MYCOPLASMA AND UREAPLASMA MYCOPLASMA Smallest lack cell freeliving

- Slides: 30
MYCOPLASMA AND UREAPLASMA
MYCOPLASMA Smallest lack cell free-living micro organisms wall. Size: Varies from spherical shape (125 -250 nm to longer branching filaments 500 -1000 nm in size. Pass through a bacterial filter. Isolated by Nocard & Roux (1898) –bovine pleuropneumonia (PPO)

PLEUROPNEUMONIA LIKE ORGANISMS”(PPLO) Later, many similar isolates were obtained from animals, human beings, plants & environmental sources – called as “Pleuropneumonia like organisms”(PPLO).
MYCOPLASMA Eaton (1944) first isolated the causative agent of the disease in hamsters and cotton rats. Also known as Eaton agent. 1956 - PPLO replaced by Mycoplasma. Myco : fungus like branching filaments Plasma : plasticity highly pleomorphic – no fixed shape or size - Lack cell wall.
MORPHOLOGY AND PHYSIOLOGY Require complex media for growth Facultative aerobe • anaerobes: Except M. pneumoniae - strict No cell wall means these are slow growing & resistant to penicillins, cephalosporins and vancomycin, etc.
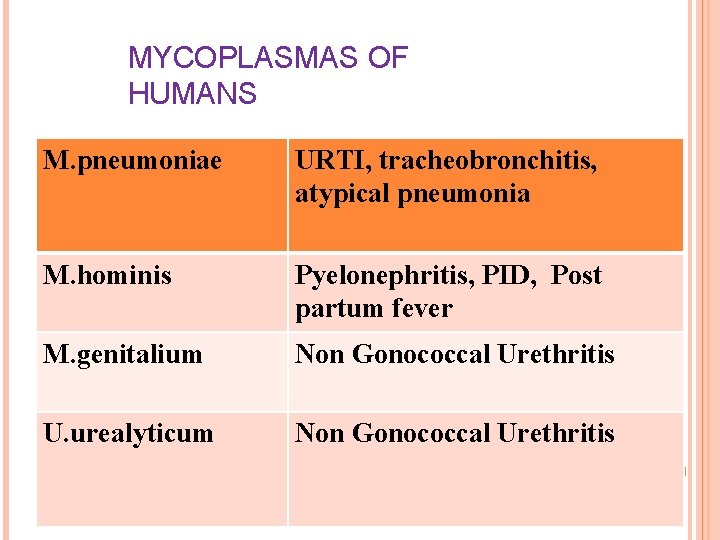
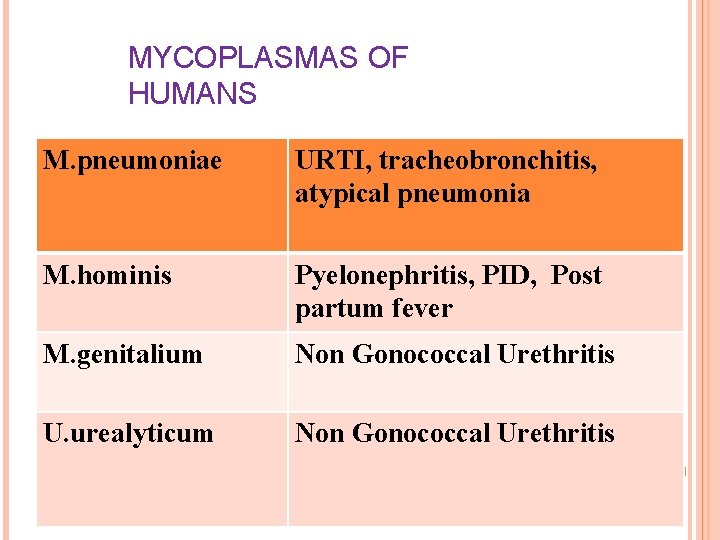
MYCOPLASMAS OF HUMANS M. pneumoniae URTI, tracheobronchitis, atypical pneumonia M. hominis Pyelonephritis, PID, Post partum fever M. genitalium Non Gonococcal Urethritis U. urealyticum Non Gonococcal Urethritis
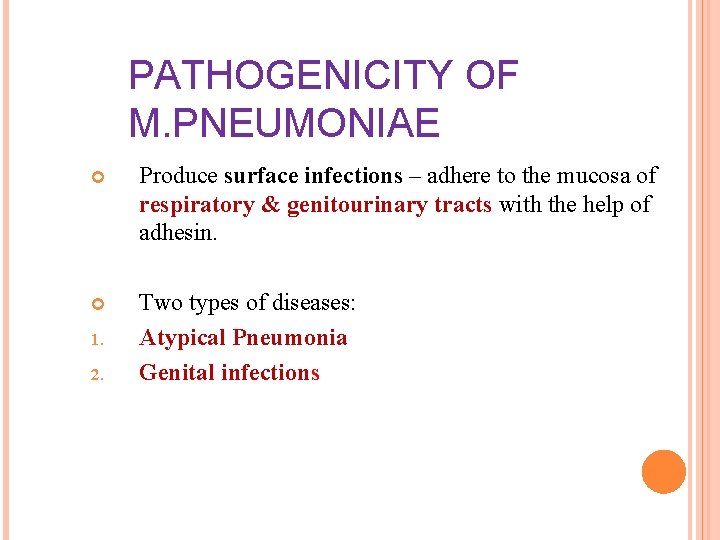
PATHOGENICITY OF M. PNEUMONIAE Produce surface infections – adhere to the mucosa of respiratory & genitourinary tracts with the help of adhesin. Two types of diseases: Atypical Pneumonia Genital infections 1. 2.
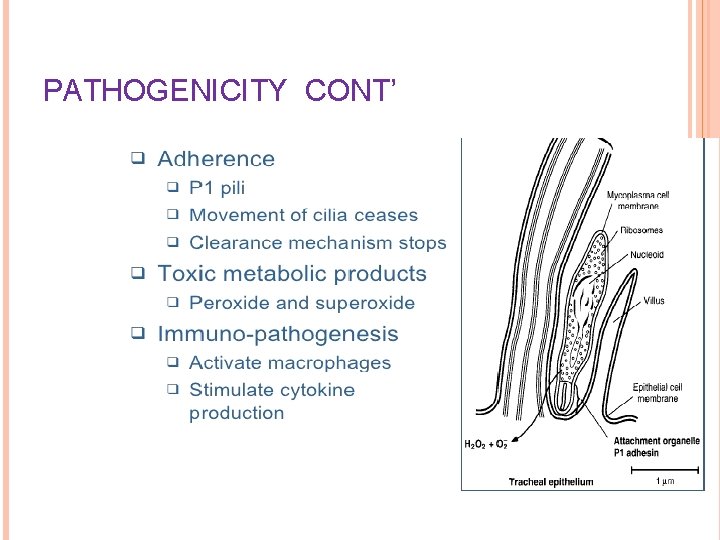
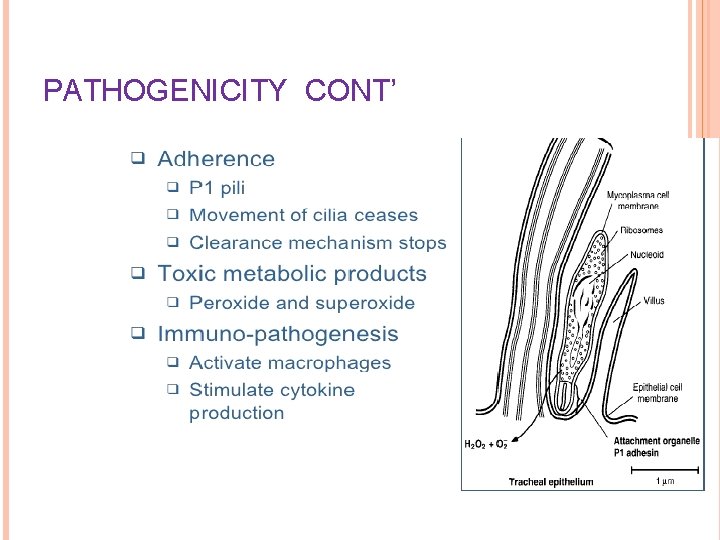
PATHOGENICITY CONT’
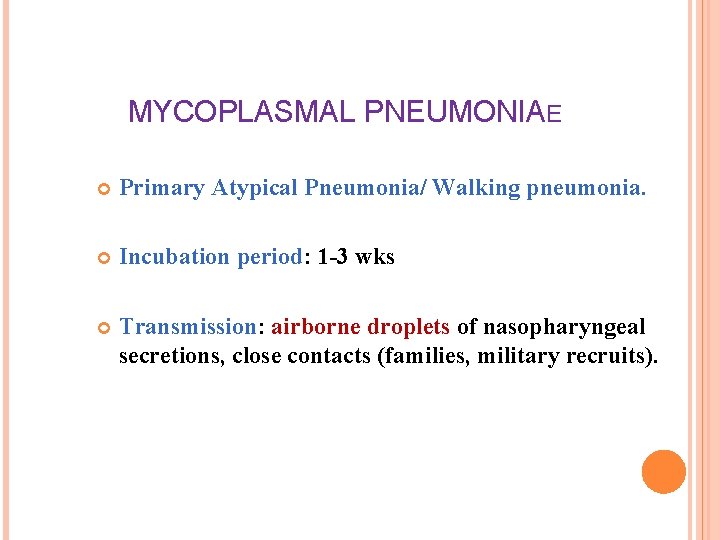
MYCOPLASMAL PNEUMONIAE Primary Atypical Pneumonia/ Walking pneumonia. Incubation period: 1 -3 wks Transmission: airborne droplets of nasopharyngeal secretions, close contacts (families, military recruits).
PRIMARY ATYPICAL PNEUMONIA Gradual onset with fever, malaise, chills, headache & sore throat. Severe cough with blood tinged sputum (worsens at night) Complications: bullous myringitis & otitis, meningitis, encephalitis, hemolytic anemia
CLINICAL SYNDROME - M. PNEUMONIAE Incubation - 2 -3 weeks Fever, headache, malaise, persistent, dry, nonproductive cough Respiratory symptoms Patchy bronchopneumonia acute pharyngitis may be present Organisms persist, Slow resolution, Rarely fatal
EPIDEMIOLOGY - M. PNEUMONIAE Occurs worldwide, No seasonal variation Proportionally higher in summer and fall Epidemics Spread occur every 4 -8 year by aerosol route (Confined populations). Disease of the young (5 -20 years), although all ages are at risk
LABORATORY DIAGNOSIS Specimens – throat swabs, respiratory secretions. Microscopy – Highly pleomorphic, varying from small spherical shapes to longer branching filaments. 1. 2. Gram negative, but better stained with Giemsa stain
LABORATORY DIAGNOSIS - M. PNEUMONIAE Culture (definitive diagnosis) Sputum (usually scant) or throat washings 1. 2. 3. Isolation of Mycoplasma (Culture) – Semi solid enriched medium containing 20% horse or human serum, yeast extract & DNA. Penicillium & Thallium acetate are selective agents. PPLO MEDIUM Incubate aerobically for 7 -12 days with 5– 10% CO 2 at 35 -37°C. Colonies seen using hand lens or Dienes staining: alcoholic solution of methylene blue & azure
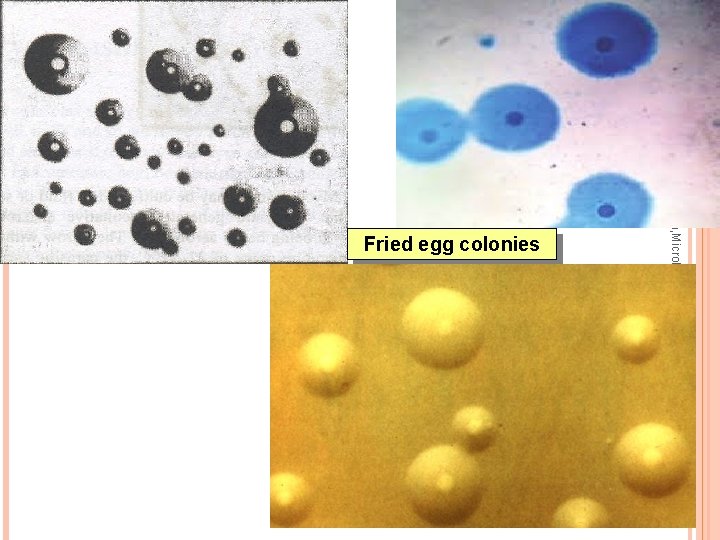
LABORATORY DIAGNOSIS Typical “FRIED EGG” appearance of colonies Central opaque granular area of growth extending into the depth of the medium, surrounded by a flat, translucent peripheral zone.
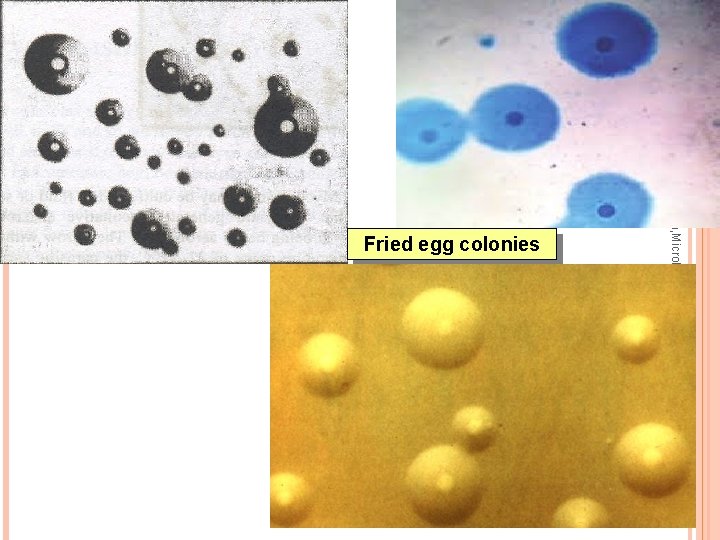
Dr Ekta, Microbiology, GMCA Fried egg colonies
IDENTIFICATION OF ISOLATES Growth Inhibition Test – inhibition of growth around discs impregnated with specific antisera. Immuno-fluorescence on colonies transferred to glass slides. Molecular diagnosis: PCR-based tests
IDENTIFICATION OF ISOLATES 1. Serological diagnosis Specific tests – IF, HAI 2. Non specific serological tests – cold agglutination tests (Abs agglutinate human group O red cells at low temperature, 4 C). 1: 32 titer or above is significant.
TREATMENT AND PREVENTION M. PNEUMONIAE Macrolides are DOC (Azithromycin) Other antibiotics: Tetracycline in adults (doxycycline) or erythromycin (children) Newer fluoroquinolones (in adults) Prevention Avoid close contact
UREAPLASMA UREALYTICUM M. hominis, M. genitaliulium, Ureaplasma: cause urogenital infections Colonize female lower urogenital tract Transmission: sexual contact/ to fetus during birth
GENITAL INFECTIONS Men - Nonspecific urethritis, proctitis, balanoposthitis & Reiter’s syndrome Women vaginitis Also – acute salpingitis, PID, cervicitis, associated with infertility, abortion, postpartum fever, chorioamnionitis & low birth weight infants
TREATMENT: Macrolides: (azithromycin) for Ureaplasma & M. genitalium infections Doxycycline : M. hominis
MYCOPLASMA AS CELL CULTURE CONTAMINANTS Contaminates continuous cell cultures maintained in laboratories Interferes with the growth of viruses in these Mistaken for viruses. cultures. Eradication from infected cells is difficult.
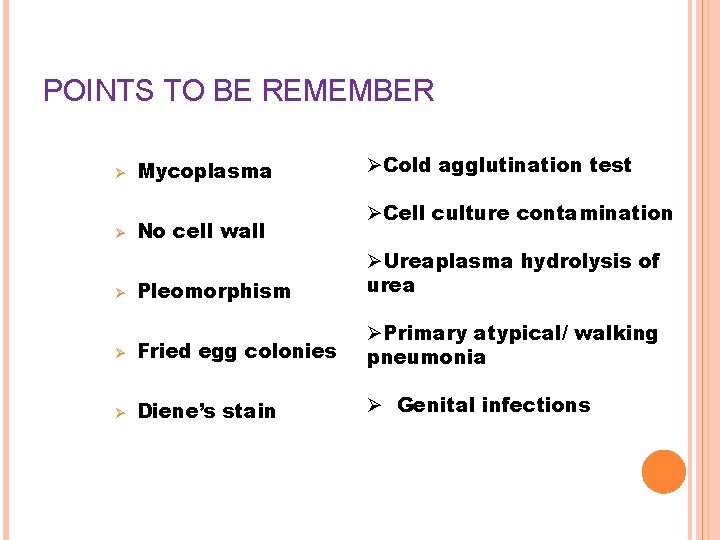
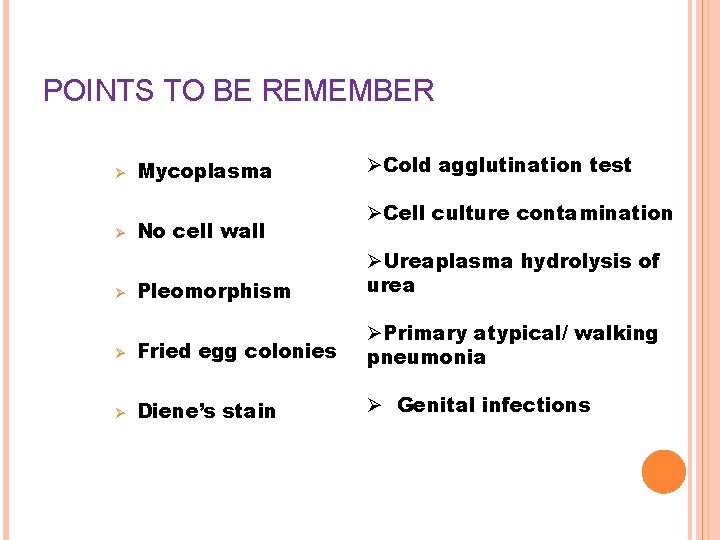
POINTS TO BE REMEMBER Ø Ø Mycoplasma No cell wall ØCold agglutination test ØCell culture contamination Pleomorphism ØUreaplasma hydrolysis of urea Ø Fried egg colonies ØPrimary atypical/ walking pneumonia Ø Diene’s stain Ø Genital infections Ø
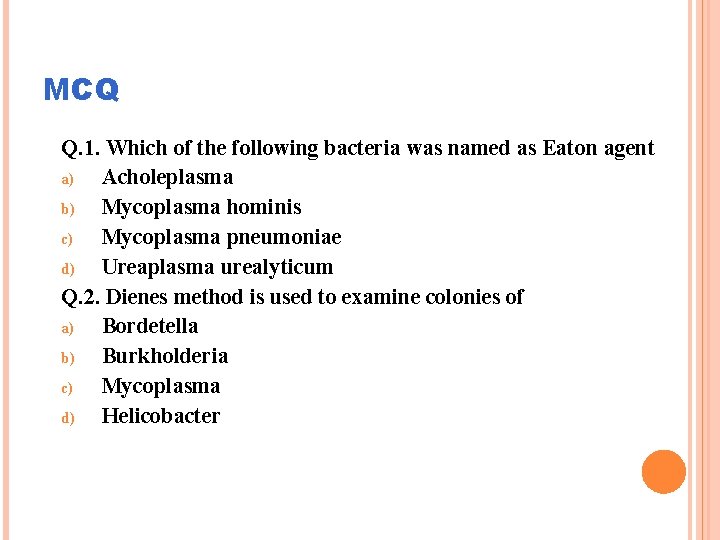
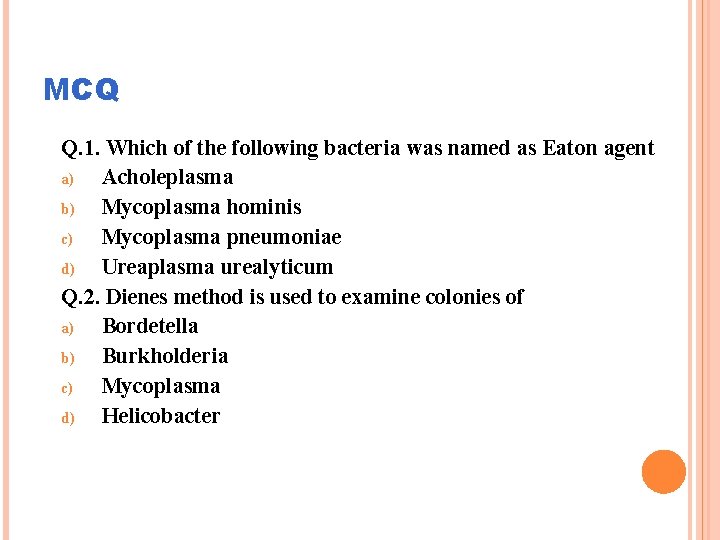
MCQ Q. 1. Which of the following bacteria was named as Eaton agent a) Acholeplasma b) Mycoplasma hominis c) Mycoplasma pneumoniae d) Ureaplasma urealyticum Q. 2. Dienes method is used to examine colonies of a) Bordetella b) Burkholderia c) Mycoplasma d) Helicobacter
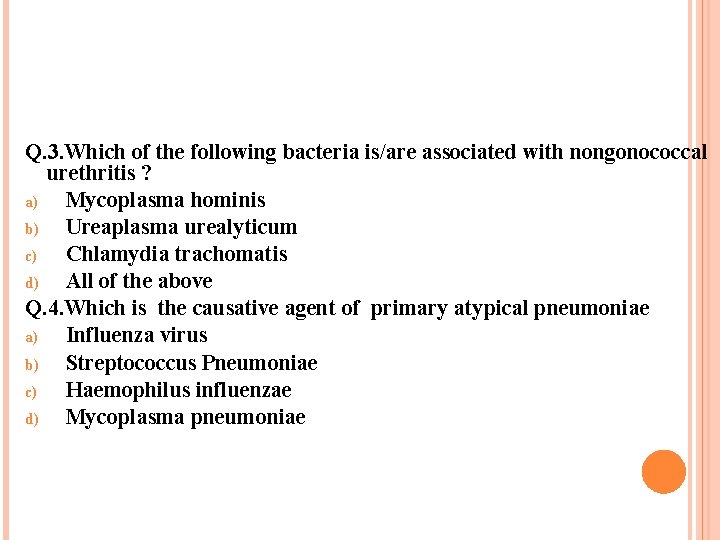
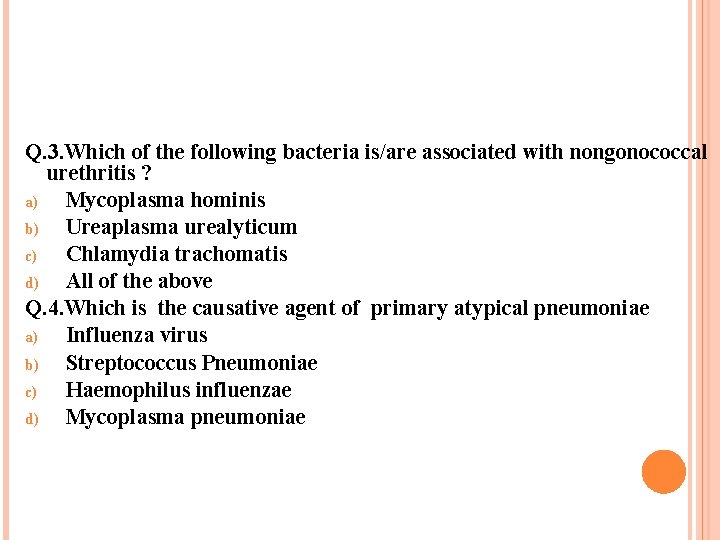
Q. 3. Which of the following bacteria is/are associated with nongonococcal urethritis ? a) Mycoplasma hominis b) Ureaplasma urealyticum c) Chlamydia trachomatis d) All of the above Q. 4. Which is the causative agent of primary atypical pneumoniae a) Influenza virus b) Streptococcus Pneumoniae c) Haemophilus influenzae d) Mycoplasma pneumoniae
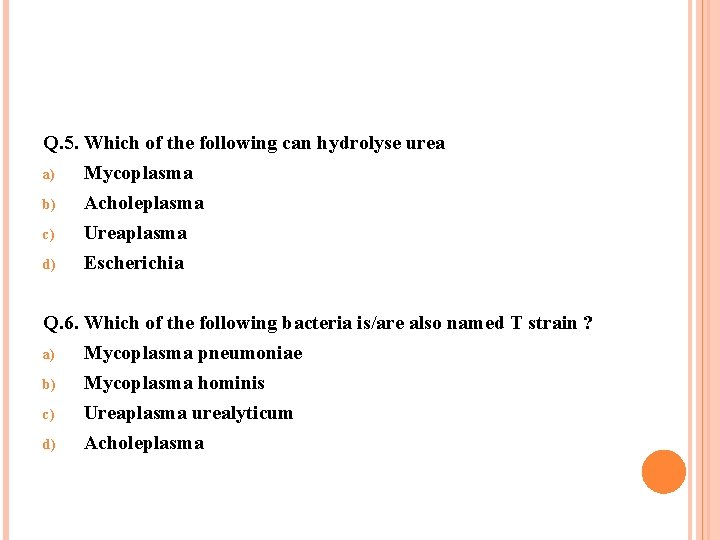
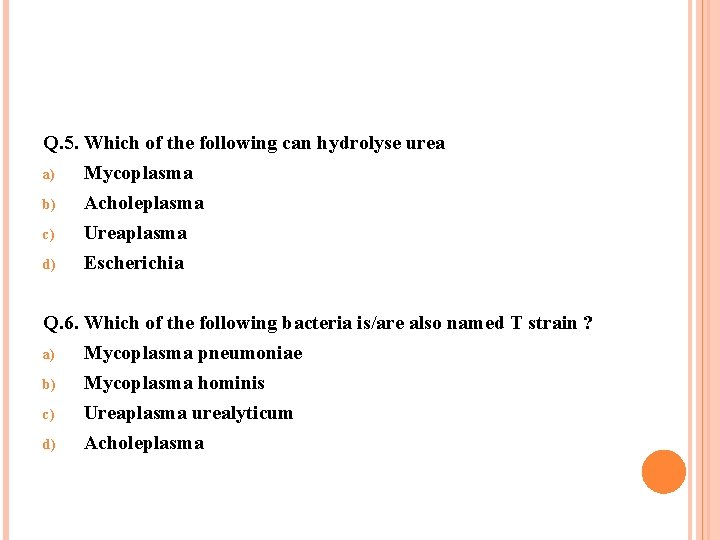
Q. 5. Which of the following can hydrolyse urea a) Mycoplasma b) Acholeplasma c) Ureaplasma d) Escherichia Q. 6. Which of the following bacteria is/are also named T strain ? a) Mycoplasma pneumoniae b) Mycoplasma hominis c) Ureaplasma urealyticum d) Acholeplasma
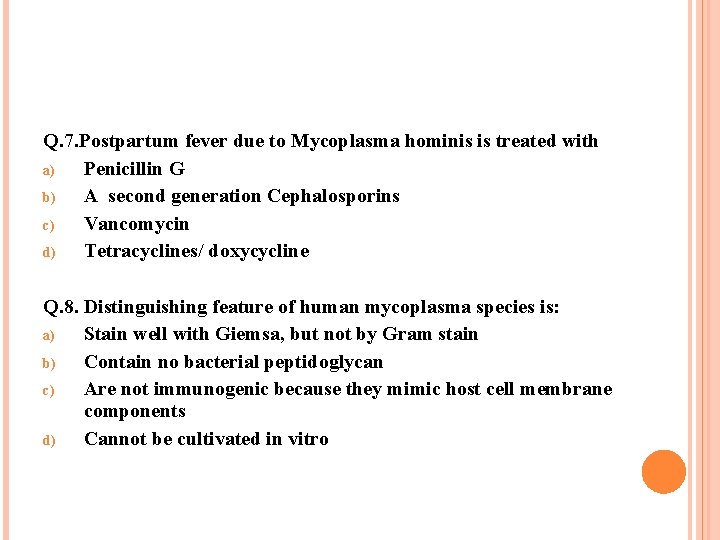
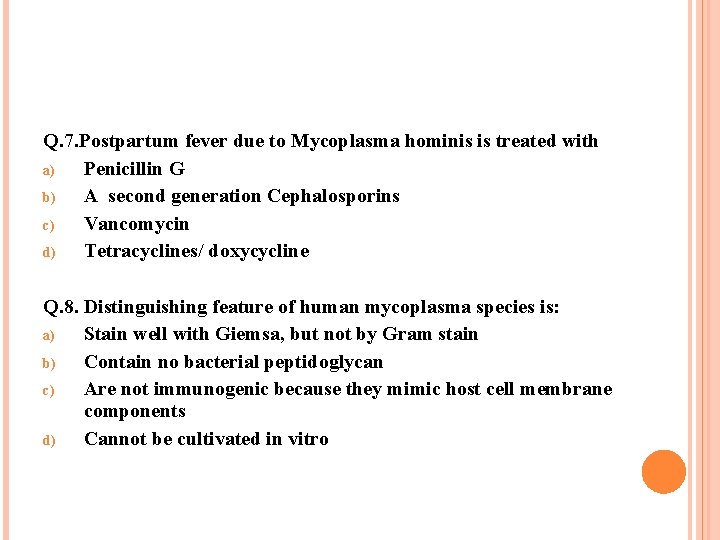
Q. 7. Postpartum fever due to Mycoplasma hominis is treated with a) Penicillin G b) A second generation Cephalosporins c) Vancomycin d) Tetracyclines/ doxycycline Q. 8. Distinguishing feature of human mycoplasma species is: a) Stain well with Giemsa, but not by Gram stain b) Contain no bacterial peptidoglycan c) Are not immunogenic because they mimic host cell membrane components d) Cannot be cultivated in vitro
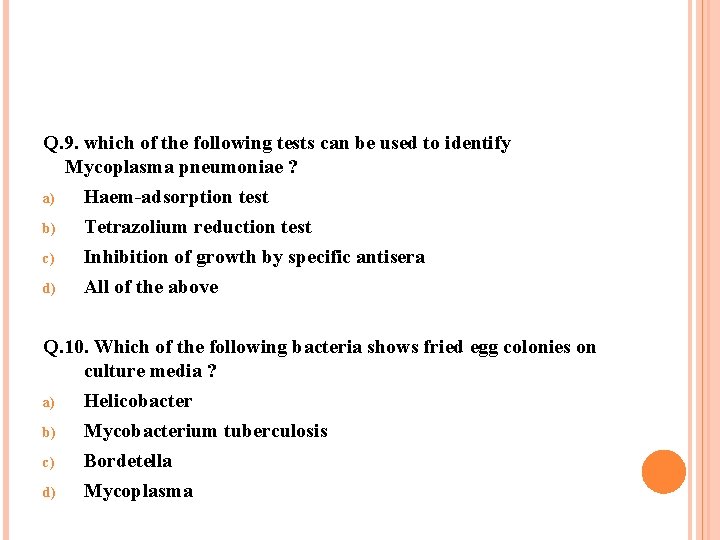
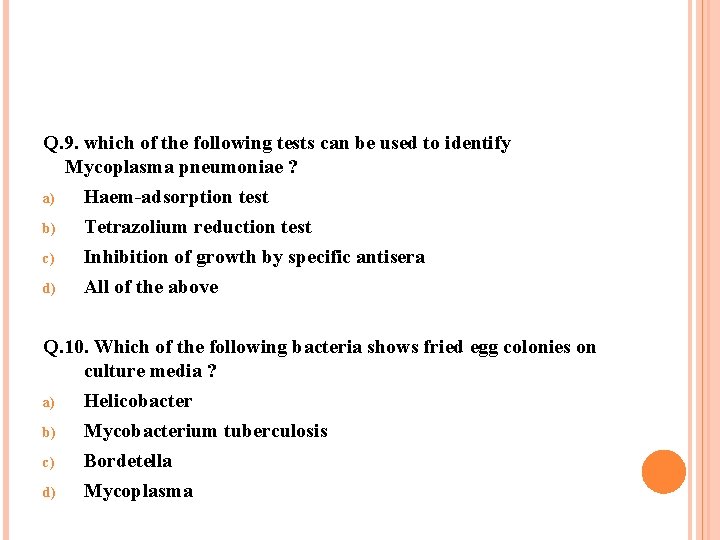
Q. 9. which of the following tests can be used to identify Mycoplasma pneumoniae ? a) Haem-adsorption test b) Tetrazolium reduction test c) d) Inhibition of growth by specific antisera All of the above Q. 10. Which of the following bacteria shows fried egg colonies on culture media ? a) Helicobacter b) Mycobacterium tuberculosis c) Bordetella d) Mycoplasma
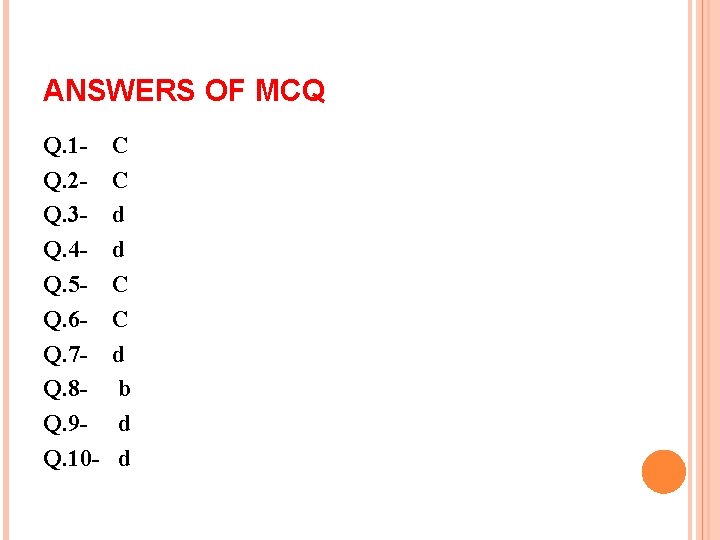
ANSWERS OF MCQ Q. 1 Q. 2 Q. 3 Q. 4 Q. 5 Q. 6 Q. 7 Q. 8 Q. 9 Q. 10 - C C d d C C d b d d