Myositis and heart disease Louise Pyndt Diederichsen MD





- Slides: 33

Myositis and heart disease

Louise Pyndt Diederichsen, MD, Ph. D Center for Rheumatology and Spine Diseases Copenhagen University Hospital Rigshospitalet Copenhagen, Denmark
Size Denmark: 42. 933 km² Minnesota: 225. 181 km² USA: 9. 834. 000 km² 4
Myositis – a systemic disease
Background – what do we know? Increased mortality in myositis compared to the general population Cardiovascular diseases one of the dominant causes of death Prevalence and type of heart involvement in myositis Cause and treatment ? 6
Background – disease mechanisms Atherosclerosis Inflammation of the heart muscle
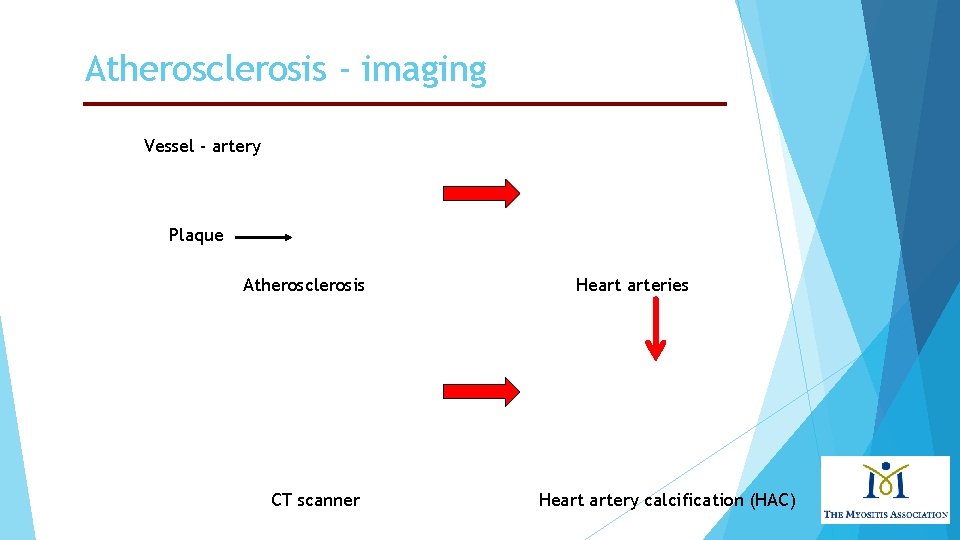
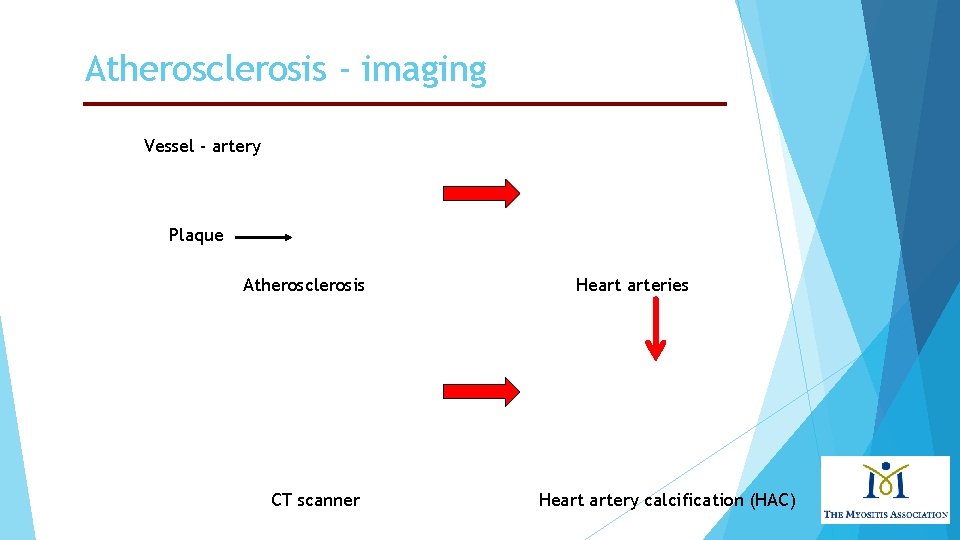
Atherosclerosis - imaging Vessel - artery Plaque Atherosclerosis CT scanner Heart arteries Heart artery calcification (HAC)
Symptoms of coronary heart disease CHD The main symptoms of CHD are: chest pain (angina) heart attacks heart failure You can also experience other symptoms, such as heart palpitations and unusual breathlessness But not everyone has the same symptoms and some people may not have any before CHD is diagnosed American Heart Association, https: //www. heart. org 9
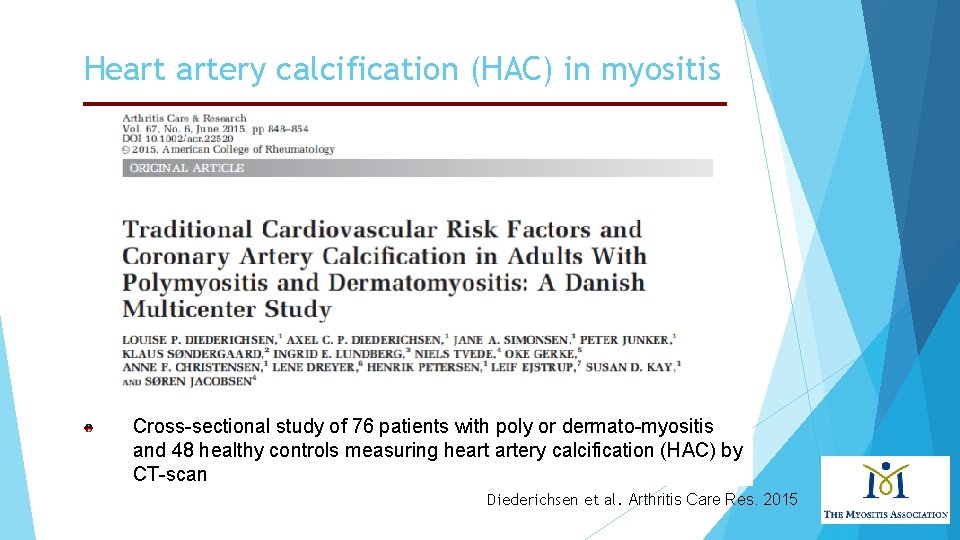
Heart artery calcification (HAC) in myositis Cross-sectional study of 76 patients with poly or dermato-myositis and 48 healthy controls measuring heart artery calcification (HAC) by CT-scan Diederichsen et al. Arthritis Care Res. 2015
Heart artery calcification (HAC) in myositis High HAC score more frequent in patients with PM/DM (20%) than in healthy controls (4%) Sectional CT images of the upper body
Heart artery calcification (HAC) in myositis 33% of the myositis patients were obese compared to 11% of the controls Hypertension and diabetes were more frequent in patients vs. controls (71 % vs. 42% and 13% vs. 0%) High HAC score not associated to the myosit disease per se, but to traditional cardiovascular risk factors as higher age and smoking
Treatment - and Your Risks to Prevent a American Heart Association, Heart Disease https: //www. heart. org Major risk factors that can’t be changed: Increasing Age Male gender Heredity Major risk factors you can modify, treat or control: Tobacco smoke Physical inactivity High blood pressure Obesity and being overweight Diabetes (High blood cholesterol) + 13
Background – disease mechanisms Inflammation of the heart muscle myocarditis Heart muscle
Myocarditis – diagnostic methods Biopsy of the heart Heart Magnetic Resonance Imaging (MRI) www. hopkinsmedicine. org
Myocarditis – Magnetic Resonance Imaging (MRI) Heart biopsy Heart MRI scanner
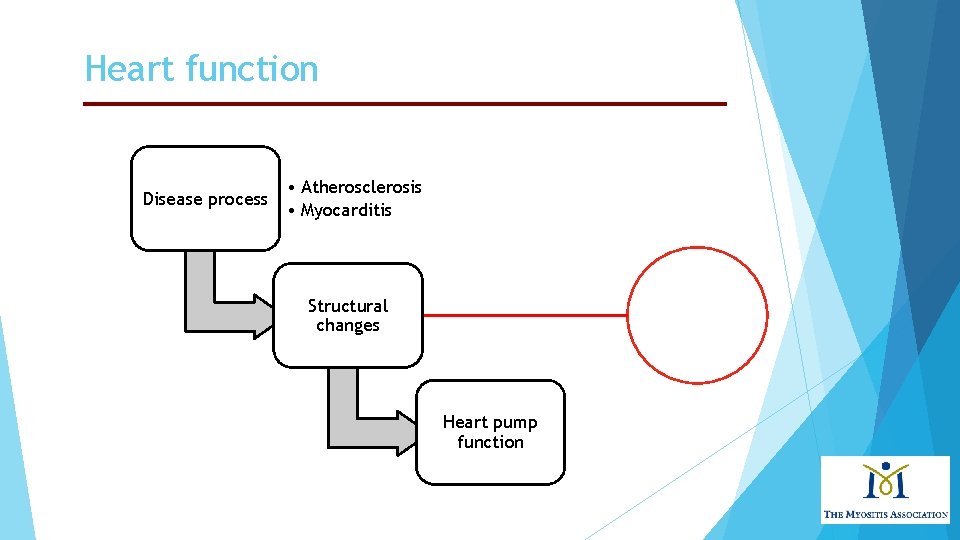
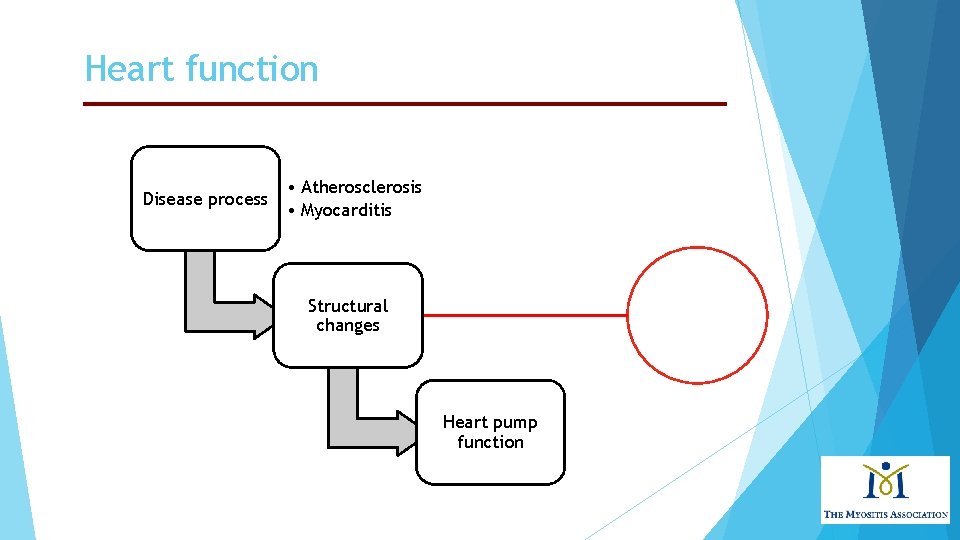
Heart function Disease process • Atherosclerosis • Myocarditis Structural changes Heart pump function
Heart function Function of the heart separated in two phases: Diastolic function (filling phase), relaxed Systolic function (pumping phase), contracted
Heart function - Echocardiography Heart function evaluated by ECHO: ultrasound measure of the heart Systolic heart function (ejection fraction (EF) Diastolic function

Systolic heart function - ECHO Systolic heart failure due to myositis is well-known, but rare The most common symptoms of heart failure are: breathlessness – this may occur after activity or at rest; it may be worse when you're lying down, and you may wake up at night needing to catch your breath fatigue – you may feel tired most of the time and find exercise exhausting swollen ankles and legs – this is caused by a build-up of fluid (oedema); it may be better in the morning and get worse later in the day Subclinical (without symptoms) systolic heart dysfunction more common American Heart Association, https: //www. heart. org
Subclinical systolic heart dysfunction 30 patients with newly diagnosed polymyositis and dermatomyositis ECHO at baseline and after 3 months of immunosuppressive treatment (Prednisolone (100%), Cyclosporine 13%) At baseline, subclinical systolic dysfunction in patients - compared to healthy controls – which normalized after 3 months of immunosuppressive treatment (Péter et al. J Reumatol. 2015)
Subclinical diastolic heart dysfunction Decreased diastolic heart function in patients with myosit compared to healthy controls, detected by ECHO Decreased diastolic heart function associated to presence of myositis autoantibodies Increased heart rhythm and conduction disturbances in patients with myosit compared to healthy controls, detected by ECG Heart findings might be induced by inflammation replaced by fibrosis, clinical significance unknown Diederichsen et al. Arthritis Care Res. 2016
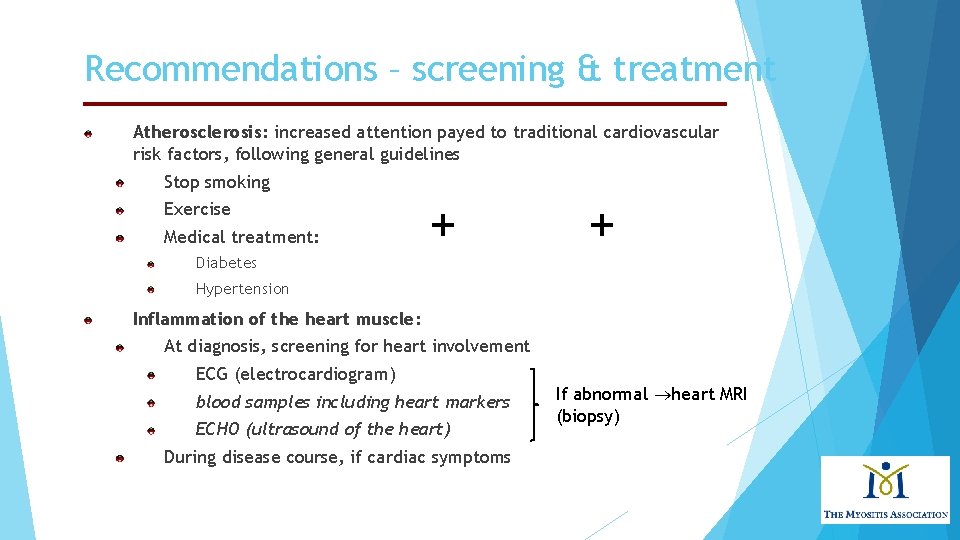
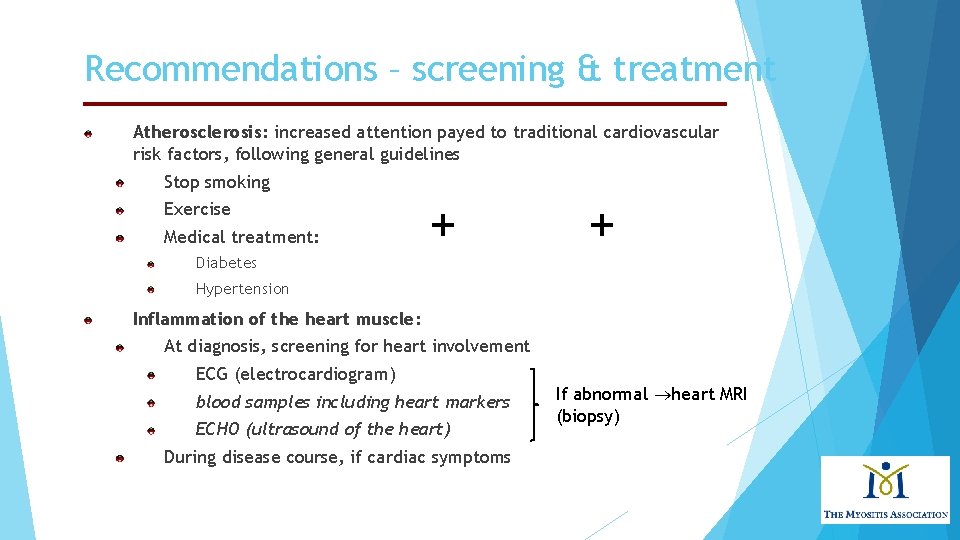
Recommendations – screening & treatment Atherosclerosis: increased attention payed to traditional cardiovascular risk factors, following general guidelines Stop smoking Exercise Medical treatment: Diabetes + + Hypertension Inflammation of the heart muscle: At diagnosis, screening for heart involvement ECG (electrocardiogram) blood samples including heart markers ECHO (ultrasound of the heart) During disease course, if cardiac symptoms If abnormal heart MRI (biopsy)
Treatment of myocarditis caused by myositis The rheumatologist/neurologist: Conventional immunosuppressive treatment of myositis Prednisolone Disease-modifying antirheumatic drugs (DMARDs): methotrexate, Azathioprine, cyclophosphamide, Mycophenolatmofetil, Rituximab, cyclosporine The cardiologist: Conventional medical treatment of heart failure and/or conduction and rythm abnormalities Global Myocardial Edema in Antisynthetase Syndrome detected and monitored by heart MRI Sado DM et al, Circulation, 2016 24
Perspectives Longitudinal studies of heart affection in larger myositis patient cohorts are needed, in an international set-up (https: //euromyositis. eu/) Prevalence and type of clinical and subclinical heart affection Cardiac biomarker(s) – autoantibodies? Treatment of heart involvement Algorithm of cardiac screening

PROJECT MYOSCL Heart Involvement and Autoantibody Profile in Myositis Sine Søndergaard Korsholm MD, future Ph. D student Center for Rheumatology and Spine Diseases Copenhagen University Hospital Copenhagen, Denmark
Primary aim To identify biomarkers for heart involvement in myositis
Heart measures Rhythm and conduction disturbances by ECG: Blood samples: Autoantibodies Cardiac damage markers: Troponins Heart structure and function by heart MRI:
Hypotheses Specific myositis-autoantibodies correlate with the presence of heart abnormalities detected by: Electrocardiogram - ECG Blood samples with heart damage markers - troponins Heart MRI Heart abnormalities detected by heart MRI are sensitive to immunosuppressive treatment
Preliminary results (DK, SE) Risk factors for ECG abnormalities in myositis and systemic sclerosis
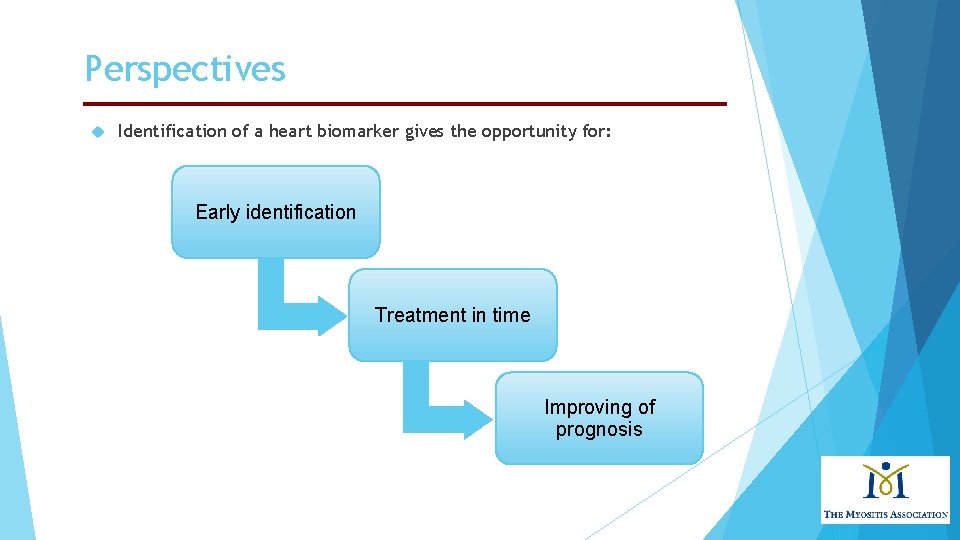
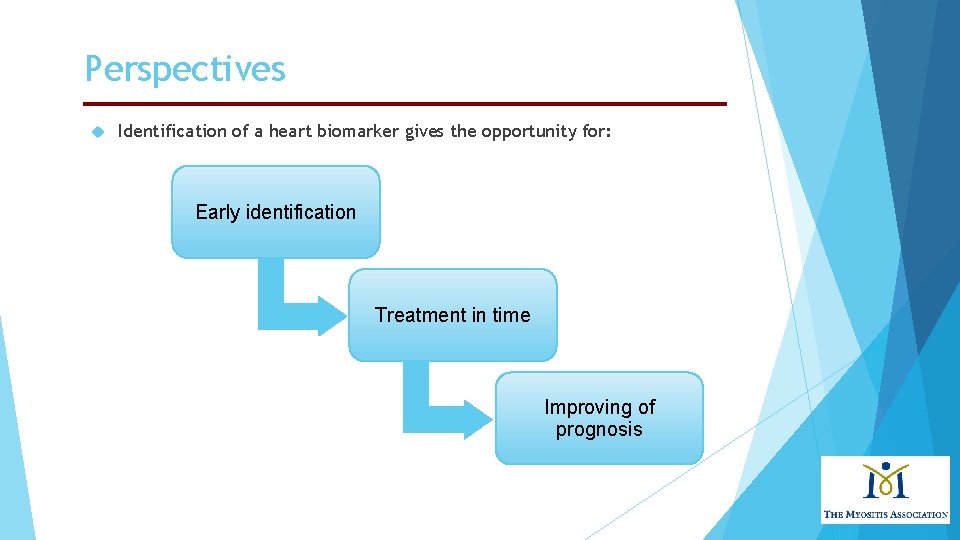
Perspectives Identification of a heart biomarker gives the opportunity for: Early identification Treatment in time Improving of prognosis
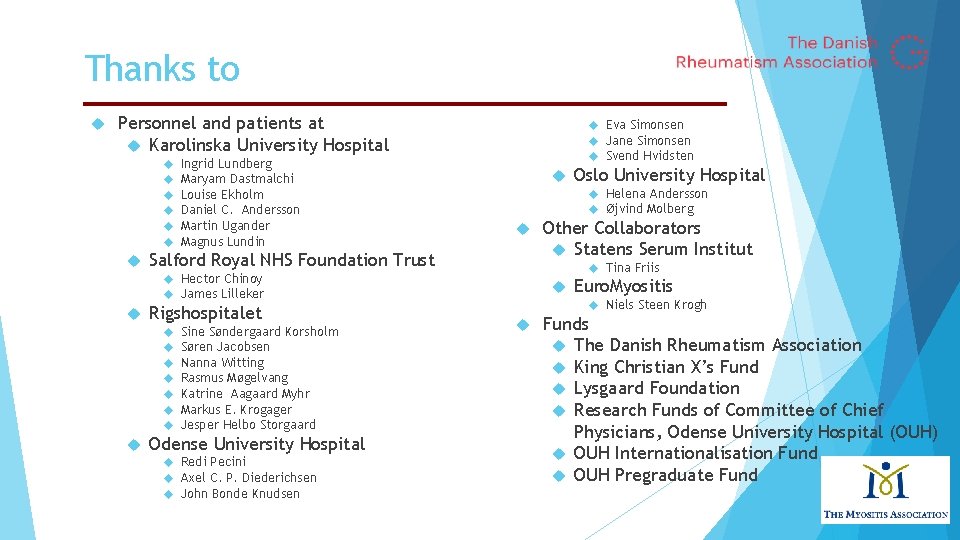
Thanks to Personnel and patients at Karolinska University Hospital Ingrid Lundberg Maryam Dastmalchi Louise Ekholm Daniel C. Andersson Martin Ugander Magnus Lundin Eva Simonsen Jane Simonsen Svend Hvidsten Helena Andersson Øjvind Molberg Salford Royal NHS Foundation Trust Rigshospitalet Sine Søndergaard Korsholm Søren Jacobsen Nanna Witting Rasmus Møgelvang Katrine Aagaard Myhr Markus E. Krogager Jesper Helbo Storgaard Odense University Hospital Redi Pecini Axel C. P. Diederichsen John Bonde Knudsen Other Collaborators Statens Serum Institut Tina Friis Hector Chinoy James Lilleker Oslo University Hospital Euro. Myositis Niels Steen Krogh Funds The Danish Rheumatism Association King Christian X’s Fund Lysgaard Foundation Research Funds of Committee of Chief Physicians, Odense University Hospital (OUH) OUH Internationalisation Fund OUH Pregraduate Fund

Thank you for your attention! Louise Pyndt Diederichsen, MD, Ph. D Center for Rheumatology and Spine Diseases Copenhagen University Hospital Rigshospitalet Copenhagen, Denmark
 Imacs myositis
Imacs myositis Muscles of mastication
Muscles of mastication Communicable disease and non communicable disease
Communicable disease and non communicable disease Differential cyanosis
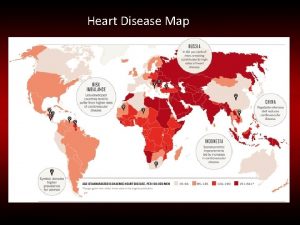
Differential cyanosis Heart disease and stroke are the world's biggest killers
Heart disease and stroke are the world's biggest killers Heart disease symptoms
Heart disease symptoms Randi sokol
Randi sokol Footbal player wordle
Footbal player wordle Tetralogy of fallot xray
Tetralogy of fallot xray Tet spell
Tet spell Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy Heart disease data
Heart disease data Ie
Ie Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Lvvo heart
Lvvo heart 5 terrible ts
5 terrible ts Upper lobe venous diversion
Upper lobe venous diversion Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Dopamine uses
Dopamine uses Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Right sided heart failure
Right sided heart failure Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Causes of valvular heart disease
Causes of valvular heart disease Beau's lines autoimmune disease
Beau's lines autoimmune disease Causes of valvular heart disease
Causes of valvular heart disease Farah garmany
Farah garmany Fish mouth buttonhole stenosis
Fish mouth buttonhole stenosis Rhuematic fever
Rhuematic fever Coronary heart disease
Coronary heart disease Ischemic heart disease classification
Ischemic heart disease classification Rheumatic heart disease
Rheumatic heart disease Rheumatic heart disease causes
Rheumatic heart disease causes Ischemic heart disease
Ischemic heart disease Aortic heart disease
Aortic heart disease