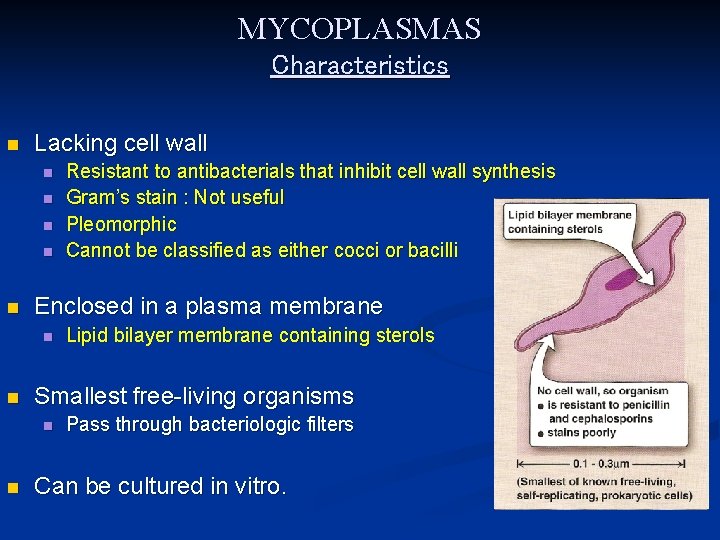
MYCOPLASMAS Characteristics n Lacking cell wall n n





- Slides: 29

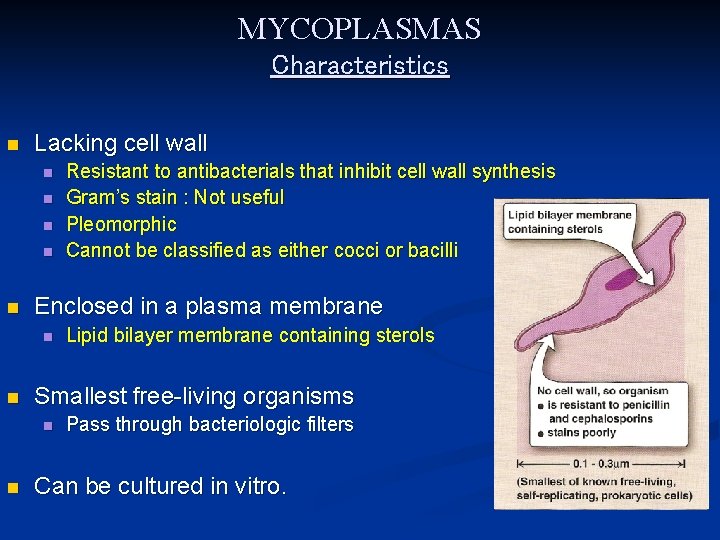
MYCOPLASMAS Characteristics n Lacking cell wall n n n Enclosed in a plasma membrane n n Lipid bilayer membrane containing sterols Smallest free-living organisms n n Resistant to antibacterials that inhibit cell wall synthesis Gram’s stain : Not useful Pleomorphic Cannot be classified as either cocci or bacilli Pass through bacteriologic filters Can be cultured in vitro.
MYCOPLASMAS Mycoplasma pneumoniae → Atypical Pneumonia Mycoplasma hominis → STI: Non-gonococcal Urethritis, Cervicitis, PID Ureaplasma urealyticum → STI: Non-gonococcal Urethritis, Cervicitis, PID
Mycoplasma pneumoniae (Eaton’s reagent) Habitat and Transmission n Habitat is the human respiratory tract. n Transmission : Respiratory droplets.
Mycoplasma pneumoniae Pathogenesis n P 1 adhesion protein n M. pneumoniae binds to respiratory ciliated epithelium Adherence results in ciliostasis & cell destruction → reduced ciliated clearance Bacteria then gain access to the lower respiratory tract n Produces hydrogen peroxide : may damage the respiratory tract. n No exotoxins produced. No endotoxin because there is no cell wall. n
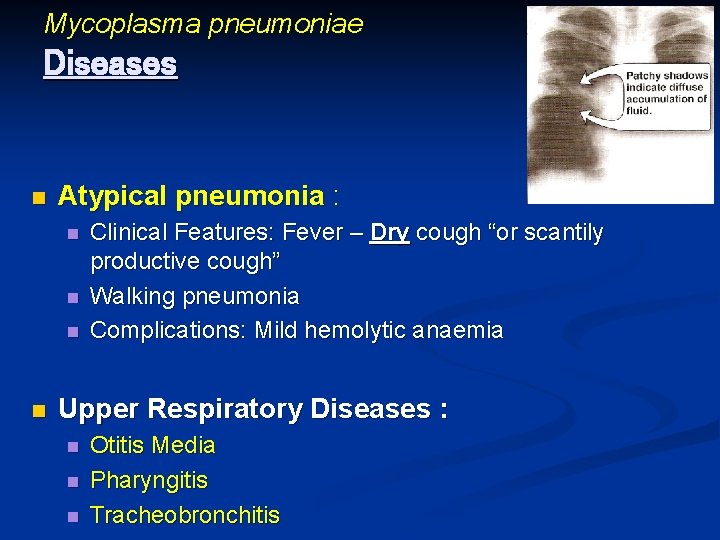
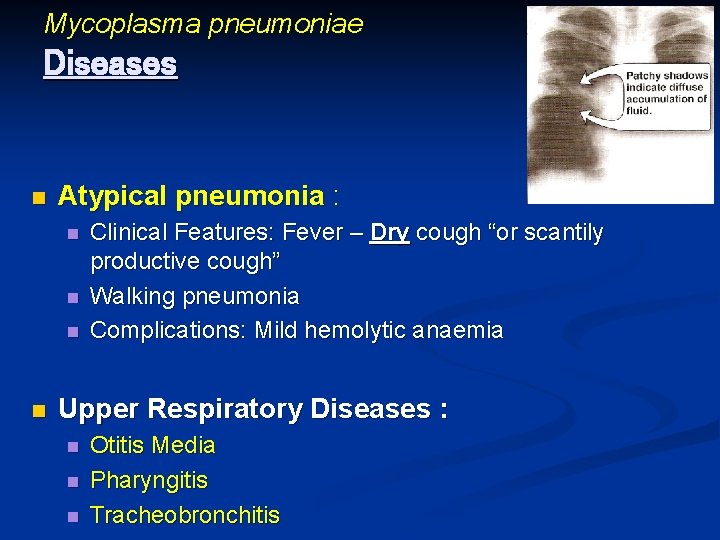
Mycoplasma pneumoniae Diseases n Atypical pneumonia : n n Clinical Features: Fever – Dry cough “or scantily productive cough” Walking pneumonia Complications: Mild hemolytic anaemia Upper Respiratory Diseases : n n n Otitis Media Pharyngitis Tracheobronchitis
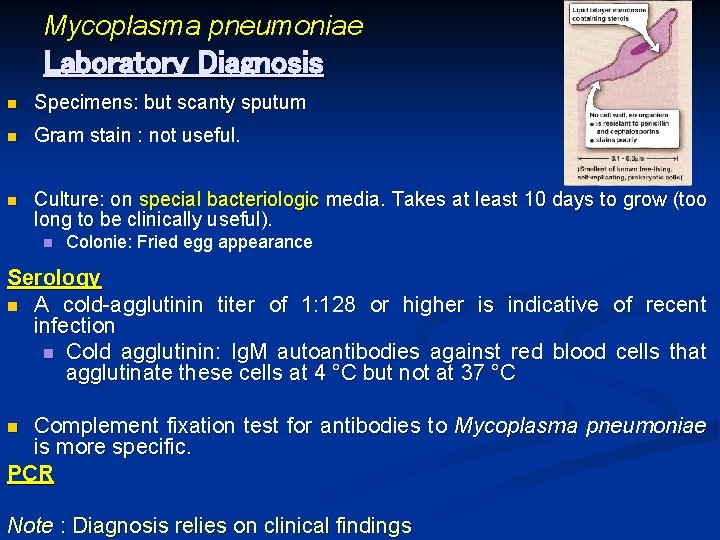
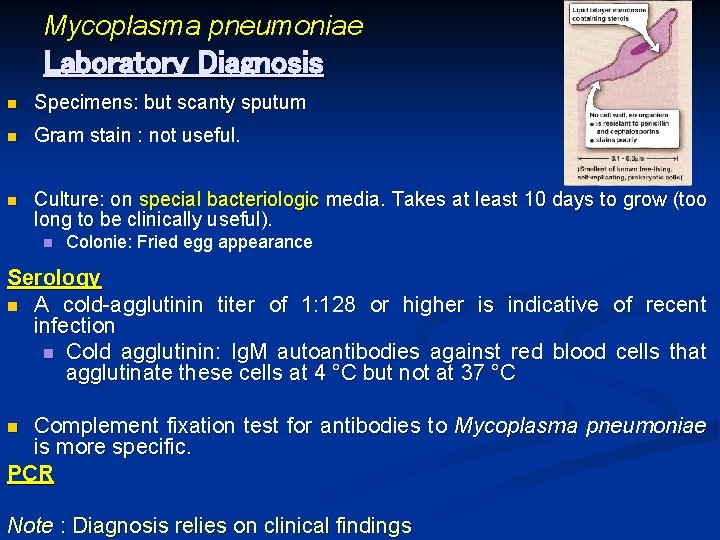
Mycoplasma pneumoniae Laboratory Diagnosis n Specimens: but scanty sputum n Gram stain : not useful. n Culture: on special bacteriologic media. Takes at least 10 days to grow (too long to be clinically useful). n Colonie: Fried egg appearance Serology n A cold-agglutinin titer of 1: 128 or higher is indicative of recent infection n Cold agglutinin: Ig. M autoantibodies against red blood cells that agglutinate these cells at 4 °C but not at 37 °C Complement fixation test for antibodies to Mycoplasma pneumoniae is more specific. PCR n Note : Diagnosis relies on clinical findings
Mycoplasma pneumoniae Treatment n Erythromycin or … n Tetracycline. Prevention n No vaccine or drug is available

Genital Mycoplasmas n Mycoplasma hominis → STD: Non-gonococcal Urethritis, Cervicitis, PID n Ureaplasma urealyticum → STD: Non-gonococcal Urethritis, Cervicitis, PID

Actinomycetes
Actinomycetes n Gram positive bacteria n Filamentous branching bacilli n Superficially resemble fungi on morphologic grounds n They are prokaryotes n Has bacterial size
Actinomycetes n Few are pathogenic to human, the most important are : Actinomyces israelii n Nocardia astroides n
ACTINOMYCETES Actinomyces israelii n Gram-positive filamentous branching bacilli n. Anaerobic n Grows slowly

Actinomyces israelii Habitat and Transmission n Habitat : Found as scanty normal commensal in the: n n n Mouth, especially anaerobic crevices around the teeth Colon Vagina n Disease begins when these normal flora enter adjacent sterile tissue e. g, by trauma, surgery n Transmission into tissues occurs during : n n n Dental extraction - Poor dental hygiene Trauma (mouth – uterus) Organism also aspirated into lungs, causing thoracic actinomycosis.
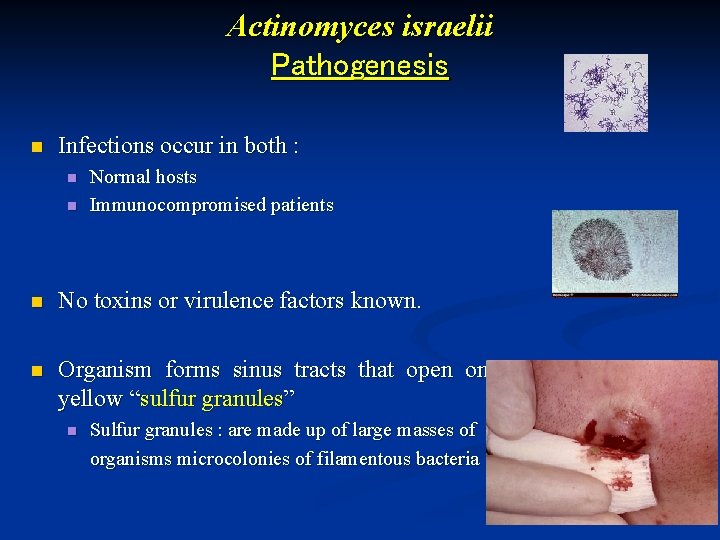
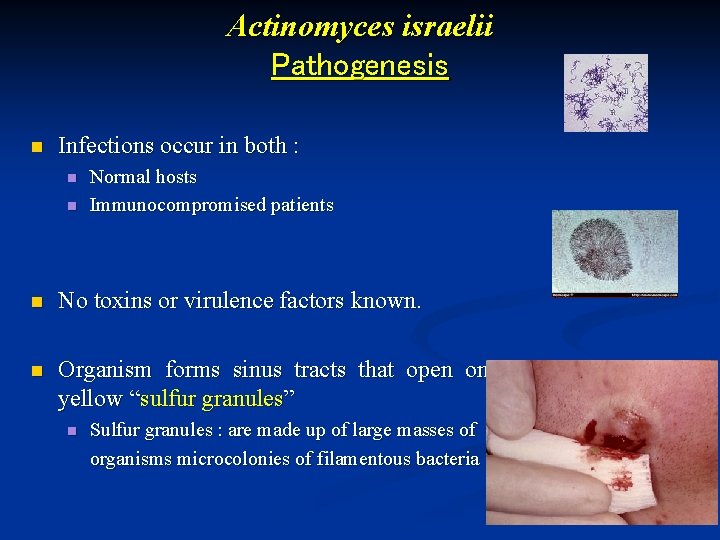
Actinomyces israelii Pathogenesis n Infections occur in both : n n Normal hosts Immunocompromised patients n No toxins or virulence factors known. n Organism forms sinus tracts that open onto skin and contain yellow “sulfur granules” n Sulfur granules : are made up of large masses of organisms microcolonies of filamentous bacteria
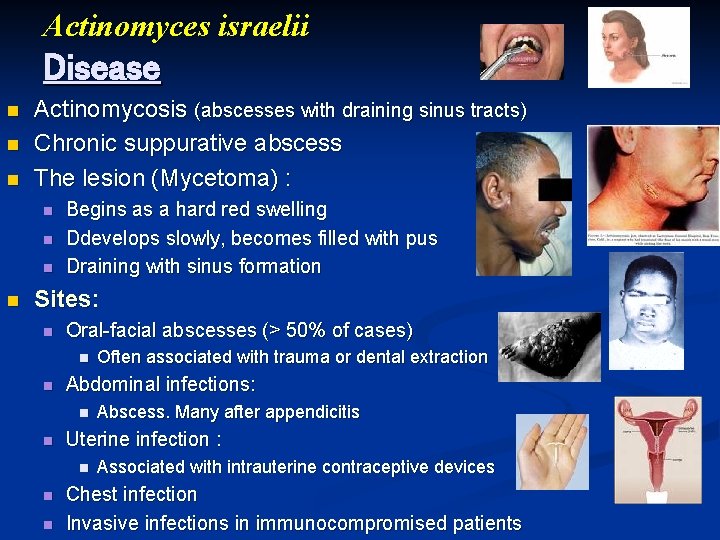
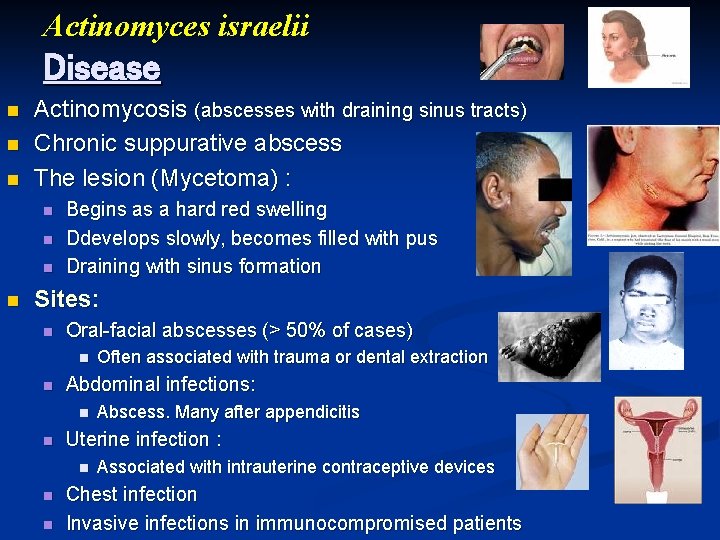
Actinomyces israelii Disease n n n Actinomycosis (abscesses with draining sinus tracts) Chronic suppurative abscess The lesion (Mycetoma) : n n Begins as a hard red swelling Ddevelops slowly, becomes filled with pus Draining with sinus formation Sites: n Oral-facial abscesses (> 50% of cases) n n Abdominal infections: n n n Abscess. Many after appendicitis Uterine infection : n n Often associated with trauma or dental extraction Associated with intrauterine contraceptive devices Chest infection Invasive infections in immunocompromised patients
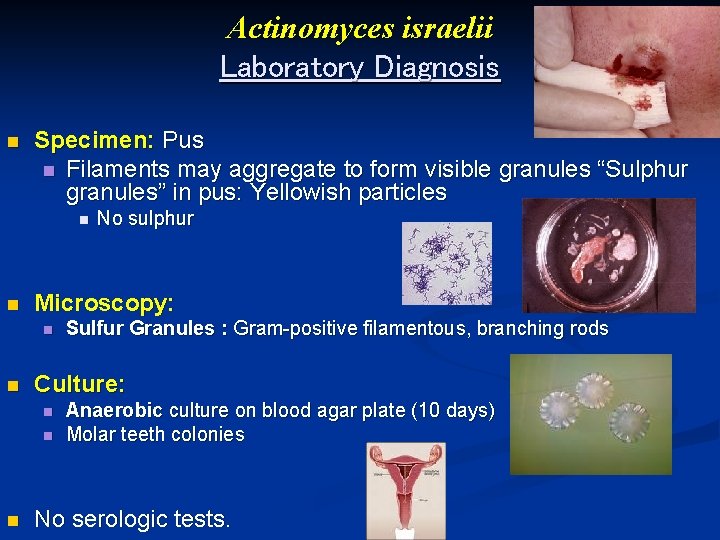
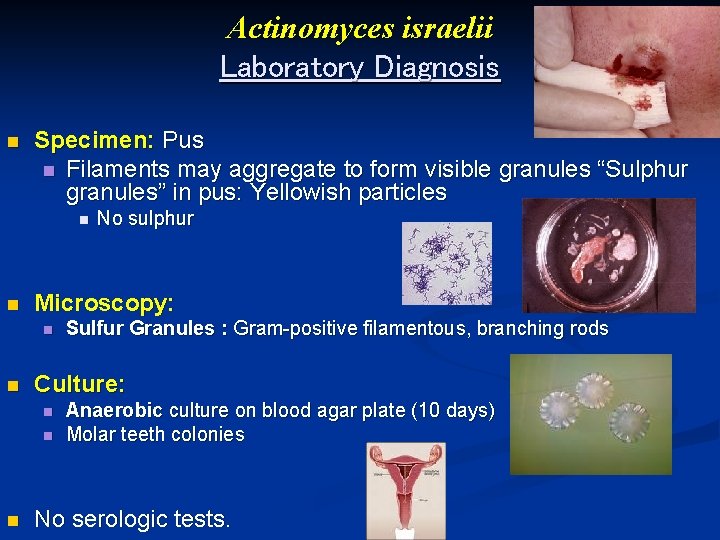
Actinomyces israelii Laboratory Diagnosis n Specimen: Pus n Filaments may aggregate to form visible granules “Sulphur granules” in pus: Yellowish particles n n Microscopy: n n Sulfur Granules : Gram-positive filamentous, branching rods Culture: n n n No sulphur Anaerobic culture on blood agar plate (10 days) Molar teeth colonies No serologic tests.
Actinomyces israelii Treatment n Penicillin n n For up to 3 -12 months Tetracyclin or Clindamycin n For penicillin-allergic patients n Surgical drainage n Prevention n Good oral hygiene Prophylactic antibiotics in association with GIT or oral trauma or surgery No vaccine is available. n n
ACTINOMYCETES Nocardia asteroides
Nocardia asteroides Disease n Nocardiosis (especially lung and brain abscesses).
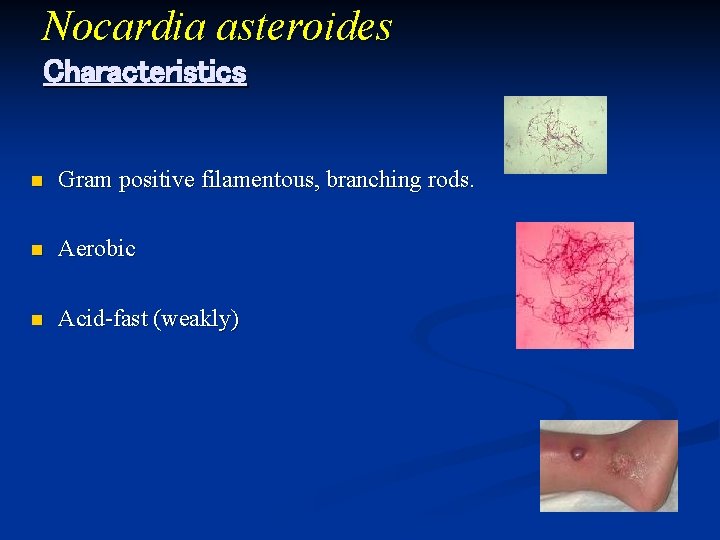
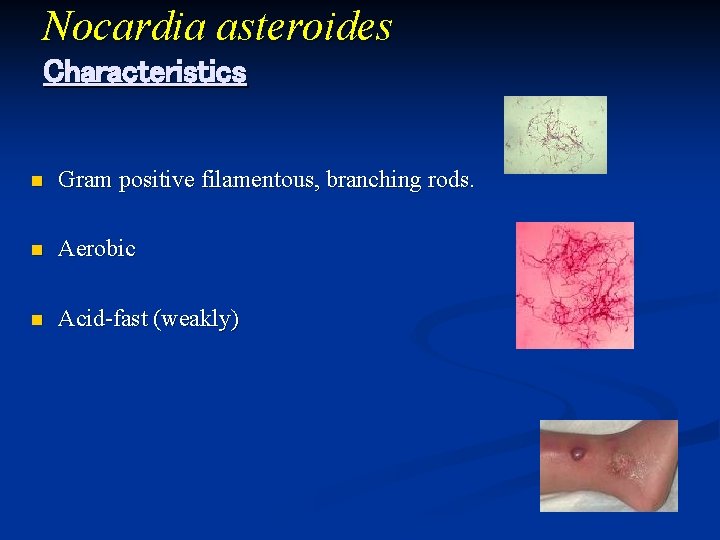
Nocardia asteroides Characteristics n Gram positive filamentous, branching rods. n Aerobic n Acid-fast (weakly)
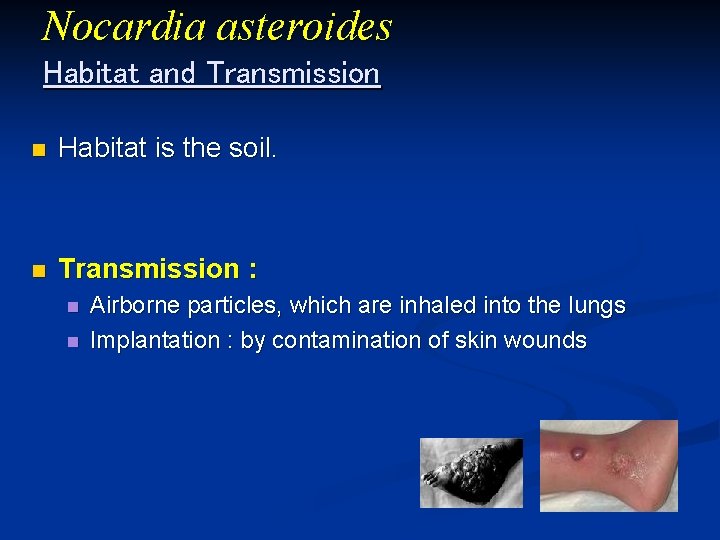
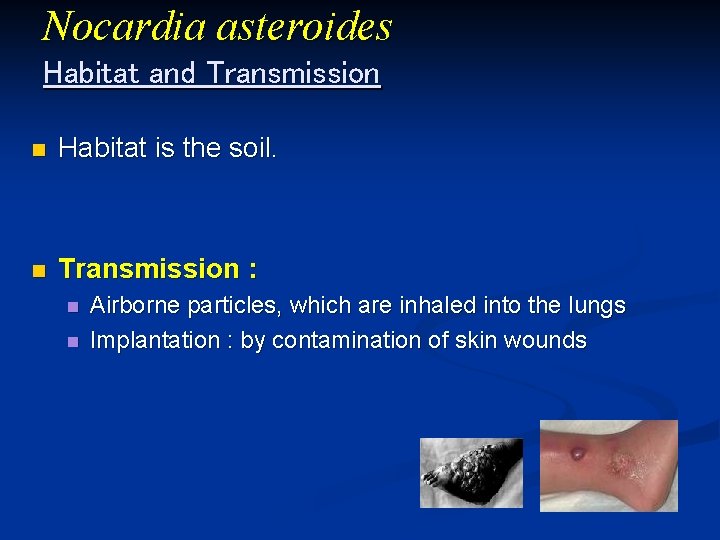
Nocardia asteroides Habitat and Transmission n Habitat is the soil. n Transmission : n n Airborne particles, which are inhaled into the lungs Implantation : by contamination of skin wounds

Nocardia asteroides Pathogenesis n Predisposing Factors: n n Immunosuppression HIV Cancer No toxins or virulence factors known.
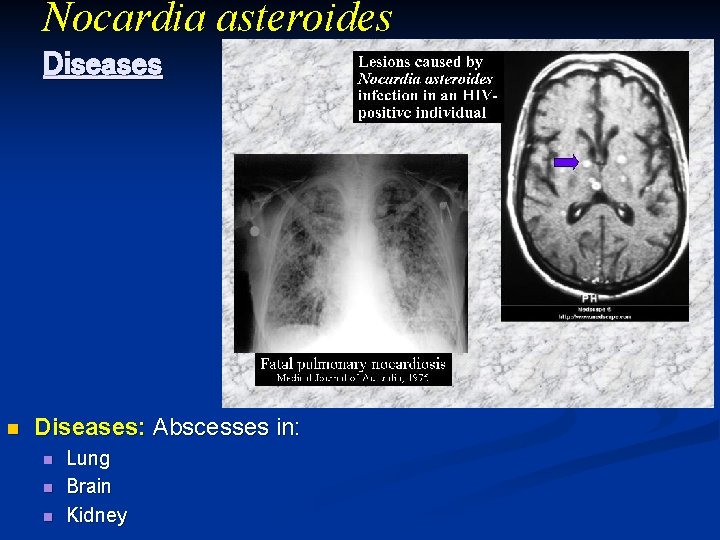
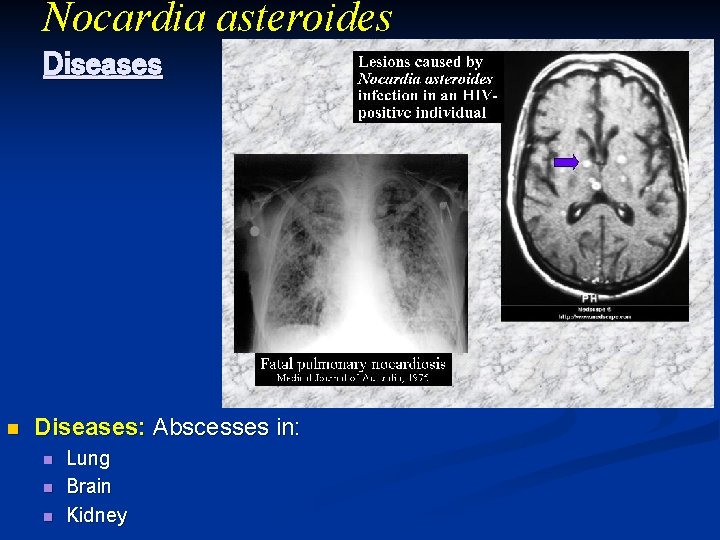
Nocardia asteroides Diseases n Diseases: Abscesses in: n n n Lung Brain Kidney
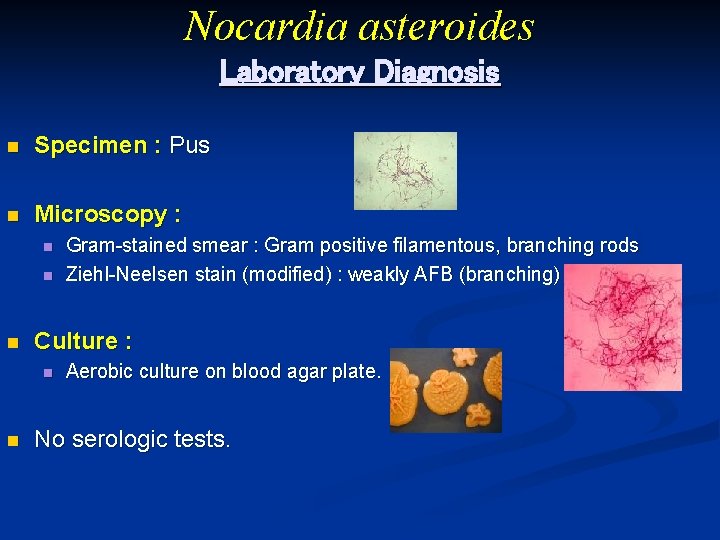
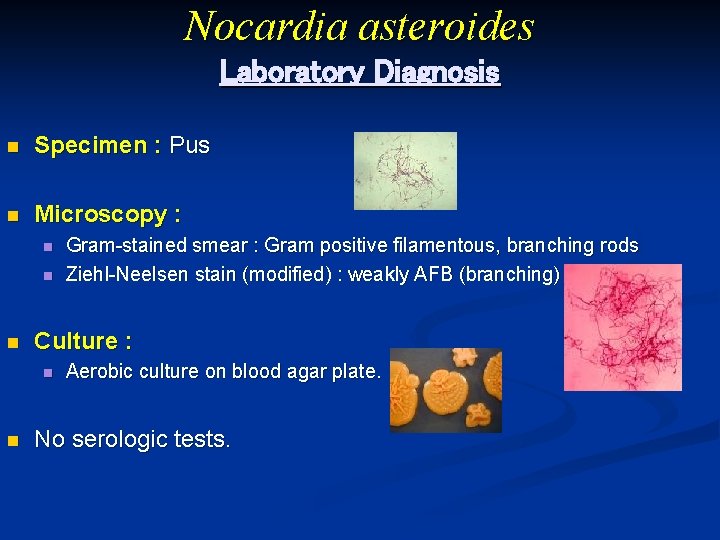
Nocardia asteroides Laboratory Diagnosis n Specimen : Pus n Microscopy : n n n Culture : n n Gram-stained smear : Gram positive filamentous, branching rods Ziehl-Neelsen stain (modified) : weakly AFB (branching) Aerobic culture on blood agar plate. No serologic tests.
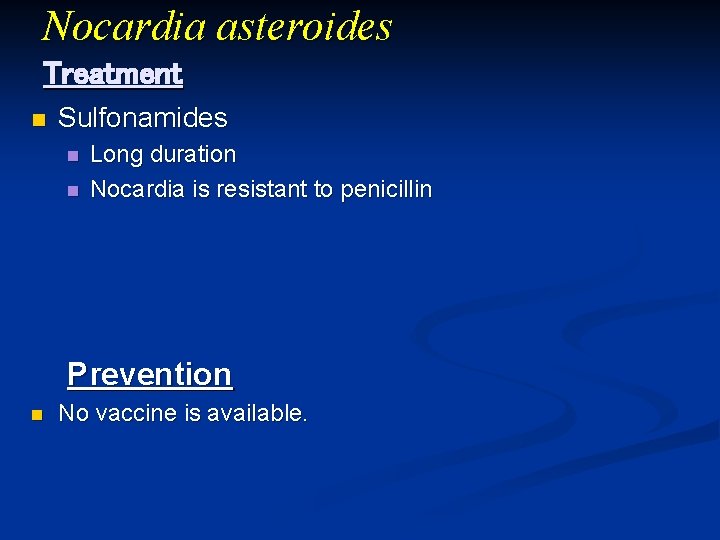
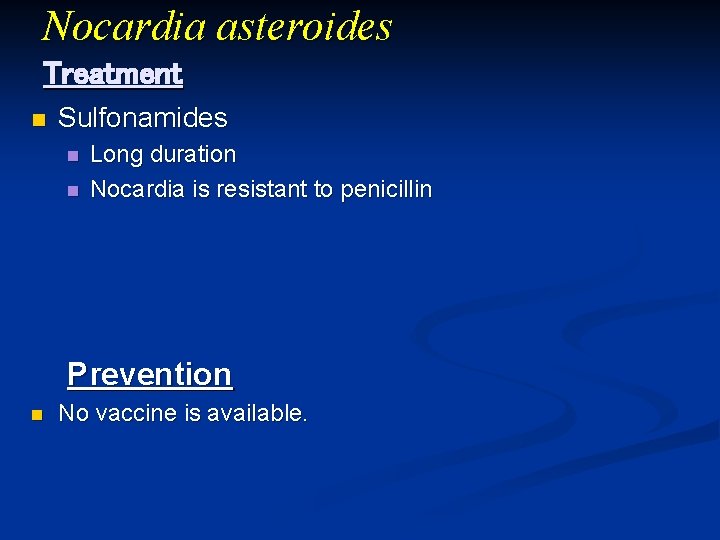
Nocardia asteroides Treatment n Sulfonamides n n Long duration Nocardia is resistant to penicillin Prevention n No vaccine is available.
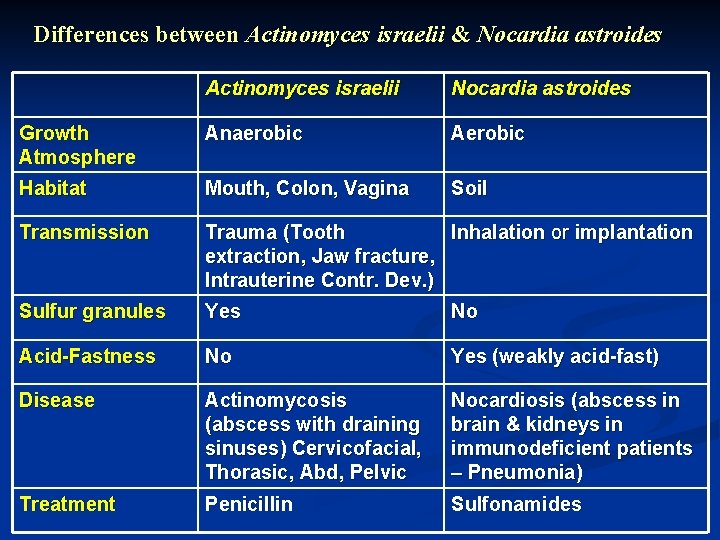
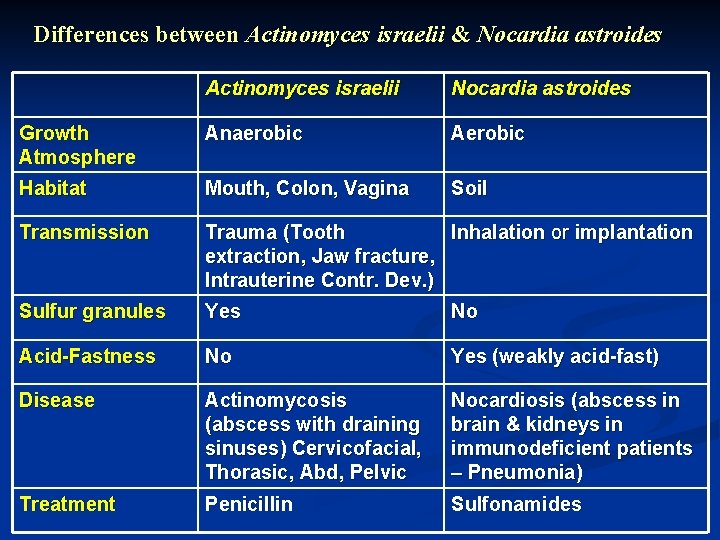
Differences between Actinomyces israelii & Nocardia astroides Actinomyces israelii Nocardia astroides Growth Atmosphere Anaerobic Aerobic Habitat Mouth, Colon, Vagina Soil Transmission Trauma (Tooth Inhalation or implantation extraction, Jaw fracture, Intrauterine Contr. Dev. ) Sulfur granules Yes No Acid-Fastness No Yes (weakly acid-fast) Disease Actinomycosis (abscess with draining sinuses) Cervicofacial, Thorasic, Abd, Pelvic Nocardiosis (abscess in brain & kidneys in immunodeficient patients – Pneumonia) Treatment Penicillin Sulfonamides