National Center for Emerging and Zoonotic Infectious Diseases












- Slides: 85
National Center for Emerging and Zoonotic Infectious Diseases Infection Prevention and Control Principles for Environmental Services Matthew J. Stuckey, Ph. D, MPH Division of Healthcare Quality and Promotion, NCEZID, CDC, Atlanta The presenters are federal employees and have no financial conflicts or disclosures to report
Objectives § Explain basic concepts of the germ theory and chain of infection as applicable in clinical settings § Describe risk recognition in the environment of care § Identify environment of care principles to break the chain of infection § Discuss ways to promote multidisciplinary collaboration when designing healthcare environments
Outline § § § § Background Germ Theory & Chain of Infection Risk Recognition EVS Cleaning Case Study Breaking the Chain of Infection Improving Cleaning Procedures Bridging Gaps: Inter-department Engagement & Collaboration

BACKGROUND
Healthcare Associated Infection (HAI) § An infection acquired in a healthcare facility by a patient who was admitted for a reason other than the infection § An infection occurring in a patient during the process of care in a hospital or other healthcare facility that was absent or incubating at the time of admission – Includes infections that appear after discharge
HAI Burden § One of the leading causes of unnecessary death and avoidable harm for patients receiving health care § Estimated 722, 000 HAIs in U. S. acute care hospitals (2011 data) § Approximately 1 in 25 hospitalized patients
HAI Exposure Risks § Infected or colonized HCP or another patient (cross-infection) § The patient’s own flora (endogenous infection) § Environmental surfaces or objects contaminated from another human source, e. g. , bed rails, IV poles, counter tops, bathroom surfaces § Contaminated medical devices, e. g. , central venous catheters, urinary catheters, endoscopes, surgical instruments, ventilators § Contaminated medications § Contaminated water sources § Contaminated air
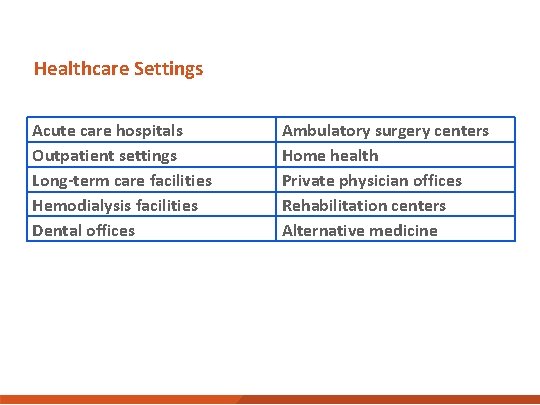
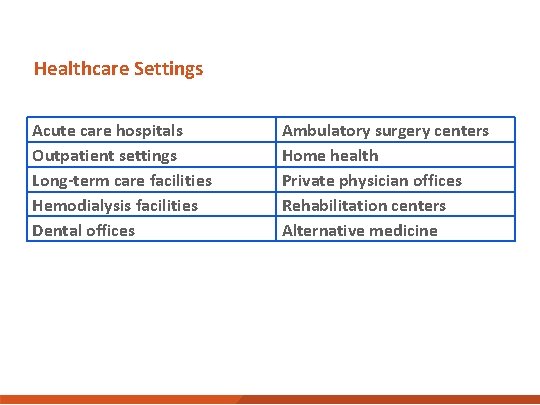
Healthcare Settings Acute care hospitals Outpatient settings Long-term care facilities Hemodialysis facilities Dental offices Ambulatory surgery centers Home health Private physician offices Rehabilitation centers Alternative medicine
Questions § What healthcare setting do you primarily work in? § Do you receive reports about your facility’s HAI data?
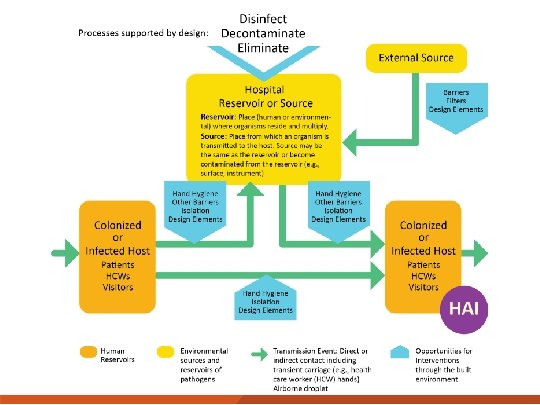
GERM THEORY & CHAIN OF INFECTION
Germ Theory § Infectious diseases are caused by microorganisms (e. g. , bacteria, virus, fungi) that invade the body and multiply § Established in the 1800 s § Recognizes contributory host factors § Basis for other theories of disease transmission, e. g. , chain of infection
Infection vs. Colonization Infection Occurs when pathogens and other microorganisms are present in the body and cause tissue damage and signs and symptoms of illness (e. g. , fever, redness, pain, sepsis). Colonization Occurs when pathogens and other microorganisms are present but do not cause signs and symptoms of illness. If the pathogen is present, disease transmission is possible
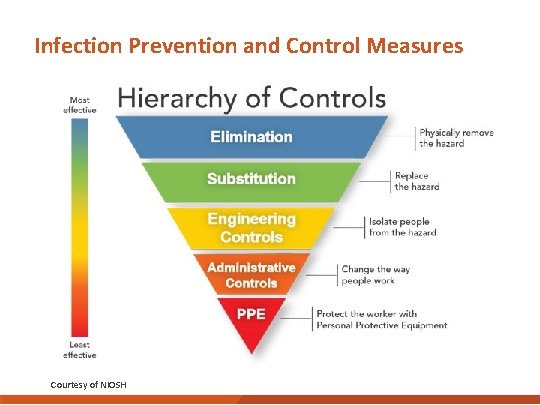
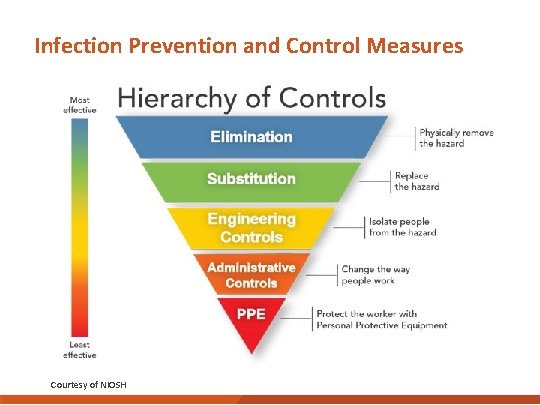
Infection Prevention and Control Measures Courtesy of NIOSH
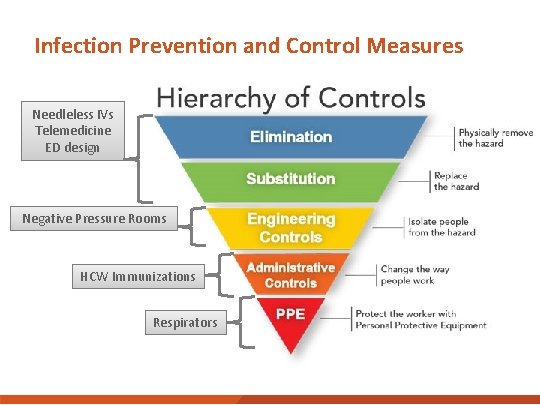
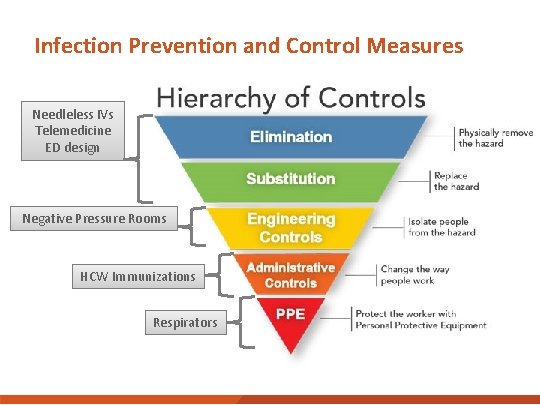
Infection Prevention and Control Measures Needleless IVs Telemedicine ED design Negative Pressure Rooms HCW Immunizations Respirators

RISK RECOGNITION
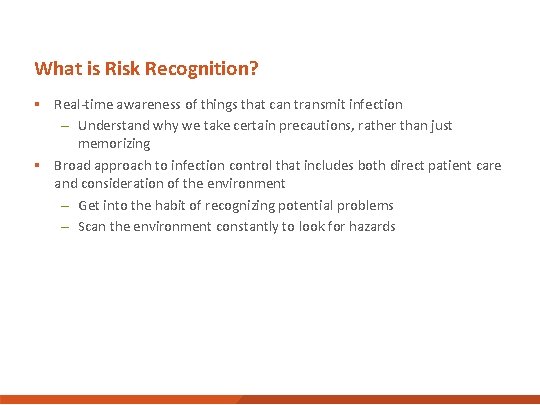
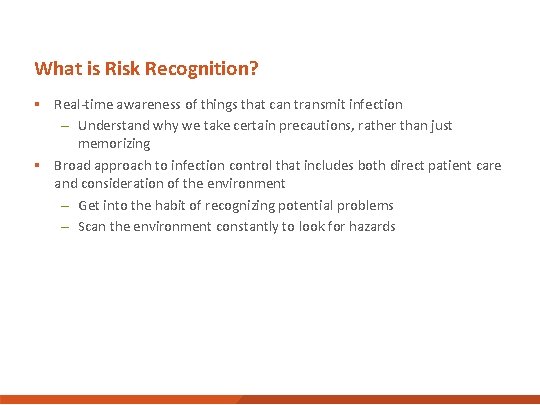
What is Risk Recognition? § Real-time awareness of things that can transmit infection – Understand why we take certain precautions, rather than just memorizing § Broad approach to infection control that includes both direct patient care and consideration of the environment – Get into the habit of recognizing potential problems – Scan the environment constantly to look for hazards
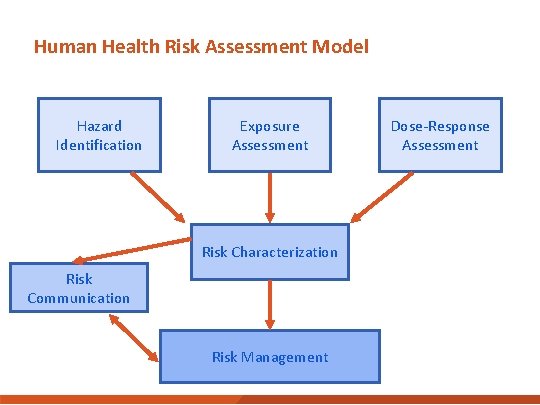
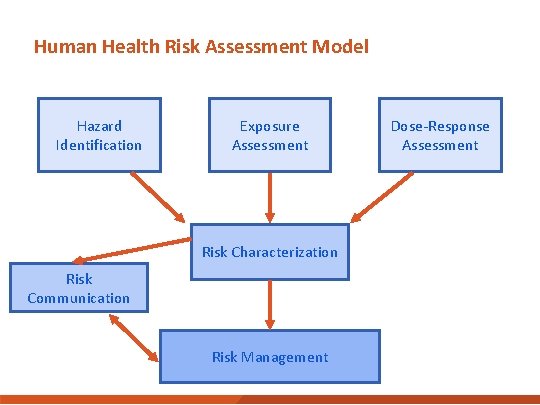
Human Health Risk Assessment Model Hazard Identification Exposure Assessment Risk Characterization Risk Communication Risk Management Dose-Response Assessment
Assessing Exposures § § § Where is the agent found? What are the routes of exposure? How many people are exposed? Who is exposed? What is the intensity, frequency, and duration of exposure?
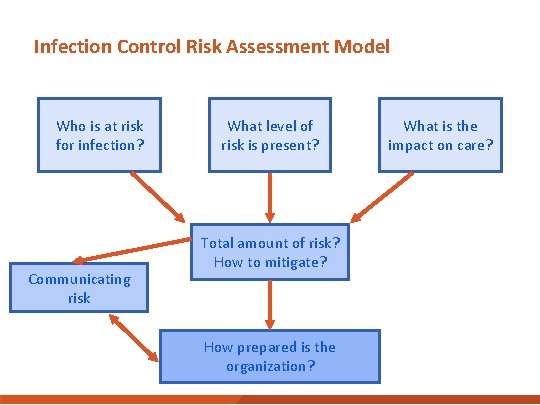
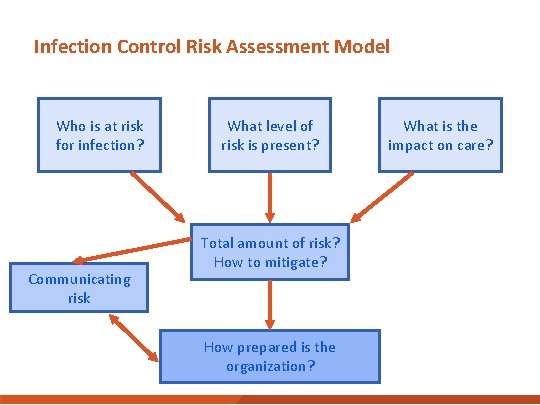
Infection Control Risk Assessment Model Who is at risk for infection? Communicating risk What level of risk is present? Total amount of risk? How to mitigate? How prepared is the organization? What is the impact on care?

RISK RECOGNITION AND THE HEALTHCARE ENVIRONMENT
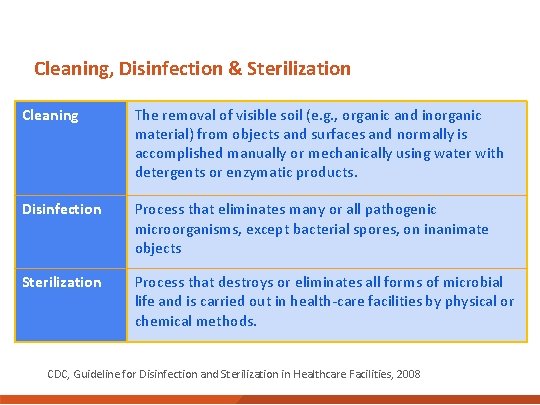
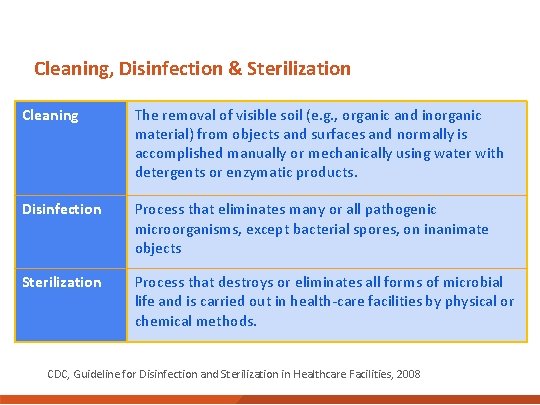
Cleaning, Disinfection & Sterilization Cleaning The removal of visible soil (e. g. , organic and inorganic material) from objects and surfaces and normally is accomplished manually or mechanically using water with detergents or enzymatic products. Disinfection Process that eliminates many or all pathogenic microorganisms, except bacterial spores, on inanimate objects Sterilization Process that destroys or eliminates all forms of microbial life and is carried out in health-care facilities by physical or chemical methods. CDC, Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008
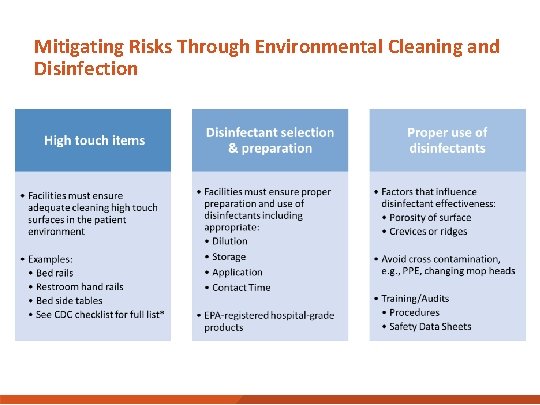
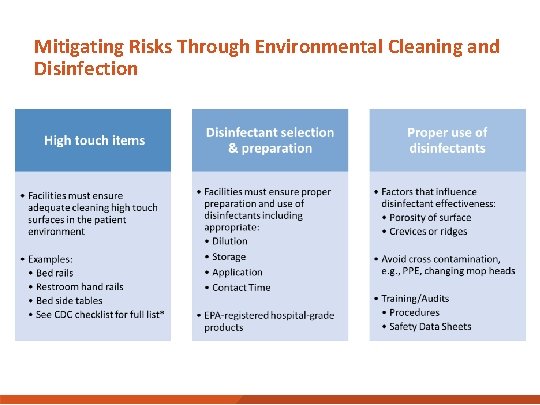
Mitigating Risks Through Environmental Cleaning and Disinfection
Practical Considerations: Constant Environmental Scan § Is there a risk of exposure to myself, my patient, visitors, or other patients in the task that I am about to perform in this environment? § If “yes”… – What basic infection prevention measures will mitigate the risks? – What specific elements of the situation are complex and interdependent?
Practical Considerations: Examples § Recognizing risks related to environmental services and supply management § New devices or procedures § Factors related to physical layout, furnishings
EVS Risk Recognition Examples § Does the EVS policy clearly state that environmental service staff will complete daily and as necessary cleaning of occupied spaces and cleaning at discharge? § Does the policy specify that patients are informed on arrival that environmental services will be performed on occupied rooms according to facility’s cleaning schedule? § Are there specific procedures that address how to effectively clean and disinfect surfaces including non-porous, high touch, upholstered surfaces and floors?
EVS Risk Recognition Examples (cont. ) § Is the quality of cleaning validated? – Direct observation – Adenosine triphosphate (ATP) – Glow germ § Does the facility have a policy requiring cleaning and maintenance of equipment (i. e. , ice machines, and whirlpools) based upon manufacturer’s instructions?
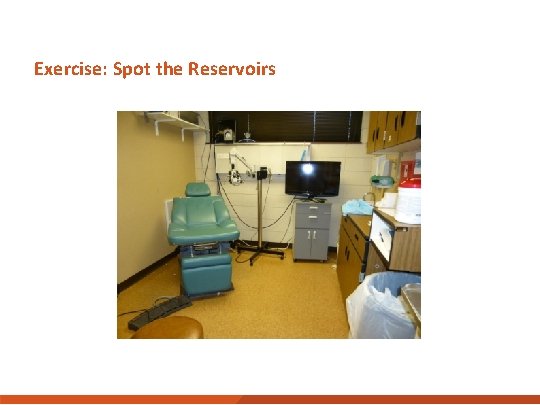
Exercise: Spot the Reservoirs
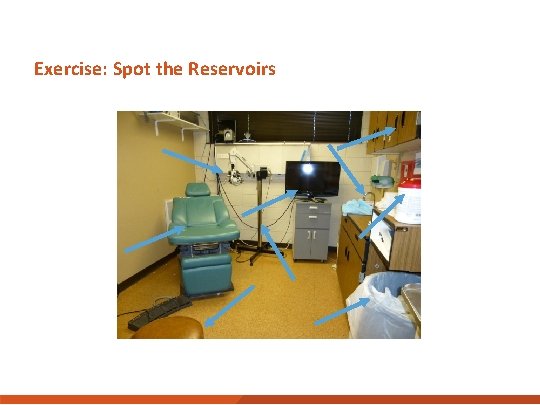
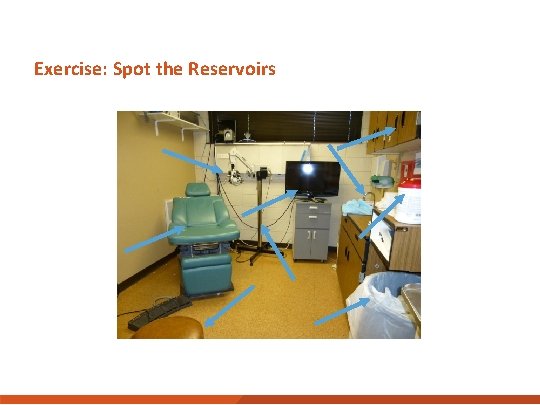
Exercise: Spot the Reservoirs

EVS CLEANING CASE STUDY
Study Aim: Measure the magnitude and determinants of pathogen emission and fate in healthcare settings § Focus on task-based exposures to pathogens and transmission § Emerging infectious diseases highlight: – Healthcare workers are at risk for infection – Some care activities are riskier than others
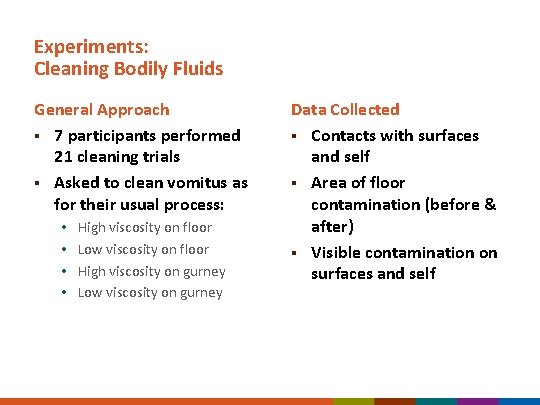
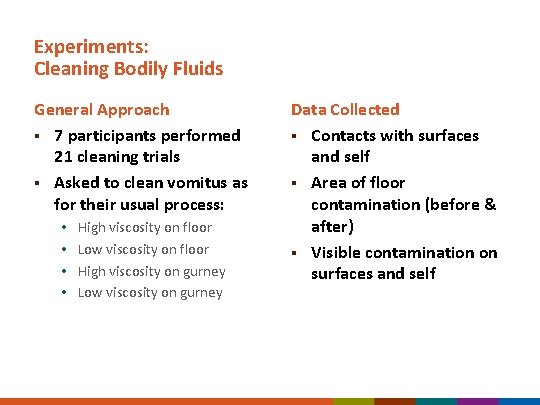
Experiments: Cleaning Bodily Fluids General Approach § 7 participants performed 21 cleaning trials § Asked to clean vomitus as for their usual process: • • High viscosity on floor Low viscosity on floor High viscosity on gurney Low viscosity on gurney Data Collected § Contacts with surfaces and self § Area of floor contamination (before & after) § Visible contamination on surfaces and self

What the Participant Can/Can’t See

Experimental Trial 173 A Low Viscosity Vomitus on Gurney Before and After Cleaning High Viscosity Vomitus
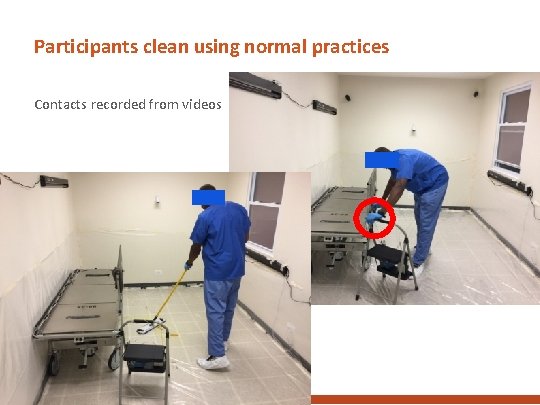
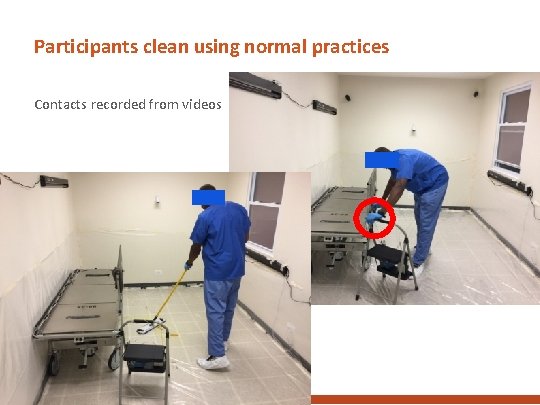
Participants clean using normal practices Contacts recorded from videos
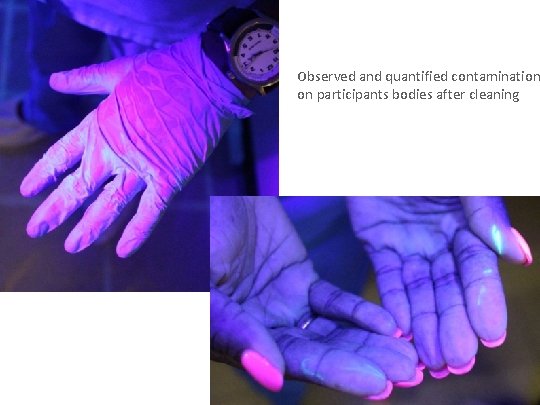
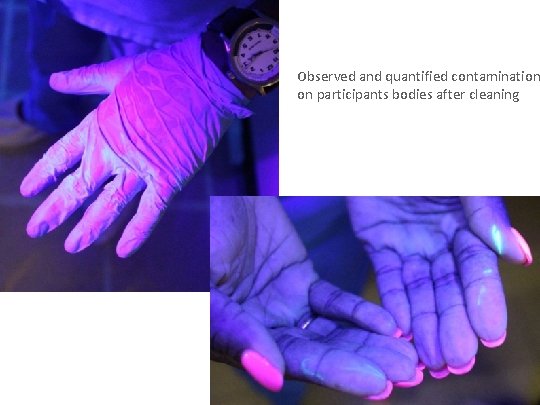
Observed and quantified contamination on participants bodies after cleaning
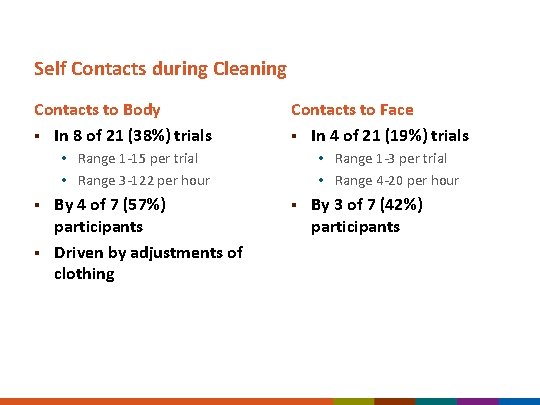
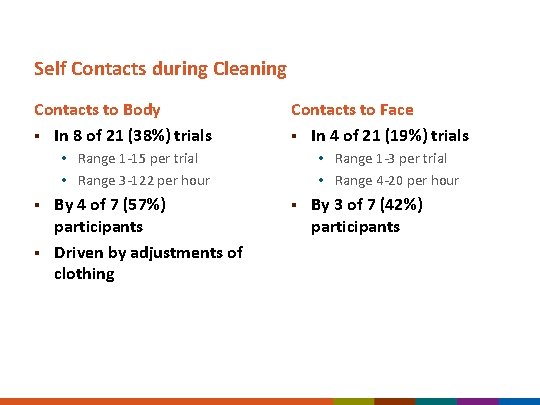
Self Contacts during Cleaning Contacts to Body § In 8 of 21 (38%) trials Contacts to Face § In 4 of 21 (19%) trials • Range 1 -15 per trial • Range 3 -122 per hour § § By 4 of 7 (57%) participants Driven by adjustments of clothing • Range 1 -3 per trial • Range 4 -20 per hour § By 3 of 7 (42%) participants
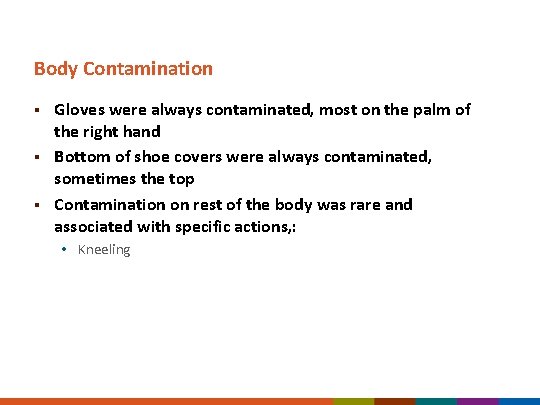
Body Contamination § § § Gloves were always contaminated, most on the palm of the right hand Bottom of shoe covers were always contaminated, sometimes the top Contamination on rest of the body was rare and associated with specific actions, : • Kneeling
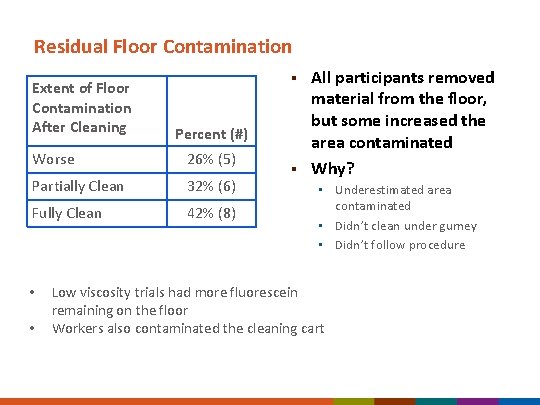
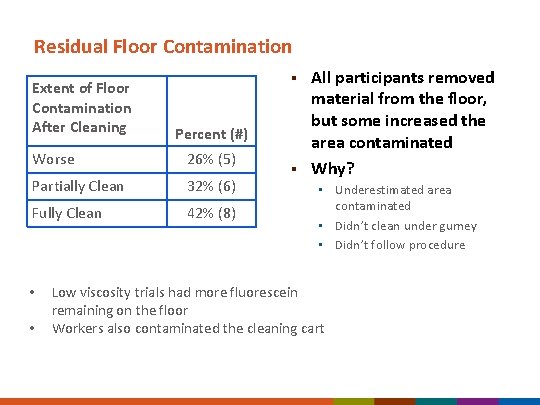
Residual Floor Contamination Extent of Floor Contamination After Cleaning § Percent (#) Worse 26% (5) Partially Clean 32% (6) Fully Clean 42% (8) • • § All participants removed material from the floor, but some increased the area contaminated Why? • Underestimated area contaminated • Didn’t clean under gurney • Didn’t follow procedure Low viscosity trials had more fluorescein remaining on the floor Workers also contaminated the cleaning cart
Skills Check You are the primary nurse and have been assigned a patient who is on Contact isolation. When you enter the patient’s room you notice the following risks: A. B. C. D. E. Empty sharps disposal container Isolation supplies (e. g. , gown, gloves, face shields) in anteroom Full hand hygiene dispenser on wall Disposable blood pressure at the head of the bed Overfilled trash receptacle
Skills Check You are the primary nurse and have been assigned a patient who is on Contact isolation. When you enter the patient’s room you notice the following risks: A. B. C. D. E. Empty sharps disposal container Isolation supplies (e. g. , gown, gloves, face shields) in anteroom Full hand hygiene dispenser on wall Disposable blood pressure at the head of the bed Overfilled trash receptacle
PERSISTENCE OF PATHOGENS ON ENVIRONMENTAL SURFACES
Microbial Reservoirs: Dry Surfaces
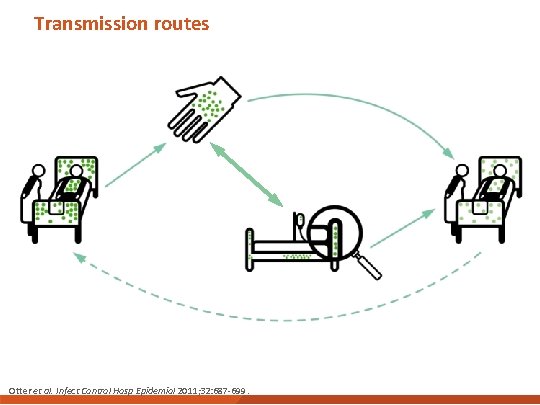
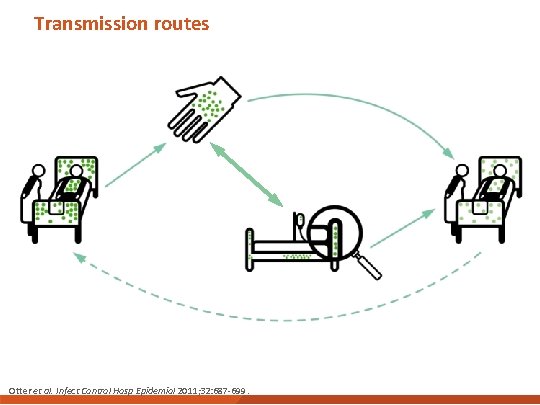
Transmission routes Otter et al. Infect Control Hosp Epidemiol 2011; 32: 687 -699.
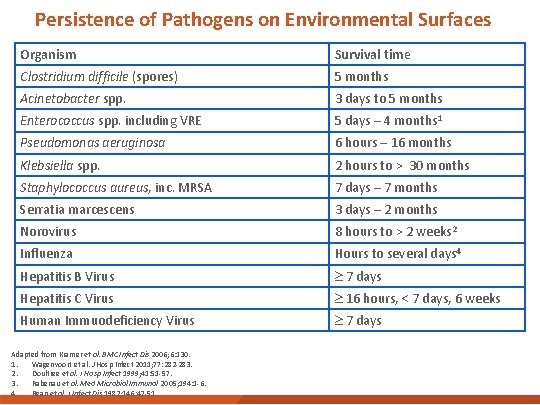
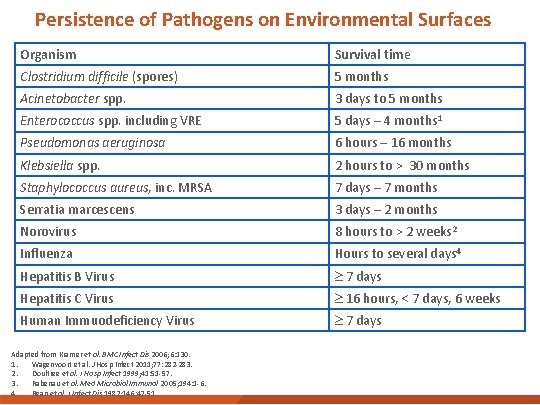
Persistence of Pathogens on Environmental Surfaces Organism Survival time Clostridium difficile (spores) 5 months Acinetobacter spp. 3 days to 5 months Enterococcus spp. including VRE 5 days – 4 months 1 Pseudomonas aeruginosa 6 hours – 16 months Klebsiella spp. 2 hours to > 30 months Staphylococcus aureus, inc. MRSA 7 days – 7 months Serratia marcescens 3 days – 2 months Norovirus 8 hours to > 2 weeks 2 Influenza Hours to several days 4 Hepatitis B Virus 7 days Hepatitis C Virus 16 hours, < 7 days, 6 weeks Human Immuodeficiency Virus 7 days Adapted from Kramer et al. BMC Infect Dis 2006; 6: 130. 1. Wagenvoort et al. J Hosp Infect 2011; 77: 282 -283. 2. Doultree et al. J Hosp Infect 1999; 41: 51 -57. 3. Rabenau et al. Med Microbiol Immunol 2005; 194: 1 -6. 4. Bean et al. J Infect Dis 1982; 146: 47 -51.
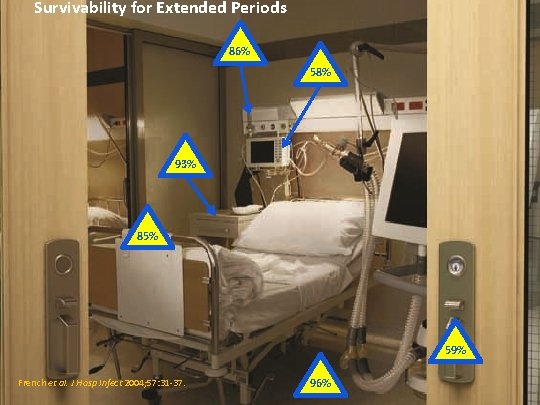
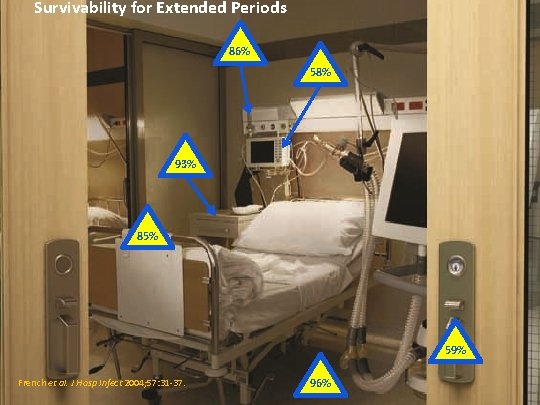
Survivability for Extended Periods 86% 58% 93% 85% 59% French et al. J Hosp Infect 2004; 57: 31 -37. 96%
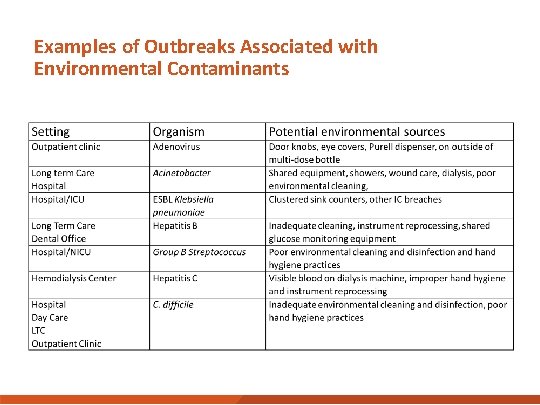
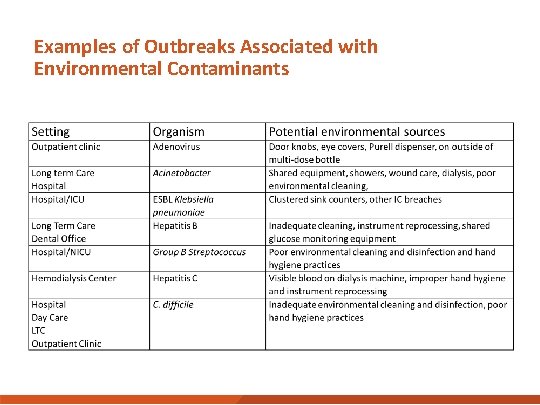
Examples of Outbreaks Associated with Environmental Contaminants
Skills Check You are the nurse manager of a medical intensive care unit. In the last month four patients on your unit have developed hospital-associated infections due to Acinetobacter. You have implemented several infection control strategies but with limited success. Transmission is on-going and you consider all of following approaches except: A. Collaborate with the EVS director to develop an auditing tool to audit the cleaning and disinfection practices of nursing and EVS staff B. Evaluate written cleaning protocols for EVS staff and nursing C. Engage EVS department in developing and conducting training session D. Immediately change cleaning and disinfection products
Skills Check You are the nurse manager of a medical intensive care unit. In the last month four patients on your unit have developed hospital-associated infections due to Acinetobacter. You have implemented several infection control strategies but with limited success. Transmission is on-going and you consider all of following approaches except: A. Collaborate with the EVS director to develop an auditing tool to audit the cleaning and disinfection practices of nursing and EVS staff B. Evaluate written cleaning protocols for EVS staff and nursing C. Engage EVS department in developing and conducting training session D. Immediately change cleaning and disinfection products

WATER-RELATED ENVIRONMENTAL INFECTION CONTROL
Microbial Reservoirs: Wet Surfaces
Exercise: Where Can Biofilms Form?
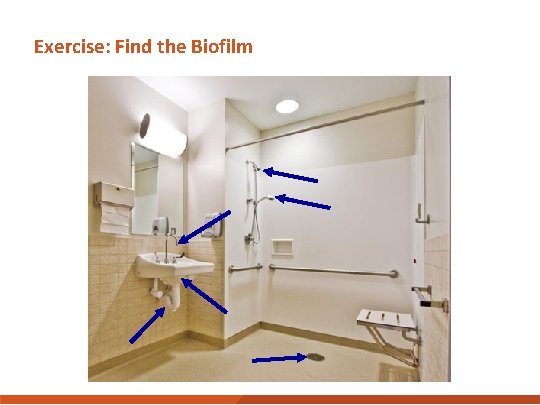
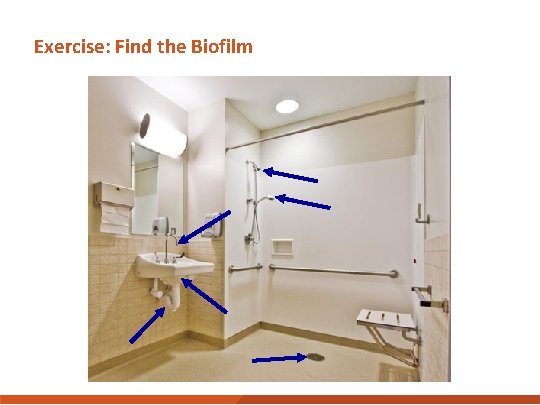
Exercise: Find the Biofilm
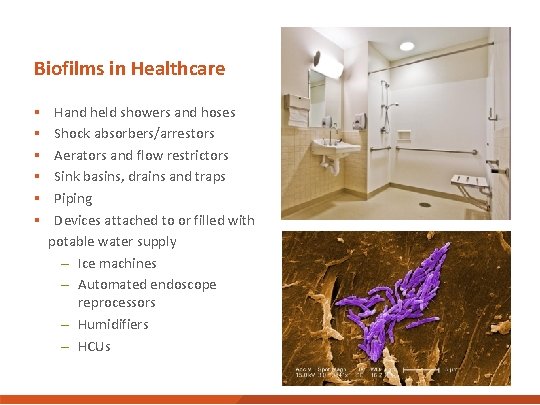
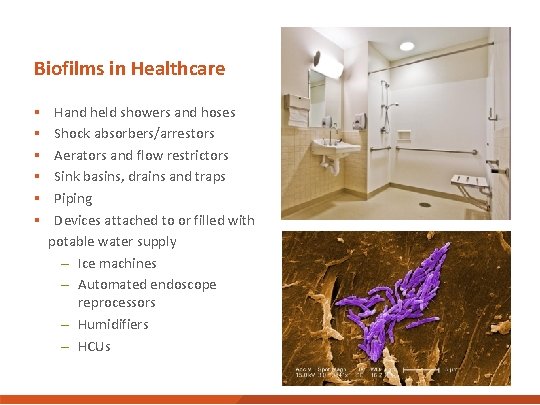
Biofilms in Healthcare § Hand held showers and hoses § Shock absorbers/arrestors § Aerators and flow restrictors § Sink basins, drains and traps § Piping § Devices attached to or filled with potable water supply – Ice machines – Automated endoscope reprocessors – Humidifiers – HCUs
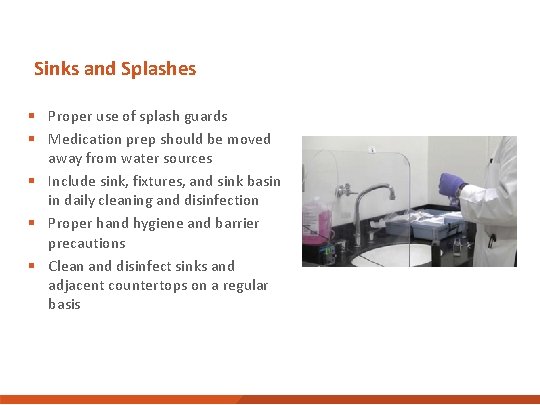
Sinks and Splashes § Proper use of splash guards § Medication prep should be moved away from water sources § Include sink, fixtures, and sink basin in daily cleaning and disinfection § Proper hand hygiene and barrier precautions § Clean and disinfect sinks and adjacent countertops on a regular basis
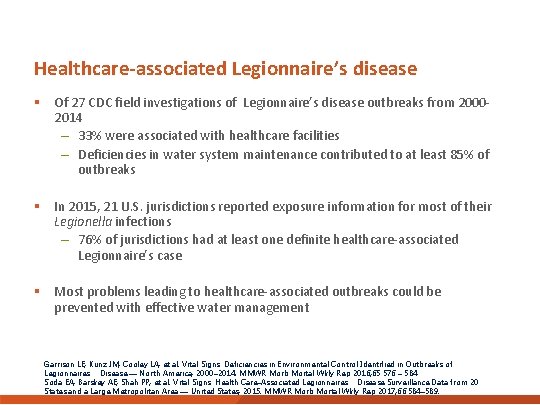
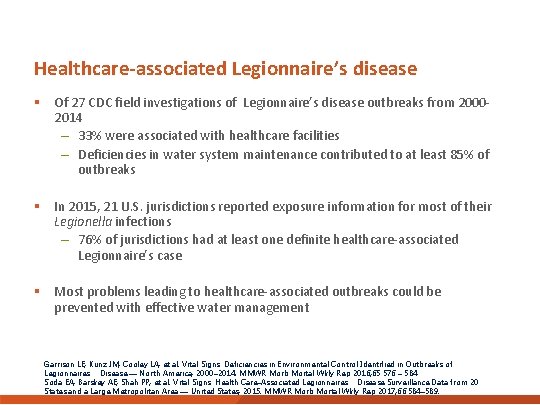
Healthcare-associated Legionnaire’s disease § Of 27 CDC field investigations of Legionnaire’s disease outbreaks from 20002014 – 33% were associated with healthcare facilities – Deficiencies in water system maintenance contributed to at least 85% of outbreaks § In 2015, 21 U. S. jurisdictions reported exposure information for most of their Legionella infections – 76% of jurisdictions had at least one definite healthcare-associated Legionnaire’s case § Most problems leading to healthcare-associated outbreaks could be prevented with effective water management Garrison LE, Kunz JM, Cooley LA, et al. Vital Signs: Deficiencies in Environmental Control Identified in Outbreaks of Legionnaires’ Disease — North America, 2000– 2014. MMWR Morb Mortal Wkly Rep 2016; 65: 576 – 584 Soda EA, Barskey AE, Shah PP, et al. Vital Signs: Health Care–Associated Legionnaires’ Disease Surveillance Data from 20 States and a Large Metropolitan Area — United States, 2015. MMWR Morb Mortal Wkly Rep 2017; 66: 584– 589.
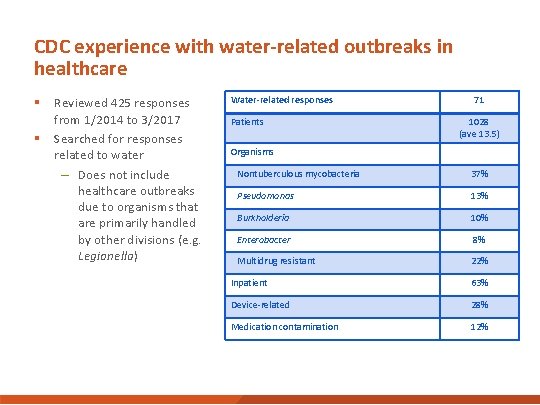
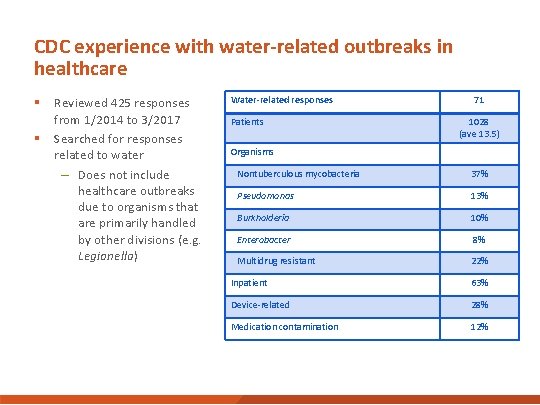
CDC experience with water-related outbreaks in healthcare § Reviewed 425 responses from 1/2014 to 3/2017 § Searched for responses related to water – Does not include healthcare outbreaks due to organisms that are primarily handled by other divisions (e. g. Legionella) Water-related responses Patients 71 1028 (ave 13. 5) Organisms Nontuberculous mycobacteria 37% Pseudomonas 13% Burkholderia 10% Enterobacter 8% Multidrug resistant 22% Inpatient 63% Device-related 28% Medication contamination 12%
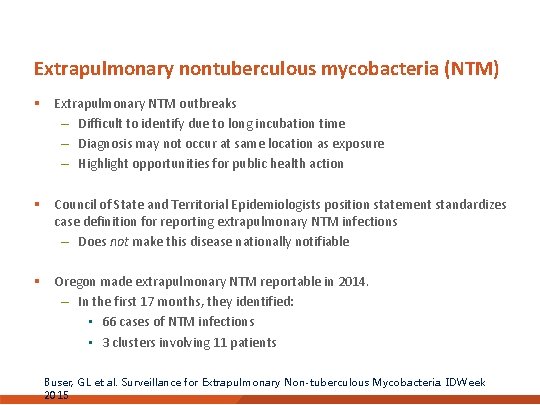
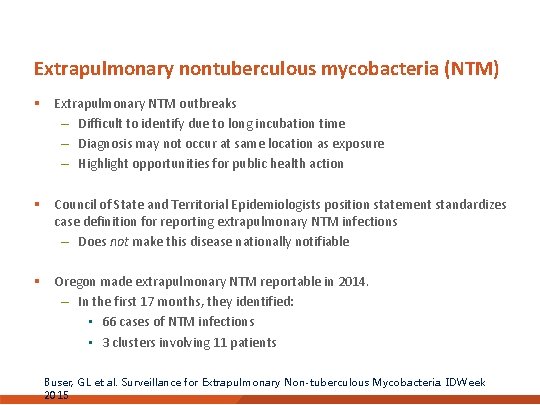
Extrapulmonary nontuberculous mycobacteria (NTM) § Extrapulmonary NTM outbreaks – Difficult to identify due to long incubation time – Diagnosis may not occur at same location as exposure – Highlight opportunities for public health action § Council of State and Territorial Epidemiologists position statement standardizes case definition for reporting extrapulmonary NTM infections – Does not make this disease nationally notifiable § Oregon made extrapulmonary NTM reportable in 2014. – In the first 17 months, they identified: • 66 cases of NTM infections • 3 clusters involving 11 patients Buser, GL et al. Surveillance for Extrapulmonary Non-tuberculous Mycobacteria. IDWeek 2015
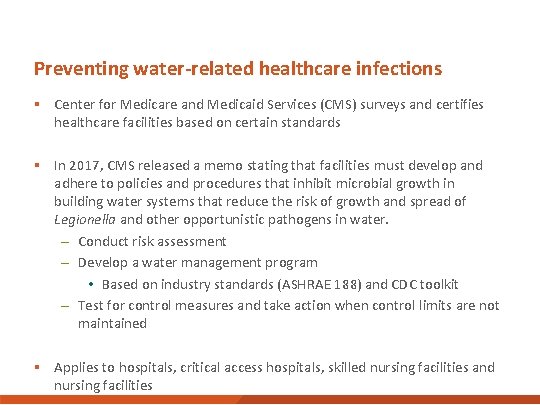
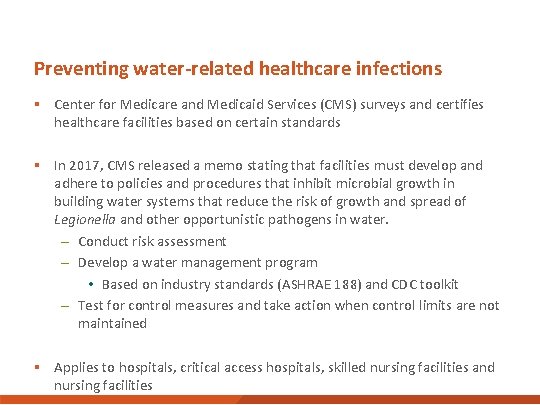
Preventing water-related healthcare infections § Center for Medicare and Medicaid Services (CMS) surveys and certifies healthcare facilities based on certain standards § In 2017, CMS released a memo stating that facilities must develop and adhere to policies and procedures that inhibit microbial growth in building water systems that reduce the risk of growth and spread of Legionella and other opportunistic pathogens in water. – Conduct risk assessment – Develop a water management program • Based on industry standards (ASHRAE 188) and CDC toolkit – Test for control measures and take action when control limits are not maintained § Applies to hospitals, critical access hospitals, skilled nursing facilities and nursing facilities
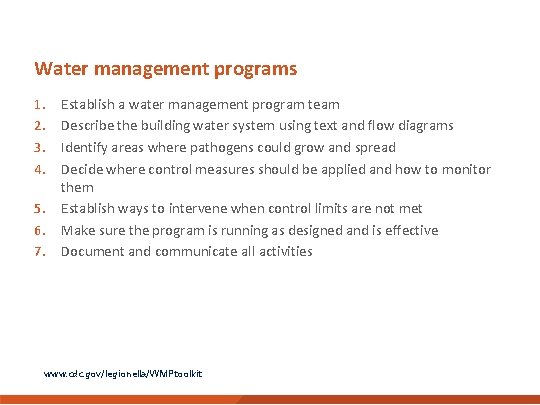
Water management programs 1. 2. 3. 4. 5. 6. 7. Establish a water management program team Describe the building water system using text and flow diagrams Identify areas where pathogens could grow and spread Decide where control measures should be applied and how to monitor them Establish ways to intervene when control limits are not met Make sure the program is running as designed and is effective Document and communicate all activities www. cdc. gov/legionella/WMPtoolkit
Focus on water supply and use
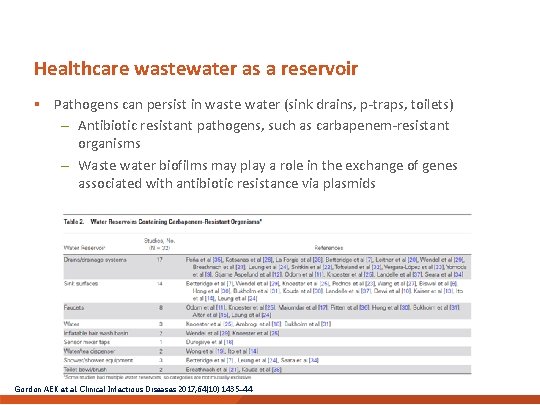
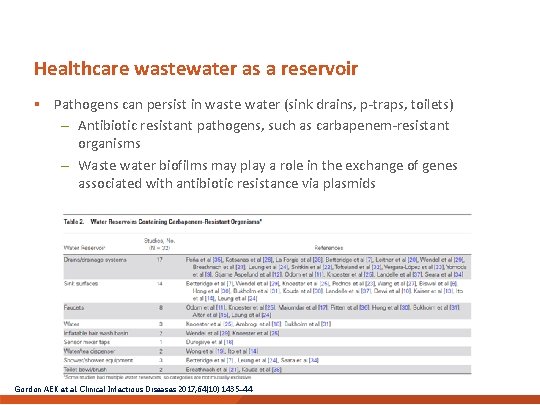
Healthcare wastewater as a reservoir § Pathogens can persist in waste water (sink drains, p-traps, toilets) – Antibiotic resistant pathogens, such as carbapenem-resistant organisms – Waste water biofilms may play a role in the exchange of genes associated with antibiotic resistance via plasmids Gordon AEK et al. Clinical Infectious Diseases 2017; 64(10): 1435– 44
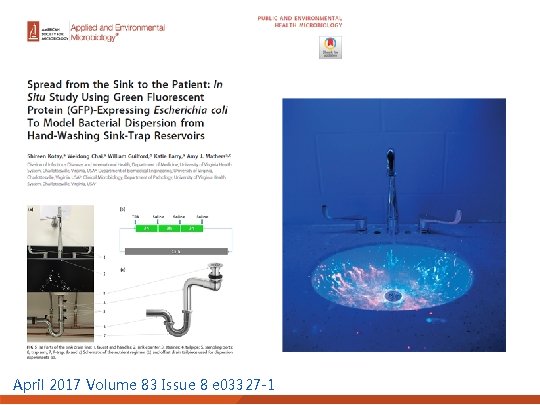
April 2017 Volume 83 Issue 8 e 03327 -1


From Plumbing to Patient: Prevention of water-related healthcare-associated infections Decrease potable water contamination Water management programs Decrease vector/device contamination Appropriate use, cleaning, disinfection Decrease patient exposure to contaminated water Considerations of host susceptibility

IMPROVING CLEANING PROCEDURES
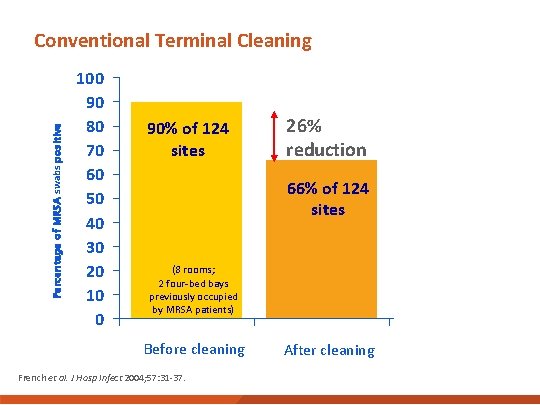
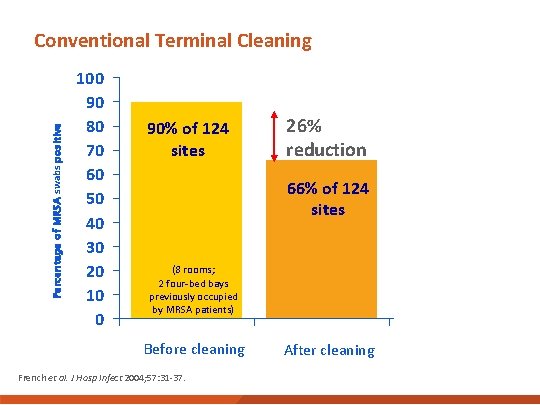
Percentage of MRSA swabs positive Conventional Terminal Cleaning 100 90 80 70 60 50 40 30 20 10 0 90% of 124 sites 26% reduction 66% of 124 sites (8 rooms; 2 four-bed bays previously occupied by MRSA patients) Before cleaning French et al. J Hosp Infect 2004; 57: 31 -37. After cleaning
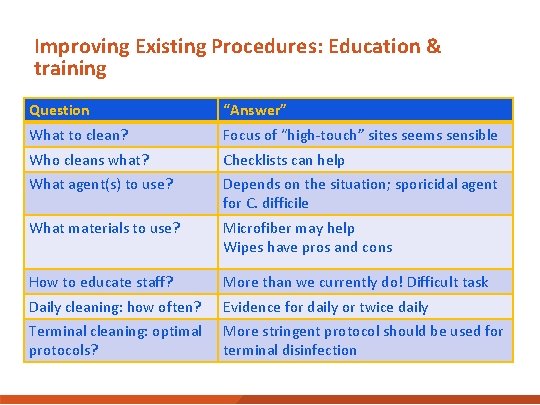
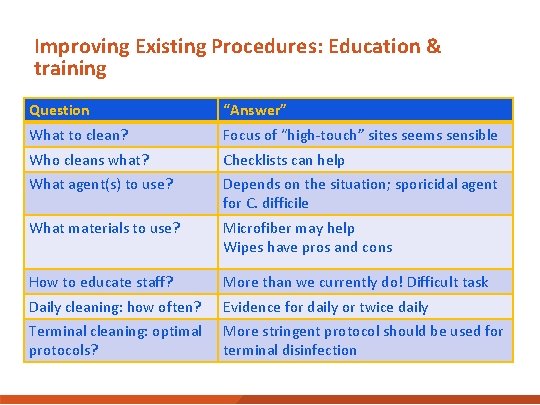
Improving Existing Procedures: Education & training Question “Answer” What to clean? Focus of “high-touch” sites seems sensible Who cleans what? Checklists can help What agent(s) to use? Depends on the situation; sporicidal agent for C. difficile What materials to use? Microfiber may help Wipes have pros and cons How to educate staff? More than we currently do! Difficult task Daily cleaning: how often? Evidence for daily or twice daily Terminal cleaning: optimal protocols? More stringent protocol should be used for terminal disinfection
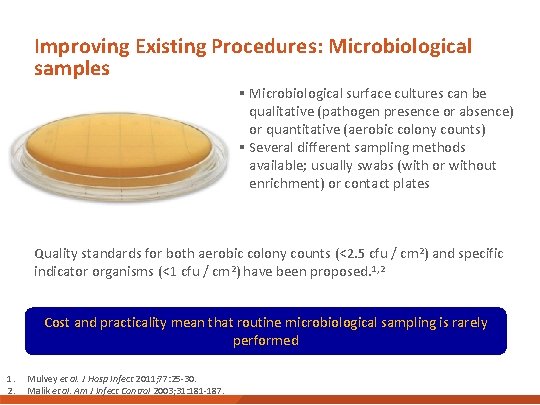
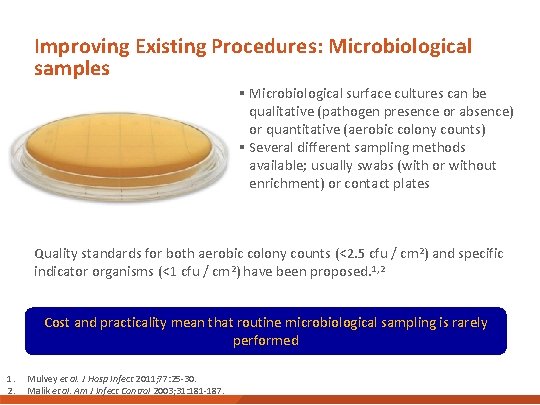
Improving Existing Procedures: Microbiological samples § Microbiological surface cultures can be qualitative (pathogen presence or absence) or quantitative (aerobic colony counts) § Several different sampling methods available; usually swabs (with or without enrichment) or contact plates § Quality standards for both aerobic colony counts (<2. 5 cfu / cm 2) and specific indicator organisms (<1 cfu / cm 2) have been proposed. 1, 2 Cost and practicality mean that routine microbiological sampling is rarely performed 1. 2. Mulvey et al. J Hosp Infect 2011; 77: 25 -30. Malik et al. Am J Infect Control 2003; 31: 181 -187.
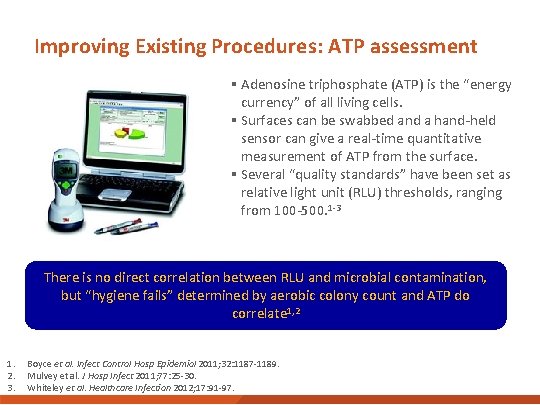
Improving Existing Procedures: ATP assessment § Adenosine triphosphate (ATP) is the “energy currency” of all living cells. § Surfaces can be swabbed and a hand-held sensor can give a real-time quantitative measurement of ATP from the surface. § Several “quality standards” have been set as relative light unit (RLU) thresholds, ranging from 100 -500. 1 -3 There is no direct correlation between RLU and microbial contamination, but “hygiene fails” determined by aerobic colony count and ATP do correlate 1, 2 1. 2. 3. Boyce et al. Infect Control Hosp Epidemiol 2011; 32: 1187 -1189. Mulvey et al. J Hosp Infect 2011; 77: 25 -30. Whiteley et al. Healthcare Infection 2012; 17: 91 -97.
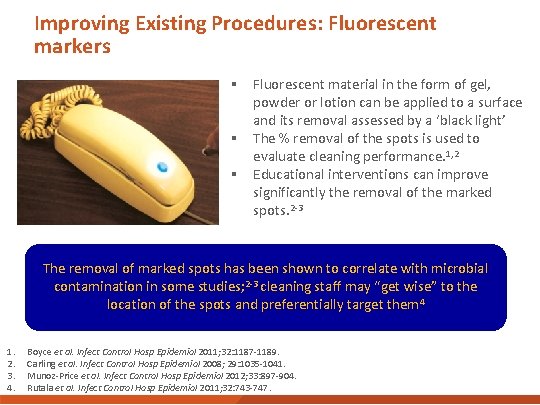
Improving Existing Procedures: Fluorescent markers § Fluorescent material in the form of gel, powder or lotion can be applied to a surface and its removal assessed by a ‘black light’ § The % removal of the spots is used to evaluate cleaning performance. 1, 2 § Educational interventions can improve significantly the removal of the marked spots. 2 -3 The removal of marked spots has been shown to correlate with microbial contamination in some studies; 2 -3 cleaning staff may “get wise” to the location of the spots and preferentially target them 4 1. 2. 3. 4. Boyce et al. Infect Control Hosp Epidemiol 2011; 32: 1187 -1189. Carling et al. Infect Control Hosp Epidemiol 2008; 29: 1035 -1041. Munoz-Price et al. Infect Control Hosp Epidemiol 2012; 33: 897 -904. Rutala et al. Infect Control Hosp Epidemiol 2011; 32: 743 -747.
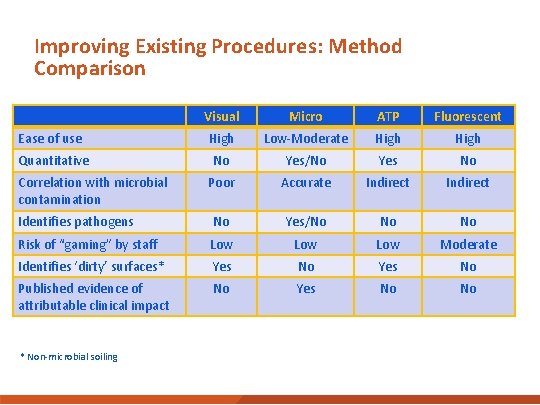
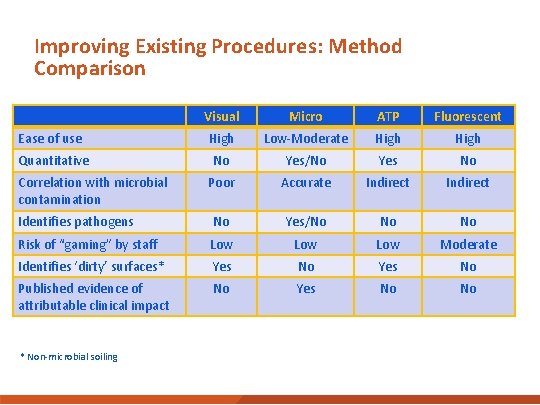
Improving Existing Procedures: Method Comparison Visual Micro ATP Fluorescent Ease of use High Low-Moderate High Quantitative No Yes/No Yes No Poor Accurate Indirect Identifies pathogens No Yes/No No No Risk of “gaming” by staff Low Low Moderate Identifies ‘dirty’ surfaces* Yes No Published evidence of attributable clinical impact No Yes No No Correlation with microbial contamination * Non-microbial soiling

New Approaches: “No Touch” Disinfection Hydrogen peroxide vapor (HPV) Otter et al. J Hosp Infect 2013; 83: 1 -13. Aerosolised hydrogen peroxide (a. HP) Ultraviolet radiation C (UVC) Pulsedxenon UV (PX-UV)
BRIDGING GAPS AND SUMMARY POINTS
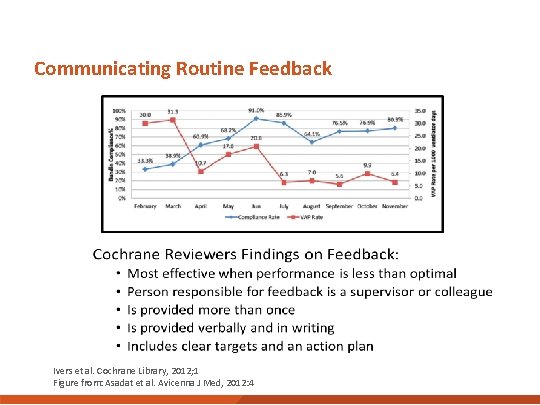
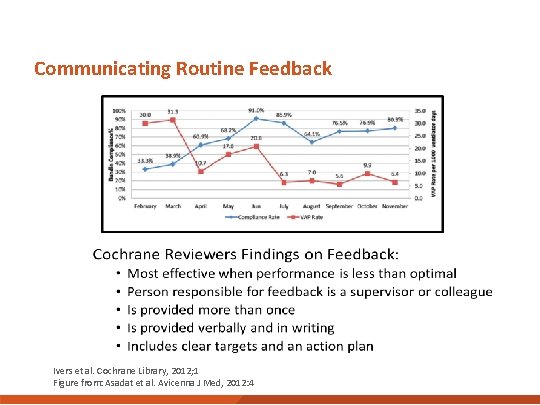
Communicating Routine Feedback Ivers et al. Cochrane Library, 2012; 1 Figure from: Asadat et al. Avicenna J Med, 2012: 4
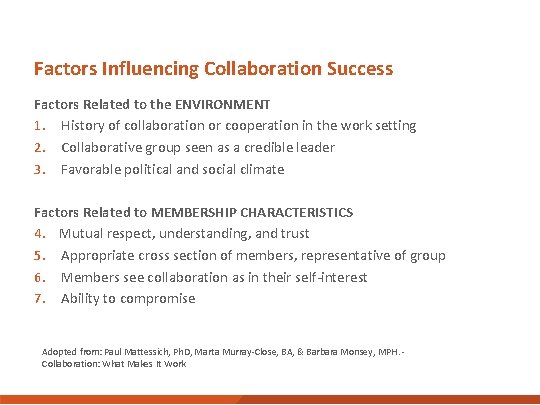
Factors Influencing Collaboration Success Factors Related to the ENVIRONMENT 1. History of collaboration or cooperation in the work setting 2. Collaborative group seen as a credible leader 3. Favorable political and social climate Factors Related to MEMBERSHIP CHARACTERISTICS 4. Mutual respect, understanding, and trust 5. Appropriate cross section of members, representative of group 6. Members see collaboration as in their self-interest 7. Ability to compromise Adopted from: Paul Mattessich, Ph. D, Marta Murray-Close, BA, & Barbara Monsey, MPH. - Collaboration: What Makes It Work
Summary: Strategies to Interrupt Transmission of Pathogens that Spread by Contact § § § Adherence to and monitoring of cleaning protocols Technologies to supplement manual cleaning Surfaces that are easy to clean Materials with antimicrobial properties for high touch surfaces Physical barriers such as single patient rooms Hand hygiene infrastructure: clearly visible sinks and gels in convenient and standardized locations
Summary: Strategies to Interrupt Transmission of Pathogens Related to Water § Decontamination of water sources – Chlorination, hyper-chlorination, superheat-and-flush, copper-silver ionization, and UV § Design elements – Selection of faucets, sinks, aerators – POC filters (cost-risk balance) – Decorative; avoid open fountain systems § Safe plumbing practices – Eliminate dead legs – Temperature and pressure
Ongoing Collaborative Activities § FGI 2022 § CDC and ASHE best practices about using the health care physical environment to prevent and control infections § HICPAC § Water management
Questions § Who is in your facility is consulted in major design or redesign decisions? And when are they consulted? § What barriers do you encounter regarding design and IPC considerations? § Are human factors considered? If so, how?
Acknowledgements § Jesse Jacob, MD – Emory University School of Medicine / Emory Midtown Hospital § Jon Otter, Ph. D – Imperial College – Healthcare NHS Trust § Rachael Jones, Ph. D, MPH, CIH – University of Illinois Chicago School of Public Health § Sujan Reddy, MD – Centers for Disease Control and Prevention, Division of Healthcare Quality and Promotion
Thank you! For more information, contact CDC 1 -800 -CDC-INFO (232 -4636) TTY: 1 -888 -232 -6348 www. cdc. gov The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.

EXTRA SLIDES
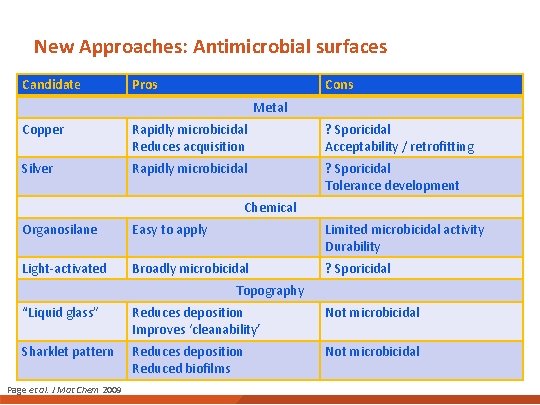
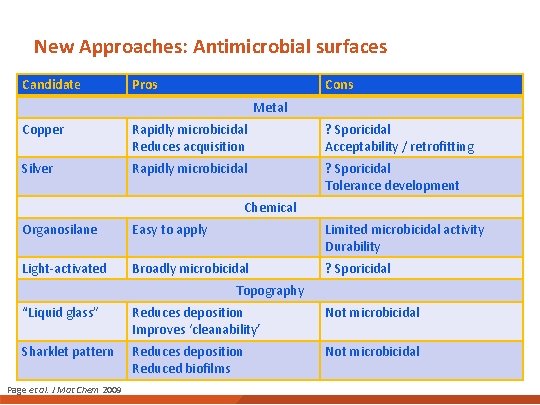
New Approaches: Antimicrobial surfaces Candidate Pros Cons Metal Copper Rapidly microbicidal Reduces acquisition ? Sporicidal Acceptability / retrofitting Silver Rapidly microbicidal ? Sporicidal Tolerance development Chemical Organosilane Easy to apply Limited microbicidal activity Durability Light-activated Broadly microbicidal ? Sporicidal Topography “Liquid glass” Reduces deposition Improves ‘cleanability’ Not microbicidal Sharklet pattern Reduces deposition Reduced biofilms Not microbicidal Page et al. J Mat Chem 2009
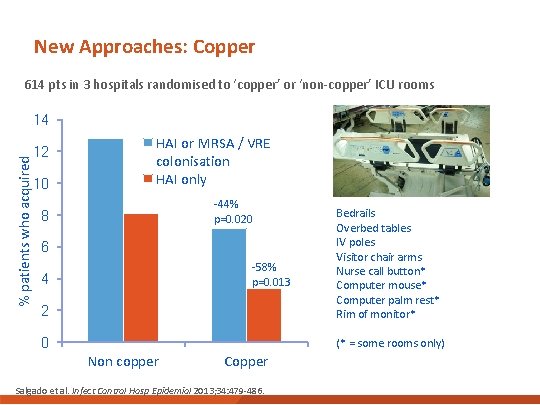
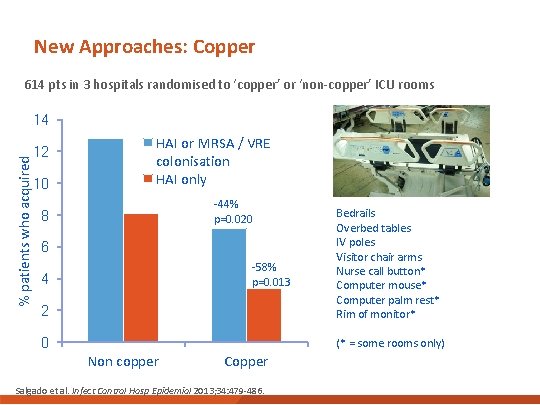
New Approaches: Copper 614 pts in 3 hospitals randomised to ‘copper’ or ‘non-copper’ ICU rooms % patients who acquired 14 12 10 HAI or MRSA / VRE colonisation HAI only -44% p=0. 020 2 Bedrails Overbed tables IV poles Visitor chair arms Nurse call button* Computer mouse* Computer palm rest* Rim of monitor* 0 (* = some rooms only) 8 6 -58% p=0. 013 4 Non copper Copper Salgado et al. Infect Control Hosp Epidemiol 2013; 34: 479 -486.