Myocardial Infarction Blood tests for diagnosis Dr Esm
Myocardial Infarction: Blood tests for diagnosis Dr Esmé Hitchcock CHEMICAL PATHOLOGIST
Myocardial Infarction Oxygen starvation & cell death of heart muscle, caused by interrupted blood supply due to occlusion of a coronary artery.
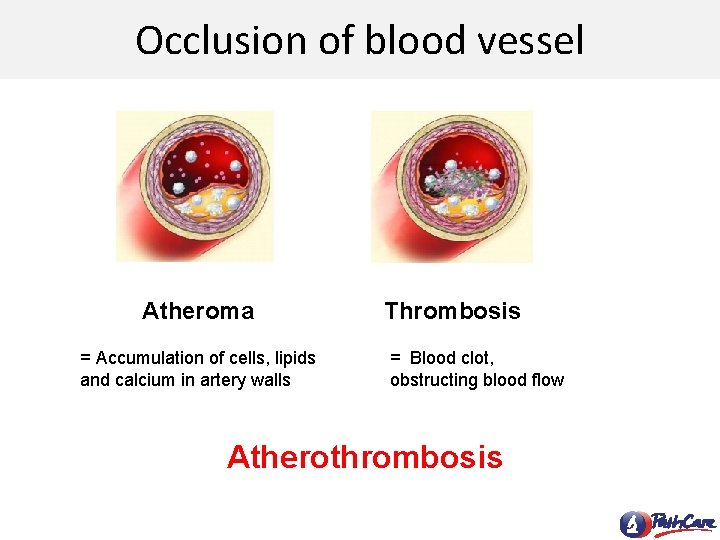
Occlusion of blood vessel Atheroma = Accumulation of cells, lipids and calcium in artery walls Thrombosis = Blood clot, obstructing blood flow Atherothrombosis
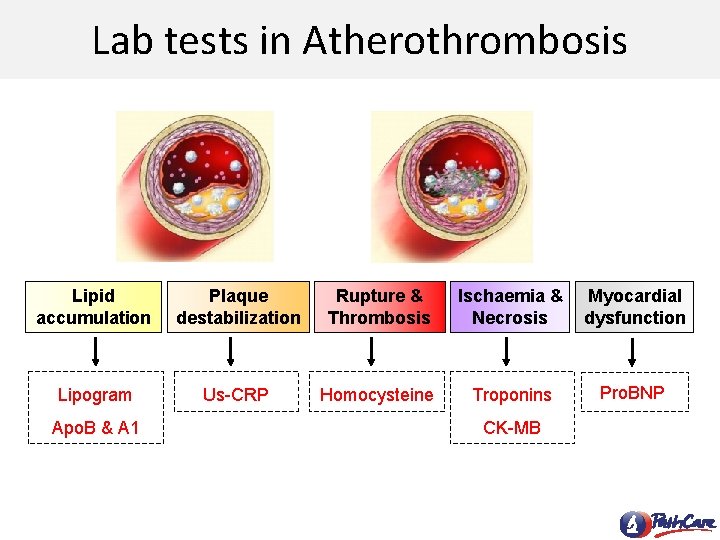
Lab tests in Atherothrombosis Lipid accumulation Plaque destabilization Rupture & Thrombosis Ischaemia & Necrosis Myocardial dysfunction Lipogram Us-CRP Homocysteine Troponins Pro. BNP Apo. B & A 1 CK-MB
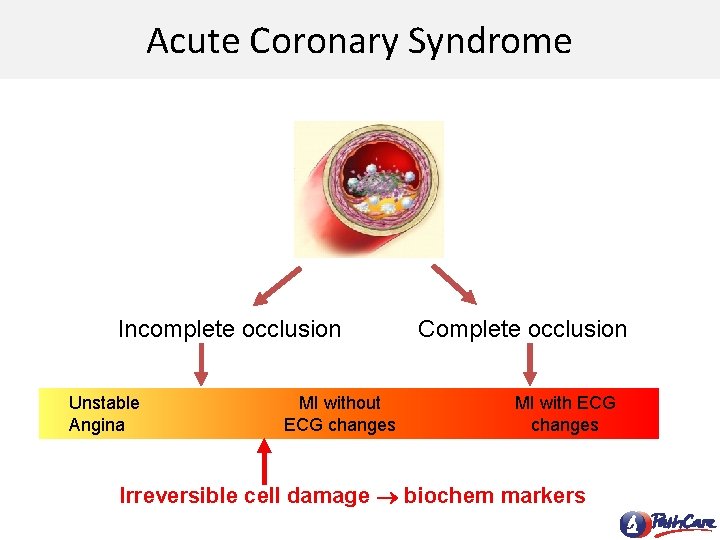
Acute Coronary Syndrome Incomplete occlusion Unstable Angina MI without ECG changes Complete occlusion MI with ECG changes Irreversible cell damage biochem markers

Biochemical markers • Molecules released into blood from damaged heart tissue. • Cardiac Markers: – CK-MB mass – Troponin T or Troponin I – gold standard for detecting myocardial damage
CK-MB mass • Muscle enzyme – Highest concentration in heart – Small amounts in skeletal muscle • Relative early marker – Starts to rise 3 -6 h after MI – Back to normal in 3 -4 days • Not entirely Cardiac Specific: – May rise with significant amount of skeletal muscle damage
Troponin • Forms part of the protein complex that regulates muscle contraction. Striated muscle
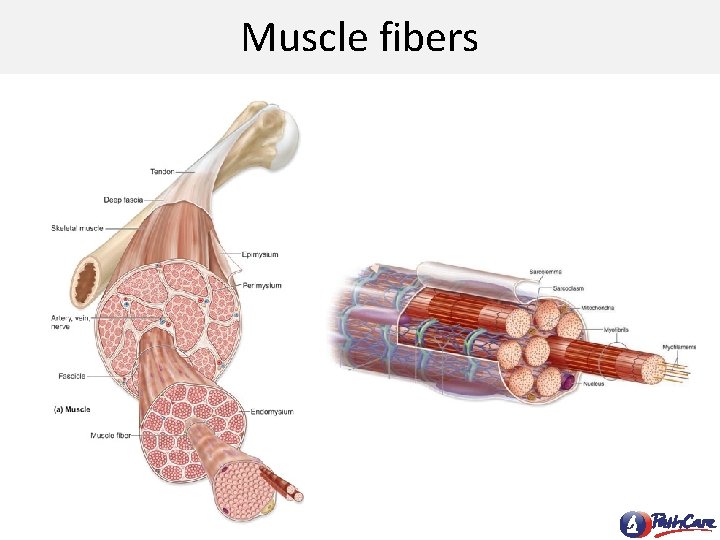
Muscle fibers
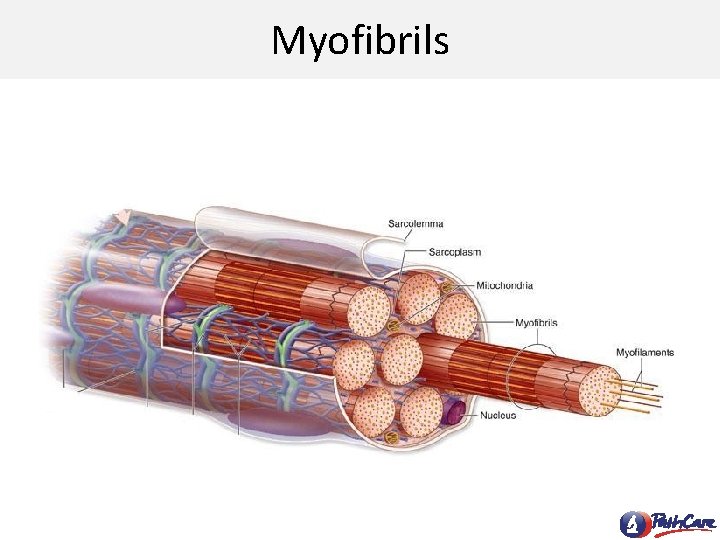
Myofibrils
Myofilaments
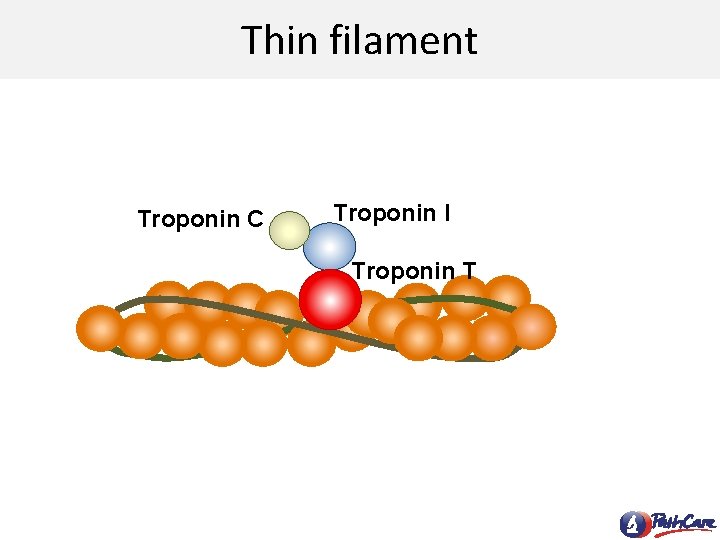
Thin filament Troponin C Troponin I Troponin T
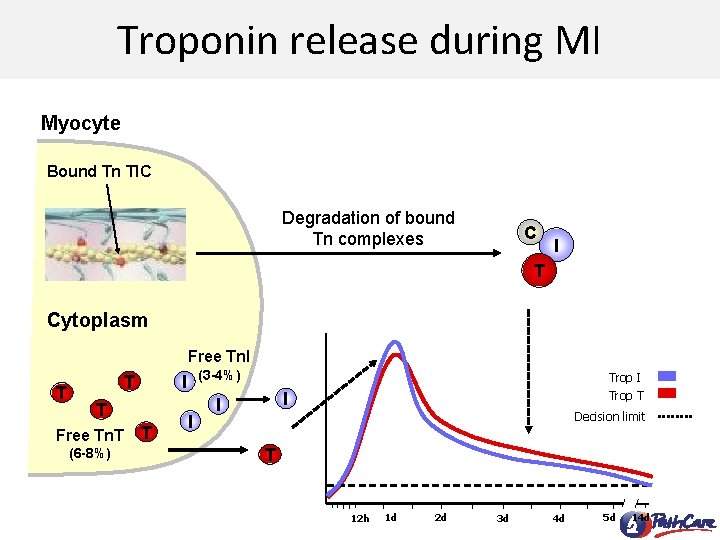
Troponin release during MI Myocyte Bound Tn TIC Degradation of bound Tn complexes C I T Cytoplasm Free Tn. I T T T Free Tn. T (6 -8%) (3 -4%) I Trop T I I Decision limit T 12 h 1 d 2 d 3 d 4 d 5 d 14 d
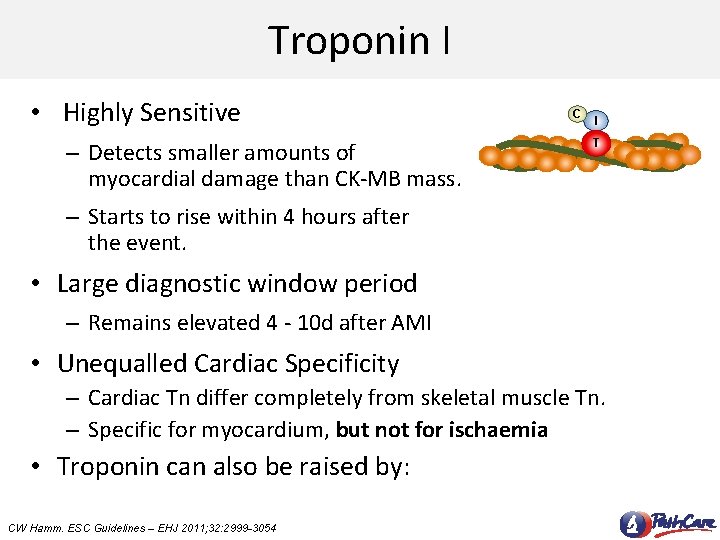
Troponin I • Highly Sensitive – Detects smaller amounts of myocardial damage than CK-MB mass. C I T – Starts to rise within 4 hours after the event. • Large diagnostic window period – Remains elevated 4 - 10 d after AMI • Unequalled Cardiac Specificity – Cardiac Tn differ completely from skeletal muscle Tn. – Specific for myocardium, but not for ischaemia • Troponin can also be raised by: CW Hamm. ESC Guidelines – EHJ 2011; 32: 2999 -3054
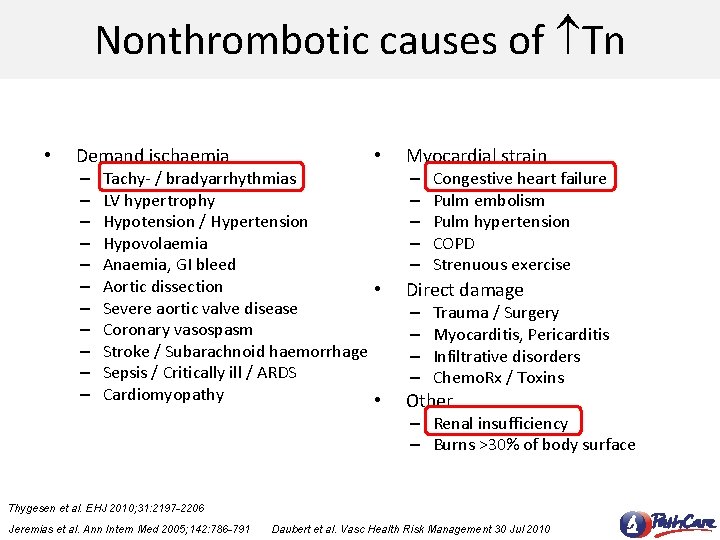
Nonthrombotic causes of Tn • Demand ischaemia – – – • Tachy- / bradyarrhythmias LV hypertrophy Hypotension / Hypertension Hypovolaemia Anaemia, GI bleed Aortic dissection • Severe aortic valve disease Coronary vasospasm Stroke / Subarachnoid haemorrhage Sepsis / Critically ill / ARDS Cardiomyopathy • Myocardial strain – – – Congestive heart failure Pulm embolism Pulm hypertension COPD Strenuous exercise Direct damage – – Trauma / Surgery Myocarditis, Pericarditis Infiltrative disorders Chemo. Rx / Toxins Other – Renal insufficiency – Burns >30% of body surface Thygesen et al. EHJ 2010; 31: 2197 -2206 Jeremias et al. Ann Intern Med 2005; 142: 786 -791 Daubert et al. Vasc Health Risk Management 30 Jul 2010
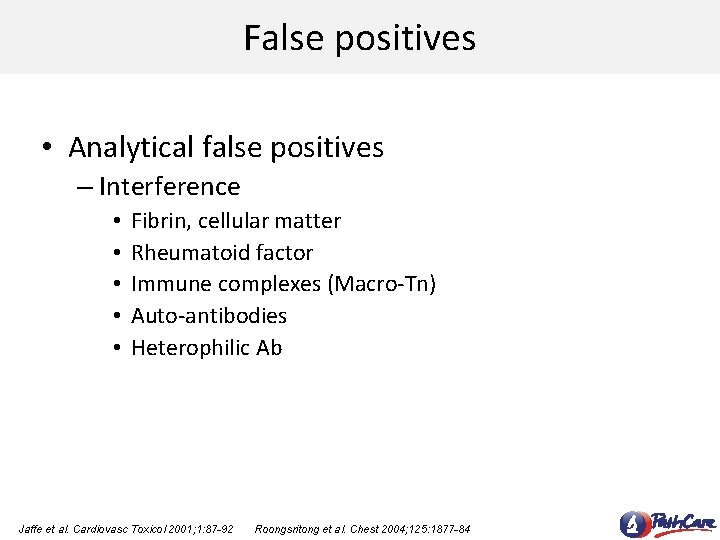
False positives • Analytical false positives – Interference • • • Fibrin, cellular matter Rheumatoid factor Immune complexes (Macro-Tn) Auto-antibodies Heterophilic Ab Jaffe et al. Cardiovasc Toxicol 2001; 1: 87 -92 Roongsritong et al. Chest 2004; 125: 1877 -84
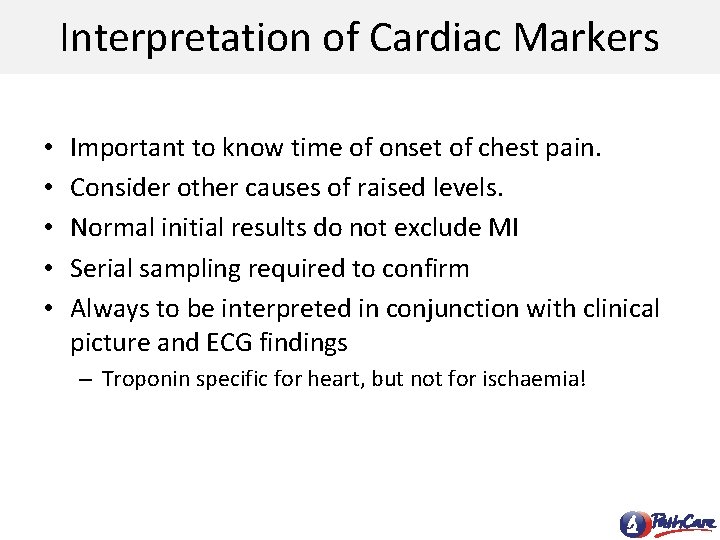
Interpretation of Cardiac Markers • • • Important to know time of onset of chest pain. Consider other causes of raised levels. Normal initial results do not exclude MI Serial sampling required to confirm Always to be interpreted in conjunction with clinical picture and ECG findings – Troponin specific for heart, but not for ischaemia!
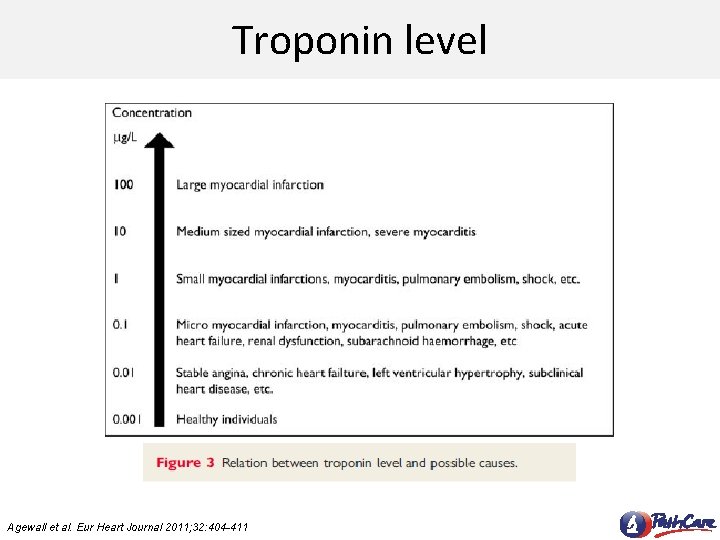
Troponin level Agewall et al. Eur Heart Journal 2011; 32: 404 -411
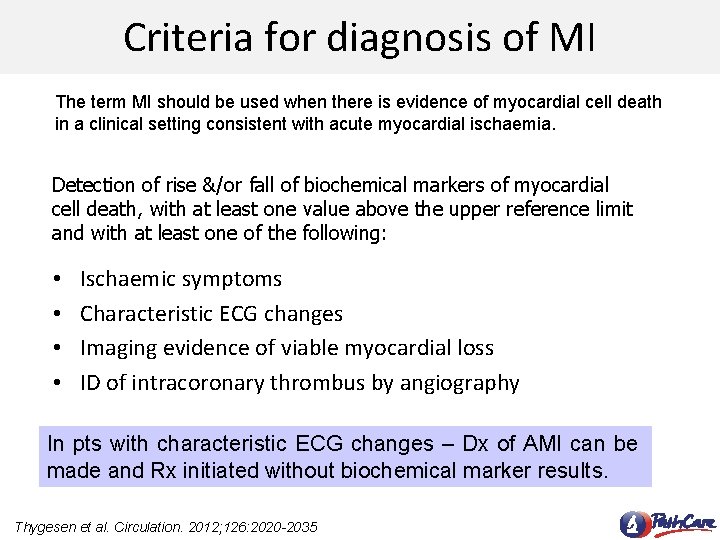
Criteria for diagnosis of MI The term MI should be used when there is evidence of myocardial cell death in a clinical setting consistent with acute myocardial ischaemia. Detection of rise &/or fall of biochemical markers of myocardial cell death, with at least one value above the upper reference limit and with at least one of the following: • • Ischaemic symptoms Characteristic ECG changes Imaging evidence of viable myocardial loss ID of intracoronary thrombus by angiography In pts with characteristic ECG changes – Dx of AMI can be made and Rx initiated without biochemical marker results. Thygesen et al. Circulation. 2012; 126: 2020 -2035
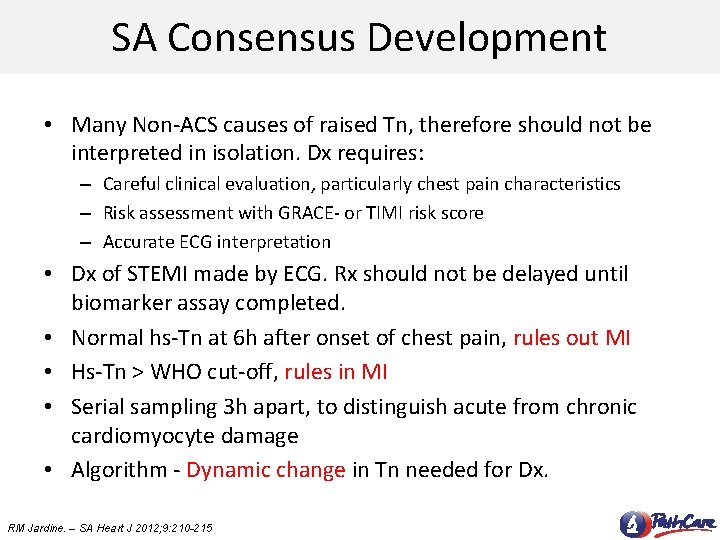
SA Consensus Development • Many Non-ACS causes of raised Tn, therefore should not be interpreted in isolation. Dx requires: – Careful clinical evaluation, particularly chest pain characteristics – Risk assessment with GRACE- or TIMI risk score – Accurate ECG interpretation • Dx of STEMI made by ECG. Rx should not be delayed until biomarker assay completed. • Normal hs-Tn at 6 h after onset of chest pain, rules out MI • Hs-Tn > WHO cut-off, rules in MI • Serial sampling 3 h apart, to distinguish acute from chronic cardiomyocyte damage • Algorithm - Dynamic change in Tn needed for Dx. RM Jardine. – SA Heart J 2012; 9: 210 -215
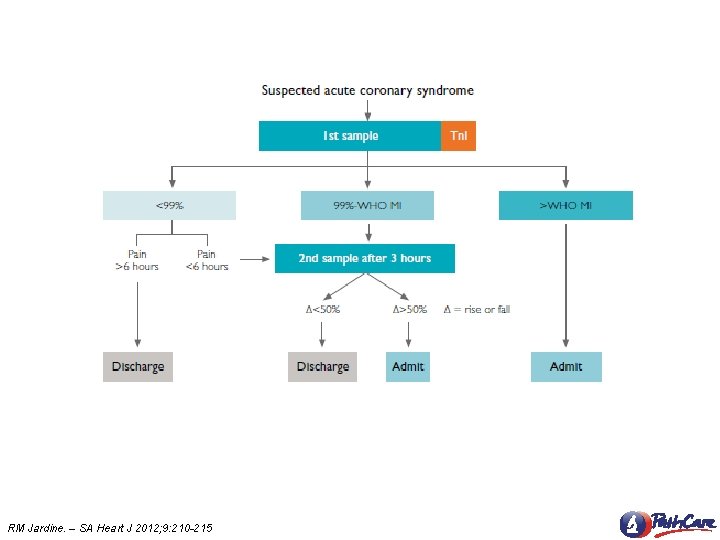
RM Jardine. – SA Heart J 2012; 9: 210 -215
Thank you
- Slides: 22