NASOGASTRIC TUBES INSERTION MANAGEMENT FEEDING Decision Making Consent
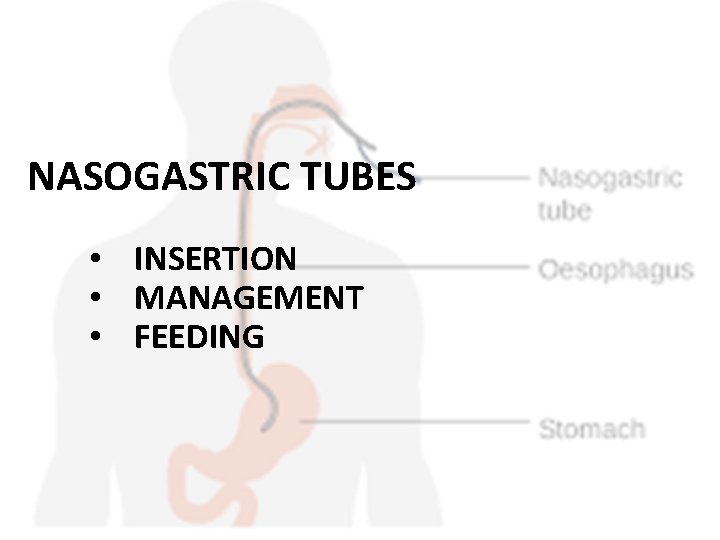
NASOGASTRIC TUBES • INSERTION • MANAGEMENT • FEEDING
Decision Making & Consent • Ensure MDT have discussed, agreed and documented that NG/OG tube placement is required and in the patients best interest. • The purpose of the procedure & associated risks should be discussed with the patient. • Where the patient has capacity their agreement should be obtained & documented. • Where patients lack capacity a ‘best interest’ decision may be required.
Risks associated with NG/OG tube insertion? • • Misplacement to lung Aspiration Bleeding secondary to trauma Pain/Discomfort during & after insertion Mucosal erosion Pneumothorax Oesophageal Perforation
Risks associated with enteral feeding? • Bowel disturbances (Diarrhoea, constipation)dieticians would dispute! • Fluid/electrolyte imbalance – Refeeding complications • • Hypoglycaemia/Hyperglyceamia Vomiting Allergies Aspiration
Indications for NG/OG tube insertion? • Enteral feeding • Enteral medication • Gastric drainage
Contra-Indications for NG/OG tube insertion?
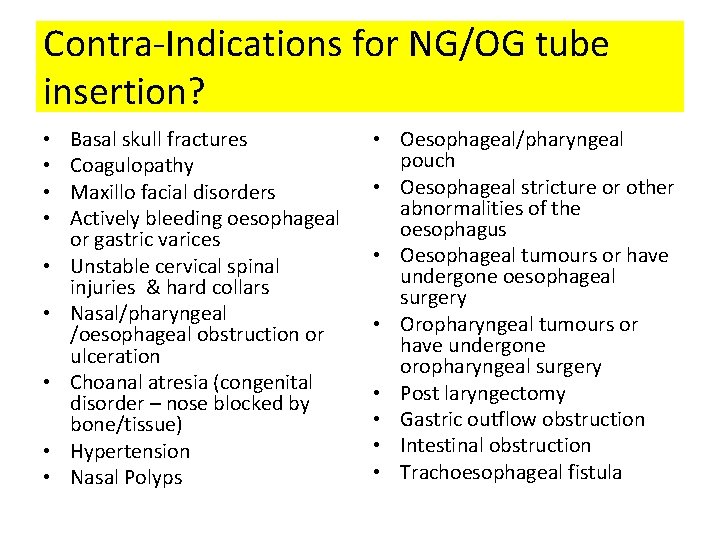
Contra-Indications for NG/OG tube insertion? • • • Basal skull fractures Coagulopathy Maxillo facial disorders Actively bleeding oesophageal or gastric varices Unstable cervical spinal injuries & hard collars Nasal/pharyngeal /oesophageal obstruction or ulceration Choanal atresia (congenital disorder – nose blocked by bone/tissue) Hypertension Nasal Polyps • Oesophageal/pharyngeal pouch • Oesophageal stricture or other abnormalities of the oesophagus • Oesophageal tumours or have undergone oesophageal surgery • Oropharyngeal tumours or have undergone oropharyngeal surgery • Post laryngectomy • Gastric outflow obstruction • Intestinal obstruction • Trachoesophageal fistula

Feeding Tube Specifications • CE accredited • Radiopaque along the length of the tube • Externally visible centimetre markings along the length of the tube • Appropriate length for the purpose of the tube (92 cm standard length for adults) • ENFit connector • Polyurethane material • Appropriate lumen size for purpose (12 and 14 Fr tubes are recommended)

Types of tubes: Wide Bore Decompression Tube • Intended use = Drainage & decompression of abdomen • Short Dwell Time - only licensed for 7 days • Entral tubes are available in 8 fr, 10 fr, 12 fr, 14 fr, 16 fr, 18 fr, 20 fr. • Meets spec on previous slide but far from ideal for feeding • Circumstances in which these tubes may be used for feeding: – Risk of intermittent ileus where drainage may be needed – Critical care Environments where drainage & frequent aspiration needed – Risk of poor absorption of feed
Types of tubes: ‘Corflo Tube’ • Intended use = Feeding • Polyurethane • Dwell Time = as long as functional • No longer need to store in fridge to stiffen before insertion – already ‘stiff enough’!
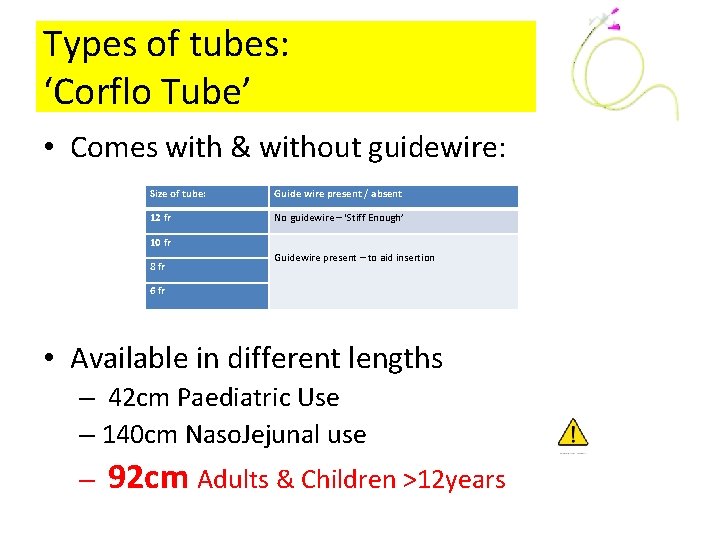
Types of tubes: ‘Corflo Tube’ • Comes with & without guidewire: Size of tube: Guide wire present / absent 12 fr No guidewire – ‘Stiff Enough’ 10 fr 8 fr Guidewire present – to aid insertion 6 fr • Available in different lengths – 42 cm Paediatric Use – 140 cm Naso. Jejunal use – 92 cm Adults & Children >12 years

Types of tubes: ‘Cor. Trak Tube’
Egg Sucking Warning
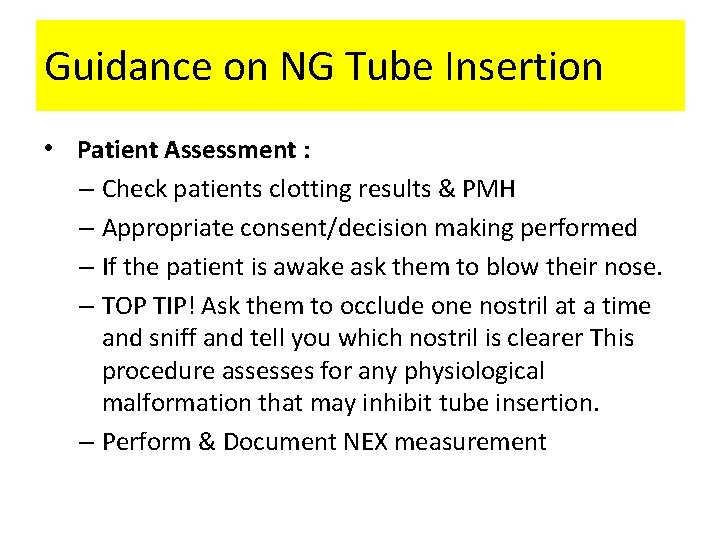
Guidance on NG Tube Insertion • Patient Assessment : – Check patients clotting results & PMH – Appropriate consent/decision making performed – If the patient is awake ask them to blow their nose. – TOP TIP! Ask them to occlude one nostril at a time and sniff and tell you which nostril is clearer This procedure assesses for any physiological malformation that may inhibit tube insertion. – Perform & Document NEX measurement

NEX measurement: • Nose • Ear • Xiphisternum § “XEN + 10”? ? (Taylor et al 2014 Nasogastric Tube depth: the ‘NEX’ guideline is incorrect British Journal of Nursing 23(12)
Guidance on NG Tube Insertion • Equipment Preparation: – Gather equipment …. – Ensure any guide wire present moves freely, but is locked firmly in to place for insertion and placement checks – Activate tube lubricant by dipping the tip of tube into water if using Corflo – DO NOT FLUSH THE INNER LUMEN OF THE TUBE WITH WATER BEFORE THE ph TEST HAS BEEN CARRIED OUT – LUBRICANT IN THE TUBES (ACTIVATED BY WATER) MAY CAUSE A FALSELY LOW READING (NPSA 2012)
Guidance on NG Tube Insertion • Patient Preparation (Awake): – Agree that the patient should swallow as they feel the tube passing the pharynx or on your command. (Give them a glass of water to use during the procedure) – Agree a signal to indicate that they are distressed & wish to stop. – Position patient sitting upright with head well supported by pillows if possible and advise them to adopt ‘chin tuck’ position • Patient Preparation (Ventilated): – Position patient sitting upright with head well supported by pillows if possible – Perform ‘chin tuck’ to aid insertion – Ensure airway safely positioned
Guidance on NG Tube Insertion • Tube Insertion: • Insert the tube into the nostril aiming towards the back of the nose & along nasopharynx. • Ensure the head is not hyperextended (increases the risk of tracheal intubation) • When you feel resistance against the tube – Ask the patient to swallow water if it they have a safe swallow – Ask the patient to do a ‘dry swallow’ if they have an unsafe swallow – Consider further ‘chin tuck’ on patients with ETT or tracheostomy.
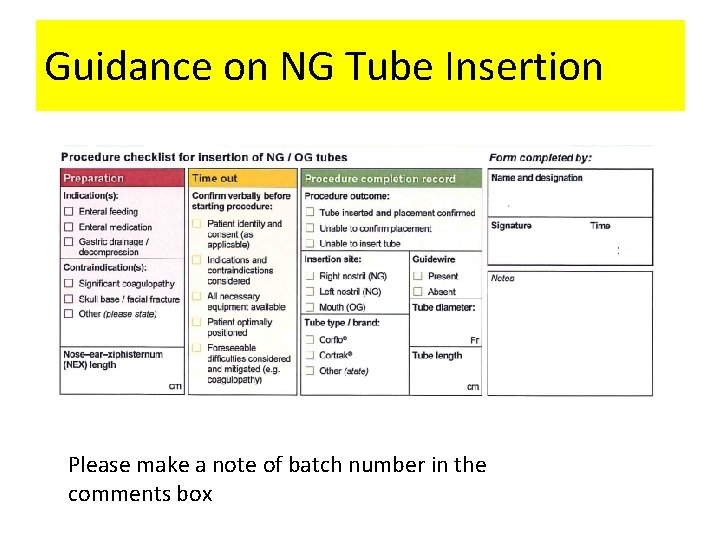
Guidance on NG Tube Insertion Please make a note of batch number in the comments box
When to STOP! • During advancement of the NG tube: • If the patient cough STOP and pull the tube back a little – check for coiling in the back of the mouth • STOP if any resistance is met and pull the tube back • It may be necessary to STOP the procedure in following circumstances: – Patient distress – Resp/CVS deterioration – Bleeding
When to STOP! A maximum of three attempts should be made, senior specialist advice should be sought if unsuccessful
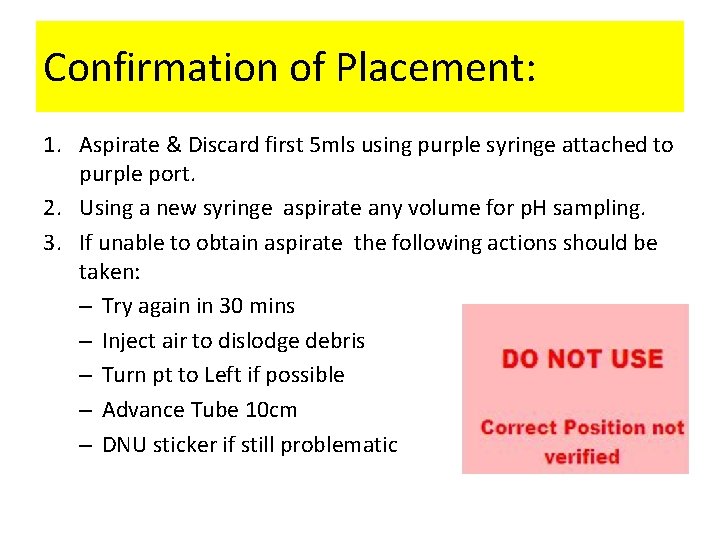
Confirmation of Placement: 1. Aspirate & Discard first 5 mls using purple syringe attached to purple port. 2. Using a new syringe aspirate any volume for p. H sampling. 3. If unable to obtain aspirate the following actions should be taken: – Try again in 30 mins – Inject air to dislodge debris – Turn pt to Left if possible – Advance Tube 10 cm – DNU sticker if still problematic
p. H checking: • 2 competent nurses to check independently on separate p. H strips Take before PPI/H 2 blocker if possible Hold stick upside down – dripping down/off Read at 10 -40 secs p. H should be less than/equal to 5. 5 on basis of NPSA guidance – Nurse 1 to record on Flow Chart – Nurse 2 to document in notes – Both nurses need to agree – if disagreement – – • proceed to CXR • Apply DNU sticker
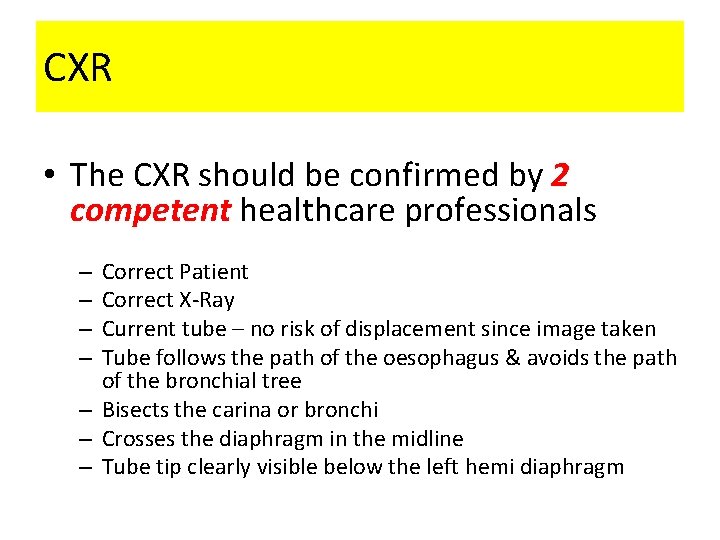
CXR • The CXR should be confirmed by 2 competent healthcare professionals Correct Patient Correct X-Ray Current tube – no risk of displacement since image taken Tube follows the path of the oesophagus & avoids the path of the bronchial tree – Bisects the carina or bronchi – Crosses the diaphragm in the midline – Tube tip clearly visible below the left hemi diaphragm – –
DO: • Record all p. H tests on trust documentation & in notes • Place a ‘Do Not Use’ sticker on tubes that are awaiting X-Ray Confirmation or any NG tube that is not used for continuous feeding • Remove any tubes that have been identified as misplaced immediately
DO NOT: • Use ‘whoosh’ or bubble test • Use Litmus paper to confirm placement • Use Cortrak to confirm placement • Interpret absence of respiratory distress or appearance of aspirate as indicator of correct positioning • Flush tubes until placement has been confirmed • Place NG/OG tubes or start feed out of hours unless needed for admin of critical meds • Re-insert guidewire to Corflo tube
Please be aware: • Tubes can enter the respiratory tract without causing symptoms. • The upper airway reflexes respond to the sensation of fluid at the back of the throat causing choking +/- coughing. • If liquid is introduced to the lung via misplaced NG Tube these reflexes have already been bypassed. Even awake patients may not display symptoms for a number of hour 2.

Daily Review • Patients should have daily p. H recorded
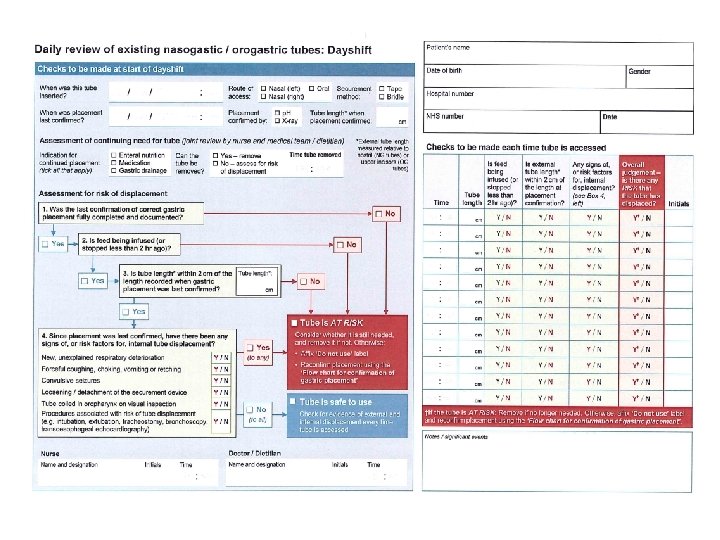
What if the tube has moved? ? • If the tube has moved by greater than 2 cm – – Reconfirm tube position • If the tube has moved by greater than 5 cm – – Remove tube

Quick Quiz! • Where should MDT decision making be documented? • What kind of tubes do we have in the trust? • What is the maximum number of attempts before senior help is sought? • Should Corflo tubes be stored in the fridge? • What methods can confirm tube position? • What methods do not confirm tube position?
- Slides: 32