen, body cooling devices ◦ Prevent shivering, use of acetaminophen, buspirone, magnesium, etc. Next
ICP Management Identify Patient Factors that INCREASE ICP (continued) ◦ Anemia ◦ Blood transfusion may be ordered if indicated ◦ Electrolyte Imbalance ◦ Hypo/hypernatremia, hypo/hyperosmolarity ◦ Osmotic diuretic or hypertonic saline may be used ◦ Fluid Overload ◦ Monitor fluid status ◦ Hypocapnia ◦ Assess ventilator settings Next
ICP Management Identify Nursing Factors that INCREASE ICP ◦ Performing hygiene ◦ Bathing, oral care, changing diapers has not been generally shown to increase ICP, it can increase for a moment and returns to baseline within minutes ◦ Noxious stimuli (i. e. needle sticks) ◦ Coughing, straining, and valsalva maneuver ◦ Due to increased intrathoracic pressure and decrease venous drainage ◦ Consider obtaining laxatives from MD/NP ◦ Suctioning ◦ May lead to transiently significant or can have sustained increase in ICP ◦ Provide oxygenation with 100% ◦ Adequate sedation to prevent movement and coughing during suctioning Next ◦ Limit suctioning to < 10 seconds for each insertion
ICP Management Nursing Interventions to REDUCE ICP ◦ Positioning – should be positioned to maintain a good body alignment and avoid extreme neck flexion, head rotation, and hip flexion ◦ Cervical collars must fit properly ◦ Patient turning can result in increases in ICP but the response is variable ◦ Patients who respond to turning with an increase in ICP should be turned passively ◦ Position head of bed to 30° - 45° ◦ If a cumulative effect of nursing care activities with an increase ICP, the care should be delayed, if applicable Next
ICP Management Nursing Interventions to REDUCE ICP (continued) ◦ Medications ◦ Osmotic diuretic: Mannitol ◦ Can be given 0. 25 - 1 g/kg body weight ◦ Infuse rapidly as a bolus (i. e. over 5 -10 minutes) ◦ Apply inline IV filter due to possible crystallization of medication ◦ Avoid systemic dehydration by targeting serum osmolality <320 m. Osm ◦ Can have rebound effect by passing osmotic particles through the disrupted blood brain barrier increasing brain edema ◦ Rebound effect may be seen after multiple doses Next
ICP Management Nursing Interventions to REDUCE ICP (continued) ◦ Medications ◦ Hypertonic Saline ◦ Examples: 1. 5%, 2%, 3%, 5%, 7%, 23. 4%, or 30% saline concentrations ◦ Central line is necessary for 23. 4% saline concentration ◦ Increases serum osmolality without causing diuresis ◦ Monitor sodium levels at least every 6 hours ◦ Caution not to increase by 10 points from baseline within 24 hours ◦ May have more prolonged effects and less rebound than mannitol ◦ May be used for fluid resuscitation Next
ICP Management Nursing Interventions to REDUCE ICP – Medications Sedation, analgesia, paralysis per MD Choice and dosing of sedatives, analgesics, & neuromuscular blocking agents is at the discretion of the prescriber (4 th Edition of TBI Guidelines) Analgesics Sedatives GABA receptor modulation ◦ Benzodiazapines ◦ Propofol (caution risk of propofol infusion syndrome) o Goal is to reduce cerebral metabolic demand Dexmedetomidine ◦ 2 agonist NSAIDs ◦ Should not be used due to effect on platelet function Opioids ◦ Morphine ◦ Fentanyl ◦ Remifentanil ◦ Hydromorphone Next
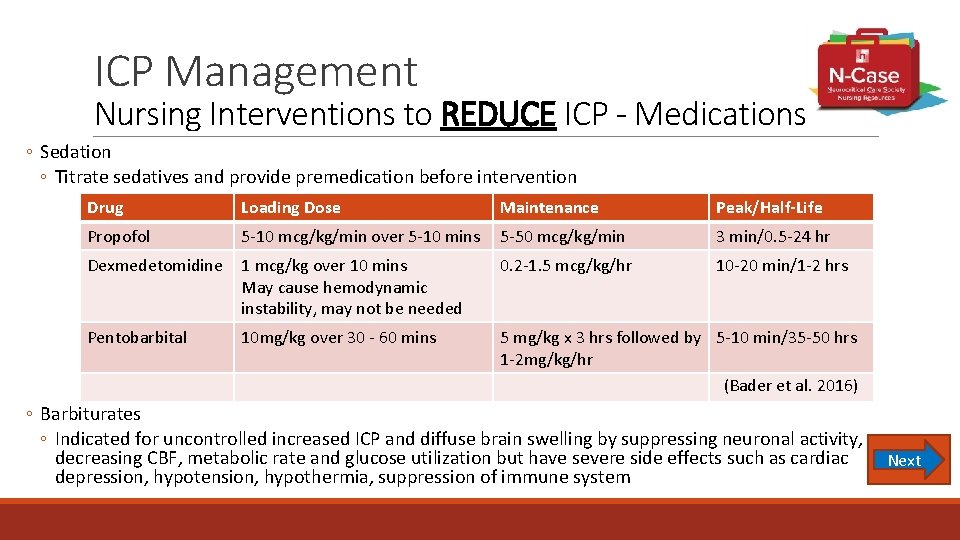
ICP Management Nursing Interventions to REDUCE ICP - Medications ◦ Sedation ◦ Titrate sedatives and provide premedication before intervention Drug Loading Dose Maintenance Peak/Half-Life Propofol 5 -10 mcg/kg/min over 5 -10 mins 5 -50 mcg/kg/min 3 min/0. 5 -24 hr Dexmedetomidine 1 mcg/kg over 10 mins May cause hemodynamic instability, may not be needed 0. 2 -1. 5 mcg/kg/hr 10 -20 min/1 -2 hrs Pentobarbital 10 mg/kg over 30 - 60 mins 5 mg/kg x 3 hrs followed by 5 -10 min/35 -50 hrs 1 -2 mg/kg/hr (Bader et al. 2016) ◦ Barbiturates ◦ Indicated for uncontrolled increased ICP and diffuse brain swelling by suppressing neuronal activity, decreasing CBF, metabolic rate and glucose utilization but have severe side effects such as cardiac Next depression, hypotension, hypothermia, suppression of immune system
Management of Common Complications Hyperglycemia ◦ Avoid Hyperglycemia (> 200 mg/d. L) ◦ Keep < 180 mg/d. L (140 – 180 mg/d. L) ◦ Avoid hypoglycemia Nutrition & Timing of Feeding ◦ Feed patients to meet basal caloric replacement (15% protein) by at least the 5 th day & no later then 7 th day post-injury is recommended to mortality (4 th edition TBI Guidelines) ◦ Transgastric jejunal feeding is recommended to reduce the incidence of VAP (4 th edition TBI Guidelines) Next
Management of Common Complications Fever • Fever (pyrexia) - systemic response to a perceived immunologic threat (infection or injury) that resets temperature at higher level • Neurogenics or central fever - disruption in the brain’s (hypothalamic) “set point” Infectious Causes Non-infectious Causes ◦ Pneumonia ◦ Drug or transfusion reaction ◦ Catheter associated urinary tract infection ◦ Deep vein thrombosis ◦ Central line associated infection ◦ Neurogenic injury Next
Fever – Pharmacologic Management Traditional Antipyretics ◦ Acetaminophen 2 – 4 gm /day ◦ Effectiveness of antipyretics depends on intact thermoregulation Treating Infection Source Control ◦ Remove unnecessary lines ◦ Start appropriate antibiotics Central Fever (Agrawal et al. , 2007) ◦ Bromocriptine ◦ Amantadine ◦ Dantrolene ◦ Propranolol Next
Fever – Normothermia Cooling Methods Surface cooling • Remove blankets • Tepid sponge bath • Ice packs over large vessels such as axilla and/or groin • Cooling blankets/mattresses • Cooling wraps Next
Management of Common Complications Seizure prophylaxis and/or seizures ◦ Prophylactic use of phenytoin or valproate is not recommended for preventing late post-traumatic seizures ◦ Phenytoin is recommended to decrease early post-traumatic seizures (within 7 days of injury) ◦ Early post-traumatic seizures is not associated with worse outcomes ◦ May consider using levetiracetam to prevent early post-traumatic seizures and toxicity, although there is insufficient evidence. (Carney, et al. , 2017) Next
Seizures Sub-clinical Seizures • Up to 48% of patient have subclinical seizures on EEG • May be associated with ICP especially delayed ICP beyond 96 hours • Look for evidence of sub-clinical seizure ◦ Changes in vital signs ◦ Conjugate eye deviation Herman, 2015 Next
Management of Common Complications Deep Vein Thrombosis ◦ Deep vein thrombosis prophylaxis treatment ◦ Low molecular weight heparin (LMWH) or low-dose unfractionated heparin may be used in combination with mechanical prophylaxis. However, there is an increased risk for expansion of intracranial hemorrhage (4 th edition TBI Guidelines) ◦ The use of graduated compression stockings with intermittent pneumatic compression (IPC) devices is recommended in patients with TBI who have a high risk of bleeding (Geerts, et al. , 2008) ◦ CLOTS 3 (2013) found the use of IPC devices was an effective tool to reduce DVT Next
Monitor for Neuro-Endocrine Dysfunction Incidence of neuro-endocrine dysfunction is 30 -50% ◦ Anterior hypopituitarism ◦ 27. 5% post-trauma (Range 5 – 30%) ◦ Posterior dysfunction ◦ 21. 6% Diabetes Insipidus (DI) ◦ Mostly severe TBI ◦ 6. 9% permanent dysfunction ◦ 12. 9% Syndrome of Inappropriate ADH (SIADH) (Agha et al. , 2004) Next
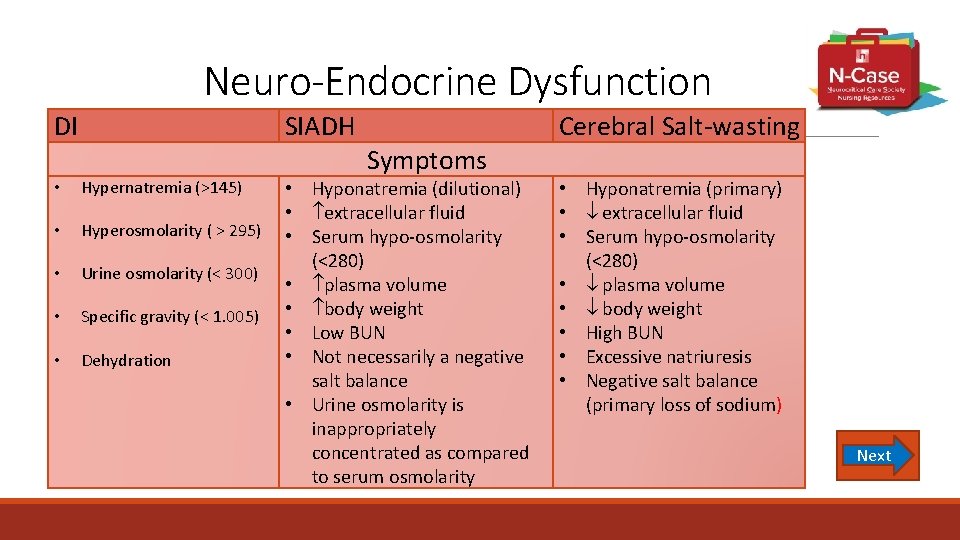
Neuro-Endocrine Dysfunction DI SIADH • Hypernatremia (>145) • Hyperosmolarity ( > 295) • Urine osmolarity (< 300) • Specific gravity (< 1. 005) • Dehydration Symptoms • Hyponatremia (dilutional) • extracellular fluid • Serum hypo-osmolarity (<280) • plasma volume • body weight • Low BUN • Not necessarily a negative salt balance • Urine osmolarity is inappropriately concentrated as compared to serum osmolarity Cerebral Salt-wasting • Hyponatremia (primary) • extracellular fluid • Serum hypo-osmolarity (<280) • plasma volume • body weight • High BUN • Excessive natriuresis • Negative salt balance (primary loss of sodium) Next
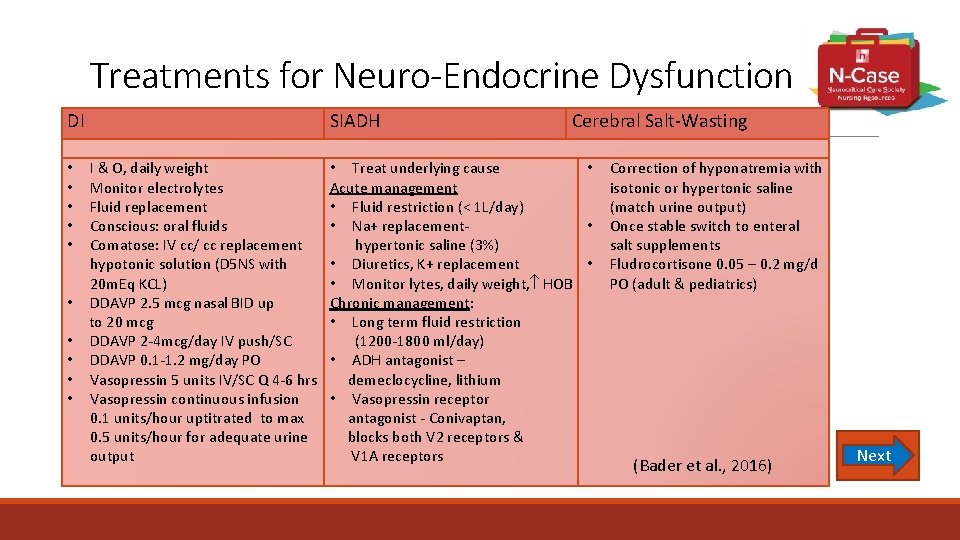
Treatments for Neuro-Endocrine Dysfunction DI SIADH Cerebral Salt-Wasting I & O, daily weight • Treat underlying cause • Monitor electrolytes Acute management Fluid replacement • Fluid restriction (< 1 L/day) Conscious: oral fluids • Na+ replacement- • Comatose: IV cc/ cc replacement hypertonic saline (3%) hypotonic solution (D 5 NS with • Diuretics, K+ replacement • 20 m. Eq KCL) • Monitor lytes, daily weight, HOB • DDAVP 2. 5 mcg nasal BID up Chronic management: to 20 mcg • Long term fluid restriction • DDAVP 2 -4 mcg/day IV push/SC (1200 -1800 ml/day) • DDAVP 0. 1 -1. 2 mg/day PO • ADH antagonist – • Vasopressin 5 units IV/SC Q 4 -6 hrs demeclocycline, lithium • Vasopressin continuous infusion • Vasopressin receptor 0. 1 units/hour uptitrated to max antagonist - Conivaptan, 0. 5 units/hour for adequate urine blocks both V 2 receptors & output V 1 A receptors • • • Correction of hyponatremia with isotonic or hypertonic saline (match urine output) Once stable switch to enteral salt supplements Fludrocortisone 0. 05 – 0. 2 mg/d PO (adult & pediatrics) (Bader et al. , 2016) Next
Check Point – Test Your Understanding Which of the following treatments are used for intracranial hypertension? a. b. c. d. Mannitol, vasopressin, hypertonic saline, propofol Hypertonic saline, hypothermia, mannitol Propofol, lorazepam, magnesium, hypertonic saline Hypertonic saline, phenylephrine, phenytoin Next
Check Point – Test Your Understanding Basic treatment for brain injury include: a. b. c. d. ABCs, head of bed elevation, fever management, trend of neurologic assessment Hypothermia, hypercarbia, hypoxia Administer D 50, hypocapnia, paralysis 100% oxygen delivery, head of bed 15 , fever management, trend of neurologic status Next
Check Point – Test Your Understanding The patient exhibits hypertension, bradycardia, & irregular respirations. This patient exhibits which of the following: a. b. c. d. Uncal herniation Cushing’s triad Horner’s syndrome Cingulate herniation Next
Case Study #3 – The End An 80 year old female patient who was brought to the ICU following a MVC. She has a history of atrial fibrillation on Warfarin, DM, CKD and CHF. Throughout her ICU stay she has been intubated for respiratory distress, had an ICP monitor placed to manage her intracranial pressures and an insulin drip to manage her diabetes. She has been stable hemodynamically and neurologically for 24 hours and it is now time to consider her transfer to a step-down unit. Her functional abilities both mentally and physically need to be evaluated at this time, if they have not already, by a physical therapist and an occupational therapist. A thorough evaluation of the patient’s post acute care needs will then need to be coordinated with the Case Manager to arrange for the patients ongoing rehabilitation and recovery. Next
Review • Primary injuries that occur with an acute severe traumatic brain injury (TBI) include: scalp, skull, contusions, hemorrhages, concussions, diffuse axonal injury and penetrating injuries. • Secondary injuries that occur with an acute severe TBI include: excitotoxicity, oxidative stress, cerebral edema, and mitochondrial dysfunction. • Subjective assessment focuses on the patient’s past medical history, mechanism of injury, and pre-hospital treatment. • Objective assessment focuses on airway, breathing and circulation priorities, along with assessing blood work results, a head to toe assessment, focused neurological assessment and neuro imaging with CT Scan & MRI. • Advanced multimodality monitoring includes ICP, transcranial cerebral oximetry, brain tissue oxygenation, cerebral blood flow, microdialysis and EEG. • Ongoing management focuses on close neurological monitoring, maintaining cerebral perfusion, avoiding increased ICP, avoiding fever, avoiding hyper/hypoglycemia, prophylaxing/treating seizures, and prophylaxis for deep vein thrombosis.
References Agha A. , Thornton E. , O’Kelly P. , et al (2004). Posterior pituitary dysfunction after traumatic brain injury. Journal of Clinical Endocrinology & Metabolism 89(12), 5987 -5992. Agrawal A. , Timothy J. , Thapa A. (2007). Neurogenic fever. Singapore Medical Journal, 48(6), 492 -494. Bader, M. K. , Littlejohns, L. R. , Olson, D. M. (2016). AANN Core Curriculum for Neuroscience Nursing. Chicago, IL: AANN. Bay, E. , Mc. Lean, S. A. (2007). Mild traumatic brain injury: An update for advanced practice nurses. Journal of Neuroscience Nursing, 39(10), 43 -57. Carney, N. , Totten, A. , O’Reilly, C. , et al. (2016). Guidelines for the management of severe traumatic brain injury 4 th Edition. Neurosurgery, 80(1), 6 -15. Next
References Dennis M. (2013) Effectiveness of intermittent pneumatic compression in reduction of risk of deep vein thrombosis in patients who have had a stroke (CLOTS 3): a multicenter randomized controlled trial. Lancet, 382, S 16 -S 24. Geerts W. H. , Bergqvist D. , Pineo G. F. , et al. , (2008). Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8 th edition). Chest, 133(6), 381 S– 453 S. Herman S. , Abend N. , Bleck T. , Chapman K. , Drislane F. , Emerson, R. , Gerard E. , Hahn C. , Husain A. , Kaplan P. , La. Roche S. , Nuwer M. , Quigg M. , Riviello J. , Schmitt S. , Simmons L. , Tsuchida T. , Hirsch L. (2015) Consensus statement of continuous EEG in critically ill adults. Journal of Clinical Neurophysiology, 32(2), 87 -95. Hickey, J. (2014). The Clinical Practice of Neurological and Neurosurgical Nursing. Philadelphia, PA: Wolters Kluwer. Lee, K. (2012). The Neuro ICU Book. New York, NY: Mc. Graw Hill. Van Wyck, D. W. , Grant, G. A. , Laskowitz, D. (2015). Penetrating traumatic brain injury: A review of current evaluation and management concepts. Journal of Neurology Neurophysiology, 6(6), 1 -7.
End of Presentation You have reached the end of the presentation Please click “Exit Presentation”
Check Point - Answer Your answer is CORRECT! What type of mechanism of injury does she have? A. Blunt Answer A there is no obvious penetration of the skull by an object Return to Presentation
Check Point - Answer Your answer is INCORRECT What type of mechanism of injury does she have? B. Penetrating There is no obvious penetration of the skull by an object Return to Presentation
Check Point - Answer You are CORRECT!!! She has a Glasgow Coma Scale (GCS) of 13 (E 3, V 4, M 6) with no focal neurological deficits. Which classification of brain injury does she have? A. Mild Brain Injury ◦ GCS: 13 – 15 B. Moderate Brain Injury ◦ GCS: 9 – 12 C. Severe Brain Injury ◦ GCS: 3 - 8 Return to Presentation
Correct! Return to Presentation
Incorrect. Return to Presentation
Check Point - Answer Your answer is CORRECT!! Your patient has a GCS of 13 and an inability to stick out her tongue. What is the most likely basilar skull fracture associated with this deficit? C. Posterior The answer is C. Your patient is noted to have raccoon eyes, only a laceration over her eye. She does not have battle sign on her mastoid on exam She complains of the smell of rubbing alcohol (CN I) and smiles at you (CN VII) indicating these cranial nerves are intact. Although rare, posterior basilar skull fractures are associated with a CN IIX palsy. Return to Presentation
What’s the Challenge? Subdural Hematoma Monitor level of consciousness ◦ Serial neurological exams, assess for seizure activity ◦ Stat CT for change in exam-especially level of consciousness Return to Presentation
What’s the Challenge? Subdural Hematoma Surgical Evacuation and Drain ◦ Craniotomy for acute subdural hematoma ◦ Burr hole evacuation for chronic subdural hematomas Subdural Evacuation Port System (SEPS) ◦ Minimally invasive ◦ Bedside procedure with local anesthetic ◦ Closed system for evacuation Return to Presentation https: //www. esutures. com/product/1 -expired/43 -medtronic/847 cranial/46226617 -medtronic-seps-cranial-access-kit-11 -0401 -CAL/
What’s the Challenge? Subdural Hematoma Position of Head of bed ◦ 45 degrees if possible ◦ Unless chronic subdural hematoma then flat for approximately 48 hours for risk of re-accumulation of blood Return to Presentation
Check Point - Answer Your are CORRECT!!! “C” is the answer Which of the following patients is most likely to survive a penetrating head injury? C. A 42 year old man, about 1 hour ago, had a witnessed ground level fall landing on a steel rake that penetrated the left side of his head. He is awake and following commands. The answer is C. The important factors to consider in survival from a penetrating injury are: time to hospital, level of consciousness, number of hemispheres involved. A (4 hours later, decreased neuro status) is incorrect, as patient not likely to survive due to timing and neuro status B (self inflicted) is incorrect, as patient not likely to survive due to nature of injury, Return to timing and neuro status Presentation
Check Point -Answer Your are CORRECT!! You walk in to assess your patient and notice that they are difficult to awaken. The most likely reason for this change in mental status is: B. Hypotension The answer is B. Although pain can be a distraction this patient does not complain of significant pain. The patient is noted to have gotten their last dose of narcotic containing medication last night at 11 pm. Hypotension can decrease cerebral perfusion resulting in a change in neurological function and secondary brain injury in the trauma patient. Return to Presentation
Check Point - Answer Your are CORRECT!! “A” is one of the answers – return to presentation to select another answer Based upon the patient’s past medical history, for what potential complications should the nurse be vigilant in monitoring initially? (Select all that apply) A (Acute Pulmonary Edema) Due to her reduced EF and potential for high volume fluid administration, the patient is at risk for pulmonary edema. Conversely, if the patient becomes hypovolemic with reduced cardiac output from her heart failure and concurrent CKD and ACE inhibitor use, the patient is at high risk for an acute-onchronic kidney injury. Return to Presentation
Check Point - Answer Your are CORRECT!! – “D” is the other correct answer Based upon the patient’s past medical history, for what potential complications should the nurse be vigilant in monitoring initially? (Select all that apply) D (Acute Kidney Injury) If the patient becomes hypovolemic with reduced cardiac output from her heart failure and concurrent CKD and ACE inhibitor use, the patient is at high risk for an acute-on-chronic kidney injury. B (Bradycardia) is incorrect, as patient will likely develop tachycardia due to her atrial fibrillation. C (Venous Thrombosis) is incorrect, as patient is at risk for increased bleeding due to her warfarin use. Return to Presentation
Check Point - Answer You are CORRECT!! What type of injury did this patient experience? B (Blunt Injury with change in level of consciousness) is correct. The patient experienced blunt trauma from the impact of her head against the steering wheel. Based upon the EMS report, the patient did experience a change in the level of her consciousness as she was not alert or speaking in full sentences. Return to Presentation
Objective ◦ Airway – “A” ◦ Can be compromised by edema from trauma or infection, foreign body, burns, anaphylaxis, or secretion management ◦ Secretion management is most common in neurologic disorders ◦ May require artificial airway to maintain patent ◦ Ensure to maintain stabilized C-Spine if potential injury present Return to Presentation
Objective ◦ Breathing – “B” ◦ Measure respiratory rate and monitor work of breathing ◦ Assess for signs of hypoxia or hypercapnia; consider ABG ◦ Maintain O 2 saturation > 90% ◦ Auscultate breath sounds and ensure present bilaterally Return to Presentation
Objective ◦ Circulation – “C” ◦ Monitor heart rate and blood pressure; Maintain SBP > 100 mm. Hg for end organ perfusion ◦ Check peripheral pulses and capillary refill ◦ Obtain parental access (intravenous line access) Return to Presentation
Check Point - Answer You are CORRECT!! What is the Glasgow Coma Scale Score for this patient? 7 total points for GCS 2 points for eye opening to pain 1 point for no verbal response 4 points for withdrawal to noxious stimulation Return to Presentation
Check Point - Answer You are CORRECT!! Based upon the objective findings, which statement is FALSE regarding this patient? B - The patient is showing no signs of heart failure exacerbation The patient has fine crackles on auscultation and hypotension with weak pulses, revealing that her left ventricle is unable to effectively pump its blood volume. Electrolyte imbalances can exacerbate arrhythmia. The elevated troponin and ST changes on ECG signal cardiac ischemia. Her respiratory compromise is evidenced by her supplemental oxygen use, increased work of breathing, and low Pa. O 2. Return to Presentation
Advanced Neuromonitoring Intracranial pressure (ICP) Monitoring ◦ Monitors pressure inside the cranial vault ◦ Device is placed most frequently into the non-dominant hemisphere ◦ Lateral ventricle, brain parenchyma, subarachnoid, subdural, or epidural space ◦ Various transducer systems available ◦ External strain-gauge (fluid filled) ◦ Internal (fiberoptic, micro-strain gauge) ◦ Maintain ICP <22 mm. Hg ◦ Transient (2 -5 minutes) increases are normal Return to ◦ Caused by coughing, pain, etc. Presentation ◦ Sustained (> 5 minutes) increases are pathological
Advanced Neuromonitoring Intraventricular (Ventriculostomy) ICP Monitoring ◦ Catheter is placed in the lateral ventricle ◦ More difficult to place in patients with mass lesions – lateral herniation, small ventricles ◦ Provides drainage of CSF in addition to ICP monitoring ◦ Allows for management with monitoring ◦ Re-calibrate external transducer as needed ◦ Must maintain external transducer level with patient ◦ Level at tragus of ear, which correlates with foramen of Monroe Return to Presentation
Advanced Neuromonitoring Intraparenchymal ICP Monitoring ◦ Catheter is placed directly into the brain tissue ◦ Does not allow for drainage of CSF ◦ Utilizes a fiber optic or micro-strain gauge catheter ◦ Transducer rests at the tip of the catheter ◦ Only zero the transducer prior to insertion ◦ Caution with drift in measurement ◦ Susceptible to breaking ◦ Does not require leveling of the device Return to Presentation
Advanced Neuromonitoring Transcranial Cerebral Oximetry ◦ Utilizes near-infrared spectroscopy ◦ Uses a disposable transducer probe applied to the forehead ◦ Measures cerebral tissue 2 -3 cm beyond cortex ◦ Proximal electrode detects hemoglobin in extracranial tissue ◦ Distal electrode detects hemoglobin in extra- and intracranial tissue ◦ Monitor determines ratio of oxygenated hemoglobin to total hemoglobin ◦ The ratio is displayed as regional oxygen saturation (r. SO 2 index) Return to Presentation
Advanced Neuromonitoring Brain Tissue Oxygen Catheter ◦ Catheter placed in white matter of brain tissue ◦ Often placed at site considered high risk for ischemic injury ◦ Measures brain tissue oxygenation (Pbt. O 2) ◦ Can be uses to determine if cerebral ischemia present at site of probe ◦ Goal is a value of ≥ 15 mm. Hg Return to Presentation
Advanced Neuromonitoring Cerebral Blood Flow Monitoring ◦ Laser doppler flowmetry ◦ Uses laser beam directed at tissue to measure flow based upon beam reflection and scattering ◦ Thermal diffusion flowmetry ◦ Sensor placed in white mater and calculates CBF using temperature difference between distal and proximal sensors ◦ Normal values are 20 – 35 m. L/100 g/minute white mater; 60 to 90 m. L/100 g/minute gray mater ◦ Decreases in flow represent hypo-perfusion in the area being monitored ◦ Patient’s neurologic condition dictates the acceptable range Next ◦ Barbiturate coma and vasospasm will cause lower values Select NEXT to see ◦ When used with other forms of monitoring, can help identify why changes in more Cerebral Blood ICP are occurring Flow Monitoring
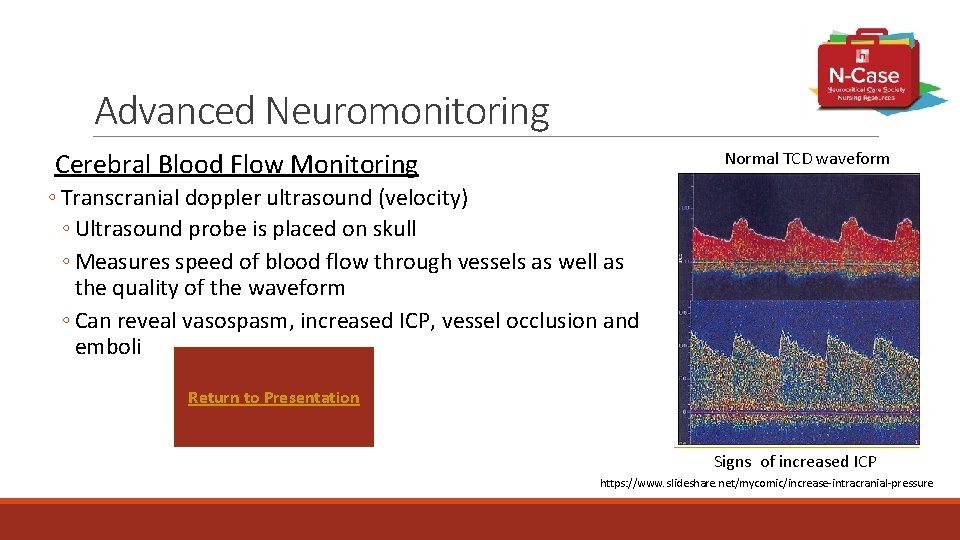
Advanced Neuromonitoring Cerebral Blood Flow Monitoring Normal TCD waveform ◦ Transcranial doppler ultrasound (velocity) ◦ Ultrasound probe is placed on skull ◦ Measures speed of blood flow through vessels as well as the quality of the waveform ◦ Can reveal vasospasm, increased ICP, vessel occlusion and emboli Return to Presentation Signs of increased ICP https: //www. slideshare. net/mycomic/increase-intracranial-pressure
Advanced Neuromonitoring Cerebral Microdialysis ◦ Microcatheter inserted into brain parenchyma ◦ Small pump delivers dialysate fluid into the brain ◦ Fluid is pumped back out into small vial and analyzed hourly ◦ Fluid is analyzed for extracellular levels of cerebral metabolites ◦ Includes glucose, lactate, pyruvate, glutamate and others ◦ Changes in the amount of these chemicals can be indicative of early ischemia Return to Presentation
Advanced Neuromonitoring Electrophysiologic monitoring with Electro. Encephalo. Graphy (EEG) ◦ Captures electrical activity of neurons ◦ Waveforms are evaluated for ◦ Frequency, amplitude, symmetry and patterns ◦ Waveforms seen reflect physiology ◦ Changes can be global or localized ◦ Global changes may represent change in coma level ◦ Also beneficial in subclinical seizure monitoring ◦ Can help with titration of seizure medications Return to Presentation
Check Point - Answer You are CORRECT!! What is the best description of the injury described by the CT report? A - Right frontal intracerebral hemorrhage which represents coup, and occipital contusion which represents contrecoup The patient is known to have struck her forehead against the steering wheel, correlating with the frontal hematoma. The occipital contusion results from the brain striking the posterior skull opposite of the original impact. Return to Presentation
Check Point - Answer You are CORRECT!! What is the purpose of implementing continuous EEG monitoring for this patient? C. Assess for subclinical seizures Because of the patient’s previous seizure, EEG is placed to monitor for subclinical seizure activity. The Propofol infusion can be titrated based upon the EEG results. Return to Presentation
Check Point - Answer You are CORRECT!! The ICP recorded on the EVD has been 18. While suctioning, the ICP increases to 26 while coughing. The ICP returns to 18 two minutes after coughing completed. What is the best nursing intervention? C - Nothing, these transient increases in ICP are normal Many normal activities can increase ICP, such as coughing, bearing down, or repositioning. It is important for the nurse to monitor that the patient’s ICP returns to baseline immediately following interventions. Sustained increases in ICP greater than 5 minutes are cause for further intervention. Return to Presentation
Check Point - Answer You are CORRECT!! the answer is “B” Which of the following treatments are used for intracranial hypertension? B is correct: HYPERTONIC SALINE (decrease cerebral edema), HYPOTHERMIA (decrease cerebral metabolism), MANNITOL (decrease cerebral edema) A is incorrect: Mannitol, vasopressin (this is not used to decrese ICP), hypertonic saline, propofol C is incorrect: Propofol, lorazepam (this is not used to decrease ICP), magnesium (this is not used to decrease ICP), hypertonic saline D is incorrect: Hypertonic saline, phenylephrine (this is not used to decrease ICP), phenytoin (this is not used to decrease ICP) Return to Presentation
Check Point - Answer You are CORRECT!! the answer is “A” Basic treatment for brain injury include: A is correct: ABC’S, HOB ELEVATED, FEVER MANAGEMENT, TREND NEURO ASSESSMENT B is incorrect: Hypothermia, hypercarbia (low normal PCO 2 30 -35 is best), hypoxia (should be avoided) C is incorrect: Administer D 50 (normoglycemia is best), hypocapnia(low norm PCO 2 is best), paralysis D is incorrect: 100% oxygen delivery (concern with O 2 toxicity), head of bed 15° (HOB 30°), fever management, trend of neurologic status Return to Presentation
Check Point - Answer You are CORRECT!! the answer is “B” Cushing’s Triad The patient exhibits hypertension, bradycardia, & irregular respirations. This patient exhibits which of the following: A is incorrect: uncal herniation is unilateral pupil dilation C is incorrect: Horner’s is ipsilateral miosis, ptosis, anhidrosis D is incorrect: cingulate herniation is coma and abnormal posturing Return to Presentation
- Slides: 148