Myocardial Infarction Dr T A DIALLO Definition According


- Slides: 24

Myocardial Infarction Dr T A DIALLO
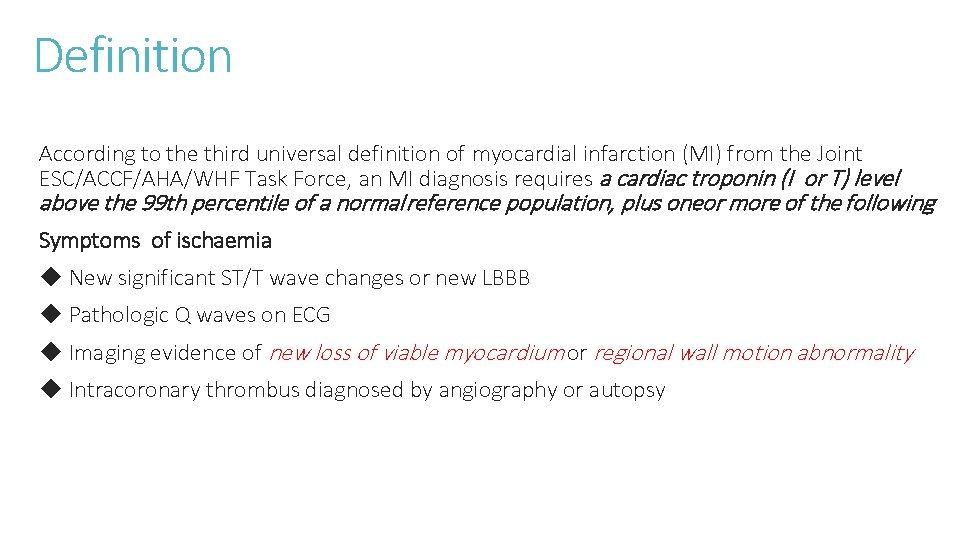
Definition According to the third universal definition of myocardial infarction (MI) from the Joint ESC/ACCF/AHA/WHF Task Force, an MI diagnosis requires a cardiac troponin (I or T) level above the 99 th percentile of a normal reference population, plus oneor more of the following Symptoms of ischaemia ◆ New significant ST/T wave changes or new LBBB ◆ Pathologic Q waves on ECG ◆ Imaging evidence of new loss of viable myocardium or regional wall motion abnormality ◆ Intracoronary thrombus diagnosed by angiography or autopsy
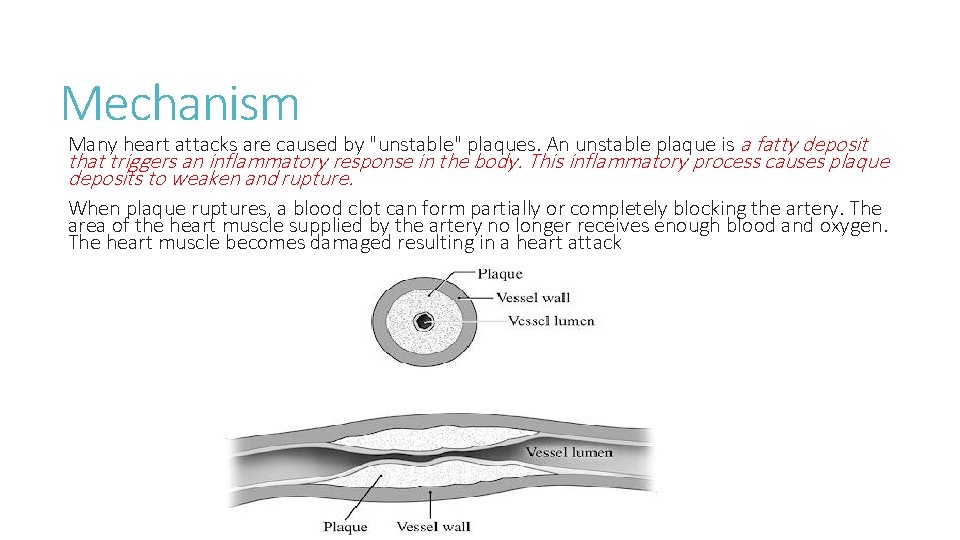
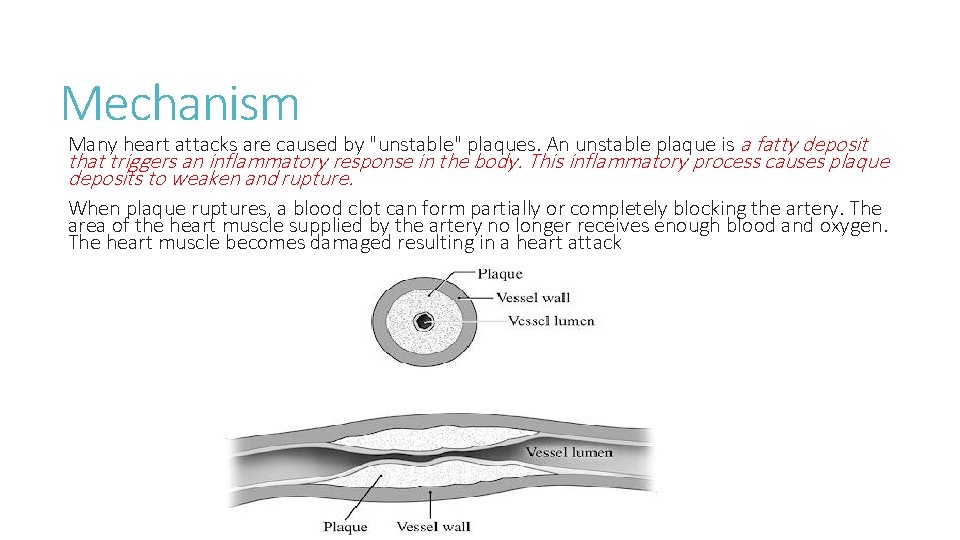
Mechanism Many heart attacks are caused by "unstable" plaques. An unstable plaque is a fatty deposit that triggers an inflammatory response in the body. This inflammatory process causes plaque deposits to weaken and rupture. When plaque ruptures, a blood clot can form partially or completely blocking the artery. The area of the heart muscle supplied by the artery no longer receives enough blood and oxygen. The heart muscle becomes damaged resulting in a heart attack
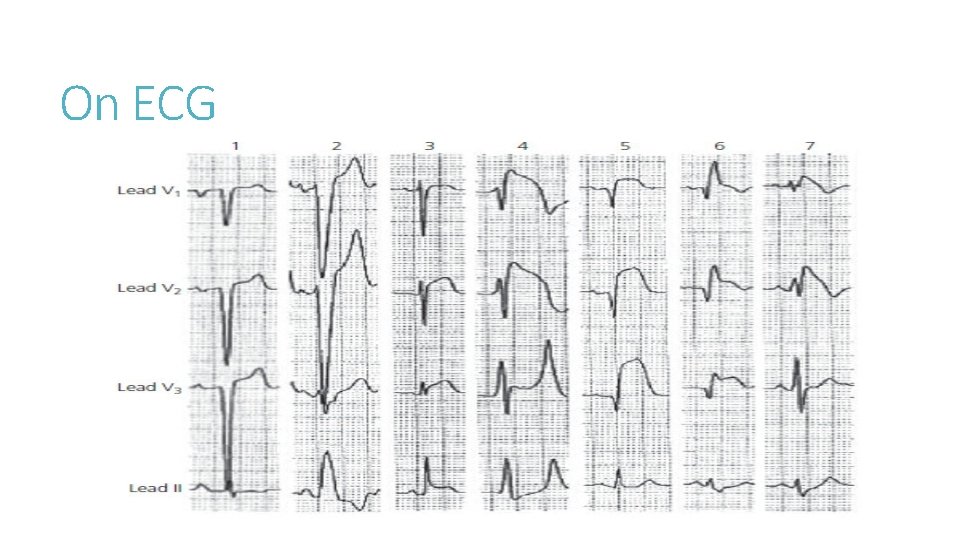
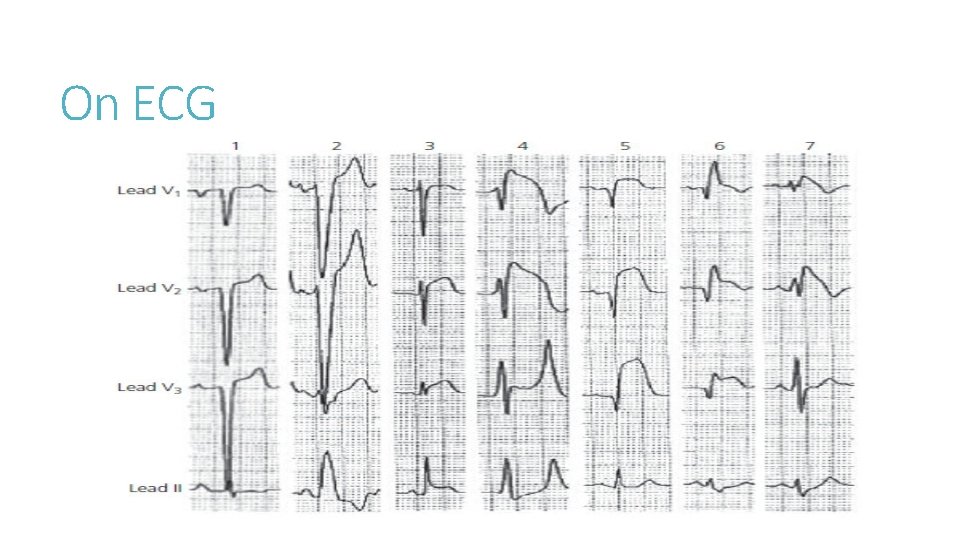
On ECG
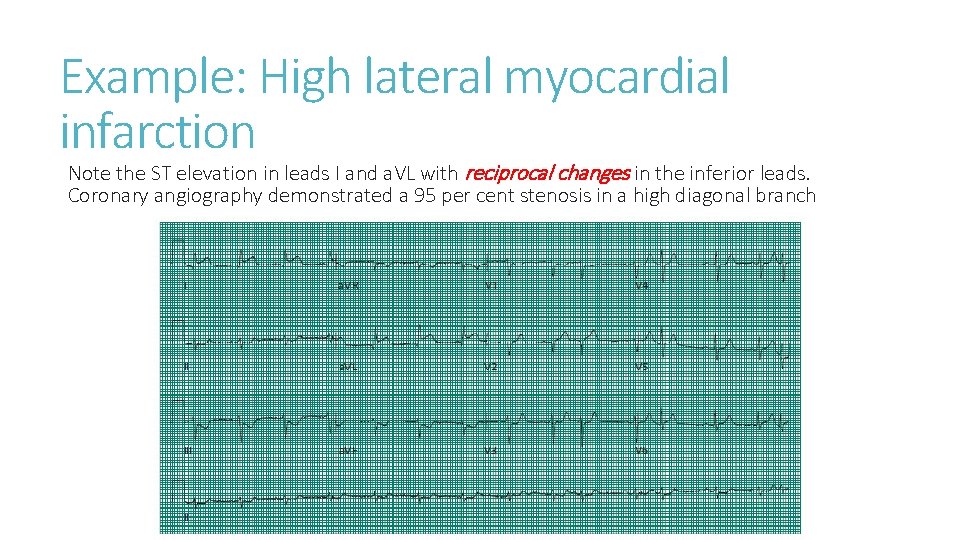
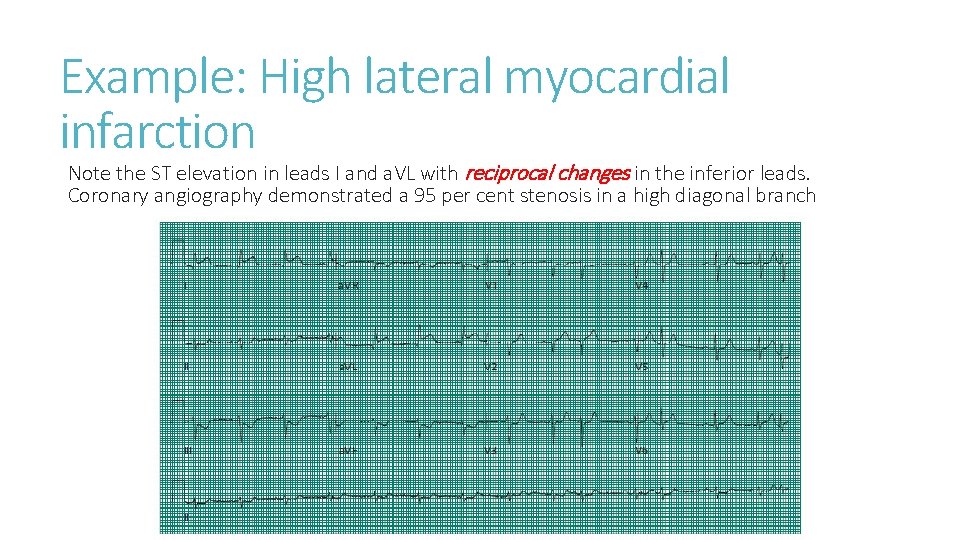
Example: High lateral myocardial infarction Note the ST elevation in leads I and a. VL with reciprocal changes in the inferior leads. Coronary angiography demonstrated a 95 per cent stenosis in a high diagonal branch
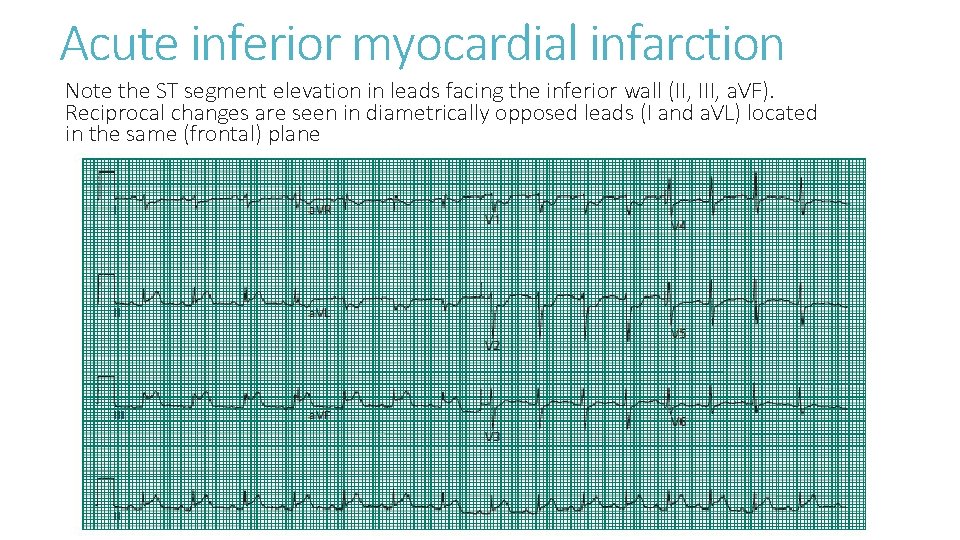
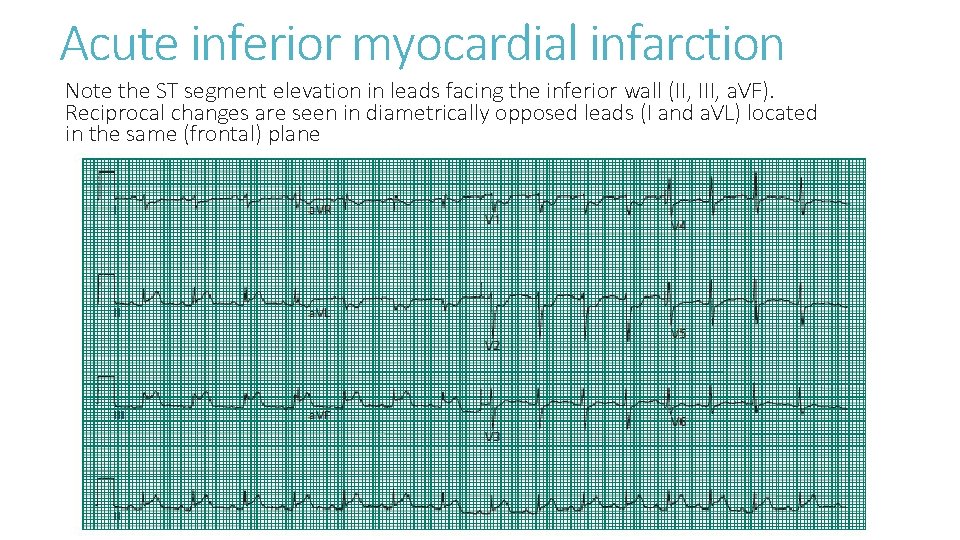
Acute inferior myocardial infarction Note the ST segment elevation in leads facing the inferior wall (II, III, a. VF). Reciprocal changes are seen in diametrically opposed leads (I and a. VL) located in the same (frontal) plane
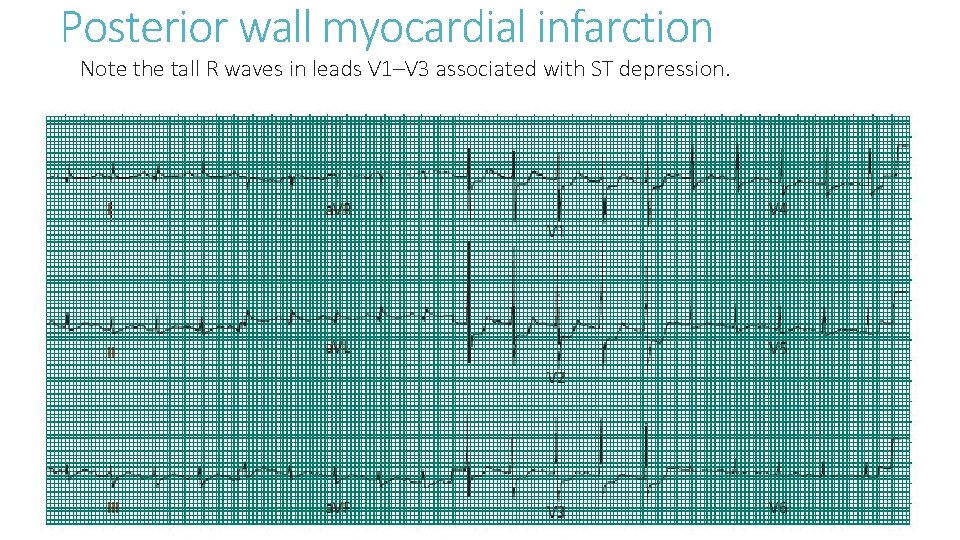
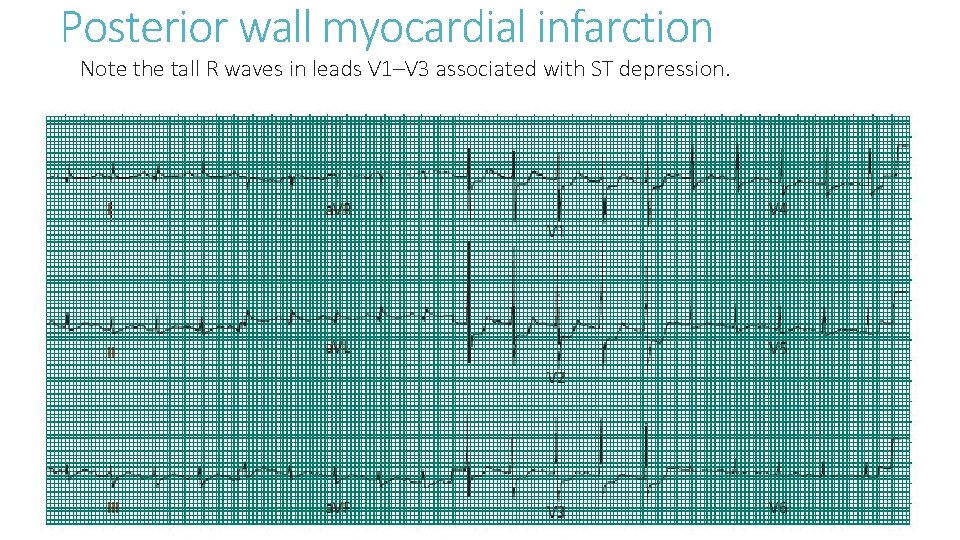
Posterior wall myocardial infarction Note the tall R waves in leads V 1–V 3 associated with ST depression.
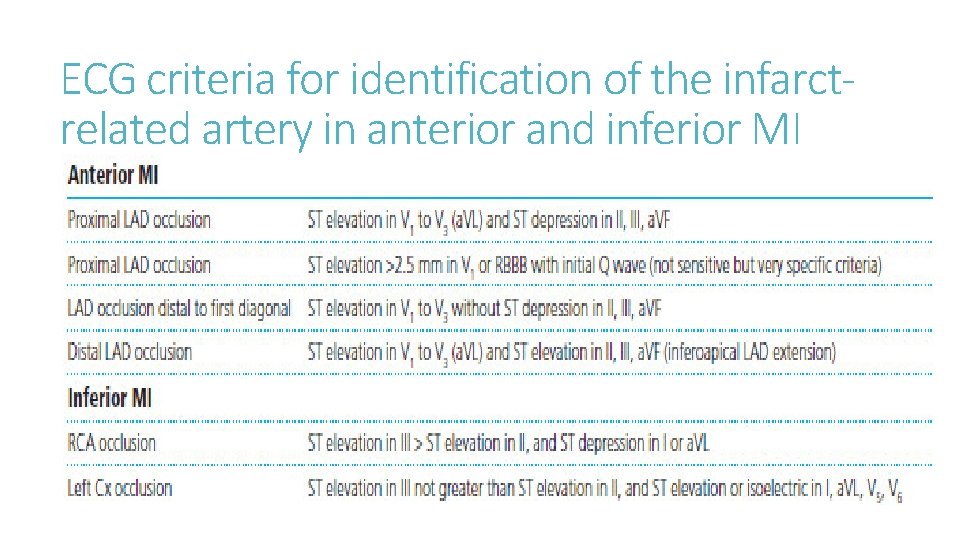
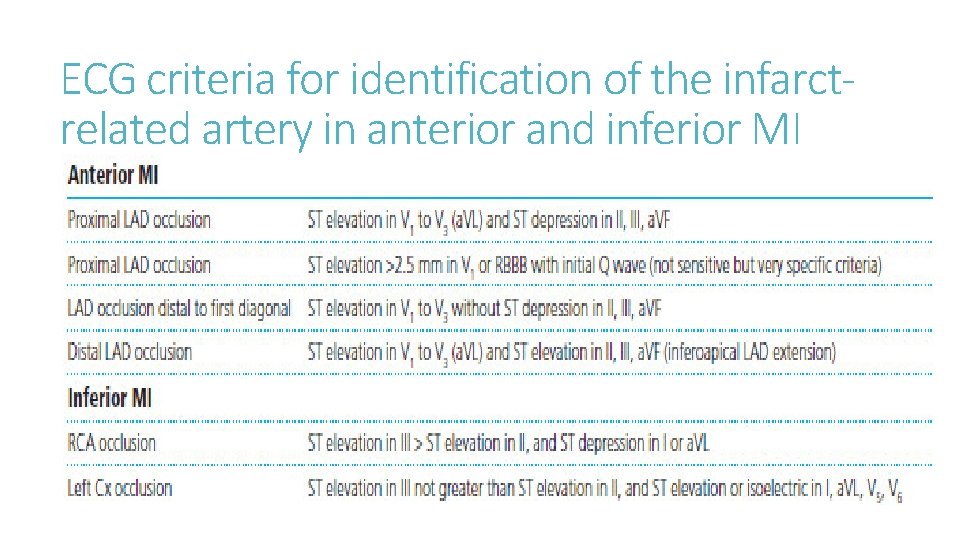
ECG criteria for identification of the infarctrelated artery in anterior and inferior MI
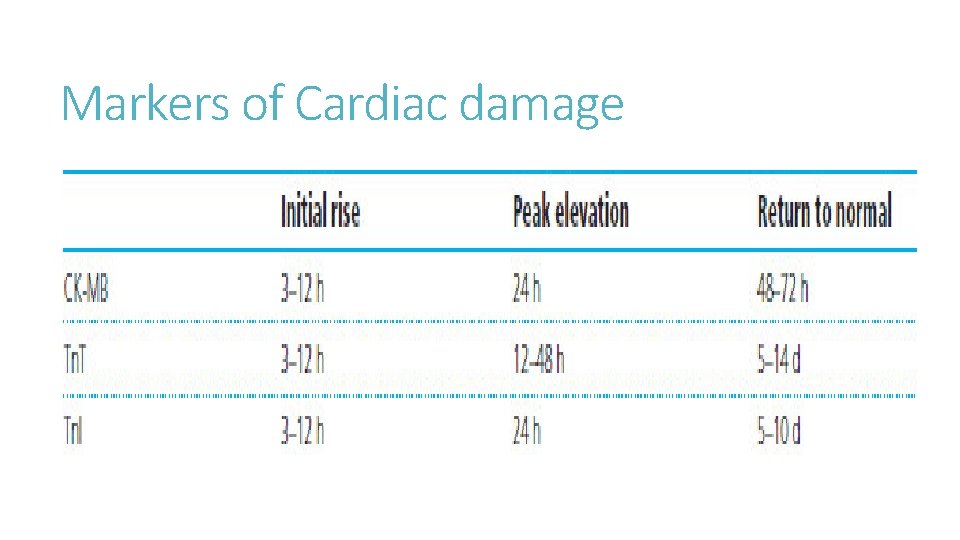
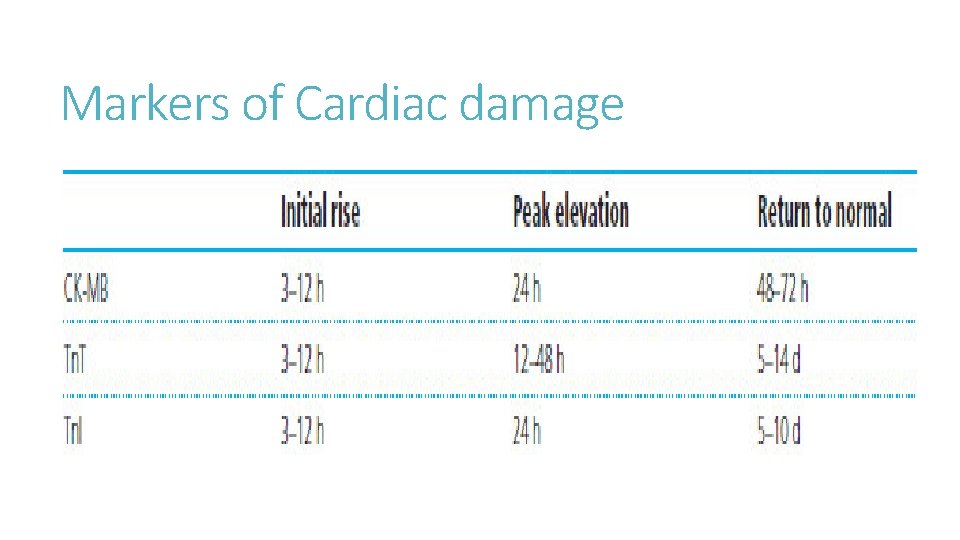
Markers of Cardiac damage
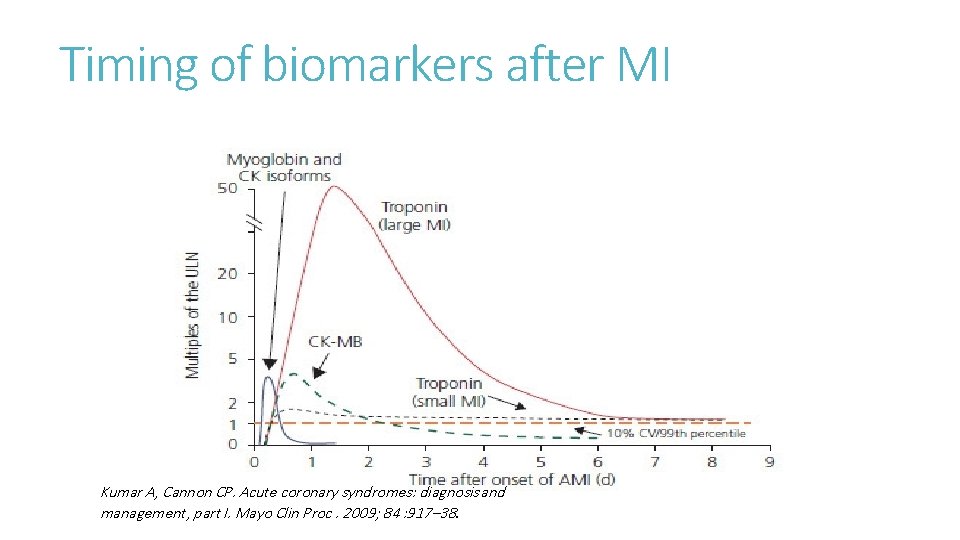
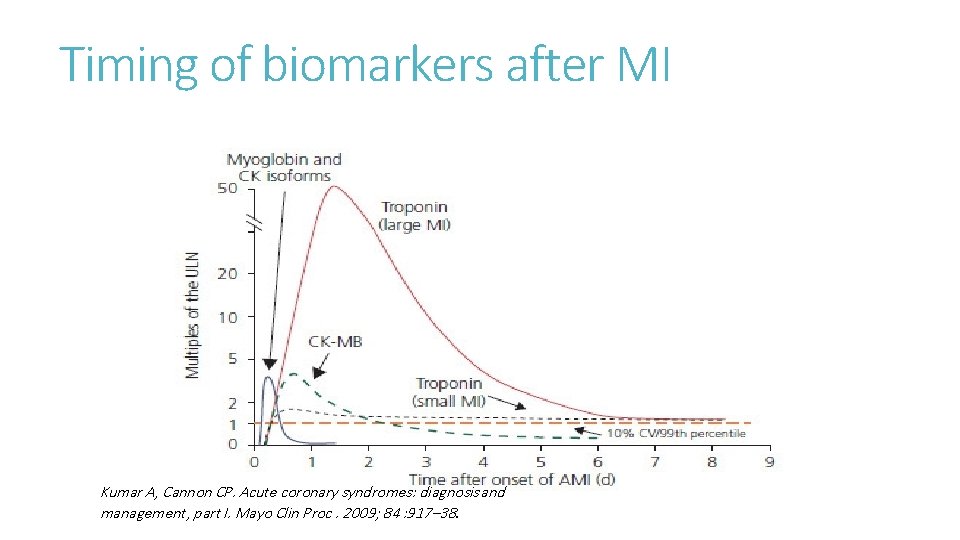
Timing of biomarkers after MI Kumar A, Cannon CP. Acute coronary syndromes: diagnosis and management, part I. Mayo Clin Proc. 2009; 84 : 917– 38.
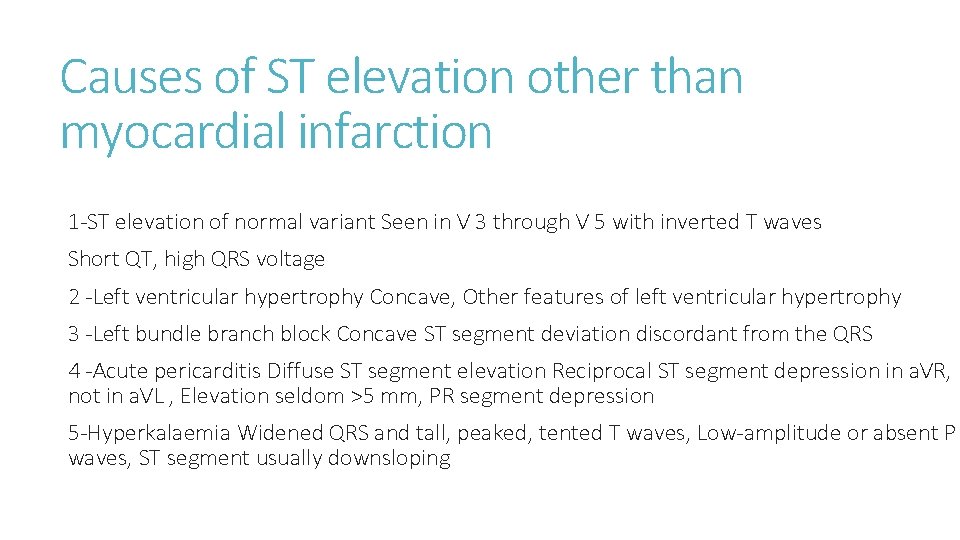
Causes of ST elevation other than myocardial infarction 1 -ST elevation of normal variant Seen in V 3 through V 5 with inverted T waves Short QT, high QRS voltage 2 -Left ventricular hypertrophy Concave, Other features of left ventricular hypertrophy 3 -Left bundle branch block Concave ST segment deviation discordant from the QRS 4 -Acute pericarditis Diffuse ST segment elevation Reciprocal ST segment depression in a. VR, not in a. VL , Elevation seldom >5 mm, PR segment depression 5 -Hyperkalaemia Widened QRS and tall, peaked, tented T waves, Low-amplitude or absent P waves, ST segment usually downsloping
Other investigations -Elevation of WBC occurs within the first 2 hours, reaches a peak 2 to 4 days after infarction (12– 15 × 10 3 /m. L), and returns to normal in 1 week. -ESR rises after the second day and remains elevated for several weeks. -Haemoglobin powerfully predicts cardiovascular events, with mortality increasing progressively as values fall below 14 mg/d. L or increase above 17 mg/d. L. -Iatrogenic bleeding is associated with a 5 -fold increase in mortality. -There is a fall of HDL cholesterol after 48 h; thus, a lipid profile should be obtained before that time or 8 weeks after the MI
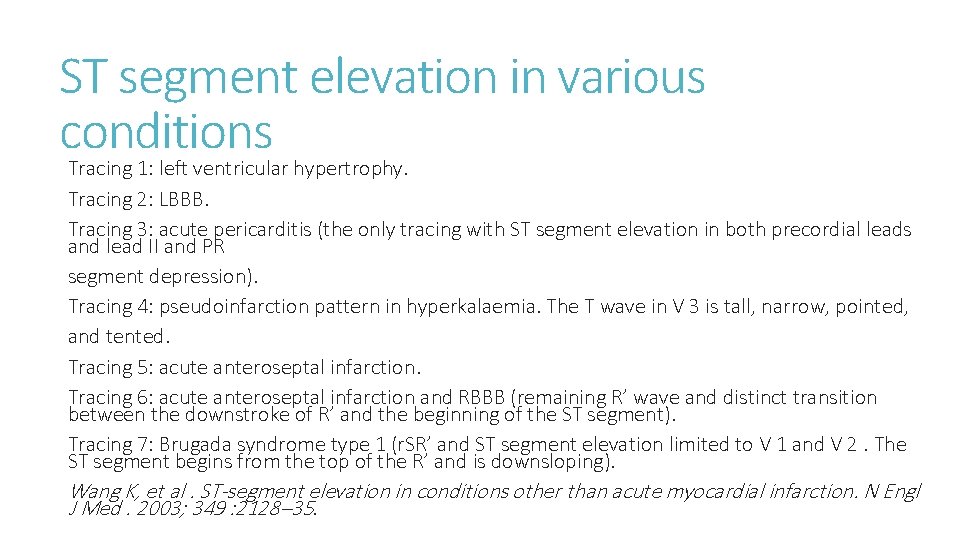
ST segment elevation in various conditions Tracing 1: left ventricular hypertrophy. Tracing 2: LBBB. Tracing 3: acute pericarditis (the only tracing with ST segment elevation in both precordial leads and lead II and PR segment depression). Tracing 4: pseudoinfarction pattern in hyperkalaemia. The T wave in V 3 is tall, narrow, pointed, and tented. Tracing 5: acute anteroseptal infarction. Tracing 6: acute anteroseptal infarction and RBBB (remaining R’ wave and distinct transition between the downstroke of R’ and the beginning of the ST segment). Tracing 7: Brugada syndrome type 1 (r. SR’ and ST segment elevation limited to V 1 and V 2. The ST segment begins from the top of the R’ and is downsloping). Wang K, et al. ST-segment elevation in conditions other than acute myocardial infarction. N Engl J Med. 2003; 349 : 2128– 35.
Continued 6 -Brugada syndrome (type 1) r. SR’ in V 1 and V 2, ST segment elevation in V 1 and V 2 , typically downsloping 7 - Pulmonary embolism Changes simulating myocardial infarction seen often in both inferior and anteroseptal leads 8 - Cardioversion Striking ST segment elevation, often >10 mm, but lasting only 1 or 2 min immediately after directcurrent shock 9 -Prinzmetal’s angina Same as ST segment elevation in infarction but transient 10 - Hiatus hernia and stomach compression Concave elevation in anterior chest leads without reciprocal inferior ST depression Modified from Wang K, et al. ST segment elevation in conditions other than acute myocardial infarction. N Engl J Med. 2003; 349 : 2128– 35 and Gard JJ, et al. Uncommon cause of ST elevation. Circulation 2011; 123 : e 259–e 261.
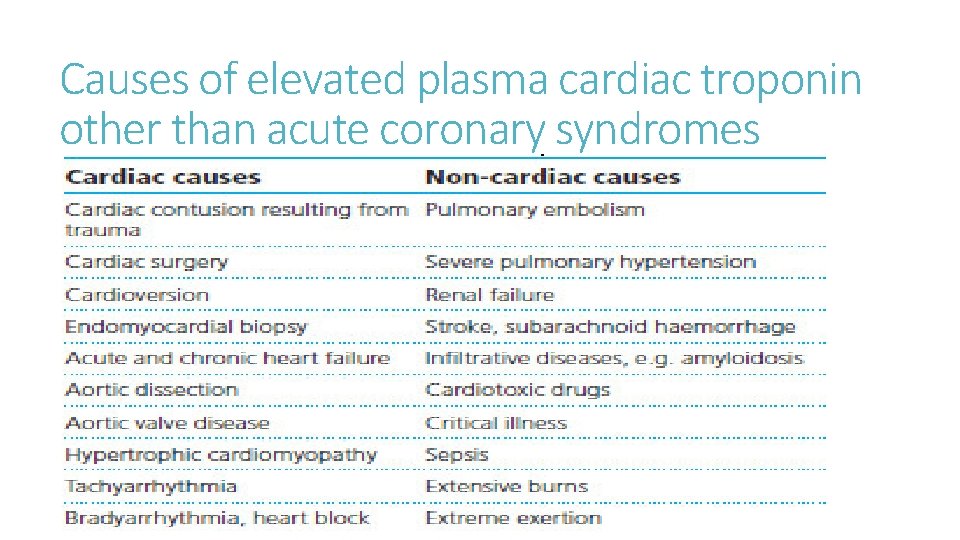
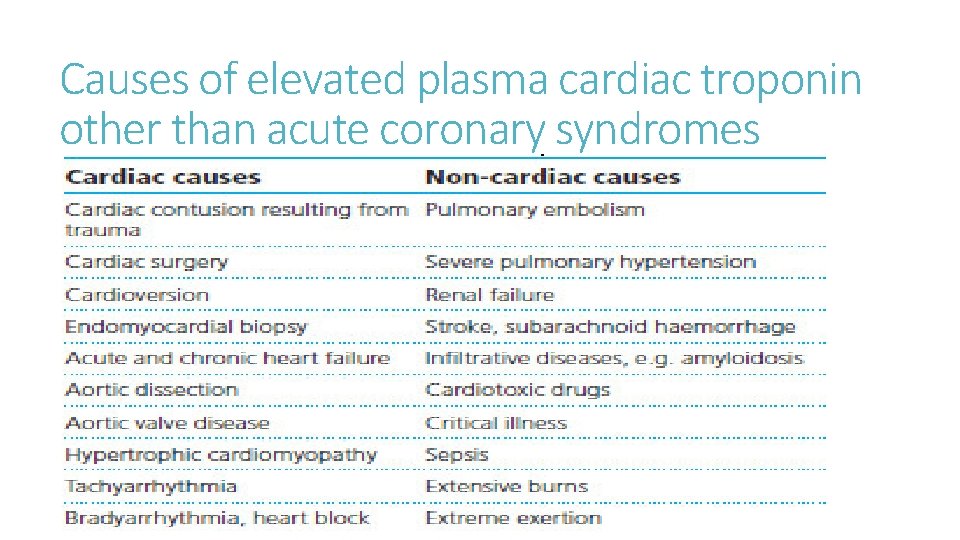
Causes of elevated plasma cardiac troponin other than acute coronary syndromes
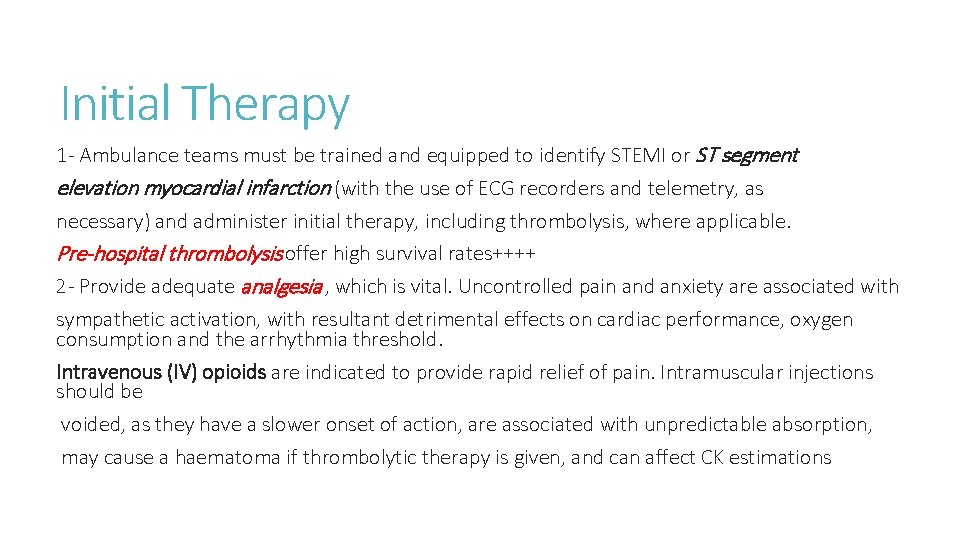
Initial Therapy 1 - Ambulance teams must be trained and equipped to identify STEMI or ST segment elevation myocardial infarction (with the use of ECG recorders and telemetry, as necessary) and administer initial therapy, including thrombolysis, where applicable. Pre-hospital thrombolysis offer high survival rates++++ 2 - Provide adequate analgesia , which is vital. Uncontrolled pain and anxiety are associated with sympathetic activation, with resultant detrimental effects on cardiac performance, oxygen consumption and the arrhythmia threshold. Intravenous (IV) opioids are indicated to provide rapid relief of pain. Intramuscular injections should be voided, as they have a slower onset of action, are associated with unpredictable absorption, may cause a haematoma if thrombolytic therapy is given, and can affect CK estimations
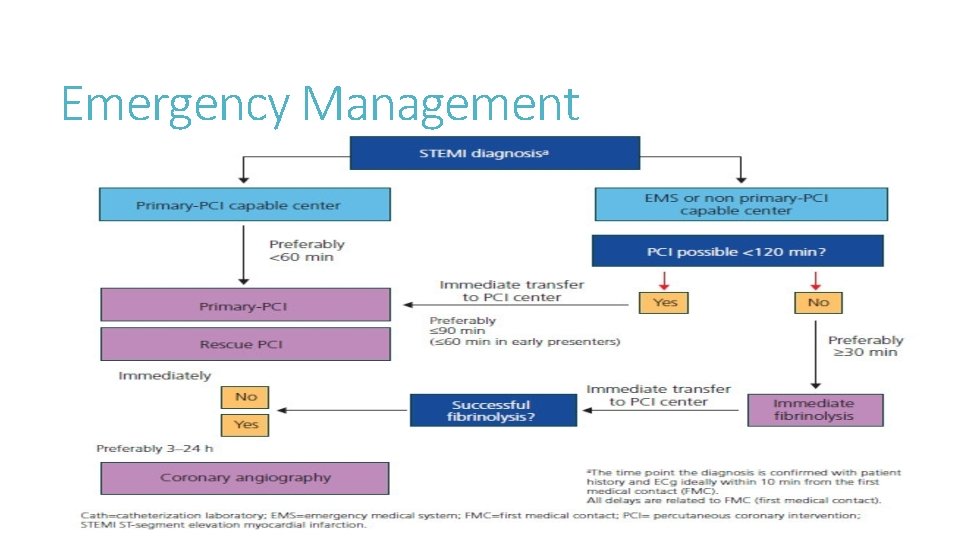
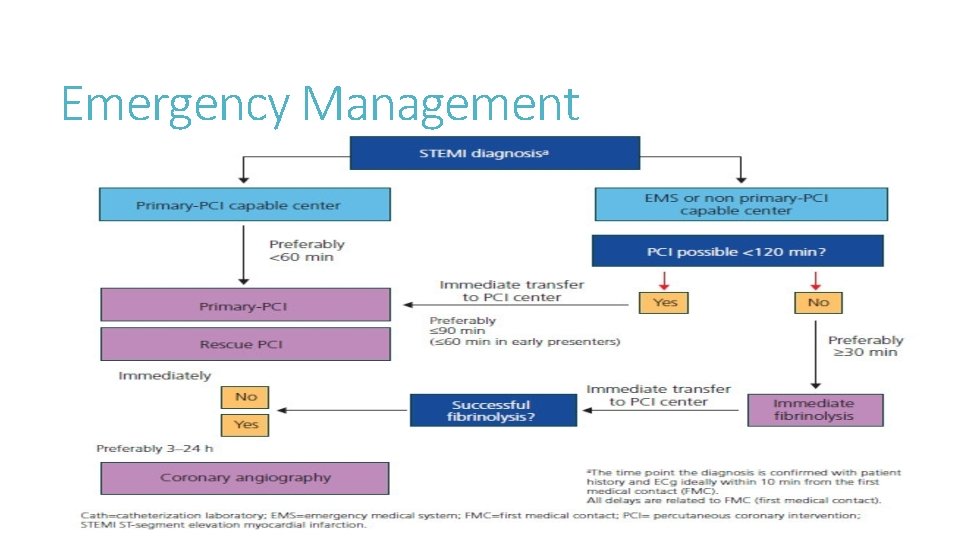
Emergency Management
Selection of thrombolytic agents 1 -streptokinase, the oldest thrombolytic 2 -Newer plasminogen activators, produced by bioengineering techniques: Fibrin-specific compounds, reteplase (r-PA) and tenecteplase (TNK), have longer half lives than the original compound, allowing for single or double bolus administration -Inclusion criteria: Presentation within 12 hours of onset of ischaemic cardiac pain in a patient with: – ST segment elevation of at least 2 mm in two adjacent chest leads – ST segment elevation of 1 mm in two adjacent limb leads – true posterior infarction or new bundle branch block
Thrombolytics 2 -Exclusion criteria, regarded as relative, to be interpreted within the clinical context. Criteria include: • known coagulation disorder, including uncontrolled anticoagulation therapy • active peptic ulceration, varices or recent GI haemorrhage (dyspepsia alone is not a contraindication) • severe hypertension (systolic >180 mm. Hg and/or diastolic >110 mm. Hg) • traumatic cardiopulmonary resuscitation (CPR) (CPR performed by trained staff is not regarded as a contraindication) • recent internal bleeding from any site (menstruation is not an absolute contraindication) • previous haemorrhagic stroke at any time
Medication All patients should receive: ◆ Aspirin (unless there is true aspirin allergy), ◆ A P 2 Y inhibitor, such as clopidogrel, ticagrelor or prasugrel (especially for PCI) An antithrombin agent (enoxaparin or unfractionated heparin or bivalirudin or fondaparinux). ◆ -Morphine sulphate 2– 8 mg IV, repeated at 5– 15 min intervals, or diamorphine (5 mg IV, causes less nausea) are the analgesics of choice in acute MI). -Oxygen (4– 5 L/min), especially when saturation is <90%. (Fondaparinux is a synthetic factor Xa inhibitor, has been found to reduce 30 -day death or myocardial infarction compared to unfractionated heparin, regardless of administration of fibrinolysis)
Other medications 1 -Glycoprotein IIb/IIIa inhibitors are mainly used for primary PCI (and can be deferred until angiography) or in combination with half-dose fibrinolysis 2 -The use of early intravenous beta blockers in acute MI reduces the risks of re-infarction and ventricular fibrillation but increases the risk of cardiogenic shock, especially during the first day or so after admission
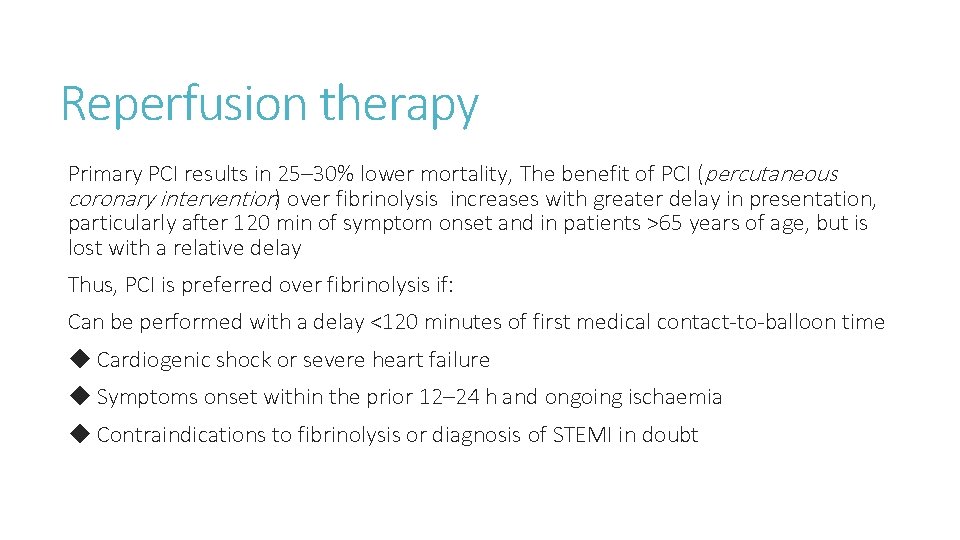
Reperfusion therapy Primary PCI results in 25– 30% lower mortality, The benefit of PCI (percutaneous coronary intervention) over fibrinolysis increases with greater delay in presentation, particularly after 120 min of symptom onset and in patients >65 years of age, but is lost with a relative delay Thus, PCI is preferred over fibrinolysis if: Can be performed with a delay <120 minutes of first medical contact-to-balloon time ◆ Cardiogenic shock or severe heart failure ◆ Symptoms onset within the prior 12– 24 h and ongoing ischaemia ◆ Contraindications to fibrinolysis or diagnosis of STEMI in doubt
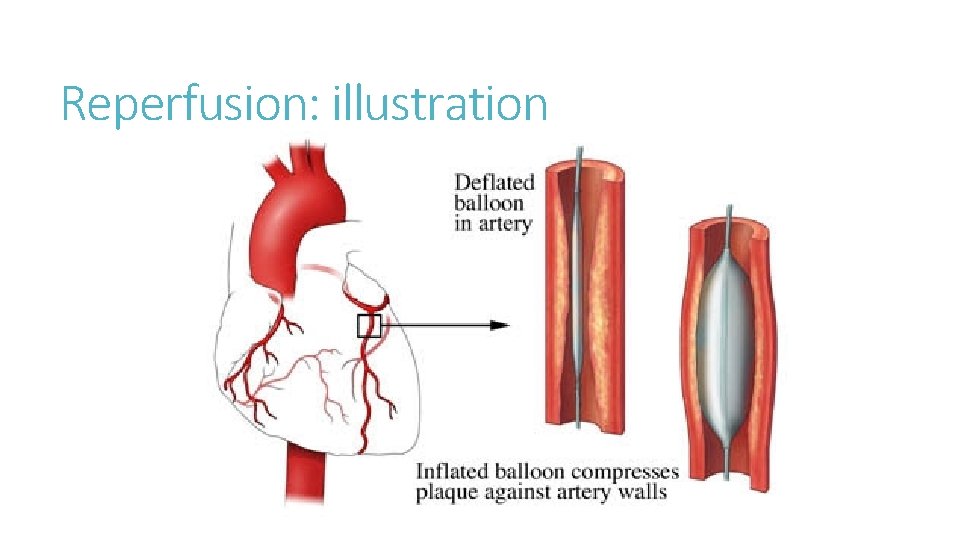
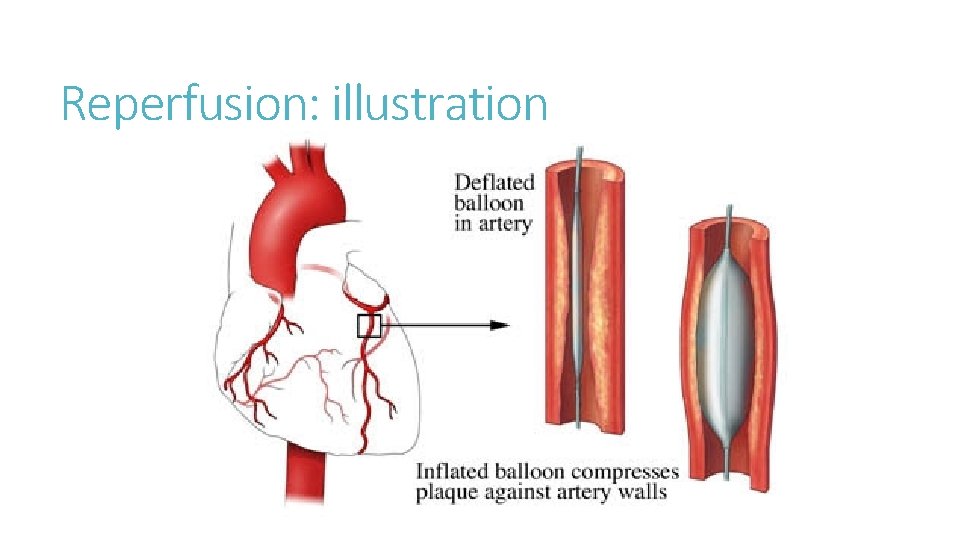
Reperfusion: illustration
