NASAL HIGH FLOW OXYGEN THERAPY Mairi Mascarenhas Clinical
- Slides: 25
NASAL HIGH FLOW OXYGEN THERAPY Mairi Mascarenhas Clinical Educator ICU
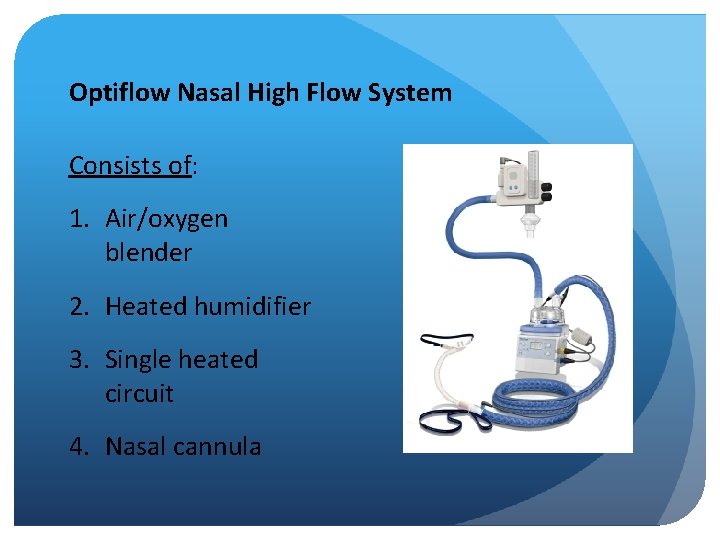
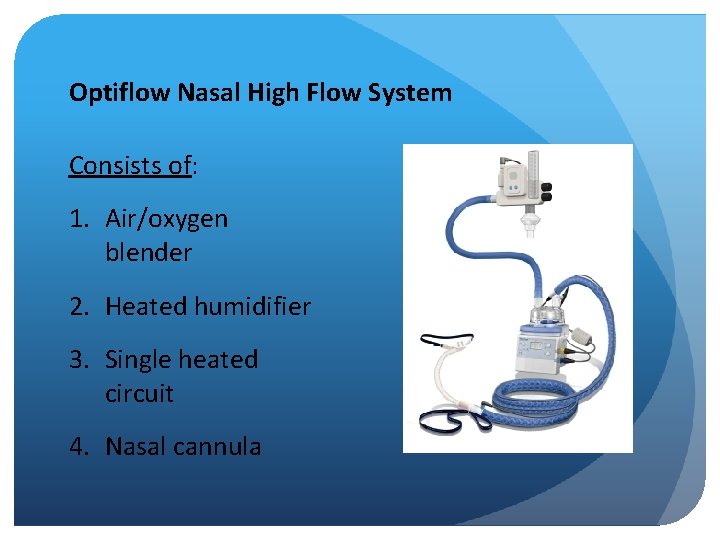
Optiflow Nasal High Flow System Consists of: 1. Air/oxygen blender 2. Heated humidifier 3. Single heated circuit 4. Nasal cannula
Background: Nasal High Flow (NHF) enables high flow blended oxygen to be delivered through its unique nasal cannula. Can deliver flow up to 60 litres. Allows comfortable, effective delivery of up to 100% oxygen. Creates an ideal solution for the hypoxemic patient in mild to moderate respiratory distress.
Benefits to patient comfort: Provides improved comfort compared to conventional oxygen delivery devices. Reduced skin breakdown when compared to NIV. Patient is able to eat, drink, talk, sleep Prevention of invasive ventilation Prevention of post-extubation respiratory failure and re-intubation
Contraindications: Contraindications or complications are rare in adults Abnormalities or surgery of the face, nose or airway that preclude an appropriate-fitting nasal cannula. Some experts avoid NHF in those following upper airway surgery to avoid theoretical risk that the high pressure may precipitate a venous thromboembolism Check with Consultant responsible for the patient’s care. Document consultant’s decision.
Complications: Complications are rare in adults. Complications include abdominal distension, aspiration and, rarely, barotrauma e. g. pneumothorax.
Limitations of traditional oxygen therapies: Limited in scope and can compromise patient comfort. Conventional low flow nasal cannulae & oxygen masks constrained by flow, humidity & accuracy of inspired oxygen. As patient’s respiratory status changes, the clinician will respond by changing oxygen therapies to balance oxygenation with patient comfort and compliance. This often results in the application of multiple oxygen therapy systems (low flow nasal cannulae, venturi masks, non-rebreather masks etc).
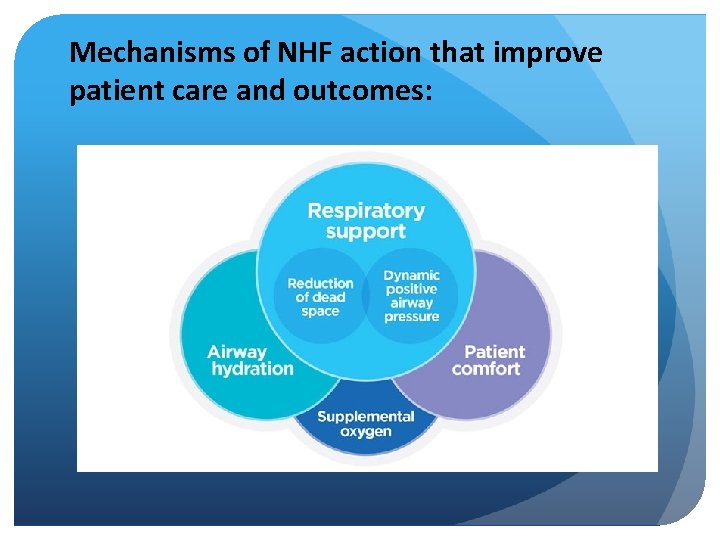
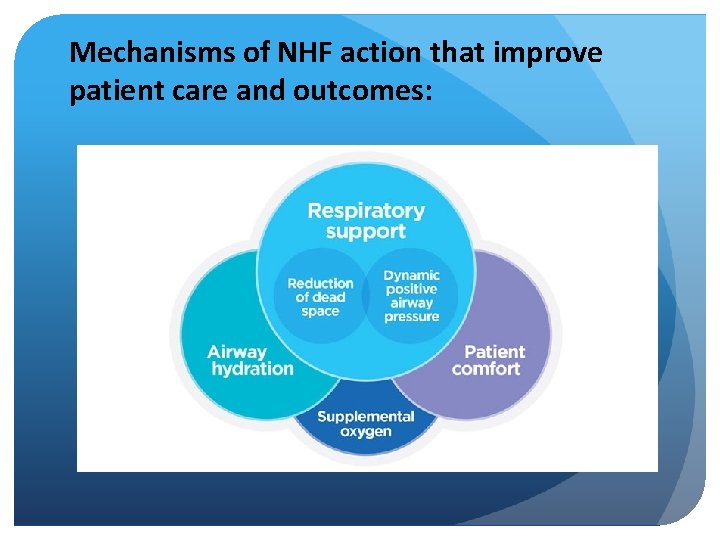
Mechanisms of NHF action that improve patient care and outcomes:
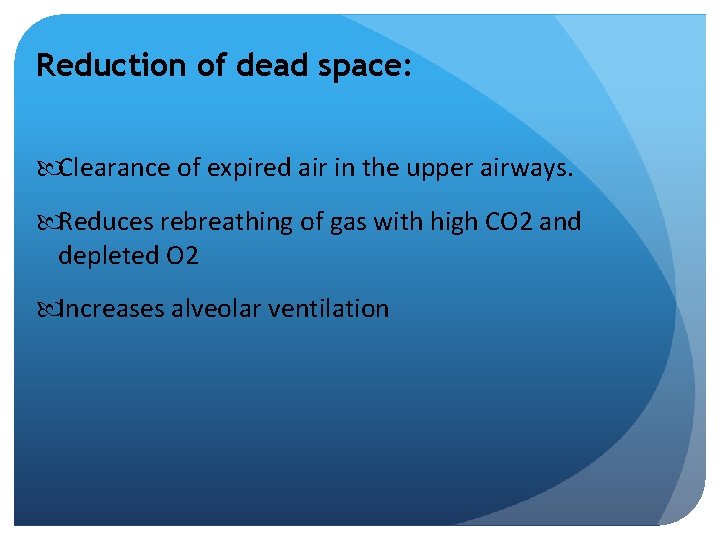
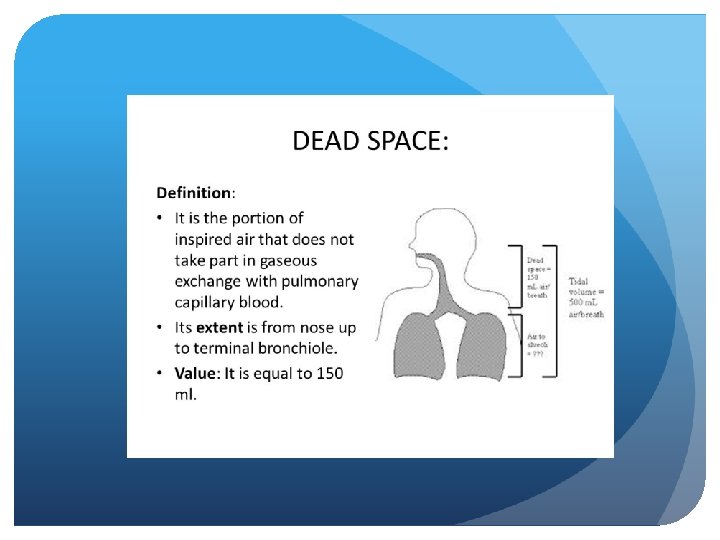
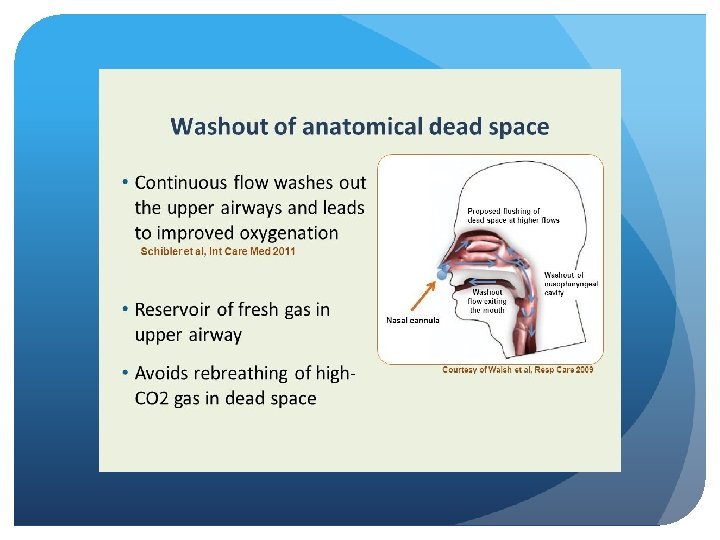
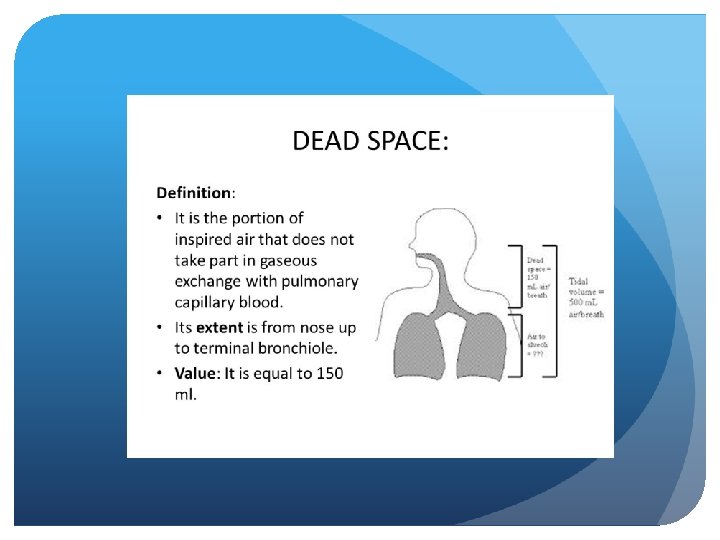
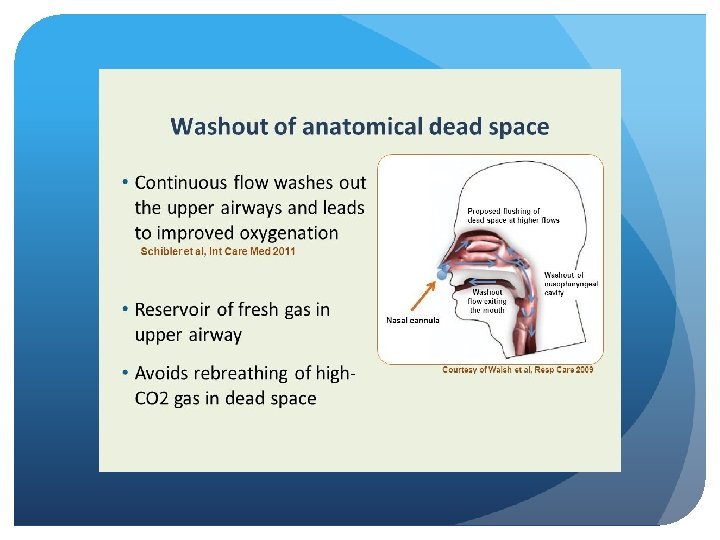
Reduction of dead space: Clearance of expired air in the upper airways. Reduces rebreathing of gas with high CO 2 and depleted O 2 Increases alveolar ventilation
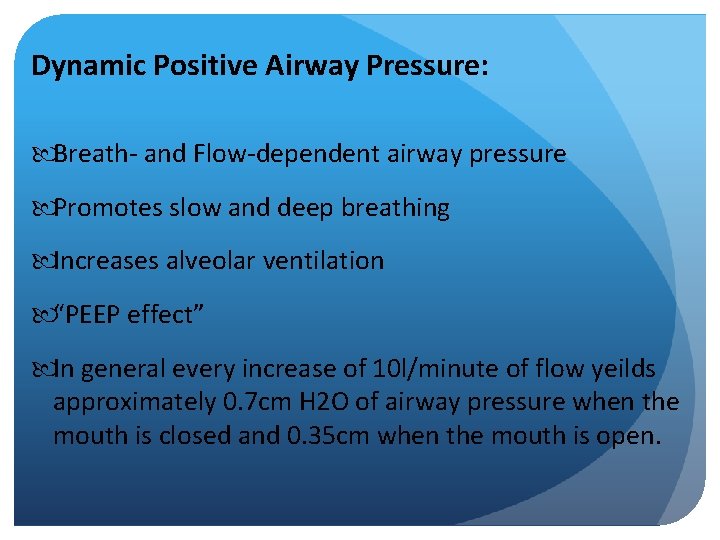
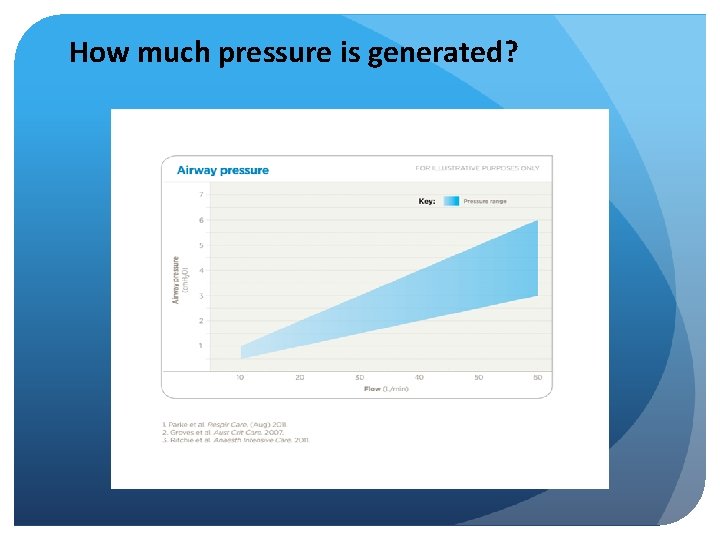
Dynamic Positive Airway Pressure: Breath- and Flow-dependent airway pressure Promotes slow and deep breathing Increases alveolar ventilation “PEEP effect” In general every increase of 10 l/minute of flow yeilds approximately 0. 7 cm H 2 O of airway pressure when the mouth is closed and 0. 35 cm when the mouth is open.
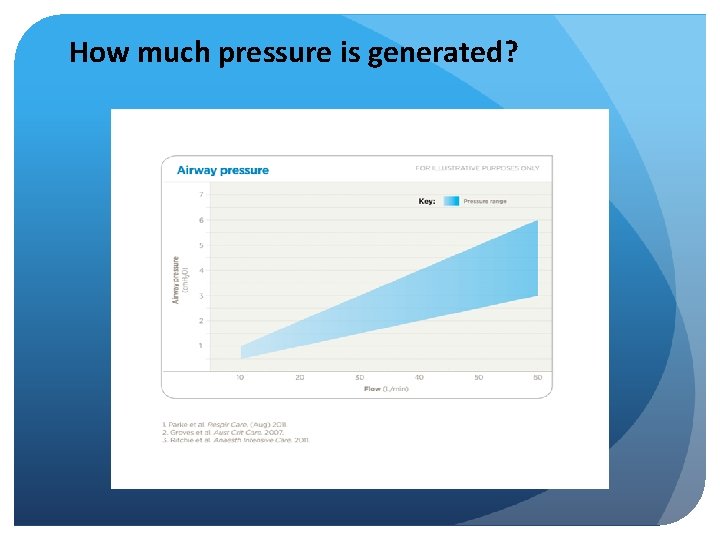
How much pressure is generated?
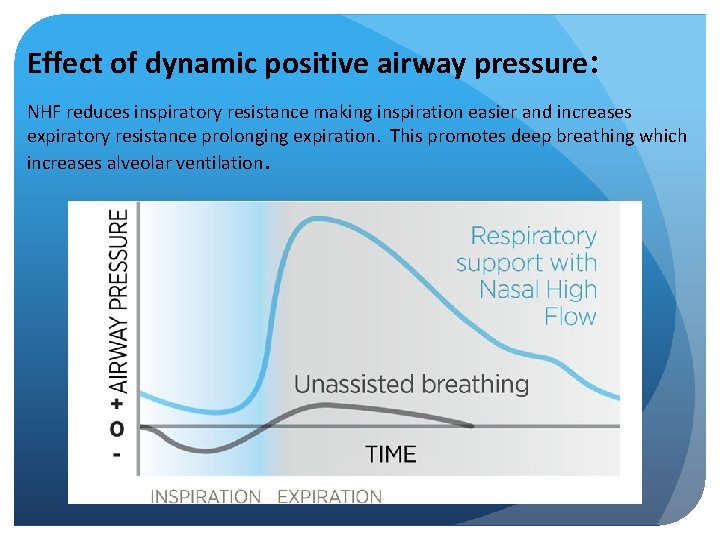
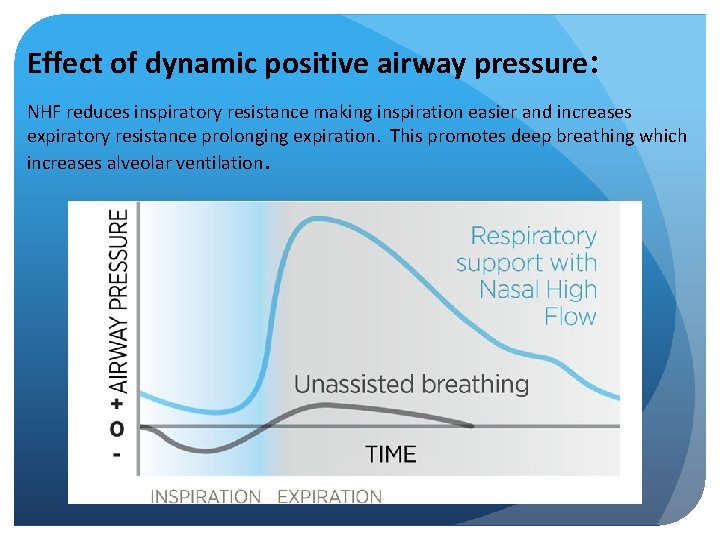
Effect of dynamic positive airway pressure: NHF reduces inspiratory resistance making inspiration easier and increases expiratory resistance prolonging expiration. This promotes deep breathing which increases alveolar ventilation.
Delivering optimal humidity: 1. Optimal humidity emulates natural balance of heat and moisture that occurs normally in healthy lungs. 2. Is essential to physiological stability in already compromised airways. 3. Humidity enables the comfortable delivery of high flow.
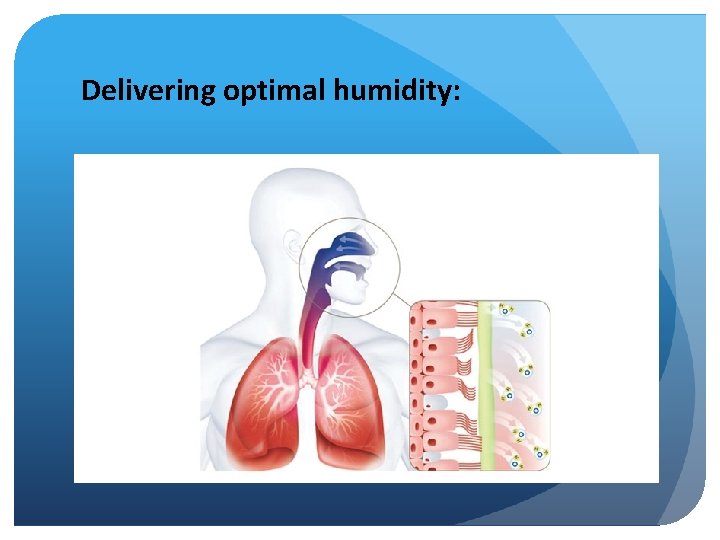
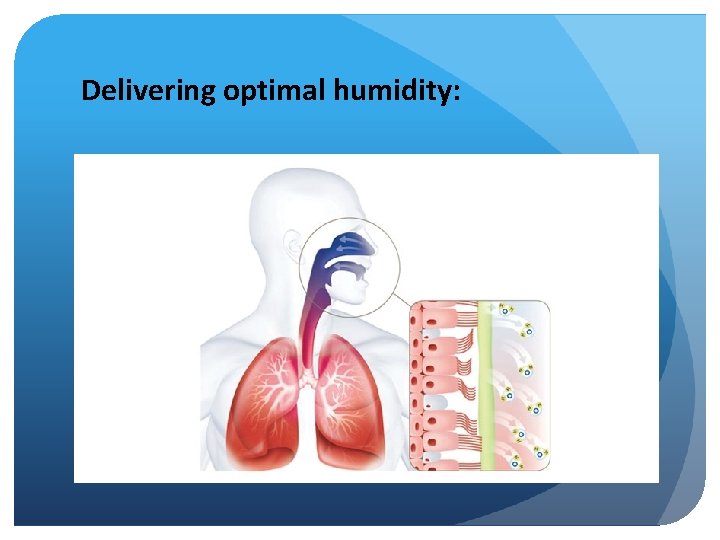
Delivering optimal humidity:
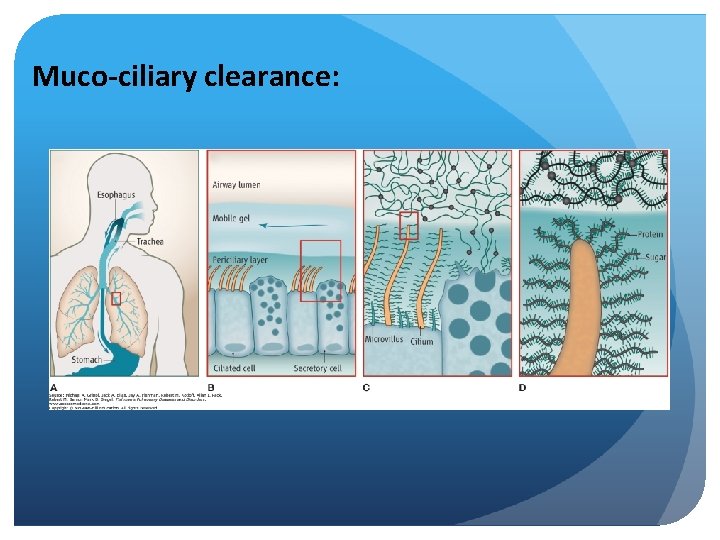
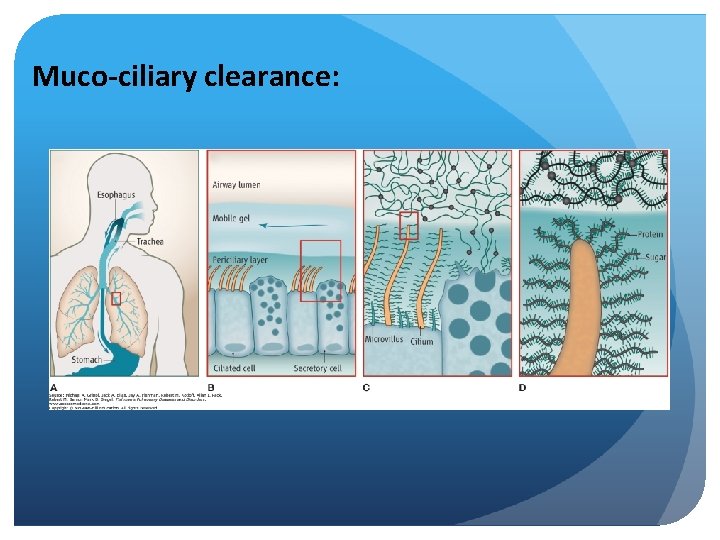
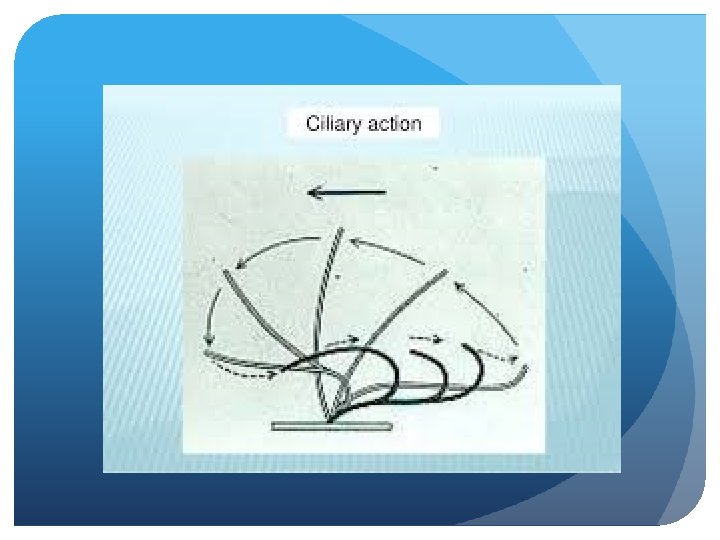
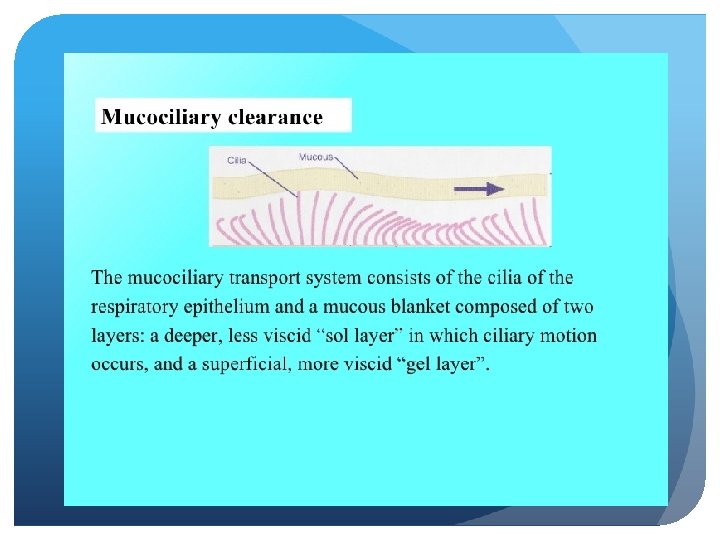
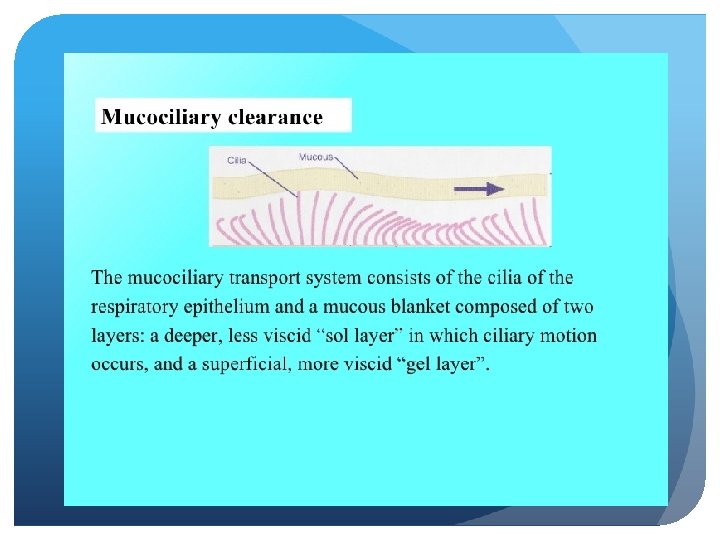
Muco-ciliary clearance:
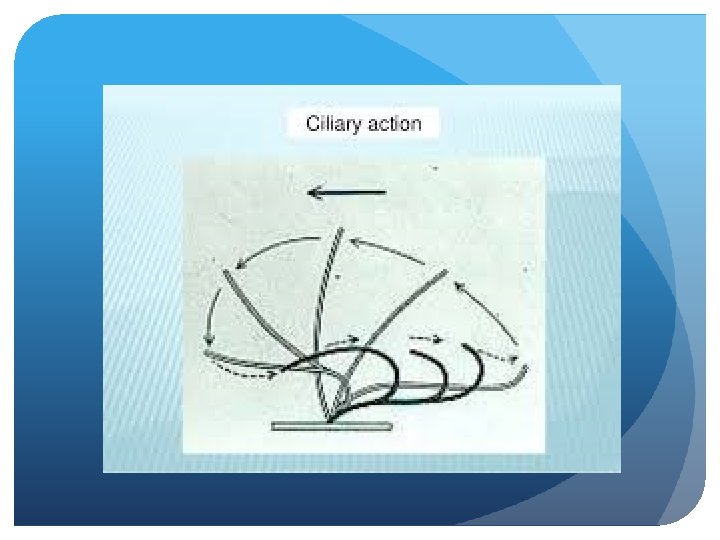
Airway hydration: Improves muco-ciliary clearance. Conditioned gas reduces drying of the airway epithelium. Helps muco-ciliary transport system by clearing secretions and reducing the risk of infections.
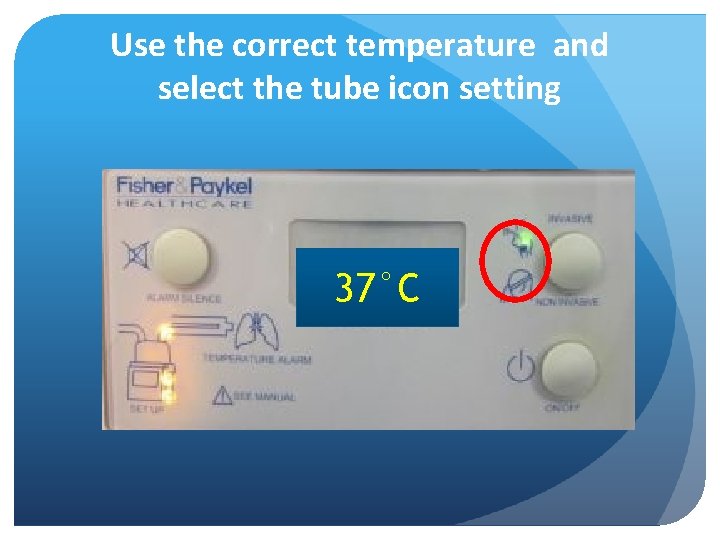
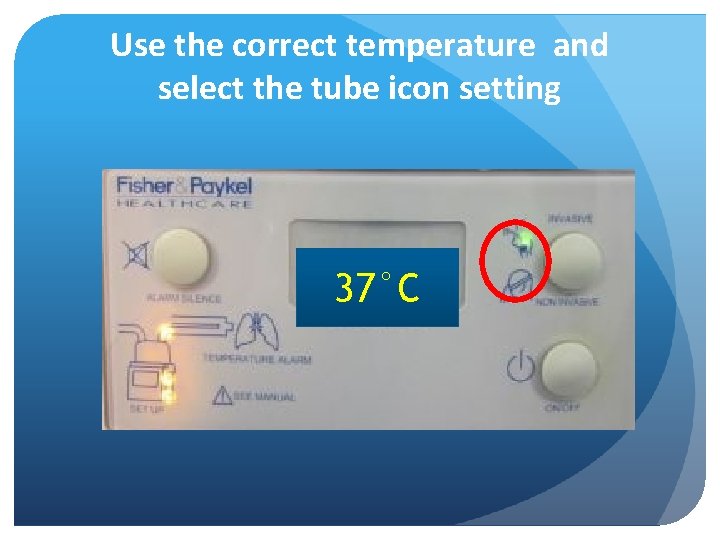
Use the correct temperature and select the tube icon setting 37°C
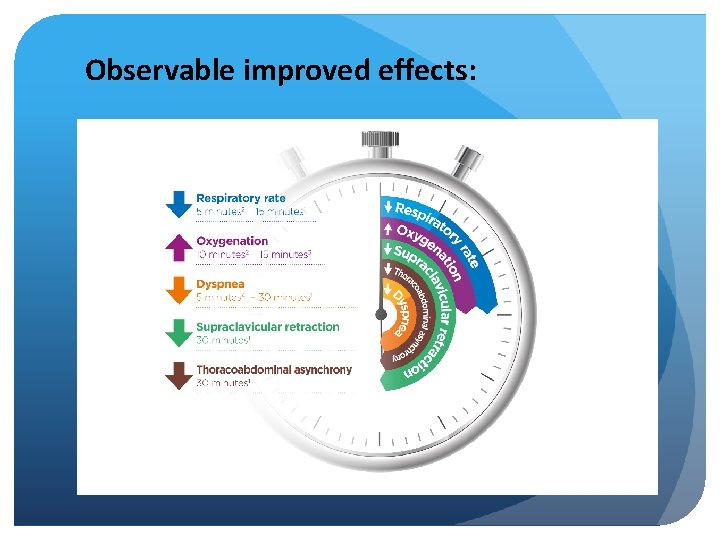
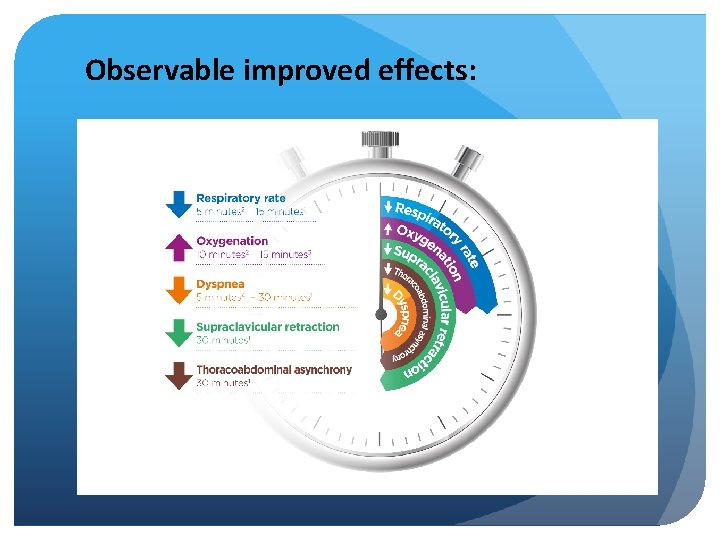
Observable improved effects:
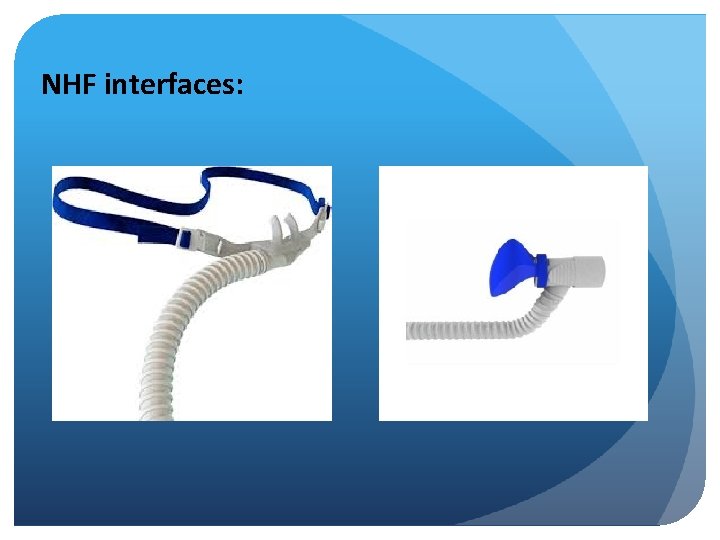
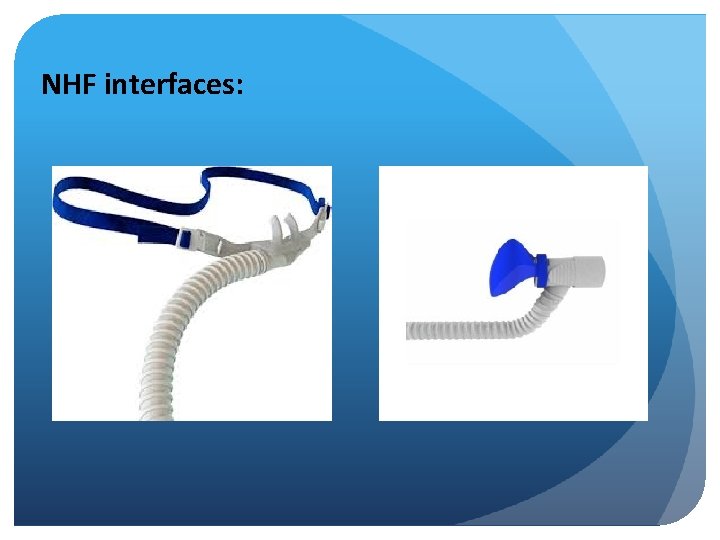
NHF interfaces:
Adult flow rates: Initiate flow rate 30 – 40 litres/min Next select oxygen concentration Review at 15 minutes If no response: increase flow rate again before increasing oxygen and then reassess. Increase oxygen if observations don’t improve
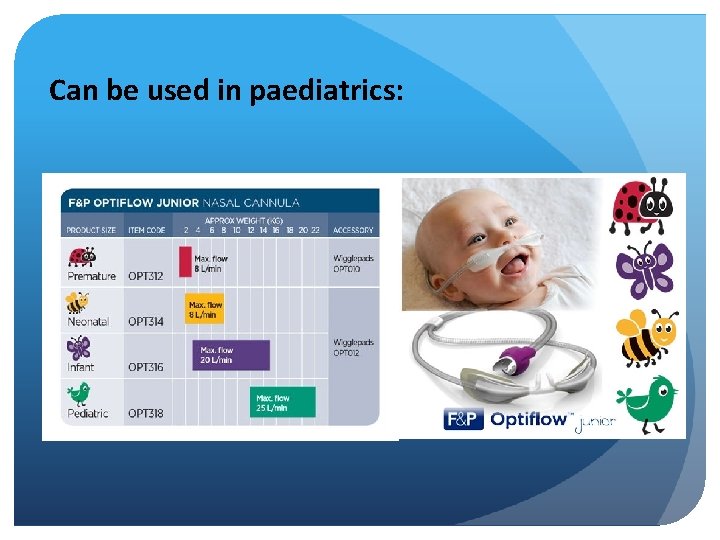
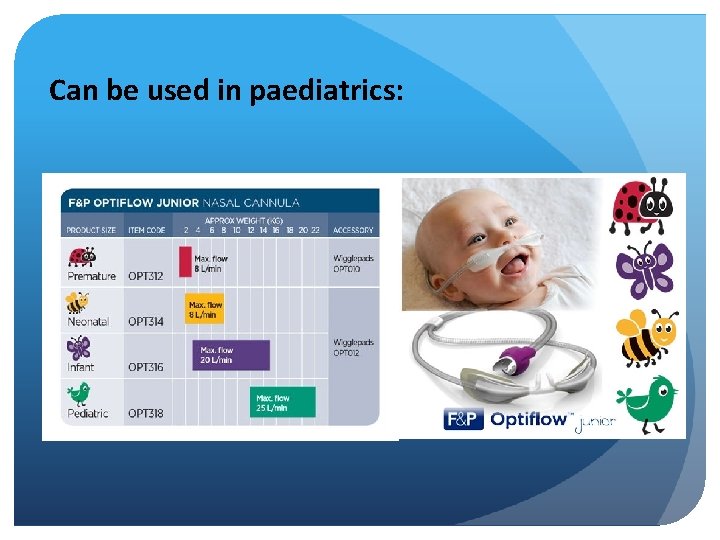
Can be used in paediatrics: