National AIDS Control Programme 1 National AIDS Control

- Slides: 20
National AIDS Control Programme 1

National AIDS Control Programme (NACP) launched under Ministry of Health & Family Welfare in 1992 NACP I (1992 – 1999) NACP II (1999 – 2006) NACP III (2007 – 2012) 2
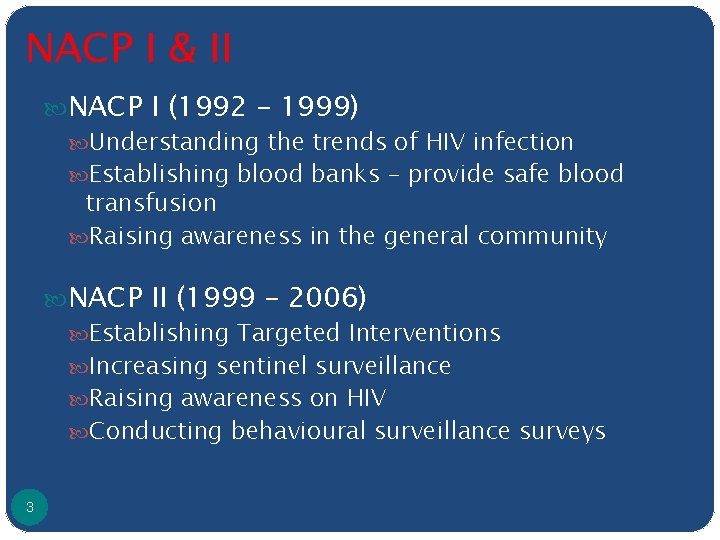
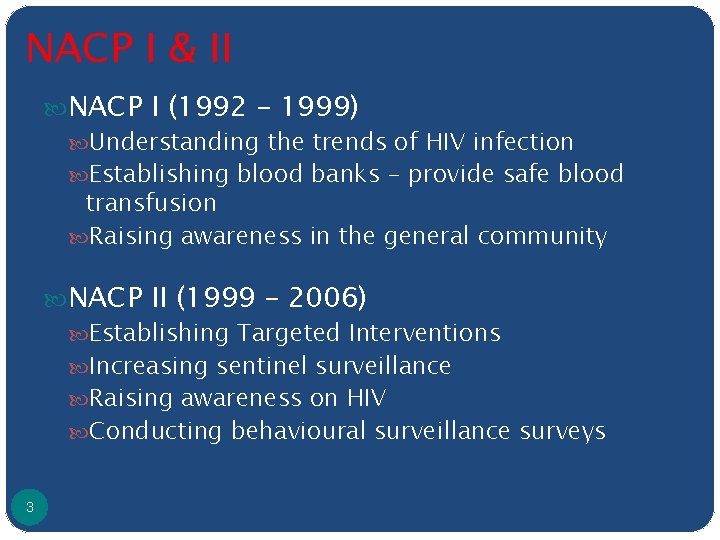
NACP I & II NACP I (1992 – 1999) Understanding the trends of HIV infection Establishing blood banks – provide safe blood transfusion Raising awareness in the general community NACP II (1999 – 2006) Establishing Targeted Interventions Increasing sentinel surveillance Raising awareness on HIV Conducting behavioural surveillance surveys 3
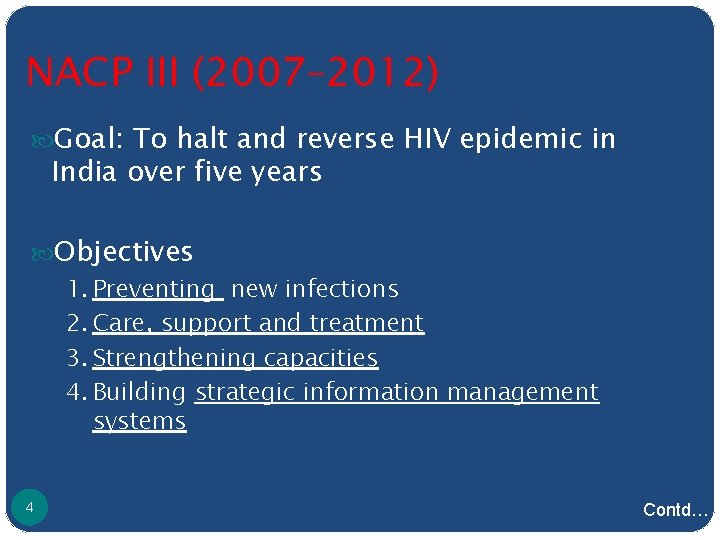
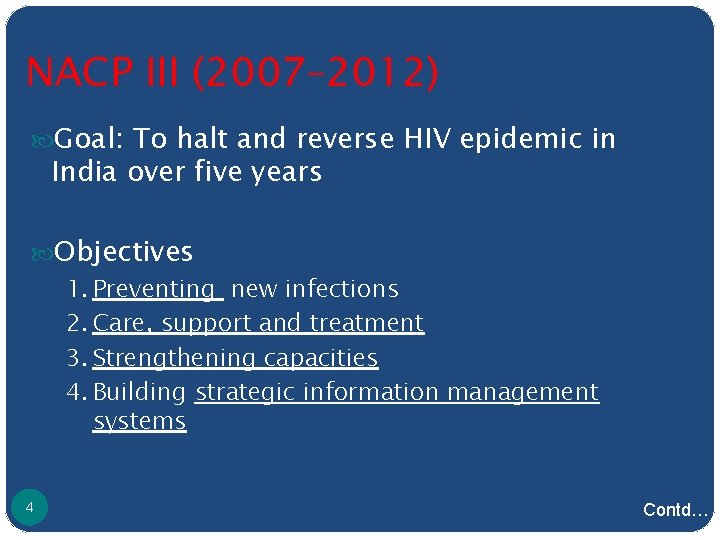
NACP III (2007– 2012) Goal: To halt and reverse HIV epidemic in India over five years Objectives 1. Preventing new infections 2. Care, support and treatment 3. Strengthening capacities 4. Building strategic information management systems 4 Contd…
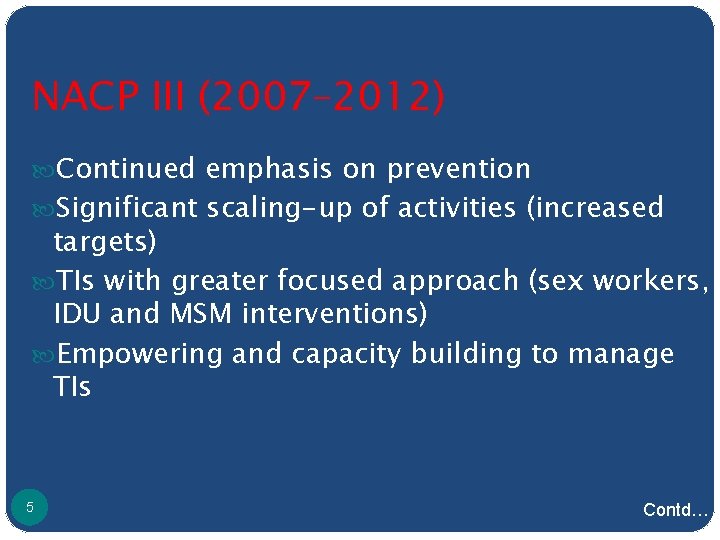
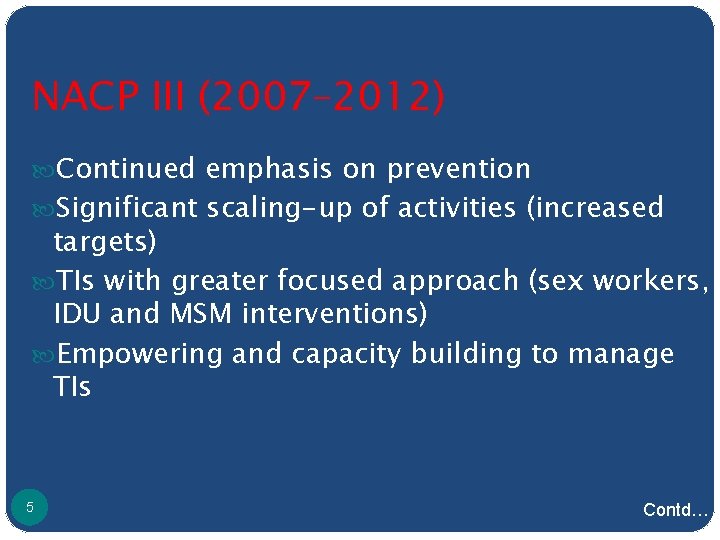
NACP III (2007– 2012) Continued emphasis on prevention Significant scaling-up of activities (increased targets) TIs with greater focused approach (sex workers, IDU and MSM interventions) Empowering and capacity building to manage TIs 5 Contd…
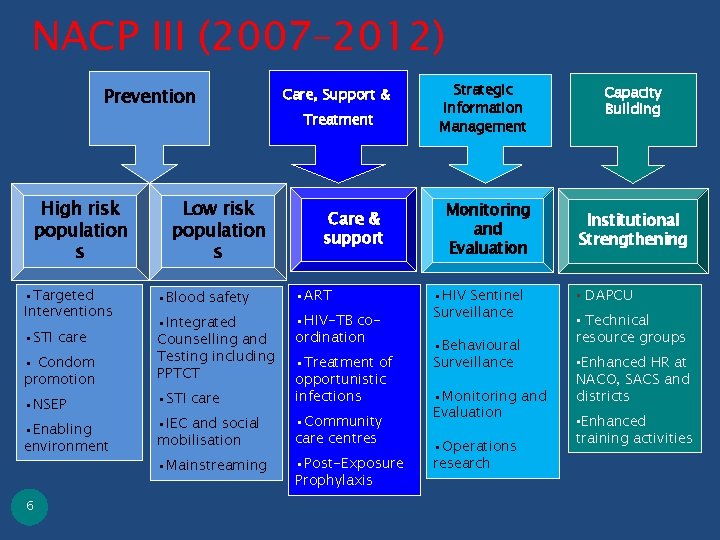
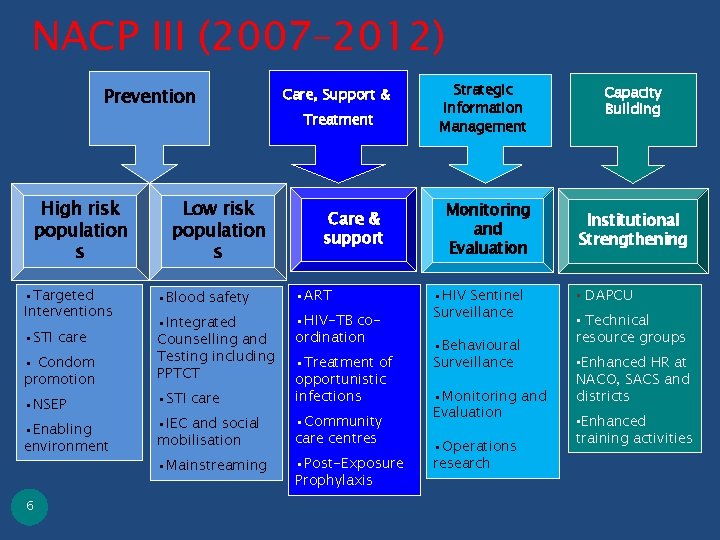
NACP III (2007– 2012) Prevention High risk population s • Targeted Interventions • STI care • Condom promotion • NSEP • Enabling environment 6 Low risk population s Care, Support & Treatment Care & support • Blood safety • ART • Integrated Counselling and Testing including PPTCT • HIV-TB coordination • STI care • Treatment of opportunistic infections • IEC and social mobilisation • Community care centres • Mainstreaming • Post-Exposure Prophylaxis Strategic Information Management Monitoring and Evaluation • HIV Sentinel Surveillance • Behavioural Surveillance • Monitoring and Evaluation • Operations research Capacity Building Institutional Strengthening • DAPCU • Technical resource groups • Enhanced HR at NACO, SACS and districts • Enhanced training activities
TARGETED INTERVENTIONS 7
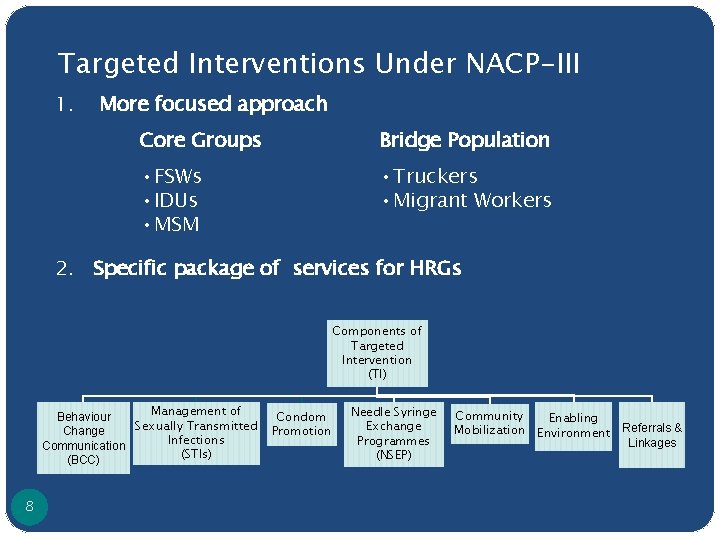
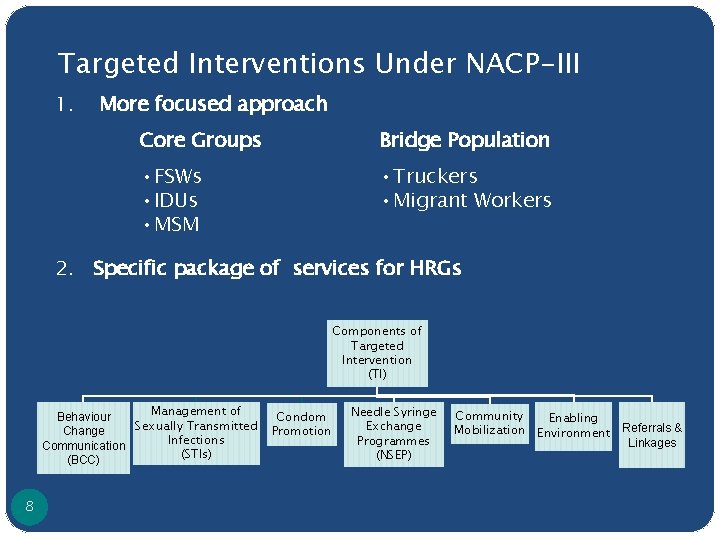
Targeted Interventions Under NACP-III 1. More focused approach Core Groups Bridge Population • FSWs • IDUs • MSM • Truckers • Migrant Workers 2. Specific package of services for HRGs Components of Targeted Intervention (TI) Management of Behaviour Sexually Transmitted Change Infections Communication (STIs) (BCC) 8 Condom Promotion Needle Syringe Exchange Programmes (NSEP) Community Enabling Mobilization Environment Referrals & Linkages
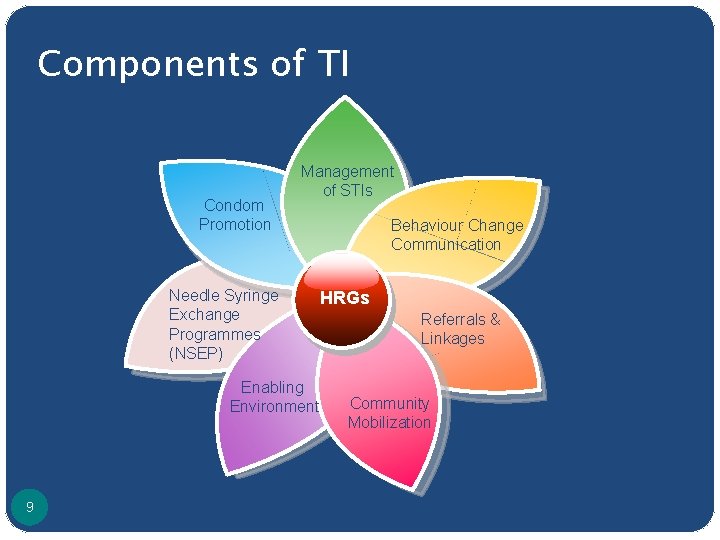
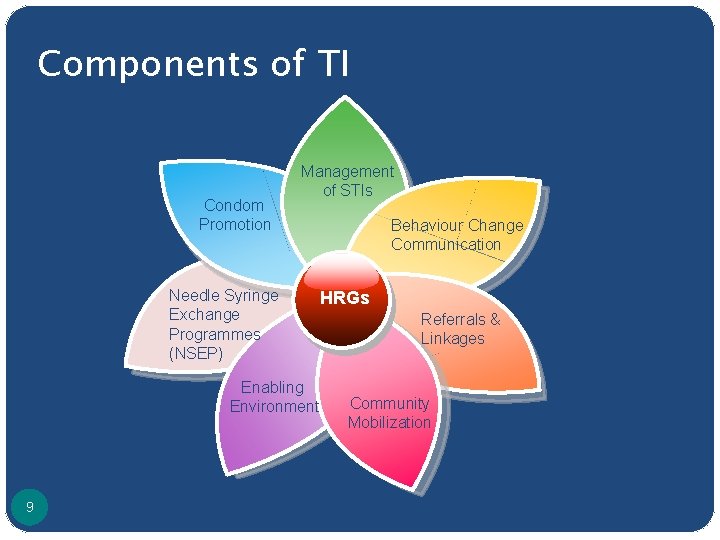
Components of TI Condom Promotion Management of STIs Needle Syringe Exchange Programmes (NSEP) Enabling Environment 9 Behaviour Change Communication HRGs Referrals & Linkages Community Mobilization
TARGETED INTERVENTIONS FOR IDUs 10
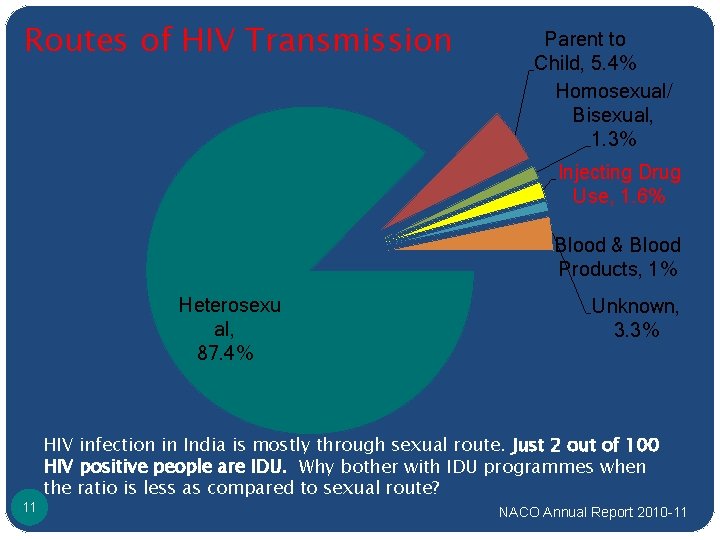
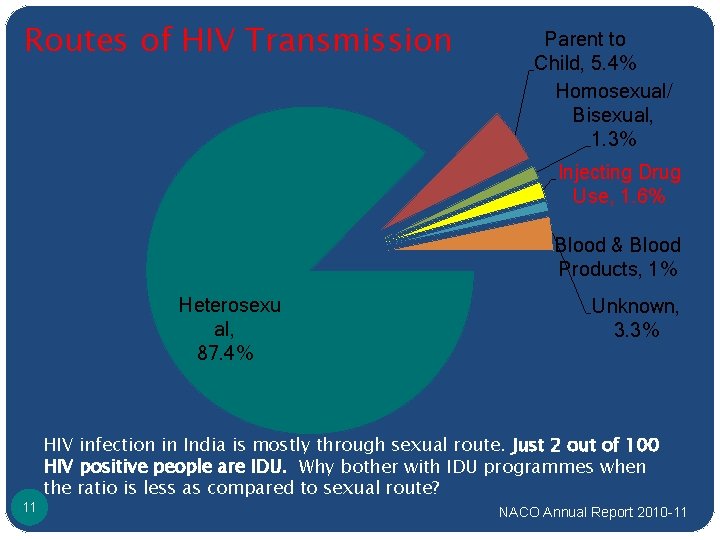
Routes of HIV Transmission Parent to Child, 5. 4% Homosexual/ Bisexual, 1. 3% Injecting Drug Use, 1. 6% Blood & Blood Products, 1% Heterosexu al, 87. 4% 11 Unknown, 3. 3% HIV infection in India is mostly through sexual route. Just 2 out of 100 HIV positive people are IDU. Why bother with IDU programmes when the ratio is less as compared to sexual route? NACO Annual Report 2010 -11
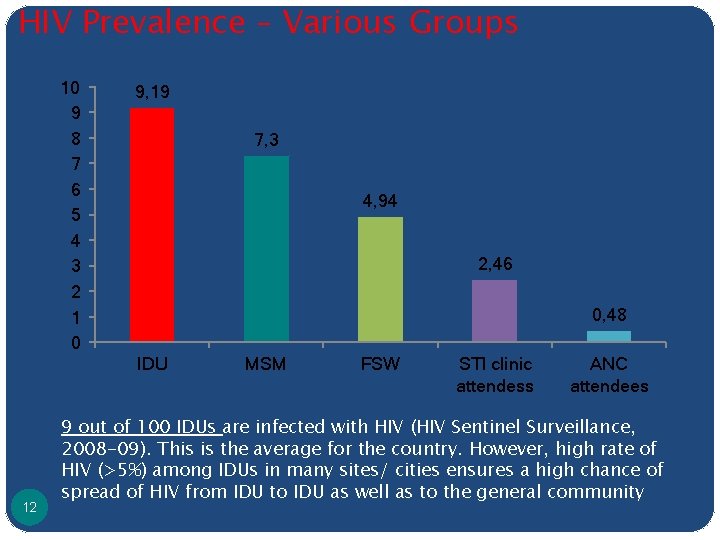
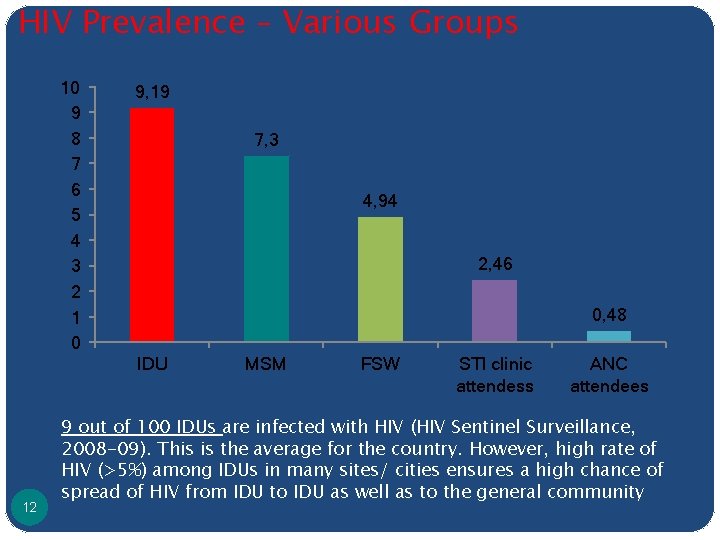
HIV Prevalence – Various Groups 10 9 8 7 6 5 4 3 2 1 0 9, 19 7, 3 4, 94 2, 46 0, 48 IDU 12 MSM FSW STI clinic attendess ANC attendees 9 out of 100 IDUs are infected with HIV (HIV Sentinel Surveillance, 2008 -09). This is the average for the country. However, high rate of HIV (>5%) among IDUs in many sites/ cities ensures a high chance of spread of HIV from IDU to IDU as well as to the general community
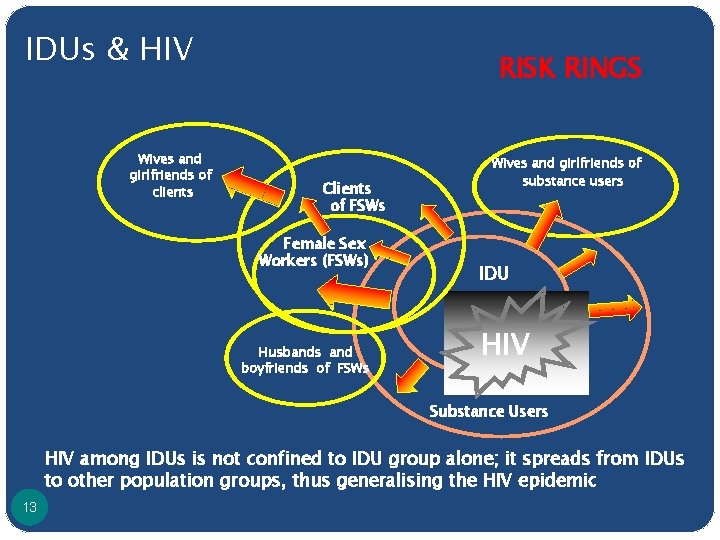
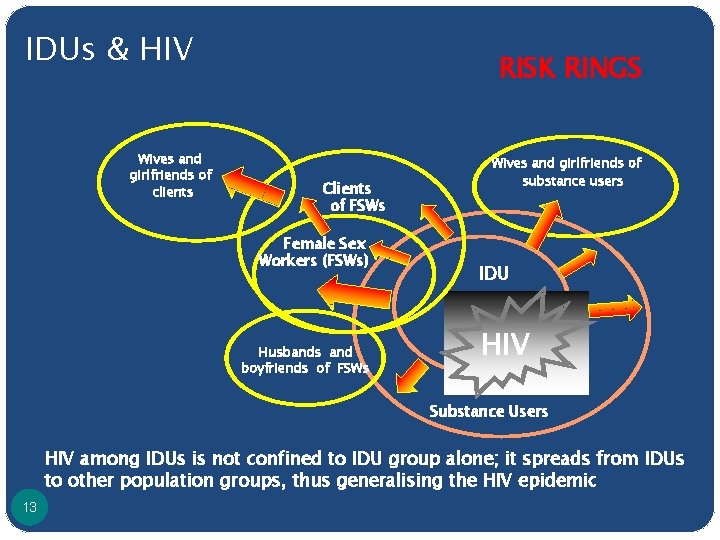
IDUs & HIV Wives and girlfriends of clients RISK RINGS Clients of FSWs Female Sex Workers (FSWs) Wives and girlfriends of substance users IDUs Husbands and boyfriends of FSWs HIV Substance Users HIV among IDUs is not confined to IDU group alone; it spreads from IDUs to other population groups, thus generalising the HIV epidemic 13
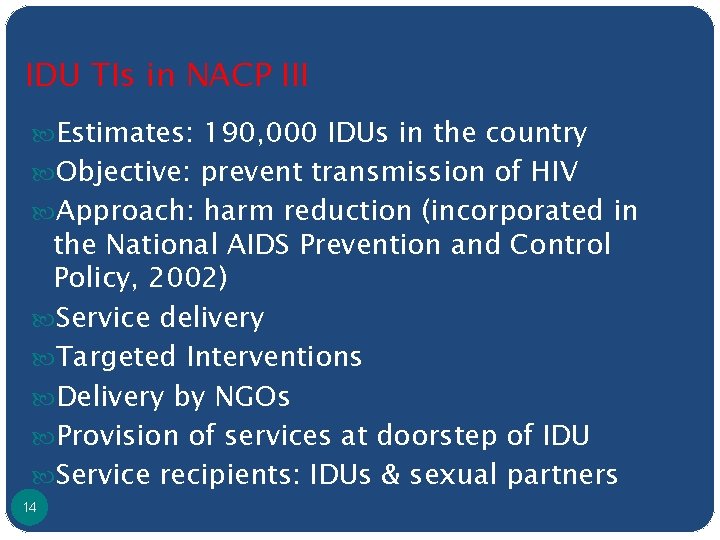
IDU TIs in NACP III Estimates: 190, 000 IDUs in the country Objective: prevent transmission of HIV Approach: harm reduction (incorporated in the National AIDS Prevention and Control Policy, 2002) Service delivery Targeted Interventions Delivery by NGOs Provision of services at doorstep of IDU Service recipients: IDUs & sexual partners 14
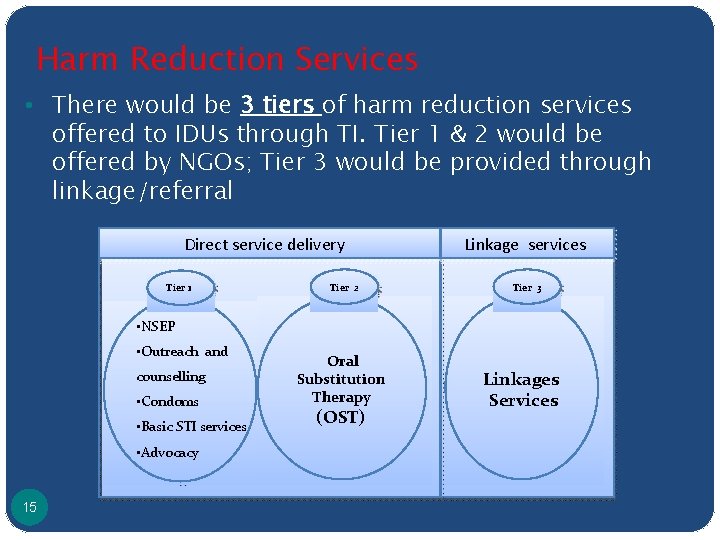
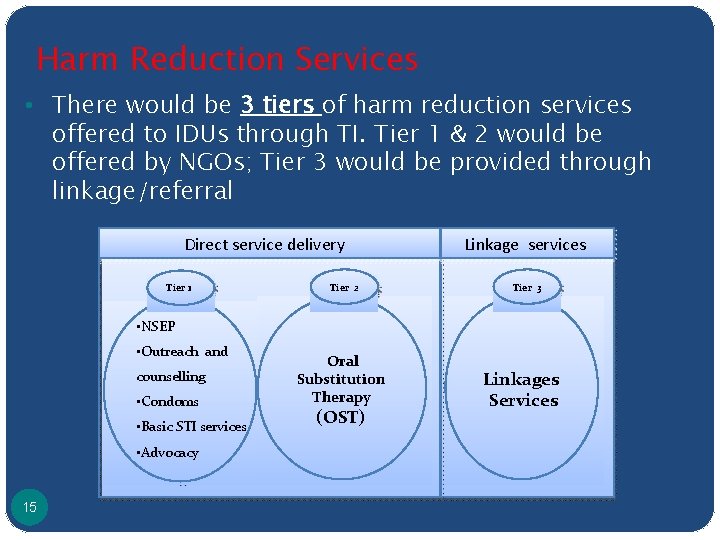
Harm Reduction Services • There would be 3 tiers of harm reduction services offered to IDUs through TI. Tier 1 & 2 would be offered by NGOs; Tier 3 would be provided through linkage/referral Direct service delivery Tier 1 Tier 2 Linkage services Tier 3 • NSEP • Outreach and counselling • Condoms • Basic STI services • Advocacy 15 Oral Substitution Therapy (OST) Linkages Services
Tier 1: Outreach Activity Ø Delivered through ORW and PE Ø Services Needle Syringe Exchange Programmes (NSEP) Condoms - free distribution & social marketing Primary health care, STI and abscess management Behaviour Change Communication (BCC) Advocacy 16
Tier 2: Opioid Substitution Treatment Delivery by NACO accredited agencies Substitution agents: Buprenorphine, Methadone Initiated by a trained physician and administered by trained personnel Psychosocial services Follow-up by PM and ORW/PE Provision/link to Tier 1 Services Strict record maintenance 17
Tier 3: Linkage Services Linkages ICTC (voluntary informed consent) ART, DOTS, RCH Accompanied referrals by ORW/ PE Established referral networks with medical, legal and welfare schemes Linkage with detoxification and rehabilitation centres 18
Enabling Environment ‘To create a milieu where IDUs are able to access services freely without interference’ Advocacy with Law enforcement agencies Community leaders Health workers General population 19
Thank you! 20