National Tuberculosis Control Guidelines Part II Prof Hala
National Tuberculosis Control Guidelines Part II Prof. Hala Abdulhameed MBBCH , MSc , MD, FCCP Chest and Critical Care diseases. Minia University
What is tuberculosis Tuberculosis is an infectious disease caused mainly by Mycobacterium tuberculosis. 2 types can cause the disease in man : human (98%) and Bovine (2%)bacilli. Mode of infection 1 -Inhalation of droplets &droplet nuclei. 2 - Ingestion of milk of infected animals 3 - Skin 4 - congental Predisposing factors Age: Below 5 years: high susceptibility to develop disease but low incidence of exposure. 5 -15 y less susceptibility above 15 y : high susceptibility to progressive pulmonary disease
Chest diseases: silicosis & asbestosis Pulmonary infections e. g. viral Pulmonary oligaimia Decrease immunity : D. M -immunosupressive e. g. corticosteroids. -AIDS-. Malignancies especiallylymphomas. Malnutrition, alcoholism&gastrectomy Race : more in black Developing countries & low scio-ecnomic classes Occupation : doctors &nurses
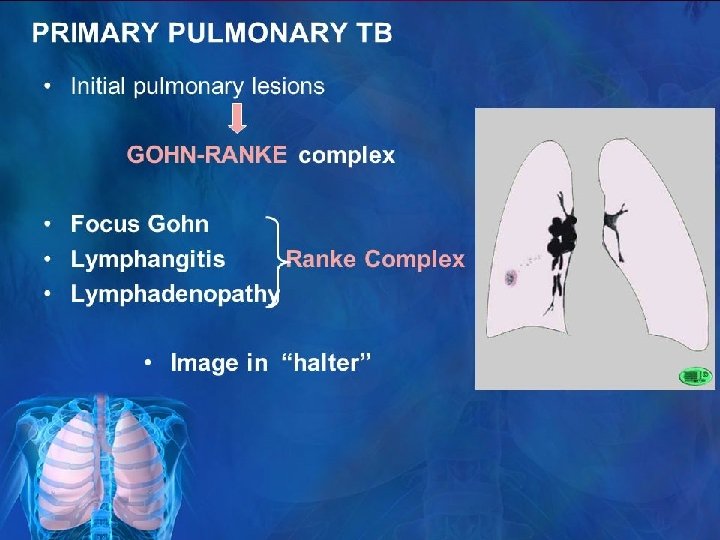
EVOLUTION OF INFCTION Primary Tuberculosis This occurs is a person who has not yet been infected. Primary tuberculosis is mostly pulmonary and may be extra – pulmonary. Primary pulmonary TB consist of Ghon s focus. hilar lymph node and intervening lymphangitis. An example of the extra – pulmonary from of primary TB is intestinal primary TB.
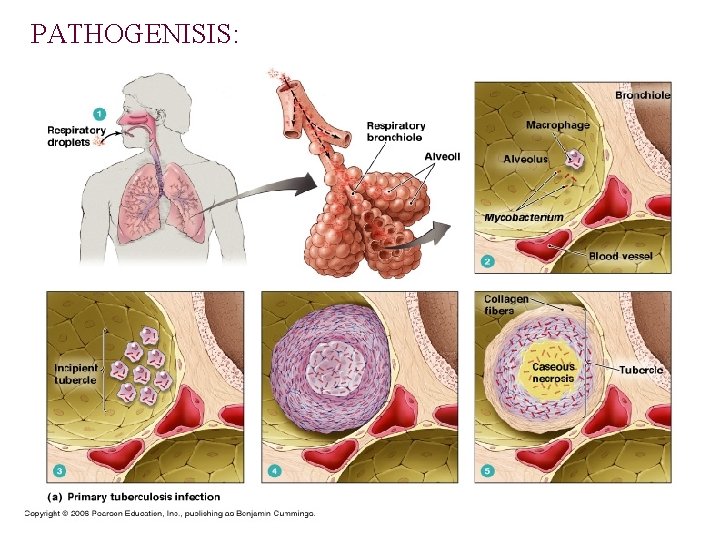
PATHOGENISIS:
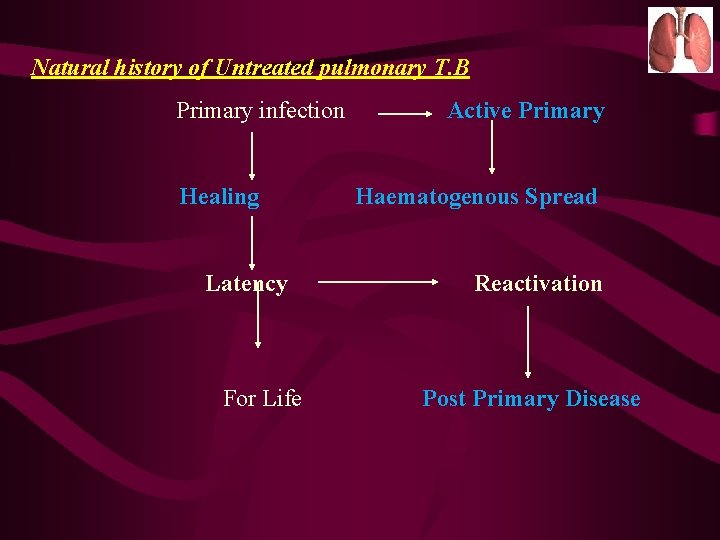
Natural history of Untreated pulmonary T. B Primary infection Healing Latency For Life Active Primary Haematogenous Spread Reactivation Post Primary Disease
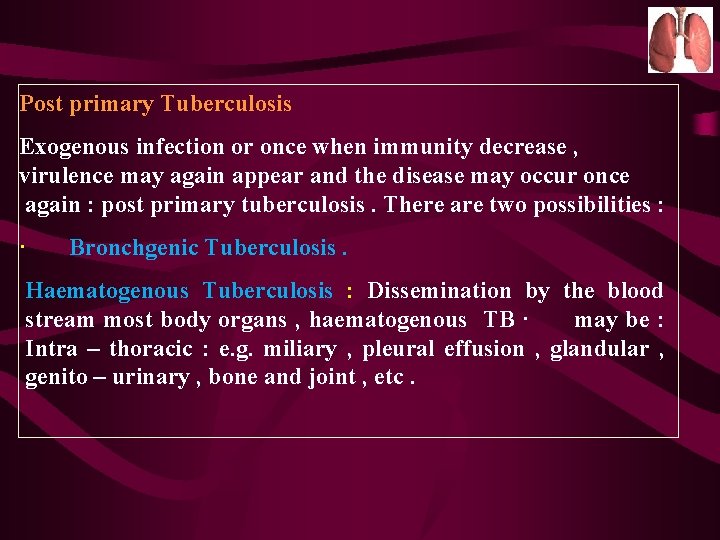
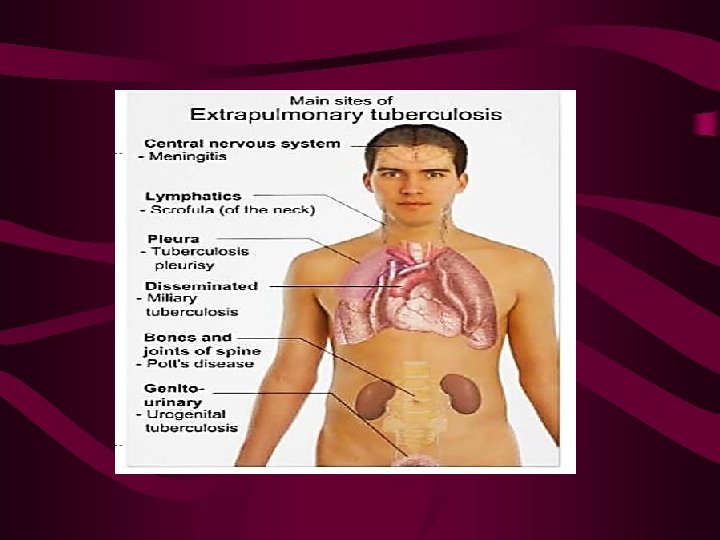
Post primary Tuberculosis Exogenous infection or once when immunity decrease , virulence may again appear and the disease may occur once again : post primary tuberculosis. There are two possibilities : · Bronchgenic Tuberculosis. Haematogenous Tuberculosis : Dissemination by the blood stream most body organs , haematogenous TB · may be : Intra – thoracic : e. g. miliary , pleural effusion , glandular , genito – urinary , bone and joint , etc.
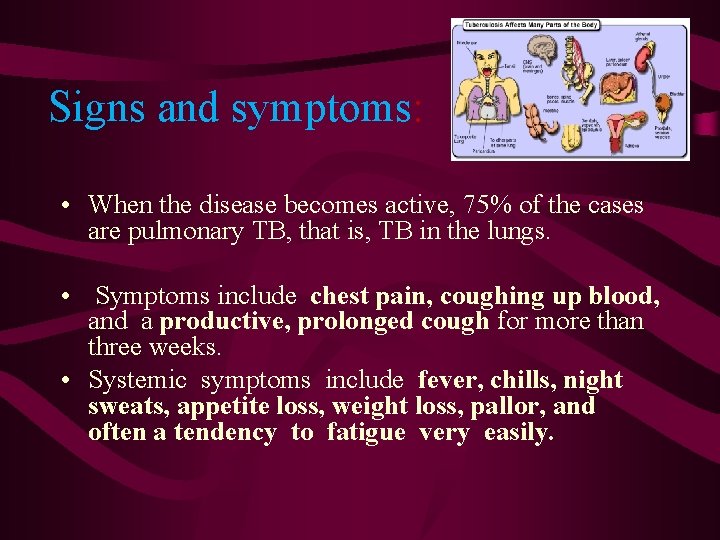
Signs and symptoms: • When the disease becomes active, 75% of the cases are pulmonary TB, that is, TB in the lungs. • Symptoms include chest pain, coughing up blood, and a productive, prolonged cough for more than three weeks. • Systemic symptoms include fever, chills, night sweats, appetite loss, weight loss, pallor, and often a tendency to fatigue very easily.
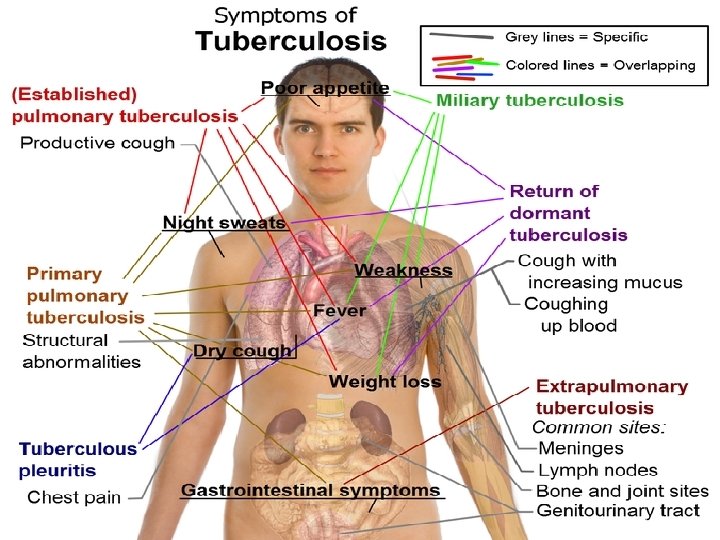

When to suspect Tuberculosis ? • Persistent cough for two weeks or more , * Presence of sputum , may blood – stained • * Breathlessness and chest pain. · * General symptoms such as fever, loss of appetite * A history of contact with a TB patient. · *The symptoms and signs of extra-pulmonary TB depend on the organ involved ,
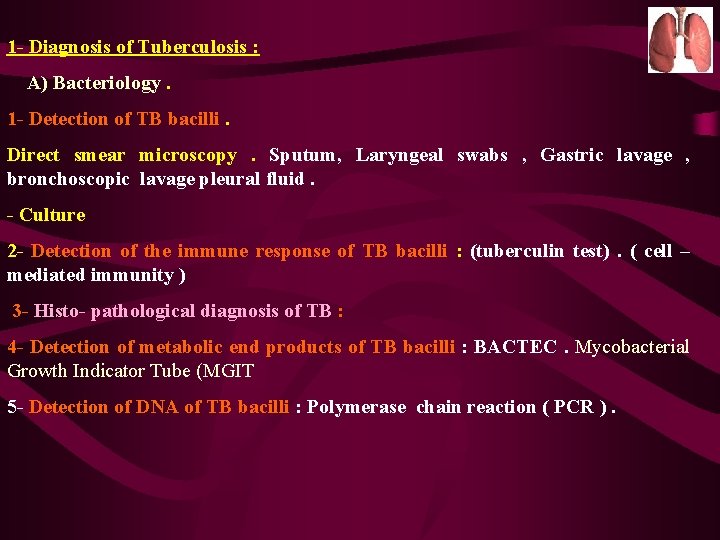
1 - Diagnosis of Tuberculosis : A) Bacteriology. 1 - Detection of TB bacilli. Direct smear microscopy. Sputum, Laryngeal swabs , Gastric lavage , bronchoscopic lavage pleural fluid. - Culture 2 - Detection of the immune response of TB bacilli : (tuberculin test). ( cell – mediated immunity ) 3 - Histo- pathological diagnosis of TB : 4 - Detection of metabolic end products of TB bacilli : BACTEC. Mycobacterial Growth Indicator Tube (MGIT 5 - Detection of DNA of TB bacilli : Polymerase chain reaction ( PCR ).
Diagnosis of Pulmonary TB is A bacteriological one. Ø Microscopic Direct Smear Examination is an easy and quick procedure. A minimum of three samples must be examined. Ø Cultures: • To confirm the diagnosis even in smear negative. • To detect drug susceptibility and resistance. • To detect the bacilli in any specimen in extrapulmonary tuberculosis.
Collection of sputum samples • A PTB suspect should submit 3 sputum samples for microscopy. • The chances of finding tubercle bacilli are greater with 3 sputum samples than with 2 samples or 1 sample. • Secretions build up in the airways overnight. • So an early morning sputum sample is more likely than a sample later in the day to contain tubercle bacilli. Sensitivity of sputum smear microscopy • Sputum smear microscopy for tubercle bacilli is positive when there at least 10, 000 organisms present per 1 ml of sputum.

Solid Conventional Culture (Lowenstein-Jansen medium) �Culture of sputum is more sensitive (require from 10 -100 mycobacteria /ml sputum
TUBERCULIN SKIN TESTING • The tuberculin skin test (TST) has limited value in clinical work, especially where TB is common. The test shows hypersensitivity to proteins of the TB bacillus, as a result either of infection with M. tuberculosis or induced by Bacille Calmette-Guérin (BCG) vaccination. The test involves injecting tuberculin purified protein derivative (PPD) into the skin (intradermal). • Previous exposure results in a local delayed type hypersensitivity reaction within 24 -72 hours

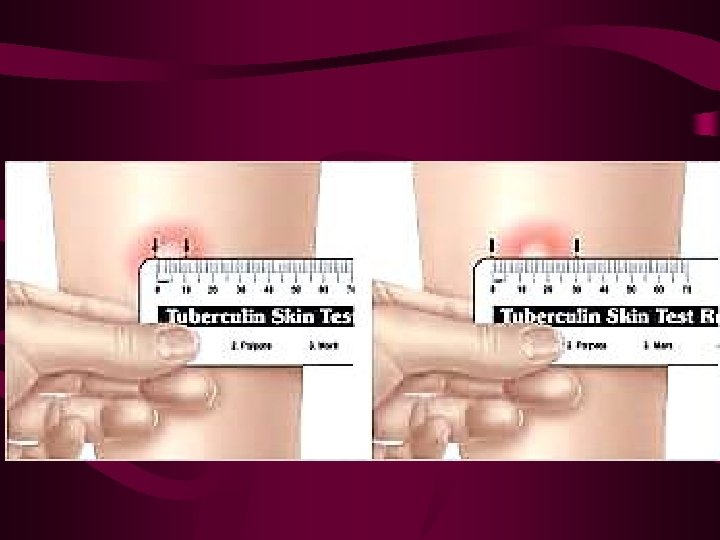

Reading interpreting a positive Tuberculin Skin Test Immune Status and age group HIV positive, malnourished, severe illness at any age HIV negative and not immune-compromised Diameter of induration to consider the test positive ≥ 5 mm If no history of BCG vaccination or after age of 6 years ≥ 10 mm If history of BCG vaccination or before age of 5 years ≥ 15 mm
CONDITIONS WHICH MAY SUPPRESS THE TUBERCULIN SKIN TEST • HIV infection • Malnutrition • Severe bacterial infections, including TB itself • Viral infections, e. g. measles, chickenpox, glandular fever • Cancer • Immunosuppressive drugs, e. g. steroids
1 - Diagnosis of Tuberculosis : A) Bacteriology. 1 - Detection of TB bacilli. Direct smear microscopy. Sputum, Laryngeal swabs , Gastric lavage , bronchoscopic lavage pleural fluid. - Culture 2 - Detection of the immune response of TB bacilli : (tuberculin test). ( cell – mediated immunity ) 3 - Histo- pathological diagnosis of TB : 4 - Detection of metabolic end products of TB bacilli : BACTEC. Mycobacterial Growth Indicator Tube (MGIT 5 - Detection of DNA of TB bacilli : Polymerase chain reaction ( PCR ).
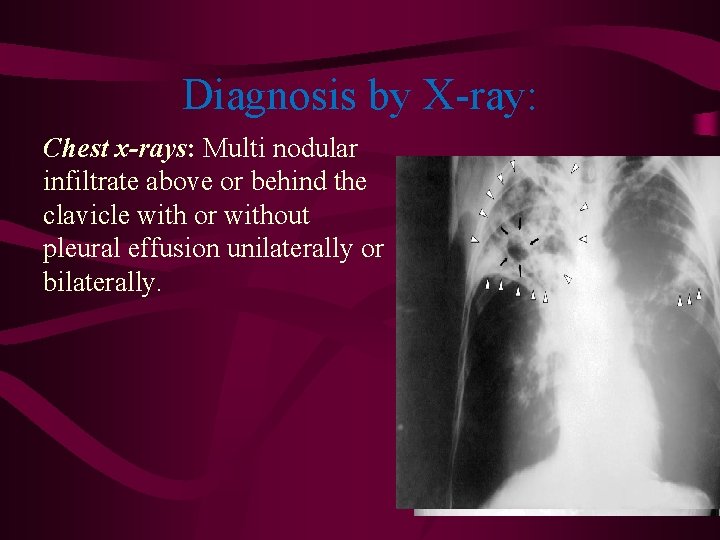
Diagnosis by X-ray: Chest x-rays: Multi nodular infiltrate above or behind the clavicle with or without pleural effusion unilaterally or bilaterally.
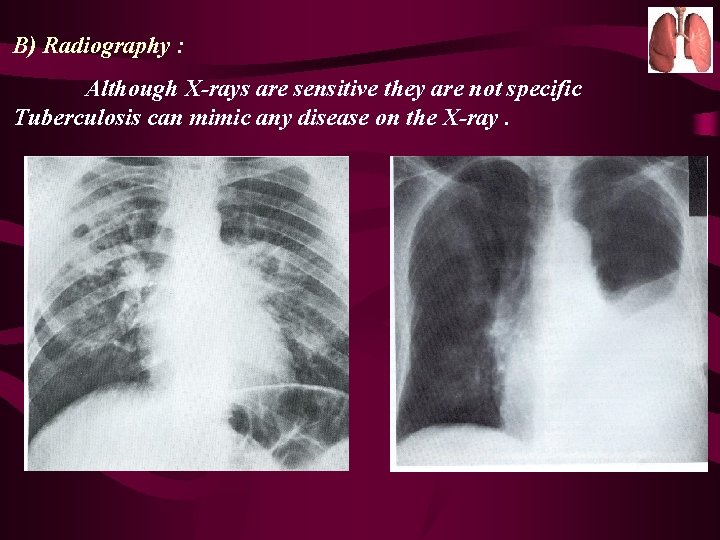
B) Radiography : Although X-rays are sensitive they are not specific Tuberculosis can mimic any disease on the X-ray.
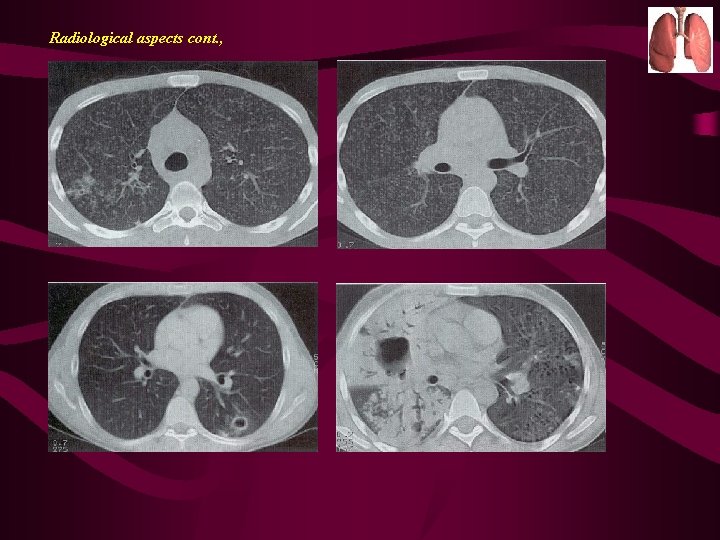
Radiological aspects cont. ,
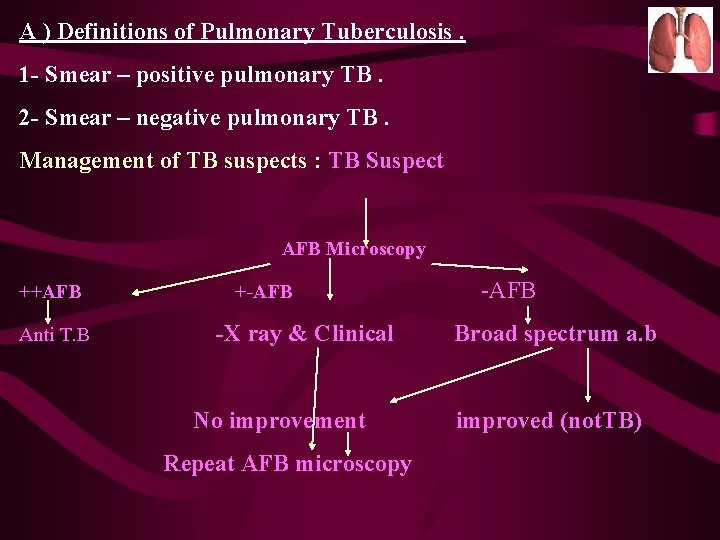
A ) Definitions of Pulmonary Tuberculosis. 1 - Smear – positive pulmonary TB. 2 - Smear – negative pulmonary TB. Management of TB suspects : TB Suspect AFB Microscopy ++AFB Anti T. B +-AFB -X ray & Clinical No improvement Repeat AFB microscopy -AFB Broad spectrum a. b improved (not. TB)

Repeat- microscopy AFB +AFB - --AFB X-ray---physician Yes TB No TB Treat as smear positive FTB Treat as smear negative FTB other diagnoses
II. Therapeutic : General care : * Rest in bed in acute phases , later on ambulatory Treatment is allowed. * Proper nutrition. Symptomtic treatment : * Antipyretics for fever. * Expectorants & mucolytics.
TB chemotherapy should be based on two important microbiological considerations: • The combination of drugs to avoid the development of resistance. • The need for prolonged chemotherapy to prevent disease relapse.
Treatment : I. Prophylactic : *(Iry) immunoprophylaxis : using BCG vaccination It is indicated in the following situations : - Countries. with a high incidence of TB ( given to neonates or as early as possible to children ). - High –risk groups e. g. : contacts of tuberculous patients. health professionals. 2 ry immunoprophylaxis using INH for 9 months - Contacts of tuberculous patients with recent tuberculin conversion. - Immunocompromised patients with chest x-ray changes
Phases of treatment: The intensive phase • • • usually covers the first 2 months of treatment. During this phase, most of the bacilli will be killed. The sputum converts from positive to negative in more than 80 % of the new patients within the first 2 months of treatment. The continuation phase • • usually lasts 4 months, depending on the treatment regimen. This phase is intended to eliminate the remaining dormant bacilli. These dormant bacilli decrease constantly as treatment intake progresses. Since it is not possible to identify which patients still have dormant bacilli, all patients should continue their treatment until the end of the prescribed period, to limit the number of relapses.
DOTS strategy DOTS means directly observed treatment with short course chemotherapy Principles of DOTS strategy • Government commitment to TB control • Case detection through sputum-smear microscopy in the general health services • Standardized short-course chemotherapy to, at least, all smearpositive TB cases under proper case management conditions • Regular, uninterrupted supply of all essential anti-tuberculous drugs • Monitoring system for programme supervision and evaluation
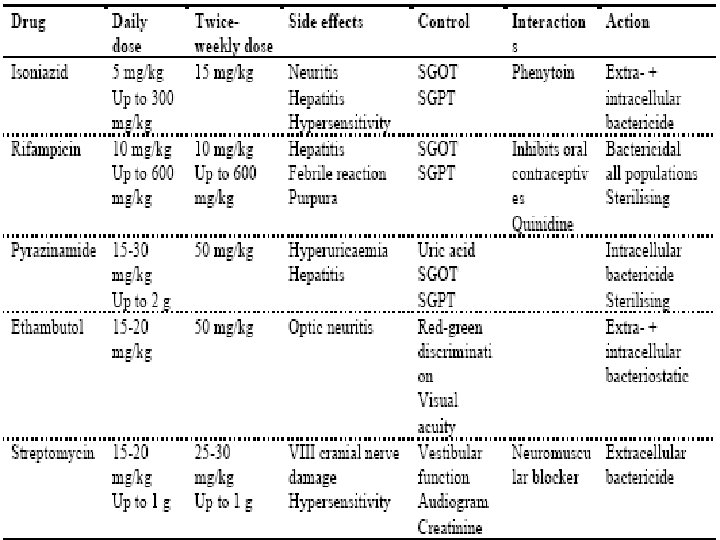
First-line anti-tuberculosis drugs, action and side effects
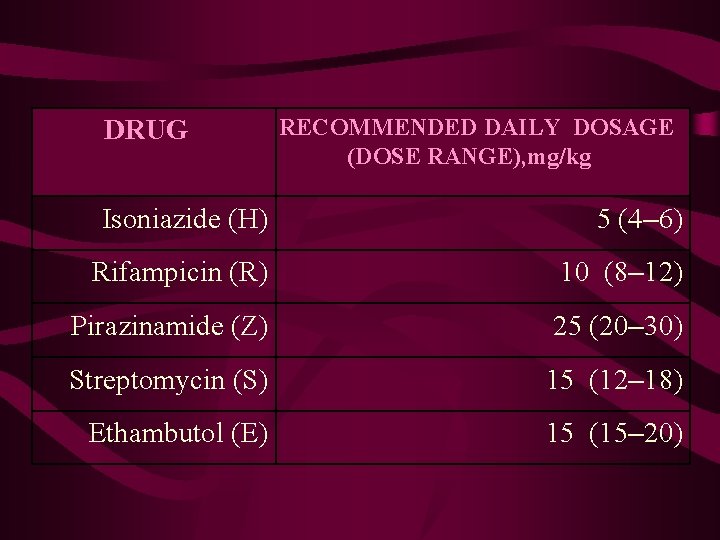
DRUG RECOMMENDED DAILY DOSAGE (DOSE RANGE), mg/kg Isoniazide (H) 5 (4– 6) Rifampicin (R) 10 (8– 12) Pirazinamide (Z) 25 (20– 30) Streptomycin (S) 15 (12– 18) Ethambutol (E) 15 (15– 20)

- Slides: 36