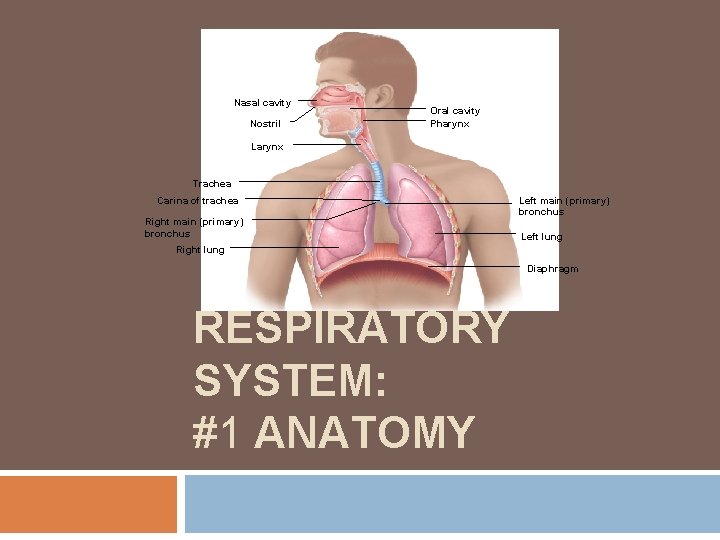
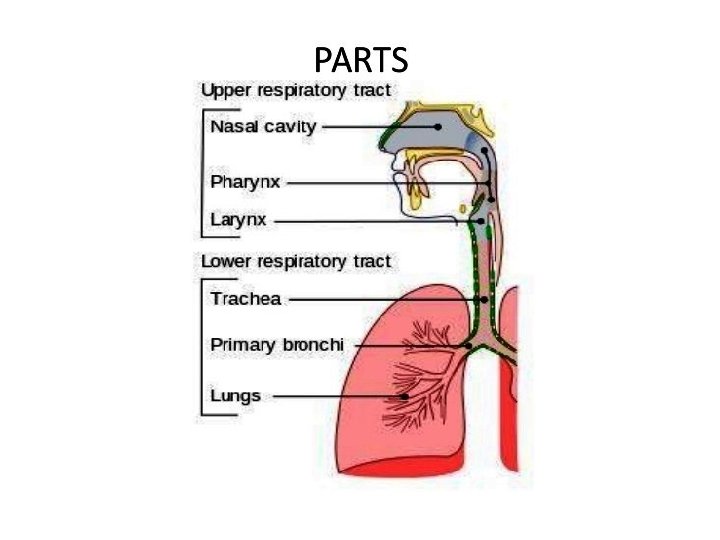
Nasal cavity Nostril Oral cavity Pharynx Larynx Trachea
- Slides: 35
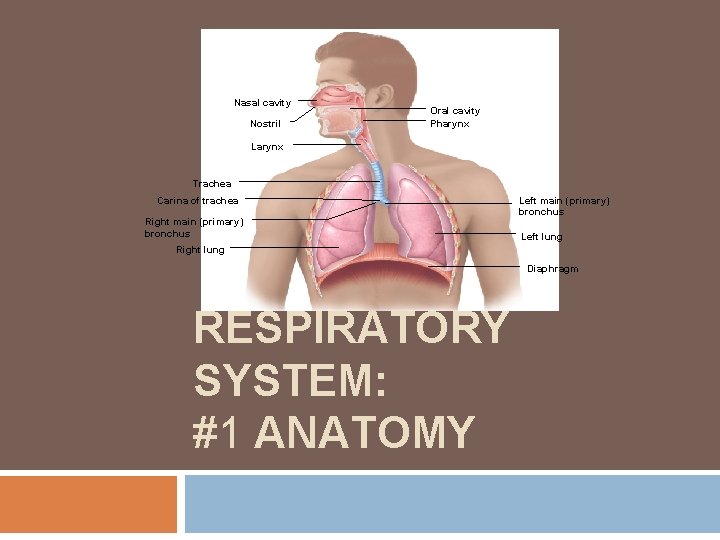
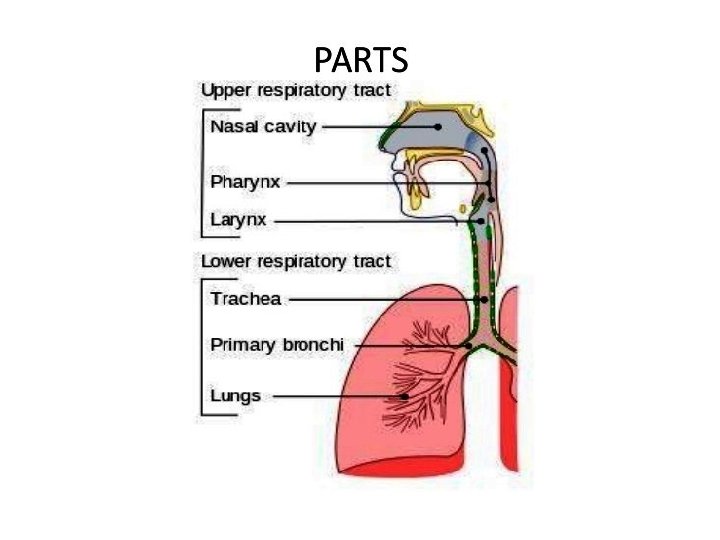
Nasal cavity Nostril Oral cavity Pharynx Larynx Trachea Carina of trachea Right main (primary) bronchus Left lung Right lung Diaphragm RESPIRATORY SYSTEM: #1 ANATOMY
Goals/Objectives Identify the organs forming the respiratory passageway(s) in descending order until you reach the alveoli Describe the location, structure, and function of each of the following: nose, paranasal sinuses, pharynx, and larynx List and describe several protective mechanisms of the respiratory system Distinguish between conducting and respiratory zone structures Describe the makeup of the respiratory membrane
Respiratory System Functions The primary functions of the respiratory system are to: 1. Provide a gas exchange surface; 2. Gas exchange between blood and lungs 3. Protect respiratory surfaces from environment; 4. Defend against invasion by pathogens. Auxiliary functions of the respiratory system include the: 5. Production of sound 6. Involvement in regulation of blood volume and pressure, and control of body p. H.
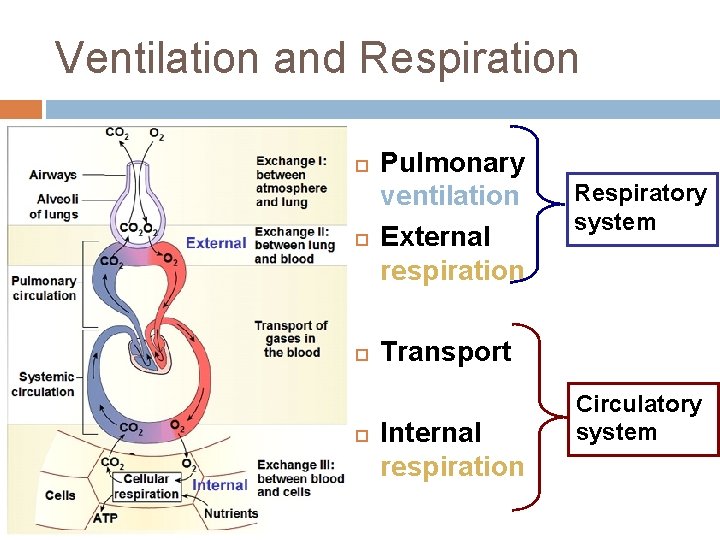
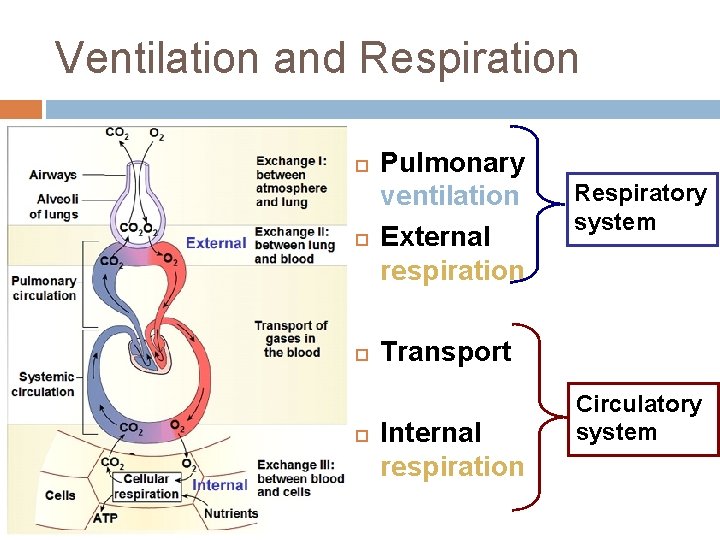
Ventilation and Respiration Pulmonary ventilation External respiration Respiratory system Transport Internal respiration Circulatory system
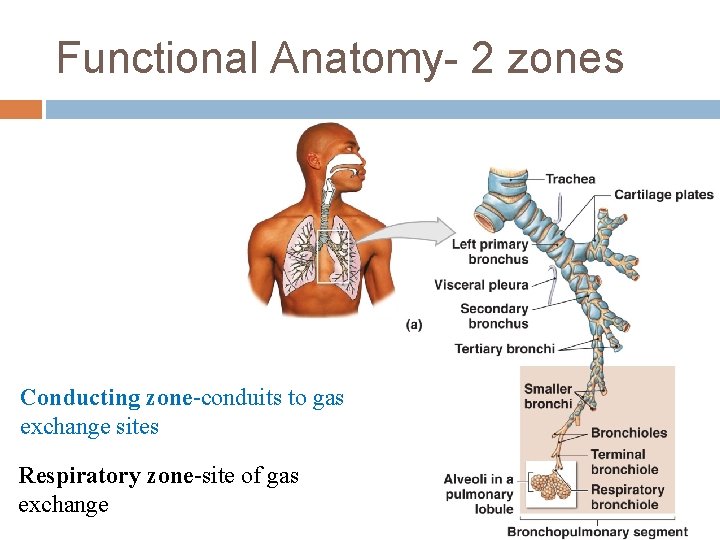
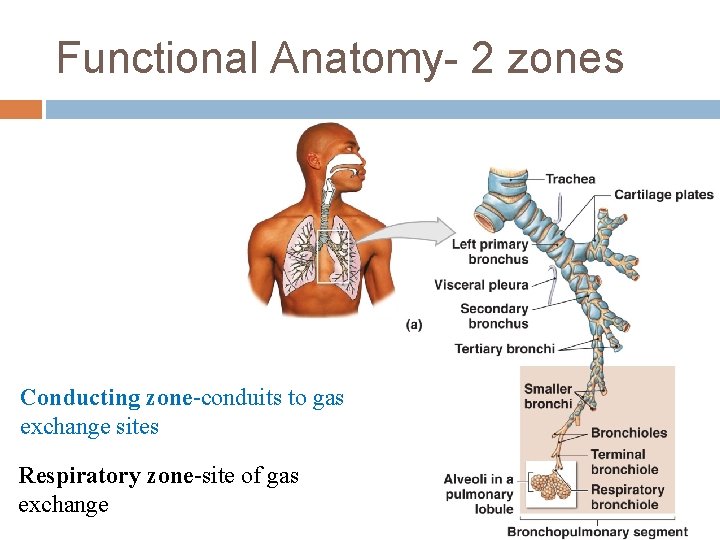
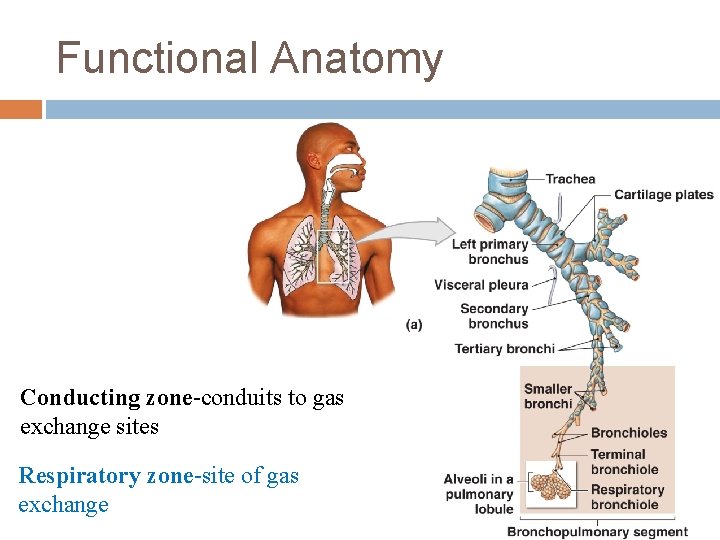
Functional Anatomy- 2 zones Conducting zone-conduits to gas exchange sites Respiratory zone-site of gas exchange © 2013 Pearson Education, Inc.
The Nose Functions �Provides an airway for respiration �Moistens and warms entering air �Filters and cleans inspired air �Serves as resonating chamber for speech �Houses olfactory receptors
The Nose – Surface Anatomy Naris (nostril)
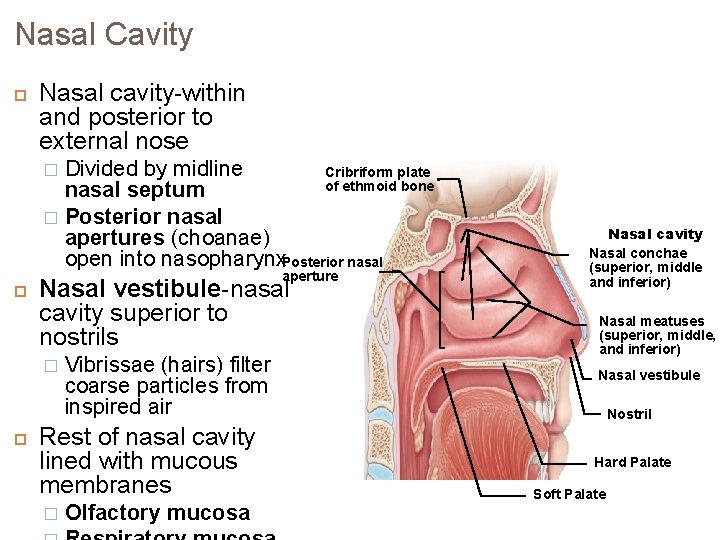
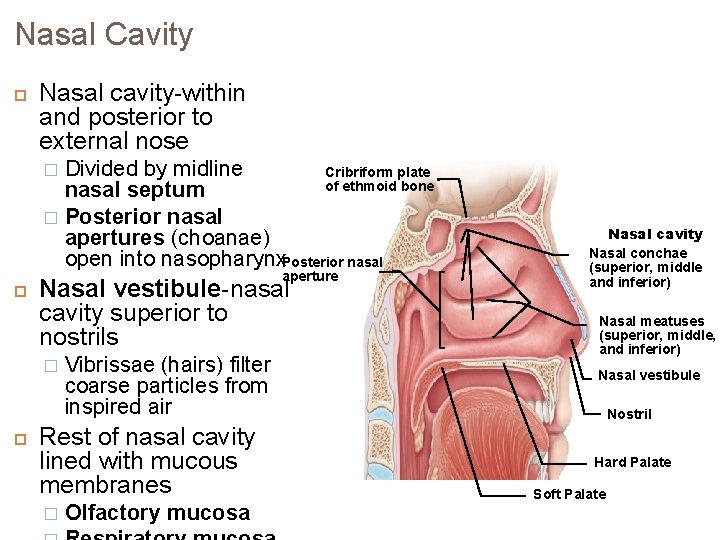
Nasal Cavity Nasal cavity-within and posterior to external nose Divided by midline Cribriform plate of ethmoid bone nasal septum � Posterior nasal apertures (choanae) open into nasopharynx. Posterior nasal � aperture Nasal vestibule-nasal cavity superior to nostrils � Vibrissae (hairs) filter coarse particles from inspired air Rest of nasal cavity lined with mucous membranes � Olfactory mucosa Nasal cavity Nasal conchae (superior, middle and inferior) Nasal meatuses (superior, middle, and inferior) Nasal vestibule Nostril Hard Palate Soft Palate
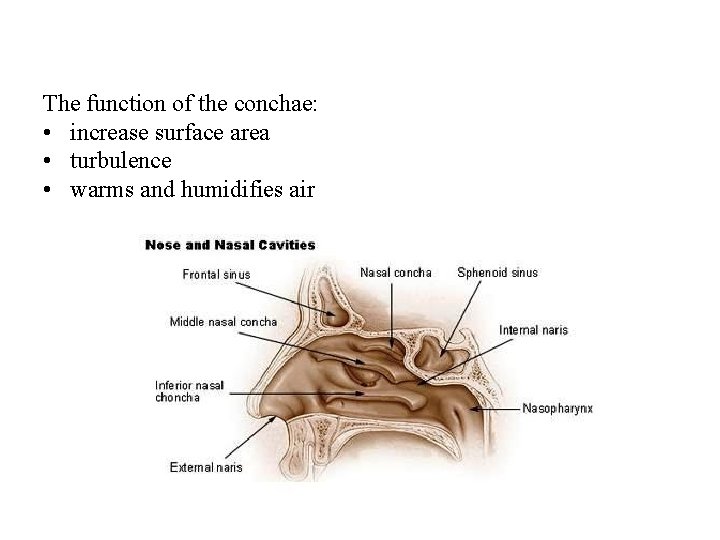
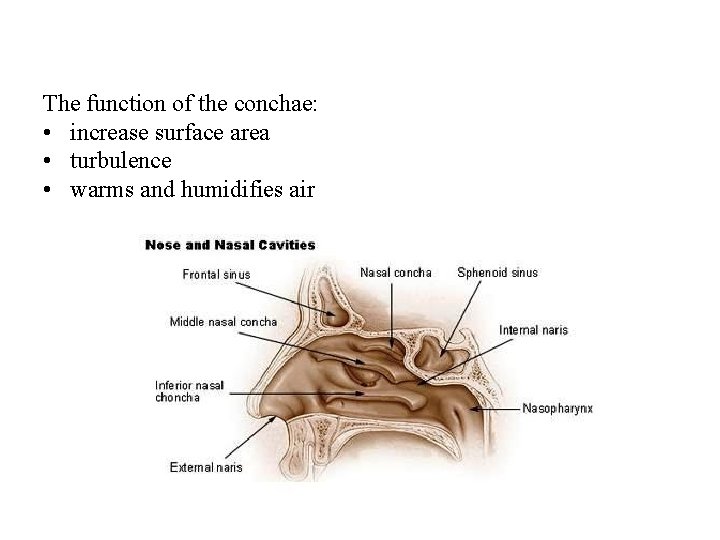
The function of the conchae: • increase surface area • turbulence • warms and humidifies air
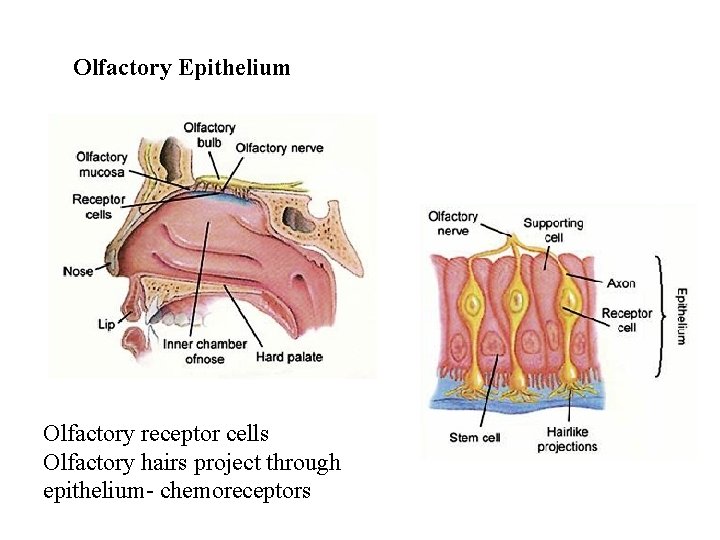
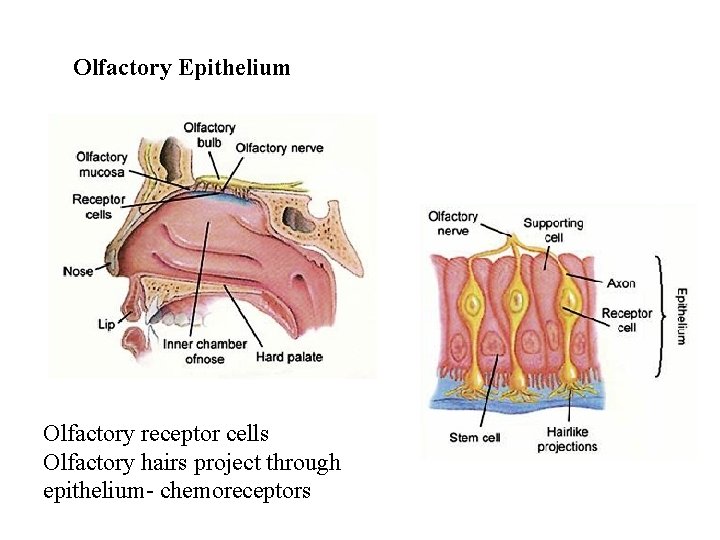
Olfactory Epithelium Olfactory receptor cells Olfactory hairs project through epithelium- chemoreceptors
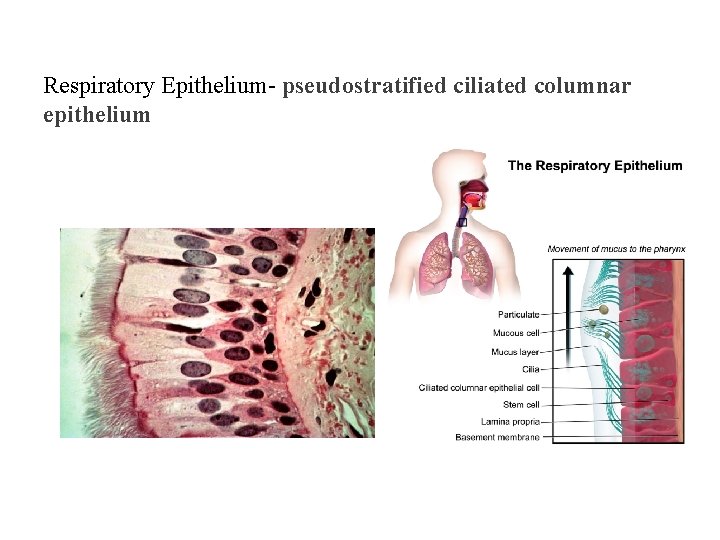
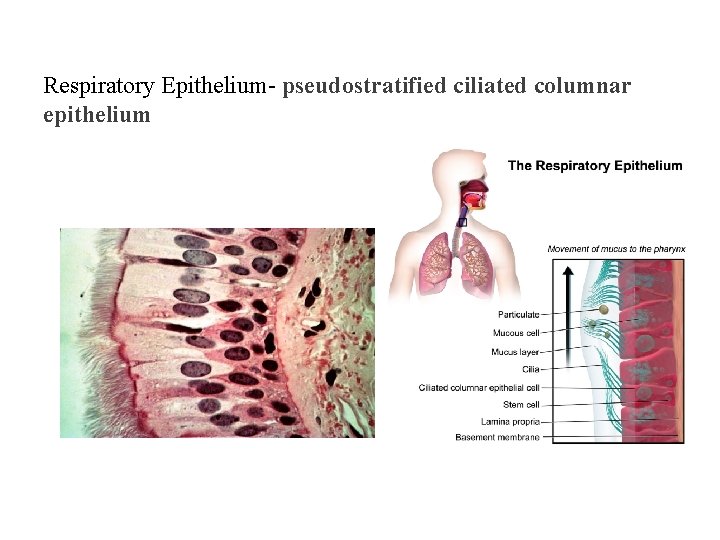
Respiratory Epithelium- pseudostratified ciliated columnar epithelium
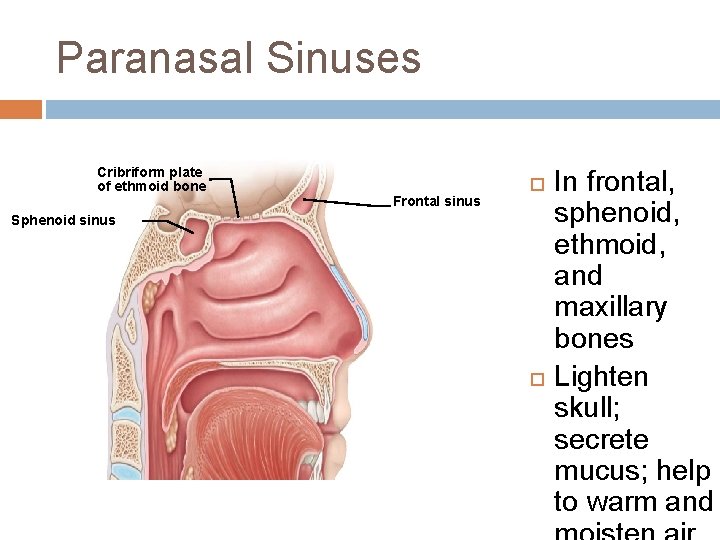
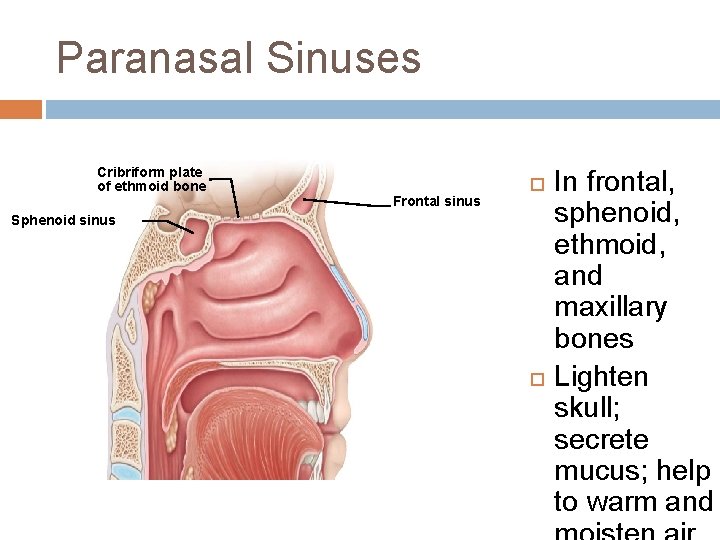
Paranasal Sinuses Cribriform plate of ethmoid bone Frontal sinus Sphenoid sinus In frontal, sphenoid, ethmoid, and maxillary bones Lighten skull; secrete mucus; help to warm and
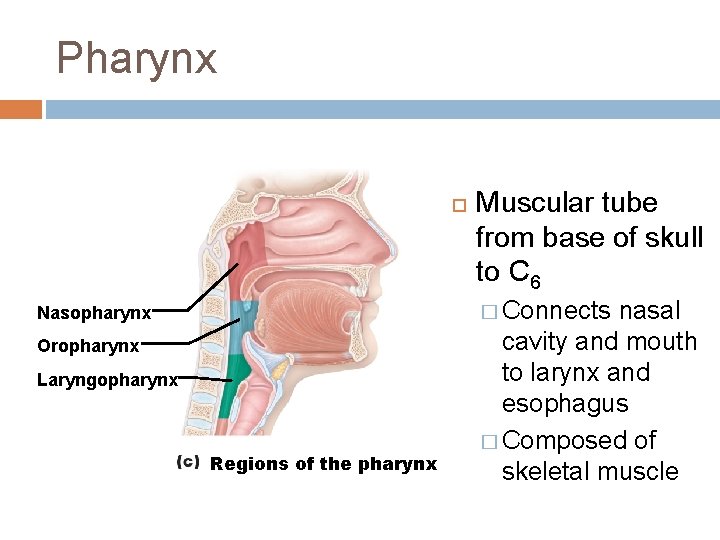
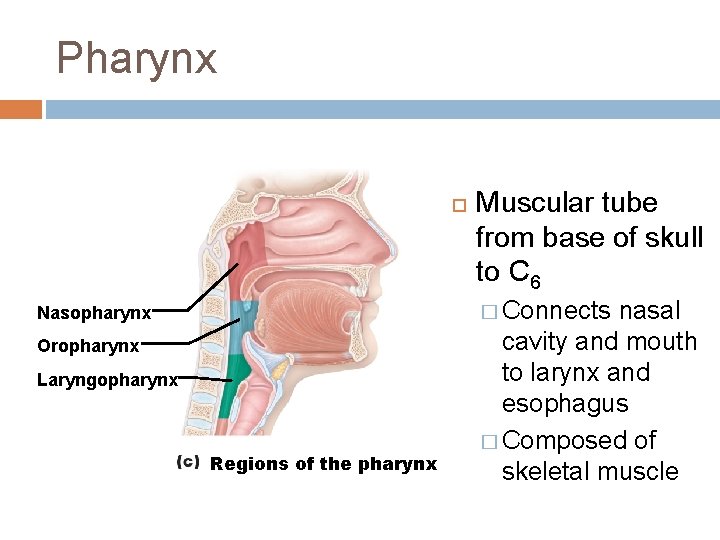
Pharynx Muscular tube from base of skull to C 6 � Connects Nasopharynx Oropharynx Laryngopharynx Regions of the pharynx nasal cavity and mouth to larynx and esophagus � Composed of skeletal muscle
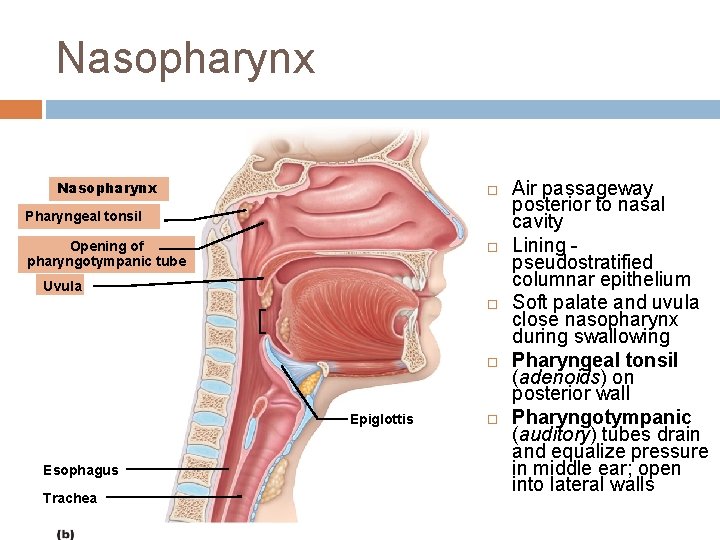
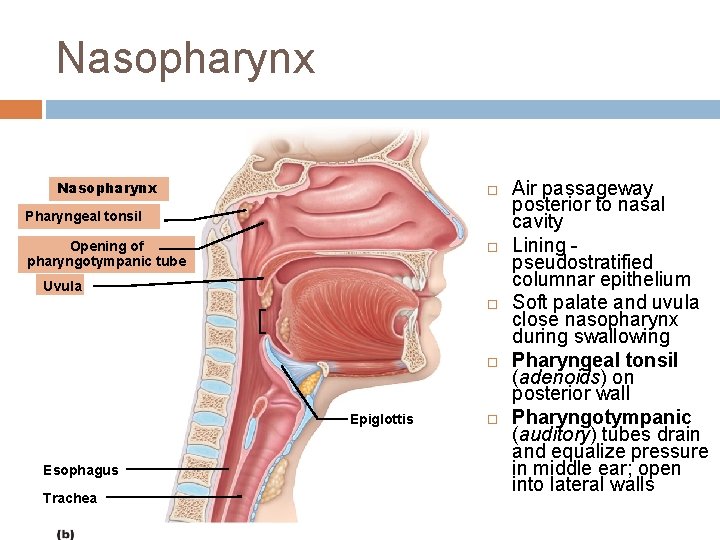
Nasopharynx Pharyngeal tonsil Opening of pharyngotympanic tube Uvula Epiglottis Esophagus Trachea Air passageway posterior to nasal cavity Lining pseudostratified columnar epithelium Soft palate and uvula close nasopharynx during swallowing Pharyngeal tonsil (adenoids) on posterior wall Pharyngotympanic (auditory) tubes drain and equalize pressure in middle ear; open into lateral walls
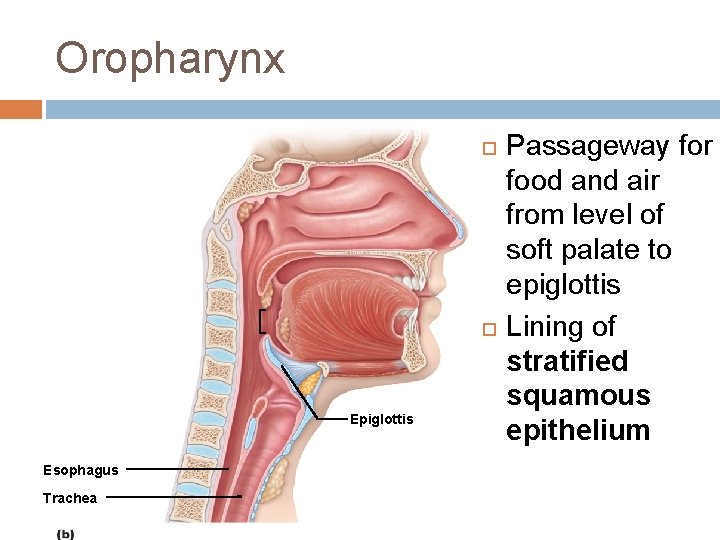
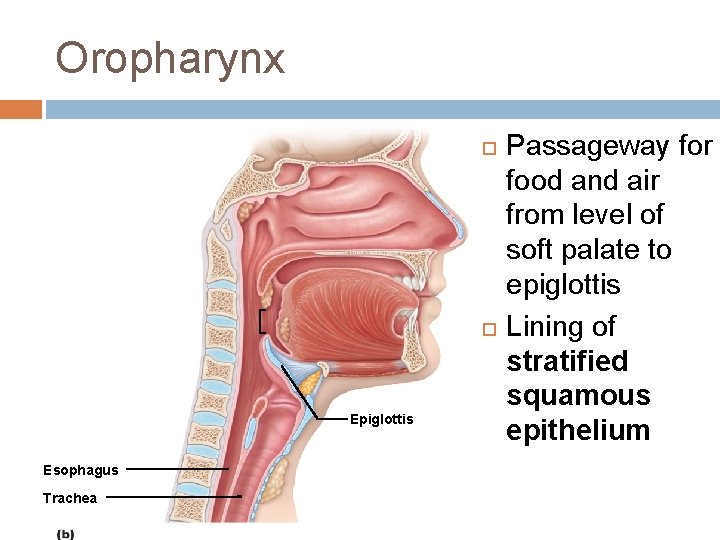
Oropharynx Epiglottis Esophagus Trachea Passageway for food and air from level of soft palate to epiglottis Lining of stratified squamous epithelium
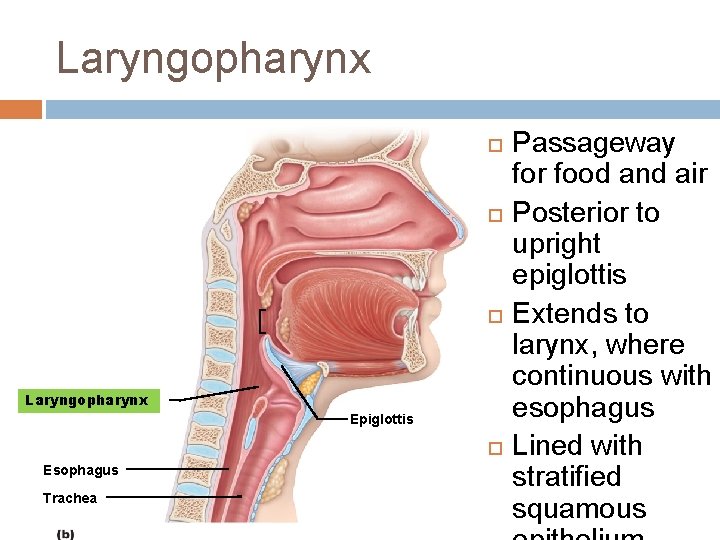
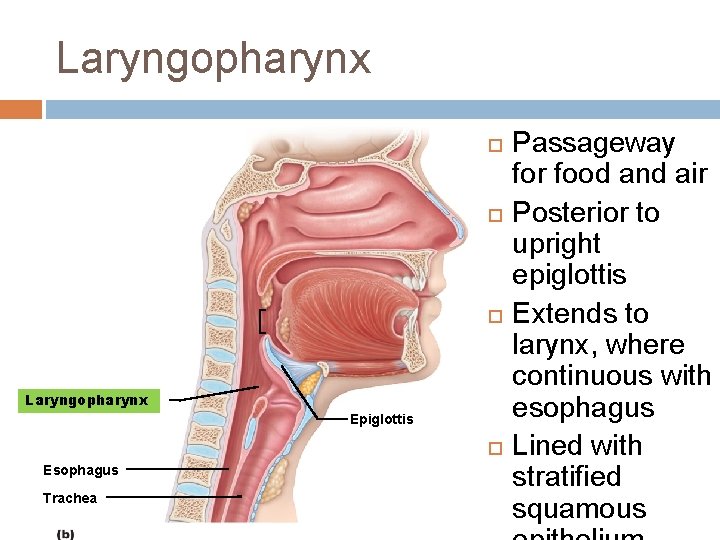
Laryngopharynx Laryngopharynx Epiglottis Esophagus Trachea Passageway for food and air Posterior to upright epiglottis Extends to larynx, where continuous with esophagus Lined with stratified squamous
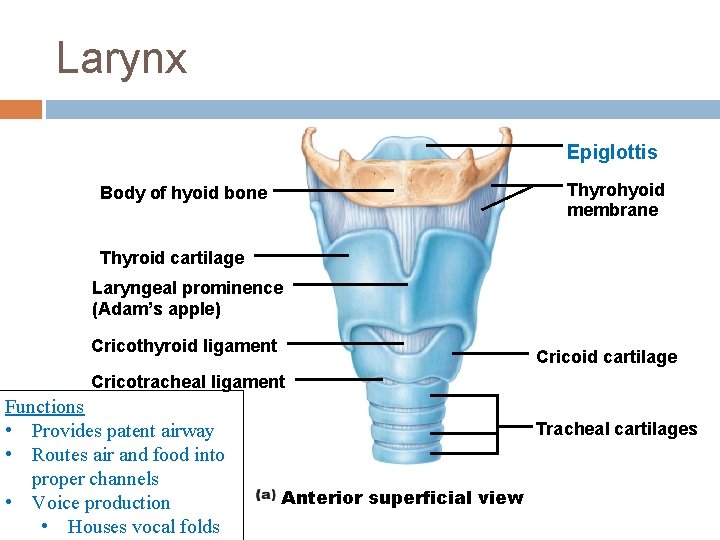
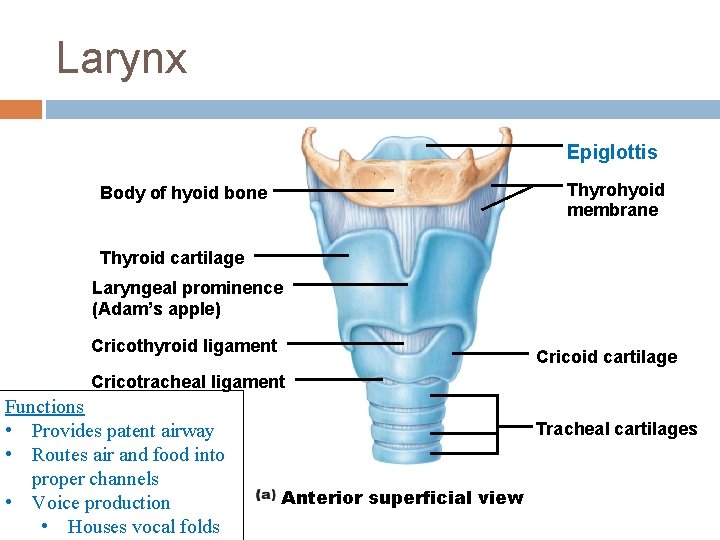
Larynx Epiglottis Thyrohyoid membrane Body of hyoid bone Thyroid cartilage Laryngeal prominence (Adam’s apple) Cricothyroid ligament Cricoid cartilage Cricotracheal ligament Functions • Provides patent airway • Routes air and food into proper channels • Voice production • Houses vocal folds Tracheal cartilages Anterior superficial view
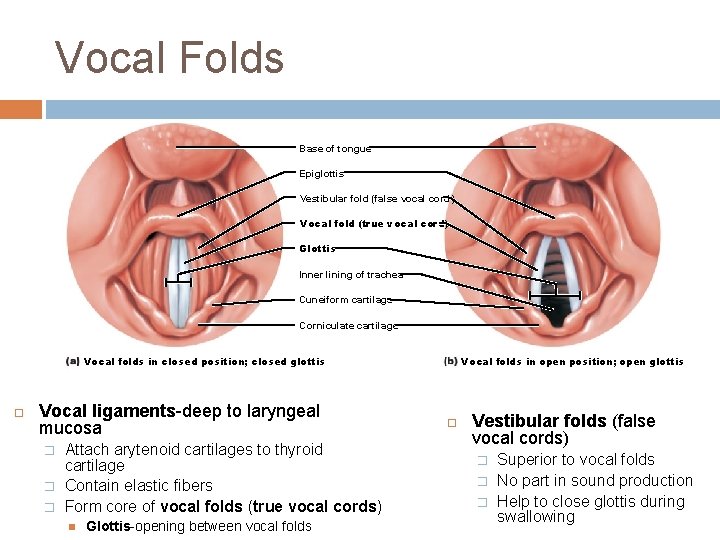
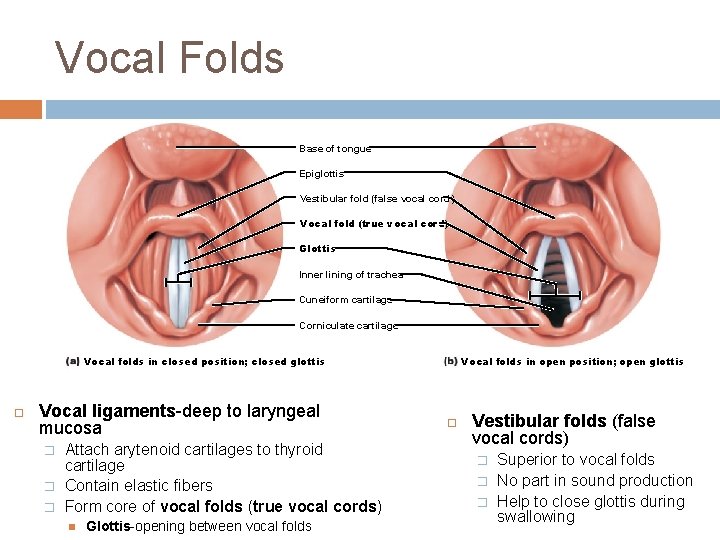
Vocal Folds Base of tongue Epiglottis Vestibular fold (false vocal cord) Vocal fold (true vocal cord) Glottis Inner lining of trachea Cuneiform cartilage Corniculate cartilage Vocal folds in closed position; closed glottis Vocal ligaments-deep to laryngeal mucosa � � � Attach arytenoid cartilages to thyroid cartilage Contain elastic fibers Form core of vocal folds (true vocal cords) Glottis-opening between vocal folds Vocal folds in open position; open glottis Vestibular folds (false vocal cords) � � � Superior to vocal folds No part in sound production Help to close glottis during swallowing
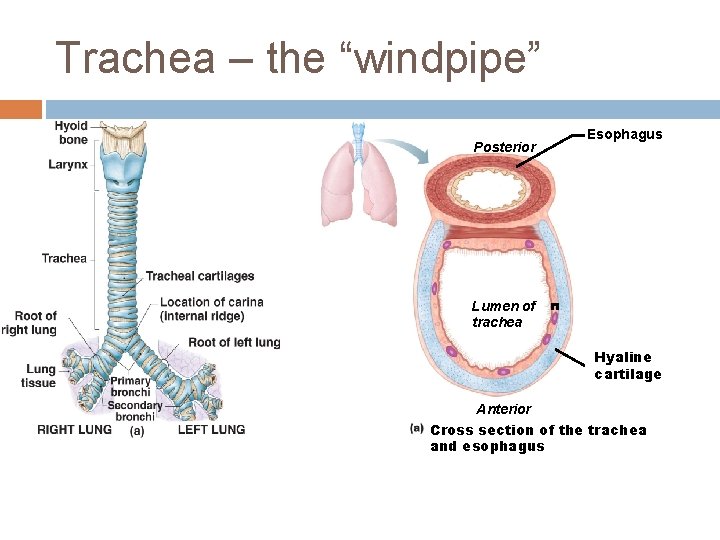
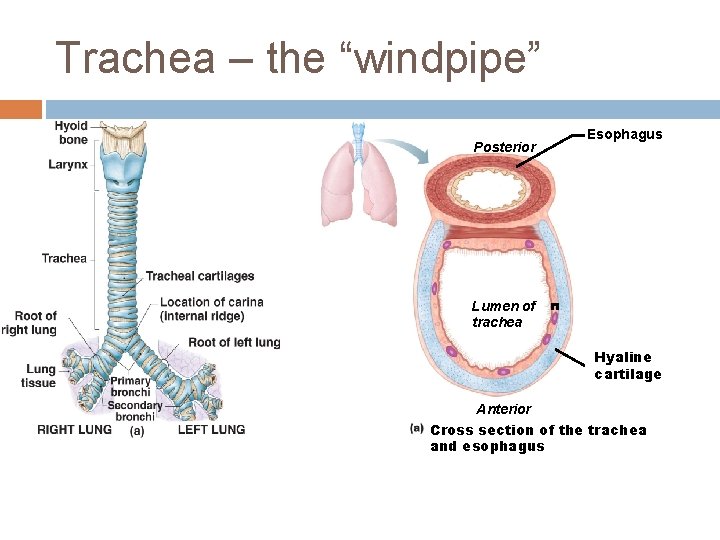
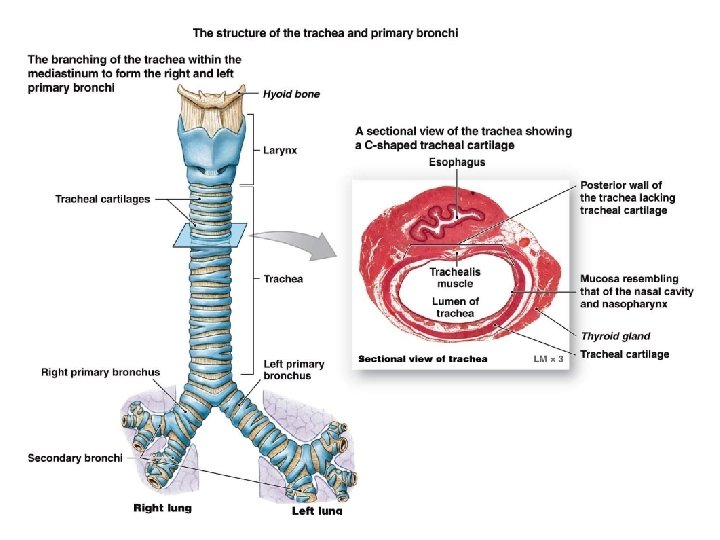
Trachea – the “windpipe” Posterior Esophagus Lumen of trachea Hyaline cartilage Anterior Cross section of the trachea and esophagus
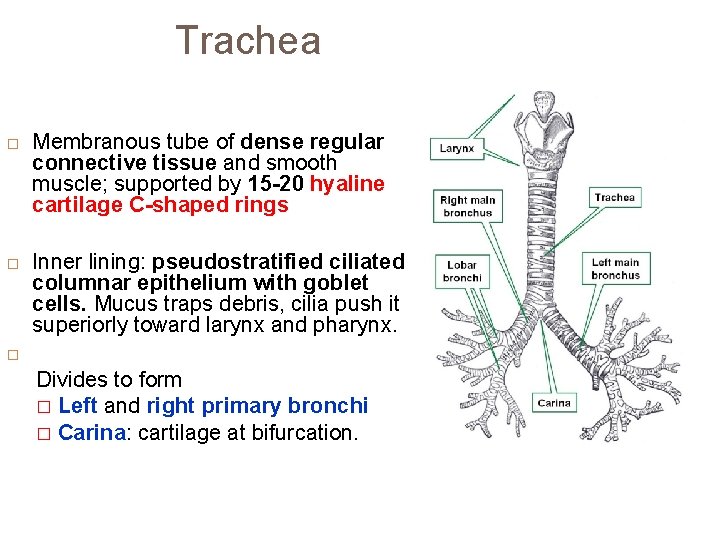
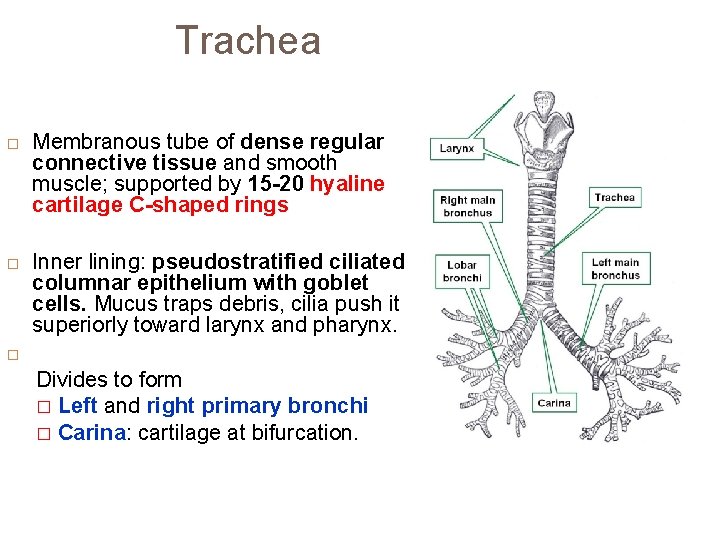
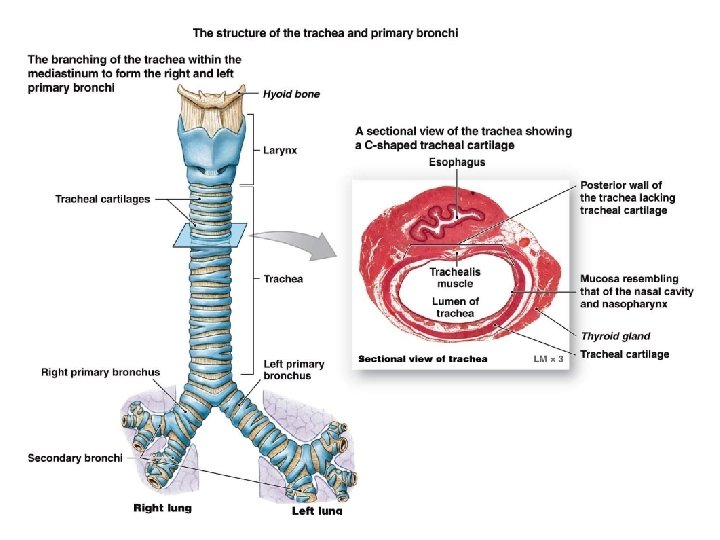
Trachea Membranous tube of dense regular connective tissue and smooth muscle; supported by 15 -20 hyaline cartilage C-shaped rings Inner lining: pseudostratified ciliated columnar epithelium with goblet cells. Mucus traps debris, cilia push it superiorly toward larynx and pharynx. Divides to form � Left and right primary bronchi � Carina: cartilage at bifurcation.
© 2013 Pearson Education, Inc.
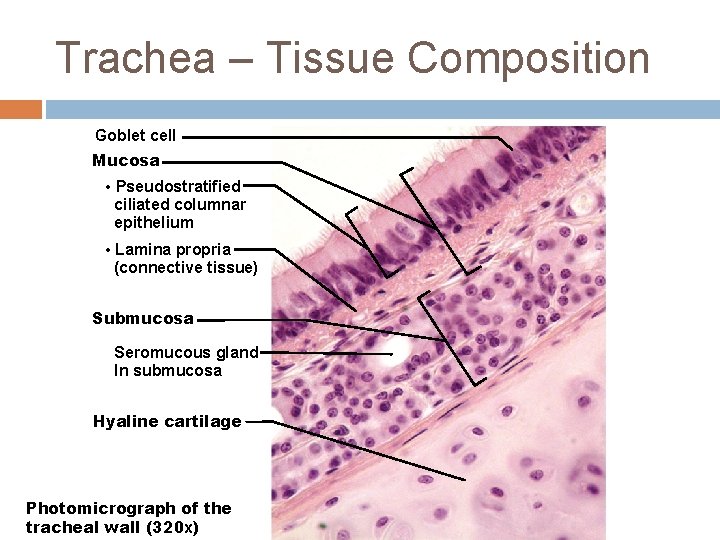
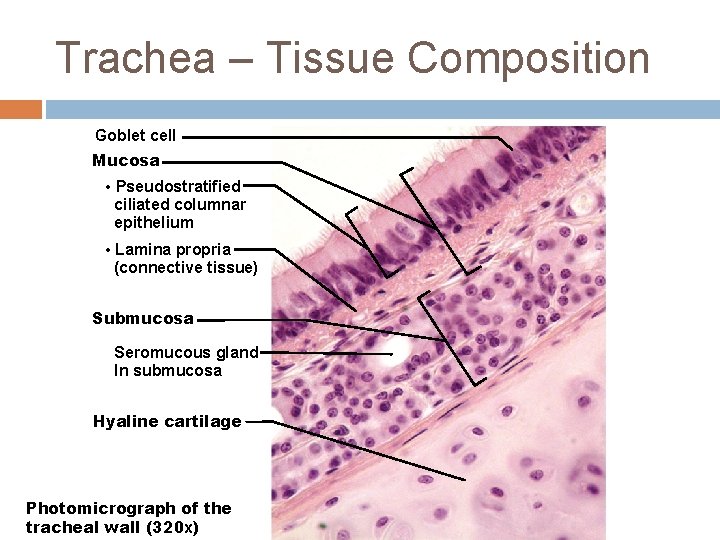
Trachea – Tissue Composition Goblet cell Mucosa • Pseudostratified ciliated columnar epithelium • Lamina propria (connective tissue) Submucosa Seromucous gland In submucosa Hyaline cartilage Photomicrograph of the tracheal wall (320 x)
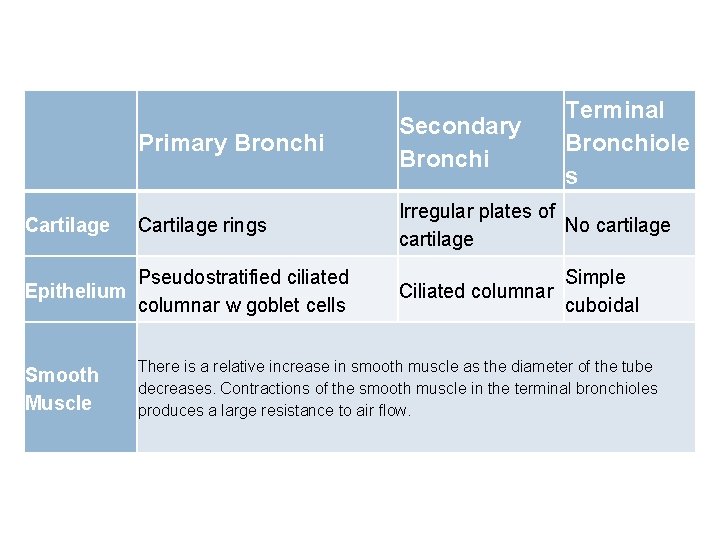
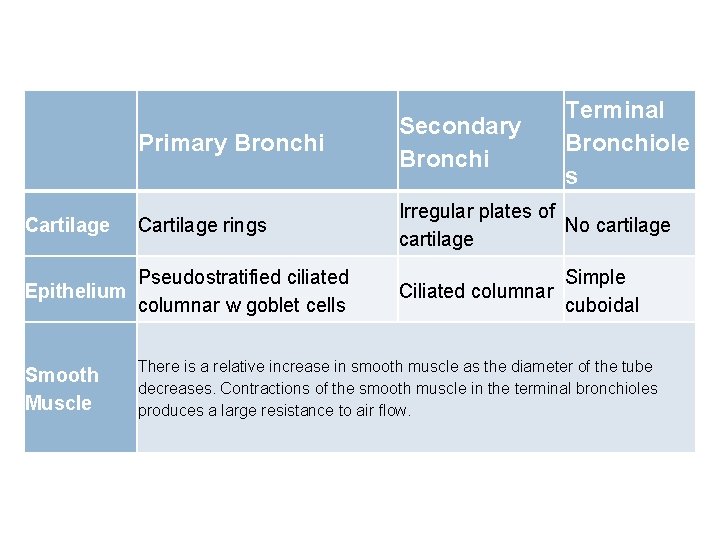
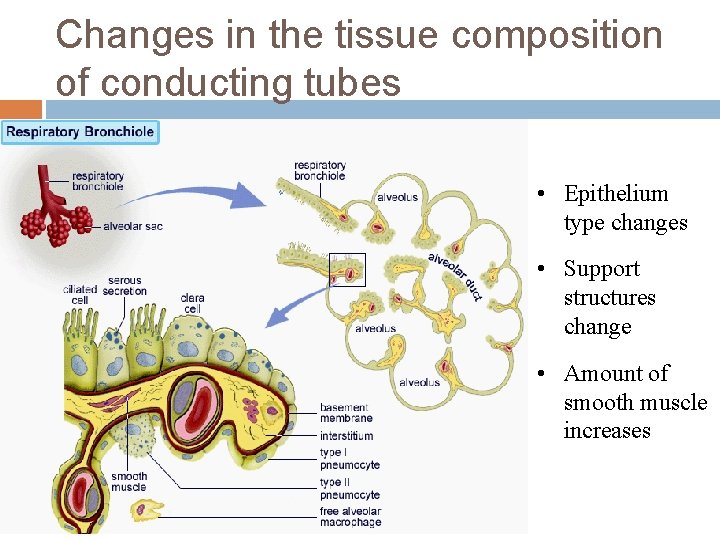
Cartilage Primary Bronchi Secondary Bronchi Cartilage rings Irregular plates of No cartilage Pseudostratified ciliated Epithelium columnar w goblet cells Smooth Muscle Terminal Bronchiole s Simple Ciliated columnar cuboidal There is a relative increase in smooth muscle as the diameter of the tube decreases. Contractions of the smooth muscle in the terminal bronchioles produces a large resistance to air flow.
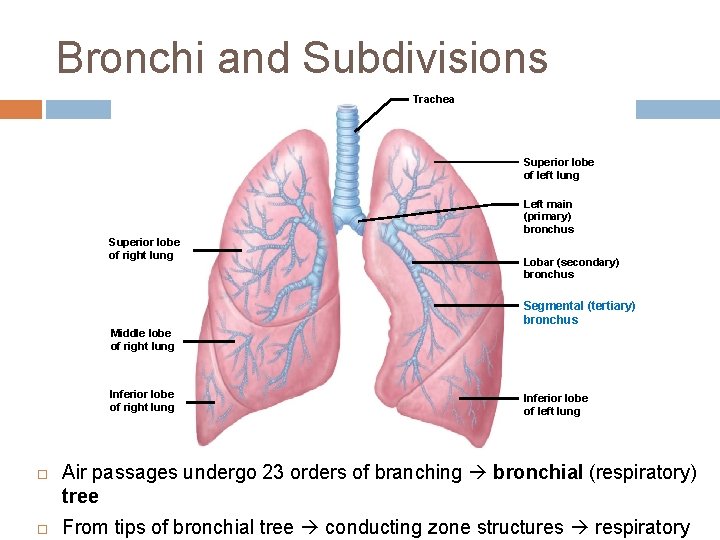
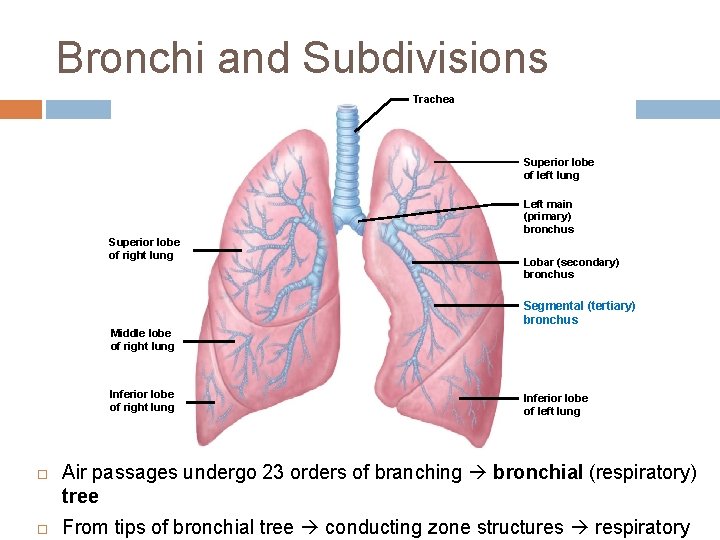
Bronchi and Subdivisions Trachea Superior lobe of left lung Left main (primary) bronchus Superior lobe of right lung Lobar (secondary) bronchus Segmental (tertiary) bronchus Middle lobe of right lung Inferior lobe of right lung Inferior lobe of left lung Air passages undergo 23 orders of branching bronchial (respiratory) tree From tips of bronchial tree conducting zone structures respiratory
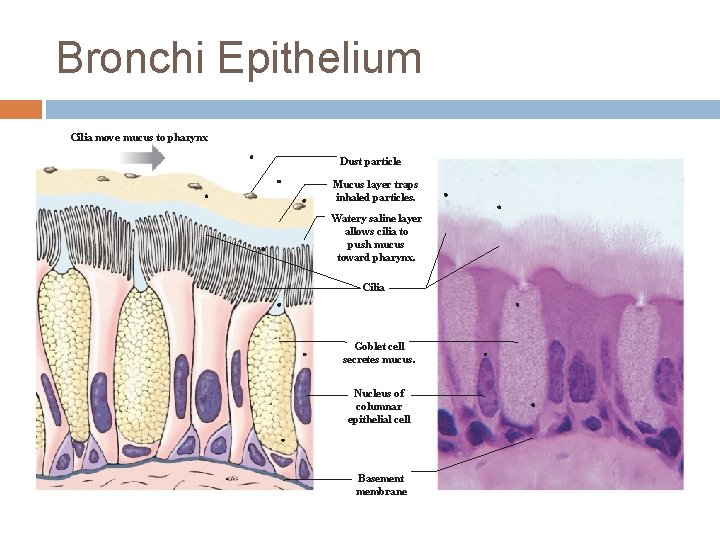
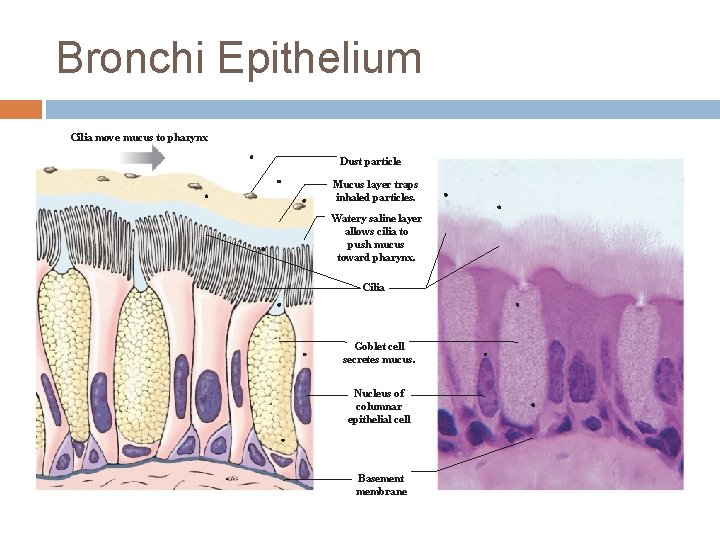
Bronchi Epithelium Cilia move mucus to pharynx Dust particle Mucus layer traps inhaled particles. Watery saline layer allows cilia to push mucus toward pharynx. Cilia Goblet cell secretes mucus. Nucleus of columnar epithelial cell Basement membrane
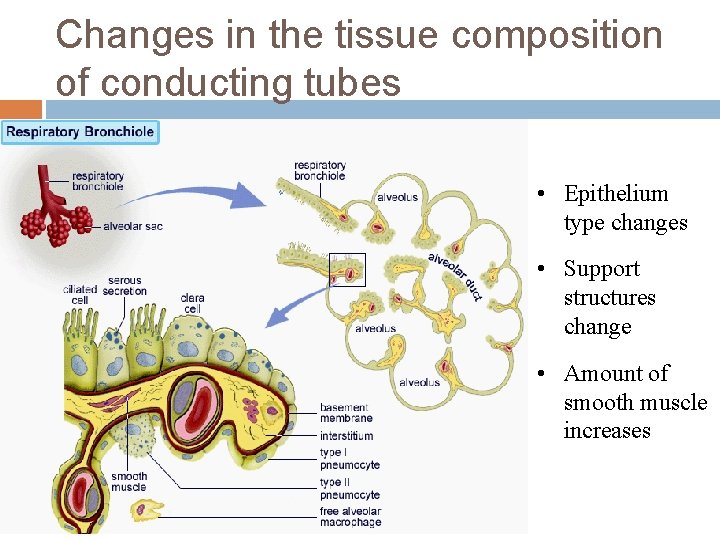
Changes in the tissue composition of conducting tubes • Epithelium type changes • Support structures change • Amount of smooth muscle increases
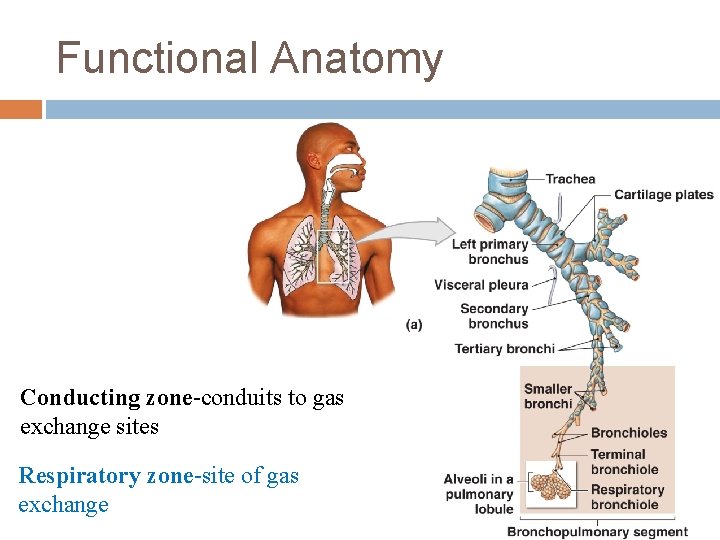
Functional Anatomy Conducting zone-conduits to gas exchange sites Respiratory zone-site of gas exchange © 2013 Pearson Education, Inc.
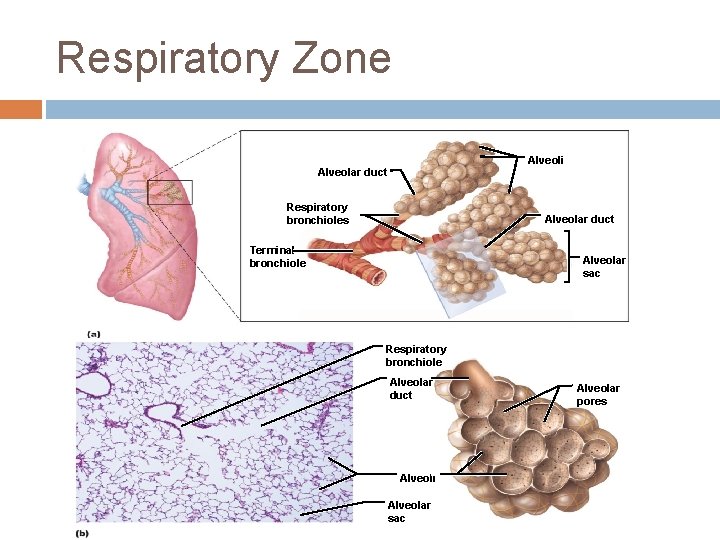
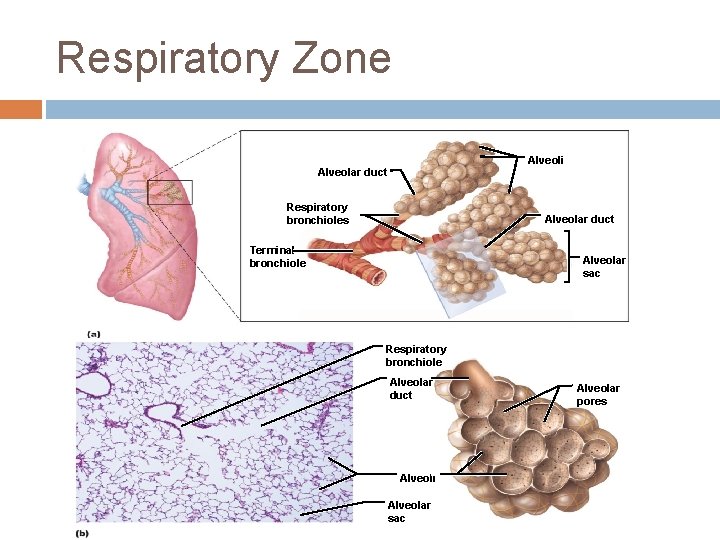
Respiratory Zone Alveoli Alveolar duct Respiratory bronchioles Alveolar duct Terminal bronchiole Alveolar sac Respiratory bronchiole Alveolar duct Alveoli Alveolar sac Alveolar pores
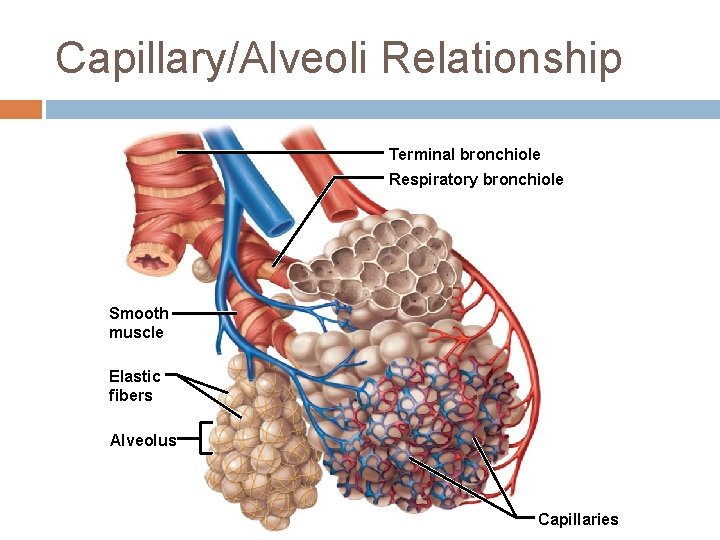
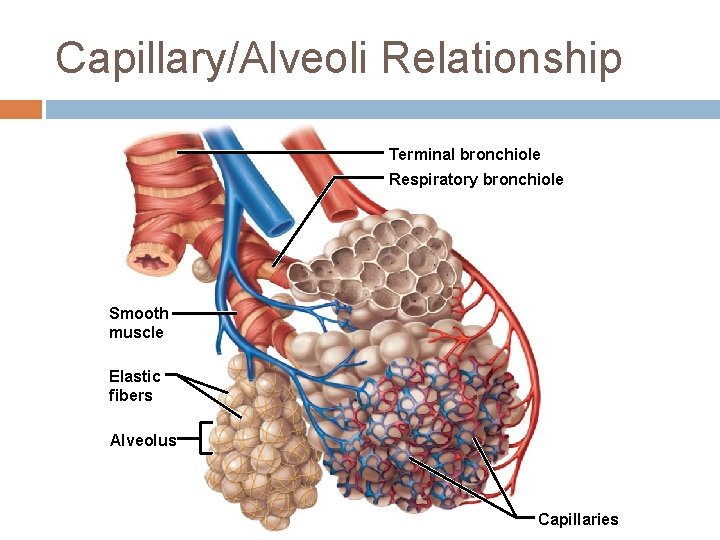
Capillary/Alveoli Relationship Terminal bronchiole Respiratory bronchiole Smooth muscle Elastic fibers Alveolus Capillaries
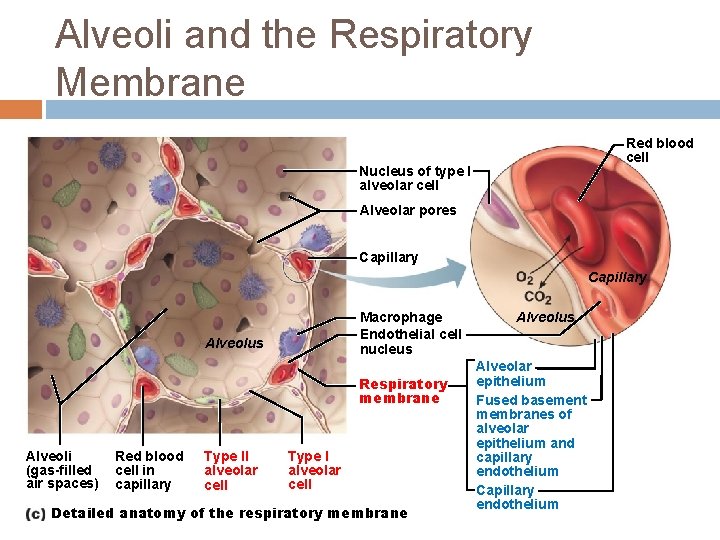
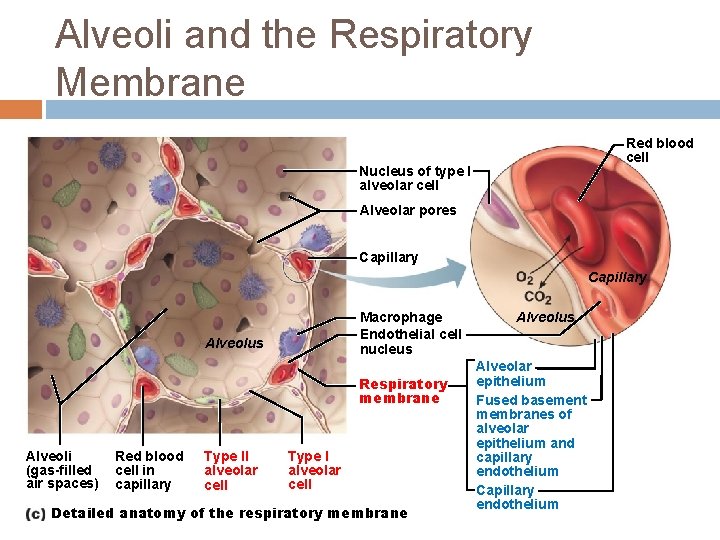
Alveoli and the Respiratory Membrane Red blood cell Nucleus of type I alveolar cell Alveolar pores Capillary Macrophage Endothelial cell nucleus Alveolus Respiratory membrane Alveoli (gas-filled air spaces) Red blood cell in capillary Type II alveolar cell Type I alveolar cell Detailed anatomy of the respiratory membrane Alveolus Alveolar epithelium Fused basement membranes of alveolar epithelium and capillary endothelium Capillary endothelium
Question The respiratory membrane is composed of ____. a) b) c) d) the alveolar sacs and pulmonary arteries the alveolar membrane, the capillary wall, and their fused basement membrane the fusion of the type I and type II alveolar cells the cells found between the alveolar pores
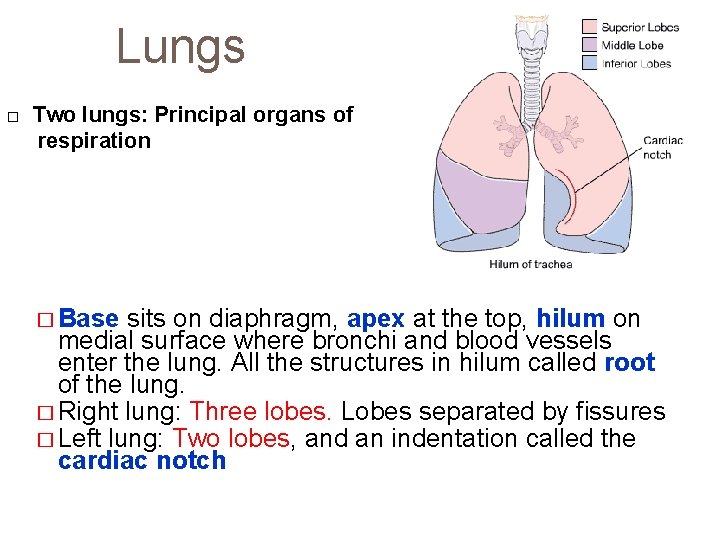
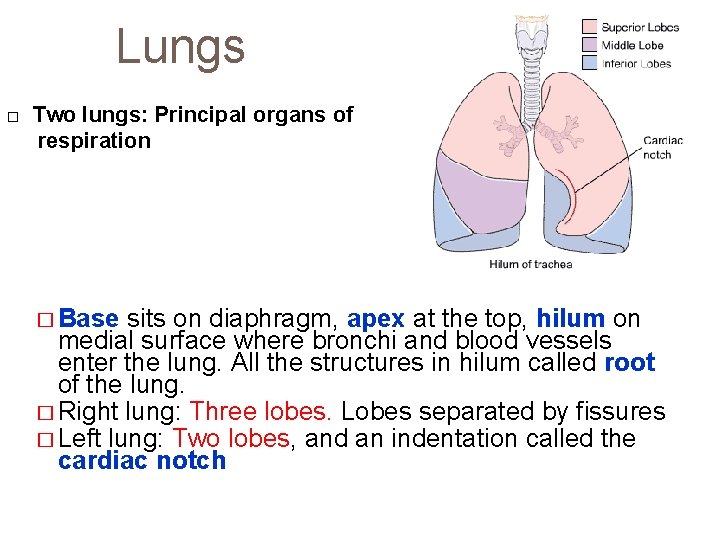
Lungs Two lungs: Principal organs of respiration � Base sits on diaphragm, apex at the top, hilum on medial surface where bronchi and blood vessels enter the lung. All the structures in hilum called root of the lung. � Right lung: Three lobes. Lobes separated by fissures � Left lung: Two lobes, and an indentation called the cardiac notch
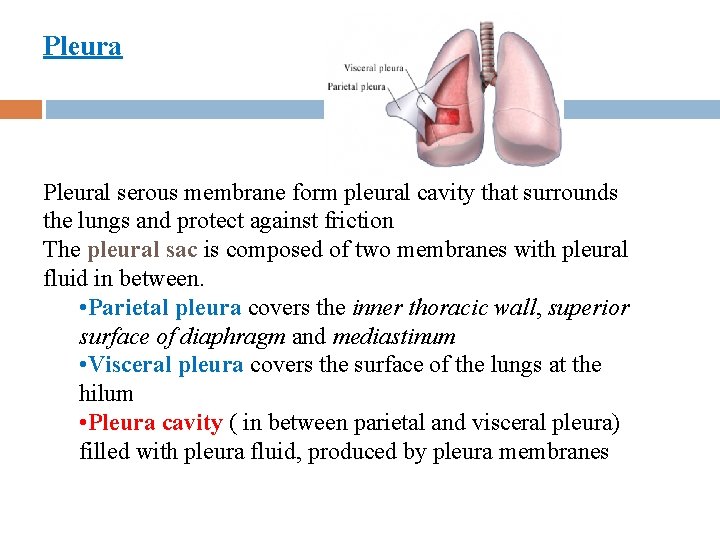
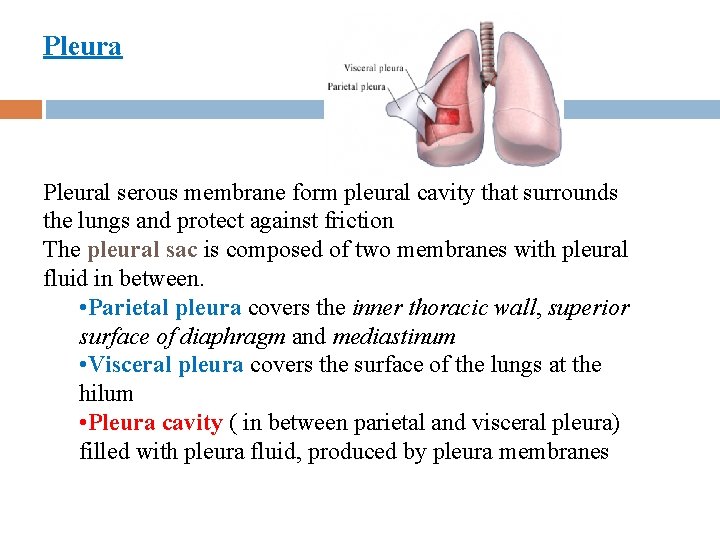
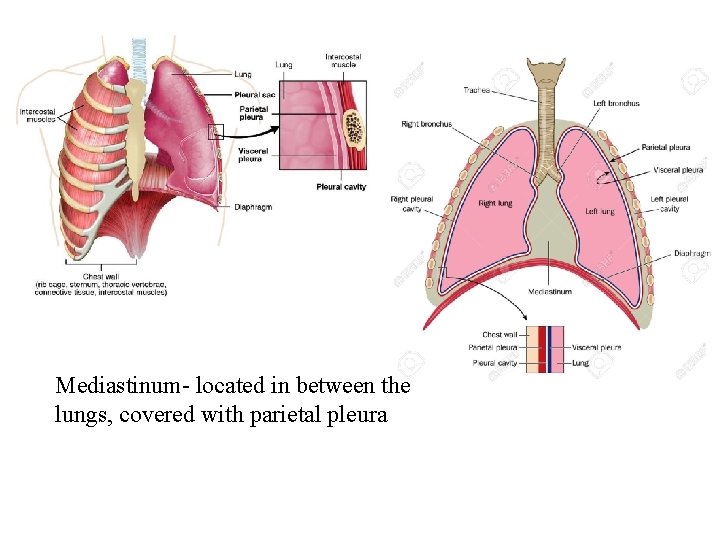
Pleural serous membrane form pleural cavity that surrounds the lungs and protect against friction The pleural sac is composed of two membranes with pleural fluid in between. • Parietal pleura covers the inner thoracic wall, superior surface of diaphragm and mediastinum • Visceral pleura covers the surface of the lungs at the hilum • Pleura cavity ( in between parietal and visceral pleura) filled with pleura fluid, produced by pleura membranes
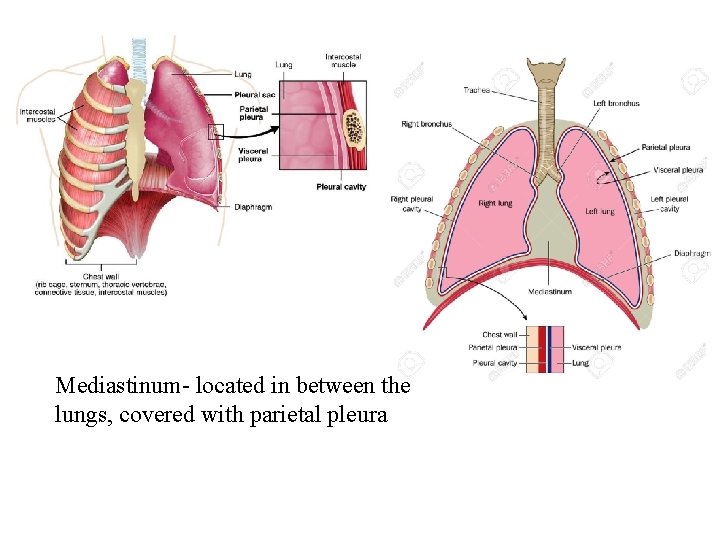
Mediastinum- located in between the lungs, covered with parietal pleura